Glandular epithelium
advertisement
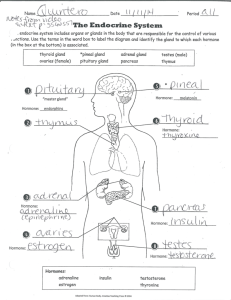
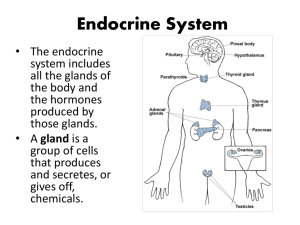
Glandular epithelium Epithelial tissue is present in 2 forms covering glandular Covering epithelium - as sheets of contiguous cells that cover the body on its external surface and line the body on its internal surface Glandular epithelium glands, which originate from invaginated epithelial cells Glands originate from epithelial cells that leave the surface CT-stroma parenchyma Glandular epithelial cells penetrate into the underlying connective tissue, manufacturing a basal lamina around them The secretory units (+ ducts) are the parenchyma of the gland, whereas elements of the connective tissue form the stroma of the gland Glandular epithelia manufacture their product intracellularly by synthesis of macromolecules Products are packaged and stored in vesicles called secretory granules The secretory product may be a polypeptide hormone (e.g., from the pituitary gland); a waxy substance (e.g., from the ceruminous glands of the ear canal); a mucinogen (e.g., from the goblet cells); or milk, a combination of protein, lipid, and carbohydrates (e.g., from the mammary glands) Gland classification on the basis of the method of product distribution Exocrine glands secrete their products via ducts onto the external or internal epithelial surface from which they originated. Endocrine glands secrete their products into the blood or lymphatic vessels for distribution Exocrine gland classification On the basis of the number of cells (unicellular or multicellular) On the basis of their mode of secretion (holocrine, merocrine, apocrine) On the basis of the nature of their secretion (mucous, serous, or mixed) Unicellular exocrine glands – goblet cells The simplest form of exocrine gland Represented by isolated secretory cells in an epithelium – e.g. intestinal or respiratory Have basal stem and apical theca, filled with membranebound secretory droplets (mucinogen granules) – their release is stimulated by chemical irritation and parasympathetic innervation Goblet cell with PAS stain (red) Simple columnar epithelium with goblet cells by TEM Mu = mucous granules BB = brush border Mv = microvilli A = absorptive (columnar epithelial) cell Simple columnar epithelium (AC) with goblet cells (GC) containing mucous granules (MG) by TEM The 4 main differentiated cell types found in the epithelial lining of the small intestine Molecular Biology of the Cell (© Garland Science 2008) Multicellular exocrine glands Exist as organized clusters of secretory units, arranged in varying degrees of organization Do not act alone and independently but instead function as secretory organs Subclassified according to organization of their secretory and duct components simple - their ducts do not branch compound (branched) - their ducts branch shape of their secretory units tubular acinar (alveolar, resembling a grape) tubuloalveolar Multicellular exocrine glands - overview Simple tubular mucus secreting glands - colon Simple acinar mucus secreting glands – male urethra Exocrine gland classification on the basis of their mode of secretion Holocrine glands (e.g., sebaceous gland) - a secretory cell matures, it dies and becomes the secretory product Apocrine glands (e.g., lactating mammary gland) - a small portion of the apical cytoplasm is released along with the secretory product Merocrine glands (e.g., parotid gland) - via exocytosis; i.e., neither cell membrane nor cytoplasm becomes a part of the secretion Exocrine gland classification on the basis of their mode of secretion Holocrine Merocrine Apocrine Larger multicellular glands have additional components Collagenous connective tissue capsule Capsule sends septae (strands of connective tissue) into the gland, subdividing it into smaller compartments known as lobes and lobules Vascular elements, nerves, and ducts utilize the connective tissue septa to enter and exit the gland. In addition, the connective tissue elements provide structural support for the gland. Exocrine glands with merocrine secretion classification on the basis of the nature of their secretion Mucous secrete mucinogens - large glycosylated proteins that, upon hydration, swell to become a thick, viscous, gel-like protective lubricant known as mucin, a major component of mucus examples Serous unicellular: goblet cells multicellular: minor salivary glands of the tongue and palate secrete an enzyme-rich watery fluid examples – pancreas, parotid salivary Mixed – have both mucous and serous components Mucous gland with a duct (arrow) Serous gland with ducts (arrows) Serous secretory unit (high magnification) Serous acinar cells at TEM – rich in RER Mixed gland with serous demilunes (SD) SA – serous acinus MA – mucous acinus StD – striated duct Serous demilunes - a group of cells in mucous acini that secrete a serous fluid Organization of a large multicellular gland – a salivary gland Myoepithelial cells Stellate or spindle-shaped cells located between the basal lamina and the basal pole of secretory or duct cells in several exocrine glands (eg, sweat, lacrimal, salivary, mammary) Possess processes which embrace an acinus as an octopus – connected via gap junctions and desmosomes Specialized for contraction (contain myosin and a large number of actin filaments) - contract around the secretory or conducting portion of the gland and thus help propel secretory products into the duct Myoepithelial cells Endocrine glands Cords Follicles Ductless, and thus their secretory products are released directly into the bloodstream or the lymphatic system Their cells can be arranged in cords or in follicles with lumens for storing the secretory product Overview of the endocrine system System of ductless glands that secrete hormones Hormones are messenger molecules (“first messenger”) Circulate in the blood Act on distant target cells Target cells respond to the hormones for which they have receptors The effects are dependent on the programmed response of the target cells Hormones are just molecular triggers Basic categories of hormones Amino acid based: modified amino acids (or amines), peptides (short chains of amino acids), and proteins (long chains of amino acids) Steroids: lipid molecules derived from cholesterol Hormones Hormones are organic chemical messengers produced and secreted by endocrine cells into the bloodstream. Hormones regulate, integrate and control a wide range of physiologic functions. Modes of cell communication autocrine paracrine juxtacrine Endocrine organs Purely endocrine organs Pituitary gland Pineal gland Thyroid gland Parathyroid glands Adrenal: 2 glands Cortex Medulla Endocrine cells in other organs Pancreas Thymus Gonads Hypothalamus Endocrine glands The hypothalamic-pituitary axis The hypothalamic-pituitary axis Hypothalamic Hormones: Gondotropin RF Corticotropin RF Thyrotropin RF Growth Hor RF Prolactin RF (CRF) Pituitary Hormones: Follicle SH & Adrenocorticoptropin Thyrotropin SH Growth Prolactin Hormone Lutenizing Hor. Hormone (ACTH) Target Gland or Structure: Ovaries & Testes (androgens, estrogen) Adrenal Gland Thyroid Gland (cortisol) (thyroxine) Cells of body Bones, breasts & cells of body Thyroid is composed of spherical follicles Follicle cells: produce thyroglobulin, the precursor of thryoid hormone (thyroxin) Colloid lumen is of thyroglobulin Parafollicular “C” cells: produce calcitonin Thyroid gland follicles F = follicle CT = connective tissue BV = blood vessel Adrenal (suprarenal) glands (“suprarenal” means on top of the kidney) Each is really two endocrine glands Adrenal cortex (outer) Adrenal medulla (inner) Unrelated chemicals but all help with extreme situations Cords of endocrine cells in adrenal cortex The Pancreas Exocrine and endocrine cells Acinar cells (forming most of the pancreas) Exocrine function Secrete digestive enzymes Islet cells (of Langerhans) Endocrine function α-cells – glucagon β-cells – insulin The Gonads (testes and ovaries) main source of the steroid sex hormones Testes Interstitial cells (of Leydig) secrete androgens Primary androgen is testosterone Maintains secondary sex characteristics Helps promote sperm formation Ovaries Androgens secreted by theca folliculi Directly converted to estrogens by follicular granulosa cells Granulose cells also produce progesterone Corpus luteum also secretes estrogen and progesterone Non-endocrine gland hormones Stomach (gastrin) Small intestine (gastrin, secretin, cholecystokinin) Heart (atrial natriuretic peptide) Kidneys (erythropoietin, active vitamin D3) Adipose tissue (over 100 adipokines) Skin Placenta (human chorionic gonadotropin, human placental lactogen, relaxin) Functions regulated by the endocrine system Growth Healing Water balance & blood pressure Calcium metabolism Energy metabolism Stress Regulation of other endocrine organs Tumors from epithelial cells Tumors that arise from epithelial cells may be benign (nonmalignant) or malignant. Malignant tumors arising from epithelia are called carcinomas; those arising from glandular epithelial cells are called adenocarcinomas. It is interesting to note that cancers in adults are most often adenocarcinomas and after age 45 about 90% are of epithelial cell origin. However, in children under 10 years of age, epithelium-derived cancers are the least prevalent type of cancer.