Primary and Secondary Prevention of Cardiac Disease Guideline
advertisement

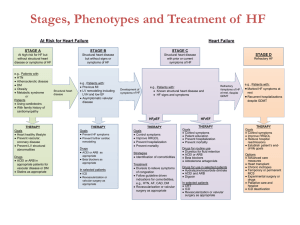
Practice Guidelines for Providers Cardiac Wellness – Primary and Secondary Prevention of Cardiac Disease Guideline Approved by Corporate Quality Management Committee: 02/13/07 Originally approved by the Quality Management Committee on: 1/10/06 Primary Prevention of Cardiovascular Disease (CVD) Initial Assessment of Risk Factors - Beginning at Age 20 to Include • • • • • Family History Smoking Status Blood Pressure (goal <120/80) Fasting Lipid Panel Dietary and Physical Activity Assessment • • • • • Assess willingness to quit Assist by counseling and developing plan to quit Arrange follow-up to special programs or pharmacotherapy BMI Calculation Past Medical History Assessment (including history of atrial fibrillation and diabetes) • Abdominal Circumference (female <35”, males <40”) • Assess for metabolic syndrome (see attached Addendum 1) Current Smoker Blood Pressure • • 120-139/80-89: Counsel on lifestyle changes, recheck 3 months. >140/90 (>130/80 for those with diabetes or chronic kidney disease): Promote lifestyle changes, begin drug therapy (See Figure 1), and agree upon blood pressure goals with patient. Monthly follow-up until blood pressure is stable, then follow-up every 3-6 months. Figure 1 Algorithm for Treatment of Hypertension Table 1 Compelling Indications for Individual Drug Classes Compelling Indications Initial Therapy Options Heart Failure THIAZ, BB, ACEI, ARB, ALDO ANT Post Myocardial Infarction BB, ACEI, ALDO ANT, ARB High CVD Risk THIAZ, BB, ACEI, CCB, ARB Diabetes THIAZ, BB, ACEI, ARB, CCB Chronic Kidney Disease ACEI, ARB Recurrent Stroke Prevention THIAZ, ACEI Key: THIAZ = thiazide diuretic, ACEI = angiotensin converting enzyme inhibitor, ARB = angiotensin receptor blocker, BB = beta blocker, CCB = calcium channel blocker, ALDO ANT = aldosterone antagonist Lipid Management • • • Total cholesterol <200 and HDL >60, triglycerides <200 Determine if lipid lowering therapy is needed (Use Table 2) Initiate therapeutic lifestyle changes or drug therapy (For protocol see Figures 2 and 3) LDL Cholesterol Goals and Cutpoints for Therapeutic Lifestyle Changes (TLC) and Drug Therapy in Different Risk Categories Table 2 Risk Category LDL Goal LDL Level at Which to Initiate TLC LDL Level at Which to Consider Drug Therapy** High Risk: CHD or CHD Risk Equivalents (including diabetes) (10 year risk >20%)* Moderately High Risk: 2+ Risk Factors (10 year risk 10-20%)* Moderate Risk: 2+ risk factors (10 year risk <10%)* Lower Risk: 1 Risk Factor <100 mg/dL (optional goal: <70 in patients with very high CV risk) >100 mg/dL >100 mg/dL (<100 mg/dL: consider drug options)** <130 mg/dL (optional goal: <100) > 130 mg/dL > 130 mg/dL (100-129 mg/dL consider drug options) <130mg/dL > 130 mg/dL > 160 mg/dL <160 mg/dL >160 mg/dL >190 mg/dL (160-189 mg/dL: LDL lowering drug optional) * Electronic 10-year risk calculators are available at www.nhlbi.nih.gov/guidelines/cholesterol. ** When LDL-lowering drug therapy is employed, it is advised that intensity of therapy be sufficient to achieve at least a 30% to 40% reduction in LDL-C levels. Model of Steps in Therapeutic Lifestyle Changes (TLC) Figure 2 Figure 3 After Initiating Therapy – Progression of Drug Therapy in Primary Prevention Dietary and Physical Activity Assessment • • Physical activity, of moderate intensity, for at least 30 minutes on most days of the week. Decrease cholesterol, saturated fat, trans fatty acids and increase fiber. BMI • Achieve and maintain BMI at 18.5 – 24.9 Kg/m 2 Diabetes • Initiate appropriate hypoglycemic therapy to A1c <7% Chronic Atrial Fibrillation • Anticoagulation with INR 2.0 – 3.0 ASA Therapy • 2 or more risk factors, especially those with CHD 10yr risk of >10%, and no contraindications–prescribe 81-162 mg/QD REFERENCES: • The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC VII) May 2003 • The Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (ATP III) May 2001 • Implications of Recent Clinical trials for the NCEP ATP III Guidelines, Circulation. 2004; 110:227-239. • AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update • Annals of Internal Medicine.Narrative Review: Lack of Evidence for Recommended Low-Density Lipoprotein Treatment Targets: A Solvable Problem. 2006.145:520-530 Addendum 1 The Metabolic Syndrome DEFINITION OF THE METABOLIC SYNDROME • • • • • Abdominal (waist) circumference greater than 40 inches for men or 35 inches for women High blood pressure (hypertension) Hyperglycemia (fasting blood sugar more than 110 mg/dL) Elevated triglycerides (a type of fat in the bloodstream) Low levels of high-density lipoprotein, also known as HDL or "good cholesterol" Having at least 3 of the above measurements means that an individual has metabolic syndrome and is at risk for developing type 2 diabetes, coronary heart disease, heart attack, or stroke. TREATING THE METABOLIC SYNDROME Lifestyle modifications include weight loss, regular exercise, stopping smoking, and reducing dietary fat intake. Losing just 10% of excess body weight lowers blood pressure and improves insulin resistance. Some persons may be able to treat high blood pressure and hyperglycemia by altering their lifestyle alone. In many individuals, lifestyle modification is not adequate, and medications must be used to decrease blood pressure, lower triglycerides, and increase the level of HDL. Because these problems are often linked, treating one aspect of the metabolic syndrome may help the other issues. For example, regular exercise can help you lose weight, reduce blood pressure, and manage hyperglycemia and insulin resistance. Combining healthful eating with a regular exercise program is the cornerstone of treating the metabolic syndrome and reducing risk for heart disease, stroke, diabetes, and other medical problems. PREVENTION • • • • • • Exercise regularly throughout your life. Encourage children to have daily physical activity and make healthful food choices. Eat a healthful, balanced diet low in saturated fats and high in nutrient-rich fruits and vegetables. Do not smoke. Recognize that you may have a genetic (inherited) predisposition for diabetes, heart disease, and the metabolic syndrome. Have regular medical check-ups and initiate early treatment for high blood pressure. FOR MORE INFORMATION • • • National Heart, Lung, and Blood Institute http://www.nhlbi.nih.gov American Heart Association http://www.americanheart.org American Diabetes Association http://www.diabetes.org Sources: National Heart, Lung, and Blood Institute; American Heart Association, National Cholesterol Education Program, American Diabetes Association Reference: Patient Page; JAMA, 2004, Vol. 295 (no.7): 850. Secondary Prevention for Patients With Coronary and Other Vascular Disease Goals Smoking Goal Complete cessation Blood Pressure Control Goal <140/90 mm Hg or <130/80 mm Hg if diabetes or renal insufficiency • • • • • Intervention Recommendations Assess willingness to quit Assist by counseling and developing plan to quit Arrange follow-up to special programs or pharmacotherapy 120-139/80-89: Initiate lifestyle modification (weight control, physical activity, alcohol moderation, moderate sodium restriction, and emphasis on fruits, vegetables, and low-fat dairy products) >140/90 (>130/80 for those with diabetes or chronic kidney disease): Promote lifestyle changes, begin drug therapy (See Figure 1), and agree upon BP goals with patient. Monthly follow-up until BP is stable, then follow-up every 3-6 months. Algorithm for Treatment of Hypertension Figure 1 Table 1 Compelling Indications for Individual Drug Classes Compelling Indications Initial Therapy Options Heart Failure THIAZ, BB, ACEI, ARB, ALDO ANT Post Myocardial Infarction BB, ACEI, ALDO ANT, ARB High CVD Risk THIAZ, BB, ACEI, CCB, ARB Diabetes THIAZ, BB, ACEI, ARB, CCB Chronic Kidney Disease ACEI, ARB Recurrent Stroke Prevention THIAZ, ACEI Key: THIAZ = thiazide diuretic, ACEI = angiotensin converting enzyme inhibitor, ARB = angiotensin receptor blocker, BB = beta blocker, CCB = calcium channel blocker, ALDO ANT = aldosterone antagonist Goals ACE Inhibitors • • β-Blockers • • • • Intervention Recommendations Treat all patients indefinitely post MI; start early in stable high-risk patients (anterior MI, previous MI, Killip class II [S3 gallop, rales, radiographic CHF]). Consider chronic therapy for all other patients with coronary or other vascular disease unless contraindicated. Start in all post-MI and acute ischemic syndrome patients. Continue indefinitely. Observe usual contraindications. Use as needed to manage angina, rhythm, or blood pressure in all other patients. BP indicates blood pressure, TG – triglycerides, BMI – body mass index, HbA1c – major fraction of adult hemoglobin, MI – myocardial infarction, CHF – congestive heart failure Goals Diabetes Management Goal HbA1c <7% • • Antiplatelet Agents / Anticoagulants • • Lipid Management • • • Primary Goal LDL <100 mg/dL (optional goal: <70 mg/dL in patients with very high CV risk) • • • • • Lipid Management Secondary Goal If TG >200 mg/dL, then non-HDL† should be <130 mg/dL Physical Activity Minimal Goal 30 minutes 3 to 4 days per week Optimal daily Weight Management Goal BMI** 18.5 – 24.9 kg/m2 • • • • • • • • • • • Intervention Recommendations Appropriate hypoglycemic therapy to achieve near-normal fasting plasma glucose, as indicated by HbA1c Treatment of other risks (eg. physical activity, weight management, blood pressure, and cholesterol management) Start and continue indefinitely aspirin 81 to 162 mg/d if not contraindicated. Consider clopidogrel 75 mg/d or warfarin if aspirin contraindicated. Manage warfarin to international normalized ratio=2.0 to 3.0 in post-MI patients when clinically indicated or for those not able to take aspirin or clopidogrel. Start dietary therapy in all patients (<7% saturated fat and <200 mg/d cholesterol) Promote physical activity and weight management. Encourage increased consumption of omega-3 fatty acids (fish oils) and plant stenols/sterols. Assess fasting lipid profile in all patients, at least every 6 months, and within 24 hours of hospitalization for those with an acute event. If patients are hospitalized, consider adding drug therapy on discharge. Add drug therapy according to the following guide: LDL <100 mg/dL LDL 100 – 129 mg/dL LDL >130 mg/dL Goal: LDL <100 mg/dL Optional Goal: <70 mg/dL (in patients with very high CV risk) Consider LDL-lowering • Intensify LDL-lowering • Intensify LDL-lowering therapy if patient is still therapy therapy at very high-risk for • Fibrate or niacin (if low • Add or increase drug future CVD events HDL or high TG) therapy with lifestyle Consider fibrate or therapies • Consider combined drug niacin if low HDL or high therapy if low HDL or • Consider referral to a TG high TG specialist Consider pill splitting or generic equivalents as available to increase patient compliance. If TG >150 mg/dL or HDL <40 mg/dL: Emphasize weight management and physical activity. Advise smoking cessation. If TG 200-499 mg/dL: Consider fibrate or niacin after LDL-lowering therapy* If TG >500 mg/dL: Consider fibrate or niacin before LDL-lowering therapy* Consider omega-3 fatty acids as adjunct for high TG Encourage minimum of 30 to 60 minutes of activity, preferably daily, or at least 3 to 4 times weekly (walking, jogging, cycling, or other aerobic activity) supplemented by an increase in daily lifestyle activities (eg. walking breaks at work, gardening, household work). Advise medically supervised programs for moderate to high-risk patients If clinically indicated, consider exercise stress test to guide prescription Calculate BMI and measure waist circumference as part of evaluation Monitor response or BMI and waist circumference to therapy Start weight management and physical activity as appropriate Desirable BMI range is 18.5 – 24.9 kg/m2 When BMI >25 kg/m2, goal for waist circumference is <40 inches in men and <35 inches in women BP indicates blood pressure, TG – triglycerides, BMI – body mass index, HbA1c – major fraction of adult hemoglobin, MI – myocardial infarction, CHF – congestive heart failure * The use of resin is relatively contraindicated when TG >200 mg/dL ** BMI calculator for use on Palm OS and Pocket PC 2003 devices: www.nhlbi.nih.gov/health/prof/other/index.htm Online BMI calculator: www.nhlbisupport.com/bmi/ † Non-HDL cholesterol = total cholesterol minus HDL cholesterol REFERENCES: • The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC VII) May 2003 • The Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (ATP III) May 2001 • Implications of Recent Clinical trials for the NCEP ATP III Guidelines, Circulation. 2004; 110:227-239. • AHA/ACC Secondary Prevention for Patients With Coronary and Other Vascular Disease: 2001 Update • Annals of Internal Medicine.Narrative Review: Lack of Evidence for Recommended Low-Density Lipoprotein Treatment Targets: A Solvable Problem. 2006. 145:520-530