Veterinary CPR Update: RECOVER Guidelines & BLS
advertisement

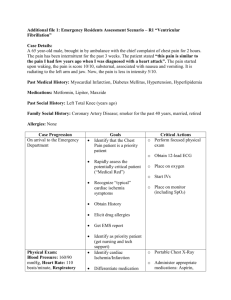
2/3/2014 CPR Update RECOVER REassessment Campaign On VEterinary Resuscitation. CPR Update RECOVER • Series of 7 articles in Journal of Veterinary Emergency and Critical Care • • evaluate the scientific evidence relevant to small animal CPR compose consensus-based clinical CPR guidelines for dogs and cats GOALS CPR Update RECOVER – 7 Parts 1 ABOUT “RECOVER” – Materials & Methods 2 Domain 1 - PREPAREDNESS AND PREVENTION 3 Domain 2 - BASIC LIFE SUPPORT (BLS) 4 Domain 3 - ADVANCED LIFE SUPPORT (ALS) 5 Domain 4 - MONITORING 6 Domain 5 - POST ARREST CARE 7 CPR GUIDELINES – All 5 domains Part 1 RECOVER Materials & Methods CPR Update RECOVER • Systematic evaluation of 74 questions having to do with small animal CPR • Generated 101 CPR Guidelines • Completed by more than 80 specialists in academia (48%) and private practice (52%) – mostly Anesthesia and Critical Care • Modeled after International Liaison Committee On Resuscitation (ILCOR) – evidence analysis for in human CPR since 1992 • Endorsed by ACVECC and VECCS • Many knowledge gaps identified – may guide research • Will reconvene every 5 years RECOVER Introduction CPA = Cardiopulmonary Arrest CPR = Cardiopulmonary Resuscitation PCA = Post Cardiac Arrest PICO = Population-Intervention-Comparison-Outcome (Q format) •<6% of dogs and cats that experience CPA in the hospital survive to discharge. •20% of people who suffer in-hospital CPA are discharged •CPA outcomes could be considerably improved in veterinary patients •Current veterinary CPR recommendations have been derived from guidelines for humans •Disagreement about how to best perform CPR even among boarded emergency and critical care veterinary specialists 1 2/3/2014 PrePre-Stocked Arrest Areas Crash Carts • • • Domain 1 Preparedness and Prevention – – – – Preparedness Prevention Crash Carts Retrospective study on cardiac arrest in human hospital: – Delay in CPR due to equipment failure 18% of the time – 9% of carts had significant deficiencies • Inaccessible location • Infrequent assessment of cart content • Too much variation in carts when there are more than one • • What is the crash cart deficiency rate in vet medicine? SOLUTIONS: – Checklists and dated log sheet for restocking – Regular re-training of staff – Cognitive Aids improve outcome • flow charts • check lists • Dose charts or calculators Arrest Etiology & Outcome • • • • anesthesia-related CPAs are associated with increased survival compared to anesthesiaarrests from other causes. Survival rate of dogs and cats for CPA is between 4 and 9.6% Survival rate in human hospitals for CPA is 10-20% Veterinary studies – – – – 36-55% of CPAs occurring under anesthesia survive to discharge 0-3% of other CPAs survive to discharge Survive to discharge is much more important than successful CPA resuscitation Drug reactions resulting in CPA also have a relatively favorable outcome Preparedness Prevention Arrest Etiology & Outcome • Human studies – operating room CPAs – Death rate 34.9-65.5% for all etiologies – Death rate 5.5% for anesthesia related CPAs – Human error is noted in 91% of anesthesia related deaths • missing equipment due to lack of return to the cart incomplete stocking Inability to identify or locate needed medications Failure to have drugs and syringes in a quick, usable form – Deficiencies and defects in resuscitation equipment PrePre-Stocked Arrest Areas • use of both pre-stocked arrest stations and cognitive aids improves compliance with CPR protocols 80% of GPs and 98% of specialists in VECC & anesthesia have a regularly maintained crash cart Most problematic are: Post resuscitation debriefing soon after the episode detects and corrects human error. Preparedness & Prevention CPR Training • • • • • CPR skills begin to decay within weeks of training, no matter the learning method used By 1-2 years after training, skills return to re-training level Annual CPR training is crucial Semi-annual CPR training is even better. American Hospital Association (AHA) – Cognitive performance • completing steps of CPR in an orderly and rapid fashion – Psychomotor skills for BLS • Proper hand position, adequate rate and depth, adequate recoil for chest compressions • Minimizing interruptions • Avoiding excessive ventilation in rate and volume 2 2/3/2014 Preparedness Prevention Preparedness Prevention CPR Team Leadership • • • • • • Presence of physician at human CPR does not necessarily improve outcome Some studies show improved outcome, some no difference and a few worse outcome when a doctor is present for CPR The flaw might be in assuming that physicians are actually more experienced (skilled) than nurses or paramedics at CPR Survival rates not affected by experience of the first responder No veterinary studies comparing outcomes of vets vs. techs for CPR CPR Leadership Training definitely improves outcome of human CPR CPR Team Leadership • • • • Rapid intervention of the first responder and application of ALS is crucial to improving survival for human CPR Leadership instruction coordinates the group CPR effort Technical instruction teaches the mechanics of CPR CPR Leadership Training improves: – – – – – – Time to initiate CPR Percentage of defibrillation within the recommended time window “hands on time” maximizing CPR time during the emergency Chest compression rate Improves cognitive skills Does not necessarily improve all psychomotor skills Preparedness Prevention CPR Team Leadership • • • Preparedness & Prevention Team Size • – 1 kennel attendant or tech to ventilate – 1 kennel attendant or tech to do chest compressions – 1 technician to be directed by the leader – intubate, establish IV line, help with cut downs, get supplies and special need items, clean up, etc. – Leader keeps the records and coordinates, doesn’t do anything that takes more than a few seconds – Clear the room of other people, leave the door open, and have others stand by if needed CPR Leaders are more effective if they do not participate in the resuscitation CPA simulation is the ideal tool for teaching CPR Leadership High fidelity manikins with immediate feedback are the best equipment for teaching CPR Leadership skills Preparedness Prevention Standardized Training • • • • • Many studies show improved outcome in CPA after standardized training for BLS and/or ALS are implemented Not widely available in Veterinary Medicine Case based learning tends to be more effective than text-book training alone TAMU does provide a first responder paramedical course for veterinary professionals and staff CPR Guidelines put forth by VECC July 2012 Veterinary CPR – Leader (vet or tech) plus three Preparedness & Prevention Debriefing • • • • • When high fidelity immediate feedback manikins are not available, post episode debriefing is the next best thing for learning psychomotor skills Debrief after each real time CPR Drill, debrief, drill, debrief, drill, debrief significant improvement in survival in human pediatric patients (33– 50%) over time with the use of mock codes and debriefing integrated into a resident teaching program Patient survival in simulations increased from 0% to 89% during a retraining for ALS certified health care workers, using mock codes and debriefing 3 2/3/2014 Preparedness Prevention Preparedness & Prevention Debriefing • • Debriefing is more effective in learning CPR than any other teaching modality used alone Debriefing can take many forms: – – – – Verbal debriefing Audio-visual playback and discussion Review of immediate feedback devices that can record Computer interactive audio-visual learning modules Post--Training Assessment Post • • A test at the end of the CPR training session improves learning retention weeks to months later Reviewing test results can be a learning tool as well. CPR Update RECOVER Preparedness & Prevention Conclusions • In light of the higher survival in dogs and cats following CPA while under anesthesia, consideration should be given to placement of arrest and algorithms in areas where animals are routinely anesthetized – anesthesia induction/prep areas – Surgical suites – Anesthetic recovery areas • At our HQHVSN Clinic, we have 2 surgery tables and one prep table – – – – – One table is always open That table is the arrest station Crash box is mobile Emergency drugs are the only drugs not kept in the lock box Anesthetic arrests most often occur during recovery Key Preparedness and Prevention recommendations for canine and feline CPR • Organized, pre-stocked arrest stations • improve performance • Located where animals are routinely anesthetized • Post-CPR debriefing improves future performance. • Standardized training programs should be developed. • have improved adherence to guidelines in human medicine • are needed in veterinary medicine. • High fidelity manikins are effective in human medicine. • Leadership and team communication training increase effectiveness. Basic Life Support ABC • Establish airway • Ventilation (breathing) Domain 2 BLS – Basic Life Support – 8-10 breaths per minute if intubated – Up to 20 mm H20 on the manometer – C:V ratio of 30:2 if not intubated (compression:ventilation ratio) • Chest compressions (circulation) – – – – 100 per minute or faster 1/3 to ½ the width of the chest Full recoil between compressions (press hard and fast) Minimize interruptions (no more than 1 every 2 minutes) 4 2/3/2014 Basic Life Support Basic Life Support ABC Training • Numerous studies have shown that the quality of BLS performed is associated with return of spontaneous circulation (ROSC) and survival in arrest victims. • Minimal equipment • Can be started immediately at onset of CPA • Every staff member should be trained in BLS 1. 2. 3. 4. Rapid recognition of CPA Rapid initiation of CPR Immediate chest compressions Begin intubation and ventilation simultaneously – At least chest compressions and breathing – All may not be able to intubate Basic Life Support Basic Life Support Training Training Rapid recognition of CPA • Incidence of CPA during anesthesia – 1. 2. 3. 4. ECG Confirms lack of effective circulation 0.17% in dogs, 0.24% in cats Patient is unresponsive Absence of breathing (agonal does not count) Absence of palpable pulses or auscultable heart sounds ECG confirms lack of effective circulation • • • • Asystole Pulseless ventricular tachycardia Other pulseless electrical activity Ventricular fibrillation If in doubt, do chest compressions • • <2% adverse effects when done when not in CPA Rib fracture, tracheal bleeding, soreness Basic Life Support Basic Life Support Training Training Rapid initiation of CPR Ventilation 1. One person is the CPR Leader & record keeper 2. One person does chest compressions unless directed to stop by the Leader 3. One person establishes the airway and ventilates unless directed to stop by the leader 4. One person begins ALS, attaches monitors and carries out other tasks as instructed by the CPR Leader • • • Hypoxia and hypercapnea reduce likelihood or ROSC Establishing oxygenation may prevent respiratory arrest from progressing to cardiac arrest When intubation is not available, rescue breathing 30:2 V:C is indicated – – – – – • Mouth to snout AmbuBag and snug fitting anesthetic mask Or anesthetic mask attached to oxygen tank MAKE SURE VAPORIZER IS OFF Watch for gastric distension and relieve with manual pressure Take the manometer to 20 cm H20 5 2/3/2014 Basic Life Support Basic Life Support Training Training Ventilation – Ambu Bags Ventilation – Ambu Bags Basic Life Support Basic Life Support Training Training Ventilation – Ambu Bags Ventilation – Masks Basic Life Support Basic Life Support Training Training Ventilation – Choosing Reservoir Bag Size (6xTV) Ventilation – Choosing ET Tube Size (handout) 6 2/3/2014 Basic Life Support Basic Life Support Training Training Ventilation – Tips for endotracheal intubation Ventilation – Tips for endotracheal intubation • • • • Visualize the arytenoid cartilages • • • • Visualize the arytenoid cartilages If you didn’t see it go in, assume it’s not in Use polypropylene catheter stylet for cats (biggest that moves freely in the ET tube – 5Fr, 8Fr, 10Fr) Use the biggest tube that passes without too much resistance Fill the cuff, but do not overfill it Tie the tube in place Set oxygen flow rate at 1 L/min for circle system (>15 lbs) and 1.5 L/min for non-rebreathing circuits (<15 lbs) Basic Life Support Basic Life Support Training Training Ventilation – Tips for endotracheal intubation Ventilation – Tips for endotracheal intubation • • Trinity Trach Tube Ties – http://trachtubeties.com • • Fiberoptic Laryngoscopes are much superior to bulb laryngoscopes (Miller blades preferred) Green plastic base on blade, green stripe on handle Different size attachment than standard laryngoscopes Basic Life Support Basic Life Support Training Training Chest Compressions Chest Compressions • • • • • • Achieve cardiac output of 25-30% normal If they generate a pulse, technique is good circumferential compression vests are not superior to manual compressions at the sternum Hand placement over the heart for lateral compressions No evidence that dorsal recumbency is superior to lateral recumbency • • • • “Given the lack of high-quality evidence, no evidence based recommendation regarding the best body position for chest compressions in dogs and cats can be made at this time.” Higher compression rates (100-120/min) are associated with better outcome than 60/minute Do not “lean” on the chest between compressions, to allow full recoil between compressions Compressions should be fast, as should the release If you have an extra person, interposed abdominal compressions do improve circulatory resuscitation Interruptions to check ECG should happen no more often than every 2 minutes 7 2/3/2014 Basic Life Support Training (CPR Flow Sheet Form) Domain 3 ALS – Advanced Life Support Advanced Life Support • • • • • • Defibrillation (BLS in CPR for people) IV fluid therapy to correct metabolic disturbances Drug therapy, including anesthetic reversal drugs Open chest CPR Strong support for epinephrine at 0.01 mg/kg Strong support for early defibrillation of Vfib or pulseless Vtach • IF BLS and ALS performed promptly, ROSC can be as high as 50% Advanced Life Support ALS Steps 1. Apply and respond to Monitors & Vital Signs – HR, RR, temp, ECG, BP, spO2, ETCO2 2. IV fluid bolus 10 ml/lb over 10-15 minutes – – – Contraindicated for congestive heart failure or oliguria/anuria Reassess and repeat as necessary Add colloids or hypertonic fluids PRN 3. Collect blood samples for Quick Assessment Tests – Glucose, BUN, creat, PCV/TS 4. Run CBC, panel, electrolytes if life can be prolonged 5. Respond to abnormalities, reassess and respond again Advanced Life Support Advanced Life Support Drugs Drugs Epinephrine – (0.01 mg/kg IV or IT) • • • • • • vasopressors vagolytics antiarrhythmics Glucocorticoids pH buffers Reversal agents • • • • • Raise blood pressure (pressor) Improve myocardial perfusion Increase tissue perfusion Increase cardiac output (increase SV, increase HR) This dose is preferred to higher doses 8 2/3/2014 Advanced Life Support Advanced Life Support Drugs Drugs Is Vasopressin preferred to epinephrine? Atropine 1:20 • • • • • • • Dose – 0.8 U/kg IV or IT Vasopressin causes no additional harm No studies in dogs and cats to show that vasopressin is better than epinephrine Vasopressin has an advantage for resuscitation of certain categories of people who suffer CPA – – – Dose – 0.4 mg/kg IV or IT Data using atropine without a pressor are lacking Reasonable to use when bradycardia or brief asystole occurs due to increased vagal tone – – – – – Asystole Prolonged CPA Hypovolemia as a cause of CPA brachycephalics Ileus, vomiting or other severe GI disease Respiratory distress Traumatic intubation Increased CSF pressure Advanced Life Support Advanced Life Support Drugs Drugs Atropine 1:20 Antiarrhythmics • • • • • • Unclear role for prolonged asystole – • Take care giving atropine when alpha agonists are on board (xylazine, dexdomitor) – • These need a shock as a last resort Pulmonary hypertension and pulmonary edema Atropine is not indicated for tachyarrhythmias: – – Lidocaine** Procainamide Amiodarone Bretylium Magnesium Ventricular fibrillation Ventricular tachycardia Advanced Life Support Advanced Life Support Drugs Drugs Antiarrhythmics Antiarrhythmics • • • No compelling evidence for routine use Use only if arrhythmia of increased automaticity is present – – – • Ventricular tachycardia Ventricular fibrillation – after defibrillation fails Pulseless vtach – after defibrillation fails Contraindicated for lack of electrical activity – – Amioderonemight be the most effective antiarrhythmic for shock resistant vfib and pulseless vtach I dogs – • • • Anaphylaxis has been reported Lidocaine is the next best choice Bretylium and magnesium play no role in treating these shock resistant arrythmias Amioderone has not been evaluated in cats Asystole bradyarrhythmias 9 2/3/2014 Advanced Life Support Advanced Life Support Drugs Drugs Lidocaine Cheat Sheet Lidocaine CRI Recipe (40-80 ug/kg/min IV) 1. 3 IV boluses over 10 minutes • – – 2 mg/kg (1cc/10lbs) IV over 1 minute x 2 4 mg/kg (2cc/10lbs) IV over 1 minute If using an IV pump (36-72 ug/kg/min IV) 1. 2. 3. 2. If not effective, then start IV CRI (40-80 ug/kg/min) • Add 50cc 2% lidocaine to 1L fluids to make a 1 mg/ml solution Set IV pump at Body Weight in pounds per hour for low end Double fluid rate for upper end of dose range If using drip rate (40-80 ug/kg/min IV) 1. 2. (CPR Drug Dose Chart) Mix as above if >30 lbs in body weight Make stronger solution if <30 lbs • • 3. 4. 5. If <5 lbs - 20cc 2% lidocaine in 100c fluid in the Buretrol (4 mg/ml) If 5-30 lbs - 10cc 2% lidocaine in 100c fluid in the Buretrol (2 mg/ml) Use 60 drop/ml IV set (use 15-20 drops/ml for 15-30 lb pets) Count seconds per drop if <30 lbs Count drops/sec if >30 lbs (drip rate chart) Advanced Life Support Advanced Life Support Drugs Drugs Buretol Corticosteroids Dial-A-Flow • No evidence that it helps, unless indicated for underlying process – – – • • Septic shock Anaphylaxis Addisonian crisis No evidence that it causes harm Not currently recommended Advanced Life Support Advanced Life Support Drugs Drugs Reversal agents Lipid therapy • • Naloxone (0.04 mg/kg IV) – – Reverses opiates on board Effects on endogenous endorphins • • • – • Reverses dexdomitor or amitraz no board Yohimbine (0.125 mg/kg IV) – • Reverses benzodiazepines on board Atimepazole (0.1 mg/kg IV) Reverses xylazine or amitraz no board Reversing other sedatives exacerbates ketamine dysphoria Lipophilic drugs – – – – Flumazenil (0.01 mg/kg IV) – • • Positive inotrope, antiarrhythmic More studies need to recommend for routine use If CPA during anesthesia is resuscitated, lipid therapy to clear lipophilic anesthetic drugs faster should be considered • Propofol, diazepam, ketamine, opiates beta blockers, calcium channel blockers parasiticides, herbicides psychotropic agents Intralipid® (Baxter) 20% lipid emulsion – – – 1.5 mL/kg over 5–15 min then 0.25 mL/kg/min over 1–2 hrs repeated in several hours if clinical signs of toxicity return, and there is no lipemia Use aseptic technique 10 2/3/2014 Advanced Life Support Advanced Life Support Drugs Drugs Buffers - bicarbonate • • • • Preponderance of evidence recommends against routine use of bicarbonate without confirming severe acidosis Could be considered in prolonged CPA Fewer harmful effects in dogs as compared to other species Indicated for confirmed metabolic acidosis Calcium • Routine use is not warranted or recommended • Indicated for: – – – Hypocalcemia calcium channel blocker overdose Severe hyperkalemia (Bicarbonate administration handout) Advanced Life Support Advanced Life Support Drugs Drugs Correcting Electrolyte/Metabolic Disturbances IV vs. IT drug administration • • • • • • Hyperkalemia – see section 5 Case Study “Tom” Hypokalemia (Potassium Supplementation Handout) Hypocalcemia – – • Calcium gluconate 10% 1.5-2.5cc IV slowly Recheck calcium in 15 minutes, re-dose PRN Hypoglycemia – – – – Dilute 1-3cc 50% Dextrose, qs to 10cc Administer IV over 1-3 minutes Serial reassessment of blood glucose and re-treat PRN Can use glucagon for insulin overdose Atropine, epinephrine, vasopressin Use high dose (10x) for IT epinephrine (Drug Dose Chart) Technique 1. 2. 3. 4. 5. 6. 7. Mark catheter at end of ET tube when end is at base of heart Draw dose and dilute qs to 3-10cc with sterile water or saline attach dose to 5-8F polypropylene catheter Disconnect endotracheal tube from ventilation (oxygen tank of ambu bag) Pass catheter to mark, inject drug Detach syringe, fill with air, and inject again to clear drug Resume ventilation Advanced Life Support Advanced Life Support Defibrillation Defibrillation • Electrical defibrillation is without question the most effective therapy for sudden cardiac death due to VF • Defibrillation should pre-empt CPR as soon as Vfib is identified, if Vfib has been present for less than 4 minutes • If Vfib more than 4 minutes, do 30 compressions and ventilate prior to defibrillation • Bipolar defibrillation is preferable to monophasic • most evidence supports prompt resumption of cardiac compressions, so single shock every 2 minutes is preferable to several in immediate succession • USE ECG cream rather than alcohol for lead contacts Increasing Defibrillator Energy • Excessively high defibrillation energy may be associated with increased myocardial damage • However, failure to successfully defibrillate is inevitably associated with death. • For monophasic defibrillators, increasing energy • doses are associated with increased success • For BP defibrillators, the evidence is less clear • an escalating protocol could be considered for both types defibrillators (increase by 50% each time) (CPR Drug Dose Handout) 11 2/3/2014 Advanced Life Support Advanced Life Support Defibrillation Defibrillation Internal Cardiac Compressions HP CodeMaster Defibrillator/ECG • Open-chest CPR is more effective than closed-chest CPR in restoring ROSC and promoting a good outcome in canine models of VFib (can visualize efficacy) • open-chest CPR requires significant resources, is a procedure that requires a skillful veterinary team, and demands advanced post-cardiac arrest supportive care. • In cases of significant intrathoracic disease it may be advisable to promptly perform open-chest CPR and defibrillation. – tension pneumothorax – Pericardial effusion Advanced Life Support Advanced Life Support Defibrillation Defibrillation Zoll Defibrillators Philips HeartStart Defibrillator / Monitor Advanced Life Support Defibrillation DRE VidaStat Biphasic Defibrillator & Monitor Domain 4 Monitoring 12 2/3/2014 Monitoring Monitoring Monitoring recommendations - Summary 1. Confirming CPA and intubation 2. Assessing adequacy of CPR and detecting ROSC 3. Continued monitoring after ROSC • Time spent verifying absent pulse may delay onset of CPR; chest compressions should be initiated immediately for apneic, unresponsive patients. • ECG analysis of an unresponsive patient may help to rule out CPA, or be used to evaluate for rhythms requiring specific therapy • End-tidal CO2 (EtCO2) should not be used as the sole confirmation of endotracheal intubation • Pauses in chest compressions to evaluate the ECG rhythm should be minimized Monitoring Monitoring Monitoring recommendations - Summary BSL - Rapid recognition of CPA • EtCO2 monitoring is useful to identify ROSC, and may be prognostic for the likelihood of ROSC • Patient monitoring following ROSC should be directed at identifying abnormalities that may portend another CPA, and should be tailored to each patient 1. Patient is unresponsive, pupils unresponsive 2. Absence of breathing (agonal does not count) 3. Absence of heart beat – – – – No palpable pulses No auscultable heart sounds No Doppler activity at pulse points or on the cornea Doppler assessment takes time, and might be more appropriate after CPR has been started, or ROSL 4. Start cardiac compressions here 5. ECG checks confirm lack of effective circulation 6. ETCO2 falls to near zero Monitoring Monitoring BSL - Rapid recognition of CPA BSL - How to Assess Breathing • • • • • Watch for chest excursions for at least 1 minute One hand lightly on the costochondral junction Fingers of the other hand in front of the nose at the same time Need to see chest movement more than once There should be clocks on the walls in all areas that are high risk for CPA – – – – – Surgery prep OR and areas for other anesthetic procedures Anesthesia Recovery ICU Clock on the crash cart is good 13 2/3/2014 Monitoring Monitoring BSL – Pulse Palpation to Detect CPA ECG to Detect CPA • Femoral pulse is preferred • lay rescuers and healthcare professionals are often unable to accurately and swiftly determine the presence or absence of a pulse • Need corroborating evidence • Pulseless electrical activity (PEA) can give a false negative for CPA • Relatively normal ECG must be corroborated by other evidence of spontaneous circulation • ECG does reliably identify arrhythmias – – – – – Vfib – defibrillate – Vtach making pulses – drugs – Pulseless Vtach – consider defibrillation then drugs Lack of apical beat Apnea agonal breathing lack of an auscultable heartbeat • Presence of dorsal pedal pulse (metatarsus) confirms MAP >80mmHg • ECG can confirm bradyarrhythmia and asystole – atropine for both (defib not indicated for asystole) • ALL CPA victims get epinephrine Monitoring Monitoring ECG to Detect CPA ETCO2 to Detect CPA • ECG can identify collapse without CPA • At constant ventilation, a rapid decline in ETCO2 value is expected during the evolution of CPA – Respiratory arrest • Start IPPV and assess for impending CPA – sudden decrease of ETCO2 to near zero is a strong indicator of CPA – Vagal surge • Atropine, ventilate, assess for impending CPA – Hypoglycemia • IV dextrose and reassess – Anaphylaxis • Epinephrine, corticosteroids, antihistamines, IV fluids – Internal hemorrhage • IV fluids, transfusion – Severe hypokalemia or acidosis • Supplement potassium first, then correct acidosis only if severe • In nonintubated patients, asphyxial CPA may elevate ETCO2 immediately prior to CPA – Subsequent ETCO2 will rapidly decrease after the first few delivered breaths unmasking the presence of CPA – Asphyxia without CPA might show improvement in ETCO2 after intubation and oxygenation • ETCO2 cannot be used alone to diagnose CPA • Rising ETCO2 during resuscitation may indicate ROSC Monitoring Monitoring Confirmation of Endotracheal Intubation ECG Monitoring During CPR • direct visualization of the ETT between the arytenoid cartilages is important • Palpate tube in the trachea • auscultation of air movement in both hemithoraces rules out bronchial intubation • observation of chest wall motion, or ETT condensation are supportive evidence • high ETCO2 immediately following intubation means endotracheal intubation is likely, due to the low amount of CO2 in the stomach and esophagus • low ETCO2 isn’t helpful • ECG can identify arrhythmias amenable to defibrillation (pulseless VT and VFib) • primary VFib remains a rare cause of CPA in veterinary patients • Most animals have initial arrest rhythm of PEA or asystole that may convert to VFib during CPR • ECG monitoring should be weighed against the risk of interrupting chest compressions for ECG rhythm check • resume chest compressions as soon as possible after defibrillation and rhythm check 14 2/3/2014 Monitoring Monitoring ETCO2 Monitoring During CPR ETCO2 Monitoring During CPR • EtCO2 serves as a noninvasive surrogate measurement of CO and myocardial perfusion during CPR • EtCO2 is frequently used as a reflection of quality of CPR when comparing approaches or devices. • alter circulatory support methods to optimize EtCO2 • EtCO2 rises steeply when ROSC occurs • continued low EtCO2 predicts nonsurvival • EtCO2 less than 10 mm Hg over several minutes during CPR is a poor prognostic indicator for ROSC • Use caution when interpreting a rise in EtCO2 after using either sodium bicarbonate or epinephrine during CPR • Increase in EtCO2 from <10 to >14 mm Hg should prompt evaluation for return of a heartbeat • Rise in EtCO2 an be used to distinguish PEA from ROSC Monitoring Monitoring Ventilation Monitoring During CPR Blood Gas and Electrolyte Assay During CPR • High ventilation rates (>10–12 breaths/min) should be avoided • increased time of positive intrathoracic pressure has negative effect on hemodynamics • Excessive ventilation during CPR commonly occurs, even with trained personnel • Venous blood gas values have better predictive value for ROSC than arterial blood gas values • Venous blood gasses are directly related to cardiac output and tissue perfusion • When cause of CPA is due to electrolyte abnormalities, electrolyte assay may allow directed therapy • Ionized hypocalcemia may be prognostic for ROSC • Identifying and correcting abnormalities may promote ROSC Monitoring Monitoring Vfib Waveform During CPR Monitoring after ROSC • coarse VF is more likely to respond with ROSC following defibrillation than fine VF • Asystole is unlikely to respond to defibrillation, despite this being commonly portrayed in medical dramas • On the other hand, little is lost by attempting to defibrillate prolonged asystole • To prevent re-arrest – treat precipitating disease – treat short term sequellae of CPA • Treat longer term sequellae of CPA – Brain hypoxia and ischemia – Cardiac ischemia and dysfunction – Reperfusion injury • Two types of post ROSC monitoring – Intensive continuous monitoring – Intermittent monitoring 15 2/3/2014 Monitoring Monitoring after ROSC • Parameters monitored – ECG - Myocardial hypoxia can result in post-resuscitation arrhythmia – BP - Episodes of hypotension following ROSC are associated with a worse outcome – Temperature – thermoregulation is a good prognostic indicator – spO2, +ETCO2 – hypoxic injury to the lungs can result in refractory pulmonary edema (ARDS) – Glucose - severity of post ROSC hyperglycemia is correlated with worse outcome Domain 5 Post--Arrest Care Post • Post ROSC seizures worsen prognosis Post Arrest Care • In humans, 60-70% of sudden CPA victims do not survive to hospital discharge despite having achieved ROSC initially • survival to discharge rates for dogs and cats range from 2-10%, despite initial ROSC of 35–45% • these patients succumb to post-cardiac arrest (PCA) syndrome – – – – multiorgan failure cardiogenic shock anoxic brain injury Sequellae of preexisting diseases Post Arrest Care Post-Arrest Recommendations – Summary • • • • • fluid therapy adjusted according to monitoring is reasonable Monitor and establish normoxemia neurologic benefit of gradual rewarming after hypothermia Conservative fluid resuscitation until cats are rewarmed no evidence to support routine administration of corticosteroids, antiseizure meds, mannitol, or metabolic protectants • Low-dose corticosteroid treatment of patients with persistent hypotension requiring sympathomimetic support may be considered Post Arrest Care Post-Arrest Recommendations – Summary • Hypertonic saline (HS) may be considered for cerebral edema as evidenced by coma, obtundation or dysphoria • Bundled therapy may have outcome benefit. – – – – Hypothermia Hypertension Normocapnia (as opposed to hypocapnia) Thiopental, methylprednisolone, phenytoin, antioxidants • More comprehensive PCA care in a specialty with ICU may have an outcome benefit CPR Guidelines 16 2/3/2014 CPR Guidelines CPR Guidelines Placement of Hands for Chest Compressions Small Animal Veterinary CPR Algorithm Post CPR Alogrithm CPR Guidelines Placement of Hands for Chest Compressions • For most dogs, do chest compressions over the widest portion of the chest • maximally employs the thoracic pump theory • Either left or right lateral recumbency are acceptable CPR Guidelines Placement of Hands for Chest Compressions • In keel-chested (i.e., deep, narrow chested) dogs like greyhounds, do chest compressions with the hands directly over the heart • in either left or right lateral recumbency CPR Guidelines Placement of Hands for Chest Compressions CPR Guidelines Placement of Hands for Chest Compressions • for barrel chested dogs like English Bulldogs, consider doing sternal compressions directly over the heart • patient in dorsal recumbency 17 2/3/2014 CPR Guidelines Placement of Hands for Chest Compressions CPR Guidelines Placement of Hands for Chest Compressions • for cats and small dogs (<10 kg) with compliant chests, a 1handed technique for circumferential chest compressions • hand wrapped around the sternum directly over the heart • An alternative is the 2-handed technique directly over the heart to employ the cardiac pump mechanism – This method may be considered in larger cats and small dogs with lower thoracic compliance – or in situations in which the compressor is becoming fatigued while doing 1-handed compressions CPR Guidelines Placement of Hands for Chest Compressions CPR Guidelines Placement of Hands for Chest Compressions CPR Guidelines Complete CPR Guidelines 18