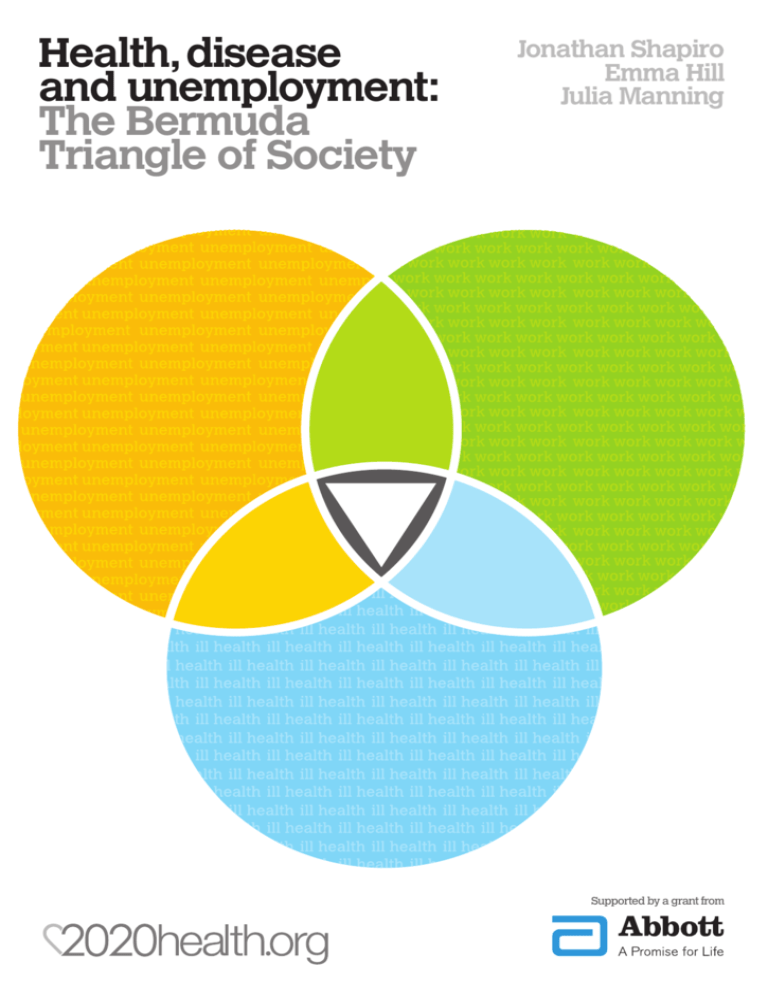
Health,disease
and unemployment:
The Bermuda
Triangle of Society
Jonathan Shapiro
Emma Hill
Julia Manning
Supported by a grant from
Health,disease
and unemployment:
The Bermuda
Triangle of Society
Jonathan Shapiro
Emma Hill
Julia Manning
Supported by a grant from
Contents
01
02
03
04
05
06
07
08
09
10
11
About this Publication
Executive Summary
Background and Context
Medical view
Good work versus bad work
Occupational health and vocational rehabilitation
Summary of Programmes designed to assist in reducing unemployment
Broader costs
Methodology
Why a Bermuda Triangle?
Themes
Generic Points
British attitudes to work
Illness and unemployment are not separate issues
Other themes
Prevention is better than cure,even with long term ill health
Occupational Health:whose services are they anyway?
Where welfare is concerned,small is beautiful
General practice:tinker,tailor,provider,landlord,
case manager,or none of the above?
The flexible workplace:oxymoron or aspiration
Incentivising the return to work
Summary of key messages
The British andWork
Prevention is better than cure,even with long term ill health
Occupational health:it is broke,so let’s fix it
Where welfare is concerned,small is beautiful
The role of general practice
The flexible workplace:oxymoron or aspiration
Incentivising the return to work
Conclusions
Footnotes
Appendices
Appendix 1 –Work Outcomes Interview Schedule
Appendix 2 – Interviewees
3
4
6
10
12
13
14
15
16
18
20
20
20
21
22
22
23
24
25
26
26
28
28
29
29
30
30
30
31
32
34
35
35
35
Bibliography
38
Health,disease and unemployment:
The Bermuda Triangle of society
01
About this
Publication
The measure of successful NHS treatment is
increasingly not a case of whether a process target has
been met, but whether that treatment was a success. In
other words, what was the final ‘outcome’? Did the
patient get better and stay well? Added to this is the
crucial question for the working age population – how
quickly did they get back to work?
This project looked at whether being at work is or could
be considered a clinical ‘outcome’ of successful health
treatment. Can keeping people in work or returning
them to work find its place as an indicator of a successful
health intervention on which professionals or institutions
can be measured? We make fourteen recommendations
and observations that we believe will be of value to
policy makers. The overall challenge is increasing the
visibility to frontline professionals and employers of
those trapped in the ‘Bermuda Triangle’ of illness,
wanting to work and unemployment - rescuing or
preventing them from getting lost there in the first place.
We are indebted to Abbott Healthcare who enabled this
research to be undertaken, and to all our sponsors for
their unrestricted funding on which we depend. As well
as driving our on-going work of involving frontline
professionals in policy ideas and development,
sponsorship enables us to communicate with and involve
officials and policymakers in the work that we do.
Involvement in the work of 2020health.org is never
conditional on being a sponsor.
Julia Manning
Chief Executive
June 2010
www.2020health.org
83 Victoria Street London SW1H 0HW
T 020 3170 7702 E admin@2020health.org
The views expressed in this document are those of the
authors alone. All facts have been checked for accuracy
as far as possible. Sponsored by Abbott. The views
expressed in this document do not necessarily reflect
those of Abbott.
2020health.org
Disclaimer
Published by 2020health.org
© 2010 2020health.org
All rights reserved. No part of this publication may be
reproduced, stored in a retrieval system, or transmitted
in any form or by any means without the prior written
permission of the publisher.
3
Health,disease and unemployment:
The Bermuda Triangle of society
The recommendations and observations that came out
of the interviews, discussions and analysis were:
02
Executive
01 The first aim of any policy change should ensure
that it is in the interests of the individual, the
employer, and society at large to align the
incentives and close the loop between health,
illness, and unemployment.
Summary
02 Raising the perception of control is key to
Recent reports have made a huge
contribution to raising the profile of the
relationship between health and work. They
have highlighted how important it is that we
have a healthy workforce, that health and
wellbeing are intrinsically connected and
that intervening early in illness is a key factor
to recovery and the return to work, whether
in the same or a different role.
improving productivity, and all the work on
leadership, engagement, and so on is actually
trying to do this. An overt focus on improving this
culture would reap rapid and sustainable benefits.
03 Getting patients back to productive and
sustainable work should become a key
objective and outcome indicator for all health
services, particularly the NHS. All forms of
clinical education need to include this aim from
their outset, and throughout both undergraduate
and continuing training.
With the increased calls for the NHS to be
held accountable for health ‘outcomes’, the
aim of this study was to establish whether
being at work is or could be considered
a clinical ‘outcome’ of successful health
treatment. Could keeping people in work or
returning them to work find its place as an
indicator of a successful health intervention
on which professionals or institutions could
be judged? This report describes how we
identified the recommendations previously
made with a view to delivering improved
health and wellbeing in the workforce. We
then used these recommendations as a basis
for interviewing experts in the field as to
their awareness of and /or agreement with
them. Their responses prompted two
particular themes that were then taken to
the front line, to test them with people
working in health, welfare and back-to-work
programmes. These were:
04 An important aspect of this emphasis must be the
inclusion in the diagnostic process of the social and
psychological aspects of an illness as well as its
physical manifestations, and treatment should
be aimed at ameliorating patients’ ability
to return to work as part of returning them
to better health.
05 One essential in this regard would be the
strengthening of direct links between the
NHS and the Department of Work and
Pensions (DWP), not damaging the formal links
and relationships that have been established
between the departments by outsourcing the
joint working.
06 There needs to be an acceptance on the part of the
employer and of wider society that it is normal
for the work environment and job roles to
change as people’s careers progress, even if
that entails physical change (seating, instrumentation,
etc), and changes to the terms as well as the
conditions of employment.
07 OH services should be made more widely
available, less focused on the needs of the
employer, and more widely based than on
Occupational Health (OH)doctors alone.
This has only been partly addressed by the
DH’s advice lines for small and mid-sized
enterprises (SMEs).
01 ‘Occupational health medicine is
irrelevant to the link between health
and work.’
02 ‘How may a return to work be
incentivised, to the benefit of the
individual, their employer, and
the state?’
4
08 Clearly, whilst there is an economy of scale in
This list reflects both that significant progress has already
been made in the understanding of the relationship
between work and health, but also that there are
noteworthy challenges ahead in changing the culture.
There was universal agreement that being able to work
should be considered a health ‘outcome’. The
challenge is increasing the visibility to frontline
professionals and employers of those trapped in
the ‘Bermuda Triangle’ of illness, wanting to work
and unemployment, and rescuing them from there
– or preventing them from getting lost there in the
first place.
providing services that help people back to work,
the clear message from this work is that any
benefits of size are more than offset by their
disbenefits in terms of intimidation and lack
of involvement.
09 There was consensus concerning the use of GP
facilities as a venue for the work and advice
required to help the workless get back to work.
Their local nature and size and relative informality
are helpful, and they could be populated by staff
from private and/or voluntary organisations. The
idea of linking the tasks associated with the return
to work to specific health care issues at a single
venue was also appealing.
10 However, predicting the absence of sickness or
a reduction in turnover require a leap of faith, and
such faith is often the missing ingredient in
introducing some of these changes. This may be
one area where legislation concerning the employee
benefits mentioned above may be appropriate.
11 It should be possible to introduce some kind of
tapering scale as health and workfullness
improve, by which welfare payments reduce
as ‘real’ income grows without any step changes
being triggered in a way that avoids the classic
benefits trap.
12 What is required is genuine early intervention,
preferably in time to preempt the whole workless
phase, particularly when predictable health issues
are causing the problem. There needs to be
increased awareness of how important
appropriate prescribing is in helping people
return to work as quickly as possible.
13 It may be that medical support for such
interventions could be an extension of the
‘fit note’ idea, using the GP’s imprimatur to
validate such discussions, and preempt any punitive
reaction by less enlightened employers.
14 With the rising awareness of and interest in work
related stress, it may be that increasing the
profile of the Health and Safety Executive
(HSE) in this area could bring sufficient pressure
to bear on employers on its prevention and more
effective treatment of stress. Fear of liability and
of compensation may be a useful adjunct to the
moral high ground.
5
Health,disease and unemployment:
The Bermuda Triangle of society
As the demography of the developed world changes,
there is a need to reconsider our attitudes to work and
unemployment, and to explore the interventions that
lead to and maintain sustainable employment. An ageing
population means a growing incidence of chronic illness
will affect those in work as well as those with caring
responsibilities. There is overwhelming evidence that
long periods away from work is detrimental to patients’
health. The annual cost of absence and the worklessness
associated with working-age ill-health is estimated to be
over £100 billion. It has been shown that
musculoskeletal disease (MSDs) and stress are the most
common health reasons for people taking time off of
work but there is also clear evidence of how not working
is detrimental to health. This review of existing
publications explores some of the recommendations that
have been made in the past few years, building largely
on four major pieces of work:
03
Background
& Context
01 In spring 2008 the Director for Health and Work,
Dame Carol Black, published Working for a
Healthier Tomorrow, the first review of its kind
that examined the health of Britain’s working age
population. It was the culmination of a crossgovernmental initiative that started in 2005 and
saw the formation of the Work, Health and
Wellbeing Directorate. The Black report made
a number of recommendations, amongst which
a number stood out: the adaptation of GP advice,
the initiation of pilots for Fit for Work service,1
a health and wellbeing consultancy service, and
more health information about the relationship
between health and work.
02 The government’s response to this review,
Improving Health and Work: Changing Lives fully
accepted Black’s advice, making both a social and
economic commitment to the 2.6 million people on
incapacity benefits and the 600,000 people who
make a new claim each year. Part of this
commitment was the intention to transform the
medical ‘sick note’, the introduction of mental
health co-ordinators in Job Centres, the creation
of occupational health advice lines for small and
mid-sized enterprises (SMEs) and a National
Centre for working age health and wellbeing.2
03 Acting on the aforementioned government
response, Dr Steve Boorman, Chief Medical
Adviser to Royal Mail Group, oversaw an NHS
review in the autumn of 2009. In its efforts to ‘get
its own house in order’ the NHS fully accepted the
need to improve the health and wellbeing of its
staff. Boorman’s report suggested that improving
the health and wellbeing of NHS staff could save
over 3.4 million working days annually, the
equivalent of 14,900 full time staff. As Europe’s
largest employer, the annual cost of staff sickness to
6
the NHS is estimated to be a staggering £555
million.3 His recommendations include a
‘prevention focused health and wellbeing strategy’
with staff health and wellbeing becoming a key
factor in senior management performance
assessments. The NHS intends to support early
interventions especially in the areas of MSDs and
mental illness, in order to facilitate earlier returns
to work. This is in line with the NHS constitution’s
intention to help keep staff fit and healthy.
However, it should be remembered that there is
a deep inherent cynicism amongst those working
in the NHS, so the notion that staff health and
wellbeing are significant priorities is likely to take
considerable time and effort to implement effectively.
•
Key Facts and Figures
•
•
•
•
04 The Marmot Review (Spring 2010), commissioned
by the Government, looked at health inequalities,
and stated six key policy objectives, one of which
was to ‘create fair employment and good work for
all’. The review recommended prioritising
employment programmes, ensuring that equality
legislation is upheld, implementing existing
guidance on stress management, and generally
creating greater security and flexibility
in employment.
•
•
•
Several of the Marmot Review’s policy objectives link
directly to the ‘world of work’; these include: enabling
people to maximise their capabilities and maintain
control of their lives; ensuring healthy standards of living
for everyone; creating healthy and sustainable places and
communities; and strengthening the role and impact of
ill health prevention.4
•
•
As the Chief Executive of the Royal College of Nursing
commented on the Marmot Review: “As a nation we simply
must not tolerate the difference in life expectancy shown in this
report, or the many years spent in preventable poor health...of course
individuals need to make health choices for themselves, but to tackle
this inequality, government, public services and communities need to
work together”.5
The relationship between work and health is
multifaceted, and impacts on areas of social justice,
generational poverty and health inequalities. There is an
archetypal public health issue in trying to get people to
stay at work, back to work or into work, and to achieve
these aims requires the adoption of new perspectives to
create open dialogues between Government, healthcare
practitioners, employers and the individual. The
traditional bio-medical model of disease is insufficient to
explain and to deal with the complexity of the underlying
issues, and a new bio-psycho-social model is required to
help understand the importance of wider preventative
measures such as job design and skills analysis.
7
175 million working days in Britain are lost due
to ill health annually
Cost of sickness absence and worklessness in
Britain estimated at £100 billion annually
The World Health Organisation estimates that
by 2020, depression will have become the second
leading cause of disability in the world6
80% of the adult population will suffer with back
pain at some time in their working lives
Approximately 6.9 million people of working age
report themselves as disabled; this equates to 19%
of the working population
7.6% of the working age population (2.6 million
people) claim incapacity benefit with 607,000 new
cases annually; 1.5 million of these have been in
receipt of this benefit for more than 5 years7
One quarter of GP consultations are work related
5.4 million people declare a work-limiting
disability, of whom 50% are in employment
1.2 million people who worked during 2009 were
suffering from an illness (long-standing as well as
new cases) that they believed was caused or made
worse by their current or past work; 551 000 of
these were new cases8
Around 46% of people with disabilities are
economically inactive9
Health,disease and unemployment:
The Bermuda Triangle of society
In 2006 an NHS Musculoskeletal Framework was
devised as part of the Government’s strategy for long
term conditions, which set out a vision in which people
with musculoskeletal conditions could access effective
clinical advice, assessment, diagnosis and treatment. It
was proposed that this would be accomplished through
systematically planned and integrated services13. As it
stands, the key service recommendation of the framework
remains woefully unheeded, with the national average for
implementation of the proposals at only 16%.14
03
Background
& Context
Health conditions are not static but can change over
time, and the means of managing these also need to be
flexible; a medical model might be appropriate during a
period of acute ill health, but within a short time
psychosocial issues are likely to predominate. After
several months, the whole nature of the illness may have
changed again, as the impact of prolonged worklessness
takes its toll10. Two of the most pervasive reasons for
employees absence from work are mental illness and
musculoskeletal disease, and these services need to be
considered differently in the context of patients, their
friends and families, employers, GPs and the wider NHS.
In 2007 the National Rheumatoid Arthritis (RA) Society
surveyed over 700 RA sufferers about their working lives.
Of those people not working, the survey found that
nearly two thirds (64.8%) were not in employment
because they gave up work early as a result of their RA,
this included people above and below the statutory
retirement age1. With 387,000 RA sufferers in the UK,
the costs generated by this burden of disease are
expected to exceed £3.8 billion annually. However
Rheumatoid Arthritis is just one specific musculoskeletal
problem, and many other people suffer with more
generalised conditions like ‘back pain’. Overall
Musculoskeletal Disorders (MSDs) affect over a million
people in the UK, accounting for 9.5 million lost
working days and a cost to society of over £7 billion in
real terms15. Apart from the purely economic costs, there
are genuine inequities as people with RA (and MSDs
more broadly) miss out on other opportunities through
their lives.
Musculoskeletal Diseases (MSDs) are common, may
be progressive and are a leading cause of disability and
sickness absence, affecting twice as many people as stress.
Despite 80% of adults suffering some form of back pain
at some point in their lives, spending per patient can vary
dramatically between parts of the country from £95 per
person in Lewisham PCT to £1379 at Western Cheshire
PCT,11 a variation that is not easily explained. In addition
to such obvious healthcare inequalities there are also
widely varying views about the MSD sufferer’s ability to
work, perhaps because MSDs are the most prevalent
cause of work-related ill health and vary enormously in
their severity, duration, and psychological impact.
In 2009 both ARMA (the Arthritis and Musculoskeletal
Alliance) and the National Audit Office evaluated the
progress of the Musculoskeletal Framework and
recommended that a national clinical director be
appointed for musculoskeletal services and that there
should be clear lines of accountability for
the implementation of the 2006 Musculoskeletal
Framework. They also suggested drawing on the existing
strategies for other specific conditions (such as cancer) to
create a model that would establish service priorities,
delivery models and funding streams1, and advised that
PCTs should not commission musculoskeletal services
without first making an accurate assessment of the needs
of their population in terms of their quality of services,
life, information, training and development16.The UK
has yet to succeed in promoting the cost effectiveness of
early intervention.
One person’s ‘aches and pains’ will be another’s ‘acute
sciatica’ and yet another’s ‘arthritis’. There is often a
strong psychological overlay to MSD symptoms,
particularly if they are protracted.
The Work Foundation has analysed the fitness of various
European countries labour force with respect to
musculoskeletal disorders. One report concludes that up
to 2% of GDP is lost to MSDs and that there is an even
higher cost in human terms with respect to sufferers’
quality of life.12
8
forum in which to discuss their difficulties. A research
report for the Department of Work and Pensions (DWP)
that surveyed line managers’ attitudes found that they
felt that supporting employees with mental health
problems placed significant demands on their time and
was hard to keep confidential21. A report for managers
on stigma claimed that ‘most of the ideas are ordinary
good management practice. The way forward is to bring
mental wellbeing within the boundaries of ordinary
working life.’22
Mental Illness had a dedicated National Service Framework
(NSF) on Mental Health introduced over ten years ago
which promised to deliver mental health promotion and
support services specifically to meet the needs of the
working age population. Since 2001 there has been an
increase of £1.7 billion on the expenditure for adult
mental health services. This has meant 64% more
consultant psychiatrists, 71% more clinical psychologists
and 21% more mental health nurses than in 199717. In
spite of this, mental illness has become the biggest cause
of sickness absence and of incapacity benefit, with claims
for the latter rising 15% proportionately between 1996
and 2006, so that despite an overall drop in incapacity
benefit claims, mental health claims have increased. Of
the 600,000 new incapacity benefit claims each year,
200,000 are related to mental illness sufferers, many of
whom feel that they would have the potential to remain
in work with the help of their employers and GPs.
The economic costs of mental illness linked to people’s
ability to work have ranged from £789m in Northern
Ireland, through £2.3 billion in Scotland, to £23.1
billion for England. These figures include nonemployment (unemployment and economic inactivity),
sickness absence, unpaid work and premature mortality.
Around 60% of people who have a common mental
illness are working, compared with 70% of people who
do not23. Conversely, mental illness sufferers have argued
that the welfare state actively discriminates against
claimants without a physical disability, who are more
likely to be branded malingerers.24
There are often mental health consequences of
unemployment for other reasons; people who become
unemployed because of a physical health condition are
much more susceptible to mental health problems, and
indeed, unemployment itself may be considered as a
factor that can precipitate mental illness. In 2009, Rachel
Perkins was commissioned by the Department of Work
and Pensions to undertake a review of mental health and
employment. In her report she suggested a vision with
three central objectives: increasing capacity; providing
support and monitoring effectively. To achieve these, the
report recommended improving ‘welfare to work’
services, commissioning employment specialists and
providing short unpaid ‘internships’ to help patients
familiarise themselves with the world of work18. In March
2010 the Department of Health published its report New
Horizon: towards a new vision for mental health. It suggested
that looking at the root causes of mental illness was
fundamental to national economic success.19
The benefits of working in a socially inclusive way are
self evident and include the removal of the severe effects
that stigma has on the individual and their family. The
RCPsych says that to achieve this, there is a need for
‘recognition of the range of interventions that can
improve both clinical and social outcomes for service
users, and ensuring that these are commissioned’.25
Rachel Perkins’ DWP review stated that ‘people with
mental health conditions remain among the most
excluded within our society, particularly in the workplace.
We know that work improves mental health and
wellbeing and most people with a mental health
condition would like to be in work and pursue a career’.26
At the end of 2009 the Department of Health launched
its New Horizons programme which built on the 2000
NSF for Mental Health. This identified multi-agency
commissioning and value for money as central strategies
to mitigate the societal, individual and economic burden
of mental illness. Proposed actions included better work
place support and employment opportunities for people
with a mental health problem, and the report identified
work as an ‘important outcome of the treatment of
mental illness in health settings.’27
It is reported that one in six workers will experience
stress, depression or anxiety at any one time, with one in
four of the whole population having a diagnosable
mental illness some time during their life. The vast
majority of these continue or return to work successfully.
Despite the NSF on Mental Health and the 1995 Disability
Discrimination Act (DDA), many of those with mental
illness never declare their health problems to their
employers, and the enduring stigma that surrounds
mental illness still results in employment discrimination.
The Royal College of Psychiatrists (RCPsych) has said
that the continued stigmatisation of mental illness in the
work arena means that many potential recruits may be
denied entry into employment as they are seen as
unsuitable, even though they meet all the competencies
for the profession20. Linked to this point is that those with
mental illness who are in employment often find the
work environment an unsuitable and inappropriate
At the same time, the Government launched the first
mental health and employment strategy Working our Way
to Better Mental Health: a framework for action. This proposed
a framework which aspired to transform the ways we as
individuals think about mental health and work; and the
ways in which employers and public bodies support
people with mental health problems.
9
Health,disease and unemployment:
The Bermuda Triangle of society
03
Background
& Context
The Sainsbury Centre for Mental Health calculated
some specific statistics which estimated the sickness
absence costs of this kind of illness to employers
annually:
•
•
•
•
Mental health services and localism
In December 2009, Health for Work Advicelines
(jointly delivered by the DWP and the NHS)
began operating in England, Scotland and Wales
in order to help SMEs support their employees
(although this is project not mental health
specific). The Mental Health Co-ordinator
Network was also launched, which aims to put a
co-ordinator in every Job Centre Plus district.
This is hoped to help to develop links between
health and employment services locally.
£8.4 billion a year in sickness absence of up to 70
million lost working days
£15.1 billion in productivity losses or
‘presentee-ism’ (when employees come to work
in spite of illness) which costs more because it
is more common among higher-paid staff
£2.4 billion a year to replace the staff who leave
their jobs because of mental ill health
Tomorrow’s People, a voluntary organisation that
helps people back into work has been
recognised as an exemplary model. In a report
evaluating how worklessness can impact on
mental health, Tomorrow’s People were able to
drive down anti-depressant drug prescription by
means of a new referral process they formed
with a local GP. Mindful Employer is another
initiative, consisting of a charter supported by
over 660 employers to think positive about
mental health. This has become a network of
supporting organisation to adopt a good practice
on mental health.1
£8 billion could be saved by British businesses
if mental health was managed more effectively
at work.28
An example of these figures being turned into action is
illustrated by the fact that BT has reported that its mental
wellbeing strategy has led to a reduction of 30% in mental
health-related sickness absence, and a return to work rate
of 75% for people absent for more than six months.29
Employment is recognised as an important component
of recovery from illness, both physically and, by dint of
its impact on confidence and self management,
psychologically. It allows a person to step out of the
sick/dependent role and so is central to self esteem and
self motivation. However there is some concern that
work could become a faddish ‘panacea’, and work as the
only acceptable outcome to an episode (be it of illness
or unemployment) could add pressure to an individual’s
situation by excluding any other possible solutions.30
Medical view
Encouraging GPs and others to recognise the part that
they play in making work a potential outcome of
treatment has been an ongoing challenge. They could
be key contributors to achieving a healthier workforce
and saving scarce welfare resources, by changing the
emphasis of their involvement when presented with a
patient absent from work from incapacity to capacity.
The ‘statement of fitness for work’ (or ‘fit note’) was
10
introduced in April 2010, and is hoped to save
£240million or more over ten years. Unlike its
predecessor sick note, this new form allows GPs to state
whether a patient ‘may be fit for some work’.
about patients’ use of other specialist services. The
conclusions of this pilot study emphasised the need for
GPs to increase their awareness of the therapeutic value
of work and the availability of support for them,
although employers had previously argued that GPs do
not understand the problems that long term sickness
absence can cause.
Although the British Medical Association (BMA)
welcomed the new move as a more intuitive way of giving
patients advice, there were reservations about employers
having the awareness and responsibility to act on the
changes. The qualification of GPs to advise on this topic
was also mentioned by BMA General Practice Committee
Chairman Dr Laurence Buckman, who was reported as
saying that ‘GPs need to be careful they are not drawn into
making comments they are not qualified to make, because,
unlike Occupational Health doctors, they are rarely in a
position to know the precise details of a patient’s working
conditions, neither do they have specialist knowledge of
workplace hazards’. The idea of ‘fit notes’ was also
received critically by Local Medical Committees who
thought that they might be open to forgery.31
To this end, there have been increasing efforts to boost
GPs’ awareness of their enhanced role in patient
employment issues. The Royal College of General
Practitioners (RCGP) is running a national education
programme (in the form of half day workshops across
the country) to tackle this knowledge deficit. Their aim
is to equip up to 4500 GPs with a better understanding
of how their duty of care extends beyond clinical
outcomes. By May 2010, roughly 1000 GPs had received
this training.34
Another requirement of the ‘fit note’ is that line
managers will need to be equipped to deal with GPs’
advice. In order to do this effectively, employers will need
to have access to current information about their
employees.35 However UK society still struggles to grasp
that health and wellbeing at work are not just medical
issues, but extend far beyond, to areas such as
engagement, and self worth, making the information
needed much greater than mere medical records. To
emphasise the point, there seems to be a clear link
between the perceived effectiveness of management at
work and employees’ feelings of wellbeing. The problem
in engaging companies and their managers is how to
deal with the apparent conflict of interests that arises
when employees at work are affected by health problems,
especially when they may have arisen from the work
environment itself. Clarifying this conflict, and finding
ways of dealing with it is key to improving health at work
and clinical interventions that have work in mind. It may
be that occupational health services could have an
enhanced role in this function.
Another anxiety in primary care was that an undue focus
on the ‘return to work’ might conflict with the traditional
role of the GP as patient advocate, and that although
the eventual work outcome would be beneficial to
patients, patients may not view it as such. GPs are
increasingly aware how job retention or an early return
to work can be beneficial to patients, but reforming the
medical statement is clearly only a part of changing this
mindset. Society also needs to review how GPs and the
other health agencies could intervene earlier and in a
different manner in order to encourage selfmanagement, and prevent the decline into ‘victim’ role
that often goes with illness and unemployment alike.
This will inevitably challenge traditional health thinking
to go beyond physical symptoms with its impending
catastrophes and over-medicalisation.32
A pilot to assess GPs’ interaction with their patients
around the subject of sick leave was intended33 to
ascertain how GPs understood their remit in this area,
the mode of their discussions with patients, and how well
connected they were with the appropriate local
specialists and organisations. Several issues were
identified as barriers to GPs’ involvement in the ‘return
to work’ process. Foremost was their perceived need to
preserve the trust of the doctor-patient relationship, as
they often felt trapped between their patients and the
benefits system or the employers (or all three). Other
factors that emerged as obstacles included the time
needed to do this work properly, the problems of
maintaining continuity of care, funding the new system,
GPs’ limited occupational health expertise and patients’
lack of knowledge of the system. As far as understanding
the other organisations that might have been involved,
there were mixed messages about GPs’ knowledge of
these, but misunderstanding of the role of the Job
Centre Plus system was widespread, as was scepticism
11
Health,disease and unemployment:
The Bermuda Triangle of society
03
Background
& Context
Although there is often an assumption that work during
illness is harmful and rest away from work is therapeutic,
the converse notion, that work is good and
unemployment is bad, is simplistic. High quality
employment is important in maintaining employees’
satisfaction and hence their performance, but the equal
opportunities implied by ‘high quality employment’ also
help to address any inequalities that arise around access
to good working opportunities. Good jobs have long had
an association with good quality education, and
education is linked to longevity.36
Good work versus bad work
Men’s working health
There is an additional benefit in incorporating
health services at the workplace. As National Men’s
Health week highlighted, men generally visit their
GPs less often than woman, work for longer hours,
do more overtime, and retire at older ages. More
men than women have symptoms without formal
diagnosis, and they are more likely to become
alcohol dependent, abuse drugs and commit
suicide. There are huge disparities between the
sexes in areas such as mental illness too, probably
more in the reporting of illness than in its incidence.
Even without formal research, it makes intuitive
sense that wellbeing at work is likely to be an
important contributory factor to this disparity, as
men are exposed to the lack of job satisfaction,
work related stress, and the pressures of long
working hours more than women, even in today’s
emancipated society.
Inequalities are also amplified by the fact that employers
give lower priority to job retention for unskilled
employees than for their more highly skilled ones.
Smaller companies often have less flexibility than large
companies to change employees’ roles as their health
varies, or to adjunct the skill mix in different roles. SMEs
are also less likely to be aware of issues surrounding
disability legislation.
Thus, the workplace may be considered an
excellent setting for public health practice, for men
in particular, and this work should include looking
at gender specific variations of health and
wellbeing. Royal Mail’s workforce, for example, is
85% male, and so the company focused on raising
health awareness amongst staff to see if this would
reduce absenteeism. Part of this initiative was to
circulate health pamphlets in a similar format to the
‘Haynes’ car maintenance manuals, and work by
the London School of Economics showed that
absence reduced from 7% to 5% as a result. (Men’s
Health Forum, National Men’s Health Week 2008)
The factors associated with good jobs have been
categorised as control, security, diversity of work,
rewards, fair procedures and social capital37. The Work
Foundation’s 2009 report Good Jobs suggests that most
employers recognise the value of ‘good jobs’, realising
that they have much to gain from them in terms of
maintaining a more productive, healthier, stable and
committed workforce. One factor that that seems to
remain relatively unrecognised is the impact on
productivity and the ‘health’ of the organisation of
sickness absence, presentee-ism and staff replacement.
Health and safety at work is another area that affects
employees’ health and wellbeing, and is still probably
underdeveloped (despite the urban myths!). The Health
and Safety Executive (HSE) reported that for 2008/9 over
1.2 million employees suffering a health condition felt that
this was made worse by work, with over half a million
reporting new issues. This meant a total loss of 24.6
million working days due to work related ill health alone.38
Alongside health and safety and job design it is evident
that in repositioning work as a health outcome there
needs to be an ability to match skills for a particular job
12
with the aptitudes of the employees. BUPA, for instance,
published a report on the future opportunities and
challenges for workplace health up to 2030 - a paper that
analysed how UK demographics, disease trends, and the
economy were likely to interact with the nature of
employment.39 The report anticipated that a knowledge
based economy was likely to change job design and that
this would have consequent effects as ‘knowledge
workers’ (often required to apply their skills flexibly and
be accessible around the clock) often have a poorer sense
of wellbeing and quality of life than other groups with
more routine in their work. Mismatches of skill sets and
job requirements will affect workers’ wellbeing. Theresa
May MP, (writing as the then shadow Secretary of State
for welfare) emphasised how a skilled workforce would
be an essential part of any welfare reforms, and that
in developing these skills, it was vital that nobody got
left behind.40
long term rehabilitation. Employers have become
increasingly aware of the benefits of OH which is
perceived as part of an employer’s duty of care to its
employees. However, the practicability of this philosophy
depends on the size of the company, the costs of
providing such a service, and the local perception of
health as a business priority.
Employers look to government promotion to widen
access to OH services, as well as wishing for reform of
the costly legal processes that accompany compensation
claims. Removal of tax disincentives such as the current
‘benefits in kind’ system would also go a long way toward
ensuring that employers invest in their employee’s health.1
From the employee perspective, OH has been seen as a
management tool, whereas it is self evident that OH
professionals should be more sensitive to both employee
and management concerns. It would be helpful if some
of the routine health checks were redesigned, and
focused more on health promotion than preemployment checks and health surveillance,1 as access
to these services is a vital component of any early
intervention. Previously it has been suggested that early
intervention itself should be streamlined with nationally
agreed service standards, taking into consideration that
professional expertise is key to reform. The need for
better referral systems and greater OH provision has also
been highlighted.1
In the context of increasing globalisation, companies
need to focus ever more tightly on communication and
the development of organisational ‘emotional
intelligence’. This should include the consideration of
mental health issues in the work place, and the
organisation of clear responsibilities at work, and for the
‘return to work pathway’ for those who have been
unwell.41 The key seems to be that a holistic approach is
vital, and needs to be consciously maintained at all times.
Line managers are not just extensions of their
corporation’s arm, they are the tangible human link to
the organisation for all employees.
Vocational rehabilitation (VR) has often been seen as
separate from the usual OH working but is actually
synonymous with many of the overall aims of OH. It is
designed to assist in whatever way possible those with
health conditions to return to or remain in work by
taking an individual approach on the return to work,
workplace accommodation and early intervention. This
“process of facilitation”42 is fundamental to the
maintenance of mental health.
“Rehabilitation cannot be a second stage after healthcare has failed”
– Palmer and Fox 2007
Occupational health and vocational rehabilitation
Traditionally Occupational Health (OH) departments
have been responsible for the health of workers, and for
a safe environment, in terms of hazard assessment. The
Black Review highlighted the fact that only one in eight
workers currently have access to any form of OH. The
review recommended a greater emphasis on OH, even
extending its reach to people who are not presently in
employment. This could be part of a new early
intervention process. In recent years much OH has been
outsourced, and internal OH departments have
increasingly been disbanded. It has yet to be seen how
this has affected employee accessibility and satisfaction
with services.
Setting up a UK framework for vocational rehabilitation
was suggested in 2004 by the HSC (now HSE) in its
‘A strategy for workplace health and safety in Great Britain to
2010’ but there has been little mention of progress. The
Government has said that it was not in a position to
implement a new approach for VR, but that it fully
supports stakeholders who want to do so.
The huge challenge to OH is to overcome its historical
detachment from mainstream healthcare. Traditional
OH departments can do various things, and a number
of measures have been recognised as helping to prevent
the drift of employees onto long term benefits. These
include risk assessment, disease and absence
management, health prevention and promotion, and
13
Health,disease and unemployment:
The Bermuda Triangle of society
incapacity benefits must attend five further WFIs. The
Pathways programme comprises a ‘choices’ package to
improve individuals’ work readiness, a £40 return to
work credit and a discretionary fund that advisers can
allocate to increase the chances of clients finding work.
03
Background
Although the programme was hailed as a success when
it was originally piloted in 2003, attempts to expand and
replicate the programme in 2006 showed that the
Pathways had had no statistically significant impact on
work, earnings or health outcomes. Within the original
pilot areas however, analysis showed that Pathways
increased the proportion of clients who were in paid
employment 19 months after they made an incapacity
benefit enquiry and reduced the chances of individuals
reporting day to day health problems. This disparity was
explained by possible variations between the studies.47
& Context
Summary of Programmes designed to assist
in reducing unemployment
In May 2009 the DWP estimated that there were 4.97
million out-of-work benefit claimants of working age, of
whom 2.62m were claimants of Employment and
Support Allowance (ESA) and/or Incapacity Benefits
(IB).43 From October 2008, ESA replaced Incapacity
Benefit and Income Support paid on the grounds of
incapacity. This benefit attempted to cut costs and
change the culture of long term sick leave, and it
included a new work capability assessment. Of 292,300
people tested since October 2008, only 89,600 were
assessed as unable to carry out full time work, which left
69% who were considered well enough to work, and
hence moved onto the Job Seeker’s Allowance (JSA).44
Presently, Pathways contracts have been assigned to
multiple organisations, the largest of which is A4e,
a multinational recruitment and training service.
Questions still remain about the cost-benefit of the
Pathways programme. If calculated conservatively, it has
been estimated that the net return to the exchequer was
£1.51 for every £1 spent on the Pathways programme.
However some costs were not incorporated in this
analysis (such as administration, tax losses and utilisation
of the NHS) and this calls the results into question.48
Interagency concerns about the Pathways work remain,
as is shown by the fact that over half of PCTs have not
made links with their local scheme.49 Furthermore
Pathways is said to have failed for those with mental
health issues and the National Audit Office have said
that the programme provides poor value for money.50
The Welfare Reform Act 2009 aimed to reduce benefit
dependency and strengthen the benefit contract. Despite
public anxiety about benefit fraud, there was more
concern among policy makers that the degree of
conditionality in the benefit system might work in a
perverse way and actually lead to less support for the
people who needed it most. It was felt that getting people
off welfare benefits should not in itself be perceived as
the goal.45
Access to Work is another Government scheme that helps
employers to make assessments and provides funding for
alterations to be made to the working environment. This
benefit contributes towards the costs of equipment an
individual may need at work, offers a communicator at
job interviews, helps to adapt premises where necessary,
and can pay for a support worker. It can also pay towards
the cost of getting to work if an individual cannot use
public transport. Reportedly between April and
September 2009, this scheme helped 26,540 individuals.51
Helping this group depends on a greater understanding
of why people make these particular benefit claims, and
adaptation of national strategies may be required to
allow a ‘fit’ in local areas. Overall there has been a
decline in the total number of claims, but with a shift
from musculoskeletal problems to mental health issues.
DWP studies have shown that alcoholism and drug
abuse have increased alongside Invalidity Benefit claims
due to mental ill health. It has been suggested that other
associated factors like poor employment history were
linked to this trend and should be taken into account
when looking at localised groups.46 Two major
programmes were initiated as part of the overarching
‘work for your benefit’ scheme; these were Pathways to
Work and Access to Work.
From April 2008, everyone on Incapacity Benefits has
been able to access Pathways to Work. Under Pathways,
any individual aged between 18 and 60 who claims
incapacity benefits must attend an initial work-focused
interview (WFI) with an IB personal advisor eight weeks
after making their claim. Most people remaining on
14
The costs and effects of absence from work have been
widely documented, but the costs of presenteeism, poor
productivity of replacement labour, and extra
management costs often go undetected. The Chartered
Institute for Personnel Development (CIPD) and the
Confederation of British Industry (CBI) found that very
few organisations make rigorous assessments of the costs
associated with employee absence, and that when they
do they tend to take an ‘accountancy approach’ without
mention of impact on productivity and profitability.52
There are clear gains to be made by improving absence
management, but this has yet to be fully grasped by
organisations in the UK. In their report the CBI also
noted that ‘Annual absence surveys are not rocket
science, but a blend of systematic use of absence
procedures and improved communication between
staff and management, supported by employee
wellbeing policies’.53
Broader costs
This ‘improved communication’ may simply comprise
earlier one-to-one follow up procedures after incidents
such as sickness absence. Employee wellness
programmes have been slow to be taken up as employers
have not perceived any impact in improving the health
and wellbeing of their workforce. This is expected to
change as the focus on corporate social responsibility
increases. A study of workplace wellness programmes
found promising cost benefits in important areas such as
sickness absence, staff turnover and accidents. These
programmes were found to be far more successful when
they were tailored to employee needs.54
It has also been suggested that the National Institute for
Clinical Excellence (NICE) guidelines on the cost
effectiveness of new medical treatments should consider
incorporating social and work factors into their
calculations as well, so that the broader benefits of new
treatments may be recognised. This raises the perpetual
public sector issue of whether the department whose
budget funds an intervention should also be the one that
reaps its rewards. A classic example would be the
potential cost shifting when the DWP saves in benefit
payments because of expenditure from NHS budget for
treatment that accelerated a patient’s return to work.
This consideration was addressed and rejected by the
Kennedy Review55 but other reports have found that a
more cross cutting approach resonates better with both
professionals and the public56. Taking this approach to
the frontline would mean that those who held local
health budgets could start thinking about savings to the
entire welfare budget and which clinical treatments have
the most impact on ability to work, hence the question
about ‘horizontal integration’ posed during this project.
15
Health,disease and unemployment:
The Bermuda Triangle of society
This report is built on the foundations of a selective
literature review which was based on expert
recommendation, selective news streams and self
published, publicly available literature from various
organisations. Many of the fact and figures come from
programme specific searches from the Department of
Health and the Department of Work and Pensions. Other
statistics have been drawn from independent studies.
04
Methodology
Ideas that emerged from the literature were then drawn
together to inform a semi-structured interview schedule
designed to combine non-directive questioning with the
opportunity to explore specific issues in some depth (see
appendix 1).
The second stage of our research was to conduct over
25 expert interviews with senior figures from a number
of diverse organisations, including the NHS, voluntary
sector, health insurance providers, private healthcare
companies, employee service providers and case
management organisations. We spoke not only to Chief
Executives, but also to local managers and health
professionals (full list available appendix 2). In each case,
interviews took place either in person or over the
telephone, and were set out relatively informally on a
semi structured basis that allowed the interviewee to lead
or elaborate. Interviewees were assured that their
comments would remain unattributed and were
encouraged to express their true opinions, even if they
were not in keeping with their organisation’s views.
16
The two themes discussed in each case were drawn from
the findings of the interviews, and were:
From the interviews were synthesised a number of
recurring themes which were tested in local communities
by carrying out a short series of workshops. In the event
three workshops were carried out, in Coventry,
Newcastle and Exeter in the period from December
2009 to January 2010. These were attended by a diverse
range of people including physiotherapists, occupational
therapists, occupational health physicians, health
industry representatives as well as people providing
employment services to mental health users and
members of professional bodies. These workshops were
designed on a ‘confirm and challenge’ approach,
intended to encourage a number of groups to take part
in active discussion on several different topics. Originally,
it had been intended to run four discussions in each
session, but the number of people attending each of the
workshops made this impractical. Instead the
participants in each workshop were divided into two
groups, each asked to discuss one of two themes. Half
way through the session, the members of each group
(except one) rotated, the remaining one acting as the
designated ‘guardian’ of the theme. They were also
responsible for facilitating and reflecting the findings of
each discussion to a plenary session at the end of
the workshop.
01 ‘Occupational health medicine is irrelevant to the
link between health and work’
02 ‘How may a return to work be incentivised, to
the benefit of the individual, their employer, and
the state?’
The findings of the workshops were collated along with
the themes emerging from the interviews, and
amalgamated into this report.
The project was supported by an external steering group
of unpaid experts with whom the process and the
findings of the work were discussed on several occasions;
we would like to acknowledge their invaluable help, and
thank them for their contributions.
17
Health,disease and unemployment:
The Bermuda Triangle of society
The original hypothesis that underpinned this piece of
work concerned the specific link between ill health and
work, in the knowledge that long term chronic
conditions such as muscular skeletal disease and mental
illness have a dramatic impact on the workforce and its
productivity. However, it soon became apparent that the
linkages are more complex, and that there is a striking
relationship between unemployment, ill health and work.
05
Why a Bermuda
Triangle?
This is quite hard to explain in concrete terms, but it is
clear that unemployment causes ill health just as ill
health causes unemployment, and that a return to work
can (but only if used appropriately) improve the health
of both groups. Thus, for example, someone with a
chronic condition such as rheumatoid arthritis (RA) or
endogenous depression risks losing their job in the
current work environment because there is rising
unemployment (and so replacing them is easy).
There are no real incentives for an employer to adapt
work circumstances to suit the needs of the disabled
person, whether in terms of flexible hours (depressed
people usually function more effectively in the latter part
of the day) or physical changes (such as special taps in
washrooms to suit the needs of those with physical
frailty). This makes getting such people back to work
highly problematic.
The issues get worse if unemployment (for any reason,
not just for those with a chronic illness) continues for any
protracted period of time, as the chances of the
unemployed person getting back to work diminish
rapidly and those who have been unemployed for longer
than six months (for any reason) have a lesser chance of
ever getting back into permanent employment. Studies
have shown that although these limits are unclear, the
best window of opportunity for a return to work is
between one month and six months.57
The next loop in the downward spiral is that there is a
clear link between long term unemployment (for any
reason) and the illnesses of low self esteem such as
depression. Ever since the rise of the Puritan work ethic,
Western societies have used employment as a key
indicator of worth, particularly where men are
concerned, so that we tend to adjust our assessment of
a person’s status according to the work that they do, and
we apply that measure to ourselves as well as to others.
Put starkly, those who are unemployed are seen (and see
themselves) as having less value as people than those in
work. This is bad enough, but the phenomenon is more
marked amongst those who have been in work and then
become unemployed.
They tend quickly to adjust their self esteem downwards,
with the rise of self doubt and the loss of confidence that
is bound to make their affect worsen, along with their
ability to get back into work, and the longer the
18
unemployment goes on, the worse it becomes, both in
their own minds, and in the minds of potential
employers. In our society, it is this final twist that
completes the vicious circle that creates and perpetuates
a lacuna of isolation and neglect, a kind of metaphorical
Bermuda Triangle.
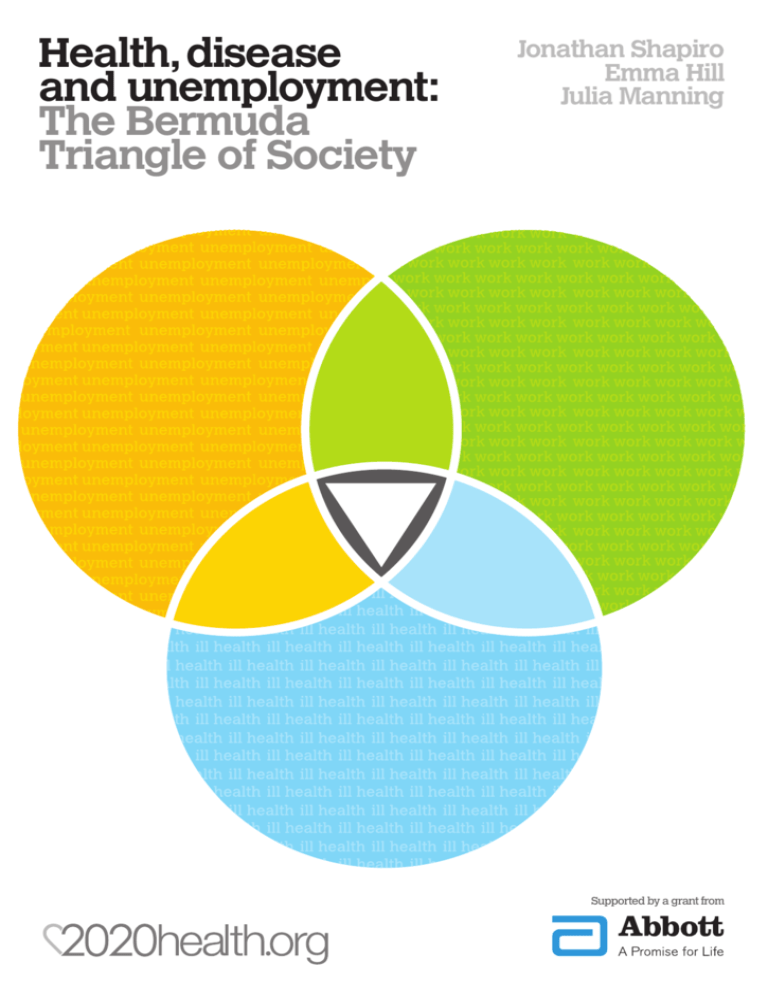
It may be more helpful to illustrate this dynamic
diagrammatically, as shown below:
Unemployment
Work
Ill Health
The Bermuda
Triangle
There is a certain invisibility to the group caught
between the three pillars of work, ill health and
unemployment, and it was that isolation and sense of
mysterious disappearance that led to the coining of the
‘Bermuda Triangle’ phrase, and most of the themes and
messages that came out of the interviews and workshops
were aimed at increasing the visibility of those trapped
in the triangle, and helping to rescue them from there.
The themes are generally arranged in no particular
order, although there are one or two generic points to be
made first.
19
Health,disease and unemployment:
The Bermuda Triangle of society
Generic points
06
Themes
Underpinning the whole of the study, and present in all
the discussions that took place as part of it was the
premise that ‘work of the right kind is good for you’. The
evidence for this has already been cited, and there is a
strong common sense element in that statement, and yet
it quickly became clear that there was a dissonance
between what people said about the subject and what
they felt about it. In everyone’s tone of voice there was
a wistfulness as they talked about the place of work in
their own lives, as if work was a necessary evil, like
medicine.
British Attitude to work
Anecdotally, this seems to be a widely prevalent attitude to
work, that might be characterised in the statement ‘I know
work is good for me, but if I won the lottery, I’d give it up
like a shot and take up something I wanted to do’.
Within that statement lie a couple of truisms: first, there
does seem to be a ‘British attitude’ to work, that is
different from (and a lot less keen than) say, an American
view. The working population in the UK appear to
demonstrate a curious paradox; they work longer hours
than any other nationality in the developed world, and
yet they are the least enthusiastic about what they do.
The second truism is that people would rather be doing
something that they enjoy, and when people feel obliged
to do anything, they tend to resent it.
The key to the paradox lies in the notion of control; if
any of us want to do something, we tend to enjoy it more
than if we have to do it. Studies show that productivity,
sickness rates, staff turnover, even life expectancy all
improve when people feel that are in some way in control
of their destiny, and worsen when they feel ‘done to’
rather than ‘doing’, and the lower down the employment
chain we work, the less sense of control we have58.
Winning the lottery is a trite way of claiming control,
and with it (in fantasy at least) comes the notion of doing
something we enjoy, something that we control, rather
than something someone else is obliging us to do.
Quite why this should be more prevalent in the British
population than elsewhere is a matter of speculation, but
there does seem to be a non-conformist streak among us
that means that whilst we rarely revolt (look at our French
neighbours for comparison), we commonly subvert. We
have a natural suspicion of authority that has generally
served us well, even if it does mean that while we hate
getting up on Monday mornings, we still do.
In practice, the implications of this observation are that
the more perception of control employees have, the
more effectively they will work. Workers on a
manufacturing line become more productive if they are
allowed to stop the line when anything is wrong; it gives
20
them a sense of control. Loosening the rules about when
breaks may be taken does the same, for the same reason.
Professional workers generally devise their own work
schedules and activities, and the clear control that this
gives them means that they enjoy their work more.
Similarly, self employed people generally enjoy their jobs
more than employees.
wellbeing is being adversely affected by their position) to
be directly linked into the NHS. The best that the system
can do is try to get them a job, or suggest that they refer
themselves into the medical hierarchy.
One essential that overcomes this arbitrary distinction is
the direct link between the NHS and the Department of
Work and Pensions (DWP) whose remit covers the
management and welfare of the unemployed. Such
‘horizontal integration’ helps to remove bureaucratic
barriers, and should make the holistic care of the
workless easier to improve. As with many of the
administrative processes that seem to get in the way of
effective public services (another classic is the artificial
barrier between the NHS and Social Services), the
realities of running a large and complex welfare state
make the simple conjunction of all these services a much
harder task than first appears, but it is a point worth
reiterating repeatedly that the welfare state was
established to ‘do the right thing’, and should not let
‘doing things right’ subsume that aim. However,
‘outsourcing’ such joint ventures to external agencies
(particularly when they are still being developed) risks
broadcasting an entirely different, and less positive
message.
Nested within this idea of control is also the notion of
‘ownership’; if a task matters to me personally, then I
will tend to do it better than if I don’t care about it at all.
This idea will percolate through many of the findings of
this study, in terms both of the ‘input’ (how events
influence people) and ‘output’ (how people may
influence events). This will show not only in the factors
that influence peoples’ perceptions of work, but also in
the most effective ways of changing these perceptions
and improving their relationship with work.
The conclusion to be drawn from this is that building in
the perception of control (and it is the perception that
matters, not the fact) helps increase productivity, reduce
staff dissatisfaction, and improve morale. It also helps to
engender a better sense of ‘ownership’ of a task,
something that will be seen to be an important aspect of
the links between work and health.
These generic observations may colour some of the
specific comments that were made during the interviews
and seminars; these have been synthesised into a
summary that attempts to sort a series of disparate
impressions into some form of order, based on the
‘journey’ from work through illness to unemployment,
and then back again.
A key finding that appeared time and again through the
work of this study was the fact that the distinction
between illness and unemployment seems to be entirely
artificial. Thus, although it is self evident that ill health
is likely to result in some inability to work effectively, the
notion of having the ability to work effectively as a
suitable target to which NHS services could aspire is
entirely missing from the lexicon of the NHS, indeed,
our research found that it is often completely absent from
the mindset of clinicians. Britain in not focused on
rehabilitation, only 1 in 6 people return to work after a
major injury compared to 50% in Scandanavia, a point
conceded in Black’s review59. Thus, when doctors review
their patients, their focus in on the amelioration of
symptoms, and of the titration of medication, but their
review is rarely carried out with the specific aim of
getting patients back to work. This is particularly so in
hospital settings; in general practice, effective practice is
carried out in the context of the so called triple
diagnosis, which includes the social and psychological
aspects of any illness as well as its physical
manifestations, and consultations may well include an
assessment of patients’ ability to return to work. But even
here, such an outcome seems to be a by-product of
getting patients better, not an end in itself.
Illness and unemployment are not separate issues
Similarly, if the problem is approached from the
unemployment end, there seem to be very few
mechanisms available that allow workless people (whose
21
Health,disease and unemployment:
The Bermuda Triangle of society
the most appropriate medication. Whilst ‘early
intervention’ was regularly cited, there was little
questioning of whether the individual was receiving the
best medical treatment for their particular condition.
This is a very relevant supposition and omission,
especially when the National Institute for Clinical
Excellence (NICE) has significantly raised the awareness
of medical choices.In many spheres involving the formal
‘professions’, our society has been moving away from an
‘age of deference’, but questioning the correctness of
prescribed medication seems only to occur when there is
an adverse side-effect. However, the fact that
medications are becoming increasingly specialised points
to the need for greater awareness that the correct
medication shouldn’t be taken for granted. Appropriate
prescribing can result in a more immediate return to
work and so is a key factor in enabling work to be seen
as a health outcome.
06
Themes
Other themes
Prevention is better than cure,
even with long term ill health
The welfare state as it is currently configured seems to
take no account of the fact that chronic illness rarely
comes completely out of the blue; whether one is
considering rheumatoid arthritis, schizophrenia,
blindness, multiple sclerosis, cancer or chronic
obstructive pulmonary disease, these all develop over
time, and their impact on sufferers’ lives may generally
be predicted, even if the pace of their progress may be
harder to define. Despite this, it is not part of our culture
to consider the implications of illness at work except in
the most binary of forms: a person can either work, or
they can’t. People suffering from a long term condition
(LTC) seem be obliged to struggle on at work until they
have to give up and retire, with all the feelings of failure
and loss of purpose that are associated with that sense of
‘giving up’. If they are very lucky, they may then be reemployed on a part time basis, but this is the exception
rather than the rule.
Generally, when we are ill we tend to deny it for a while,
then consider the immediate crisis of treatment and
diagnosis, and only much later consider the long term
consequences of our condition. Partly, this is part of our
hope and expectation for health and longevity, but there
is also a genuine uncertainty about the path of most
LTCs, so that we do not (and indeed, should not)
consider ourselves as being crippled by arthritis at the
first twinge of any joint pain.
It takes time before an acute illness becomes seen as
chronic, and so the challenge is to know when that
change occurs (at an emotional level as well as a clinical
one), and then intervene as soon as possible after that.
On the part of the employer and of wider society, there
would need to be an acceptance that it was normal for
the work environment and job roles to change as people’s
careers progressed, even if that entailed physical change
(seating, instrumentation, etc), and changes to the terms
as well as the conditions of employment. Not only
would this be helpful in keeping those with LTC at work,
but it would fit in with the emerging zeitgeist about
deferring retirement; the same attitudinal changes could
apply as age and energy (as well as motivation) affected
people’s work abilities, thus helping to maintain people’s
presence at work and optimising their effectiveness.
There seem to be no general mechanisms whereby those
who know that they have a LTC can work with their
employer to plan for the future, and modify their
working conditions appropriately; after all, someone with
a LTC may well need to live with it for decades, and it is
clearly a waste for (as well as a drain on) society to lose
the benefit of that person’s contribution to the work
place for all that time, to say nothing of the impact on
their own sense of self worth and life satisfaction.
Several interviewees who worked with organisations that
championed the needs of patients with particular
diseases made this point, and suggested that early
intervention was a key example of prevention being
better than cure: if people who knew that they had a
LTC could negotiate the appropriate changes to their
working conditions, then they would be able to lead a
much more positive, contributory life to the benefit of
society as a whole as well as to themselves and their
families. To do so would take some cultural changes: the
most important of these would be the need for those
with potential LTCs themselves to consider this far
earlier than happens at present. On reflection it was
noticeable that the implicit assumption was made by
most interviewees that individuals are automatically on
22
The third strand of poor perception was based on the
apparent strong biomedical bias of OH services, that
was seen to favour the physical aspects of disease and
disability, rather than including the social and
psychological aspects too. This probably originates from
the medical roots of the specialty, and of the general
human propensity to prefer those markers that lend
themselves to easy measurement over those which
(although conceivably important) are based on intuition
and empathy. Thus, OH services were seen as being
dominated by doctors whose interests lay in muscular
ability and biochemical abnormality more than in the
issues of affect and emotional disturbance.
Occupational Health: whose services
are they anyway?
Both the interviews and the seminars exposed significant
issues about the current nature and purpose of
occupational health (OH), as well as offering some
interesting and practical suggestions as to how these
services might be improved.
There was a general consensus that occupational health
services are currently unwieldy, archaic, and of limited
utility. The starting point for these perceptions is that the
place of occupational health within the health sector
‘scheme of things’ is obscure and poorly understood.
The NHS itself has an OH service, which applies to staff
within the NHS, and is also offered to external
companies on a commercial basis. Beyond that, some
employers do provide an OH service (either in house, as
large employers sometimes do, or on a contracted basis
from the NHS (as described above) or from commercial
OH companies, whilst others (usually SMEs that find the
price of such a service too high to be cost effective)
provide none at all.
In summary (and with a degree of generalisation!), OH
services were seen as patchy in their availability, partisan
in their application, and narrow in the scope of ‘disease’ with which they could deal. However, there were
several suggestions as to how these perceptions could be
improved in order to allow more appropriate, useful
models of OH to bloom: these are based on the notions
of making OH services more widely available, less
focused on the needs of the employer, and more widely
based than on doctors alone. For example, the entire
professional group of occupational therapists was
notable in this study by its absence (although we had
some stalwart attendees at the seminars), and there
would seem to be a niche waiting to be carved out by
them. A new cadre of occupational practitioners was
mentioned in several of the interviews; another group
not bound by the strictures of a very traditional medical
training. In terms of their utility, it may be helpful to
combine the input end of their function (‘what is going
on?’) with the output end (‘what should we do about it?’),
and such an approach might also help to establish and
maintain the neutrality of such a service. The ‘OH
helpline’ for SMEs, recommended by Carol Black’s
report and introduced as a result by the Department of
Health, are one step on this route, but most interviewees
thought that this represented a first step towards a more
enlightened OH service, rather than an end in itself.
The second issue informing this perception is that there
is confusion over the role of the OH service; is the
service there to help the ill person, or to assist the
employer? In other words, who is the client? This
question was almost always posed in an adversarial way
with the needs of the patient being perceived as
diametrically opposite to those of the employer, and only
rarely did anyone see them as aligned.
Once again, this seems to link to the issue of ‘ownership’;
in one of the workshops, for example, it was suggested
that in a small company owned by its workers, it would be
in everybody’s interests to minimise sickness, and that the
occupational health needs of the company would be the
same as those of the employees. It was only when the
interests of the employees became separated from those
of the company that the dichotomy arose, and so one way
to obviate the issue is to remove that distinction, by
increasing the sense of ‘ownership’ amongst employees.
For most interviewees, OH services were largely seen as
representing the employer, policing the sickness of the
workforce to ensure that people returned to work as
quickly as possible, or were helped to leave if return was
seen to be uncertain or unduly delayed. Again, this view
may partially be explained by the sometimes ambivalent
British attitude to work. There was also a sense that ‘he
who pays the piper calls the tune’, and that the needs of
the employer were bound to take precedence over the
needs of the employee.
23
Health,disease and unemployment:
The Bermuda Triangle of society
By nurturing these in a relatively risk free way, the
agencies are fulfilling a task far larger than merely
‘signposting’ the journey back to employment, or acting
as brokers for available employment, which is how the
larger, more impersonal agencies such as Job Centre Plus
are perceived. They are helping to rebuild the skills and
attitudes that are needed for survival and success in the
work place.
06
Themes
Clearly, there is an economy of scale in providing
services that help people back to work (particularly those
that are directly funded by the public purse, where thrift
and probity are paramount), but the clear message from
this work is that any benefit of size is more than offset by
the dis benefits in terms of intimidation and lack of
involvement that go with large scale. It may be that the
compromise is to allow the commissioning of such
services by public agencies through smaller, more nimble
private and voluntary organisations that may be held to
account on the basis of their results; such an approach
would allow probity and efficiency to be served, whilst
maintaining the human scale required for effectiveness,
and injecting a measure of competition and
contestability for good measure too. However, any such
an approach would need to be ‘lubricated’ by simplifying
the complex and bureaucratic tendering processes that
currently discourage many suitable organisations from
offering their services in the first place.
In the struggle to move from worklessness (whether due
to ill health or some other reason) back to full
employment, an important observation that came out of
all the work of this study was the inverse relationship
between the size of a ‘helping’ organisation and its
perceived utility. Time and again, interviewees and
seminar attendees reinforced the daunting nature of
dealing with State bureaucracies, and the relative relief
felt when working with smaller, more focused
organisations that were less formal and more human in
their scale. Beyond the obvious link between the
bureaucracy associated with size, it is hard to say why
this was; perhaps the symbolism of size and State act as
a subtle reflection of the link between self esteem and
authority.
Where welfare is concerned, small is beautiful
Whatever the reason, it became increasingly clear
through all the discussions (both with the helping
organisations themselves and with the various lobby and
expert groups involved) that people seeking assistance to
get back to work found it more helpful to deal with small
organisations than with large bureaucracies. ‘Job Centre
Plus’ in particular was seen as by many as being
particularly impersonal and unhelpful, whereas smaller,
more directly involved groups such as Tomorrow’s
People were seen as offering better advice and seemed
to be more in tune with their users’ needs.
This was especially marked when (as was the case with
Tomorrow’s People) these agencies made use of clients to
help in their running (often on a voluntary, unpaid basis).
Such involvement seemed to help to build up clients’
confidence, perhaps because there was less ‘performance
anxiety’ when there were no wages or formal obligations
involved, and hence get them re-familiarised with the
routines and rituals of the workplace: timekeeping,
socialisation, formal tasks, and so on. At a more
conceptual level, the involvement with a small
organisation that was run by people who had themselves
been in a similar position of unemployment, promoted
a sense of ‘belonging’ and help to engender the sense of
ownership (this time of the organisation) that is needed
if the responsibility, motivation, and pride that are vital
for sustainable and satisfying employment are to be
developed.
24
Taken one step further, is there a role for GPs to take up
such a function more formally, and work as a ‘neutral
agent’ in the area of occupational health?
General practice: tinker, tailor, provider, landlord,
case manager, or none of the above?
In the area of general health care, much is written about
the place of primary care in the delivery of services, and
many of the policies of the past twenty years have been
predicated on the transfer of activity and responsibility
to primary care in general, and general practice in
particular. During our work on the ‘Bermuda Triangle
of society’, the place of general practice was raised in a
number of ways, and these are discussed below:
General practice as venue for case management: finally,
bringing together the idea of care ‘closer to home’, case
management, and the notion of ‘small is beautiful,
interviewees had some interesting views regarding the
use of general practice (or other community based
facilities) as the local base for the provision of services
and advice.
General Practitioner as case manager: the GP has a
Interestingly, there was little consensus as to the place of
general practice in solving the conundrum of the
Bermuda Triangle. Where the issue of case management
was concerned, whilst most people acknowledged the
place of GP as the conceptual case manager in a medical
context, there was not much support for the idea of
letting him/her act as case manager in the field of
unemployment and the return to work. Some put this
down to a perceived lack of skills and interest amongst
GPs, whilst others felt that this approach would be
medicalising a social issue in an inappropriate way.
Others again liked the notion, but felt that GPs were
already overwhelmed with their current tasks without
taking on a new burden.
central place within the NHS as the co-ordinator of care.
They are the person who ‘holds the ring’ of what is
provided to their patients, and keeping a record so that
the overall provision of care is appropriate, co-ordinated,
and contextualised by the GP’s knowledge of their
patients in terms of their physical, social, and
psychological needs (the so-called ‘triple diagnosis’
already discussed above). How well could this concept
be applied to the area of health and unemployment,
where the complexity of issues is at least as diverse as in
‘ordinary’ illness, and where the case for continuity and
someone to act as mentor and guide is at least as strong?
GP as social security fundholder: in the medical field,
there has been a growing awareness that GPs effectively
control hospital activity by dint of their referrals, and
this has been used as the basis of a number of initiatives
that linked their clinical control to a financial interest.
By giving these ‘fundholding’ GPs a vested interest in the
outcome of their actions (inducing the same sense of
ownership that has already been mentioned in a number
of different contexts), the theory was that these GPs
would feel more involved and act more responsibly in
carrying out their referrals. Where returning patients to
the world of work is concerned, there is an hypothesis
that giving GPs a similar vested interest in the outcome
(of a healthy and sustainable return to work) by giving
them control of the resources to manage that return
might reap the same benefits.
A similar logic informed interviewees’ responses to the
idea of GP as fundholder in the field of worklessness; in
addition to the perceived lack of interest/expertise/time,
there was a feeling that there might be political
difficulties in allocating public funds to GPs to disburse
as they saw fit without enough accountability. Where
GPs as OH physicians was concerned, views were more
mixed; there was a theoretical agreement with the move
away from ‘sick notes’ towards the idea of defining how
well a person was, but there were mixed views about the
specific notion: one positive view expressed was based
on the idea of the GP merely defining that the patient
was fit for ‘some’ work, and letting the employer then
decide how best to utilise the patient’s working abilities.
However, interviewees were concerned that if GPs were
expected to define the extent of their patient’s fitness,
they would have to develop a sense of all the skills
required by local employers, a full understanding of
occupational health, and be prepared to accept a degree
of accountability (including, presumably, legal liability)
for their decisions. Once again, there were doubts
expressed about GPs’ inclinations/expertise/time to
carry out this role. One interesting view expressed was
the idea of incorporating some work related targets into
GPs’ Quality and Outcomes Framework (QOF), whose
achievement is linked to their practice income.
So interviewees were asked their views about GPs being
given (at least some of) the social security budget to allow
them to spend it more flexibly (say in treatments such as
physiotherapy, occupational therapy, or even other less
conventional approaches) in the attempt to get patients
back to work more quickly.
GP as occupational health physician: part of the
report produced by Carol Black introduced the notion of
the ‘wellness note’, by which GPs signal their patients’
ability to return to some measure of work activity. This
idea is currently being developed and rolled out, so
interviewees were asked their views on the idea of GP
as OH diagnostician, deciding who is able to work, and
to what level.
25
Health,disease and unemployment:
The Bermuda Triangle of society
hours and a variety of permutations of chairs, desks, and
equipment, its ability to do even this would depend on its
size; a company of 300 employees should be able to offer
more flexibility in any of these factors than a company
of ten employees. Conversely, it would be hard for a
construction company to take on (or retain) labouring
staff with conditions such as rheumatoid arthritis, unless
those staff were able and willing to be completely
retrained in desk jobs that might be totally alien to them.
06
Themes
The area in which there was most consensus concerning
the role of general practice was in the use of GP facilities
as a venue for the work and advice required to help the
workless get back to work. The local nature of such
facilities means that such services may be provided in
ways suitable for each local community; they are also
small and informal enough to avoid the sense of
bureaucracy and disempowerment linked to the
enormous edifices of the State. Such centres could be
populated by staff from private and/or voluntary
organisations, or by more traditional providers of advice,
but the idea of linking the tasks associated with the
return to work to the specific health issues at a single
venue was appealing to most who expressed a view.
Part of the problem is perceptual and commercial; there
is good evidence that supportive companies that treat
their staff well and are prepared to be flexible have
reduced staff turnover (and hence lower training time
and costs), increased productivity, and better longevity.
However, commercial pressures are often perceived as
being overwhelming, and many companies take a very
short term view of staff welfare. This is particularly so at
the unskilled end of the market, where training, and
professional judgment may matter less than sheer
muscle, and where recruitment is relatively easy and
retention therefore less important.
To make matter worse, in trying to persuade companies
to (say) initiate an occupational health function, it is
difficult to demonstrate that they would reap benefits
because those benefits are measured in absences, and
negatives are always much harder to prove: predicting
the absence of sickness or a reduction in turnover
require a leap of faith, and such faith is often the missing
ingredient in introducing some of these changes.
If we continue categorising the findings of the study in
a notional chronology, then the next stop after the
support and rehabilitation offered during worklessness
should be the re-entry to work, and here we come up
against the fact that the variety of workplaces is almost
infinite, making specific responses to bringing people
back to work impossible to prescribe.
The flexible workplace: oxymoron or aspiration
Finally, to close the circle that runs from the occurrence
of illness through worklessness and back to the
workplace, it is worth noting interviewees’ thoughts on
the incentives (both positive and perverse) that exist to
aid and abet in the this process. In this, there is a strong
politicial element, as peoples’ views on welfare payments
vary considerably. Most participants agreed however
that those who were workless through no fault of their
own needed support; the challenge was how to wean
them off it without creating unnecessary hardship.
Incentivising the return to work
However, there are probably a number of generic
principles that one could apply to the manner in which
employers respond when their staff are unable to work
due to ill health, or to the way in which they might
respond to applications to work from those who are
chronically workless. These might include:
•
•
•
•
Be prepared to be flexible in the working
conditions (physical and temporal) that you offer
Intrinsic to this puzzle is the eternal welfare conundrum:
make benefits too good, and nobody wants to give them
up; make them too poor, and people suffer. This paper is
not the place for a detailed answer, but out of the
interviews emerged the notion of some kind of tapering
scale, that married a welfare payment that reduced as
‘real’ income grew without any ‘step changes’ being
triggered that would invoke the classic ‘benefits trap’.
Take a long term view of staff morale and
wellbeing: loyalty breeds profits
Offer appropriate occupational health support
Tailor the tasks to the abilities of your staff,
and be prepared to modify these
In reality, of course, the ability of companies to live up
to these promises depends on many factors, some
absolute, some relative, and many a matter of opinion
and attitude. Thus, whilst an office based agency doing
computer based work might be able to offer flexible
Such a taper is clearly meant to be applied at the end of
the story when ‘they lived happily ever after’. At the
‘once upon a time’ end, views from the respondents were
fairly consistent that the current interventions happened
26
far too late: companies rarely identified potential health
or performance issues in time to deal with them while
employees were still working; state run interventions to
get people back to work or to stabilize their payments
happened only after they had been workless for several
months.
What was required was genuine early intervention,
preferably in time to preempt the whole workless phase,
particularly when it was a predictable health issue that
was causing the problem. Thus, rather than waiting until
the rheumatoid arthritis had become so bad that one’s
usual work had become completely impossible, it would
be better to have discussed with one’s employer the
possible alternatives, and set them up so that work of
some kind could be set up in a sustainable way that
maintained continuity of income for the employee,
continuity of output for the employer, and one less
person on State Welfare. Of course, measures would
have to be taken to ensure that employees would not be
disadvantaged by their employer for their openness. It
may be that medical support for such interventions could
be an extension of the ‘fit note’ idea, using the GP’s
imprimatur to validate such discussions, and preempt
any punitive reaction by less enlightened employers.
The incentives are fairly clear for both the victim and
the State; however, as the system currently runs, it
requires an enlightened employer to see that the long
term advantages of looking after their employees far
outweigh the short term costs of keeping them at work
at a lower level of productivity whilst their problems are
being resolved.
Moreover, it takes a particularly enlightened company
to be prepared to accept back into the workplace an
employee with limited capacity, who may need physical
adaptations as well as concessions in terms of working
hours, job role and so on.
One possible lever for change suggested by an
interviewee was the HSE (Health and Safety Executive).
Until now, most of the HSE’s recommendations have
been based on physical changes to make the working
environment safer for employees. However, with the
rising awareness of and interest in work related stress, it
may be that increasing the profile of the HSE in this area
could bring sufficient pressure to bear on employers on
their prevention and more effective treatment of the
condition when it occurs at work. Fear of liability and
of compensation, whilst not the most altruistic of
drivers, may be a useful adjunct to the beatitudes of the
moral high ground.
27
Health,disease and unemployment:
The Bermuda Triangle of society
07
Summary of
It is clear that unemployment causes ill health just as ill
health causes unemployment, and that a return to work
can (if used appropriately) improve health. Those who are
unemployed are seen (and see themselves) as having less
value as people than those in work. This phenomenon is
more marked amongst those who have been in work and
then become unemployed. There are currently no real
incentives for employers to adapt work circumstances to
suit the needs of the disabled person, which makes getting
such people back to work highly problematic.
The British and Work
Key Messages
01 It would therefore seem sensible for the first aim of
any policy change to make it in the interests of the
individual, the employer, and society at large to
align the incentives and close the loop between
health, illness, and unemployment.
There is a dissonance in British culture between what
people say about the benefits of work and what they feel
about it; work is often seen as a necessary evil. This view
is more marked the lower the perceptions of control felt
by workers; productivity, sickness rates, staff turnover,
even life expectancy all worsen when employees feel
‘done to’ rather than ‘doing’, and the lower down the
employment chain people work, the less sense of control
they have.
02 Raising the perception of control is key to
improving productivity, and all the work on
leadership, engagement, and so on is actually
trying to do this. An overt focus on improving this
culture would reap rapid and sustainable benefits.
Given that the distinction between illness and
unemployment seems to be artificial, it is self evident
that ill health is likely to result in some inability to
work effectively.
03 Getting patients back to productive and sustainable
work should become a key objective and outcome
indicator for all health services, particularly the
NHS. All forms of clinical education need to
include this aim from their outset, and throughout
both undergraduate and continuing training.
04 An important aspect of this emphasis must be the
inclusion in the diagnostic process of the social and
psychological aspects of an illness as well as its
physical manifestations, and treatment should be
aimed at ameliorating patients’ ability to return to
work as part of returning them to better health.
Conversely,
increasing
the
awareness
that
unemployment per se adversely affects health would help
to overcome the isolation surrounding the workless, and
help to preempt the vicious circle of unemployment and
chronic illness.
28
the employees are different to those of the company, that
the dichotomy arises, and so one way to obviate the issue
is to remove that distinction.
05 One essential in this regard would be the
strengthening of direct links between the NHS
and the Department of Work and Pensions (DWP).
OH services are often seen as policing workforce sickness
to ensure that people return to work as quickly as
possible, or are helped to leave if return is seen to be
unduly delayed. They are seen to have a strong
biomedical bias, that favours the physical aspects of
disease and disability, rather than including the social
and psychological aspects.
Such ‘horizontal integration’ will continue to make the
holistic care of the workless (for whatever reason) easier
to manage, and would signal the Government’s intentions
to continue to tie health and work policies more closely
together. Strengthening these links directly would also
allow those working in either sector to begin to make the
interpersonal contacts that are key to the development of
effective and sustainable relationships. ‘Outsourcing’ such
joint ventures to external agencies (particularly when they
are still being developed) risks broadcasting an entirely
different, and less positive message.
Overall, OH services are seen as patchy in their
availability, partisan in their application, and narrow in
the scope of ‘dis-ease’ with which they currently deal.
07 These perceptions could be improved by making
OH services more widely available, less focused on
the needs of the employer, and more widely based
than on OH doctors alone . In terms of their
utility, it would be helpful to combine the input end
of their function (‘what is going on?’) with the
output end (‘what should we do about it?’), and
such an approach might also help to establish and
maintain the neutrality (real and perceived)
of such a service.
Prevention is better than cure,
even with long term ill health
Chronic illness rarely comes completely out of the blue
yet our society seems only to consider the implications
of illness at work in binary terms: a person can either
work, or they can’t. If people who knew that they had a
long term condition (LTC) could negotiate much earlier
the appropriate changes to their working conditions,
then they would be able to lead a much more positive,
contributory life to the benefit of society as a whole as
well as to themselves and their families. Early
intervention is the LTC version of prevention being
better than cure.
06 To do this, there needs to be an acceptance on the
part of the employer and of wider society that it is
normal for the work environment and job roles to
change as people’s careers progressed, even if that
entails physical change (seating, instrumentation,
etc), and changes to the terms as well as the
conditions of employment.
Such a change would also chime with our changing
attitudes to retirement; the same attitudinal changes
could apply as age and energy (as well as motivation)
affected people’s work abilities, thus helping to maintain
people’s presence at work and optimising their
effectiveness.
Occupational Health (OH) services are currently seen as
unwieldy, archaic, and of limited utility. Their position
within the health sector is poorly understood, and
employers vary in their OH provision. There is
confusion about whether OH services are there to help
the ill person, or to assist the employer. The needs of the
patient are often perceived as opposing those of the
employer; rarely are they seen as aligned, and then only
when employees have a strong sense of ‘ownership’ of
their jobs and their companies. It is when the interests of
Occupational health: it is broke, so let’s fix it
29
Health,disease and unemployment:
The Bermuda Triangle of society
a new burden. Similar logic underpinned responses to
the idea of GP as ‘fundholder’ in the field of
worklessness; in addition to the perceived lack of interest
and/or expertise and/or time, it was felt that there might
be political difficulties in allocating public funds to GPs
to disburse as they saw fit without much visible
accountability. In principle, there was agreement with
the move away from ‘sick notes’ towards the idea of
defining how well a person was, but there were mixed
views about the specific notion, and its practical
difficulties in terms of skills, and accountability
(including legal liability).
07
Summary of
Key Messages
There is an inverse relationship between the size of a
‘helping’ organisation and its perceived utility. Dealing
with State bureaucracies is seen as daunting compared
with working alongside smaller, more focused
organisations that are less formal and more human in
their scale. This is especially marked when such agencies
make use of clients to help in their running. Involvement
of this kind seems to help to build up clients’ confidence,
and get them re-familiarised with the workplace, as well
as promoting the sense of ‘belonging’ vital if sustainable
and satisfying employment are to be developed.
Where welfare is concerned, small is beautiful
09 There was more consensus concerning the use
of GP facilities as a venue for the work and advice
required to help the workless get back to work.
Their local nature and size and relative informality
are helpful, and they could be populated by staff
from private and/or voluntary organisations. The
idea of linking the tasks associated with the return
to work to specific health care issues at a single
venue was also appealing.
Such agencies are fulfilling a task far more significant
than merely ‘signposting’ the journey back to
employment, or acting as brokers for available
employment, which is how the larger, more impersonal
agencies such as Job Centre Plus are perceived.
In an ideal work/health world, employers should:
The flexible workplace: oxymoron or aspiration
•
•
08 Clearly, whilst there is an economy of scale in
providing services that help people back to work,
the clear message from this work is that any
benefits of size are more than offset by the
disbenefits in terms of intimidation and lack of
involvement that go with large scale. Allowing the
commissioning of such services by public agencies
through smaller, more nimble (yet accountable)
private and voluntary organisations may overcome
this apparent conundrum.
•
•
Be prepared to show flexibility in the working
conditions (physical and temporal) offered
Take a long term view of staff morale and
wellbeing: loyalty breeds profits
Offer appropriate occupational health support
Tailor work tasks to the abilities of their staff,
and be prepared to modify these
Whilst there may be practical difficulties in
implementing all these aspirations in all companies, it is
clear that companies that treat their staff well and are
prepared to be flexible have reduced staff turnover, sick
leave, and absenteeism.
Such an approach would need to be ‘lubricated’ by
simplifying the complex and bureaucratic tendering
processes that currently discourage many suitable
organisations from offering their services in the
first place.
10 However, predicting the absence of sickness or a
There was little consensus as to the place of general
practice in solving the mystery of the Bermuda Triangle.
There was not much support for the idea of letting GPs
act as case managers in the field of unemployment and
the return to work, partly because of their perceived lack
of skills and interest, and partly because their approach
might be medicalising a social issue.
When the macro economy is struggling, persuading
Governments to make this same leap of faith may be as
difficult as doing it with reluctant companies.
reduction in turnover require a leap of faith, and
such faith is often the missing ingredient in
introducing some of these changes. This may
be one area where legislation concerning
the employee benefits mentioned above
may be appropriate.
The role of general practice
Others liked the notion, but felt that GPs were already
overwhelmed with their current tasks without taking on
30
14 One possible lever for change raised by this study is
the Health and Safety Executive (HSE). Currently,
most HSE recommendations are based on physical
changes needed to make the working environment
safer for employees. However, with the rising
awareness of and interest in work related stress, it
may be that increasing the profile of the HSE in
this area could bring sufficient pressure to bear on
employers on their prevention and more effective
treatment of stress. Fear of liability and of
compensation may be a useful adjunct to the
moral high ground.
The eternal welfare conundrum (make benefits too good,
and nobody wants to give them up; make them too poor,
and people suffer), has always suffered from its position
trapped between opposing political philosophies. In the
current political climate, we may have a rare opportunity
to allow it to escape and be solved.
Incentivising the return to work
11 It should be possible to introduce some kind of
tapering scale as health and workfullness improve,
by which welfare payments reduce as ‘real’ income
grows without any ‘step changes’ being triggered in
a way that avoids the classic ‘benefits trap’.
At the ‘front’ end of worklessness and ill health, helpful
interventions currently happen far too late: companies
rarely identify potential health or performance issues in
time to deal with them while employees are still working;
state run interventions to get people back to work or to
stabilize their payments happen only after they have
been workless for several months.
12 What is required is genuine early intervention,
preferably in time to preempt the whole workless
phase, particularly when predictable health issues
are causing the problem. There needs to be
increased awareness of how important appropriate
prescribing is to helping people return to work as
quickly as possible.
It would be better at the outset of such a condition to
discuss with one’s employer the possible alternatives, and
arrange them so that work of some kind could be set up
in a sustainable way that maintains continuity of income
for the employee, continuity of output for the employer,
and one less person on welfare for the State. Of course,
measures would have to be taken to ensure that
employees would not be disadvantaged by their
employer for their openness.
13 It may be that medical support for such
interventions could be an extension of the ‘fit note’
idea, using the GP’s imprimatur to validate such
discussions, and preempt any punitive reaction by
less enlightened employers.
However, in the current system it requires an enlightened
employer to see that the long term advantages of looking
after employees far outweigh the short term costs of
keeping them at work at a lower level of productivity
whilst their problems are being resolved, or accepting into
the workplace an employee with limited capacity who
may need physical adaptations as well as concessions in
terms of working hours, job role and so on.
31
Health,disease and unemployment:
The Bermuda Triangle of society
This project started by looking at the links between ill
health and employment, under the working title of ‘work
as a health outcome’. It soon became apparent that the
issue was more complex than a simple linear relationship
between these two, and the concept of the interaction
between health, illness and unemployment arose, with a
powerful image emerging of the Bermuda Triangle of
isolated people invisible to the outside world, and almost
impossible to rescue. The paper used a variety of methods
to deconstruct some of the issues, and then reconstruct
them through a series of interviews and seminars.
08
Conclusion
The issue is too multifaceted to be able to produce a
simple set of recommendations. Dame Carol Black’s
Report has suggested a number of specific changes,
some of which have been implemented. However, the
overall impression taken away from the interviews was
that uptake of the Report’s findings had been limited by
lack of political interest.
Thus for instance, one of the Black suggestions was the
extension of OH services to cover organisations that
would not currently be in a position to use them. The
mechanism mooted was the introduction of telephone
based OH assistance, which should be available to all
employers. Whilst the idea is intriguing, and would
clearly be useful, the problems with such a scheme lie in
its extent. A telephone based service can never be
substitute for proper physical examination, and the level
of coverage required to make this anything other than a
symbolic gesture is probably not feasible in the short
term, especially in straitened financial circumstances,
without the political clout to make it really fly.
32
Even with such a careful developmental approach, issues
might still be raised about funding and organisational
format; could employers be persuaded to pay for a
service that was not beholden to them? Would it be
reasonable to expect such a service to part of the NHS
itself ? Is there a viable argument to suggest that users of
such a service should contribute to its running costs?
On the other hand, an approach that makes use of
existing facilities is relatively cheap, and incremental,
evolutionary development is usually more easily
assimilated into the national (as well the professional)
psyche than expensive, disruptive (and professionally
threatening) large scale change.
With this in mind, it may be that we should looking at
basing relatively low level OH services in community
settings (such as NHS facilities including community
clinics and GP surgeries), to be run by a combination of
staff who are able between them to cover both the
assessment (‘diagnostic’) and delivery (‘treatment’) ends
of the service. The use of that metaphor is ironic, and
perversely highlights that it would be preferable for such
a model to encompass the medical model without being
confined to it, so that the other psychosocial factors that
influence the interaction of work, health and illness in a
far less linear way than simple ‘diagnosis’ and ‘treatment’
may be incorporated into the system.
Funding also raises the issue of the place of the State in
dealing with the Bermuda Triangle. Much of the work
of both this study and its predecessors is predicated on
the basis that lifting the fog of confusion that surrounds
its murky centre would liberate the capacity and
capability of those who were trapped there, thereby
improving their situations as well as increasing the stock
of society at large. The spending required to achieve this
should be seen as an investment, not a cost, for in
unraveling this knotty problem, not only will the
individuals involved benefit, but the first steps will have
been taken to change for the better Society’s paradigm
of values where work, health, and illness come together.
Such services would need to be seen as neutral agencies,
looking after the needs of their attendees rather than
those of the employing organisation, and this suggests a
place for the private and voluntary sectors, with their
small scale and local ownership.
33
Health,disease and unemployment:
The Bermuda Triangle of society
09
Footnotes
1
2
3
4
5
6
7
8
9
Health, Wellbeing and Work Directorate 2005
32 McGee, Bevan and Quandrello pp 52
Boorman Review 2009 Exec Summary pp 2
34 RCGP. National Education Programme for General
33 Mowlam A, Lewis J. 2005 pp 2
Department of Health. 7th Dec 2009
practitioners. See http://www.rcgp.org.uk/news_and_events/
courses__events/health_and_work_training.aspx
Marmot review 2010 pp 9-20
http://www.ucl.ac.uk/gheg/marmotreview/FairSocietyHealthyLives
ExecSummary
35 Black C. pp17
36 Marmot Review 2009 pp 3
Rose D. 11th February 2010
37 Constable S et al. 2009 pp 6
Lichfield P. 2007 pp 3.
38 HSE. Health and Safety Statistics 2008/9 National Statistics
DWP administrative data 2007
39 Vaughn-Jones H, Barham L. pp 38
HSE. National Statistics, Health and Safety 2008/9
40 May 2009. pp 4
Department of Work and Pensions, Vocational Rehabilitation
2004 pp 16
41 Palmer KT, Cox RAF, Brown I. 2007 pp 77
10 Aylward M. 2003, pp 287-299
42 Odonnell M, Reymon J. October 2009
11 ARMA 2007 pp 3
43 DWP 2009 http://research.dwp.gov.uk/asd/stats_summary.asp
12 See www.fitforworkeurope.eu
44 Wallop H. The Daily Telegraph 1st Feb 2010
13 Department of Health, Musculoskeletal services framework
45 SCMH. Briefing 40: Removing Barriers. July 22nd 2009
2006
46 Brown J, Hanlon P, Turok I, Webster D, Arnott J, Macdonald
14 ARMA 2009. pp 3
EB. Oct 2008:1-7
15 NAO 2009. pp 5
47 Bewley H, Dorsett R and Salis S. DWP Research Report
601 2008
16 ARMA 2009. pp 5
17 Department of Health, New Horizons 2009
48 Adam et al. DWP Research Summary 498 2008
19 http://www.direct.gov.uk/en/DisabledPeople/HealthAndSupport/
50 Black C. pp 17
49 ARMA Joint Working 2006
18 Perkins R, Farmer P and Lichfield P. December 2009 pp 12
MentalHealth/DG_179325
51 DWP Access to Work Statistics January 2010
20 Fitch C, Daw R, Balmer N, Gray K and Skipper M. 2008
52 Marsden D, Marcioni S. pp 1
21 Sainsbury et al. Research report no. 513 2008
53 Ibid pp 17
22 SHiFT Line Manager’s Resource 2007 pp 6
54 PricewaterhouseCoopers 2008 pp 7
23 Fitch C, Daw R, Balmer N, Gray K and Skipper M. 2008 pp 11
55 Kennedy I. 2009
24 DWP.
56 Kanovos P, Manning J, Taylor D, Schurer W, Checchi K. 2010
25 RCPsych position statement 2009 pp 7
57 Wadell G, Burton K. 2006 pp 146
26 Perkins R, Farmer P and Lichfield P. December 2009
58 Constable S et al. 2009 pp 6
27 DH New Horizons 2009 pp 36, 42
59 Black C. pp 76
28 SCMH. Briefing 40: Removing Barriers July 2009
60 PricewaterhouseCoopers 2008 pp 7
29 Wilson A. 2007
30 SCMH. Shepard G, Boardman J and Slade M. SCMH 2008 pp 5
31 BMA press release April 20th 2010
34
Health,disease and unemployment:
The Bermuda Triangle of society
10
Appendices
Appendix 1
Work Outcomes Interview Schedule
Interviewees asked about their name and position and
introduced to the project in a preamble that confirmed
that participants understood the objective of the review
and their willingness to contribute.
Questions
9. What (if anything) do you know about Carol
Black’s ‘Working for a healthier tomorrow’,
and the Government’s response ‘Improving
Health andWork:changing lives’?
(try to get their sense of these: recommendations, opinions on
their relevance, usefulness, etc)
1. Personal details and role in your organisation
(Brief outline of professional role and career path to date,
Job title, role, CV, ambitions)
2. How (if at all) does your organisation’s work
impinge on the ‘world of work’?
(specific work in this area, keeping people at work, returning
them there, etc)
10. Given a clean slate,what would you do to make
work a health outcome?
(personally and organisationally)
3. What do you think is the relationship between
health and work?
(personally and organisationally)
11. Have you any other thoughts or observations?
12. Closure
(re-iterate confidentiality, future progress of project, feedback
from process)
4. What are your views on the notion of ‘work as a
health outcome’?
(irrelevant, exciting, obvious; explore in some detail)
13. Emerging themes and messages
(main issues, plus any other observations (e.g. interview
dynamics etc))
5. Are there any areas of ill health where this is more
(in)appropriate?
(musculoskeletal, mental health, social, disability, illness linked
to unemployed etc)
Jonathan Shapiro & Julia Manning
October 2009
6. How could NHS mechanisms be better used to get
people back to work more quickly,and in
a sustainable way?
(role of GP, clinical services (e.g. physio), referral process, 1°/2°
care interface issues, technological solutions etc)
7. How could non-NHS mechanisms be better used
to get people back to work more quickly,and in
a sustainable way?
(local authority, social security, voluntary/private sector: health
insurers, employers, etc)
8. Have you heard of the ‘fit for work’schemes?
(if so, can you describe them? Who should be responsible for
their implementation? On what (if anything) is their
success contingent?)
35
Health,disease and unemployment:
The Bermuda Triangle of society
10
Appendices
Appendix 2
Interviewees
Name
Title
Organisation
Samantha Peters
CE
British Society of Rheumatology
Leonie Dawson
Professional Advisor
Chartered Society
of Physiotherapy
Rachel Hunter
Clinical Director
RehabWorks
Delia Skan
HSENI, civil servant
Faculty of Occupational
Medicine of the Royal College
of Physicians
Ann McCraken
Chair
International Stress
Management Association UK
Prof. Alan
Maryon-Davis
President
Faculty of Public Health
Dr Jed Boardman
Consultant Clinical Psychiatrist
SCMH Royal College
of Psychiatrists
Prof. Jonathan Ayres
Environmental & Respiratory Medicine
Professor and Director of the Institute of
Occupational and Environmental Medicine
University of Birmingham.
Col.Malcolm Braithwaite
Army Professor of Occupational Medicine
and Honorary Senior Lecturer
University of Birmingham.
Mike Sobanja
Chief Officer
NHS Alliance
Karen Charman
Head of Employment Services
NHS Employers
Steve Shrubb
Director of the Mental
Health Network
NHS Confederation
David Colin Thome
National Director of Primary Care
Department of Health
36
Name
Title
Organisation
Ros Meek
Director
Arthritis and
Musculoskeletal Alliance
Brian Kaiser
CE
British Occupational Health
Research Foundation
Helen Bunyan
Membership Manager
National Rheumatoid
Arthritis Society
Steve Swan
Director of Welfare to Work
Tomorrow's People
Prof. Bob Grove
Joint Chief Executive
SCMH
Paul Corry
Director of Public Affairs
Rethink
Richard Frost
Vocational Services Manager
WorkWays
David Hawley
Operation Manager
Working Links
Andy Jones
Medical Director
Nuffield Health
Dudley Lusted
Head of Corporate
Healthcare Development
AXA PPP Healthcare
Dr Mike O’Donnell
Chief Medical Officer
UNUM
Helen Merfield
CEO
HCML
Bronwen Williams
Occupational Therapist
UK QBE
Kelly Du Preez
Physiotherapist
UK QBE
37
Health,disease and unemployment:
The Bermuda Triangle of society
Bewley H, Dorsett R and Salis S. The Impact of
Pathways to Work on work, earnings and self reported
health in the April 2006 Expansion Areas , DWP
Research Report 601. London, Department for Work
and Pensions. 2008.
http://research.dwp.gov.uk/asd/asd5/summ20092010/601summ.pdf
11
Bibliography
Black C. Working for a Healthier tomorrow, Dame
Carol Black's Review of the health of Britain's working
age population Cross-government Health, Work and
wellbeing Programme, TSO. March 2008.
http://www.workingforhealth.gov.uk/documents/working-for-ahealthier-tomorrow-tagged.pdf
ABI. Improving Health at Work: Employers’ attitudes
to occupational health. Oct 2006.
www.abi.org.uk/content/contentfilemanager.aspx?
contentid=24840
Adam S, Bozio A, Emmerson C, Greenberg D, Knight
GA. Cost-benefit analysis of Pathways to Work for new
and repeat incapacity benefits claimants. Department
for work and pensions. 2008.
http://research.dwp.gov.uk/asd/asd5/report_abstracts/rr_abst
racts/rra_498.asp
BMA. New fit note means onus is now on employers to
act, says BM. Press release April 1st 2010.
http://web2.bma.org.uk/pressrel.nsf/wlu/SGOY844FKF?OpenDocument&vw=wfmms
Boorman M. NHS Health and wellbeing Review.
Crown, Department of Health. Nov 2009.
http://www.nhshealthandwellbeing.org/pdfs/NHS%20Staff
%20H&WB%20Review%20Final%20Report%20VFinal
%2020-11-09.pdf
Aylward M, Sawney P . Support and Rehabilitation:
restoring fitness for work, In Fitness for Work Ed.
Palmer, K. Brown, I., & Cox, R Oxford University
Press, Oxford. 2006.
BOHRF. Summer 2008 newsletter. Aug 2008
http://www.bohrf.org.uk/content/news.html#nrpl1rehab
Aylward M. Needless Unemployment: the public
health crisis in What about the Workers? Ed. HollandElliot, K. The Royal Society of Medicine Press,
London. 2004.
British Society of Rehabilitation Medicine. Vocational
rehabilitation - the way forward. 2nd ed report of a
working party Chaired by Frank AO. London, British
Society of Rehabilitation Medicine. 2003.
Aylward M. Origins, practice and limitations of
disability assessment medicine. In Malingering and
illness deception. Edited by: Halligan PW, Bass C,
Oakly DA. Londen: OUP; 2003:287-299.
Brown J, Hanlon P, Turok I, Webster D, Arnott J,
Macdonald EB. Mental health as a reason for claiming
incapacity benefit – a comparison of national and local
trends. Journal of Public Health. Oct 2008:1-7.
ARMA. Joint Working? An audit of the
implementations of the Department of Health’s
musculoskeletal framework ARMA. July 2009.
http://www.arma.uk.net/pdfs/MSF%20Review_FINAL1.pdf
CBI. At work and working well? CBI/AXA absence
and labour turnover. 2008.
http://connect.axa.co.uk/files/insights/documents/Absence%2
0report%202008.pdf
Barnes M, Buck R, Cohen D, Aylward M. Beliefs
about common health problems and work: a
qualitative study. Social Science and Medicine.
2008;67:657-655.
Chang D, Irving A. Evaluation of the GP Education
Pilot: Health and Work in general Practice.
Department for Work and Pensions research report
479. Norwich 2008.
http://research.dwp.gov.uk/asd/asd5/rports20072008/rrep479.pdf
Bevan S, Hayday S. Costing Sickness absence in the
UK. Report 382, Institute for Employment Studies.
October 2001.
Bevan S, Passmore E, Mahdon M. (2009) Fit for
work? Musculoskeletal Disorders and labour market
participation The work foundation, Abbott.
http://www.fitforworkeurope.eu/Websitedocuments/44_fit_for
_work_small.pdf
Chapman C. Delivery healthy and happy staff. HSJ 15
Oct 2009:15.
Constable S, Coats D, Bevan S, Mahdon M. Good
Jobs. The Work Foundation. London 2009.
http://www.theworkfoundation.com/assets/docs/publications/
226_good_jobs2.pdf
38
Department of Health. A joint responsibility: doing it
differently – the musculoskeletal services framework. 2006.
http://www.18weeks.nhs.uk/Content.aspx?path=/achieveand-sustain/Specialty-focussed-areas/Orthopaedics/MSF/
Health, Work and wellbeing Directorate. Reforming
the medical statement, consultation on draft
regulations May 2009
http://www.dwp.gov.uk/docs/reforming-the-medical-statementconsultation-28may2009.pdf
Department of Health. Radical overhaul of support for
people with mental health conditions. 7th Dec 2009.
http://www.dh.gov.uk/en/News/Recentstories/DH_109719
Health, Work and Wellbeing directorate. Working our
way to better mental health: a framework for action.
Crown December 2009.
http://www.workingforhealth.gov.uk/documents/Working-ourway-to-better-mental-health-tagged.pdf
Department of Health. NHS Next Stage Review Final
Report. June 2008.
http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalass
ets/@dh/@en/documents/digitalasset/dh_085828.pdf
HM Government. Work, Recovery and Inclusion.
Emplyment support for people in contact with
secondary mental health services. National Mental
Health Development Unit, London. December 2009.
http://www.nmhdu.org.uk/silo/files/work-recovery-andinclusion.pdf
Department of Health. New Horizons, Towards a
shared vision for mental health. Consultation. Dec 2009.
http://newhorizons.dh.gov.uk/assets/Reports/EXEC%20SU
MMARY%20NewHorizonsCon_ACC.pdf
Department for Work and Pensions. Access to work
official statistics. Januray 2010.
http://research.dwp.gov.uk/asd/workingage/atw/atw0110.pdf
HSE. Health and safety statistics 2007/08, October 2008.
http://www.hse.gov.uk/statistics/overall/hssh0708.pdf
HSE. Health and Safety Statistics 2008/9. National
Statistics, Suffolk. Oct 2009.
http://www.hse.gov.uk/statistics/overall/hssh0809.pdf ?ebul=
slips/nov-09&cr=10
Department for Work and Pensions. Building Capacity
for Work: A Uk Framework for Vocational
Rehabilitation. Oct 2004.
http://www.scmh.org.uk/pdfs/dwp_vocational_rehabilitation.pdf
Kanovos P, Manning J, Taylor D, Schurer W, Checchi
K. Implementing value based pricing for
pharmaceuticals in the UK. Final report
2020health.org .March 2010.
http://www.2020health.org/export/sites/2020/pdf/2020vp
blow27-04.pdf
Department for Work and Pensions. Ready for work.
London. 2007.
http://www.dwp.gov.uk/docs/readyforwork.pdf
Department for Work and Pensions. Statistical releases
January 2010.
http://research.dwp.gov.uk/asd/stats_summary.asp
Kemp PA, Davidson J. Routes onto incapacity benefit:
findings from a survey of recent claimants. DWP
research report 469. 2007.
Duncan Smith I. The Big Issue? Mental health. First
published The Big Issue 2008.
http://www.centreforsocialjustice.org.uk/default.asp?pageRef=332
Kendall NAS, Linton SA, Main CJ. Guide to Assessing
Psycho-social Yellow Flags in Acute Low Back Pain:
Risk Factors for Long-Term Disability and Work Loss.
Accident Compensation Corporation and the New
Zealand Guidelines Group, Wellington, New Zealand.
Oct, 2004 Ed. 1997.
Fitch C, Daw R, Balmer N, Gray K and Skipper M.
Fair Deal for Mental Health. Policy Unity, Royal
College of Psychiatrists. 2008.
http://www.rcpsych.ac.uk/pdf/Fair%20Deal%20manifesto_f
or%20website%201%20Julyy.pdf
Kennedy I. Appraising the value of innovation and
other benefits. A short study for NICE. 22nd July 2009.
http://www.nice.org.uk/media/98F/5C/KennedyStudyFinal
Report.pdf
Frank A, Sawney P. Vocational Rehabilitation. J Royal
Soc Med. 2003:96:522-523.
HSE. Management competencies for preventing and
reducing stress at work. Prepared by Goldsmiths,
University of London for the HSE. Research Report
553. 2007. http://www.hse.gov.uk/research/rrpdf/rr553.pdf
Kings Fund. Perceptions of patients and professionals
on rheumatoid arthritis care. A Consultancy Report by
The King’s Fund for the Rheumatology Futures
Group. Jan 2009.
http://www.rheumatoid.org.uk/download.php?asset_id=615&
link=true
39
Health,disease and unemployment:
The Bermuda Triangle of society
Nice K, Thornton P. Job Retention and rehabilitation
pilot: Employer’s management of long term sickness
absence. National Centre for Social Policy Research
Unit, University of York on behalf of the NRAS.
Iwant to work....Employment and Rheumatoid
Arthritis. A National Picture. National Rheumatoid
Arthritis Survey 2007.
http://www.rheumatoid.org.uk/download.php?asset_id=636&
link=true
11
Bibliography
Lelliott P, Tulloch S, Boardman J, Harvey S,
Henderson M, Knapp M. Mental Health and Work.
Royal College of Physchiatrists Report commisioned
by the Health Work and Wellbeing directorate.
http://www.workingforhealth.gov.uk/documents/mental-healthand-work.pdf
Department of Work and Pensions. Research report
227. Norwich 2004.
http://research.dwp.gov.uk/asd/asd5/rports20032004/rrep227.pdf
O’Donnell M. Rehabilitation Keeping people in work.
Chief Medical Officer’s Report 2006 UNUM
Provident. 2006.
http://www.unum.co.uk/NR/rdonlyres/9BD9F1FF-A47145A2-9427-347A660D0C18/0/CMOreport2006_UP125
0.pdf
The Marmot Review. Fair Society, Healthy Lives.
February 2009.
http://www.ucl.ac.uk/gheg/marmotreview/
FairSocietyHealthyLives
May T. Speech Theresa May: Labour cannot afford to
duck the challenge of welfare reform Wednesday,
March 25 2009.
http://www.conservatives.com/News/Speeches/2009/03/Th
eresa_May_Labour_cannot_afford_to_duck_the_challenge_of_
welfare_reform.aspx
Palmer KT, Cox RAF, Brown I. Fitness for work – the
Medical Aspects. Faculty of occupational Medicine 4th
ed. 2007
PricewaterhouseCoopers LLP. Building the case for
wellness. Commisioned by the Health, Work and
Wellbeing directorate. Feb 2008.
http://www.workingforhealth.gov.uk/documents/dwp-wellnessreport-public.pdf
Men’s Health Forum. National Men’s Health week
2008, improving men’s health by taking action in the
workplace – A policy briefing paper. 2008.
http://www.menshealthforum.org.uk/content/mhw08policydocpdf
Perkins R, Farmer P and Lichfield P. Realising
Ambition: better employment support for people with
a mental health condition. Department of Work and
Pensions. December 2009.
http://www.dwp.gov.uk/docs/realising-ambitions.pdf
McGee R, Bevan S and Quadrello T. Fit for work?
Musculoskeletal disorders and the Austrian labour
market The Work Foundation May 2009.
http://www.fitforworkeurope.eu/WebsiteDocuments/ffw_Austria180609.pdf
Pugner KM, Scott DL, Holmeds JW, Hieke K .The
costs of rheumatoid arthritis: an international longterm view. Semin. Arthritis Rheum. 2000;29: 305-320.
National Audit Office. Services for people with
rheumatoid arthritis – report by the controller and
Auditor General. July 2009.
http://www.nao.org.uk/publications/0809/services_for_people
_with_rheum.aspx
Rose D. Poorest Britons suffer 17 more years of ill
health and disability. The Times. February 11th 2010.
http://www.timesonline.co.uk/tol/life_and_style/health/article
7022784.ece
National Audit Office. Services for people with
rheumatoid arthritis - international comparisons. July
2009.
http://www.nao.org.uk/publications/0809/rheumatoid_arthrit
is.aspx
Sainsbury R, Irvine A, Aston J, Wilson S, Williams C,
Sinclair A. Mental health and employment. SPRU and
IES on behalf of the Department of Work and
Pensions. Research Report 513. Norwich 2008.
http://research.dwp.gov.uk/asd/asd5/rports20072008/rrep513.pdf
NHS Information Centre, Indicators for Quality
Improvement, Full Indicator List, Available at:
https://mqi.ic.nhs.uk/IndicatorsList.aspx
40
Sainsbury R , Nice K, Nevill C, Wood M, Dixon J,
Mitchell M. The Pathways Advisory Service: Placing
employment advisers in GP surgerues. SPRU and
NCDR on behalf of Department of Work and
Pensions. Research Report 494. Norwich 2008.
http://research.dwp.gov.uk/asd/asd5/rports20072008/rrep494.pdf
Wallop H. Two thirds on disability benefits are fit to
work. The Daily Telegraph. 1st Feb 2010.
http://www.telegraph.co.uk/news/uknews/7120922/Twothirds-on-disability-benefits-are-fit-to-work.html
Young A. Early Rheumatoid Arthritis study
rheumatoid.org.uk May 2004
http://www.rheumatoid.org.uk/article.php?article_id=42
SCMH. Briefing 40: Removing Barriers. The facts
about mental health and employment. SCMH July
22nd 2009.
http://www.scmh.org.uk/pdfs/briefing40_Removing_barriers_
employment_mental_health.pdf
Shell S. LMCs warn that fit notes more open to
forgery than sick notes. healthcarerepublic.com April
20th 2010.
http://www.healthcarerepublic.com/search/news/997725/L
MCs-warn-fit-notes-open-forgery-sick-notes/?DCMP=ILCSEARCH
SHiFT. Line Managers Resource. 2007.
http://kc.csip.org.uk/viewdocument.php?action=viewdox&pid=
0&doc=36315&grp=586
UK Government Improving health and work:
changing lives. Department of health and Department
of work and pensions. Crown TSO 2008
http://www.workingforhealth.gov.uk/documents/improvinghealth-and-work-changing-lives.pdf
Vaughn-Jones H, Barham L. Healthy Work Challenges
and Opportunities to 2030 Bupa 2009
http://www.bupa.com/jahia/webdav/site/bupacom/shared/
Documents/PDFs/ourcommitment/publication/health_at_work-report.pdf
Waddell G, Burton K, Kendall N. Vocational
rehabilitation: what works, for whom and when?
London, TSO. 2008.
Waddell G, Burton K. Is work good for your health
and wellbeing London, TSO. 2006.
Waddell G, Aylward M, Sawney P. Back Pain,
Incapacity for Work and Social Security Benefits: an
international literature review and analysis, The Royal
Society of Medicine Press, London. 2002.
Waddell G, Aylward M. Models of Sickness and
Disability: Applied to Common Health Problems. The
Royal Society of Medicine: London: 2009.
41
Health,disease
and unemployment:
The Bermuda
Triangle of Society
Jonathan Shapiro
Emma Hill
Julia Manning
The measure of successful NHS treatment is increasingly not
a case of whether a process target has been met, but whether
that treatment was a success. In other words, what was the
final ‘outcome’? Did the patient get better and stay well?
Added to this is the crucial question for the working age
population – how quickly did they get back to work?
This project looked at whether being at work is or could be
considered a clinical ‘outcome’ of successful health
treatment. Can keeping people in work or returning them to
work find its place as an indicator of a successful health
intervention on which professionals or institutions can be
measured? We make fourteen recommendations and
observations that we believe will be of value to policy makers.
The overall challenge is increasing the visibility to frontline
professionals and employers of those trapped in the
‘Bermuda Triangle’ of illness, wanting to work and
unemployment - rescuing or preventing them from getting
lost there in the first place.
2020health.org
83 Victoria Street
London SW1H 0HW
T 020 3170 7702
E admin@2020health.org
Published by 2020health.org
© 2010 2020health.org
Price £10
ISBN 978-1-907635-06-9