Pre-eclampsia – the “uterine reinnervation” view.
advertisement

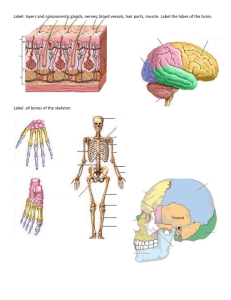
Medical Hypotheses (Abstract 330 words) (Article 2062 words, 32 references, 2 figures) Pre-eclampsia – the “uterine reinnervation” view. MJ QUINN, MB ChB, MD, MRCOG, LLM. The author declares no financial interests or conflicts of interest associated with this article. Corresponding author: MJ Quinn, MD, LLM. 38 Harwood Road, Fulham, London, SW6 4PH. Telephone: E-mail: 0044-7710-288477 mjquinn001@btinternet.com The “uterine reinnervation” view. Summary Difficult vaginal deliveries, gynaecological surgery, and, persistent straining during defaecation injure uterine nerves. Cytokines released from injured, uterine nerves cause regeneration of new nerves with altered structures and functions. In structural terms, these new nerves proliferate in chaotic and dysfunctional patterns with abnormal, cross-sectional profiles. In functional terms they are particularly sensitive to “stretch” or mechanosensory transduction. Release of neural cytokines also causes hyperplasia of the walls of adjacent, denervated uterine arterioles that may reduce uteroplacental blood flow during pregnancy. In the “uterine reinnervation” view, “stretch” applied to injured uterine nerves triggers uterorenal nerves to cause vasoconstriction in the renal cortex, hypertension and proteinuria i.e. the key features of preeclampsia. There are two intrauterine mechanisms that stretch injured, uterine nerves (a) in the placental bed, (b) in the extraplacental myometrium, respectively. In “early-onset” preeclampsia (<34 weeks), continuing increases in maternal plasma volume, increase blood flow through denervated, and, narrowed uterine arterioles in the placental bed, stretching injured perivascular nerves resulting in preeclampsia with a small-forgestational-age fetus. In “late-onset” preeclampsia (>34 weeks), nulliparity, multiple pregnancy, concealed abruption and polyhydramnios increase myometrial tension and results in preeclampsia with an appropriate-for-gestational-age fetus. Widespread activation of autonomic nerves results in multi-system features of these syndromes. Changes in placental site and circulatory compliance may contribute to different phenotypes of the preeclamptic syndromes in subsequent pregnancies. The “uterine reinnervation” view offers an explanation of the common clinical features of the preeclamptic syndromes through a single pathophysiological mechanism, namely, prepregnancy injury to uterine nerves. Importantly, it offers 2 The “uterine reinnervation” view. an explanation for resolution of the symptoms and signs of preeclampsia with delivery of the fetus, the “early” and “late-onset” preeclamptic syndromes, and, the established clinical associations of the condition including nulliparity, hydramnios, multiple pregnancy, molar pregnancy, concealed abruption, etc. Establishing the presence of injured nerves expressing mechanoreceptors in the uterus, and, neural cytokines in thickened, uterine arterioles, will assist in developing this view. However, myometrial hyperplasia during the second half of pregnancy separates injured uterine nerves from injured uterine arterioles ensuring that the key pathoanatomical relationship in preeclampsia will be difficult to demonstrate. 3 The “uterine reinnervation” view. Preeclampsia is characterized by the onset of hypertension and proteinuria in the second half of pregnancy (140/90 mm, >0.3g proteinuria per 24 hours). It affects 5-8% of women with increased incidences in teenagers, women over 35 years of age, and, first-degree relatives (1). Clinical associations of preeclampsia include nulliparity, multiple pregnancy, polyhydramnios, concealed abruption, hydatidiform mole, pre-existing hypertension, diabetes mellitus, obesity, and, renal disease. Severe preeclampsia (BP 160/110 mm, > 5g proteinuria per 24 hours) frequently results in multi-system disease that manifests as thrombocytopenia, abnormal liver function, pulmonary oedema, and seizures. Recent clinical and histological observations suggest there are two, distinct, clinical and placental phenotypes of the pre-eclamptic syndromes (2). Preeclampsia prior to 34 weeks gestation (“early-onset”) demonstrates placental hypoplasia with many placental vascular lesions that result in a small-for-gestational-age fetus. After 34 weeks gestation (“late-onset”) there are fewer placental lesions and an appropriatefor-gestational-age fetus. Evidence from retrospective, cohort studies suggests that women with preeclampsia delivering small-for-gestational-age babies, suffer increased risks of cardiovascular disease in later life (3). Different, though overlapping, intrauterine mechanisms may account for the development of preeclampsia, and, their remote consequences, in these two, distinctive clinical syndromes. 4 The “uterine reinnervation” view. Previous theories of preeclampsia The “uterine reinnervation” view describes some of the diverse and varying consequences of injuries to uterine nerves (Fig. 1). It brings together two previous strands of research in the history of preeclampsia; the “mechanical distension” theory and the “placental ischaemia” theory. Both take origin from the initial observation of proteinuria in women with eclampsia by Dr Charles Lever (1843, Guy’s Hospital, London) (4). The “mechanical distension” theory gathered momentum in the second half of the nineteenth century when WH Dickinson (1868, St Georges Hospital, London) proposed that proteinuria resulted from compression of the renal veins and inferior vena cava by the pregnant uterus (5). In 1929, RH Paramore (Rugby Hospital) published an updated version of the “mechanical distension” theory though it received less attention with the emergence of the “placental ischemia” theory in the 1930’s (6). The “placental ischemia” theory originated in 1914 when Dr James Young (University College Hospital, London) found histological evidence of villous overcrowding adjacent to areas of placental infarction on the fetal side of the maternal-fetal interface. However, Young continued to attribute preeclampsia to “toxins” released from these infarcts (7). Dr EW Page (1939, University of California at San Francisco) formally set out the “placental ischaemia” hypothesis that achieved histopathological endorsement with the observations of Drs. HG Dixon and WB Robertson (8, 9). They described irregular narrowing of uterine spiral arterioles in the placental bed on the maternal side of the maternal-fetal interface that may be the source of the placental infarcts described by Dr Young and earlier workers [7, Fig. 2a-d]. In recent years narrowing of uterine arterioles has been associated with different patterns of reproductive loss including miscarriage, cornual ectopic pregnancy, 5 The “uterine reinnervation” view. midtrimester loss, intrauterine growth retardation, preterm labour and placental abruption (10). Originally, this lesion was held to arise from “two waves of trophoblast invasion” though there are continuing doubts about the site and timing of these histological events (11). The lesion also occurs in non-pregnant women with endometriosis-associated infertility, and, in cornual, ectopic pregnancies at eight weeks gestation (12, Fig. 2b-d). Narrowing of uterine spiral arterioles may, therefore, be a non-specific finding indicative of an injury to uterine vasomotor nerves, that is an antecedent of both preeclampsia and other forms of reproductive loss. The “uterine reinnervation” view has its modern origins in statements by Dr Otto Spiegelberg (1878, Breslau) who said that eclampsia was caused by “severe renal vasospasm, reflexly elicited by uterine distention, and that prolongation of the vasoconstriction would result in irreversible renal disease” (13). In his scholarly account (14), Dr Chesley records that both Gabelchoverus (1596) and Mauriceau (1694) attributed preeclampsia to “irritation of the uterus” (15, 16). He further notes that GJ Sophian revived this hypothesis when observing the experimental basis for neural connections between the uterus and kidneys in rabbits (17). He found that distending an intrauterine balloon caused reflex renal vasoconstriction, and, that cutting the nerves between the uterus and kidneys abolished this reflex (17). Recent Doppler studies demonstrating increases in the resistance of uterine and renal circulations that vary directly with increasing blood pressure, provide evidence for uterorenal connections in women with preeclampsia though further studies describing their relationships with changes in the uterine artery waveform, and, their changes at delivery might be helpful (18, 19). These abstracted observations within the history of research into preeclampsia do not sit in any coherent theoretical framework, however, they contribute important elements to the “uterine reinnervation” view. 6 The “uterine reinnervation” view. Injuries to uterine nerves Uterine sympathetic nerves take origin from T10-12 and L1-2 whilst parasympathetic fibres arise from S2-4. They traverse the hypogastric plexi before entering the uterus with the uterine artery, and, through the uterosacral ligaments (Fig. 1). Subserosal and endometrial-myometrial nerve plexi sparsely innervate the myometrium before the nerves continue into the muscle layers of the Fallopian tube. Injuries to uterine nerves result from, difficult first labours, excessive traction to the cervix and over-vigorous curettage during minor gynaecological procedures, and, persistent straining during defaecation (Fig. 2b, 20, 21). Physical efforts during defaecation affect 20-30% of Western populations, and, may affect different pelvic organs depending on the shape of the pelvis, and, pattern of straining efforts (22). The site, nature and extent of the neurological injury affects its histological appearance and clinical consequences (20, 21, 23). Injuring uterine vasomotor nerves causes regenerating aberrant nerves to sprout in close apposition to adjacent, denervated blood vessels (Fig. 2a-d). These injuries contrast with chaotic reinnervation following difficult vaginal deliveries, and, traction to the cervix, or, over-vigorous curettage during minor gynaecological procedures (21). Varying injuries to autonomic nerves have diverse consequences including changes in visceral form and, function (20, 24). The structural effects in the uterus include myometrial and endometrial hyperplasia that results in some forms of leiomyoma and adenomyosis (21, 25). The functional effects include altered afferent function where stretching injured, myometrial nerves generates autonomic signals between the uterus and kidneys that result in renal vasoconstriction, hypertension and proteinuria [26]. There is clear evidence from bladder studies that stretching epithelial cells releases adenosine triphosphate (ATP) that acts on injured nerves to 7 The “uterine reinnervation” view. initiate impulses in sensory pathways (27). Clinical evidence suggesting that myometrial “stretch” is important in the aetiology of some forms of preeclampsia includes increased rates of preeclampsia in nulliparous women, multiple pregnancy, hydramnios, hydatidiform mole and concealed, antepartum haemorrhage. Daily clinical experience confirms that removal of the “stretch” stimulus at delivery of the fetus and placenta leads to prompt resolution of the clinical syndrome; a feature of the condition that has not been satisfactorily explained by previous theories (1). 8 The “uterine reinnervation” view. The “uterine reinnervation” view The central feature of the “uterine reinnervation” view is that applying stretch to regenerated, intrauterine nerves at different anatomical sites and different gestational ages, generates neural signals in the uterorenal nerves that cause renal vasoconstriction, hypertension and proteinuria. In the “early onset” syndrome (before 34 weeks) it is also necessary to explain concurrent narrowing of uterine arterioles in the placental bed that results in a small-for-gestational-age baby (SGA). (a) Narrowing of uterine arterioles Prepregnancy injuries to uterine vasomotor nerves have important consequences. Firstly, release of neural cytokines at the time of the injury results in regeneration of “new” nerves in close proximity to the arteriole. These nerves have different anatomical profiles, and, different properties. Specifically, in anatomical terms there are many more nerves after the injury, and, the cross-sections of these nerves are abnormal (Fig. 2b-d). At the same time the flood of neural cytokines released from the proximal stump of the nerve also act on the now-denervated, arteriolar walls, causing irregular hyperplasia of the vessel walls with narrowing of their lumens (Fig. 2b-d). Uteroplacental flow is reduced, and, may lead to a small-forgestational-age fetus in a subsequent pregnancy. In this account, narrowing of uterine arterioles is simply a marker of injury to uterine vasomotor nerves; it is not specific to any form of pregnancy loss. (b) Intrauterine “stretch” receptors In addition to the anatomical changes in the injured uterine nerves, there are important changes in their functional properties. The key change is that these new, regenerative nerves are particularly sensitive to “stretch”. There is clear evidence in the bladder that injured nerves express purinergic mechanoreceptors e.g. P2X2, P2X3, P2X7, that are sensitive to “stretch” and use adenosine triphosphate as a 9 The “uterine reinnervation” view. neurotransmitter. Such receptors have yet to be demonstrated in the uterus in hypertensive pregnancy though regenerating autonomic nerves may generically, express these receptors in different forms depending on the nature of the injury and the tissue of origin. In the “uterine reinnervation” view they form the primary sensory mechanism that activate the uterorenal nerves to cause renal vasoconstriction, hypertension and proteinuria. (c) “Early” and “late” onset syndromes There are two, distinct, mechanisms that stretch injured, uterine nerves. In “earlyonset” preeclampsia (before 34 weeks), continuing increases in maternal plasma volume up to 34 weeks gestation, increase blood flow through denervated uterine arterioles in the placental bed, and, stretch injured perivascular nerves resulting in preeclampsia with a small-for-gestational-age fetus (Fig. 2d). In “late-onset” preeclampsia (after 34 weeks), nulliparity, multiple pregnancy, concealed abruption and polyhydramnios increase myometrial tension and results in preeclampsia with an appropriate-for-gestational-age, fetus. In both circumstances, stretch (mechanosensory transduction) results in neural signals from the uterus to the kidney that lead to vasoconstriction in the renal cortex with hypertension and proteinuria. (d) Clinical variations of preeclampsia There are many clinical variations of the preeclamptic syndromes that require explanation within the framework of “uterine reinnervation”. Concomitant injuries to uterorenal nerves may result in a small-for-gestational-age fetus without the renal consequences of hypertension and proteinuria (Fig. 2d). In exceptional circumstances, proliferating molar tissue in injured uterine arterioles may account for severe preeclampsia in the first half of pregnancy, as well as concomitant pulmonary metastases (28). Pre-existing hypertension and renal disease may reduce renal thresholds for developing hypertension and proteinuria. Preterm labour and 10 The “uterine reinnervation” view. placental abruption complicating preeclampsia, represent further diverse consequences of denervation of the lower genital tract that may include opportunist infection, and, injury to denervated, myometrial blood vessels (29). Post-partum “eclampsia” on days 5-6 arises from temporary hypertension associated with physiological readjustments of the maternal circulation, rather than the consequences of intrauterine changes (30). (e) Physical separation of nerve and blood vessels during pregnancy Uterine nerves do not elongate during the myometrial hypertrophy of the second half of pregnancy (30). This physiological process separates injured uterine nerves, that do not stretch along their longitudinal axis, from denervated uterine blood vessels that do respond to the endocrine environment during this phase of pregnancy (31). Confirmatory evidence for this anatomical separation arises from histology of narrowed uterine spiral arterioles that show diminishing evidence of injured perivascular nerves during the first half of pregnancy (Fig. 2b-c), and, that continues into the second half of pregnancy (Fig. 2d). Previous studies in the placental bed in women with adverse pregnancy outcomes have shown no evidence of nerves in a small number of uteri, as might be anticipated (32). (f) Autonomic denervation in the uterus and other pelvic organs Many clinical conditions result from the diverse and varying consequences of injuries to autonomic nerves that include changes in form and function, sensitivity to infection and different toxins, pain and sensitization of the central nervous system (22, 23). In reproductive biology, the three primary uterine pathologies of leiomyoma, adenomyosis and endometriosis result from injuries to uterine nerves (20, 21, 24). Most forms of pelvic, uterine, vaginal and vulval pain are consequences of injuries to uterine nerves (20, 21). Irritative bladder and bowel symptoms also demonstrate aberrant reinnervation (23). Now, in this framework, it seems likely that many of “great obstetric syndromes” including preeclampsia, 11 The “uterine reinnervation” view. preterm labour, placental abruption, etc. may be consequences of autonomic denervation (33). A woman’s reproductive health may depend on the integrity of her pelvic autonomic nerves. Preventing injury to these nerves through common procedures such as good diet and bowel habits, better gynaecological surgery, and, improved first labours, is a feasible ambition for contemporary clinical care. Moreover, many extrapelvic, Western diseases demonstrate unexplained denervation or reinnervation that may also result from similar injuries (23). Conclusion The “uterine reinnervation” view provides a mechanism for many of the clinical and histopathological features of the preeclamptic syndromes. Straining during defaecation and minor gynaecological surgery prior to a first pregnancy, injure uterine nerves that regenerate to express primitive stretch receptors. Applying stretch to these injured uterine nerves at different anatomical sites and gestational ages, stimulates uterorenal nerves to cause vasoconstriction in the renal cortex, hypertension and proteinuria. Key evidence to support this view might include demonstrating neural cytokines in the walls of injured blood vessels, and, demonstrating mechanoreceptors on injured, uterine nerves. For the first time, this view offers explanations for the key associations of preeclampsia including nulliparity, hydramnios, multiple pregnancy, concealed abruption, molar pregnancy, etc., the early and late-onset syndromes, and, the resolution of hypertension and proteinuria with removal of intrauterine “stretch” at the time of delivery. However, many clinicians are unfamiliar with the morphology of the pelvic autonomic nerves, and, myometrial hypertrophy during the second half of pregnancy separates injured uterine nerves from denervated uterine blood vessels, concealing the key pathoanatomical relationship in preeclampsia. 12 The “uterine reinnervation” view. References (1) Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005; 365(9461):785-99. (2) Nelson DB, Ziadie MS, McIntyre DD, Rogers BB, Leveno KJ. Placental pathology suggesting that preeclampsia is more than one disease. Am J Obstet Gynecol 2014; 210:66.e1-7. (3) Barker DJP, Osmond C, Winter PD, Margetts B, Simmonds SJ. Weight in infancy and death from ischaemic heart disease. Lancet 1989; 2(8663):577-80. (4) Lever JCW. Causes of puerperal convulsions with remarks. Guys Hospital Reports 1843; 1 (2d series): 495-517. (5) Dickinson WH. On the pathology and treatment of albuminuria. London, Longmans Green, 1868, p115. (6) Paramore RH. An introduction to the mechanistic conception of eclampsia. Lancet 1928; 2:914. (7) Young J. The Aetiology of Eclampsia and Albuminuria and their Relation to Accidental Haemorrhage: (An Anatomical and Experimental Investigation.). Proc R Soc Med. 1914;7(Obstet Gynaecol Sect):307-48. (8) Page EW. The relation between hydatid moles, relative ischemia of the gravid uterus, and the placental origin of eclampsia. Am J Obstet Gynecol 1939; 37:291-3. (9) Dixon HG, Robertson WB. A study of the vessels of the placental bed in normotensive and hypertensive women. J Obstet Gynaecol Br Emp. 1958; 65(5):803-9. (10) Brosens IA, Pijnenborg R, Vercryusse L, Romero R. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol 2011; 204(3):193-201. (11) Pijnenborg R, Dixon G, Robertson WB, Brosens I. Trophoblastic invasion of human decidua from 8 to 18 weeks of pregnancy. Placenta. 1980; 1(1):3-19. (12) Wu XQ, Chen HY, Wan L, Quinn MJ. Abnormal innervation of uterine blood vessels in cornual ectopic pregnancy. J Obstet Gynaecol 2014 (in press). 13 The “uterine reinnervation” view. (13) Spiegelberg O. Lehrbuch der Geburtsch fur Artze u. Studierende. Schauenburg. Lahr. 1878. (14) Chesley LC. Hypertensive disorders in pregnancy. Appleton-Century-Crofts, 1978. (15) Gabelchoverus. Artzneybuch, darninnen vast fur alle des menschlichen Leibs, anlingen und Gebrechen, ausserlesene und bewehrte Artzneyen usw. Tubingen., Gruppenback, 1596. (16) Mauriceau F. Traite des Maladies des Femmes Grosses, et celles Qui Sone Accouchees Einseignant la Bonne et Verritable Methode pour Bien Aider , etc. Book II, Chap 28, Paris, d’Houry, 1694. (17) Sophian GJ. Toxaemias of pregnancy. London: Butterworth, 1953. (18) Miyake H, Nakai A, Koshino T, Araki T. Doppler velocimetry of maternal renal circulation in pregnancy-induced hypertension. J Clin Ultrasound. 2001; 29(8):449-55. (19) Nakai A, Miyake H, Oya A, Asakura H, Koshino T, Araki T. Reproducibility of pulsed Doppler measurements of the maternal renal circulation in normal pregnancies and those with pregnancy-induced hypertension. Ultrasound Obstet Gynecol. 2002; 19(6):598-604. (20) Quinn MJ. Endometriosis; the consequence of uterine denervation-reinnervation. Arch Obstet Gynaecol 2011; 284:1423-9. (21) Atwal G, du Plessis D, Armstrong G, Slade R, Quinn M. Uterine innervation after hysterectomy for chronic pelvic pain with, and without, endometriosis. Am J Obstet Gynecol. 2005;193(5):1650-5. (22) Heaton KW, Cripps HA. Straining at stool and laxative taking in an English population. Dig Dis Sci 1993; 38(6):1004-8. (23) Quinn M Autonomic denervation and Western diseases. Am J Med 2014; 127(1):3-4. (24) Quinn M. Uterine innervation in fibroids: a qualitative study. J Obstet Gynaecol. 2007; 27(5):489-92. 14 The “uterine reinnervation” view. (25) Quinn MJ. Perivascular nerve fibre proliferation: the consequence of prolonged straining. J Obstet Gynaecol. 2007; 27(2):185-8. (26) Goldblatt H, Lynch J, Hanzel RF, Summerville WW. Studies on experimental hypertension. I. The production of persistent elevation of systolic blood pressure by means of renal ischemia. J. Exp. Med. 1934; 59:347–379. (27) Burnstock G. Purinergic mechanosensory transduction and visceral pain. Mol Pain. 2009; 30(5):69-81. (28) Page EW. On the pathogenesis of pre-eclampsia and eclampsia. J Obstet Gynaecol Br Commonw. 1972 ;79(10):883-94. (29) Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008; 371(9606):75-84. (30) Walters BN, Thompson ME, Lee A, de Swiet M. Blood pressure in the puerperium. Clin Sci (Lond). 1986; 71(5):589-94. (31) Wikland M, Lindblom B, Dahlström A, Haglid KG. Structural and functional evidence for the denervation of human myometrium during pregnancy. Obstet Gynecol. 1984 ; 64(4):503-9. (32) Khong TY, Tee JH, Kelly AJ. Absence of innervation of the uteroplacental arteries in normal and abnormal human pregnancies. Gynecol Obstet Invest. 1997; 43(2):89-93. (33) Brosens I, Pijnenborg R, Vercruysse L, Romero R. The “great obstetrical syndromes” are associated with disorders of deep placentation Am J Obstet Gynecol 2011; 204(3):193-201. 15 The “uterine reinnervation” view. 16