837 Professional Health Care Claim
advertisement

Companion
Document
837P
837 Professional Health Care Claim
Basic Instructions
This section provides information to help you prepare for the ANSI ASC X12N 837 Health Care
transaction for professional claims. The remaining sections of this appendix include tables that
provide information about 837 Claim segments and data elements that require specific instructions
to efficiently process through Anthem Blue Cross and Blue Shield, Connecticut, Maine, and New
Hampshire (East Region) systems.
Use this companion document in conjunction with both the Transaction Set Implementation Guide
“Health Care Claim: Professional, 837, ASC X12N 837 (004010X098),” May 2000, and the subsequent
Addenda (004010X098A1), October 2002, published by the Washington Publishing Co.
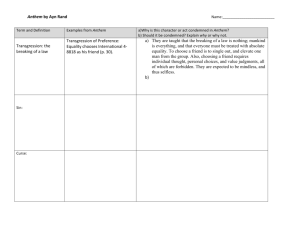
EDI Transmission Structure
Communications Transport Protocol
Interchange Control Header (ISA)
Functional Group Header (GS)
Transaction Set
Transaction Set
Functional Group 1 Wrap
Transaction Set Header (ST)
Transaction Set Header (ST)
Detail Segment 1
Transaction Set Trailer (SE)
EDI Transaction Structure
Interchange Control Header (ISA)
Detail Segment 2
Functional Group Header (GS)
Transaction Set Trailer (SE)
Transaction Set Header (ST)
Header
Envelope
Transaction Set Header (ST)
Envelope
Transaction Set
Transaction Set Header (ST)
Transaction Set
Functional Group Header (GS)
Envelope
Functional Group Trailer (GE)
Functional Group 2 Wrap
Interchange Control Wrap
Communications Session
Functional Group Header (GS)
Detail
Summary
Detail Segment 1
Transaction Set Trailer (SE)
Transaction Set Trailer (SE)
Functional Group Trailer (GE)
I t
h
C
t
lT
il
(IEA)
Detail Segment 2
Transaction Set Trailer (SE)
Functional Group Trailer (GE)
Interchange Control Trailer (IEA)
Communications Transport Protocol
Anthem Blue Cross and Blue Shield - East Region
Page 1 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
1
X12 and HIPAA Compliance Checking, and Business Edits
Level 1. The East Region returns a 997 Functional Acknowledgment to the submitter for
every inbound 837 transaction received. Each transaction passes through edits to ensure that
it is X12 compliant. If the X12 syntax or any other aspect of the 837 is not X12 compliant,
the 997 Functional Acknowledgment will also report the Level 1 errors in AK segments and
indicate that the entire transaction set has been rejected.
Level 2. HIPAA Implementation Guide edits are strictly enforced. In addition, the East
Region applies business edits, such as provider and member number validation to each 837
transaction. If a HIPAA compliance, code set or business error is encountered, a Level 2
Status Report will be returned to the submitter indicating the particular claim has failed.
2
HIPAA Compliant Codes
Follow the 837 Professional IG precisely. Use HIPAA-Compliant codes from current versions
of the sources listed in the 837 Professional IG, Appendix C: External Code Sources.
3
Uppercase Letters
All alpha characters must be submitted in UPPERCASE letters only.
4
Diagnosis Codes
According to the 837 Professional IG (P.254), a transaction is not X12 compliant if decimal
points are used in diagnosis codes – Loop 2300 HI Health Care Diagnosis Code. Therefore,
should a diagnosis code contain a decimal point, the East Region will return a 997 Functional
Acknowledgment to the submitter indicating that the transaction has been rejected.
5
Delimiters
The East Region accepts any of the standard delimiters as defined by the ANSI standards.
The more commonly used delimiters include the following:
Data Element Separator, Asterisk, (*)
Sub-Element Separator, Colon, (:)
Segment Terminator, Tilde (~)
These delimiters are for illustration purposes only and are not specific recommendations or
requirements.
Anthem Blue Cross and Blue Shield - East Region
Page 2 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
6
Numeric Values, Monetary Amounts and Unit Amounts
East Region adjudication systems support numeric values that are consistent with
the current NSF Version 3.01. Values which require a field length greater than those
specified by NSF Version 3.01 will not pass our business rule edits.
The East Region pays all claims in US dollars and, therefore, accepts monetary amounts
in US dollars only. If codes related to foreign currencies are used, then a Level 2 Status
Report will be returned to the submitter and the claim will be rejected.
The East Region recognizes unit amounts in whole numbers only.
The East Region recognizes unit amounts in values of less than 9999 and greater than
or equal to zero.
If
negative values are submitted in any of the two data elements in Loop 2400 SV1
Professional Service (See 837P IG, P.383), then the East Region will return a Level 2
Status Report to the submitter and reject the claim.
SV102 Monetary Amount – Line Item Charge Amount
SV104 Quantity – Service Unit Count
7
Coordination of Benefits
Specific 837 data elements work together to coordinate benefits between the East Region
and Medicare or other carriers. The tables in the section that follow (Loop 2320), identify
the data elements that pertain to Coordination of Benefits (COB) with Medicare (Providerto-Payer-to-Payer COB model) and with other carriers (Payer-to-Provider-to-Payer COB
model).
The East Region recognizes submission of an 837 transaction to a sequential payer populated
with data from the previous payer’s 835 (Health Care Claim Payment/Advice). Based on the
information provided and the level of policy, the claim will be adjudicated without the paper
copy of the Explanation of Benefits from Medicare or the primary carrier.
When more than one payer is involved on a claim, payer sequencing is as follows:
If a secondary payer is indicated, then all the data elements from the primary payer must also
be present.
If a tertiary payer is involved, then all the data elements from the primary and secondary
payers must also be present.
If these data elements are omitted, the East Region will fail the particular claim.
Anthem Blue Cross and Blue Shield - East Region
Page 3 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
8
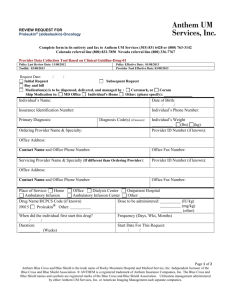
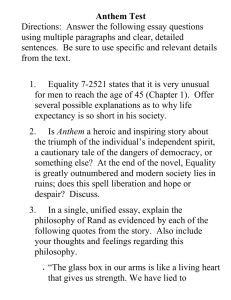
Sending Attachments to Support a Claim
To expedite processing of a claim:
If you are sending an attachment to support a claim, populate Loop 2300 PWK02 with a value
of ‘BM’ (By Mail).
Download the Attachment Face Sheet from www.anthem.com/edi
Mail the attachment to the appropriate address listed at the bottom of the Attachment Face
Sheet on the same day the claim is submitted.
Do not send a copy of the claim with the attachment.
Send the completed Attachment Face Sheet with the attachment.
The Attachment Face Sheet includes the
following fields:
Anthem East
(CT, ME, NH)
Attachment Face Sheet
Claim Supplemental Information
PWK; Loop 2300 Original Service Line Number
PWK; Loop 2400 Line Supplemental Information
1)
Date Claim Transmitted
2)
Line of Business
(Professional, Institutional)
3)
Member’s Contract Number
(Including Prefix)
Member’s Contract Number
(Prefix Included)
4)
Patient Name
Name of Patient
5)
Date of Service
6)
Provider Name
State Services were
Rendered In
7)
State Where Services Were Rendered
Identification Code
(Attachment Control #)
8)
Identification Code. This is the
Attachment Control Number, an
alphanumeric code created by the
provider for his records.
The paper documentation included in this mailing supports the electronically submitted claim.
Date Claim Transmitted
Line of Business
ð Professional
ð Institutional
Date of Service
Name of Provider
(If the correspondence is not received in 7 calendar days and is necessary to adjudicate the claim, Anthem will fail the
claim. After 7 calendar days, the claim will be reviewed on an inquiry basis only.)
Anthem BCBS
Professional
PO Box 533
North Haven, CT
06473
Anthem BCBS
Institutional
PO Box 537
North Haven, CT
06473
BlueCare Family
Plan (CT only)
Professional
PO Box 1076
North Haven, CT
06473
P00292
FEP Claims CT
PO Box 37790
Louisville, KY
40233-7790
BlueCare Family
Plan (CT only)
Institutional
PO Box 1077
North Haven, CT
06473
FEP Claims ME
PO BX 37980
Louisville, KY
40233-7980
National Claims
PO Box 726
North Haven, CT
06473
FEP Claims NH
PO Box 36500
Louisville, KY
40233-6500
Teamster’s Claims
PO Box 726
North Haven, CT
06473
An independent licensee of the Blue Cross and Blue Shield Association.
â Registered marks of the Blue Cross and Blue Shield Association.
Anthem Blue Cross and Blue Shield - East Region
Page 4 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
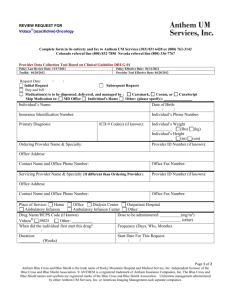
Claim Supplement
Information
Claim File
received
with PWK
segment
populated
Professional Health Care Claim
Attachment to Support a Claim
Attachment Face
Sheet
By Mail
June
15
June
16
June
17
June
18
June
19
June
20
June
21
June
22
All documentation must be received within 7 calendar days of the electronic submission.
If supporting documentation is not received but is required to process the claim, the East
Region will deny the claim.
For example (as shown above):
On June 15, a claim is received with the PWK segment populated.
On June 22, the 7 day time period expires. The claim will be denied if the attachment has not
been received and is required for adjudication.
9
Taxonomy Codes (PRV)
The Healthcare Provider Taxonomy code set divides health care providers into hierarchical
groupings by type, classification, and specialization, and assigns a code to each grouping.
The Taxonomy consists of two parts: individuals (e.g., physicians) and non-individuals (e.g.,
ambulatory health care facilities). All codes are alphanumeric and are 10 positions in length.
These codes are not “assigned” to health care providers; rather, health care providers select the
taxonomy code(s) that most closely represents their education, license, or certification. If a health
care provider has more than one taxonomy code associated with it, a health plan may prefer
that the health care provider use one over another when submitting claims for certain services.
It is strongly recommended that the taxonomy be populated in PRV segments for all
applicable claims that you are filing. Refer to the CMS website for a listing of codes,
www.wpc-edi.com/taxonomy.
Anthem Blue Cross and Blue Shield - East Region
Page 5 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Claim Header
The 837 Claim Header identifies the start of a transaction, the specific transaction set, and
its business purpose. Also, when a transaction set uses a hierarchical data structure, a data
element in the header, BHT01 (Hierarchical Structure Code) relates the type of business data
expected within each level. The following table indicates the specific values of the required
header segments and data elements for East Region processing.
837 Professional Health Care Claim—Header
IG
Segment
Reference
Designator(s)
ST Transaction Set Header
P.61 ST
ST01
Transaction Set Transaction Set
Header
Identifier Code
ST02
Transaction Set
Control Number
Beginning of Hierarchical Transaction
P.62 BHT
BHT06
Beginning of
Transaction Type
Hierarchical
Code
Transaction
Loop ID 1000B—Receiver Name
P.72 NM1
NM103
Receiver Name Last Name or
Organization Name
NM109
Identification Code
Anthem Blue Cross and Blue Shield - East Region
Value
Definitions and Notes
Specific to East Region
837
837 - Health Care Claim
(Identical to
SE02)
Unique number assigned by the sender and
generated by the sender's system.
CH
All submissions recognized as chargeable.
ANTHEM BLUE
CROSS AND
BLUE SHIELD
00060
00680
00770
Receiver Name
00060 - Connecticut
00680 - Maine
00770 - New Hampshire
Page 6 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Claim Detail
The 837 Detail level has a hierarchical level (HL) structure based on the participants involved
in the transaction. The three levels for the participant levels include:
1
1)
Information Source (Billing/Pay-to Provider)
2)
Subscriber (Can be the Patient when the Patient is the Subscriber)
3)
Dependent (Patient when the Patient is not the Subscriber)
837 Claim Detail: Billing/Pay-to Provider Hierarchical Level
The first hierarchical level (HL) of the 837 Claim Detail, Billing/Pay-to Provider HL, identifies
the original entity who submitted the electronic claim to the destination payer.
837 Professional Health Care Claim—Detail
Billing/Pay-to Provider Hierarchical Level
IG
Segment
Reference
Value
Designator(s)
Loop ID 2000A—Billing/Pay-to Provider Hierarchical Level
P.76 PRV
PRV01
BI
Provider Code
Billing/Pay-to
Provider
(Provider
PRV03
Specialty
Reference
Taxonomy Code)
Information
Identification
P.78
Definitions and Notes
Specific to East Region
BI - Billing
When using NPI, enter the taxonomy code that
applies to the service on the claim that you are
filing (NOTE to Clearinghouses - DO NOT
DEFAULT).
USD - US Dollars
CUR02
USD
CUR
Currency Code
Foreign
Monetary amounts recognized in US dollars
Currency
only.
Information
Loop ID 2010AA—Billing Provider Name
XX - National Provider Identifier
P.81 NM1
NM108
XX
24 - Employer's Identification Number
Billing Provider ID Code Qualifier 24
34 - Social Security Number
Name
34
• NPI ('XX') for Non-Exempt providers
NM109
(Billing Provider
• Tax ID ('24') and SSN ('34') for Exempt
Identification
Primary ID No.)
providers
Code
P.84 N3
For correct claim adjudication, Anthem requests the address of
N301, 302
Billing Provider Address
the physical location at which services were rendered , not
Information
Address
from where the services were billed.
P.87 REF
1B - Blue Shield Provider Number
REF01
1B
EI - Employer's Identification Number
Billing Provider Reference ID
EI
SY - Social Security Number
Secondary
Qualifier
SY
Identification
• Provider's Tax ID ('EI')
REF02
(Billing Provider
• Provider's Social Security No. ('SY')
Reference
Additional
• Assigned Provider No. ('1B') - for Exempt
Identification
Identifier)
Providers
Anthem Blue Cross and Blue Shield - East Region
Page 7 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
2
837 Claim Detail Subscriber Hierarchical Level
The second hierarchical level (HL) of the 837 Detail is the Subscriber HL. It is strongly
recommended that each interchange (ISA-IEA envelope) be limited to 3000 claims for
processing efficiency.
837 Professional Health Care Claim—Detail
Subscriber Hierarchical Level
IG
Segment
Reference
Value
Designator(s)
Loop ID 2000B—Subscriber Hierarchical Level
P.105 SBR
SBR01
P, S, T
Subscriber Payer
Information Responsibility
Sequence
Number Code
SBR09
BL
Claim Filing
MC
Indicator Code
Definitions and Notes
Specific to East Region
Usage of 'S' or 'T' must be accompanied by information
populated in Loop 2320.
BL - BlueCross/ Blue Shield
MC - Medicaid (BlueCare Family Plan)
If value BL or MC is not used, a Level 2 Status Report will
be returned to the submitter.
Loop ID 2010BA—Subscriber Name
P.112 NM1
Applies to:
Format Explanation
NM109
Enter one of the
Subscriber Identification
following formats:
Name
Code
***ALL ALPHA CHARACTERS MUST BE IN UPPERCASE LETTERS.
J (uppercase) followed by 9-position
BlueCare
(J099999990)
numeric subscriber ID code.
Family Plan e.g. J123456789
R (uppercase) followed by 8-position
FEP
(R99999999)
numeric subscriber ID code.
e.g. R12345678
Enter the ID Number exactly as it appears on the front
All other
of the ID card, including ANY PREFIX.
products
3-character alpha prefix (uppercase)
(XXX999999)
followed by 6-position numeric
e.g. PTH123456
subscriber ID code.
3-character alpha prefix (uppercase)
(XXX9999999)
followed by 7-position numeric
e.g. TSJ1234567
subscriber ID code.
3-character alpha prefix (uppercase)
(XXX99999999)
e.g. PTH12345678 followed by 8-position numeric
subscriber ID code.
3-character alpha prefix (uppercase)
(XXX999999999)
e.g. YTA123456789 followed by 9-position numeric
subscriber ID code.
3-character alpha prefix (uppercase)
(XXX9999999999)
e.g. OCI1234567899 followed by 10-position numeric
subscriber ID code.
(XXX99999999999) 3-character alpha prefix (uppercase)
followed by 11-position numeric
e.g.
subscriber ID code.
YGC12345678901
3-character alpha prefix (uppercase)
(XXX9999X99999)
followed by 4-position numeric, 1e.g.
character alpha, and 5-position
XVG0000A11111
numeric subscriber ID code.
Anthem Blue Cross and Blue Shield - East Region
Page 8 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
3
837 Claim Detail Patient Hierarchical Level
The third hierarchical level (HL) of the 837 Claim Detail is the Patient HL. It is strongly
recommended that each interchange (ISA-IEA envelope) be limited to 3000 claims for
processing efficiency. Enveloping
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference
Designator(s)
Loop ID 2010CA—Patient Name
P.154 DMG
DMG02
Patient
Date Time
Demographic Period
Information
Loop ID 2300—Claim Information
P.160 CLM
CLM01
Claim
Claim
Information
Submitter's
Identifier
CLM02
Monetary
Amount
CLM05-3
Claim
Frequency Type
Code
CLM08
Yes/No
Condition or
Response Code
P.199 PWK
PWK02
Claim
Report
Supplemental Transmission
Information
Code
PWK05
ID Code
Qualifier
PWK06
Identification
Code
P.205 AMT
Patient
Amount
Paid
AMT01
Amount
Qualifier Code
AMT02
Monetary
Amount
P.216 REF
REF02
Reference
Original
Reference No. Identification
(ICN/DCN)
Anthem Blue Cross and Blue Shield - East Region
Value
Definitions and Notes
Specific to East Region
(Patient Birth
Date)
When the patient's date of birth falls after the
patient's date of service (Loop 2400, DTP03), a
Level 2 Status Report will be returned to the
submitter.
(Patient Account
Number)
ƒ Represents the Patient Control No. returned on
the 835.
ƒ Do not use special characters as part of value.
(Total Claim
Charge Amount)
Value must equal the total amount of submitted
charges for service lines in Loop 2400, SV102.
7, 8
'7' - Replacement (Replacement of Prior Claim)
'8' - Void (Void/Cancel of Prior Claim)
(Benefits
Assignment
Indicator)
BM
For National Accounts, an "N" value indicates
benefits have not been assigned to the provider.
Claim payment is sent to the member and not the
provider.
ƒ Supporting documentation and Attachment Face
Sheet accepted by mail (BM) only within 7
calendar days of the electronic transmission
otherwise the claim will be denied.
ƒ Illegible information will delay processing.
AC
AC - Attachment Control Number
(Attachment
Control Number)
ƒ Self-assigned number, max. 10 alphanumeric
characters on the Attachment Face Sheet.
ƒ Digits drawn from the left to match the
Attachment with the appropriate electronically
submitted claim.
F5 - Patient Amount Paid
F5
(Patient Amount
Paid)
Represents the Patient Amount Paid.
(Claim Original
Reference
Number)
• Must be submitted for frequency codes of '7'
(replacement), '8' (void) in CLM05-3.
• Represents the Original Claim Reference No.
returned on electronic and paper remittances.
Page 9 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference
Value
Designator(s)
Loop ID 2300—Claim Information (cont'd)
P.228 REF
REF02
(Medical Record
Medical
Reference
Number)
Record No. Identification
HI01-2
HI05-2 (Diagnosis Code)
P.254 HI
HI06-2
Health Care HI02-2
HI03-2
HI07-2
Diagnosis
HI04-2
HI08-2
Code
Definitions and Notes
Specific to East Region
ƒ Represents the Medical Record No. returned on
the 835.
ƒ Do not use special characters as part of value.
Blue Shield claims are adjudicated based only on
the primary diagnosis.
Industry Code
Loop ID 2310A—Referring Provider Name
Referring Provider recognized 1) at the claim level and 2) for managed care only.
XX - National Provider Identifier
P.271 NM1
NM103, (NM104) (Referring
24 - Employer's Identification Number
Referring
Last (First) Name Provider Last
34 - Social Security Number
Provider
or Organization (First) Name)
Name
Name
NM108
XX
ID Code Qualifier 24
34
• NPI ('XX') for Non-Exempt providers
NM109
(Referring
Identification
Provider Primary • Tax ID ('24') and SSN ('34') for Exempt providers
Code
Identifier)
P.276 REF
1B - Blue Shield Provider Number
REF01
1B
1G - Provider UPIN Number
Referring
Reference ID
1G
EI - Employer's Identification Number
Qualifier
Provider
EI
SY - Social Security Number
Secondary
SY
Identification REF02
• Provider's Tax ID ('EI')
(Referring
• Provider's Social Security No. ('SY')
Reference
Provider
• Assigned Provider No. ('1B') and UPIN ('1G') - for
Identification
Secondary ID)
Exempt Providers
Loop ID 2310B—Rendering Provider Name
Rendering Provider recognized at the claim level only.
XX - National Provider Identifier
P.278 NM1
NM108
XX
24 - Employer's Identification Number
Rendering
ID Code Qualifier 24
34 - Social Security Number
Provider
34
• NPI ('XX') for Non-Exempt providers
NM109
(Rendering
Name
• Tax ID ('24') and SSN ('34') for Exempt providers
Identification
Provider
Code
Identifier)
P.283 REF
1B - Blue Shield Provider Number
REF01
1B
EI - Employer's Identification Number
Rendering
Reference ID
EI
SY - Social Security Number
Provider
Qualifier
SY
Secondary
• Provider's Tax ID ('EI')
REF02
(Rendering
Identification Reference
• Provider's Social Security No. ('SY')
Provider
• Assigned Provider No. ('1B') - for Exempt
Identification
Secondary
Providers
Identifier)
Anthem Blue Cross and Blue Shield - East Region
Page 10 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference
Value
Designator(s)
Loop ID 2310D—Service Facility Location
P.290 NM1
NM101
FA
Service
Entity Identifier Code
Facility
NM108
XX
Location
ID Code Qualifier
24
34
NM109
(Lab/ Facility
Identication Code
Primary ID)
Definitions and Notes
Specific to East Region
FA - Facility
XX - National Provider Identifier
24 - Employer's Identification Number
34 - Social Security Number
• NPI ('XX') for Non-Exempt providers
• Tax ID ('24') and SSN ('34') for Exempt providers
P.296 REF
1A - Blue Cross Provider Number
REF01
1A
TJ - Tax ID
Service
Reference ID Qualifier TJ
• Provider's Tax ID ('TJ')
Facility
REF02
(Laboratory
• Assigned Provider No. ('1A') - for Exempt
Location
Reference
or Facility
Providers
Secondary
Identification
Secondary
Identification
Identifier)
Loop ID 2320—Other Subscriber Information
When East Region is secondary , following data elements required for Coordination of Benefits (COB):
P.303 SBR
• Use of ‘S’ requires that primary payer information
SBR01
P
be present in Loop 2320.
Other
Payer Responsibility S
• Use of ‘T’ requires that both primary and
Subscriber
Sequence Number
T
secondary payer information be present in Loop
Information
Code
2320.
P.308 CAS
Populate CAS segment with quantity, monetary amounts, and appropriate
Claim Level adjustment reason codes 1 = deductible, 2 = coinsurance, 3 = copayment.
Adjustments CAS02,5,8,11,14,17 (Adjustment Identifies the reason for claim being adjusted.
Claim Adjustment
Reason
CAS03,6,9,12,15,18 (Adjustment Represents the amount being adjusted.
Monetary Amount
Amount)
CAS04,7,10,13,16,19 (Adjustment Represents the units of service being adjusted.
Quantity
Quantity)
P.317 AMT
COB Payer Paid Amount must be populated for COB claims.
D - Payor Amount Paid
COB Payer AMT01
D
Paid Amount Amount Qualifier Code
Represents the Payer Paid Amount
(Payer Paid
AMT02
Monetary Amount
Amount)
AAE - Approved Amount
P.318 AMT
AAE
AMT01
COB
Amount Qualifier Code
Approved
Represents the Approved Amount
AMT02
(Approved
Amount
Monetary Amount
Amount)
P.319 AMT
COB Allowed Amount must be populated for COB claims.
B6 - Allowed-Actual
COB Allowed AMT01
B6
Amount
Amount Qualifier Code
Represents the Allowed Amount
AMT02
(Allowed
Monetary Amount
Amount)
Anthem Blue Cross and Blue Shield - East Region
Page 11 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference Designator(s)
Value
Definitions and Notes
Specific to East Region
Loop ID 2320—Other Subscriber Information (cont'd)
When East Region is secondary , following data elements required for Coordination of Benefits (COB):
F2 - Patient Responsibility - Actual
P.320 AMT
F2
AMT01
COB Patient
Amount Qualifier Code
Responsibility AMT02
Represents the Other Payer
(Other Payer Patient
Patient Responsibility Amount.
Amount
Monetary Amount
Responsibility
Amount)
P.321 AMT
AU - Coverage Amount
AMT01
AU
COB Covered Amount Qualifier Code
Amount
(Other Payer Covered Represents the Other Payer
AMT02
Covered Amount.
Monetary Amount
Amount)
P.322 AMT
D8 - Discount Amount
AMT01
D8
COB Discount Amount Qualifier Code
Amount
(Other Payer Discount Represents the Other Payer
AMT02
Discount Amount.
Monetary Amount
Amount)
P.323 AMT
DY - Per Day Limit
AMT01
DY
COB Per Day
Amount Qualifier Code
Represents the Other Payer Per
Limit Amount
(Other Payer Per Day
AMT02
Day Limit Amount.
Monetary Amount
Limit Amount)
P.324 AMT
F5 - Patient Amount Paid
AMT01
F5
COB Patient
Amount Qualifier Code
Represents the Other Payer
Paid Amount
(Approved Amount)
AMT02
Patient Paid Amount.
Monetary Amount
P.325 AMT
T - Tax
AMT01
T
COB Tax
Amount Qualifier Code
Amount
Represents the Other Payer Tax
(Other Payer Tax
AMT02
Amount.
Monetary Amount
Amount)
P.326 AMT
T2 - Total Claim Before Taxes
AMT01
T2
COB Total
Amount Qualifier Code
Represents the Other Payer PreClaim Before
AMT02
(Other Payer Pre-Tax
Taxes Amount Monetary Amount
Tax Claim Total Amount.
Claim Total Amount)
P.332 MOA
MOA01
(Reimbursement Rate) Represents the Outpatient
reimbursement rate, expressed as
Medicare
Percent
a decimal.
Outpatient
Adjudication
Information
Loop ID 2330B—Other Payer Name
P.349 DTP
Represents when the primary
DTP03
(Adjudication or
payer made payment and is
Claim
Date Time Period
Payment Date)
recognized for processing
Adjudication
Coordination of Benefits.
Date
Anthem Blue Cross and Blue Shield - East Region
Page 12 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference
Value
Definitions and Notes
Designator(s)
Specific to East Region
Loop ID 2400—Service Line
P.381 LX
LX01
Accept up to 50 service lines per claim.
Service Line Assigned
Number
P.383 SV1
When billing unlisted HCPCS (NOC codes), include the
SV101-2
(Procedure
drug and dosage at the service line in Loop 2400 NTE02
Professional Procedure Code Code)
(Description). Report the corresponding NDC# in Loop
Service
2410 LIN03.
ƒ Maximum of 4 procedure modifiers accepted.
SV101-3ʊ6
(Procedure
Procedure
Modifier 1-4) ƒ A value of ‘99’ is defined as “multiple modifiers”.
Modifier
ƒ Sum of service line charges must equal the Total Claim
SV102
(Line Item
Charge Amount in Loop 2300 CLM02.
Monetary
Charge
ƒ Value cannot be less than zero, or greater than
Amount
Amount)
$999,999.99.
ƒ Accept values greater than or equal to zero, and up to
SV103
MJ
9999.
Unit or
UN
ƒ Report anesthesia time in units ('UN').
Measurement
Code
(Service Unit Accept values greater than or equal to zero, and up to
SV104
9999.
Quantity
Count)
SV105
(Place of
For HMO/PPO claims, values for 1) assistant surgery, 2)
Facility Code
skilled nursing facility and 3) cardiac rehabilitation place
Service
Value
of services accompanies facility code values (Loop
Code)
2310D, Service Facility Location).
41, 42
P.391 SV5
Durable
Medical
Equipment
Service
P.416 DTP
Date Service Date
SV505
Monetary
Amount
(DME
Purchase
Price)
Ambulance services using values ’41’ and ‘42’ is
submitted with a SV101-3 value greater than zero.
Anthem defines the DME Purchase Price as the
Manufacturer's Suggested Retail Price which does not
include shipping/handling or tax.
A Level 2 Status Report will be returned to the submitter
if value is: 1) prior to the patient’s Date of Birth (Loop
2010CA, DMG02) or 2) "From Date" precedes the "To
Date."
East Region accepts procedure text at the line level only.
When billing unlisted HCPCS (NOC codes) in Loop 2400
P.467 NTE
NTE02
(Line Note
SV101-2 (Procedure Code), include the drug and
Line Note
Description
Text)
dosage.
DTP03
Date Time
Period
(Service
Date)
For Medicare Private Fee for Service claims, submit the
dates when the provider assumed/relinquished patient
to/from post-operative care.
Loop ID 2410—Drug Identification
P.459 LIN
(National
LIN03
Drug
Product/Service Drug Code)
Identification ID
Anthem Blue Cross and Blue Shield - East Region
NDC# (without hyphens) corresponds to unlisted
HCPCS (NOC codes) in Loop 2400 SV101-2, and the
drug and dosage in Loop 2400 NTE02. Example: NDC#
12345-6789-10 is recognized as 12345678910.
Page 13 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Professional Health Care Claim—Detail
Patient Hierarchical Level
IG
Segment
Reference
Designator(s)
Loop ID 2420E—Ordering Provider Name
P.513 NM1
NM103, (NM104)
Ordering
Last (First) Name or
Provider
Organization Name
Name
NM108
ID Code Qualifier
Value
(Ordering
Provider Last
(First) Name)
XX
24
34
NM109
(Order Provider
Identification Code
Primary Identifier)
P.519 REF
REF01
1B
Ordering
Reference ID Qualifier EI
Provider
SY
Secondary
REF02
(Ordering
Identification Reference
Provider
Identification
Secondary ID)
Definitions and Notes
Specific to East Region
The First and Last Name, or Organization
Name of the Ordering Provider for radiology
services is recognized.
XX - National Provider Identifier
24 - Employer's Identification Number
34 - Social Security Number
• NPI ('XX') for Non-Exempt providers
• Tax ID ('24') and SSN ('34') for Exempt
1B - Blue Shield Provider Number
EI - Employer's Identification Number
SY - Social Security Number
• Provider's Tax ID ('EI')
• Provider's Social Security No. ('SY')
• Assigned Provider No. ('1B') - for Exempt
Providers
Loop ID 2430—Line Adjudication Information
P.536 SVD
SVD segment must be populated for COB claims.
Matches Loop 2330B NM109 identifying
Service Line SVD01
(Other Payer ID
Other Payer.
Adjudication Identification Code
Code)
(Service Line Paid Represents paid amount by the primary
SVD02
payer.
Monetary Amount
Amount)
HC - HCPCS Code
HC
SVD03-1
IV - HIEC Product/Service Code
Product/Service ID
IV
ZZ - Mutually Defined
Qualifier
ZZ
SVD03-2
(Procedure Code) Represents procedure code.
Product/Service ID
Represents procedure modifier, if applicable.
SVD03-3, -4, -5, -6
(Procedure
Product/Service ID
Modifier)
Qualifier
(Paid Service Unit Represents paid units of service by the
SVD05
primary payer.
Quantity
Count)
P.540 CAS
When Loop 2430 SVD02 service line amount differs from Loop 2400 SV102 total
Line
charge amount, the CAS segment must be populated with quantity, monetary
Adjustment
amounts, and appropriate adjustment reason codes.
Identifies the reason for claim being adjusted.
CAS02,5,8,11,14,17 (Adjustment
Claim Adjustment
Reason Code)
Reason Code
Represents the amount being adjusted.
CAS03,6,9,12,15,18 (Adjustment
Monetary Amount
Amount)
Represents the units of service being
CAS04,7,10,13,16,19 (Adjustment
adjusted.
Quantity
Quantity)
P.548 DTP
Line
Adjudication
Date
DTP03
Date Time Period
Anthem Blue Cross and Blue Shield - East Region
(Adjudication or
Payment Date)
Represents when the primary payer made
payment and is recognized for processing
Coordination of Benefits.
Page 14 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
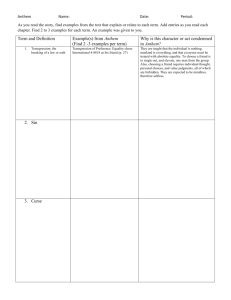
Enveloping
EDI envelopes control and track communications between you and Anthem. One envelope
may contain many transaction sets grouped into functional groups. The envelope consists of
the following:
Interchange Control Header (ISA)
Functional Group Header (GS)
Functional Group Trailer (GE)
Interchange Control Trailer (IEA)
837 EDI Transaction Structure
Interchange Control Header (ISA)
Functional Group Header (GS)
Envelope
Envelope
Envelope
Transaction Set Header (ST)
Header
Detail
Transaction Set Trailer (SE)
Functional Group Trailer (GE)
Interchange Control Trailer (IEA)
Anthem Blue Cross and Blue Shield - East Region
Page 15 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
837 Envelope Control Segments – Inbound
1
837 Health Care Claim Interchange Control Header (ISA)
The ISA segment is the beginning, outermost envelope of the interchange control structure.
Containing authorization and security information, it clearly identifies the sender, receiver, date,
time, and interchange control number. Anthem requests all data in the ISA-IEA segment to be
entered in UPPER CASE.
837 Professional Health Care Claim
Interchange Control Header (ISA)
Segment
ISA
Interchange
Control
Header
Reference
Designator(s)
Value
ISA01
00
Auth Info Qualifier
ISA02
(10 Spaces)
Authorization Info
ISA03
00
Security Info Qualifier
ISA04
Security Information
ISA05
Interchange ID
Qualifier
ISA06
Interchange Sender
ID
ISA07
Interchange ID
Qualifier
ISA08
Interchange Rec ID
ISA09
Interchange Date
ISA10
Interchange Time
ISA11
Interchange Control
Standards Identifier
ISA12
Interchange Control
Version Number
ISA13
Interchange Cntrl No.
00 - No Authorization Information Present
Enter 10 positions.
00 - No Security Information Present
(10 Spaces)
Enter 10 positions.
ZZ
ZZ - Mutually Defined
(Submitter ID)
ƒ Format - Fixed length of 15 positions, alphanumeric.
ƒ Left-justified followed by spaces.
ƒ Identical to GS02.
ZZ - Mutually Defined
ZZ
(YYMMDD)
ƒ ANTHEM - Anthem Plans
ƒ Left-justified followed by spaces.
Value must be a valid date in YYMMDD format.
(HHMM)
Value must be a valid time in HHMM format.
U
U - U.S. EDI Community of ASC X12, TDCC, and UCS
00401
00401 - Draft Standards for Trial Used Approved for
Publication by ASC X12 Procedures Review Board
through October 1997
ƒ Format - Fixed length 9 positions, numeric.
ƒ Unique value greater than zero and not used in any
HIPAA transmission within last 365 calendar days.
ƒ Right-justified, filled with leading zeroes.
ƒ Identical to IEA02.
0 - No Acknowledgment Requested
1 - Interchange Acknowledgment Requested
Submitter ID must be approved to submit production
data (P - Production Data; T - Test Data).
ƒ X - 1 character contained in Basic or Extended
Character set.
ƒ Value must not equal A-Z, a-z, 0-9, "space", and
special characters which may appear in text data (i.e.,
hyphen, comma, period, apostrophe).
ANTHEM
(Assigned by
Sender)
ISA14
0, 1
Ack Requested
ISA15
P, T
Usage Indicator
ISA16
(X)
Component Element
Separator
Anthem Blue Cross and Blue Shield - East Region
Definitions and Notes
Specific to Anthem
Page 16 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
2
837 Health Care Claim Functional Group Header (GS)
The GS segment identifies the collection of transaction sets that are included within the functional
group. More specifically, the GS segment identifies the functional control group, sender, receiver,
date, time, group control number and version/release/industry code for the transaction sets.
Anthem requests that all data in the GS-GE segment be entered in UPPERCASE.
837 Professional Health Care Claim
Functional Group Header (GS)
Segment
GS
Functional
Group
Header
Reference
Designator(s)
GS01
Functional Identifier
Code
GS02
Application
Sender's Code
GS03
Application
Receiver's Code
GS04
Date
GS05
Time
GS06
Group Control
Number
Value
Definitions and Notes
Specific to Anthem
HC
HC - Health Care Claim (837)
(Submitter ID)
ANTHEMCT
ANTHEMME
ANTHEMNH
20012
(CCYYMMDD)
ƒ Format - 2-15 positions, alphanumeric.
ƒ Left-justified with no trailing zeroes or spaces.
ƒ Identical to ISA06.
Routing of batched transactions to:
ANTHEMCT - CT BCBS Plan
ANTHEMME - ME BCBS Plan
ANTHEMNH - NH BCBS Plan
20012 - Machigonne Benefits
Value must be a valid date in CCYYMMDD format.
(HHMM)
Value must be a valid time in HHMM format.
(Assigned by
Sender)
ƒ Format - 1-9 positions, numeric.
ƒ Unique value greater than zero and not used in any
HIPAA transmission within last 365 calendar days.
ƒ Left-justified with no trailing zeroes or spaces.
ƒ Identical to GE02.
X - Accredited Standards Committee X12
X
GS07
Responsible
Agency Code
GS08
Version / Release / 004010X098A1
Industry Identifier
Code
Operationally used to identify the transaction:
004010X098A1 - 837 Professional Claim
NOTE. Critical Batching and Editing Information.
**Transactions must be batched in separate functional group by Application Receiver’s Code (GS03).
***Group Control Number (GS06) may not be duplicated by submitter. Files containing duplicate or
previously received group control numbers will be rejected.
Anthem Blue Cross and Blue Shield - East Region
Page 17 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002
837P Health Care Claim Companion Document
3
837 Health Care Claim Functional Group Trailer (GE)
The GE segment indicates the end of the functional group and provides control information.
837 Professional Health Care Claim
Functional Group Trailer (GE)
Segment
GE
Functional
Group
Trailer
4
Reference
Designator(s)
GE01
Number of
Transaction Sets
Included
GE02
Group Control
Number
Value
(Total Number of
Transaction Sets in
Functional Group or
Transmission)
(Control Number)
Definitions and Notes
Specific to Anthem
ƒ Format - 1-6 positions, numeric.
ƒ Left-justified with no trailing zeroes or spaces.
ƒ Format - 1-9 positions, numeric.
ƒ Left-justified with no trailing zeroes or spaces.
ƒ Identical to GS06.
837 Health Care Claim Interchange Control Trailer (IEA)
The IEA segment is the ending, outermost level of the interchange control structure. It indicates
and verifies the number of functional groups included within the interchange and the interchange
control number (the same number indicated in the ISA segment).
837 Professional Health Care Claim
Interchange Control Trailer (IEA)
Segment
IEA
Interchange
Control
Trailer
Reference
Designator(s)
IEA01
Number of Included
Functional Groups
IEA02
Interchange Control
Number
Anthem Blue Cross and Blue Shield - East Region
Value
(Number of Functional
Groups GS/GE Pairs in
Interchange)
(Control Number)
Definitions and Notes
Specific to Anthem
ƒ Format - 1-5 positions, numeric.
ƒ Left-justified with no trailing zeroes or spaces.
ƒ Format - Fixed length 9 positions, numeric.
ƒ Unique value greater than zero.
ƒ Identical to ISA13.
Page 18 of 18
Release 23 (February 2011)
Version 004010A1 - Oct 2002