Guidelines for the interpretation of the neonatal electrocardiogram
advertisement

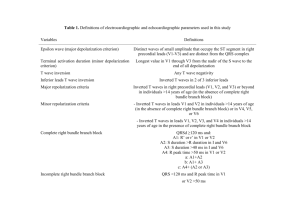
European Heart Journal (2002) 23, 1329–1344 doi:10.1053/euhj.2002.3274, available online at http://www.idealibrary.com on Task Force Report Guidelines for the interpretation of the neonatal electrocardiogram A Task Force of the European Society of Cardiology P. J. Schwartz1 (Chair), A. Garson, Jr2, T. Paul3, M. Stramba-Badiale4, V. L. Vetter5, E. Villain6 and C. Wren7 1 Department of Cardiology, University of Pavia and IRCCS Policlinico S. Matteo, Pavia, Italy; 2University of Virginia, Charlottesville, VA, U.S.A.; 3The Children’s Heart Program of South Carolina, Medical University of South Carolina, Charleston, SC, U.S.A.; 4Pediatric Arrhythmias Center, IRCCS Istituto Auxologico Italiano, Milan, Italy; 5Division of Pediatric Cardiology, Department of Pediatrics, Children’s Hospital of Philadelphia, University of Pennsylvania School of Medicine, Philadelphia, PA, U.S.A.; 6Division of Pediatric Cardiology, Department of Pediatrics, Hôpital Necker Enfants Malades, Paris, France; 7Department of Paediatric Cardiology, Freeman Hospital, Newcastle upon Tyne, U.K. Introduction.............................................................1329 Normal electrocardiogram in the newborn .............1330 Normal values......................................................1330 Technology ..........................................................1330 Artefacts...............................................................1332 Electrocardiographic measurements ....................1332 Heart rate.............................................................1332 P wave..................................................................1332 QRS complex.......................................................1332 QT interval ..........................................................1333 ST segment and T wave ......................................1333 Abnormal electrocardiogram in the newborn .........1333 Heart rate.............................................................1333 Sinus arrhythmia..............................................1333 Sinus tachycardia .............................................1333 Sinus bradycardia.............................................1335 Other bradycardias...........................................1335 P wave..................................................................1335 Atrioventricular conduction.................................1335 Complete (3rd) atrioventricular block .............1335 1st and 2nd atrioventricular block...................1336 Intraventricular conduction .................................1336 Bundle branch block ........................................1336 Non-specific intraventricular conduction abnormalities....................................................1336 Wolff–Parkinson–White syndrome ..................1336 QRS axis and amplitude......................................1338 Right ventricular hypertrophy .........................1338 Correspondence: Peter J. Schwartz, MD, FESC, FACC,, FAHA, Professor & Chairman, Department of Cardiology, Policlinico S. Matteo IRCCS, Viale Golgi, 19-27100 Pavia, Italy. 0195-668X/02/$35.00 Left ventricular hypertrophy............................1338 Low QRS voltage.............................................1338 Ventricular repolarization....................................1338 QT prolongation: differential diagnosis ...........1339 Long QT syndrome..........................................1339 ST segment elevation .......................................1341 Atrial and ventricular arrhythmias......................1341 Atrial/junctional ...............................................1341 Premature atrial beats ..................................1341 Supraventricular tachycardia........................1342 Atrial flutter .................................................1342 Ventricular arrhythmias ...................................1342 Premature ventricular beats..........................1342 Ventricular tachycardia ................................1343 Accelerated ventricular rhythm ....................1343 Conclusion...............................................................1343 Acknowledgements ..................................................1343 References................................................................1343 Introduction Most cardiologists who care for adults have no or minimal experience with electrocardiograms (ECGs) recorded in infants. So far, this has had no practical implications because only seldom are they requested to examine a neonatal ECG. This situation, however, may change as some European countries have begun to consider the possibility of introducing in their National Health Services the performance of an ECG during the first month of life in all newborns, as part of a cardiovascular screening programme. 2002 Published by Elsevier Science Ltd on behalf of The European Society of Cardiology 1330 Task Force Report The background of this evolution is multiple, but it lies largely in the realization that early identification of life-threatening arrhythmogenic disorders, which often manifest in infancy, childhood or even later, may allow initiation of effective preventive therapy. A large prospective study has indicated that some infants with prolonged QT interval in the first week of life had sudden death, and would have previously been labelled as victims of the Sudden Infant Death Syndrome[1]. Furthermore, in infants with this diagnosis, post-mortem molecular screening may reveal the presence of the long QT syndrome (LQTS)[2]. As with most screening tests, a single ECG must be put into context (e.g. family history, etc.). Additionally, it is traditional to examine neonatal ECGs looking for those with parameters below the 2nd or exceeding the 98th percentile. While it is true that these values are ‘abnormal’ in a strict statistical sense, very often ‘abnormality’ does not imply the presence of a disease, or of a risk for clinically relevant events. This depends largely on the parameter under examination. However, also the reverse may be true and, in the neonate, a completely normal ECG may be seen with multiple types of congenital heart defects and with the entire spectrum of arrhythmias. This call for caution does not detract from the valid concept that the identification of ECG abnormalities in the newborn can be the first step toward a meaningful act of preventive medicine. Should this neonatal screening indeed be introduced as part of National Health Services, then hospital cardiologists — most of whom are unfamiliar with neonatal ECGs — would be asked to read these tracings. The European Society of Cardiology (ESC) has realized the potential implications for European cardiologists and for health care, and has acted accordingly. Through the Committee for Practice Guidelines and Policy Conferences, chaired by Werner Klein, it has instituted this Task Force. The experts were designated by the Guidelines Committee and approved by the Board of the ESC. The panel was composed of physicians and scientists involved in clinical practice in University and non-University hospitals. Members were selected to represent experts of different European countries; in addition, two nonEuropean members were included for their worldwide recognized expertise in the field of pediatric electrocardiography. The ESC considers medical education and the improvement of clinical practice among its major obligations. The main objective of the present report is to present adult cardiologists with a consensus document designed to provide guidelines for the interpretation of the neonatal ECG, focusing on the most clinically relevant abnormalities and on the ensuing management and referral options. This document aims also at providing paediatricians and neonatologists with updated information of clinical relevance that can be detected from a neonatal ECG. Eur Heart J, Vol. 23, issue 17, September 2002 The procedure used for developing and issuing these guidelines was in accordance with the recently issued ‘Recommendations for Task Force creation and report writing’, (http://www.escardio.org/scinfo/guidelines_ recommendations.htm) which is a position document of the ESC Committee for Practice Guidelines and Policy Conferences. This document was reviewed and approved by the Commitee for Practice Guidelines and Policy Conferences. It was endorsed by the Board of the ESC and represents the official position of the ESC with regard to this subject. These guidelines will be reviewed two years after publication and considered as current unless the ‘Guidelines’ Committee revises or withdraws them from circulation. This Task Force was financed by the budget of the Committee for Practice Guidelines and Policy Conferences of the ESC and was independent of any commercial, health or governmental authorities. Normal electrocardiogram in the newborn Normal values Changes occur in the normal ECG from birth to adult life. They relate to developmental changes in physiology, body size, the position and size of the heart relative to the body, and variations in the size and position of the cardiac chambers relative to each other. The major changes in the paediatric ECG occur in the first year of life with the majority of normal adult values being abnormal in the newborn. Likewise, many normal newborn values and patterns would be abnormal in the adult. Normal electrocardiographic values in the paediatric population traditionally derive from those published in 1979 by Davignon et al.[3]. From the ECGs of 1027 infants less than 1 year of age and among these, 668 in the first month of life, the percentile distribution of electrocardiographic variables was calculated. It is important to refer to tables of normal values as shown in Table 1. A recent large study by Rijnbeek et al.[4] included an extremely low number of neonates (n=44) but no one below 3 weeks of age. Thus, the percentile tables published by Davignon are recommended for use in clinical practice. Other references on the reading of ECGs in neonates and children are available[5,6]. Technology The normal newborn ECG should include 12 leads. Other leads, V3R, V4R and V7, may provide additional information to evaluate possible congenital heart lesions. The current use of computerized digital ECG systems affects newborn ECGs to a greater extent than those of older children or adults[7]. The newborn ECG may have 93–154 (123) 91–159 (123) 90–166 (129) 107–182 (149) 121–179 (150) 0–1 days 1–3 days 3–7 days 7–30 days 1–3 months +59 +64 +77 +65 +31 to to to to to +192 (135) +197 (134) +187 (132) +160 (110) +114 (75) Frontal plane QRS axisa (degrees) From ref. [3]. a 2nd–98th percentile (mean) b 2nd–98th percentile (1 mm=100 V) c 98th percentile (1 mm=100 V) Heart rate (beats . min 1) Normal neonatal ECG standards* Age group Table 1 2·8 2·8 2·9 3·0 2·6 P wave amplitude (mm) 0·08–0·16 (0·11) 0·08–0·14 (0·11) 0·08–0·14 (0·10) 0·07–0·14 (0·10) 0·07–0·13 (0·10) P-R intervala (s) 0·02–0·08 (0·05) 0·02–0·07 (0·05) 0·02–0·07 (0·05) 0·02–0·08 (0·05) 0·02–0·08 (0·05) QRS durationa V5 5·2 5·2 4·8 5·6 5·4 1·7 2·1 2·8 2·8 2·7 Q IIIc QV6c (mm) (mm) 5–26 5–27 3–24 3–21·5 3–18·5 RV1b (mm) 0–22·5 0–21 0–17 0–11 0–12·5 SV1b (mm) 9·8 6 9·7 7 7·4 R/S V1c 0–11 0–12 0·5–12 2·5–16 5–21 RV6b (mm) 0–9·8 0–9·5 0–9·8 0–9·8 0–7·2 10 11 10 12 12 28 29 25 22 29 52 52 48 47 53 SV6b SV1 +RV6c R+SV4c R/S V6c (mm) (mm) (mm) Task Force Report 1331 Eur Heart J, Vol. 23, issue 17, September 2002 1332 Task Force Report a higher voltage and shorter duration QRS complexes resulting in a higher percentage of high frequency components. The recommendations of a number of groups vary as to the best bandwidth cutoffs and sampling frequency to reduce error[8,9]. Higher bandwidth cutoffs may alter amplitude of signals by as much as 46%[10]. This would make standards determined from analogue signals or digitized signals at lower sampling rates and lower frequency cutoffs different from those at higher settings. The current American Heart Association recommendation for paediatric ECGs is 150 Hz as a minimum bandwidth cutoff and 500 Hz as a minimum sampling rate[11]. The Rijnbeek study reported normals using a higher sampling rate of 1200 Hz. Compared to Davignon’s study, which used a sampling rate of 333 Hz, the newborn upper limits in Rijnbeek’s study were 12–25% higher than in Davignon’s[3,4]. Artefacts Artefacts are common in newborn ECGs and include limb lead reversal and incorrect chest lead positioning. In addition, electrical interference, usually 60 cycles, can occur in hospital settings from bedside monitors, warmers or other equipment. Other artefacts occur because of various types of patient movement common in neonates. These artefacts may be random as with hiccoughs or limb movement. Normal complexes are seen along with the artefacts, and the intrinsic rhythm of the patient is not affected. Other common artefacts include a fine, often irregular undulation of the baseline from muscle tremors or jitteriness. Again, the intrinsic rhythm is not affected. The size of the QRS complex and the baseline may wander in a cyclic fashion with respirations. It should be noted that the neonate breathes from 30–60 times per min. The main clue in determining the presence of an artefact is to evaluate whether it affects the intrinsic rhythm and if it is timed such that it could be a true depolarization. A signal within 80 ms from a true QRS complex could not occur from an electrophysiologic point of view. Electrocardiographic measurements Because of the current limitations of electronic measurements in newborn ECGs, intervals should be hand measured as the computerized systems are often inaccurate in the newborn. Intervals in children increase with increasing age, reaching most of the adult normal values by 7–8 years of age. Heart rate Heart rate can be determined by a variety of methods. It should be noted that normal neonates may have rates Eur Heart J, Vol. 23, issue 17, September 2002 between 150–230 beats . min 1, especially if they are crying or agitated. Over 200 beats . min 1, one-half small box can make an appreciable difference in heart rates. Heart rates between the 2nd and 98th percentile in the first year of life are shown in Table 1. The normal heart rate increases from the first day of life, it reaches a peak between the first and the second month and then declines returning to the values recorded at birth by the sixth month. During the following 6 months, it remains rather stable and then slowly declines after 1 year due to maturation of vagal innervation of the sinus node[12]. Clinically significant gender differences in heart rate are not seen in the neonatal period. P wave The P wave axis is a vector indicating the direction of activation, which is away from the site of origin. By identifying the quadrant location of the P wave axis one can determine the site of origin of the rhythm. For example, sinus rhythm originates in the high right atrium transcribing a P wave with an axis in the quadrant bordered by 0 and +90. Measurements are available for P wave amplitude (Table 1). The P wave is generally pointed in lead II and aVF and more rounded in other leads. Lead V1 may be diphasic. The PR interval is measured from the onset of the P wave to the Q or R wave if no Q wave is present. The PR interval, measured in lead II, increases with age and decreases with heart rate. The normal neonatal PR interval ranges from a minimum of 70 ms to a maximum of 140 ms, with a mean of 100 ms. QRS complex The normal full-term neonate has an axis between 55 and 200 but by 1 month, the normal upper limit has fallen to 160 or less. Although one might identify an axis of 120 as right axis deviation in an adult, it is a normal finding in a newborn. The QRS axis in the premature newborn ECG ranges between 65 and 174. The duration of the QRS complex is measured from the beginning to the end of the ventricular depolarization complex and it should be measured in a lead with an initial Q wave[5]. QRS duration in the newborn and infant is narrow (<80 ms). Normal QRS duration increases with age. Normal values for QRS complex duration in lead V5 are displayed in Table 1. QRS morphology in the newborn may have more notches and direction changes than seen in older children or adults. The direction of the Q wave in the precordial or horizontal plane indicates the direction of septal depolarization. Normally, there is a Q wave in leads V5–V6 indicating depolarization from left to right. Normal values of Q wave amplitudes vary with the lead and with age. Q wave amplitudes may be as high Task Force Report as 0·55 mV in lead III or 0·33 mV in aVF at 1 month. Q wave duration >30 ms is abnormal. The appearance of secondary r waves (r or R) in the right chest leads is frequent in normal neonates. Davignon et al.[3] provided ‘normal’ values in infants. The use of 2nd and 98th percentiles to define normality implies that 4% of the population are ‘abnormal’ for any given single measurement, so ‘normal’ ranges have to be interpreted with caution (Table 1). Thomaidis et al. published normal voltages from healthy term and premature neonates[13]. 1333 10 ms (1/4 of a mm) while we recognize that this may be within measurement error. ST segment and T wave ST segment elevations >1 mm above the isoelectric line are uncommon in the newborn. In neonates and infants it is better to consider as the isoelectric line the TP segment instead of the PQ segment. T waves are normally quite variable in the first week of life. After 1 week, the T wave is negative in lead V1 and positive in V5–V6. QT interval The QT interval is the interval between the beginning of the QRS complex and the end of the T wave. The QT measurement should be made in leads II, V5, and V6 with the longest value being used. The main difficulty lies in identifying correctly the point where the descending limb of the T wave intersects the isoelectric line. Due to the fast heart rate of infants the P wave may be superimposed on the T wave, particularly when the QT interval is prolonged. In this case, the end of the T wave should be extrapolated by drawing a tangent to the downslope of the T wave and considering its intersection with the isoelectric line. The QT interval duration changes with rate and it is usually corrected (QTc) by using Bazett’s formula. Correction of the QT interval requires a stable sinus rhythm without sudden changes in the RR interval. QTc is equal to QT interval in seconds divided by the square root of the preceding RR interval in seconds. To avoid timeconsuming calculations, a simple chart (Fig. 1) where the value of QTc is easily obtained by matching QT and RR interval in millimetres (given the paper speed at 25 mm . s 1) has been produced. When heart rate is particularly slow or fast the Bazett’s formula may not be accurate in the correction but it remains the standard for clinical use. The mean QTc on the 4th day of life is 40020 ms[1] and, at variance with the adult, no gender differences are present[14]. Therefore, the upper normal limit of QTc (2 standard deviations above the mean, corresponding to the 97·5 percentile) is 440 ms. By definition, 2·5% of normal newborns are expected to have a QTc greater than 440 ms. In healthy infants there is a physiological prolongation of QTc by the second month (mean 410 ms) followed by a progressive decline[15], so that by the sixth month QTc returns to the values recorded in the first week. Pitfalls with QT measurement. Despite its apparent simplicity the measurement of the QT interval is fraught with errors. The simple fact that a small square on the ECG paper is equivalent to 40 ms explains why healthy scepticism should accompany claims of clinical importance attached to very small degrees of ‘QT prolongation’. An attempt should be made to measure with Abnormal electrocardiogram in the newborn Heart rate Sinus arrhythmia Since sinus arrhythmia is less pronounced at fast heart rate, neonates show a more regular rhythm than young children and adolescents, particularly in the first week of life. Sinus arrhythmia should be differentiated from wandering pacemaker, which manifests itself with a gradual change of P wave axis and morphology and that is due to a shift of the pacemaker from the sinus node to the atrium and the atrioventricular (AV) junction. Although wandering pacemaker may accompany other types of bradyarrhythmia, it has no pathologic meaning. Work-up No work-up should be necessary unless significant bradycardia coexists. Sinus tachycardia Sinus tachycardia is a sinus rhythm with a heart rate above the normal limit for age. In the newborn the upper normal limit (98th percentile) is 166 beats . min 1 in the first week and 179 beats . min 1 in the first month. After the sixth month the upper normal limit declines to approximately 160 beats . min 1 and at 1 year is 151 beats . min 1. These values have been measured from ECGs recorded when infants were awake and quiet. It has to be noted that newborn infants may transiently reach a heart rate up to 230 beats . min 1. Causes. Sinus tachycardia may be a sign of any condition associated with an increase of cardiac output. The most frequent causes of sinus tachycardia in the neonatal period are represented by fever, infection, anaemia, pain, and dehydration (hypovolaemia). Other causes of sinus tachycardia include neonatal hyperthyroidism and myocarditis, particularly when it is not proportionate to the level of fever. Myocarditis is usually, but not necessarily, associated with other clinical signs, such as gallop rhythm, or ECG abnormalities, including T wave changes and conduction disturbances. Eur Heart J, Vol. 23, issue 17, September 2002 Figure 1 Chart for calculation of QTc. QTc, according to the Bazett’s formula is obtained by matching QT and RR interval in millimetres, given the paper speed at 25 mm . s 1. Corresponding values of RR interval and uncorrected QT interval are also indicated. 1334 Task Force Report Eur Heart J, Vol. 23, issue 17, September 2002 Task Force Report Finally, several drugs that are commonly used during infancy, e.g. beta adrenergic agonists or theophyllin, may induce sinus tachycardia. In the newborn, these may have been transmitted across the placenta or through breast milk. Work-up The evaluation of these patients should be performed according to the underlying condition. If myocarditis is suspected an echocardiogram should be performed. Appropriate acute treatment of causes of tachycardia may be considered. Persistence of elevated rates should be further evaluated. Sinus bradycardia Sinus bradycardia is defined as a sinus rhythm with a heart rate below the normal limit. In the neonatal period the lower normal limit (2nd percentile) is 91 beats . min 1 during the first week and 107 beats . min 1 in the first month of life. At the first month the lower limit increases to 121 beats . min 1 and declines to approximately 100 beats . min 1 in the following months. At 1 year the lower normal limit is 89 beats . min 1. These values apply to an ECG recorded in the awake state when heart rate is measured over two respiratory cycles. Causes. Central nervous system abnormalities, hypothermia, hypopituarism, increased intracranial pressure, meningitis, drugs passed from the mother to infant, obstructive jaundice, and typhoid fever represent causes of sinus bradycardia. As a consequence when sinus bradycardia is present on the surface ECG such conditions should be excluded. Hypothyroidism is another cause of bradycardia and is often associated with the so-called ‘mosque sign’, a dome-shaped symmetric T wave in the absence of a ST segment. Transient sinus bradycardia has been observed in newborns from antiRo/SSA positive mothers, especially women with lupus erythematosus or other connective diseases. A lower than normal heart rate has been described in patients affected by LQTS, a phenomenon which is evident in the neonatal period[16]. It may sometimes represent the first sign of the disease during the foetal period[17]. Work-up 24-h Holter monitoring may be helpful for further evaluation when a heart rate below 80–90 beats . min 1 is present on surface ECG during infancy. Evaluation for underlying conditions should be performed. Other bradycardias Sinus pauses in newborns may last from 800 to 1000 ms. Pauses >2 s are abnormal. Sinus pauses may be followed by escape beats which arise from the atria or from the AV-junction. It has to be noted that even healthy neonates may show periods of junctional rhythm, i.e. a sequence of narrow QRS complexes in the absence of preceding P waves. Causes. Infants with autonomic nervous system dysfunction consisting of augmented vagal tone may have sinus 1335 bradycardia, or significant sinus pauses of several seconds. These generally occur during feeding, sleep, defecation, or other times of increased vagal tone. Apparent life-threatening events (ALTE), described as loss of consciousness accompanied by pallor and hypotonia, have been related to vagal overactivity which may manifest as sinus pauses or abrupt bradycardia. ALTE may be associated with apneic episodes, or gastroesophageal reflux, that may precede severe bradycardia. Infants with LQTS not only tend to have sinus bradycardia but may also have sinus pauses. Work-up 24-h Holter monitoring may be useful for the assessment of significant bradycardia. Long pauses secondary to excessive vagal tone may be eliminated by the use of atropine, and rarely require pacemakers. Treatment of other underlying diseases should be undertaken. P wave Abnormal P waves may be seen in infants with atrial enlargement or non-sinus origin of the P wave. Ectopic atrial rhythms originate most commonly from the low right atrium (0 to 90), high left atrium (+90 to +180) or the low left atrium (+180 to +270). Right atrial enlargement and/or hypertrophy typically produces increased P wave amplitude with a normal P wave duration. The P wave axis usually remains normal so the effect is usually best seen in lead II. Left atrial enlargement and/or hypertrophy typically produces an increased and prolonged negative terminal deflection of the P wave in lead V1 (generally accepted as >40 ms in duration and 0·1 mV in amplitude). Left atrial enlargement also causes exaggerated notching of the P wave in lead II although this is not a specific sign. Work-up An echocardiogram should be performed when clinically indicated. Atrioventricular conduction During atrial tachycardia, it is possible to observe 1/1 conduction through the atrio-ventricular node at rates over 300 beats . min 1. Complete (third degree) atrioventricular block Complete AV block implies complete absence of conduction from atrium to ventricle. ECG shows normal atrial activation and slower dissociated regular QRS complexes. Congenital complete block is observed in complex congenital heart malformations[18]. Approximately one out of every 15 000 to 20 000 live births results in a baby with isolated AV block. The association between isolated neonatal AV block and maternal connective tissue disease is well established and ascribed to the presence of anti Ro/SSA and La-SSB antibodies in the mothers. Nearly every mother with an affected child has circulating antibodies. However, only 2 to 5% of women with known antibodies will have a Eur Heart J, Vol. 23, issue 17, September 2002 1336 Task Force Report first child with AV block[19]. Mortality rate in patients with neonatal AV block is still high, especially during the first 3 months of life[20]. Acquired complete AV block is rare in neonates. It is mainly infective (viral myocarditis, HIV infection) or may be related to tumours. First and second degree atrioventricular block Neonates may present with first or second degree AV block and rare reports exist demonstrating progression to complete AV block after birth in children with and without antibody mediated conduction disorders[21]. Long QT syndrome is occasionally complicated by impaired atrioventricular conduction, mostly 2:1 AV block[22,23]. Functional AV block can be observed in neonates because they have a fast atrial rate and the P wave falls within the very prolonged T wave. Cases of infra-Hisian block location at the His-Purkinje level have been demonstrated[24,25]. In spite of different treatment modes including the use of high doses of betablockers and pacing, there is still significant mortality. Heart block associated with prolonged QT interval has been described in neonates and infants receiving cisapride. Second degree AV block due to QT interval prolongation has been also reported with the use of other agents such as diphemanil[26] or doxapram in premature infants. Work-up In neonates and infants with AV conduction abnormalities clinical history of autoimmune disease and plasma titres of maternal antibodies (anti Ro/SSA and antiLa/ SSB) should be performed. When neonates have abnormal AV nodal conduction without maternal antibodies, an ECG should also be performed on the parents and siblings (see intraventricular abnormalities). Neonates with first degree AV block should be followed with additional ECGs in the following months. Neonates and infants with second or third degree AV block need a complete paediatric cardiologic work-up, including an echocardiogram. The only effective treatment of congenital complete AV block in neonates with symptoms or a low ventricular escape rhythm is permanent artificial pacing. Intraventricular conduction Bundle branch block Congenital isolated complete right (RBBB) and left bundle branch block are very rare in neonates. Southall et al. found only one case of complete RBBB in a population of 3383 apparently healthy newborn infants[27]. The classical ECG in Ebstein’s anomaly of the tricuspid valve displays a prolonged PR interval and a wide RBBB. Left anterior fascicular block is found in association with congenital heart malformations such as atrio-ventricular canal defects and tricuspid atresia. In severe cardiomyopathy, interruption of the left bundle, which results from the involvement of the left ventricle and/or its conduction system, has been reported and carries a poor prognosis[28]. Eur Heart J, Vol. 23, issue 17, September 2002 Hereditary bundle branch block is an autosomal dominant genetic disease that was mapped in some families to the long arm of chromosome 19[29,30]. Affected individuals have various combinations of conduction defects such as RBBB, left or right QRS axis deviation or AV block; the r pattern may as well be the prelude to a conduction block. Abnormalities have been described in patients as young as 15 days. Non-specific intraventricular conduction abnormalities Non-specific intraventricular conduction abnormalities are very rare in neonates and infants with normal heart structures[31]. They may be a manifestation of inflammation in myocarditis or endocarditis. Work-up Neonates and infants with intraventricular conduction abnormalities need a complete paediatric cardiologic work-up. Evaluation of possible underlying causes should be performed. An ECG should also be performed on the parents and siblings. Wolff–Parkinson–White syndrome The anatomical substrate of preexcitation in Wolff– Parkinson–White (WPW) syndrome is a direct muscular connection between the atria and ventricles. Since accessory pathways rarely show decremental conduction, the electrical impulse is conducted prematurely to the ventricles resulting in a short PR interval. Conduction through the atrioventricular node and the accessory pathway results in collision of two electrical wavefronts at the ventricular level causing a delta wave and a fusion QRS complex with prolonged duration. The diagnosis of preexcitation is solely based on the findings of the surface ECG (Fig. 2). Intermittent preexcitation is not uncommon in newborns and infants. Depending on the location of the accessory pathway as well as the conduction properties of the atrioventricular node, even continuous preexcitation may be subtle and only detected in the mid-precordial leads. A study in newborns indicated a high prevalence of WPW syndrome when two of the four following characteristics were noted: PR interval c100 ms, QRS complex duration d80 ms, lack of a Q wave in V6 and left axis deviation[32]. Short PR intervals are also observed in mannosidosis, Fabry’s disease, and Pompe’s disease[5]. A common cause of a short PR interval in a normal heart is a low right atrial pacemaker. In this instance, the P wave is negative in lead aVF and positive or isoelectric in lead I. The intraatrial conduction time from the high to low right atrium is eliminated and therefore the PR interval may be up to 40 ms less than normal. The prevalence of WPW syndrome in the paediatric population has been estimated at 0·15 to 0·3%[33] with an incidence of newly diagnosed cases of approximately four per 100 000 persons per year for all age groups[34]. Numbers, however, vary greatly depending upon symptoms, age, gender and the intracardiac anatomy of the population studied[35,36]. In children with structural heart disease, the prevalence has been estimated at 0·33 to 0·5%[37]. Ebstein’s anomaly of the tricuspid valve, Figure 2 ECG in a neonate showing subtle signs of WPW. Note delta waves in V5 and V6 with absence of Q waves. Task Force Report 1337 Eur Heart J, Vol. 23, issue 17, September 2002 1338 Task Force Report l-transposition of the great arteries, hypertrophic cardiomyopathy and cardiac tumours are associated with an increased prevalence of preexcitation[36,37]. Clinical counterparts. In WPW syndrome the typical form of paroxysmal supraventricular tachycardia (orthodromic) results from reentry antegradely through the atrioventricular node and retrogradely through the accessory pathway. As digoxin shortens the antegrade effective refractory period of the accessory pathway and promotes rapid atrioventricular conduction during atrial flutter or atrial fibrillation over the pathway, the use of digoxin is contraindicated at any age [38,39]. Verapamil should also be avoided as it may increase the ventricular response rate during atrial fibrillation in those patients, and may cause cardiovascular collapse in infants and young children. The incidence of sudden death in preexcitation syndrome during childhood has been estimated to be as high as 0·5%[34] and cardiac arrest may be the initial presentation in children with preexcitation[35]. However, data on newborns and infants are lacking. One study on a series of 90 newborns and infants with WPW syndrome and supraventricular tachycardia reported sudden death in two patients with a normal heart during follow-up. Both infants, however, had been treated with digoxin[36]. Finally, there are no sufficient data on newborns and infants with an incidental finding of preexcitation on ECG concerning the occurrence of paroxysmal supraventricular tachycardia later on during their life. Work-up Congenital heart disease is more common in infants and young children with preexcitation, with a prevalence as high as 45% for infants with an ECG pattern consistent with a right-sided accessory pathway[36]. Thus, in every young patient with a preexcitation pattern on surface ECG, a complete 2-dimensional echocardiographic work-up is recommended to rule out any intracardiac abnormality. Assessment of the conduction properties of the accessory pathway, i.e. the antegrade effective refractory period and the shortest RR-interval with preexcitation, by transesophageal programmed stimulation may be useful in selected patients for risk stratification and mode of therapy. QRS axis and amplitude Abnormal axis implies a mean frontal plane QRS vector outside the normal range and must take into account the relative right axis deviation seen in normal neonates. Left axis deviation is seen in a variety of abnormalities including atrioventricular septal defect, ventricular septal defect, tricuspid atresia, and WPW syndrome, but may be occasionally observed in otherwise normal infants. Right ventricular hypertrophy Right ventricular hypertrophy may be suspected from a QR complex in V1, an upright T wave in V1 (normal in Eur Heart J, Vol. 23, issue 17, September 2002 the first week of life), increased R wave amplitude in V1, and increased S wave amplitude in V6 (according to the Davignon criteria). Sensitivity and specificity has not been tested in the neonate. QR patterns are commonly seen with pressure overload congenital lesions, rSR patterns are seen in volume overload lesions. Left ventricular hypertrophy The performance of the ECG in recognition of left ventricular hypertrophy is poorer than generally recognized and, again, has not been specifically tested in neonates. Left ventricular hypertrophy is expected to produce increased left sided voltages. Garson[5] described the most helpful ECG signs in children as being T wave abnormalities in leads V5 and V6, increased R wave amplitude in V6, increased S wave amplitude in V1 (according to the Davignon criteria), and a combination of these last two variables. Left to right shunt lesions may result in left ventricular hypertrophy, but this may be in association with right ventricular hypertrophy and manifested as biventricular hypertrophy. Left ventricular hypertrophy in the newborn may be attenuated by the normal right-sided predominance of the newborn. The normal premature heart may not have developed the right-sided predominance, especially if <28 weeks gestation, and left ventricular predominance may be present. Low QRS voltage In the limb leads the total amplitude of R+S in each lead c0·5 mV may be indicative of myocarditis or cardiomyopathy. Work-up Evaluation of the underlying causes should be performed. An echocardiogram should be performed when clinically indicated. Ventricular repolarization There is a simple reason that makes clinically important the analysis of ventricular repolarization abnormalities: their presence could be the harbinger of a significant risk for life-threatening arrhythmia. It is established that newborns found to have a prolonged QTc (>440 ms) on the fourth day of life have an increased risk for sudden death[1]. Some of these sudden deaths have previously been labelled as Sudden Infant Death Syndrome. On the other hand, the presence of confounding factors — above all the ambiguities in their quantification — calls for caution before making hasty diagnoses associated with need for therapy and with considerable parental anxiety. Ventricular repolarization can be evaluated on the surface ECG by measuring the QT interval duration and by analysing the morphology of the ST segment and of the T wave. Measurements of the QT interval should be performed by hand. It is important to remember that QT duration may change over time. Accordingly, it is recommended Task Force Report 1339 Figure 3 ECG tracings of three newborns with LQTS diagnosed in the first months of life. Mutations on the potassium channel gene KvLQT1 (panel A) and on the sodium channel gene SCN5A (panel B) were identified. Panel B modified from ref. [44]. repeating the ECG in those infants found to have a prolonged QTc on the first ECG. While exceptions do exist, the more prolonged the QTc interval, the greater the likelihood of its clinical significance. A QTc close to 500 ms implies a clear abnormality even taking into account potential measurement errors. QT interval prolongation: differential diagnosis Electrolyte disturbances are fairly common and may cause QT prolongation. Among them, hypocalcaemia (less than 7·5 mg . dl 1) usually produces a distinctive lengthening of the ST segment. Hypokalaemia and hypomagnesaemia, often encountered in infants who have had vomiting or diarrhoea, usually decrease T wave amplitude and increase U wave amplitude. Central nervous system abnormalities can produce QT prolongation and T wave inversion. Several drugs commonly used in the neonatal period and during infancy may induce QT interval prolongation; among them are macrolide antibiotics such as spyramycin[40], erythromycin, clarithromycin and also trimethoprim. Prokinetics such as cisapride have been positively linked to QT interval prolongation. All these drugs share one action: they block IKr, one of the ionic currents involved in the control of ventricular repolarization. Neonates born from mothers with autoimmune diseases and positive for the anti-Ro/SSA antibodies may also show QT interval prolongation, sometimes with QTc values exceeding 500 ms[41], which tends to be transient and to disappear by the sixth month of life, concomitantly with the disappearance of the anti Ro/ SSA antibodies. Finally, some of the neonates with QT interval prolongation may be affected by the congenital LQTS. This possibility has to be carefully evaluated because of its implications for management. Long QT syndrome Long QT syndrome, whose prevalence appears to be close to 1/3000–1/5000, is characterized by the occurrence of syncopal episodes due to torsades de pointes ventricular tachycardia (VT) and by a high risk for sudden cardiac death among untreated patients[42]. Importantly, in 12% of patients with LQTS, sudden death was the first manifestation of the disease and in 4% this happened in the first year of life[42]. This point alone mandates the treatment of all those diagnosed as affected, even if there are no symptoms. Long QT syndrome is a genetic disease due to mutations of several genes all encoding ionic (potassium or sodium) currents involved in the control of ventricular repolarization. In most cases, several members of the same family are gene-carriers. Low penetrance exists in LQTS, which means that gene-carriers may not show the clinical phenotype and may have a normal QT interval[43]. Therefore a normal QT in the parents does not rule out familial LQTS. In addition, approximately 30% of cases are due to ‘de novo’ mutations which imply unaffected parents and no family history. ‘De novo’ Eur Heart J, Vol. 23, issue 17, September 2002 1340 Task Force Report Figure 4 QT prolongation management flow chart. Electrolytes, echocardiogram, intracranial ultrasound are recommended in the appropriate clinical situation. In cases of positive genetics and QTc >440 ms, therapy is indicated. #In cases of a positive family history (Hx) for LQTS; *See text. LQTS mutations have been demonstrated in infant victims of cardiac arrest and sudden death diagnosed as Sudden Infant Death Syndrome[2,44,45]. Even though relatively few LQTS patients have cardiac events during the first year of life, the vast majority become symptomatic later on, either during childhood or adolescence according to genetic subgroups[46]. Therefore treatment must continue. Beta-blockers are the first choice therapy in LQTS and are effective in preventing recurrences in 80% of already symptomatic patients; different degrees of protection exist according to genetic subgroups[46]. If beta-blockers are unable to prevent new cardiac events, additional drug therapy, left cardiac sympathetic denervation, pacemakers or the implantable cardioverter defibrillator should be considered based on evidence, with due consideration for body size. ECG tracings of newborns with LQTS are shown in Fig. 3. Work-up It is well understood that the likelihood of having LQTS increases with increasing QTc; however, since a small percentage of LQTS patients has a QTc <440 ms[47], the correlation between QT prolongation and the presence of the syndrome is not absolute. Therefore, the following discussion is presented as guidelines based upon experience and current knowledge, and is likely to be updated frequently. Given the life-threatening potential of the disease, once the diagnosis of LQTS becomes probable, it is recommended that these infants are referred to a specialist as soon as possible. First ECG: QTc above 440 ms, the upper limit of normal. Exclude other causes of acquired QT interval prolongation and obtain a detailed family history for the possibility of familial LQTS. Episodes of early sudden death, fainting spells, and seizures-epilepsy should alert to this possibility. The ECG should be repeated after a few days to confirm the abnormal finding. Subsequent management depends on (1) presence or absence of family history suggestive for LQTS, and (2) the degree of QT interval prolongation. The presence of complex ventricular arrhythmias would Eur Heart J, Vol. 23, issue 17, September 2002 have additional importance. The following stepwise approach involves infants with and without a family history for LQTS (Fig. 4). If family history is positive, then — as LQTS is an autosomal dominant disease — the infant has a 50% probability of being affected and complete diagnostic procedures should be performed, as always with LQTS families. The second ECG is normal. If the first QTc was <470 ms, dismiss the case. If the first QTc was d470 ms, then plan a third ECG after 1–2 months to remain on the safe side. The second ECG shows a QTc between 440 and 470 ms. In these cases with persistent borderline QT prolongation, electrolytes, including calcium and magnesium, should be checked. Clinical history of autoimmune disease and plasma titres of maternal antibodies (anti Ro/SSA and antiLa) should be performed. T wave morphology may be helpful; for example, the presence of notches on the T wave in the precordial leads further suggests the presence of LQTS[48]. Additionally, mild bradycardia can also be found in LQTS. ECGs should be obtained from the parents and siblings of the neonate. In the absence of family history of LQTS, symptoms or arrhythmias, a 24-h Holter monitoring should be obtained to look for T wave alternans, complex ventricular arrhythmias or marked QTc prolongation, and the ECG should be periodically checked during the first year. No treatment is currently recommended. With a positive family history, the probability of LQTS becomes high. Additional diagnostic procedures (24-h Holter monitoring, echocardiogram and genetic screening) should be performed and initiation of therapy could be considered. The second ECG shows a QTc d470 and <500 ms. All diagnostic procedures listed above should be performed and a third ECG should be planned within a month. In case of a positive family history, therapy should be initiated. Even without a family history, therapy should be considered. Even in infants with a very prolonged QTc in the first month of life, the ECG may normalize. If subsequent Task Force Report 1341 Figure 5 ECG tracings of a newborn with blocked atrial bigeminy which simulates sinus bradycardia. Blocked P waves are present when examining the T waves. ECGs and diagnostic procedures do not confirm the presence of LQTS, it is logical to progressively withdraw therapy and to return to periodic observations. The second ECG shows a QTc d500 ms. Infants with a QTc d500 ms are very likely to be affected by LQTS and to become symptomatic. All diagnostic procedures listed above should be performed and these infants should be treated. Highest risk. The presence of QTc close to 600 ms, or of T wave alternans, or of 2:1 AV block secondary to major QT prolongation, or of hearing loss, identify infants at extremely high risk[47,49]. ST segment elevation Causes. There are multiple causes of ST segment elevation in infancy. The most frequent is pericarditis. Less frequent causes of ST segment elevation with or without T wave abnormalities are hyperkalaemia, intracranial haemorrhage, pneumothorax and pneumopericardium, subepicardial injury due to anomalous left coronary artery or to Kawasaki disease with cardiac involvement. Whenever an anomalous left coronary artery or, more frequently, Kawasaki disease produce an acute myocardial infarction, QT prolongation may also be present. ST segment elevation with a RBBB pattern in the right precordial leads (V1–V2) is the typical finding of the Brugada syndrome, a genetic disorder associated with a high incidence of sudden cardiac death secondary to ventricular fibrillation, in the absence of cardiac structural abnormalities[50]. The ST segment elevation is typically downsloping or ‘coved’ and it is followed by a negative T wave, at variance with the early repolariz- ation syndrome where ST segment elevation has an upward concavity, it is confined to mid-precordial leads and is associated with a positive T wave. The diagnosis of the Brugada syndrome is made difficult by the intermittent nature of the ECG abnormalities, as 40% of cases may normalize transiently. Rare cases of Brugada syndrome have been reported during infancy[51,52]. Work-up Whenever the underlying cause has been identified, it should be treated. If the Brugada syndrome is suspected, careful family history should be collected, 24-h Holter monitoring obtained, and the patient should be referred to a specialist. Atrial and ventricular arrhythmias Atrial/junctional Premature atrial beats. A premature atrial beat is a premature P wave. Premature atrial beats usually have a different morphology and mean vector from sinus P waves. In regular sinus rhythm at a normal rate, a P wave that occurs before the next expected P wave is a premature atrial beat. A premature atrial beat may be conducted to the ventricles normally, or with ventricular aberration or not conducted or ‘blocked’. Occasionally, blocked premature atrial beats occur in a bigeminal sequence, so-called ‘blocked atrial bigeminy’. This rhythm simulates sinus bradycardia; it is important to examine the T waves carefully for blocked P waves (Fig. 5). In infants, since the refractory periods of the bundle branches are similar, premature atrial beats may be conducted with either RBBB or left bundle branch Eur Heart J, Vol. 23, issue 17, September 2002 1342 Task Force Report Table 2 Distinguishing tachyarrhythmias in infants Sinus tachycardia SVT Atrial flutter VT History Sepsis, fever, hypovolaemia, etc. Usually otherwise normal Most have a normal heart Many with abnormal heart Rate Almost always <230 b/min Most often 260–300 b/ min Atrial 300–500 b/min. Vent. 1:1 to 4:1 conduction 200–500 b/min R-R interval variation Over several seconds may get faster and slower After first 10–20 beats, extremely regular May have variable block (1:1, 2:1, 3:1) giving different ventricular rates Slight variation over several beats P wave axis Same as sinus almost always visible P waves 60% visible P waves, P waves do not look like sinus P waves Flutter waves (best seen in LII, LIII, aVF, V1) May have sinus P waves continuing unrelated to VT (AV dissociation), retrograde P waves, or no visible P waves QRS Almost always same as slower sinus rhythm After first 10–20 beats, almost always same as sinus Usually same as sinus, may have occasional beats different from sinus Different from sinus (not necessarily ‘wide’) SVT=Supraventricular tachycardia. VT=ventricular tachycardia. aberration. It is relatively common in the same strip to see premature atrial beats conducted normally, aberrantly and blocked. It is relatively uncommon for an infant to have both premature atrial beats and premature ventricular beats, although it does occur. Therefore, in an infant with premature P waves and wide QRS complexes on the same strip, a careful search should be made for a premature P wave preceding a wide QRS, before making the diagnosis of both premature atrial beats and premature ventricular beats on the same strip. Work-up In patients with frequent premature atrial beats, a follow-up ECG at 1 month may be performed. Relatively long periods of blocked atrial bigeminy may simulate sinus bradycardia. The distinction is important since blocked atrial bigeminy is most often benign while severe sinus bradycardia may accompany systemic illness. Supraventricular tachycardia. Supraventricular tachycardia (SVT) is a rapid regular tachyarrhythmia, which results from an abnormal mechanism originating proximal to the bifurcation of the bundle of His and does not have the morphology of atrial flutter. This definition of SVT specifically excludes sinus tachycardia (Table 2) and premature wide QRS. The usual infant with SVT has an extremely regular R-R interval after the first 10–20 beats, most often at rates greater than 230 beats . min 1 and usually 260–300 per min. In 60% of cases, the P waves are visible, but the P waves almost always have a different morphology from sinus. In over 90% of infants and children with SVT, the QRS complex is narrow and in only 3% is the QRS complex different from the underlying sinus QRS. Therefore, the persistent aberration of SVT in infants is exceedingly rare, implying that in the majority of infants with a QRS complex different from sinus, the diagnosis is VT. In very rare Eur Heart J, Vol. 23, issue 17, September 2002 cases of SVT in infants, there may be atrial tachycardia with AV block or junctional tachycardia with AV dissociation. Work-up It is important to document SVT with a 12-lead ECG before attempting conversion of the rhythm unless the infant is critically ill. After sinus rhythm is achieved, the WPW pattern should be sought on a 12-lead ECG. Treatment to prevent further episodes of SVT in infancy is generally recommended. An echocardiogram is indicated to determine ventricular function or the presence of congenital heart disease. Atrial flutter. Atrial flutter is characterized by a rapid, regular form of atrial depolarization: the ‘flutter wave’. The picket fence morphology is similar to adults. However, the flutter wave durations are generally 0·09 to 0·18 s with atrial rates in infants between 300–500 beats . min 1. In general, there is variable AV conduction from 1:1 to 4:1 yielding an irregular ventricular rate. The QRS complex is usually the same as in sinus rhythm although there may be occasional aberrancy (Table 2). Due to the occasional association with WPW, this pattern should be specifically sought. Other types of supraventricular arrhythmias such as atrial fibrillation or multifocal tachycardia are extremely rare in the neonate. Work-up Conversion to sinus rhythm should be attempted. An echocardiogram is worthwhile to determine ventricular function and the possible presence of congenital heart disease. Ventricular arrhythmias Premature ventricular beats. A premature ventricular beat is manifest on the surface ECG as a premature abnormal QRS (not similar to the sinus QRS complex) that is not preceded by a premature P wave. It is Task Force Report important to recognize that in infants, the QRS duration may be normal — or slightly prolonged (i.e. less than 0·08 s) — but if the complex has a different morphology from the sinus, and is not preceded by a premature P wave, the diagnosis is a premature ventricular beat. The relationship between morphology and the site of origin is not exact enough to be able to predict which ventricle is causing the arrhythmia. It is not possible to distinguish premature ventricular beats from premature atrial beats with aberrancy on the basis of QRS morphology. Work-up The QT interval should be measured carefully during periods of sinus rhythm (see section on repolarization abnormalities). In complex ventricular arrhythmias, 24-h Holter monitoring may be worthwhile. An echocardiogram may be performed to determine ventricular function or structural abnormalities. Occasionally maternal drugs that cause ventricular arrhythmias may be transferred in utero or post-natally in breast milk. Ventricular tachycardia. Ventricular tachycardia is a series of three or more repetitive complexes that originate from the ventricles. The complexes are therefore different from the patient’s normal QRS; usually, the QRS duration is prolonged for the age of the patient (0·09 s or more in infants). It is therefore usually a ‘wide QRS’ tachycardia. However, infants may have a QRS duration in VT less than 0·09 s but clearly different from the sinus complex (Table 2). The specific morphology of the QRS is generally not helpful to distinguish VT from supraventricular tachycardia with aberration. However, SVT in infants with a different QRS beyond the first 10–20 beats is rare, therefore, in this situation, a diagnosis of VT should be strongly considered. In infants, the rate of VT may be from 200–500 beats . min 1. There may be a slight variation in the R-R interval over several beats. There may be sinus P waves continuing unrelated to VT (AV dissociation), retrograde P waves or no visible P waves. There may also be fusion and capture beats. The diagnosis of VT should be strongly considered if the patient has premature ventricular beats during times of sinus rhythm with a similar morphology to the tachyarrhythmia. Work-up An underlying cardiac or central nervous system abnormality may be found in infants with VT. The QT interval should be carefully measured (see section on repolarization abnormalities), 24-h Holter monitoring and echocardiogram should be obtained. Treatment is generally indicated. Accelerated ventricular rhythm. Accelerated ventricular rhythm is also known as ‘slow VT’ — generally the rate is <200 beats . min 1. It occurs at approximately the same rate as the infant’s sinus rate, and the rhythms tend to alternate. Work-up While these infants most often have a normal heart, a work-up similar to VT is indicated. 1343 Conclusion The main objective of the present document was to provide cardiologists, who work with adults, with a practical approach to neonatal electrocardiography, and paediatricians and neonatologists with a tool that should facilitate medical interaction on cardiologic issues. There are important differences between neonatal and adult ECGs. When a cardiologist examines the ECG of an apparently normal and healthy infant the focus has to be on distinguishing between patterns that should cause no alarm and those that require action or additional investigations. To provide clues for this distinction is what the members of the Task Force have attempted to do and, whenever possible or appropriate, steps in management have also been suggested. This document is not intended to be all-inclusive or to substitute for textbooks on paediatric and neonatal ECG. The manuscript has been reviewed by the Members of the CPGPC: Werner Klein (Chair), Maria Angeles Alonso, Gianfranco Mazzotta, Carina Blomström Lundqvist. The authors are grateful to Pinuccia De Tomasi, BS, for expert editorial support in the preparation of the manuscript. References [1] Schwartz PJ, Stramba-Badiale M, Segantini A et al. Prolongation of the QT interval and the sudden infant death syndrome. N Engl J Med 1998; 338: 1709–14. [2] Schwartz PJ, Priori SG, Bloise R et al. Molecular diagnosis in a child with sudden infant death syndrome. Lancet 2001; 358: 1342–3. [3] Davignon A, Rautaharju P, Boisselle E, Soumis F, Megelas M, Choquette A. Normal ECG standards for infants and children. Pediatr Cardiol 1979; 1: 123–52. [4] Rijnbeek PR, Witsenburg M, Schrama E, Hess J, Kors JA. New normal limits for the paediatric electrocardiogram. Eur Heart J 2001; 22: 702–11. [5] Garson A Jr. Electrocardiography. In: Garson A Jr, Bricker JT, Fisher DJ, Neish SR, eds. The Science and Practice of Paediatric Cardiology, 2nd edn. Baltimore, MD: Williams & Wilkins, 1998: 713–88. [6] Tippel M. Interpretation of electrocardiograms in infants and children. Images Paediatr Cardiol 1999; 1: 3–13 available at: http://www.health.gov.mt/impaedcard/issue/issue1/ecg1/ ect1.htm#top [7] Garson A Jr. Clinically significant differences between the ‘old’ analog and the ‘new’ digital electrocardiograms. Am Heart J 1987; 114 (1 Pt 1): 194–7. [8] Rijnbeek PR, Kors JA, Witsenburg M. Minimum bandwidth requirements for recording of paediatric electrocardiograms. Circulation 2001; 104: 3087–90. [9] Yamamoto H, Miyahara H, Domae A. Is a higher sampling rate desirable in the computer processing of the paediatric electrocardiogram? J Electrocardiol 1987; 20: 321–8. [10] Macfarlane PW, Coleman EN, Pomphrey EO, McLaughlin S, Houston A, Aitchison T. Normal limits of the high-fidelity paediatric ECG. Preliminary observations. J Electrocardiol 1989; 22 (Suppl): 162–8. [11] Bailey JJ, Berson AS, Garson A Jr et al. Recommendations for standardization and specifications in automated electrocardiography: bandwidth and digital signal processing. A report for health professionals by an ad hoc writing group of the Committee on Electrocardiography and Cardiac Electrophysiology of the Council on Clinical Cardiology, American Heart Association. Circulation 1990; 81: 730–9. Eur Heart J, Vol. 23, issue 17, September 2002 1344 Task Force Report [12] Stramba-Badiale M, Lazzarotti M, Schwartz PJ. Development of cardiac innervation, ventricular fibrillation, and sudden infant death syndrome. Am J Physiol 1992; 263: H1514–22. [13] Thomaidis C, Varlamis G, Karamperis S. Comparative study of the electrocardiograms of healthy fullterm and premature newborns. Acta Paediatr Scand 1988; 77: 653–7. [14] Stramba-Badiale M, Spagnolo D, Bosi G, Schwartz PJ. Are gender differences in QTc present at birth? MISNES Investigators. Multicenter Italian Study on Neonatal Electrocardiography and Sudden Infant Death Syndrome. Am J Cardiol 1995; 75: 1277–8. [15] Schwartz PJ, Montemerlo M, Facchini M et al. The QT interval throughout the first 6 months of life: a prospective study. Circulation 1982; 66: 496–501. [16] Vincent GM. Heart rate of Romano–Ward syndrome patients. Am Heart J 1986; 112: 61–4. [17] Hofbeck M, Ulmer H, Beinder E, Sieber E, Singer H. Prenatal findings in patients with prolonged QT interval in the neonatal period. Heart 1997; 77: 198–204. [18] Ho SY, Fagg N, Anderson RH, Cook A, Allan L. Disposition of the atrioventricular conduction tissues in the heart with isomerism of the atrial appendages: its relation to congenital complete heart block. J Am Coll Cardiol 1992; 20: 904–10. [19] Brucato A, Frassi M, Franceschini F et al. Risk of congenital complete heart block in newborns of mothers with anti-Ro/ SSA antibodies detected by counterimmunoelectrophoresis: a prospective study of 100 women. Arthritis Rheum 2001; 44: 1832–5. [20] Buyon JP, Hiebert R, Copel J et al. Autoimmune-associated congenital heart block: long-term outcome of children and immunogenetic study. J Am Coll Cardiol 1998; 31: 1658–66. [21] Geggel RL, Tucker L, Szer I. Postnatal progression from second to third degree heart block in neonatal lupus syndrome. J Pediatr 1988; 113: 1049–52. [22] Trippel DL, Parsons MK, Gillette PC. Infants with long-QT syndrome and 2:1 atrio-ventricular block. Am Heart J 1995; 130: 1130–4. [23] Gorgels APM, Al Fadley F, Zaman L, Kantoch MJ, Al Halees Z. The long QT syndrome with impaired atrioventricular conduction: a malignant variant in infants. J Cardiovasc Electrophysiol 1998; 9: 1225–32. [24] Van Hare GF, Franz MR, Roge C, Scheinman MM. Persistent functional atrio-ventricular block in two patients with prolonged QT intervals: elucidation of the mechanism of block. PACE 1990; 13: 608–18. [25] Lupoglazoff JM, Cheav T, Baroudi G et al. Homozygous SCN5A mutation in long QT syndrome with functional two-to-one atrioventricular block. Circ Res 2001; 89: e16–e21. [26] Villain E, Kachaner J, Le Bidois J et al. Bloc auricoloventriculaire partiel et allongement de QT chez quatre prématurés recevant du diphémanil. Arch Fr Pediatr 1990; 47: 33–5. [27] Southall DP, Johnson AM, Shinebourne EA, Johnston PG, Vulliamy DG. Frequency and outcome of disorders of cardiac rhythm and conduction in a population of newborn infants. Paediatrics 1981; 68: 58–66. [28] Gnota JF, Samson RA. Left bundle branch block in infants with dilated cardiomyopathy conveys a poor prognosis. Cardiol Young 1999; 9: 55–7. [29] Stephan E, de Meeus A, Bouvagnet P. Hereditary bundle branch defect: right bundle branch blocks of different causes have different morphologic characteristics. Am Heart J 1997; 133: 249–56. [30] Brink PA, Ferreira A, Moolman JC, Weymar HW, van der Merwe PL, Corfield VA. Gene for progressive familial heart block type I maps to chromosome 19q13. Circulation 1995; 91: 1633–40. [31] Ewing LL. Intraventricular conduction disturbances in children. Prog Pediatr Cardiol 1994; 4: 11–19. [32] Perry JC, Giuffre RM, Garson A. Clues to the electrocardiographic diagnosis of subtle Wolff–Parkinson–White syndrome. J Pediatr 1990; 117: 871–5. Eur Heart J, Vol. 23, issue 17, September 2002 [33] Sorbo MD, Buja GF, Miorelli M et al. The prevalence of the Wolff–Parkinson–White syndrome in a population of 116 542 young males. G Ital Cardiol 1995; 25: 681–7. [34] Munger TM, Packer DL, Hammill SC et al. A population study of the natural history of Wolff–Parkinson–White syndrome in Olomsted County, Minnesota, 1953–1989. Circulation 1993; 87: 866–73. [35] Paul T, Guccione P, Garson A Jr. Relation of syncope in young patients with Wolff–Parkinson–White syndrome to rapid ventricular response during atrial fibrillation. Am J Cardiol 1990; 65: 318–21. [36] Deal BJ, Keane JF, Gillette PC, Garson A. Wolff–Parkinson– White syndrome and supraventricular tachycardia during infancy: management and follow-up. J Am Coll Cardiol 1985; 5: 130–5. [37] Perry JC, Garson A. Supraventricular tachycardia due to Wolff–Parkinson–White syndrome in children: early disappearance and late recurrence. J Am Coll Cardiol 1990; 16: 1215–20. [38] Saul JP, Walsh EP, Triedman JK. Mechanisms and therapy of complex arrhythmias in paediatric patients. J Cardiovasc Electrophysiol 1995; 6: 1129–48. [39] Villain E, Bonnet D, Acar P, Aggoun Y, Sidi D, Kachaner J. Recommendations for the treatment of recurrent supraventricular tachycardia in infants. Arch Pediatr 1998; 5: 133–8. [40] Stramba-Badiale M, Nador F, Porta N et al. QT interval prolongation and risk of life-threatening arrhythmias during toxoplasmosis prophylaxis with spiramycin in neonates. Am Heart J 1997; 133: 108–11. [41] Cimaz R, Stramba-Badiale M, Brucato A, Catelli L, Panzeri P, Meroni PL. QT interval prolongation in asymptomatic anti-SSA/Ro-positive infants without congenital heart block. Arthritis Rheum 2000; 43: 1049–53. [42] Schwartz PJ, Priori SG, Napolitano C. The long QT syndrome. In: Zipes DP, Jalife J, eds. Cardiac electrophysiology: from cell to bedside, 3rd edn. Philadelphia: WB Saunders, 2000: 597–615. [43] Priori SG, Napolitano C, Schwartz PJ. Low penetrance in the long QT syndrome. Clinical impact. Circulation 1999; 99: 529–33. [44] Schwartz PJ, Priori SG, Dumaine R et al. A molecular link between the sudden infant death syndrome and the long-QT syndrome. N Engl J Med 2000; 343: 262–7. [45] Ackerman MJ, Siu BL, Sturner WQ et al. Postmortem molecular analysis of SCN5A defects in sudden infant death syndrome. JAMA 2001; 286: 2264–9. [46] Schwartz PJ, Priori SG, Spazzolini C et al. Genotypephenotype correlation in the long-QT syndrome: gene-specific triggers for life threatening arrhythmias. Circulation 2001; 103: 89–95. [47] Garson A Jr, Dick M 2nd, Fournier A et al. The long QT syndrome in children. An international study of 287 patients. Circulation 1993; 87: 1866–72. [48] Malfatto G, Beria G, Sala S, Bonazzi O, Schwartz PJ. Quantitative analysis of T wave abnormalities and their prognostic implications in the idiopathic long QT syndrome. J Am Coll Cardiol 1994; 23: 296–301. [49] Villain E, Levy M, Kachaner J, Garson A Jr. Prolonged QT interval in neonates: benign, transient, or prolonged risk of sudden death. Am Heart J 1992; 124: 194–7. [50] Brugada J, Brugada R, Brugada P. Right bundle branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation 1998; 97: 457–60. [51] Priori SG, Napolitano C, Giordano U, Collisani G, Memmi M. Brugada syndrome and sudden cardiac death in children. Lancet 2000; 355: 808–9. [52] Suzuki H, Torigoe K, Numata O, Yazaki S. Infant case with a malignant form of Brugada Syndrome. J Cardiovasc Electrophysiol 2000; 11: 1277–80.