Concept Map
advertisement

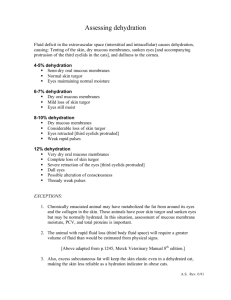
Ineffective airway clearance related to dry mucous membranes as evidenced by inability to cough up secretions, thick mucous secretions, difficulty swallowing **Monitor Sp02, suction oral cavity secretions every hour, HOB elevated 45 degrees, assess lung sounds and RR (maintained at 12 – 20 br/min), assess oral cavity and airway for patency **The patient will demonstrate effective cough, breath sounds will be clear, no cyanosis and dyspnea (capable of removing the sputum, breathes easily, no pursed lips), has a patent airway (does not feel suffocated, breath rhythm and respiratory frequency in the normal range, no abnormal breath sounds) Risk for aspiration related to dysphagia, thick mucous secretions, decreased level of consciousness, depressed cough **Provide oral hygiene to decrease risk for infection should aspiration occur, elevate HOB at 45 degrees, suction PRN, assess LOC, assess ability to swallow, assess nutrition status, insert NG tube if patient cannot tolerate intake), provide adequate IV fluids, monitor for s/s of infection, assess lung fields for crackles **The patient will be free of aspiration, maintain a patent airway, and be free of pneumonia or other lung infection Decreased tissue perfusion related to as evidenced by decreased BP, decreased fluid intake, infection as evidenced by capillary refill > 4 seconds, cold extremities, non-palpable pedal pulses **Assess extremities for diminished tissue perfusion, document baseline mental status and monitor for improvement (if diminishing, assess for decreased perfusion to brain), place SCD on patient’s legs, keep patient warm, provide IV fluids **The patient will demonstrate BP within normal range for client, baseline mental status, extremities warm with absence of pallor and cyanosis, palpable peripheral pulses, capillary refill<3 seconds, absence of edema, urine output at least 30 ml/hour Infection related to the state of the nutrition as evidenced by elevated WBC count, positive bacteria culture, fever, **Administer IV antibiotics (Cefazolin), improve fluid status, provide wound care, monitor temperature, **Upon adherence to IV antibiotics, patient will be free of infection as evidenced by normal vital signs, and absence of purulent drainage from wounds Reason for Seeking Health Care -E.J. is an 88 YO AA Male who presented to the ED on 12/01 with lethargy and acute confusion as a result of severe dehydration. His daughter states that his live-in girlfriend has neglected to care for him in the recent months and states that his girlfriend let him lie on the couch for 7 plus days without care. E.J. was unable to eat or drink for this period of time and also was forced to void on himself because his girlfriend would not assist him to the bathroom. Present illness: -E.J. has dry skin, ulcerative lesions, dry mucous membranes, severe agitation coupled with delirium, increased temperature of 99.6F, increased heart rate (120 – 144), decreased blood pressure (90/44), positive for gram+ staphylococcus infection Pertinent laboratory results: Na+ 155 (high), K+ 3.8, Cl- 119 (high), BUN 13.1 (high), Creatinine 3.4 (high), WBC 26,000 (high), Platelet ct 649mm3 (high) Past medical/surgical history Hypertension, confirmed delirium, constipation, penile cancer, Medical diagnosis Dehydration: lack of fluids and electrolytes required to meet the body's needs Impaired skin integrity related to physical immobilization, dry skin as evidenced by early-stage pressure ulcer in the left heel (redness, inflammation, pressure, and tenderness and warmth in the left heel), dry, cracked non-elastic skin turgor, stage-2 ulcer on left coccyx region. **Monitor for s/s of infection (redness, swelling, increased pain, purulent drainage from ulcers, temperature of 99.8 or greater), WBC (should not rise above 10,000mm3), assess current open ulcer wounds, and assess nutritional status, enhance mobility (to help reduce chances of stasis ulcers, improve current ulcers, and to enhance blood perfusion), provide adequate skin care, encourage fluid intake/start IV fluids **The patient will demonstrate no new abrasions, will have elastic skin turgor upon rehydration, will have marked improvement of current ulcers on skin, will have clean/dry skin Fluid volume deficit related to inadequate fluid intake, electrolyte imbalances, increased metabolic rate, and fluid shifts as evidenced by dry mucous membranes, inelastic skin turgor, edema of lower extremities, fever, decreased urine output, capillary refill > 4 seconds, decreased mental status, elevated platelet count, elevated Na+, elevated BUN, elevated creatinine. ** Monitor urinary output (notify physician if UOP<30ml/hr), administer IV NS, administer IV heparin (monitor PT/INR), assess urine color, assess skin turgor and mucous membranes), document baseline mental status and monitor for improvement, monitor blood pressure (giving fluids increases risk for fluid overload and cardiac problems) **The patient will regain adequate fluid volume and electrolyte balance as evidenced by urine output>30 ml per hr, normotensive blood pressure, heart rate between 80 – 100 beats per min, consistency of weight, and normal skin turgor