Vallerie Gordon BSc, MD, FRCPC Medical Oncologist Assistant
advertisement

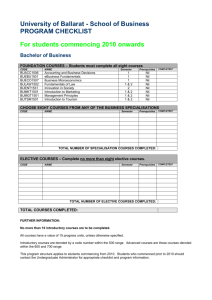
Vallerie Gordon BSc, MD, FRCPC Medical Oncologist Assistant Professor University of Manitoba & CancerCare Manitoba Conflict of Interest Disclosure: Type of Affiliation/Financial Support Name of Commercial Organization Self Spouse or immediate family Consultant nil nil Speaker Bureau nil nil Grants/Research Support Unrestricted educational grant Roche Pharmaceuticals x nil Advisory Board Membership Roche Pharmaceuticals x nil Honorarium Recipient nil nil Stockholder (Not as part of Mutual Fund) nil nil Trustee/Director nil nil Other (Describe): nil nil Objectives: At the end of this session participants will be able to recognize the use and potential for misuse of tumour markers to: 1. Identify or diagnose disease. 2. Monitor patients for response to treatment of disease. 3. Assess for recurrence of disease. Examples of Tumour Markers Tumour Marker Cancer Use AFP (Alfafetoprotein) Liver cancer and germ cell tumours (testicular and ovarian) Testing on blood To help diagnose liver Ca and germ cell tumours, follow response to treatment, to stage, prognosticate and for response to treatment and to identify recurrence of germ cell cancers B2M Multiple myeloma, CLL and some lymphomas Blood test – to prognosticate and follow response to treatment Beta-hCG Choriocarcinoma and testicular cancer To assess stage, prognosticate and follow response to treatment and identify recurrence CA15-3(CA = Breast Cancer To assess treatment response CA19-9 Pancreatic , gallbladder, bile duct, gastric and colon cancers Blood test – to follow for treatment response or progression CA125 Ovarian cancer Blood test – for assessment of response to treatment, assessment for recurrence carbohydrate antigen) Tumour Marker Cancer Use Calcitonin Medullary thyroid cancer Blood test – to aid diagnosis, assess for treatment response, and assess for recurrence CEA Colorectal and breast cancer Blood test – to assess for progression, or treatment response in colon cancer and breast cancer, and assess for recurrence in colon cancer Chromogranin A (CgA) Neuroendocrine tumours Blood test – to help with diagnosis, assessment of treatment response, and evaluate for recurrence Immunoglobulins Multiple myeloma and Waldenstom macroglobulinemia Blood and urine (SPEP & UPEP) – to diagnose disease, assess response to treatment and watch for recurrence LDH Germ cell tumours To assess stage, prognosis, and response to treatment PSA Prostate cancer Blood test – to help with diagnosis, assess response to treatment, and watch for recurrence Thyroglobulin Thyroid cancer Blood test – to evaluate response to treatment and watch for recurrence Cancer of Unknown Primary? What is CUP? A cancer that has been thoroughly worked up diagnostically with no confirmed diagnosis With CUP, the tumour markers will often be assessed at presentation by the medical oncologist, and if elevated, they may be useful to follow treatment response Like in colon cancer, would suggest test pre each cycle For Diagnostic purposes? Utility? Cancer of uncertain Primary In the setting of widespread metastatic disease diagnosis can be challenging Tumour markers are helpful only with a clear assessment of the extent of disease and suspected diagnosis to point in the direction of the most common diagnosis Should be done after all other staging complete (imaging) Colon Cancer: CEA +/- CA19-9 Preoperatively in resectable disease - in known colorectal cancer - may be helpful to assess for CEA levels (identify secretory disease) Adjuvant disease setting CEA Every 3 months for 3 years, then guidelines do not recommend, but at discretion of medical oncologist may check every 6 months for additional 2 years Metastatic disease setting No clear guidelines, but CEA and CA19-9 often checked pre each cycle to follow for progression between scans Expect initial rise in one or other with treatment, then expect it to fall if effective Absolute value less important than the trend generally Why CA19-9? If both CEA and CA19-9 are decreasing or stable - highly supports a “lack of progression” of disease Often elevated with peritoneal involvement Pancreas, Gall Bladder, Biliary tract, and Gastric Cancers & CA19-9 For assessment of metastatic disease on treatment to assess response Checked prior to each cycle of treatment for indication of disease progression May be useful for detection of recurrence after resection but currently no guidelines recommending use (no proven quality of life or survival benefit) Breast Cancer: CA15-3 & CEA Useful to monitor disease progression when treating metastatic disease Not useful for diagnostic purposes generally Expected trends: As with CEA in colon cancer, values may increase initially, then should fall if responding to treatment Absolute number is not important, the trend over a few cycles is the important message Generally with each assessment: On endocrine therapy – every 2 – 3 months On chemotherapy – pre each cycle Prostate Cancer and PSA Screening: Still an area of contention Canadian Urologic Association (CUA) suggests PSA be tested for screening purposes, not supported by the US group Canadian Cancer Society suggested a discussion rather than routine PSA screening Generally checked every 3 – 6 months after surgery to assess for biochemical recurrence Metastatic disease – generally monitor with each assessment on treatment Endocrine therapy – every 2 – 3 months Chemotherapy – prior to each cycle Ovarian Cancer and CA125 Not useful for diagnosis generally, but in setting of unclear, potentially operable, peritoneal disease may play a role preoperatively In metastatic disease may help to determine treatment response – again, check pre treatments with each evaluation Following surgery and chemotherapy, may aid in early diagnosis of recurrent disease – checked with each reevaluation Testicular or Germ Cell Tumours: AFP & b-hCG Checked at diagnosis or with suspected diagnosis Post surgical: used to assess for recurrence if elevated preoperatively – guidelines recommend evaluation by oncologist with set intervals postoperatively Post operatively, expect that if no residual disease, the levels should normalize AFP – should do so in 25 – 30 days (depends on value at presentation) b-hCG – should do so in 7 -10 days Postoperative chemotherapy – used to monitor for disease response and expect the values to fall as for post operative decline Metastatic disease – used to assess for response to therapy Neuroendocrine Tumors: chromogranin (CgA) and u5HIAA Chromogranin - Checked in the post resection period for high risk disease first every 3 months, then every 6 months For patients on treatment, check with each reevaluation – generally every 3 months Urine 5HIAA – checked less frequently and requires dietary changes prior to the test Chromogranin - Must be ordered by a medical oncologist in Manitoba Not done in Manitoba – samples are sent for evaluation in USA by Mayo clinic from Manitoba currently