Endotracheal intubation confirmation- a review 1 Introduction
advertisement

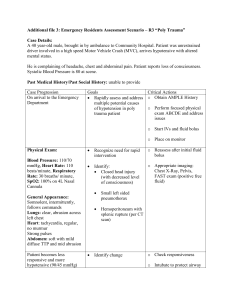
Endotracheal intubation confirmation- a review Dror Lederman, PhD, EMT-P Department of Radiology, University of Pittsburgh 3362 Fifth Avenue, Pittsburgh, PA, 15217, USA Tel. 412-641-2581, Fax 412-641-2582 Abstract In this paper, the problem of endotracheal intubation confirmation is addressed. A review of recent studies which addressed this life-threatening problem is given. The results are analyzed and discussed. Commonly used techniques and some state-of-the-art technologies for correct tube position confirmation are presented, and their advantages and disadvantages are discussed. Keywords- Airway management, Endotracheal intubation confirmation, esophageal intubation detection. 1 Introduction During general anaesthesia, anaesthetic gasses are introduced through the lungs. This state of deliberate pharmacological unconsciousness might also cause airway obstruction. In addition, various types of surgeries and lung diseases mandate stopping spontaneous respiration of a patient and ventilating him artificially. The common denominator of all of the above instances is the widespread necessity to protect the patient’s airways by creating a safe artificial corridor for the air to enter the lungs without obstruction. This task is accomplished by introducing a plastic ventilating tube (endotracheal tube - ETT) into the trachea by a medical procedure called “intubation”. The correct position of the endotracheal tube is between 2cm and 5cm above the bifurcation of the trachea, named “carina”. Unfortunately, the anatomy of the patient does not always allow easy insertion of the ETT. Failing to insert the ETT may result in a failure to ventilate the patient, hypoxia and many other complications such as Pneumonitis [1]. Incorrect positioning of the tube might cause severse complications. Unintentional esophageal intubation can produce catastrophic results as the patient might be deprived of oxygen. Late detection of esophageal intubation has been shown to be correlative with a high mortality rate [2, 3]. Over-insertion might position the tube past the carina. It might therefore be placed in one of the main bronchuses, usually the right one, such that only one lung is ventilated. This condition is called endobronchial intubation or one-lung intubation (OLI). Some patients might suffer oxygen deficiency while ventilated in only one lung. Prolonged one lung ventilation might also cause other serious pulmonary complications such as pneumonia, collapse of the contralateral lung and hyperinflation of the intubation lung. This might cause hypoxia and pneumothorax, respectively, and has been associated with a significatant increase in morbidity [4, 5]. In addition, tube dislodgment might occur from many reasons, for example, due to neck flextion during general anesthesia [6, 7]. Misplacement of the tube during or prior to securing it, or 1 during changes in the patient’s position may result in esophageal intubation subsequent to correct initial placement [8, 9]. This phenomenan is prominent especially in infants and neonates [10]. This papers reviews recent studies which investigated the extent and prevalence of endotracheal tube misplacement both in the hospital and in out-of-hospital setting. The paper proceeds as follows. Section 2 reviews representative studies which investigated the rates of tube misplacement both in the hospital and in the out-of-hospital settings. Section 3 presents the techniques and devices commonly used to confirm tube position. Some state-of-the art devices are presented as well and a discussion of the advantages and disadvantages of each one of the techniques and devices are given. A discussion and summary are given in Section 4. 2 Endotracheal intubation confirmation- a summary of recent studies Unrecognized OLI and esophageal intubation are the most serious complications of attemped tracheal intubation [11]. According to a closed malpractice claims analysis of the American society of anesthesiologists (ASA), 4.5% of the claims are attributed to esophageal intubations [12]. A higher proportion of patients are those who underwent nonoperating-room anesthesia claims than those who underwent operating room anesthesia. Furthermore, unrecognized esophageal intubation was identified as an important cause of cardiac arrest attributed solely to anesthesia at one institution [13]. 2.1 In-hopsital intubations Though the effectiveness and benefits of out-of-hospital intubations have been depated (see for example [14]), it is still considered the definitive airway securing and ventilation method. Intubations performed in the hospital, particularly in the intensive care unit and operating room (OR) are performed under almost ideal conditions- in a quiet environment, with a number of health providers usually available, equipment, space, and the availability to muscle-relaxant drugs. Nevertheless, misplacement and mislodgement of the ETT occur. In [15], 297 trachea intubation performed in the ICU were re-assessed. Out of 25 intubations, 8% of the intubations were esophageal intubation. Some of the out of which 32 were detected by clinical criteria, and 3 were not detected until there was a decrease in the oxyhemoglobin saturation as measured by pulse oximetry. In the OR, unrecognized esophageal intubation accounts for 15% of all catastrophic injuries to patients including brain damage and death, making it the single-most critical anesthetic incident associated with injuries of this type [16, 17]. 2.2 Out-of-hopsital intubations In most of EMS services around the world, paramedics are the major health providers rather than physicians. Paramedics gain a relatively short training, while most of their intubation training is performed on manikins. Additionally, as opposed to the OR setting, paramedics perform the intubation in adverse scenarios, including noisy, under total darkness or intense daylight, poor patient positioning, cervical spine immobilization, lack of neuromuscular blocking agents, combative patients, blood and 2 vomitus in the airway, on the beach or in a crashed car. Out-of-hospital patients are critically ill and often severly injured, and most would be considered “difficult” or high-risk intubations by in-hospital anesthesia standards [18]. Hence, intubation becomes even more challenging and complex when performed in the uncontrolled out-of-hospital setting than in the hospital. Naturally, the rate of complications in the prehospital setting will be much higher than in the OR. Numerous studies have investigated the endtroacheal misplacement rate in the prehospital setting. Several studies reported a misplacement rate between 0% and 7.8% [2, 19-21]. These studies were based on self-reports by the health providers and are thus subject to reporting bias [18, 22]. As such, the methodologies used in these studies, do not allow reliable estimation of tube misplacement error rates. Misplacement rate varies from 50% for providers who do not frequently perform tracheal intubation [20], but high misplacement rates were reported even when experienced anesthesiologists performed the intubation [3, 6, 23, 24] and even in the hospital [7]. In [25], 136 critically ill patients undergoing endotracheal intubation by experienced physicians at the intensive care unit were re-assessed. In 39% of all intubations which were examined, complications occured. Severe complications occurred in 24% of all intubations, out of which an esophageal intubation rate of 7.4% was reported. The results coincide with other studies [15, 26-28]. Other studies, based re-assessment by independent observers, consistently report higher misplacement rates between 6% and 25% [1-3, 29-31]. Timmermann et al. [3] reported an OLI incidents rate of 10.7% (16 out of 149 cases), and an esophageal intubation rate of 6.7% (10 cases). The authors reported that the actual error rates might be higher since some esophageal intubation might not have been detected as some of the patients died in the scene and were therefore not re-assessed by an independent observer. In [31], 108 paramedic endotracheal intubation performed in patients arriving at a regional trauma center in Florida were evaluated. It was found that more than 25% of the endotracheal tubes were misplaced. Two thirds of these intubations were esophageal. A later study by Silvestri et al. [2] reported a decrease in the unrecognized esophageal intubations by paramedics from 25% to 9% with the implementation of a new airway management protocol that required continuous end-tidal CO2 monitoring of all intubated patients. They observed no esopgeal intubations when there was 100% compliance with the protocol. A similar study was performed by Jemmett et al. [29]. In this study, 109 paramedic endotracheal intubations were re-assessed upon arrival at the emergency department in Maine. A similar tube misplacement rate of 12% was reported. In a larger multi-center study [1, 32], out of 1953 evaluated endotracheal intubations, tube misplacement, including esophageal intubation, delayed recognition, unrecognized, and dislodgment were reported in 3.1% of the intubations. More than 22% of patients experienced 1 or more complications, including multiple intubation attempts and failure to perform intubation. A lower rate of 5.8% was reported by Jones et al. [30], which evaluated 208 intubations in Indianapolis. In this study, which included data from one geographical area, most of the evaluated intubations were performed by one EMS system while the paramedics were aware of the study, thus allowing the so called Haythorne effect [33]. 3 The differences between the reported misplaced rate may be due to the provider’s experience, the quality assurance protocols used in the participating EMS system, the prevalence use of secondary confirmation devices and the number of confirmation devices used. Clearly, many errors are identified only through invasive tests or autospy [34, 35]. Moreover, many people undergoing resucitation outside the hospital are pronounced dead at the scene, without being re-assessed by independent observers. In such cases, tube misplacement errors might not be detected. Table . שגיאה! מקור ההפניה לא נמצאsummarizes the results of representative studies. However, there is no question that even with the use of secondary confirmation devices, misplaced intubation do occur, where the exact rate heavily depend on the above-mentioned factors. The studies presented above confirm the fact that unrecognized misplaced intubation represents a significant life-threatening problem. Accordingly, systemic efforts to better equip health providers with continuous tube position monitoring and screening devices are indicated. 3 Common methods and devices for endotracheal intubation confirmation Due to the catastrophical risks associated with misplaced endotraheal intubation, the problem has attracted increasing attention over the last years. Various techniques and devices have been proposed for confirmation of correct tube positioning. In this section, a summmary of the most commonly used techniques for ETT confirmation will be presented. 3.1 Visualization techniques Direct visualization is usually used before all other methods. For decades, it has been considered as “gold standard” for confirming endotracheal intubation. By visualizing the tube as it is passed through the cords, the operator can reasonably assume that the tube has been placed in the trachea. Obviously, this method can not be used when the cords are not visible, due to large tongue, prominent teeth, a short neck, blood and secretions. In addition, tube dislodgement might occur either before or after it has been secured. Inadvertent esophageal intubation has been reported in cases where the operator visualized tube passage through the cords and was certain of endotracheal placement [36]. Moreover, the method may be used only under optimal clinical circumstances when the practitioner can easily view the glottis with standard laryngoscopy [37]. Consequently, this method is unreliable as the sole method for tube position verification [36]. Obviously, the method does not allow continuous monitoring. Fiberoptic bronchoscopy is an excellent method to confirm ETT placement. Performing bronchoscopy through the ETT and visualizing the carina may reliably confirm proper placement. However, massive secretions, blood, or gastric contents may block a bronchoscope view. It is labor intensive, required appropriate training and not cost-effective to perform in all cases (e.g. [38, 39]). Recently developed visualization tools include video laryngoscopy and videointuboscopic devices [40, 41]. These tools may aid in visualizing the glottis in many difficult conditions. As fiberoptic bronchoscopy, these tools require appropriate 4 training, continuous monitoring and they might be obscured due to blood and secretions. Their use in out-of-hospital setting, such as intensive daylight, is problematic. In addition, these tools are not cost-effective. Anyway, whether visualization is performed directly or using visualization devices, without re-checking by an additional observer, this viewing is not foolproof [42]. 3.2 Chest radiography Chest radiography is commonly performed in patients who underwent tracheal intubation outside the OR. Chest radiography is not useful for detecting esophageal intubation as the esophagus lies posterior to the tracha. Furthermore, it requires appropriate equipment, adequate training, it is expensive per use, and time-consuming. Obviously, it’s use is limited to in-hospital settings. Moreover, it is not fullproof. For instance, in [43] an ETT misplacement rate of 14% with the use of chest radiography was reported. 3.3 Analysis of breath sounds The stethoscope is probably the most primitive and widely used technique. Auscultation of the lung sounds using the stethoscope requires high attention, and its reliability has been shown to be low [9, 43-50]. Auscultation of breath sounds in both axillae may result in misdiagnosis due to the sounds produced by the air passing through the esophagus. Auscultation of epigastic sounds may improve accuracy. However, gastric distention might result also from previous bag-valve-mask ventilation, regardless of tube placement [45, 46], hence leading to misdiagnosis. Massive unilateral aspiration can lead to diminished lung sounds, which may be misinterpreted as bronchial intubation. In addition, in thin patients, tracheal breath sounds may be transmitted to the epigastic area simulating gastric insufflation [47]. On the other hand, in esophageal intubations, abdominal distention does not always occur, therefore, leaving the esophageal intubation undetected. In [47, 48], for example, 90% of esophgeal intubations were incorrectly judged to be tracheal intubations using auscultation using the stethoscope. In [44], 48% of the esophageal intubations were not detected though the documented use of auscultation. In [43], 60% of the reported OLI occurred despite the presence of equal breath sounds on examination. Similar results were reported in other studies (e.g. [48, 51]). Detecting incorrect tube positioning based on auscultation may be very difficult in infants and small children. In fact, according to [7, 32], auscultation of bilateral breath sounds does not rule out endobronchial intubation in children. Computerized analysis of breath sounds has been proposed in several papers [5256]. Using two or more microphones located at the back or chest of the patient, the acoustical breath signals are recorded and analyzed using smart signal processing algorithms. Basically, these methods mimic ausculation of lung sounds by the health care providers. Therefore, while they allow continuous automatic monitoring of the tube position, they heavily depend on background noise and require several microphones to be attached to the patient’s chest or back, thus making the technique impractical for both in-hospital and out-of-hospital use. These methods potentially suffer from the similar disadvantages as auscultation of lung sounds by the health care providers, and as such their reliability is questionable and in any case yet to be evaluated. 5 3.4 Gas exchange-based techniques Pulse oximeter devices, which measure the oxygen saturation, are also in common clinical use. These devices suffer from a significant and critical latency time of 25min, which makes them irrelevant for detection of tube positioning. In cases of adequate preoxygenation, oxygen desaturation may take several minutes to occur in patients with misplaced ETT [47, 57]. At the time of desaturation, the deleterious consequences of hypoxia to the brain and heart may already be prominent. Moreover, oxygen saturation is dependent on adequate perfusion and blood pressure, and therefore pulse oximetry can not be used in many medical conditions such as cardiopulmonary resucitation and hypovalemic shock. Another disadvantage of pulse oximetry is that it is unreliable for OLI incidents detection since in such cases oxygen saturation may be high for quite a long time. In [58], the use of oxygen saturation has been shown to be unreliable for endotracheal tube verification. Additionally, intense daylight, fluorescent, incandescent, xenon, and infrared light sources have been reported to cause spurious pulse oximetry readings [59]. Various other interferences might caused by Hemoglobin variants, hypothermia, hypotention, anemia, and nail polish [59, 60]. Another well known technique is the esophageal detector device (EDD). The EDD consists of either a self-in-flating bulb or a 60-mL syringe, has become a widely used method of verification [61]. This technique relies on the fact that the trachea is rigid and permits free aspiration of air from the pulmonary dead space, while aspiration from the esophagus causes collapse of the esophagreal wall and delayed or absent reinflation. However, in cases in which the patients are ventilated prior to aspiration, rapid reinflation might occur regardless of tube location [61, 62]. Moreover, incorrect determination of the tube position might occur in patients with morbid obesity, late pregnancy or severe asthma or when there are significant tracheal secretions. In such cases, the trachea may collapse when aspiration is attempted [11, 63]. As pulse oximetry, neither this technique can be used to detect OLI incidents. In [64], as low as 50% accuracy in detecting esophgeal intubation in out-of-hispital scenarios were reported, not including 11 cases in which the paramedic was unable to interpret the result. Tanigawa et al. [65] investigated 48 intubations in which an EDD was used to confirm correct intubation. Sensitivity rates of 72.9% and 70.8% were found for the syringe EDD and bulb test, respectively. Other similar tools are esophageal intubation detector (EID) and tracheal detectingbolb (TDB). As EDD, significant error rates were reported using these methods. Inaccurate results have been reported in patients with morbid obesity, pulmonary edema, bronchospastic disease or ETT obstruction as in the case of an airway contaminated with blood or vomitus [66, 67]. Specifically in obese patients with a body mass index (BMI) greater than 35, the device has a false negative rate of 11-30% [66]. Furthermore, these tools cannot provide continuous breath-to-breath monitoring of ETT position. Additionally, their use is contraindicated in pregnant patients ahd children under 5 years old [67]. Poor performances were documents by the use of paramedics [64]. In recent years, carbon dioxide detection (CO2) has became the gold standard-defacto for confirming the tube position. Measurement of end-tidal CO2 (ETCO2) using 6 either quantitive (capnometer) or qualitive (capnography) devices. Both devices have been studied in many occations (e.g. [15, 17, 68-70]). Given the efficacy of capnography, the American Society of Anesthesiology has included ETCO2 detection in their standards [71]. This action, combined with the availability of inexpensive devices, has established ETCO2 detection as the standard of care for endotracheal intubation in the hospital [72]. The use of colorimetric devices in patients in cardiac arrest has some limitations. In cardiac arrest, low ETCO2 may represent esophgeal intubation, or tracheal intubation with markedly dimished pulmonary blood flow despite endotracheal placement of the tube [9]. In this case, it is the low cardiac output that results in very low delivery of CO2 to the lungs for excretion that causes a low ETCO2. For patients in cardiac arrest, Ornato [68] and Macleod [17] studies showed sensitivities and specificities of 69-72% and 100%, respectively. Capnography has some advantage in such cases over quantitive devices- the threshold for detection of exhaled CO2 is significantly lower in capnography comparing to colorimetric capnometry [73]. Additionaly, crucial discriminative information may be obtained from the CO2 waveform. In [74, 75], it has been shown that capnography is superior to semiquantitative colorimetric devices in a prehospital setting in both arrest and non-arrest patients. However, it is well known that measurement of the exhaled CO2 can not be performed or is unreliable in many emergencies. For instance, during cardiopulmonary resucitation, low CO2 levels may indicate either an esophageal intubation or tracheal intubation because of profoundly dimished or absent cardiac output, pulmonary blood blow, and alveolar CO2 concentration [9, 11, 62, 69]. Severe airway obstruction may prevent sufficient CO2 exhalation to be detected by ETCO2-based devices [76]. If the tube is positioned neigher in the trachea nor in the esophagus, an open glottis may allow detection of CO2. Li [77] reported that small concentrations of CO2 may be detected even in esophageal intubation, especially if bag-and-mask ventilation has insufflated previously exhaled air into the stomach [77]. Likewise, patients who have recently ingested carbonated beverages may have CO2 detected in the stomach [77]. False negative capnograhpy readings might result in cases of obstructed tube, due to plugging the tip of the tube with mucus or blood, or when the tube abuts the tracheal wall and thus impedes or prevents exhalation. Apnea and severe bronchospasm lead to dramatically reduced exhalation and thus to false negative results [9]. Furthermore, ETCO2-based devices are unreliable for detection of OLI incidents because the capnograpm is generally typical in shape and shows normal end-tidal values [9, 78]. A method based on a technology similar to sonar signal processing has been suggested [79, 80]. The SCOTI device analyses the reflections obtained when sound waves are emitted from a small sound generator at the tip of the tube. A similar idea, in which the acoustic reflections are used to generate an image of the airways has been proposed by Raphael et al. [81, 82]. Both techniques have been tested only on smallsize population, in quiet environment. Their performance in noisy environment, and/or in the presence of vomitus and secretions, is still to be evaluated. Table . שגיאה! מקור ההפניה לא נמצאpresent the features calculated: Recently, methods based on impedance analysis were suggested [83-85] were suggested. The technique is based on the assumption that a ventilated lung will have 7 increased impedance. Therefore, by measuring the impedance over the chest cavity, a discrimination between esophageal (constant impedance) and tracheal intubation (changing impedance) is performed. Preliminary studies showed promising results. However, it is not clear whether the method may be used to detect OLI incidents. Furthermore, the method might fail to detect esophageal intubation in spontaneouslybreathing patients. Ultrasound-based methods have been proposed by several research groups [86-90]. In one type of devices, ultrasound-based imaging are used to visualize the diaphragmatic and pleural motion. In this way, lung expansion can be measured as an indication of the tube position in non-breathing patients. Another type of devices is based on direct ultrasound visualization of the ETT. Small-sized population studies showed promising results. As in the case of the previous devices, it is not clear whether this device can be used for OLI detection. 8 Intubation Errors Authors Schwartz et al. [15] Jacobs et al. [19] Steward et al. [20] Pointer et al. [21] Silvestri et al. [2] Timmerm ann et al. [3] Katz et al. [31] Wang et al. [1, 32] Jemmett et al. [29] Jones et al. [30] Timmerm ann et al. [24] No of Patients OLI Intubatio / study ns type 297 ICU 4%1 Esoph. Intub. Total misplaced 11.8% Comment s and weakness es complic Others ations 15% 3 2 Unexperi enced Providers 153 149 108 1953 50% Prospec tive Prospec tive Retrosp ective Retrosp ective 109 208 Prospec tive -- 8.5% 9% 10.7 % 6.7% 17.4% 16% 4 25% 22% 1.8% 11.9% NR NR 1 5.8% NR were not detected by clinical examination and ofund only in the chest radiograph obtained immediately after intubation. 2 three esophageal intubations were not recognized until there was a decrease in the oxyhemoglobin saturation as measured by pulse oximetry. One more patient, not included in the study, suffered from esophageal intubation which was not detection before death. 3 8% difficult intubation; 4% post-intubation aspiration; 3% died within 30 min; requiring more than two attempts at laryngoscopy by a physician skilled in airway management; 4.4% required four or more attempts, 0.6% required ten or more attempts. 4 Based on self reports. 5 Up to 40% in selected EMS; based on self-reports 9 5 Griesdale et al. [25] 136 critically ill patients ICU, Prospec tive 7.4% 24% *13.2% require d >= 3 attempt s; 6.6% difficult intubati ons 253 ICU, Prospec tive 5% 28% Verghese et al. [7] Sakles et al. [26] Jaber et al. [27] Benedett o et al. [28] Katz and Falk McGillic uddy 108 157 ICU, retrospe ctive NR 16.7% 25% 6.5% 0.6% 19% NR = not rated 4 Summary In summary, none of the techniques used for confirmation of the ET position, have been proven to be 100% reliable and none of them are reliable for detection of OLI incidents [11]. Indeed, according to the guidelines of the American Heart Association [91] confirmation of correct tube positioning should be performed using several secondary confirmation devices, and re-confirmation should be performed any time the patient is moved or neck flexion or extension performed, or any other case in which tube dislodgement is suspected. 6 Video-laryngoscope or fiber-optic bronchoscope was usually used in multiple attempts 10 6 References [1] H. E. Wang, L. J. Cook, C. H. Chang, D. M. Yealy, and J. R. Lave, “Outcomes after out-of-hospital endotracheal intubation errors,” Resuscitation, vol. 80, no. 1, pp. 50–55, Jan. 2009. [2] S. Silvestri, G. A. Ralls, and B. Krauss, “The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system,” Ann. Emerg. Med., vol. 45, pp. 497–503, 2005. [3] A. Timmermann, S. G. Russo, C. Eich, M. Roessler, U. Braun, W. H. Rosenblatt, and M. Quintel, “The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians,” Crit. Care and Trauma, vol. 104, no. 3, pp. 619–623, Mar. 2007. [4] C. W. Zwillich, D. J. Pierson, and C. E. Creagh, “Complications of assisted ventilation. a prospective study of 354 consecutive espisodes,” Am. J. Med., vol. 57, pp. 161–170, 1974. [5] R. L. Owen and F. W. Cheney, “Endobronchial intubation: a preventable complication,” Anesthesiology, vol. 67, pp. 255–257, 1987. [6] S. J. Yap, R. W. Morris, and D. A. Pybus, “Alterations in endotracheal tube position during general anesthesia,” Anaesth. Crit. Care, vol. 22, pp. 586–588, 1994. [7] S. T. Vergese, R. S. Hannallah, M. C. Slack, R. R. Cross, and K. M. Patel, “Auscultation of bilateral breath sounds does not rule out endobronchial intubation in children,” Anesht. Analg., vol. 99, pp. 56–58, 2004. [8] P. A. Contrady, L. R. Goodman, F. Laine, and M. M. Singer, “Alterations of endotracehal tube position. flexion and extension of the nexk,” Crit. Care Clin., vol. 4, pp. 7–12, 1976. [9] J. S. Gravenstein, M. B. Jaffe, and D. A. Paulus, Eds., Capnography clinical aspects.1em plus 0.5em minus 0.4emCambrdige University Press, 2004. [10] Y. K. Bosman and P. A. Foster, “Endotracheal intubation and head position in infants,” S. Afr. Med., vol. 52, pp. 71–73, 1977. [11] J. P. Nolan, C. D. Deakin, and J. Soar, “European resuscitation council guidelines for resuscitation 2005. section 4. adult advanced life support.” Resuscitation, vol. 67, no. 1, pp. S39–S86, 2005. [12] C. G. Miller, “Management of the difficult intubation in closed malpractice claims,” ASA newsletter, Tech. Rep. 6, Jun. 2000. [13] R. I. Keenan and C. P. Boyan, “Cardiac arrest due to anesthesa: a study of incidence and causes,” I. Am. Med. Assoc., vol. 253, pp. 2373–2377, 1985. [14] H. E. Wang and D. M. Yealy, “How many attempts are required to accomplish out-of-hospital endotracheal intubation? ” Acad Emerg Med., vol. 13, no. 4, pp. 372–377, Apr. 2006. [15] D. E. Schwart, M. A. Matthay, and N. H. Cohen, “Death and other complications of emergency airway management in critically ill adults. a prospective investigation of 297 tracheal intubations,” Anesthesiology, vol. 82, pp. 367–376, 1995. 11 [16] J. S. Goldberg, P. R. Rawle, J. L. Zehnder, and R. N. Sladen, “Colorimetric endtidal carbon dioxide monitoring for tracheal intubation,” Anesth. Analg., vol. 70, pp. 191–194, 1990. [17] B. A. Macleod, M. B. Heller, J. Gerard, D. M. Yealy, and J. J. Menegazzi, “Verification of endotracheal tube placement with colorimetric end-tidal co2 detection,” Ann. Emerg, vol. 20, pp. 267–270, 1991. [18] H. E. Wang and D. M. Yealy, “Out-of-hospital endotracheal intubation: Where are we? ” Ann. of Emer. Med., vol. 46, no. 6, pp. 532–541, Jun. 2006. [19] L. M. Jacobs, L. D. Berrizbeitia, B. Bernnett, and C. Madigan, “Endotracheal intubation in the prehospital phase of emergency medical care,” JAMA, vol. 250, pp. 2175–2177, 1983. [20] R. D. Stewart, P. M. Paris, and P. M. Winter, “Field endotracheal intubation by paramedical personnel: success rates and complications.” Chest, vol. 85, pp. 341– 345, 1984. [21] J. E. Pointer, “Clinical characteristics of paramedics’ performance of endotracheal intubation,” J. Emerg. Med., vol. 6, pp. 505–509, 1988. [22] J. D. Nolan, “Prehospital and resuscitative airway care: should the gold standard be reassessed? ” Curr. Opin. Crit. Care, vol. 7, pp. 413–421, 2001. [23] E. Tovar, S. Abshier, A. Borsari, and R. Patel, “Mainstem bronchial intubation: An unrecognized source of hypotension during coronary artery bypass surgery,” Journal of Cardiothoracic and Vascular Anesthesia, vol. 11, no. 5, pp. 615–618, 1997. [24] A. Timmermann, C. Eich, and S. G. Russo, “Prehospital arirway management: a prospective evaluation of anaesthesia trained emergency physicians,” Resuscitation, vol. 70, pp. 179–185, 2006. [25] D. E. G. Griesdale, T. L. Bosma, T. Kurth, G. Isac, and D. R. Chittock, “Complications of endotracehal intubation in the critically ill,” Intens. Care. Med., vol. 34, pp. 1835–1842, Jul. 2008. [26] J. C. Sakles, E. G. Laurin, A. A. Rantapaa, and E. A. Panacek, “Airway management in the emergency department: a one-year study of 610 tracheal intubations,” Ann. Emerg. Med., vol. 31, pp. 325–332, 1998. [27] S. Jaber, J. Amraoui, J. Y. Lefrant, C. Arich, R. Cohendy, L. Landreau, Y. Calvet, X. Capdevila, A. Mahamat, and J. J. Eledjam, “Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study,” Crit. Care Med., vol. 34, pp. 2355–2361, 2006. [28] W. J. Benedetto, D. R. Hess, E. Gettings, L. M. Bigatello, H. Toon, W. E. Hurford, and U. Schmidt, “Urgent tracheal intubation in general hospital units: an observational study,” J. Clin. Anesth., vol. 19, pp. 20–24, 2007. [29] M. E. Jemmett, K. M. Kendal, and M. W. Fourre, “Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting,” Acad. Emer. Med., vol. 10, pp. 961–965, 2003. [30] J. H. Jones, M. P. Murphy, and R. L. Dickson, “Emergency physician-verified out-of-hospital intubation: miss rates by paramedics,” Acad. Emer. Med., vol. 11, pp. 707–709, 2004. 12 [31] S. H. Katz and J. L. Falk, “Misplaced endotracheal tubes by paramedics in an urban emergency medical services system,” Ann. Emerg. Med., vol. 37, pp. 32– 37, 2001. [32] H. E. Wang, J. R. Lave, C. A. Sirion, and M. Yealy, “Paramedic intubation errors: isolated events or symptoms of larger problems? ” Health Affairs, vol. 25, no. 2, pp. 501–509, 2006. [33] H. A. Landsberger, Hawthorne Revisited.1em plus 0.5em minus 0.4emCornell University, Ithaca, N.Y., 1958. [34] K. Jaeger, H. Ruschulte, and A. Osthaus, “Tracheal injury as a sequence of multiple attempts of endotracheal intubation in the course of a preclinical cardiopulmonary resuscitation,” Resuscitation, vol. 43, pp. 147–150, 2000. [35] H. L. Mizelle, S. G. Rothrock, and S. Silvestry, “Preventable morbidity and mortality from prehospital paralytic assisted intubation: can we expect outcomes comparable to hospital-based practice? ” Prehosp. Emerg. Care, vol. 6, pp. 472– 475, 2002. [36] S. J. White and C. M. Slovis, “Inadvertant esophageal intubation in the field: reliance on a fool’s "gold standard",” Acad. Emerg. Med., vol. 4, pp. 89–91, 1997. [37] P. Rudraraju and L. A. Eisen, “Confirmation of endotracheal tube position: A narrative review,” J. of Intensive Care Medicine, vol. 24, pp. 283–292, Aug. 2009. [38] M. Suarez, A. Chediak, P. Ershowsky, and B. Krieger, “Evaluation of a flexible fiberoptic catheter in confirming endotracheal tube placement in the intensive care unit,” Respir. Care, vol. 32, no. 2, pp. 81–84, 1987. [39] Y. G. Weiss and C. S. Deutschman, “The role of fiberoptic bronchoscope in airway management of the critically ill patient,” Crit. Care Clin., vol. 16, no. 3, pp. 445–451, 2000. [40] M. Weiss, U. Schwarz, C. M. Dillier, and A. C. Gerber, “Video-intuboscopic monitoring of tracheal intubation in pediatric patients,” Candadian Journal of Anesthesia, vol. 48, no. 7, pp. 691–696, Jul. 2001. [41] M. Weiss, K. Hartmann, J. Fischer, and A. C. Gerber, “Video-intuboscopic assistance is a useful aid to tracheal intubation in pediatric patients,” Cardiothoracic anesthesia, respiration and airway, 2000. [42] A. E. Bair, D. Smith, and L. Lichty, “Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers,” J. Emerg. Med., vol. 28, no. 4, pp. 403–407, 2005. [43] W. Brunel, D. L. Coleman, and D. E. Schwartz, “Assessment of routine chest reoentgenograms and the physical examination to confirm endotracheal tube position,” Chest, vol. 96, pp. 1043–1045, 1989. [44] R. A. Caplan, K. L. Posner, R. J. Ward, and F. W. Cheney, “Adverse respiratory events in anesthesia: a closed claims analysis,” Anesthesiology, vol. 72, pp. 828– 833, 1990. [45] A. W. Peterson and L. M. Jacker, “Death following inadvertent esophageal intubation: a case report,” Anesth. Analg., vol. 52, pp. 398–401, 1973. [46] T. H. Howells, “Oesophageal misplacement of a tracheal tube,” Anaesthesia, vol. 40, p. 387, 1985. 13 [47] P. K. Birmingham, F. W. Cheney, and R. J. Ward, “Esophageal intubation: a review of detecting techniques,” Anesth. Analg., vol. 65, pp. 886–891, 1986. [48] K. H. Andersen and A. Hald, “Assessing the position of the tracheal tube: the reliability of different methods,” Anaesthesia, vol. 44, pp. 984–985, 1989. [49] I. D. Klepper, R. K. Webb, J. V. D. Walt, G. L. Ludbrooks, and J. Cockings, “The stethoscope: Application and limitation- an analysis of 2000 incident reports,” Anaesth. Intens. Care, vol. 21, no. 5, pp. 575–578, 1993. [50] G. R. Wodicka, P. D. DeFrain, and S. S. Kraman, “Bilateral asymmetry of respiratory acoustic transmission,” Med. Biol. Eng. Comp., vol. 32, no. 5, pp. 489–494, 1994. [51] K. Linko, M. Paloheimo, and T. Tammisto, “Capnography for detection of accidental oesophageal intubation,” Acta Anaesthesiol. Scand., vol. 27, pp. 199– 202, 1983. [52] C. J. O’connor, h. Mansy, R. A. Balk, K. J. Tuman, and R. H. Sandler, “Identification of endotracheal tube malpositions using computerized analysis of breath sounds via electronic stethoscopes,” Anesth. Analg., vol. 101, no. 3, pp. 735–739, 2005. [53] S. Tejman-Yarden, D. Lederman, N. Weksler, and G. Gurman, “Acoustic monitnoring of double lumen ventilated lungs for the detection of selective unilateral lung ventilation,” Anesth. Analg., vol. 103, pp. 1489–1493, 2006. [54] D. Lederman, “An energy ratio test for one lung intubation detection,” in Proceedings of the 18th Biennial International EURASIP Conference, Brno, Czech Republic, 2006., 2006. [55] S. Tejman-Yarden, A. Zlotnik, L. Weizman, J. Tabrikian, A. Cohen, N. Weksler, and G. M. Gurman, “Acoustic monitoring of lung sounds for the detection of onelung intubation,” Anesth. Analg., vol. 105, no. 2, pp. 397–404, Aug. 2007. [56] L. Weizman, J. Tabrikian, and A. Cohen, “Detection of one-lung intubation incidents,” Annals of Biomed. Eng., vol. 36, no. 11, pp. 1844–1855, Nov. 2008. [57] H. Guggenberger, G. Lenz, and R. Federle, “Early detection of inadvertent oesophageal intubation pulse-oximetry vs. capnography,” Acta Anaesthesiol. Scand., vol. 33, pp. 112–115, 1989. [58] S. M. Szekely, R. K. Webb, J. A. Williamson, and W. J. Russell, “The Australian incident monitoring study. problems related to the endotracheal tube: an analysis of 2000 incident reports,” Anesth. Intens. Care, vol. 21, pp. 611–616, 1993. [59] C. D. Hanning and J. M. Alexander-William, “Pulse oximetry: a practical review,” BMJ, vol. 311, no. 7001, pp. 367–370, 1995. [60] M. Yelderman and W. New, “Evaluation of pulse oximetry,” Anesthesiology, vol. 59, no. 4, pp. 349–352, 1983. [61] M. Wee, “The esophageal detector device,” Anaesthesia, vol. 46, pp. 1086–1087, 1991. [62] D. G. Bjoraker, Capnography clinical aspects.1em plus 0.5em minus 0.4emCambrdige University Press, 2004, ch. Airway management in the operating room, pp. 39–44. [63] M. R. Salem, “Verification of endotracheal tube position,” Anesth. Clin. North Am., vol. 19, no. 4, pp. 813–819, 2001. 14 [64] M. Pelucio, L. Halligan, and H. Dhindsa, “Out-of-hospital experience with the syringe esophageal detector device,” Acad. Emerg. Med., vol. 4, pp. 563–568, 1997. [65] K. Tanigawa, T. Takeda, E. Goto, and K. Tanaka, “The efficacy of esophageal detector devices in verifying tracheal tube placement: A randomized cross-over study of out-of-hospital cardiac arrest patients,” Anesth. Analg., vol. 92, pp. 375– 378, 2001. [66] D. J. Lang, Y. Wfai, M. R. Salem, E. A. Czinn, A. A. Halim, and A. Baraka, “Efficacy of self-inflating bulb in confirming tracheal intubation in the morbidly obese,” Anesthesiology, vol. 85, pp. 246–253, 1996. [67] D. A. Coonz and M. Gratton, “Rules of engagement how to reduce the incidents of unrecognized esophageal intubation,” J. Emerg. Med. Serv., vol. 27, pp. 44– 59, Jun. 2002. [68] J. P. Ornato, J. B. Shipley, E. M. Racht, C. M. Slovis, K. D. Wrenn, P. E. Pepe, S. L. Almeida, V. F. Ginger, and T. V. Fortre, “Multicenter study of a portable, hand-size, colorimetric end-tidal carbon dioxide detection device,” Ann. Emerg. Med., vol. 21, no. 5, pp. 518–523, 1992. [69] S. M. Bhende and A. E. Thompson, “Evaluation of an end-tidal co2 detector during pediatric cardiopulmonary resuscitation,” Pediat., vol. 95, no. 3, pp. 395– 399, Mar. 1995. [70] W. P. Bozeman, D. Hexter, H. K. Liang, and G. D. Kelen, “Esophageal detector device versus detection of end-tidal carbon dioxide level in emergency intubation,” Ann Emerg Med., vol. 27, no. 5, pp. 595–599, May 1996. [71] American Society of Anesthesiology House of Delegates, “Standards of basic intra-operative monitoring„” Oct. 1986, amended Oct 1990. [72] W. H. Ginsberg, “When does a guidline become a standard? the new american society of anesthesiologys guidelines give us a clue,” Ann. Emerg. Med., vol. 22, pp. 1891–1896, 1993. [73] R. E. O’connor and R. A. Swor, “Verification of endotracheal tube placement following intubation,” Prehosp. Emerg. Care, vol. 3, no. 3, pp. 248–250, 1999. [74] A. Singh, R. E. Megargel, M. R. Schnyder, and R. E. Oconnor, “Comparing the ability of colorimetric and waveform end tidal capnography to verify endotracheal tube placement in the prehospital setting,” Acad. Emerg. Med., vol. 10, pp. 466–467, 2003. [75] S. Grmec, “Comparison of three different methods to confirm tracheal tube placement in emergency intubation,” Intens. Care. Med., vol. 28, pp. 701–704, 2002. [76] ------, “Capnography- reliable technique for indentifying correct tube placement in cardiac arrest endotracheal intubation,” Resuscitation, vol. 77, no. 3, pp. 416– 417, 2008. [77] J. Li, “Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation,” J. Emerg. Med., vol. 20, no. 3, pp. 223–229, 2001. [78] R. K. Webb, J. H. V. D. Walt, W. B. Runciman, J. A. Williamson, J. Cockings, W. J. Russell, and S. Helps, “Which monitor? an analysis of 2000 incident reports,” Anaesth. Intens. Care, vol. 21, no. 5, pp. 529–542, Oct. 1993. 15 [79] D. Murray, M. E. Ward, and J. W. Sear, “SCOTI- a new device for identification of tracheal intubation,” Anaesthesia, vol. 50, no. 12, pp. 1062–1064, 1995. [80] A. Trikha, C. Singh, V. Rewari, and M. K. Arora, “Evaluation of the SCOTI device for confirming blind nasal intubation,” Anaesthesia, vol. 54, pp. 347–349, 1999. [81] D. T. Raphael, “Acoustic reflectometry profiles of endotracheal and esophageal intubation,” Anesthesiology, vol. 92, no. 5, May 2000. [82] ------, “Acoustic reflectometry imaging of the airway,” Seminar in Anesthesia, Perioperative Medicine and Pain, vol. 26, pp. 210–217, 2007. [83] M. Absolom, R. Roberts, U. B. Bahlmann, J. E. Hall, T. Armstrong, and A. Turley, “The use of impedance respiraometry to confirm tracheal intubation in children,” Anaesthesa, vol. 61, pp. 1145–1148, 2006. [84] D. Steinmann, C. A. Stahl, J. Minner, S. Schumann, T. Loop, A. Kirschbaum, H. J. Priebe, and J. Guttmann, “Electrical impedance tomography to confirm correct placement of double-lumen tube: a feasbility study,” British Journal of Anaesthesia, vol. 101, no. 3, pp. 411–418, Jun. 2008. [85] J. Kramer-Johansen, J. Eilevstjonn, T. M. Olasveengen, A. E. Tomlinson, E. D. E, and P. A. Steen, “Transthoracic impedance changes as a tool to detect malpositioned tracheal tubes,” Resuscitation, vol. 76, no. 1, pp. 11–16, 2008. [86] R. K. Visaria and D. R. Westenskow, “Model-based detection of endobronchial intubation,” Anesth. Analg., vol. 103, no. 4, pp. 888–893, 2006. [87] J. Galicianao, A. J. Bush, and S. A. Godambe, “Use of bedside ultrasonography for endotracheal tube placement in pediatric patients: a feasibility study,” Pediatrics, vol. 120, pp. 1297–1303, 2007. [88] S. C. Park, J. H. Ryu, S. R. Yeom, J. W. Jeong, and S. J. Cho, “Confirmation of endotracheal intubation by combined ultrasonographic methods in the emergency department,” Emerg. Med. Austr., vol. 21, no. 4, pp. 293–297, Jul. 2009. [89] E. Göksu, V. Sayrac, C. Oktay, M. Kartal, and M. Ackimen, “How stylet use can effect confirmation of endotracheal tube position using ultrasound,” Am. J. Emerg. Med., vol. 28, pp. 32–36, 2010. [90] M. Blaivas and J. W. Tsung, “Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation,” J. Ultrasound Med., vol. 27, pp. 785–789, 2008. [91] American Heart Association, “Guidelines for cardiopulmonary resuscitation and emergency, part 7.1: Adjuncts for airway control and ventilation,” Circulation, vol. 112, pp. 51–57, 2005. 16