Addressing sexual pain,
anxiety and pelvic floor
dysfunction with
physical therapy
Talli Y. Rosenbaum, MSc., PT,
IF
AASECT Certified Sex Therapist
www.tallirosenbaum.com
Pain with
arousal/orgasm/clitorodynia
*common cause of superficial dyspareunia in women in their
childbearing years affecting estimated 12 -21% of women
(Laumann,1999 Danielson,2003 Harlow, 2008)
Question #1
Vaginismus and localized provoked vulvodynia
are two distinctly separate clinical entities
which require different treatment approaches
A. True
B. False
Overlap in conditions
• DSM V : genito-pelvic pain/penetration disorder
(Binik, et al 2011)
• Pain and anxiety are components of both
vaginismus and PVD (Watts & Nettle ,2012, Khandker, et al,
2012)
• Increase in pelvic floor hyperactivity is
component of both conditions (Van der Velde, 2007,
Reissing, 2005, Gentilcore-Saulnier, 2010, Rosenbaum, 2007) as well
as IC/PBS ( Bassaly, R.et al, 2010).
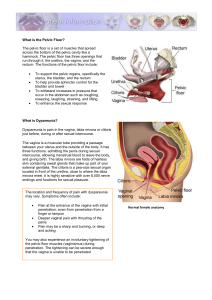
The Pelvic Floor
• Maintains continence
• Supports pelvic
organs
• Plays a role in sexual
function
• Functional definitions
of normal, overactive,
underactive, or nonfunctioning (Messelink,
2005)
Pelvic floor dysfunction
and sexual pain
• PF overactivity is a component of pelvic and
genital pain (Tu, 2008, Reissing, 2005 Engman, 2004)
• Affects blood supply to the vulva affecting genital
arousal and lubrication
• Inadequate lubrication, increased friction,
fissures, and more pain
• Superficial and deep pelvic pain with intercourse
Physiotherapists as PF
rehab specialists
• PF as part of an
integrated unit
• Breathing, posture, joint
mobility, trunk and
extremity strength and
length may affect IAP,
continence, prolapse
and pelvic pain.
Physical Therapy
• Musculoskeletal aspects and myofascial
components
• Exercise
• Pelvic floor relaxation
• Biofeedback
• Electrical stimulation
• Dilator therapy
• Manual therapy
• Dry needling
The biopsychosocial model
Physician
Psychologist
Sex therapist
Vaginismus
Dyspareunia
Physiotherapist
Designate:
• the psycho-social aspects including anxiety and
aversion, to mental health professionals (MHPs).
• the physiological aspects of treatment to medical
professionals (MPs)
• PT addresses the pelvic floor
Question #2
The ideal model for multidisciplinary
management of SPD is that physicians diagnose
and treat medically, mental health professionals
address anxiety and other psychosexual
components, and physiotherapists treat muscles.
A. True
B. False
Problem with this model
•Anxiety and aversion to touch are significant
characteristics of the patient’s response to physical
examination and treatment, mirroring the sexual
setting
•Disassociation and triggering of trauma are most
likely to occur in this setting.
•Home program may not be appropriate
•Sexual counseling is often appropriate
The pelvic floor
• Hyperactivity of the pelvic floor is not simply an
isolated dysfunction, but a physical
manifestation of the patient’s emotional state.
(Rosenbaum, 2012)
• Increased PF activity as a defensive reaction. (
Van der Velde et al.,2001.)
• Trait anxiety/habits affect baseline tone (Anderson,
Wise, 1993)
• 3 or more PF symptoms related to sexual abuse
(Beck, et al, 2009)
• Guilt, responsibility, lack of autonomy
• Expression of
emotional state
• Soft tissue: introitus,
mucosal dryness
• Orthopedic (trigger
points)
• Neurological
• Visceral
Question #3
A hip pathology may result in dyspareunia.
A. True
B. False
Orthopedic and neurological
contributors
• The back: OA, disc,
scoliosis, coccydynia,
SI, pubic symphysis
• Hips: labral tears,
femoro-acetabular
impingement
• Pudendal or other
nerve involvement
(lat fem cutaneous,
obturator, ilioinguinal)
The PT Exam
• History
• Observation of gait
and movement
patterns
• Musculoskeletal/
postural evaluation
• Vulvar and vaginal
exam
• Pelvic floor
assessment
Measuring the Pelvic Floor
• Most scales measure PF symptoms (van Lunsen, 2002,
Laan, in prep)
•
•
•
•
Visual and digital assessment
sEMG
Dynamometric speculum (Morin, 2006)
Ultrasound (Braaken, 2009, )
Measurement problems
• Valid and reliable tools are
lacking
• Manual examination is
subjective and difficult to
standardize particularly
with high tone and anxiety
• sEMG unreliable: Contact
mucosa, degree of
lubrication and thickness of
the vaginal tissue can all
greatly affect signal
detection (Merletti, 2004)
Techniques to address anxiety
• Explain everything you are about to do before
you do it
• Always ask permission
• Maintain eye contact
• Be alert for signs of dissociation
• OK to stop at any time
• Awareness of conflict between thoughts and
emotions
Pelvic Floor Manual Examination:
gold standard
• Awareness and ability to
isolate muscles
• Balance and symmetry
• Muscle tension/ muscle
stiffness
• Presence of trigger points
and pattern of referral
• Dysenergy
• Strength: force, lift, no.,
duration
Hartmann, D 2010
Mindfulness based intervention
• Lying on the bed fully
dressed, covered with
a sheet
• Bend knees and
separate legs
• Self rate anxiety
• Increasing exposure:
shorts, underwear, no
underwear with and
without sheet
(Rosenbaum, 2011)
Mindful dilator exercises
•
•
•
•
•
•
•
Not just about insertion and containment
Stay present
Feel the pelvic floor relax and the vagina open
Wait until your vagina lets it in
Be aware and accept anxious feelings
Do not judge the pain
Gradual trust
Question #4
Physical therapy for the pelvic floor does NOT
typically involve:
A. Biofeedback
B. Behavioral therapy
C. Relaxation techniques
D. Manual Therapy
E. Acupuncture
Manual therapy
• Facilitate muscle relaxation, normalize tone, and improve
circulation and mobility in the pelvic and genital region
(Rosenbaum, 2005, Kotararinos, 2003)
• Pelvic and vaginal trigger point massage described in
the treatment of pelvic pain and IC (Weiss, 2001)
• Improved irritative bladder symptoms and decreased
PFM tone (n=21) IC/PBS (Oyama, 2006)
• Randomized multi-center feasibility trial of myofascial
physical therapy for the treatment of urological chronic
pelvic pain syndromes..(Fitzgerald, MP 2009)
• Lowered PFM tone, improved vaginal flexibility, and
improved PF relaxation capacity in women with PVD
(n=11). (Gentilcore-Saulnier, 2010)