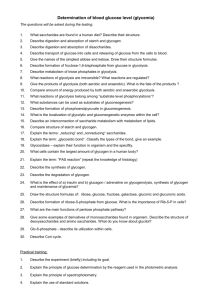
CARBOHYDRATE METABOLISM Formatted
advertisement

BIOLOGICAL CHEMISTRY
Chapter 5: CARBOHYDRATE METABOLISM
Dr. T.K. Bose
Department of Zoology,
Miranda House,
University of Delhi,
Delhi-110007, India
Date of Submission 2/9/2009
CONTENTS
Introduction
Sections:
5.1 GLYCOLYSIS
5.2 OXIDATION OF PYRUVATE
5.3 CITRIC ACID CYCLE
5.4 HEXOSE MONOPHOSPHATE PATHWAY
5.5 GLYCOGEN METABOLISM
5.5.1
Glycogenolysis
5.5.2
Glycogenesis
5.5.3
Reciprocal regulation of glycogenolysis and glycogenesis
5.6 GLUCONEOGENESIS
5.6.1
Pathway of gluconeogenesis
5.6.2
Reciprocal regulation of glycolysis and gluconeogenesis
5.7 MAINTENANCE OF BLOOD GLUCOSE
Credits for illustrations
2
CARBOHYDRATE METABOLISM
INTRODUCTION
Carbohydrates constitute a major part of our diet and our food is the ultimate source of all the
sugars that enter our metabolic pathways. About two-thirds of ingested carbohydrate is the plant
polysaccharide, starch. Disaccharides like lactose and sucrose and some other polysaccharides like
cellulose are also a part of our food, but our intake of free monosaccharides like glucose, fructose
and galactose is relatively minimal.
The table below indicates the class of dietary carbohydrate from which we derive the main sugars
that enter our blood stream.
TABLE 5.1. COMMON CARBOHYDRATES IN OUR FOOD
(Source: Vander, Sherman and Luciano, 2001, p 562)
Ingested food is digested by enzymatic hydrolysis in our gastrointestinal tract (GIT) and the
products obtained are simpler, absorbable molecules. All the hydrolytic reactions in digestion are
exergonic and proceed to completion. Starch is digested by the enzyme α-amylase (present in
saliva and pancreatic juice) to yield maltose and short-chain dextrins. These products, together
with other ingested disaccharides, are degraded to their constituent monosaccharides by
disaccharidases present in the luminal membranes of epithelial cells in the small intestine.
We do not have enzymes to digest cellulose and some other polysaccharides that constitute the
“fiber” in our diet, but bacteria in the colon can partially metabolize them.
The products of successful carbohydrate digestion are primarily glucose, fructose and galactose.
They are absorbed from the intestinal lumen i.e. transported across the intestinal epithelium into
the blood. Fructose enters the epithelial cells by facilitated diffusion while glucose and galactose
enter by secondary active transport coupled to sodium. All of them are then transported across the
baso-lateral membranes of the epithelial cells to the blood using facilitated diffusion transporters.
The portal vein carries the absorbed monosaccharides from the small intestine to the liver.
Subsequently the sugars enter the pathways of carbohydrate metabolism in the hepatic cells or in
the cells of our body tissues.
3
Glucose is the central molecule in carbohydrate metabolism. An overview of carbohydrate
metabolism (fig. 5.1) shows the links of glucose to almost all major groups of biomolecules in the
cell. Fructose and galactose have more restrictive routes of utilization.
RNA
DNA
Ribose
phosphate
Glucose
G LYC O G EN
O T H ER SU G AR S
G LYC O C O N J U G AT ES
Triose phosphate
ET H AN O L
LIPID S
LAC T AT E
Pyruvate
AM IN O
AC ID S
F AT T Y AC ID S
Acetyl-Co A
PR O T EIN S
citric
acid cycle
C O2
electron
transport chain
H ++ e-
O2
Fig 5.1.
AT P
H 2O
Overview of carbohydrate metabolism: Glucose is the central molecule in carbohydrate metabolism and its
metabolites form links with protein, lipid and nucleic acid metabolism. (Reversibility of pathways has not
been indicated).
All major pathways of carbohydrate metabolism are connected to conversions of glucose (fig.
5.2). This is not surprising since glucose is the main sugar in the blood and the main energy fuel in
the body. The metabolic pathways that we will deal with in this chapter are:
1.
Glycolysis
2.
Oxidation of Pyruvate
3.
Citric Acid Cycle
4.
Pentose Phosphate Pathway
5.
Glycogen metabolism:
a. glycogenolysis
b. glycogenesis
6.
Gluconeogenesis
4
Glycolysis, oxidation of pyruvate, citric acid cycle, pentose phosphate pathway and
glycogenolysis are catabolic pathways, while glycogenesis and gluconeogenesis are anabolic in
nature.
When considered in isolation, the first three pathways in the list above, involve only a modest gain
of energy as ATP. However a substantial gain in ATP is obtained when the products of the
pathways are linked to the mitochondrial electron transport chain. The other pathways (4, 5 and 6)
do not directly involve a major gain or loss of ATP.
Pathways 1 to 4 provide reductants (NADH, FADH2 and NADPH) for other metabolic reactions.
Glycogen metabolism and gluconeogenesis provide glucose or store it for later use. They are
typical to the animal system only.
Glycogen
( C6 )
n
glycogenesis
glycogenolysis
G LU C O SE
C6
pentose phosphate
pathway
gluconeogenesis
C skeleton from
non - carbohydrates
lactate
fermentation
2 Lactate
C3
glycolysis
2 Pyruvate
C3
Ribose + C O 2
C5
alcohol
fermentation
oxidative
decarboxylation
2 C O2
2 Ethanol + 2 C O 2
C2
2 Acetyl- Co A
C2
citric acid cycle
4 C O2
Fig. 5.2.
Major pathways of glucose metabolism, showing transformations of its C-skeleton. Anabolic pathways
are in blue; catabolic pathways are in pink.
The six pathways, their energy implications and their regulatory mechanisms are described in
separate sections of this chapter (Sections 1 to 6). We have briefly touched upon the regulation of
blood glucose in Section 7. We have primarily dealt with carbohydrate metabolism in
heterotrophs. Some of the pathways (Pathways 1 to 4) are common to plants.
5
However, photosynthesis which is an anabolic pathway converting CO2 to glucose, and is typical
to autotrophs, will not be discussed in this chapter.
Chapter 5 Section 1
GLYCOLYSIS
(Embden-Meyerhoff Pathway)
INTRODUCTION
Glycolysis is an almost universal pathway for catabolism of glucose in animals and plants. It
occurs in all cells of our body. The process is a partial oxidation of glucose where the 6-C
molecule is cleaved to form two 3-C units (pyruvate), and the energy released is conserved in the
form of ATP and NADH. The objective of glycolysis is to provide (i) energy and (ii)
intermediates for other metabolic pathways.
Ingested
carbohydrate
Cellular
glycogen
GLUCOSE
ATP
FRUCTOSE
1 , 6 - BISPHOSPHATE
ATP+ N AD H
PYRUVATE
anaerobicstate
aerobicstate
all cells
yeast
muscle , RBC
ETHANOL + C O 2
ACETYL - CoA
N AD H
+
LACTATE + N A D
Citric acid
cyc le
CO 2
N A D H + FADH
2
O2
Oxidative
phosphorylation
NAD
+
+ FA D + H O + A T P
2
Fig 5.1.3 Summary of glycolysis and processing of pyruvate by aerobic (green) and anaerobic (blue) methods. Only
the main intermediates and products are shown; stoichometry has not been indicated.
6
The major sources of glucose for glycolysis are dietary carbohydrates and cellular glycogen.
Ingested carbohydrates are digested to their constituent monosaccharides, absorbed in the
intestine, conveyed by blood to the liver and then distributed to the tissues. Glucose is also
obtained by degradation of glycogen reserves in the liver and muscle.
Other monosaccharides that enter glycolysis are fructose and galactose, and to some extent,
mannose.
Glucose (Glc) from the blood enters the cell, using membrane-located, tissue-specific glucose
transporter(s) ((e.g. GLUT2: liver, pancreatic β-cells; GLUT4: muscle, adipose tissue). Normally
muscle cells have a low-capacity transport system, which requires insulin for maximum uptake of
glucose. On the other hand, hepatocytes have a high-capacity, insulin-insensitive rapid transport
system for entry of glucose.
Fig. 5.1.4. Proposed model of a glucose transporter, GLUT 1 (Source: Nelson and Cox, 2005, p 393 fig 11-30)
REACTIONS OF GLYCOLYSIS
Glucose undergoes glycolysis by a sequence of 10 cytosolic reactions, seven of which are
reversible while three are irreversible. The first five reactions (Reactions 1 to 5 in Fig 5..1.2
constitute the “preparatory” or “investment” phase since they use ATP, while the last five
reactions (Reactions 6 to 10 in Fig 5..1.2) constitute the “pay-off” or “dividend” phase and yield
ATP.
7
Fig. 5.1.5.
The pathway of glycolysis: Numbers represent the order of the reactions. Reactions 1 to 5
constitute the ‘preparatory phase’ in which ATP is consumed while reactions 6 to 10 constitute
the ‘pay-off phase’ in which ATP is produced. The end product pyruvate, can be processed
anaerobically or aerobically (see text).The enzymes catalyzing reactions 1 to 10 are:
1. hexokinase/glucokinase
2. phosphohexoisomerase
3. phosphofructokinase
4. aldolase
5. triose phosphate isomerase
6. glyceraldehyde 3-phosphate dehydrogenase
7. phosphoglycerate kinase
8. phosphoglycerate mutase
9. enolase
10. pyruvate kinase
(Source: Vander et al 2001, p 71 fig 4-19)
8
For ease in understanding details of the glycolytic pathway, we have grouped the sequence of ten
reactions into four parts. We emphasize, however, that there is no actual division in the pathway.
I. Conversion of Glucose to Fructose 1,6-bisphosphate:
This sequence of 3 reactions activates glucose by phosphorylation and commits it to glycolysis as
fructose 1,6-bisphosphate (Fru 1,6-BP). The required phosphoryl groups are obtained from ATP.
H
HO
6
1
6
CH O H
2
O
H
OH
H
H
OH
ADP
ATP
M g2
H
OH
+
Glucose
H
H
HO
OH
H
H
OH
H
OH
3
O
H
H
OH
CH O H
2
HO
OH
H
OH
CH O H
2
HO
OH
H
Fructose 6-phosphate
∆G’o = 1.7 k J/mol
6
C H OP
2
O
isomerase
Glucose 6-phosphate
∆G’o = -16.7 k J/mol
6
C H OP
2
phoshpohexose
O
H
hexokinase/
glucokinase
2
C H OP
2
6
ADP
ATP
C H OP
2
1
O
C H OP
2
+
Mg2
phosphofructokinase-1
H
H
OH
H
Fructose 6-phosphate
HO
OH
H
Fructose 1,6-bisphosphate
∆G’o= -14.2 k J/mol
Fig 5.1.6. Conversion of glucose to fructose 1,6-bisphosphate with consumption of 2 molecules of ATP for every
molecule of glucose.
Reaction 1 is a ‘priming’ reaction in which glucose is activated to glucose 6-phosphate (Glc 6-P)
by phosphorylating it with ATP. The reaction is irreversible and catalyzed by the enzymes
hexokinase (HK) or glucokinase (GK), depending on the tissue concerned. Both kinases are
isozymes and have two substrates, glucose and Mg2+-ATP.
Fig. 5.1.7. Model of hexokinase with bound glucose (red)
(Source: Nelson and Cox, 2005, p 218 fig 6-22)
9
HK is a highly active enzyme in all cells except the liver parenchyma, where GK (also called
hexokinase IV) is dominant. The properties of these two enzymes reflect the difference in the role
of hepatic cells vis-a-vis non-hepatic cells in glucose metabolism. HK has a high affinity for
glucose and initiates glycolysis even when available Glc concentrations are low. GK has low
affinity for glucose and operates optimally only when blood Glc is >5 mmol/L (normal = 4.5 5.55 mmol/L). Thus the liver does not normally utilize glucose as energy fuel. HK can use other
dietary monosaccharides like fructose or mannose as substrate, but GK is specific for only
glucose.
Reaction 2 is a reversible isomerization in which phosphohexose isomerase converts Glc 6-P
(aldose), to fructose 6-phosphate (Fru 6-P; ketose)). Re-arrangement of C=O and –OH between C1 and C-2 of glucose is necessary for subsequent phosphorylation and cleavage in reactions 3 and
4.
Reaction 3 is another irreversible phosphorylation, catalyzed by phosphofructokinase-1 (PFK1), a
key enzyme of glycolysis. The product is fructose 1,6-bisphosphate (Fru 1,6-BP). This is the first
committed step of glycolysis;
Glc 6-P and Fru 6-P can be diverted to other pathways but Fru 1,6-BP will only continue with
glycolysis.
Reactions 1 and 3 are both exergonic and each consumes one molecule of ATP. Hence, the
reaction sequence 1 to 3 results in an energy loss of 2 ATP molecules per molecule glucose.
II. Cleavage of Fructose
Glyceraldehyde 3- phosphate:
CH 2 O P
CH 2 O P
O
H
1,6-bisphosphate
C H 2O P
4
aldolase
HO
C= O
H
OH
H
OH
to
+
Dihydroxyacetonephosphate
H
C= O
H
C
C H 2 OH
OH
C H 2O P
H
Fructose
1,6-bisphosphate
Dihydroxyacetone
phosphate
Glyceraldehyde
3-phosphate
∆G’o = 23.8 k J/mol
5
C H 2O P
C =O
triose phosphate
isomerase
H
C =O
C HO H
C H 2O P
C H 2O H
∆G’o = 7.5 k J/mol
Fig. 5.1.8. Cleavage of fructose 1,6-bisphosphate to the functional isomers dihydroxyacetone phosphate and
glyceraldehyde 3-phosphate.
10
and
Reaction 4 is essentially an aldol cleavage. Aldolase catalyzes cleavage of the 6-C unit of Fru 1,6BP into two 3-C units, producing an aldose, glyceraldehyde 3-phosphate (Glyc3-P), and a ketose,
dihydroxyacetonephosphate (DHAP). Glyc-3P is directly used in the subsequent step of
glycolysis, but DHAP can be used only after isomerization to Glyc 3-P in reaction 5. The forward
direction of reactions 4 and 5 depends on the utilization of Glyc 3-P in subsequent steps.
The interconversion of the triose phosphates by triose phosphate isomerase in reaction 5 makes C1, C-2 and C-3 of the starting glucose molecule indistinguishable from its C-6, C-5 and C-4
respectively.
Fig 5.1.9.
Derivation of carbon atoms of glyceraldehyde 3-phosphate from the 6 carbon atoms of glucose
6- phosphate. (Source: Nelson and Cox, 2005, p 522)
There is no gain or loss of ATP in this reaction. Although the aldolase reaction has a strongly
positive free energy change in the direction of Fru 1,6-BP, the low concentrations of reactants in
the cell ensures that there is little change in free energy of the system.
Subsequently, both triose units obtained from glucose undergo all the reactions 6 to 10.
Summary of the “investment” phase of glycolysis:
Reactions 1 to 5 consume 2ATP per molecule of glucose
11
III. Conversion of Glyceraldehyde 3-P to 3-Phosphoglycerate:
O
6
H
C= O
H
C
OH
N A D+
N A D H + H+
H
+ H 3 P O4
glyceraldehyde
3-phosphate
dehydrogenase
C H 2 OP
Glyceraldehyde
3-phosphate
C
OP
C
OH
C H 2O P
1,3-bisphosphoglycerate
∆G’o = 6.3 k J/mol
7
O
H
C
OP
C
OH
+ A DP
phosphoglycerate
kinase
C H 2OP
Mg
2+
COOH
C
OH + A T P
C H 2OP
1,3-bisphosphoglycerate
3-phosphoglycerate
∆G’o = -18.5 k J/mol
Fig. 5.1.10. Conversion of glyceraldehyde 3-phosphate to 3-phosphoglycerate which results in the production of
ATP and NADH. This sequence constitutes ‘a coupled reaction’ and is an example of ‘substrate level
phosphorylation (see text below).
Reactions 6 and 7 together constitute a crucial energy-coupling step in which reaction 6
produces a high-energy phosphoester derivative, 1,3-bisphosphoglycerate (1,3-BPG), which then
directly transfers ~ P to ADP producing ATP in reaction 7.
12
Fig. 5.1.11. Details of the reaction catalyzed by glyceraldehyde 3-phosphate dehydrogenase to show phosphorylation
of the substrate using inorganic phosphate.
(Source: Murray et al 2003, p 139 fig 17-3)
Let us examine the details of reaction 6. The reaction is endergonic and stores free energy in 1,3BPG. Glyceraldehyde 3-phosphate dehydrogenase is a tetramer with 4 identical subunits, each
with two binding sites viz one for its co-enzyme NAD+ and the other for its substrate, Glyc3-P.
The enzyme-substrate complex is a thio-hemiacetal with its terminal -CHOH oxidized to a
thioester by NAD+. The reduced co-enzyme NADH.H+, is easily displaced by a second molecule
of NAD+. The –C~S– bond of the thioester is then replaced by a high-energy phosphoester bond
using inorganic phosphate. The product 1,3-BPG is released and the original state of the enzyme is
restored.
In reaction 7, phosphoglycerate kinase converts 1,3-BPG to 3-phosphoglycerate (3-PGA). The
reaction is strongly exergonic and the stored energy of the previous reaction is used to generate
ATP. This is the 1st substrate-level phosphorylation, where a phosphoryl group is transferred
from the substrate 1,3-BPG to ADP, without using mitochondria or molecular oxygen.
The overall reaction sequence (6+7) is exergonic, though both reactions are individually reversible
under cellular conditions.
This is the first “pay-off” step of glycolysis. In terms of energy, it yields 1ATP and 1NADH.H+
(extramitochondrial) for every 3-C unit obtained from glucose.
13
IV. Conversion of 3-Phosphoglycerate to Pyruvate:
9
8
COOH
C
OH
phosphoglycerate
mutase
C H 2O P
Mg
2+
COOH
C
OP
COOenolase
C H 2 OH
3-Phosphoglycerate
C
O P + H 2O
C H2
2-Phosphoglycerate
∆G’o = 4.4 k J/mol
Phosphoenolpyruvate
∆G’o = 7.5 k J/mol
10
COOC
COO-
OP + A DP
pyruvate kinase
Mg
2+
, K+
C H2
C= O + A T P
CH3
Phosphoenolpyruvate
Pyruvate
∆G’o = -31. 4 k J/mol
Fig. 5.1.12. Conversion of 3-phosphoglycerate to pyruvate with further yield of ATP
This sequence of 3 reactions generates ATP. Reaction 8 is catalyzed by phosphoglycerate mutase,
which shifts a phosphoryl group from C-3 to C-2, thus converting 3-PGA to 2-PGA. The enzyme
itself participates in the reaction and Mg2+ is essential. Reaction 9 causes a redistribution of
energy in 2-PGA by dehydrating the molecule and generates a high-energy intermediate,
phosphoenolpyruvate (PEP). The enzyme used is enolase.
Reaction 10 is a 2nd substrate-level phosphorylation catalyzed by pyruvate kinase. The
phosphoryl group is transferred from PEP to ADP producing ATP, and the final product of
glycolysis, i.e. pyruvate. Pyruvate kinase requires K+ and Mg2+/Mn2+ for its action.
The standard free energy change of PEP hydrolysis is -61.9 kJ/mol. Approximately half of this
energy is conserved as ATP (-30.5 kJ/mol) and the rest is used to drive the reaction towards ATP
synthesis.
The system gains 1 ATP for every 3-C unit acted on by pyruvate kinase.
Recall that glucose yielded two 3-C units at the end of reaction 4. Since both 3-C units have gone
through reactions 6 to 10, hence 2 ATP molecules have been produced in each of the reactions 7
and 10 i.e. 4 ATP have been obtained per glucose molecule.
14
Summary of the “dividend” phase of glycolysis:
Reactions 6 to 10 directly generate 4ATP per molecule of glucose
We can now write the overall equation for glycolysis:
Glucose + NAD+ +2ADP + 2Pi à 2 Pyruvate + 2 NADH + 2H+ + 2ATP + 2H2O
Summarizing the net energy change in glycolysis, we have:
Reactions 1 to 5 utilize: 2 ATP/glucose molecule
Reactions 6 to 10 generate: 4 ATP/glucose molecule
Net gain = (4-2) ATP = 2 ATP/glucose molecule
Hence:
Glycolysis of 1 glucose molecule results in a direct net gain of 2 ATP molecules
Under actual cellular concentrations of reactants and products, the energy released in conversion
of glucose to pyruvate is recovered as ATP with an efficiency of >60%. The remaining chemical
energy in pyruvate can yield more ATP if pyruvate undergoes oxidation in the TCA cycle.
ENTRY OF OTHER SUGARS INTO GLYCOLYSIS
Several sugars in the diet are processed for entry into glycolysis as shown below:
MONOSACCHARIDES
ADP
ATP
Fructose
( in liver )
Mg
2+
fructokinase
Fructose
1 - phosphate
fructose 1- phosphate
aldolase
Glyceraldehyde
ATP
triose kinase
Mg
Dihydroxy
acetone phosphate
2+
isomerase
ADP
Glyceraldehyde
3 - phosphate
15
GLYCOLYSIS
ADP
ATP
Ma nnose
Mg 2 +
Mannose
6-phosphate isomerase
hexokinase
Fructose
6-phosphate
GLYCOLYSIS
ADP
A TP
Galactose
2+
Mg
Galactose 1-phosphate
galactokinase
galactose 1-phosphate
uridylyl transferase
Glucose 1-phosphate
U DP- Glucose
N A D+
U D P - galactose 4 - epimerase
U DP- Galactose
phosphoglucomutase
Glucose 6-phosphate
GLYCOLYSIS
m altase
GLYC OLYSIS
DISACCHARIDES
Ma ltose + H 2 O
La ctose + H 2 O
S ucrose + H 2 O
lactase
m altase
2 Glucose
Glucose + Galactose
Glucose + Fructose
GLYC OLYSIS
GLYC OLY S IS
Fig.5.1.13. The route of entry of common sugars into glycolysis. Breakdown of disaccharides is primarily a process
of digestion in the intestine but the processing of monosaccharides is a metabolic sequence.
Fructose enters glycolysis by two different pathways depending on the tissue. In adipose tissue
and muscle, hexokinase converts Fructose to Fru 6-P which enters glycolysis. The affinity of HK
for fructose is several times less than that for glucose. In the liver a specific enzyme, fructokinase,
converts fructose to Fru 1-P which cannot enter glycolysis. An aldol type cleavage of Fru 1-P to
glyceraldehyde and DHAP followed by phosphorylation enables entry into glycolysis.
Certain polysaccharides and glycoproteins in food yield mannose. It is first converted to mannose
6-P by HK and then isomerized to Fru 6-P for glycolysis.
Galactose (Gal) is a digestion product of lactose. A sequence of 4 reactions in the liver converts
galactose to Glc 6-P for entry into glycolysis. First, galactokinase phosphorylates Gal to Gal 1-P.
In the next step, uridylyl transferase shifts UDP from UDP-Glc to Gal 1-P, forming Glc 1-P and
UDP-Galactose. Phosphoglucomutase now isomerizes Glc 1-P to Glc 6-P for glycolysis. UDPGal-4-epimerase converts UDP-galactose back to UDP-glucose for re-entry into the transferase
reaction. The epimerization involves an oxidation and reduction at C-4, and the coenzyme used is
NAD+.
16
Lack of the enzymes transferase, epimerase or galactokinase causes a clinical disorder called
galactosemia.
REGENERATION OF NAD+
A cell has limited reserves of NAD+. For continuation of glycolysis it is essential that the
coenzyme is quickly regenerated. The method for regeneration depends on the redox state of the
tissue:
I. Anaerobic state – occurs in active skeletal muscle (when oxygen supply < demand), in RBC
(no mitochondria), and in deep-sea animals (O2-deficient environment). These tissues carry out
anaerobic glycolysis.
∆G’o = -25.1 kJ/mol
Fig. 5.1.14. Regeneration of NAD+ by anaerobic conversion of pyruvate to lactate. The reaction is carried
out by lactate dehydrogenase. Reversibility of the reaction has not been shown.
(Source: Vander et al 2001, p 72 fig 4-20)
Muscle and RBC carry out lactate fermentation. Pyruvate is reduced to lactate in the cytosol by
lactate dehydrogenase (LDH). The reductant used is NADH.H+ so that NAD+ is regenerated to
continue glycolysis. Lactate accumulating in the tissues, is carried away by the blood for
gluconeogenesis in the liver. This prevents metabolic acidosis. There are several tissue-specific
isozymes of LDH, and their identification is useful in clinical diagnosis.
In mammalian RBC, 90% of total energy yield is from lactate fermentation. Additionally, the
reaction catalyzed by phosphoglycerate kinase may be by-passed, producing 2,3bisphosphoglycerate (instead of 1,3-BPGA). The 2,3-BPGA combines with hemoglobin,
decreases its affinity for O2 and thereby facilitates unloading of O2 from oxyhemoglobin. The bypass reaction is not linked to the phosphorylation of ADP to ATP and hence, there is no energy
gain in the process.
17
Glyceraldehyde
3 - phosphate
bisphospho glycerate
mutase
1, 3 - Bisphospho glycerate
2 , 3 - Bisphos pho
glyce ra te
H2 O
ADP
phosphoglycerate
kinase
ATP
Pi
2 , 3 - bisphospho
glycerate
phosphatase
3 - phosphoglycerate
Fig 5.1.15. Production of 2,3-bisphosphoglycerate in mammalian RBC.
C OOC =O
CH 3
Pyruvate
C O2
TPP
Mg 2+
H
pyruvate
dehydrogenase
N A D H + H+
C= O
CH 3
N A D+
alcohol
dehydrogenase
Acetaldehyde
C H 2OH
CH 3
Ethanol
Fig 5.1.16. Fermentation of pyruvate to ethanol.
In yeast, anaerobic glycolysis is by ethanol fermentation and the final products are ethanol and
CO2. The enzyme pyruvate decarboxylase, which enables the reaction, is absent in mammals. As
Elliot and Elliot (2005) very aptly comment, its absence is beneficial for us, otherwise vigorous
exercise would have been a very intoxicating experience!
In all the above anaerobic conditions the regeneration of NAD+ is not associated with yield of
ATP.
Hence:
NET GAIN IN ANAEROBIC GLYCOLYSIS REMAINS AT 2 ATP PER MOLECULE OF GLUCOSE
It is known that ∆G’o for the reaction Glucose à Lactate = -196 kJ/mol
The energy conserved in 2 molecules of ATP = (2 x 30.5) kJ/mol = 61 kJ/mol
Hence, under standard conditions, the efficiency of anaerobic glycolysis in conserving energy is
approximately 31%.
II. Aerobic state – The NADH.H+ produced in glycolysis is extramitochondrial. Its re-oxidation
in the mitochondrial electron transport system (ETS) can generate ATP. Since the mitochondrial
membrane does not allow free passage of NADH.H+, a shuttle system is ingenuously used to
transport reducing equivalents from cytosolic NADH.H+ to acceptor molecules in the
mitochondrial matrix. The yield of ATP depends on the type of shuttle system used.
18
Fig 5.1.17. The glycerophosphate shuttle for transfer of reducing equivalents from cytosol to mitochondrial electron
transport chain. The outer mitochondrial membrane is not a barrier to transport and has not been shown.
(Source: Nelson and Cox, 2005, p 715 fig 19-28)
The glycerophosphate shuttle is used in skeletal muscle. Cytosolic glycerol 3- phosphate
dehydrogenase transfers electrons (and H+) from NADH.H+ to DHAP and regenerates NAD+ to
continue glycolysis. Concomittant reduction of DHAP produces glycerol 3-phosphate. An
isozyme of the dehydrogenase, bound to the inner mitochondrial membrane, now regenerates
DHAP by transferring the reducing equivalents from glycerol 3-phosphate to FAD for oxidative
phosphorylation in the ETS. This process yields 1.5 ATP per molecule of NADH.H+ re-oxidised,
i.e. 3 ATP per molecule of glucose that undergoes glycolysis.
. Fig. 5.1.18 The malate shuttle for transfer of NADH from cytosol to mitochondrion. The colored ovals represent
antiport proteins, one for malate-α-keoglutarate (blue) and the other for gluamate-aspartate (red). The
permeable outer mitochondrial membrane has not been shown.
(Source: Lodish et al, 2003, p 311 fig 8-10)
19
The malate-aspartate shuttle operates in the liver and heart and is more energy-efficient. In this
case the reducing equivalents from cytosolic NADH.H+ are carried by malate and transferred
finally to mitochondrial NAD+ for oxidative phosphorylation. Hence the energy yield is 2.5 ATP
per molecule of NADH.H+ i.e. 5 ATP per molecule of glucose that undergoes glycolysis.
We can now state that:
Net gain in aerobic glycolysis = (2 + 3/5) ATP = 5/7 ATP per molecule of glucose
REVERSIBILITY OF GLYCOLYSIS
A re-look at the values of ∆G’o for the ten reactions of glycolysis shows that seven of them are
physiologically reversible. For the reactions catalyzed by hexokinase, phosphofructokinase and
pyruvate kinase, the equilibrium lies too far to the right. Hence, the overall glycolytic pathway is
irreversible in the cell.
In order to reverse glycolysis, the three irreversible reactions are “by-passed”. We discuss these
methods in gluconeognesis. (Section 6)
INHIBITORS OF GLYCOLYSIS
Arsenate is a competitive inhibitor of glyceraldehyde 3-phosphate dehydrogenase. It competes
with Pi to form 1-arseno, 3-phosphoglycerate, which spontaneously yields 3-phosphoglycerate
and heat without producing ATP. Iodoacetate also blocks the substrate-binding site of the same
enzyme.
Fluoride inhibits enolase. It is used to prevent glycolysis in blood samples which have been
collected for glucose estimation.
REGULATION OF GLYCOLYSIS
Glycolysis is the major pathway for using glucose as an energy fuel. Accordingly, its regulation
depends on the energy state of the cell and on the levels of blood glucose. Regulatory mechanisms
maintain nearly constant ATP levels as well as an adequate supply of useful glycolytic
intermediates for other pathways. In times of need, regulation attempts to ensure that adequate
glucose is conserved for the brain and RBC.
The regulatory enzymes of glycolysis are hexokinase/glucokinase, phosphofructokinase-1 and
pyruvate kinase. The sites for control are the three irreversible reactions:
•
Glucose à Glucose 6-phosphate
•
Fructose 6- phosphate à Fructose 1,6-bisphosphate
•
Phosphoenolpyruvate à Pyruvate
The activity of the three regulatory enzymes is controlled by allosteric and covalent mechanisms
and depends on the secretion of the hormones insulin and glucagon. When blood glucose is low,
the pancreas secretes a high ratio of glucagon to insulin; the ratio is reversed when blood glucose
increases above normal levels.
1. Regulation of Hexokinase/Glucokinase
It is economical for a cell to control the 1st reaction of a metabolic pathway. In extrahepatic tissues
hexokinase is inhibited allosterically (product feedback inhibition) by Glc 6-P i.e. the activity of
the enzyme responds to the local needs of the cell. High [Glc 6-P] is a signal that the cell does not
need glucose for energy or for any other purpose. However, control of HK is not the most
effective step in regulation of glycolysis since Glc 6-P is needed for other pathways like
glycogenesis and HMP.
20
In the liver, glucokinase is an inducible enzyme. It is not inhibited by Glc 6-P but it responds to
the nutritional and hormonal state of the body. When blood levels of glucose fall, preferential
uptake of glucose by the muscle, RBC and brain vis-a-vis the liver, is ensured by the low affinity
of GK for glucose. GK is kept in the nucleus and released for optimal activity only when glucose
levels are high. Thus, the system ensures that Glc 6-P is produced primarily for storage as
glycogen in the liver, only when blood glucose is high. Insulin induces synthesis of GK, whereas
the antagonistic hormone, glucagon, is its repressor.
Fig.5.1.19. Regulation of glucokinase (hexokinase IV). The regulator protein in the nucleus allows release of the
enzyme from the nucleus to the cytosol for catalytic activity only when the concentration of glucose is
high. (Source: Nelson and Cox, 2005, p 578 fig 15-17}
2. Regulation of Phosphofructokinase-1
The most important regulatory enzyme in glycolysis is phosphofructokinase-1, which catalyzes
the first committed step of glycolysis by producing Fru 1,6-BP. Increase in the levels of Fru 1,6bisphosphate stimulates the rate of glycolysis. The levels of Fru 1,6-BP depend on the relative
activity of two opposing enzymes: PFK-1 which produces it from Fru 6-P, and fructose
bisphosphatase-1 (FBPase-1) which dephosphorylates it back to Fru 6-P. Allosteric modulators of
these enzymes ensure that [Fru 1,6-BP] is maintained according to the requirements of the cell.
21
G LU C O N EO G EN ESI S
Fructose 6-phosphate
Fructose 6-phosphate
ATP
citrate
-
-
A M P , A DP
+
P F K -1
F BP ase- 1
-
+
H+
-
Fru 2,6-BP
Fructose 1,6-bisphosphate
Fructose 1,6-bisphosphate
G LYC O LYSIS
Fig 5.1.20.
Allosteric modulators of PFK-1 (phosphofuctokinase-1) and FBPase-1 (fructose 1,6- bisphosphae-1)
The allosteric factors in regulation of PFK-1 are:
a. Ratio of [ATP] : [AMP] – High [ATP] inhibits while high [AMP] stimulates PFK-1
b. [Citrate] – Glycolysis is the natural feeder pathway for the TCA cycle in which citrate is the
first product. If citrate accumulates in the mitochondrion, further channelizing of pyruvate into the
cycle is wasteful. The system ensures that high [citrate] inhibits PFK-1, thus preventing formation
of more pyruvate.
c. [Fru 2,6-bisphosphate] – A crucial regulatory step in the liver is played by fructose 2,6bisphosphate (Fru 2,6-BP). It is a strong allosteric activator of PFK-1 and inhibitor of the
gluconeogenic enzyme, FBPase-1 It prevents the two opposing pathways viz. glycolysis and
gluconeogenesis, from occurring simultaneously.
6
P O C H2
OP
O
H
HO
H
2
CH 2 OH
OH
H
Fig 5.1.21. Structure of fructose2,6-bisphophate
The production of Fru 2,6-BP depends on [Fru 6-P] from which it is synthesized using a
bifunctional polypeptide having two enzyme activities viz. phosphofructokinasase-2 (PFK-2)
and fructose 2,6-bisphosphatatase (FBPase-2). These enzymatic functions are different from those
of normal PFK-1 and FBPase-1.
22
ADP
ATP
ATP
ADP
P F K-1
Fructose 1,6-bisphosphate
P F K- 2
Fructose 6-phosphate
FBPa s e-1
H 2O
Fructose 2,6-bisphosphate
FBPa s e-2
Pi
Pi
H 2O
Fig 5.1.22.Comparison of the action of enzymes PFK-1 / PFK-2 and FBPase-1 / FBPase-2 (PFK =
phosphofructokinase; FBPase = fructose 1,6-bisphosphatase)
Catalytic
activity
of
the
bifunctional
polypeptide
depends
on
its
own
phosphorylated/dephosphorylated state. This in turn determines whether Fru 2,6-BP is produced
by PFK-2, or converted back to Fru 6-P by FBPase-2. Thus, the levels of Fru 2,6-BP depend on
the relative activity of PFK-2 and FBPase-2
.
*
PFK - 2
[
PFK - 2
FBP
ase
phosphorylated
*
-2
*
FBP
ase
-2 *
dephosphorylated
P FK - 2
FB P
ase
]
Fructose 2,6-bisphosphate
*
*
-2
[
]
Fructose 2,6-bisphosphate
Fig 5.1.23. Schematic representation of the bifunctional polypeptide which has phosphofructokinase -2 and fructose
1,6-bisphosphatase-2 activities (PFK-2 and FBPase respectively). The green and red asteriks indicate
active and inactive states respectively.
When blood glucose falls, glucagon triggers a cAMP-dependent enzyme cascade mechanism
(refer Section 5) to phosphorylate the bifunctional polypeptide. This enhances its FBPase-2
activity. The resultant decrease in [Fru 2,6-BP] inhibits PFK-1 and the rate of glycolysis goes
down. Conversely, when blood glucose is high, insulin causes dephosphorylation of the
23
bifunctional polypeptide, increasing its PFK-2 activity. The resulting increase in [Fru 2,6-BP]
stimulates PFK-1 and the rate of glycolysis is enhanced.
STARVATION
[ Blood Glucose]
GLUCAGON
secretion
c A MP- mediated
enzyme cascade
BIFUNCTIONAL
[ Fructose 2,6-bisphosphate]
P F K- 1
inactive
POLYPEPTIDE
phosphorylated
G LYC O LYSIS
A.
d. [H+] – PFK-1 is inhibited by increase in H+ ions and hence a fall in pH (e.g when lactate
accumulates), decreases the rate of glycolysis. This reduces lactate formation and controls
metabolic acidosis.
24
WELL - FED
STATE
[ Blood Glucose]
INSULIN
secretion
BIFUNCTIONAL
POLYPEPTIDE
de phosphorylated
[ Fructose 2,6-bisphosphate]
P F K-1
active
G LYC O LYSI S
B.
Fig 5.1.24. Schematic diagram of the effect of the dietary state on the release of glucagon and insulin and the
resultant effect on the rate of glycolysis.
3. Regulation of Pyruvate Kinase
Regulation of pyruvate kinase (PK) controls formation of pyruvate, a glycolytic product also
linked to other metabolic pathways (refer below). Pyruvate kinase has several isozymes of which
L type is present in the liver and M type is found in the muscle. Both are allosterically inhibited by
high levels of ATP and acetyl-CoA (i.e. energy charge of cell is high) and stimulated by Fru 1,6BP (i.e glucose breakdown is on). Pyruvate kinase is also inhibited by alanine, a precursor of
gluconeogenesis.
25
A TP
fructose 1,6-bisphosphatase
-
acetyl- Co A , long-chain
fatty acids
,
-
alanine
+
PYR U VAT E KI N AS E *
dephosphorylated
PE P
+
A DP
-
pyruvate
+
A TP
A.
PYR U VAT E KIN ASE *
phosphorylated
A DP
+
H2O
protein
phosphatase
protein
kinase A
Pi
A TP
c A M P- mediated
enzyme cascade
+
G LU C AG O N
PYR U VAT E KI N ASE *
dephosphorylated
PE P
+
A DP
pyruvate
+
A TP
B.
Fig 5.1.25.
Regulation of pyruvate kinase: Fig A shows allosteric modulation of the enyme in all tissues. Fig B
shows covalent modification of the enzyme in the liver
The L form of PK is further subject to a covalent mode of regulation by reversible
phosphorylation. When blood glucose is low, glucagon works via cAMP to activate a protein
kinase (PKA), which phosphorylates and inactivates PK. Conversely, when blood glucose is high,
glucagon is not secreted and a protein phosphatase dephosphorylates and activates PK.
Additionally, insulin induces synthesis of active pyruvate kinase. The net result is that glycolysis
is facilitated in all cells.
On a longer time scale, the type of diet and diseases/metabolic disorders may lead to the hormonal
induction or repression of the genes synthesizing the glycolytic enzymes. These adaptive changes
are primarily enabled by insulin and glucagon. Tumors that cause hypoxia induce increased
synthesis of glycolytic enzymes.
(To the young reader: The entire mechanism of regulation is confusing to everybody at this stage!
It will become more comprehensible after you study glycogen metabolism and gluconeogenesis,
and attempt to make your own flow diagrams).
26
FATES OF PYRUVATE
The pyruvate molecule is at the cross-roads of many metabolic pathways. Glycolysis degrades
glucose to pyruvate in all tissues, while gluconeogenesis synthesizes glucose from pyruvate in the
liver. Transamination interconverts pyruvate and alanine, linking carbohydrate metabolism with
protein metabolism.
GLU COSE
gluconeogenesis
glycolysis
ALAN IN E
transamina tion
PYR UVATE
reduction
LACTATE
oxidative
decarboxylation
carboxylation
OXALOAC ETATE
AC ETYL-CoA
Fig 5.1.26. Metabolic fates of pyruvate
Under anaerobic conditions, pyruvate undergoes fermentation into lactate or ethanol. In the
aerobic state, pyruvate is oxidized to acetyl-CoA in the mitochondrion and enters the citric acid
cycle with the ultimate purpose of producing ATP and biosynthetic intermediates. Pyruvate also
connects with lipid metabolism via acetyl CoA and NADPH.H+, necessary precursors in the
synthesis of fatty acids.
In the next section we will follow the aerobic metabolism of pyruvate, a pathway which has the
potential to conserve energy as ATP.
SUMMARY 5.1: GLYCOLYSIS
Carbohydrate metabolism is constituted by anabolic, catabolic and amphibolic pathways, most of
which deal with glucose or its metabolic products. Glycolysis is a major catabolic pathway of
glucose which occurs in the cytosol. It is a well-regulated pathway that provides energy to cells
under both anaerobic and aerobic conditions. A series of ten reactions degrade glucose to
pyruvate, and also reduce the coenzyme, NAD. Under anaerobic conditions, a small net yield of
ATP is obtained essentially by substrate level phophorylations. The reduction of pyruvate to
lactate regenerates NAD from NADH to continue glycolysis. When pyruvate and NADH are
processed aerobically in the mitochondrion, a much larger yield of ATP can be obtained. Shuttle
systems enable transfer of reduced equivalents to the mitochondrion.
27
Chapter 5 Section 2
OXIDATION OF PYRUVATE
The oxidative decarboxylation of pyruvate (C3) to acetyl-CoA (C2) is the link reaction between
glycolysis and the citric acid cycle. Before we embark on the citric acid cycle in Section 3 of this
chapter, let us first understand the way in which pyruvate provides the essential C-2 unit to the
TCA cycle.
The conversion of pyruvate to acetyl-CoA occurs in the mitochondrion. Decarboxylation degrades
the carbon skeleton of pyruvate from C3 to C2, and oxidation leads to formation of acetyl-CoA, a
key metabolite in several metabolic pathways. The overall reaction is highly exergonic and
irreversible.
O
C H3 C
_
COO-
+
CoA
_
SH
+
NAD+
pyruvate
dehydrogenase
complex
Pyruvate
O
C H3 C
~ S CoA
Acet yl
+
N A D H. H +
- CoA
+
H
+ CO2
∆G’o = -33.4 k J/mol
Fig 5.2.1. Overall reaction of the conversion of pyruvate to acetyl-CoA by the pyruvate dehydrogenase complex
Oxidative decarboxylation is catalyzed by a remarkable multi-enzyme complex called pyruvate
dehydrogenase complex (PDH complex), located in the inner mitochondrial membrane. It is
essentially comprised by 3 enzymes and 5 cofactors:
•
pyruvate dehydrogenase
dehdrogenase (E3)
(E1),
dihydrolipoyl
transacetylase
(E2),dihydrolipoyl
•
dissociable coenzymes : NAD+ and CoA
•
enzyme-bound cofactors: thiamin diphosphate (TDP), lipoamide and FAD
Fig 5.2.2. Model of the three-dimensional structure of PDH complex: The core is constituted by 60 molecules of
(green) to which the peripheral E1 molecules (yellow) are connected by the lipoyllysyl arms (blue);
subunits are in red and are also bound to the core. (Source: Nelson and Cox, 2005, p 604 fig 16-5)
28
E2
E3
Multiple copies of the enzymes are clustered together to form a very large complex (diameter =
30-50 nm).The enzymes are spatially positioned in an organized manner, and their regulatory
proteins are also associated with the complex. The movement of individual enzymes is restricted.
The multi-enzyme complex has a very high catalytic efficiency. The movement of individual
enzymes is restricted. The reaction intermediates remain bound to the enzymes so that high local
concentrations of substrates are maintained. Substrates are passed from one enzyme to the next in
the sequence (substrate-channeling), thus preventing any of the substrates from going astray into
other pathways. Consequently, enzyme-substrate interactions are quick and reaction rates are high.
Regulation of the enzymes is also easily co-ordinated.
Fig 5.2.3a. Domain structure of dihydrolipoyl transacetylase (E2) (Source: Nelson and Cox, 2005, p 604 fig 16-5)
E1 binds TPP while E3 attaches FAD at their respective active sites. E2 presents an unusual and
intriguing structure with three distinct domains. A long side-chain at the amino terminal end in E2
bears a lysyl residue which attaches lipoate. The lipoamide so formed, is now located at the end of
a long, flexible arm, which can swing from the active site of E1 to the active sites of E2 and E3.
Lipoate has two thiol (-SH) groups which can be reversibly oxidised to a disulphide (-S-S-). It
functions as a carrier of both hydrogen and an acyl group. Coenzyme A can carry an “activated”
acyl group, bonded covalently as a thioester.
Fig 5.2.3b. Lipoyllysyl arm of dihydrolipoyl transacetylase (E2) (Source: Nelson and Cox, 2005, p 603 fig 16-4)
29
The basic E1 -E2 -E3 structure is conserved in evolution and used in similar metabolic reactions like
the oxidations of α-ketoglutarate and branched-chain amino acids. It is an amazing molecular
system which has evolved to consolidate a specific reaction sequence in an environment
(mitochondrial matrix) where so many other enzymes are always in action!
SEQUENCE OF REACTIONS
Pyruvate is produced in the cytosol. It is translocated to the mitochondrial matrix by an antiport
mechanism whereby hydroxyl from the matrix is transferred to the cytosol.
Fig 5.2.4. Steps in the oxidative decarboxylation of pyruvate to acetyl-CoA by the pyruvate dehydrogenase
complex. Note the movements of the lipoamide arm of E2. (E1 = pyruvate dehydrogenase; E2 =
dihydrolipoyl transacetylase; E3 = dihydrolipoyl dehydrogenase; TPP = thiamin pyrophosphate)
(Source: Boyer, R., 1999, fig. 16.3; p 484)
The oxidative decarboxylation of pyruvate is a sequence of five reactions:
Reaction 1 is catalyzed by pyruvate dehydrogenase (E1), an enzyme which also determines the
substrate specificity of the multi-enzyme complex. Pyruvate is decarboxylated at C-1, releasing
CO2. The remaining hydroxyethyl (C-2) unit is attached to TPP, to produce acetol-TPP.E1 .The
reaction is slow and limits the overall rate of oxidative decarboxylation. Reaction 1 is irreversible
and is the determinant for the reaction sequence to proceed from pyruvate towards acetyl-CoA.
Reaction 2 is catalyzed by dihydrolipoyl transacetylase (E2). The acetol unit is transferred from
TPP to oxidized lipoamide on E2. As a result the disulphide of the lipoyl group is reduced to two
thiol groups, one of which is then esterified and a high-energy thioester bond is created. The
product is acetyl-lipoamide.E2.
30
Reaction 3 is also catalyzed by E2.The long lipoyllysyl arm of E2 transfers the acetyl group to the
–SH of CoA, producing acetyl-CoA. The energy-rich thioester bond is preserved in acetyl-CoA.
Reduced lipoamide (dihydrolipoamide.E2) remains attached to E2 while acetyl-CoA is released.
Reaction 4: The flavoprotein enzyme, dihydrolipoyl dehdrogenase (E3), containing FAD, reoxidizes dihydrolipoamide and enzyme-bound FADH2 is obtained.
Reaction 5 is also catalyzed by E3. FADH2 is re-oxidized to FAD by NAD+. The NADH.H+
formed is released and subsequently passed to the electron transport chain for generation of ATP.
After the 5th reaction the PDH complex is in a catalytically active form again, ready to receive
another molecule of pyruvate for the next round of oxidative decarboxylation.
Energy yield
Oxidative decarboxylation of a pyruvate molecule yields one molecule of NADH.H+. Since the
reaction takes place in the mitochondrion, the reduced coenzyme is directly passed into the ETS
and can generate 2.5 ATP per molecule of NADH.H+. The transfer of electrons from FADH2 to
NAD+ is contrary to the usual direction of transfer in the ETS and is possible owing to the unusual
electron transfer potential of FAD bound to E3.
Hence:
ENERGY YIELD OF OXIDATIVE DECARBOXYLATION IS 2.5 ATP PER MOLECULE OF PYRUVATE.
REGULATION OF THE PDH COMPLEX
The PDH complex plays a key role in providing acetyl-CoA from carbohydrate sources to the
citric acid cycle. It is a well-regulated system, primarily governed by the energy state of the cell.
The rate of conversion of pyruvate to acetyl-CoA depends on the irreversible reaction catalyzed
by pyruvate dehydrogenase i.e. E1, and hence this is the most appropriate site for regulation.
The mechanisms of regulation are:
1. End-product inhibition of PDH
CoA
Pyruvate
CO2
+ NAD+
Acet yl
- CoA
P D H complex
_
Fig 5.2.5a.
_
End-product inhibition of pyruvate dehydrogenase.
31
+ N A D H. H +
+
H
The end products of pyruvate oxidation viz. acetyl-CoA, and NADH.H+, inhibit PDH
allosterically. The inhibition is enhanced if acetyl-CoA is concomittantly produced by β-oxidation
of fatty acids. Conversely, when the availability of C-2 unit for the TCA cycle is insufficient, the
low concentrations of acetyl-CoA and NADH.H+ are ineffective, and PDH actively oxidizes more
pyruvate to acetyl-CoA.
2. Covalent modification of PDH
PDH (E1) can be reversibly phosphorylated at serine residues by the converter enzymes PDH
kinase and PDH phosphatase. E1 is active only in the dephosphorylated state. PDH kinase
phosphorylates and inactivates E1 while PDH phosphatase promotes pyruvate oxidation by
dephosphorylating and activating E1.
[ Acet yl - CoA ] / [CoA ]
Pyruvate
_
+
Dichloroacetate
Ca2 +
[ N A D H ] / [ N A D +]
_
+
[ A T P] / [ A D P]
+
_
P D H k ina s e
Mg 2 +
active
E1 _
A DP
ATP
OH
dephosphorylated
2+
+
Mg , C a 2
+
2-
O P O3
inactive
phosphorylated
P D H phos pha ta s e
+
INSULIN
H2O
Pi
Fig 5.2.5b.
E1 _
Covalent modification of pyruvate dehydrogenase (E1)
The kinase is stimulated allosterically by high ratios of [ATP]:[AMP], [NADH]:[NAD+] when the
energy state of
cell is high, and by increased ratio of [acetyl-CoA]: [CoA] during starvation/intake of a high fat
diet. Increased kinase activity inhibits E1 and pyruvate oxidation is suppressed.
In this way the cell conserves glucose when acetyl-CoA is either not required for the TCA cycle,
or is provided by fatty acids. On the other hand, accumulation of pyruvate inhibits PDH kinase, so
that E1 continues to be active and accelerates the conversion of pyruvate to acetyl-CoA.
32
Muscle contraction is associated with intracellular release of Ca2+, which also acts via covalent
modification to activate E1 so that the availability of acetyl-CoA for the TCA cycle is increased
and more ATP can be generated.
Insulin, secreted when blood levels of glucose are high, stimulates PDH phosphatase to
dephosphorylate and activate E1 for increased oxidation of pyruvate.
SUMMARY 5.2: OXIDATION OF PYRUVATE
When aerobic conditions prevail, the end-product of glycolysis i.e. pyruvate, is processed in the
mitochondrion. A unique multi-enzyme system called the pyruvate dehydrogenase complex,
oxidatively decarboxylates pyruvate to acetyl-CoA. NADH and carbon dioxide are also endproducts. Oxidation of pyruvate makes acetyl-CoA available within the mitochondrion for use in
the citric acid cycle as well as for fatty acid synthesis. NADH yields ATP when passed into the
mitochondrial respiratory chain.
Chapter 5 Section 3
CITRIC ACID CYCLE
(Kreb’s cycle/TCA cycle)
The citric acid cycle is the final common pathway for oxidation of carbohydrates, lipids and
many amino acids. It takes place in aerobic organisms within cells that have mitochondria. Its
main purpose is to oxidize acetyl-CoA and concomitantly reduce NAD+ and FAD. Re-oxidation of
the reduced co-enzymes in the mitochondrial respiratory chain uses molecular O2 and generates
ATP. The cycle also provides biosynthetic intermediates for other metabolic pathways.
CARBOHYDRATE
LIPID
PROTEIN
C2 Acetyl - CoA
ETS
NADH
C6
C4
C4
CI TRI C ACI D
C4
ETS
FADH 2
C6
NADH
CYCLE
ETS
CO2
C5
C
4
NADH
C4
ETS
CO
2
GT P / AT P
Fig 5.3.1. Overview of the citric acid cycle (ETS = Electron Transport System)
33
REACTIONS OF THE TCA CYCLE
Each turn of the TCA cycle is constituted by 8 reactions, catalyzed by the sequential action of 7
enzymes and one multi-enzyme complex. The enzymes are present in the mitochondrial matrix,
in close proximity to the electron transport chain on the mitochondrial cristae. The essential
precursors for the TCA cycle are acetyl-CoA and oxaloactetate (OAA). Two C atoms are received
as an acetyl unit, and oxidation produces two molecules of CO2. There are four oxidationreduction steps which yield H+ and electrons to reduce NAD+ and FAD to NADH.H+ and FADH2
respectively. There are 8 intermediates in the cycle and one 4-C unit i.e. OAA, is regenerated.
Fig 5.3.2.The reactions of the citric acid (TCA) cycle. Refer to the text for details. (Source: Nelson and Cox, 2005, p
607 fig 16-7)
34
Reaction 1: Conversion of acetyl-CoA to citrate (∆G’o = -31.5 kJ/mol)
Acetyl-CoA (2-C) and the keto-acid oxaloacetate (4-C), undergo condensation to form citrate (6C) in a reaction catalyzed by citrate synthase. On binding OAA, the enzyme undergoes a
remarkable conformational change which facilitates attachment of its 2nd substrate, acetyl-CoA.
The reaction involves an aldol condensation followed by a hydrolysis in which H2O is used. The
equilibrium for the hydrolysis lies far to the right so that the overall reaction moves towards the
synthesis of citrate, driving the cycle forward.
Reaction 1 is irreversible under cellular conditions.
Reaction 2: Isomerization of citrate to isocitrate (∆G’o = ~5 kJ/mol)
Citrate is channeled directly to the active site of the next enzyme, aconitase, to undergo a two-step
reaction that converts it to isocitrate (ICA). Aconitase carries 3 different Fe:S clusters which bind
citrate and enable the reaction.
Fig 5.3.3. An Iron-sulfur center (pink) in aconitase which binds citrate (blue). ‘B’ is a basic residue in the enzyme
which helps to position the substrate for binding and catalysis.
(Source: Nelson and Cox, 2005, p 610 fig 16-10)
The symmetrical citrate molecule is acted on asymmetrically by aconitase so that an –OH is
shifted from C-3 in citrate and attached to C-4, a carbon atom derived originally from OAA. The
reaction involves a dehydration followed by a hydration, with cis-aconitate as intermediate.
Though the aconitase reaction is reversible, it is pulled to the right by the rapid utilization of its
product, ICA, in the next step.
Reaction 3: Oxidative decarboxylation of isocitrate to α-ketoglutarate
(∆G’o = -21 kJ/mol)
Isocitrate (6-C) is irreversibly oxidized and decarboxylated to α-ketoglutarate (5-C) in a two-step
reaction catalyzed by isoctrate dehydrogenase (IDH). The enzyme uses NAD+ as a reductant and
requires Mn2+. NADH.H+ is produced in the the 1st step. Enzyme-bound intermediate,
oxalosuccinate, is an unstable β-keto acid which loses CO2.
The rate of formation of α-ketoglutarate (α-KGA) is important in determining the overall rate of
the TCA cycle.
35
Reaction 4: Oxidative decarboxylation of α-ketoglutarate to succinyl-CoA
kJ/mol)
(∆G’o = -33
This reaction is catalyzed by a multi-enzyme complex, α-ketoglutarate dehydrogenase complex
(α-KGA-DH complex), which functions in a manner identical to the PDH complex for pyruvate.
The α-KGA-DH complex and the PDH complex are homologous enzyme assemblies with the
main function of transferring a keto group to CoA. The 1 st and 3rd enzymes here, α-ketoglutarate
dehydrogenase (α-KGA-DH) and trans-succinylase respectively, are functionally similar to E1 and
E3 of the PDH complex. The 2nd enzyme, dihydrolipoyl dehydrogenase, is identical in both
complexes. Oxidative decarboxylation of α-KGA yields succinyl-CoA (C-4), CO2 and NADH.H+.
The overall reaction is exergonic and irreversible. The energy released is conserved in the
thioester bond of succinyl-CoA (∆G’o for hydrolysis of succinyl-CoA = -36 kJ/mol).
Reaction 5: Conversion of succinyl-CoA to succinate (∆G’o = -2.1 kJ/mol)
Succinyl-CoA synthetase (= succinate thiokinase) converts succinyl-CoA to succinate, a 4-C
compound. The reaction is a substrate-level phosphorylation in which the energy released on
breaking the thioester bond of succinyl-CoA, is coupled to the phosphorylation of GDP/ADP to
GTP/ATP respectively (∆G’o = -2.9 kJ/mol). Animal cells generally use GDP though some (e.g.
liver) have isozymes for both GDP and ADP. (Plant cells and bacteria use only ADP). The
terminal phosphate group of GTP is transferred to ADP by nucleoside diphosphate kinase.
GT P
+
A DP
nucleoside
diphosphate
kinase
G DP
+
AT P
(∆G’o = 0 kJ/mol)
Fig 5.3.4. Phosphorylation of ADP with GTP
Reaction 5 is reversible. The intermediates formed in subsequent reactions of the cycle, viz.
fumarate, malate and OAA, are 4-C compounds.
Reaction 6: Conversion of succinate to fumarate (∆G’o = +6 kJ/mol)
Succinate dehydrogenase (SDH) oxidizes succinate to fumarate, while its co-factor, FAD, is
reduced to FADH2. SDH is embedded in the inner mitochondrial membrane (all other
dehydrogenases are in the matrix) and transfers hydrogen and electrons directly from the substrate
to FAD, without involving NAD+. The enzyme also has 3 different kinds of Fe:S clusters through
which electrons flow from FADH2 to the ETS.
Reaction 7: Hydration of fumarate to malate (∆G’o = -3.4 kJ/mol)
Fumarase adds –H and –OH in the trans position across the double bond of fumarate, converting it
to L-malate.
36
Reaction 8: Regeneration of oxalacetate (∆G’o = +29.7 kJ/mol)
Malate is oxidized to OAA by malate dehydrogenase (MDH). Its coenzyme NAD+ is reduced to
generate the 3rd molecule of NADH.H+ in the cycle. Regenerated OAA is now ready to accept
another molecule of acetyl-CoA for the next round of the cycle.
The equilibrium favors malate formation over OAA, but is driven forward by the strongly
exergonic condensation of OAA with acetyl-CoA in the next turn of the cycle, and the continuous
re-oxidation of NADH.H+ in the ETS.
Overall reaction of one turn of the TCA cycle
Acetyl-CoA + NAD+ + FAD + GDP + Pi + H2O à 2 CO2 + 3 NADH + FADH2 +GTP +
2H+ + CoA
The citric acid cycle completely catabolizes acetyl-CoA. A tally of C, H and O atoms which enter
the cycle with those that leave the cycle is as follows:
Carbon atoms:
Entry as 1 CH3.CO.SCoA = 2
Release as 2 CO2 = 2
Hence: Carbon atoms entering the cycle are fully oxidized
Hydrogen atoms:
Entry as 1 CH3.CO.SCoA = 3
Entry as 2 H2O = 4
Entry from 1 Pi (H3PO4) = 2
Total = 9 Hydrogen atoms enter the cycle
Released as 3 NADH.H+ = 6
Released as 1 FADH2 = 2
Released as 1 CoASH = 1
Total = 9 Hydrogen atoms are released from the cycle
Oxygen atoms:
Entry as 1 CH3.CO.SCoA = 1
Entry as 2 H2O = 2
Entry from 1 Pi (H3PO4) = 1
Total = 4 Oxygen atoms enter the cycle
Release as 2 CO2 = 4
Total = 4 Oxygen atoms are released from the cycle
37
In each turn of the cycle the C atoms derived from acetyl-CoA have definite locations in the
molecules from citrate to succinyl-CoA, but the positions are variable in the later intermediates of
the cycle. During the conversion of succinyl-CoA to succinate, there is randomization in the order
of carbon atoms. Consequently, the two atoms that leave as CO2 in a particular turn of the cycle,
are not the same two carbon atoms that had entered as acetyl-CoA in that turn. Additional turns of
the cycle are required to remove these carbon atoms as CO2.
Water is the ultimate source for the H atoms not derived from acetyl-CoA, and of the oxygen
which is used to produce CO2, though its components, H and O, are utilized indirectly.
Since there is no net removal of OAA in the TCA cycle; hence one molecule of OAA can
theoretically bring about the oxidation of an infinite number of acetyl groups. In practice,
however, the supply of OAA needs to be replenished, since it is used by other metabolic pathways
as well.
REVERSIBILITY OF THE CYCLE
All the reactions of the cycle are reversible except those catalyzed by citrate synthase, IDH and αketoglutarate dehydrogenase. These reactions have a sufficiently large ∆G value to be irreversible
and account for an overall ∆Go’ of -40 kJ/mol. Hence the cycle operates unidirectionally.
ENERGY YIELD
The step-wise degradation and oxidation of acetyl-CoA in the citric acid cycle is an efficient
process for extraction of energy. The available energy is not released in one burst; it is transferred
step-by-step to small packets of NADH and FADH2 to be carried to the electron transport system
(ETS).
In every turn of the cycle involving one molecule of acetyl-CoA, 3 hydride ions (i.e. 6 electrons)
are transferred to 3 NAD+ molecules while one pair of hydrogen atoms (i.e. 2 electrons) are
transferred to an FAD molecule. Re-oxidation of 3 NADH and 1 FADH 2 by oxidative
phosphorylation in the ETS generates (7.5 +1.5) ATP i.e. 9 ATP (recall that ATP yield is 2.5/
NADH and 1.5/FADH2 if source is mitochondrial). In addition 1 GTP/ATP has also been
obtained.
Hence, for every turn of the citric acid cycle:
TOTAL YIELD IS 10 ATP PER MOLECULE OF ACETYL COA
38
THE FINAL BALANCE SHEET
From Sections 1, 2 and 3 of this chapter we can now summarise the energy yield in terms of ATP
when one molecule of glucose undergoes complete oxidation to CO2 and water:
Gain of ATP by substrate-level phosphorylation:
•
Glycolysis = 4 ATP
•
Citric acid cycle = 2 ATP
Gain by oxidative phosphorylation:
•
2 NADH (cytosolic) in glycolysis = 3/5 ATP (depends on use of glycerophosphate/malate
shuttle)
•
2 NADH (mitochondrial) by PDH complex = 5 ATP
•
6 NADH (mitochondrial) from TCA cycle = 15 ATP
•
2 FADH2 from TCA cycle = 3 ATP
Thus, total yield = 32/34 ATP per molecule of glucose oxidised
Loss by utilization in glycolysis = 2 ATP
Hence:
NET ENERGY YIELD IN AEROBIC OXIDATION = 30/32 ATP PER MOLECULE OF
GLUCOSE
Compare this to the net energy yield of a mere 2 ATP per molecule of glucose oxidized
anaerobically.
It is estimated that by synthesizing ATP, the efficiency of trapping the energy released in glucose
oxidation is 65%, This is calculated on the basis of actual free energy changes that occur in
cellular conditions of pH, and low, unequal concentrations of ATP, ADP and Pi.
PROVISION OF SUBSTRATES FOR THE TCA CYCLE
Essential substrates for the cycle are acetyl-CoA (2-C) and oxaloacetate (4-C).
Acetyl-CoA is required in stoichometric amounts for each turn of the cycle and is obtained from:
•
Glucose – as explained in sections 1 and 2
•
Fatty acids – by β-oxidation (refer Ch 6)
Normally, OAA is present in the cell in very low concentrations. Since it is regenerated in every
round of the cycle, OAA is required only in catalytic amounts. However, the TCA cycle may
become deficient in its OAA supply if this keto-acid is pilfered by other metabolic pathways like
gluconeogenesis and transamination. In order to keep the cycle operating at a steady rate, the
system takes the help of anaplerotic reactions which replenish OAA, or other cycle
intermediates.
39
Pyruvate
+ H CO 3 +
_
PEP
PEP
+
Pyruvate
Glutamic
acid
+
+ CO2 +
pyruvate
carboxylas e
AT P
G DP
PEP
carboxy kinase
PEP
carboxylase
_
H CO 3
+ H CO 3 + N A D(
_
+
N A D( P )
+
OA A
+
P )H. H
+
OA A
OA A
A DP
+ GT P(
+
P i ( liver )
muscle )
P i ( higher plants, bacteria, yeast )
malic enzyme
glutamate
dehydrogenase
H2 O
+
a - K GA
Malat e
+
+ N A D(
N A D( P )
+
P ) H. H
+
+ NH3
Fig 5.3.5. Anaplerotic reactions that replenish intermediates of the TCA cycle. ( PEP = Phosphoenolpyruvate;
OAA = Oxaloacetate; a-KGA = α-Ketoglutarate)
The pyruvate carboxylase reaction is one of the most important anaplerotic reactions. Pyruvate
carboxylase is allosterically stimulated by acetyl-CoA and concomitantly increases production of
OAA from pyruvate when [acetyl-CoA] becomes high. Succinyl-CoA is produced by oxidation of
odd-chain fatty acids (see Chapter VI), and the catabolism of amino acids like Ileu, Met and Val.
Transamination and deamination reactions of amino acids are reversible and depending on
metabolic demand, they also replenish cycle intermediates (see Chapter VII).
The Glyoxylate cycle is an alternative pathway, which processes isocitrate without
decarboxylations, and can provide succinate, OAA and other intermediates of the TCA cycle. It
occurs in germinating seeds and some microbes. Unlike the TCA cycle, the glyoxylate cycle
enables net conversion of acetyl-CoA into 4-C intermediates.
Four C atoms enter the cycle as two molecules of acetyl-CoA and four C atoms leave as succinate.
Only one molecule of NADH.H+ is produced per turn of the cycle.
40
Acetyl - CoA
+
N A D H. H
CoA
Citrat e
OA A
H2 O
+
NAD
Iso citrat e
Malat e
CoA
malate
synthas e
Acetyl - CoA
isocitrat e
lyase
H2O
GLYOXYLATE
Succinat e
C O OH
_
C
O
Fig 5.3.6. The glyoxylate cycle in plant glyoxysomes.
ROLE OF VITAMINS
Four vitamins of the B-complex group are essential constituents of co-factors used in the TCA
cycle:
•
Riboflavin – for FAD, used by α-KGA-DH, SDH and also PDH
•
Niacin – for NAD, used by IDH, α-KGA-DH, MDH and also PDH
•
Thiamin (TDP) – used by α-KGA-DH and also PDH
•
Pantothenic acid – is a part of Coenzyme A which carries the acetyl and succinyl groups
ACTION OF INHIBITORS
Malonate competes with succinate and inhibits SDH. Accumulation of succinate in a malonicinhibited system stops the TCA cycle. Tissue preparations inhibited by malonate, continue with
the cycle if stoichometric amounts of fumarate/malate or OAA are added but not if the
tricarboxylic acids or α-KGA are provided.
Fluoroacetate combines with OAA to form fluorocitrtate, which inhibits aconitase. Citrate
accumulates in such a system and the TCA cycle is suspended.
Arsenite complexes with –SH group of lipoamide to inhibit α-KGA-DH complex so that α-KGA
accumulates and the cycle is stopped.
METABOLIC ROLE OF THE TCA CYCLE
The TCA cycle has a pivotal role in metabolism. It is essentially amphibolic and is connected to
several catabolic as well as anabolic pathways. The 8 intermediates in the cycle are links to
metabolites in other metabolic pathways.
Catabolic role:
The citric acid cycle oxidizes carbohydrates, lipids and amino acids. The 2-C, 4-C and 5-C endproducts of other catabolic processes undergo degradation when fed into the cycle as acetyl-CoA,
41
succinyl-CoA or any of the other intermediates. The C-skeleton is oxidized to CO 2 while the
hydrogen is finally passed on to molecular oxygen to form water. We take below an example of
the amino acid Isoleucine:
Propionyl - CoA
Isoleucine( 6 - C )
+ Acet yl - CoA + CO2
TC A cycl e
CO 2
2 CO 2
Succinyl - CoA
TC A cycl e
OA A
PEP
carboxy kinase
PEP
+ CO 2
pyruvate kinase
Pyruvate
PDH compl e x
Acet yl - CoA
+ CO 2
TC A cycl e
2 CO 2
Fig 5.3.7. Catabolic role of the TCA cycle as shown in the metabolism of the carbon skeleton of Isoleucine. The C
skeleton is traced in red (OAA = oxaloacetate; PDH complex = pyruvate dehydrogenase complex; PEP =
phosphoenol pyruvate)
42
Anabolic role
Glucose
PEP
Ser, Gly , Try
Cys , Phe , Tyr
Fatty acids , sterols
Acetyl - CoA
OA A
CITRATE
Asp , Arg
Gln , Pro , Arg
CITRIC ACID
Pyrimidines
CYCLE
a - KGA
SUCCINYL CoA
Glu
Purines
Porphyrins
Heme
Fig 5.3.8. Schematic diagram of the anabolic role of the TCA cycle. Abbreviated names of the amino acids have
been used: PEP = Phosphoenolpyruvate; OAA = Oxaloacetate; a-KGA = α-Ketoglutarate. (Adapted
from Nelson and Cox, 2005, p 617 fig 16-15)
The cycle is a major source of precursors for many biosynthetic pathways:
•
Gluconeogenesis – all major acids from citrate to OAA can undergo gluconeogenesis to
form glucose. The key enzyme required is PEP-carboxykinase. The acids enter the TCA
cycle from various sources, the chief one being OAA from pyruvate (using pyruvate
carboxylase). The products leave the mitochondrion via malate for gluconeogenesis in the
cytosol. (refer Section 6)
•
Synthesis of amino acids – the C-skeleton of cycle intermediates are a source for
synthesis of non-essential amino acids. Transamination and deamination reactions are
reversible and ideal for this purpose.
43
Reversal of the glutamate dehydrogenase reaction:
a - K GA
+
+
N A D( P ) H . H
+ N H3
glutamate
dehydrogenase
Glutamic
acid
+
+
N A D( P )
+
H2 O
Transaminations:
+ Alanine
a - K GA
OA A
+ Alanine
glutamate
amino transferase
Glutamat e
alanine
amino transferase
Aspartat e
+ Pyruvate
+ Pyruvate
Fig 5.3.9. Synthesis of amino acids from intermediates of the TCA cycle.
Fatty acid and cholesterol synthesis – is linked to citrate of the TCA cycle. The enzymes for
fatty acid synthesis are located in the cytosol. A citrate transporter conveys mitochondrial citrate
to the cytosol where the enzyme ATP-citrate lyase cleaves it to provide acetyl-CoA for fatty acid
synthesis
Fig 5.3.10.
TCA cycle and fatty acid synthesis.
(Source: Murray et al, 2003, p 135 fig 16-5)
•
Purine and pyrimidine nucleotides – are synthesized from α-KGA and OAA
•
Porphyrin ring of heme groups – are synthesized from succinyl-CoA and used in
synthesis of hemoglobin, myoglobin and cytochromes
44
REGULATION OF TCA CYCLE
The TCA cycle is at the junction of many major metabolic pathways and regulation of its activity
is crucial to the well-being of an aerobic organism. The rate of the TCA cycle is primarily geared
to the energy needs of the cell at any particular point in time. The regulation of the PDH complex,
as also that of the –oxidation of fatty acids, are major determinants of the rate of provision of
acetyl-CoA to the cycle. The factors that regulate the TCA cycle and the PDH complex are similar
in many respects so that the two processes are co-ordinated.
A T P, acet yl -CoA , N A D H, fatty acids
+
+
A M P, CoA , N A D , C a 2
N A D H, succinyl - CoA
citrat e , A T P
+
_
_
PDH complex
Pyruvate
Acet yl
- CoA
citrat e syn thas e
+
CITRATE
OA A
MALATE
A DP
ISOCITRATE
I DH
A T P, N A D H
succinyl - CoA
_
+
FUMARATE
_
OA A
A D P, C a 2 +
a - KGA
SDH
Ca2 +
+
SUCCINATE
SUCCINYL CoA
a- KGA- D H
complex
_
NA DH
succinyl - CoA
Fig 5.3.11. Regulators of the citric acid cycle: green signs indicate stimulation and red signs indicate inhibition.
(PDH = pyruvate dehydrogenase; IDH = isocitrate dehydrogenase ; α-KGA-DH = α-ketoglutarate
dehydrogenase; SDH = succinate dehydrogenase)
The rate-determining steps are the 3 exergonic reactions catalyzed by citrate synthase (CS), IDH
and α-KGA-DH. The mechanism of regulation depends on local molecules in the cell, many of
which are part of the cycle itself. Regulation is therefore quick, effective and in tune with the
existing needs of the cell. Surprisingly, covalent modification of the regulatory enzymes by the
phosphorylation-dephosphorylation cycle, does not take place. In addition, hormones have no
direct role in regulating the cycle.
There are three fairly simple means by which the TCA cycle is regulated:
o Substrate availability
o End-product inhibition
o Competitive feedback inhibition
45
Substrate availability is a key factor in determining whether the cycle can fulfill its purpose. The
supply of acetyl-CoA, OAA and NAD+, is particularly important. The supply of acetyl-CoA is
determined by the activity of the PDH complex and β-oxidation of fatty acids, while the continued
availability of OAA is ensured, if necessary, through anaplerotic reactions. Thus, if [acetyl-CoA]
is high but availability of OAA is limited (by diversion into other metabolic pathways), then high
[acetyl-CoA] stimulates pyruvate carboxylase allosterically to increase OAA production from
pyruvate. When the rate of glycolysis is greater than the rate of the TCA cycle, accumulating
citrate inhibits PFK-1. In this way, the production and utilization of acetyl-CoA is balanced so that
the TCA cycle can proceed at the required rate. If TCA is inhibited at some other step (e.g. by
NADH), increased OAA does not accelerate the cycle; instead OAA equilibrates with malate and
is transported out of the mitochondrion.
End-product inhibition is a direct inhibition of an enzyme by accumulation of the products of the
reaction catalyzed by it. All three regulatory enzymes of the TCA cycle are inhibited in this way
by mass action. Thus:
•
CS is inhibited by high [citrate]
•
IDH is severely inhibited by increased [NADH]
•
α-KGA-DH is severely inhibited by high [NADH] and by [succinyl-CoA]
The concentrations of the end-products not only affect their own specific enzymes but also result
in a “domino” effect on other enzymes.
Feedback inhibitions are caused by intermediates which are products of later reactions. Thus, CS
and IDH are inhibited by succinyl-CoA, which is a product of a subsequent step of the cycle.
Succinyl-CoA competes with OAA for citrate synthase. Inhibition of CS by NADH, and of IDH
by ATP are also examples of feedback inhibition.
Some of the molecules regulating the enzymes are allosteric modulators:
•
high [ADP] – activates CS and IDH
•
high [ATP] – inhibits CS and IDH
•
Ca2+ release – which signals muscle contraction, stimulates PDH, IDH and α-KGA-DH so
that increase in rate of TCA cycle makes more ATP available for muscle contraction
•
Long-chain acyl CoA – inhibit CS
The rates of all the reactions producing NADH are dependent on the availability of NAD+, which
in turn depends on re-oxidation of NADH in the respiratory chain. High ratio of [NADH]/[NAD+]
inhibits all three regulatory enzymes of the cycle as well as the PDH complex.
The rate of the TCA cycle is closely linked to glycolysis and the electron transport chain.
Glycolysis also responds to the cellular levels of ATP, NADH and citrate, so that the provision of
pyruvate matches the rate of its utilization in the TCA cycle. When the energy state of the cell is
high, the [ADP] available is low. This reduces the rate of oxidative phosphorylation and hence,
the rate of re-oxidation of NADH. The consequent reduction in the supply of NAD + decreases the
rate of the TCA cycle. Thus, the TCA cycle is under “respiratory control”.
Evidence now shows that some enzymes of the citric acid cycle may be associated as
supramolecular complexes (metabolons) which enable more efficient substrate channeling during
reaction sequences. Obviously mechanisms regulating the citric acid cycle need further
elucidation.
46
SUMMARY 5.3: CITRIC ACID CYCLE
The citric acid cycle is a major amphibolic pathway which occurs in the mitochondrion. It is a
crucial metabolic pathway which accounts for the final oxidation of carbohydrate, lipid and
protein in aerobic organisms. Acetyl-CoA, a common end-product in intermediary metabolism,
condenses with oxaloacetate and enters the cycle as citrate. In every turn of the cycle, a series of
dehydrogenases degrade a citrate molecule, oxidizing two carbon atoms to carbon dioxide and
reducing the co-enzymes NAD and FAD. OAA is regenerated to continue the cycle.
The location of the citric acid cycle is in close proximity to the mitochondrial electron transport
system. The reduced co-enzymes produced in the cycle, yield ATP when passed through this
respiratory chain.
Several catabolic and anabolic pathways are linked to intermediates of the citric acid cycle.
Anaplerotic reactions replenish cycle intermediates which are diverted to other pathways.
The availability of substrates and the concentrations of end-products regulate enzymes of the citric
acid cycle.
Chapter 5 Section 4
HEXOSE MONOPHOSPHATE PATHWAY (HMP)
(Pentose phosphate pathway/Hexose monophosphate shunt)
The hexose monophosphate pathway is an alternate route for glucose oxidation. Its main purpose
is to generate reducing power as NADPH.H+ and not energy. It occurs in those tissues/cells
which require:
•
NADPH for
o (a) synthesis of fatty acid/cholesterol (e.g. liver, adipose tissue, adrenal, gonads)
o (b) detoxification (e.g.erythrocytes)
•
Ribose 5-phosphate for nucleic acid synthesis when mitotic activity is high (e.g. skin)
A single run through the hexose monophosphate pathway achieves a partial oxidation of glucose
without any production of ATP. Complete oxidation of glucose is possible only by a multicyclic
process in which repetitions of the pathway and links with glycolysis are necessary.
47
Fig 5.4.1 Overview of the hexose monophosphate pathway (Source: Nelson and Cox, 2005, p 550 fig 14-20)
SEQUENCE OF REACTIONS
The HMP takes place entirely in the cytosol. The reactions can be grouped into two major phases:
•
Oxidative – in which glucose (6-C) is oxidized to pentose (5-C) and CO2, while NADP+ is
simultaneously reduced to NADPH. The process is irreversible.
•
Non-oxidative – involves a series of recombinations of 7-C, 5-C, 4-C and 3-C sugar
isomers, without use of NADP+. The process is reversible.
1. Reactions of the Oxidative phase
Glucose enters HMP pathway as glucose 6-phosphate (Glc 6-P) and its oxidative
decarboxylation is carried out by a sequence of four reactions. The overall equilibrium for this
phase lies far to the right.
48
Fig. 5.4.2.
Reactions of the oxidative phase of the HMP pathway. The four reactions of this phase are
explained in the text. Three of the reactions are shown here. The fourth reaction, in which ribulose 5-phosphate is
isomerised to ribose 5-phosphate, is shown in Fig 5.4.4. (Adapted from Murray et al, 2003, p165 fig 20-2)
Reaction 1 (oxidation): is catalyzed by glucose 6-phosphate dehydrogenase (Glc 6-P-DH), which
carries NADP as coenzyme. Glucose 6-P is oxidized at C-1 to an intramolecular ester, 6phosphoglucono-δ-lactone, while NADP is reduced to NADPH. The reaction is irreversible under
physiological conditions.
Reaction 2 (hydration): The enzyme, lactonase,
phosphogluconolactone to an acid, 6-phosphogluconate.
uses
water
to
convert
the
6-
Reaction 3 (oxidation): is catalyzed by 6-phosphogluconate dehydrogenase, which also has
NADP as its coenzyme. Removal of hydrogen from C-3 of 6-phosphogluconate produces 3-keto,
6-phosphogluconate and NADPH. The keto acid is unstable and undergoes spontaneous
decarboxylation to form ribulose 5-phosphate.
Reaction 4 (isomerization): Ribulose 5-phosphate (a ketose) is isomerized to ribose 5-phosphate
(an aldose) by ribulose 5-phosphate isomerase.
At this stage the HMP pathway is terminated in those tissues which require both NADPH and
ribose 5-P in balanced amounts.
NET YIELD:
2 NADPH AND 1 PENTOSE 5-PHOSPHATE PER MOLECULE OF GLUCOSE
49
2. Reactions of the non-oxidative phase
The reactions of the non-oxidative phase follow the oxidative phase in non-dividing tissues which
require more
NADPH than ribose 5-P. A series of reversible reactions constitute this phase with the final goal
of producing glucose 6-P or glycolytic intermediates from pentose phosphates. The main enzymes
here are transketolase and transaldolase, which transfer C-2 and C-3 moieties respectively from a
ketose donor to an aldose acceptor.
RIBOSE- 5 P
SEDOHEPTULOSE -7P
FRUCTOSE - 6 P
RIBULOSE - 5 P
XYLULOSE - 5 P
GLYCERALDEHYDE - 3 P
ERYTHROSE- 4 P
FRUCTOSE - 6 P
Another
XYLULOSE - 5 P
GLYCERALDEHYDE - 3 P
Fig 5.4.3. Summary of the non-oxidative phase of the HMP pathway. Fructose 6-phosphate and glyceraldehyde 3phosphate can enter the pathways of glycolysis or gluconeogenesis.
We break up the non-oxidative sequence into 4 parts to enable a clear understanding of the
reactions. All through these molecular interchanges it would help to remember that only C-1 to C3 of the molecules are involved.
A. Interconversion: (C5 ↔ C5 ↔ C5)
Ribose 5-P
Ribulose 5-P
Xylulose 5-P
Fig 5.4.4. Interconversion of pentose phosphates. Compare the enclosed functional groups in ribose 5-P and xylulose
5-P with equivalent positions in ribulose 5-phosphate.
50
Interconversion of ribose 5-P, ribulose 5-phosphate, and xylulose 5-P is readily catalyzed by the
enzymes isomerase and epimerase. This is necessary since both transketolase and transaldolase
use ketose sugars as group donors.
B. Recombination 1: (C5 + C5 ↔ C3 + C7)
Xylulose 5-P
Ribose 5-P
Glyceraldehyde 3-P
Sedoheptulose 7-P
Fig 5.4.5. Action of transketolase, showing the transfer of a 2-C unit (enclosed in green) transferred by the enzyme
from a 5-C ketose to a 5-C aldose.
This is the 1st reaction catalyzed by transketolase. The enzyme transfers a 2-C unit (activated
glycolaldehyde moiety) from a ketose donor (xylulose 5-P) and attaches it to the C-1 of an aldose
acceptor (ribose 5-phosphate). The 5-C sugar is thereby upgraded to a 7-C sugar, sedoheptulose 7P. The second product, glyceraldehyde 3-P, is an important intermediate shared by glycolysis,
HMP, gluconeogenesis and photosynthesis. Transketolase requires TPP and Mg2+ for its activity.
The two molecules of pentose phosphate used in this reaction, are obtained from the processing of
two molecules of glucose 6-P in the oxidative phase.
C. Recombination 2: (C7 + C3 ↔ C4 + C6)
Sedoheptulose 7-P Glyceraldehyde 3-P
Erythrose 4-P
Fructose 6-P
Fig 5.4.6. Action of transaldolase, showing the 3-C unit (enclosed in green) transferred by the enzyme from a 7-C
ketose to a 3-C aldose.
51
A transaldolase transfers a 3-C unit, dihydroxyacetone moiety, from sedoheptulose 7-P (ketose)
to glyceraldehyde 3-P (aldose), producing erythrose 4-P and fructose 6-P. While continues into the
final step of HMP, fructose 6-P can enter glycolysis or the gluconeogenic pathway.
D. Recombination 3: (C5 +C4 ↔ C3 + C6)
Xylulose 5-P
Erythrose 4-P
Glyceraldehyde 3-P
Fructose 6-P
Fig 5.4.7. Another reaction catalyzed by transketolase to transfer a 2-C unit from a ketose to an aldose.
Transketolase catalyzes a 2nd transfer of a 2-C unit from xylulose 5-P to erythrose 4-P, yielding the
final products fructose 6-P and glyceraldehyde 3-P. It is to be remembered that the availability of
a 2nd molecule of xylulose 5-P for this reaction indicates that a third molecule of glucose 6-P was
utilized as its source.
OVERALL REACTION
3 GLUCOSE 6-P + 6 NADP+ + 3 H2Oà
3 CO2+2 FRUCTOSE 6-P+ GLYCERALDEHYDE 3-P + 6 NADPH.H+
The 2 molecules of fructose 6-P can be isomerized to glucose 6-P to re-enter the HMP shunt, or
can be diverted to glycolysis. Glyceraldehyde 3-P can enter either glycolysis or gluconeogenesis.
In this way the HMP pathway becomes a link to glycolysis and gluconeogenesis for dietary
pentoses and other sugars.
The HMP pathway is never a route for the complete oxidation of glucose in metabolism. However
since the final products fructose 6-P and glyceraldehyde 3-P, can be reconverted to glucose 6-P, it
is possible for a 6-C unit (equivalent to glucose 6-P) to be repeated re-cycled, with release of 6
CO2.
REGULATION OF HMP
Glucose 6-P is processed by HMP or glycolysis as per the current need of the cell. The reactions
of the HMP, glycolysis and gluconeogenesis occur in the cytosol and share common intermediates
like glyceraldehyde 3-P. The fate of the triose phosphates is determined by the cell’s need for
pentose phosphates, NADPH and ATP.
52
The 1st reaction of the oxidative phase, catalyzed by glucose 6-P dehydrogenase, is irreversible
and rate-limiting for the whole pathway. Control is mainly by the availability of NADP+: high
levels of NADP+ stimulate glucose 6-P dehydrogenase allosterically. When the cell uses NADPH
(e.g. in lipid synthesis), the high [NADP+] stimulates the dehydrogenase and increases the rate of
HMP. The rate of the non-oxidative branch of the pathway depends on the availability of
substrates.
Fig 5.4.8.
Role of NADPH in regulation of HMP pathway (Source: Nelson and Cox 2005, p 554 fig 14-27)
The relative requirements of NADPH and ribose 5-P within the cell determines the actual
sequence of the reactions:
1. Need for NADPH more than for ribose 5-P (e.g. adipose tissue)
Fig 5.4.10a. Mode of HMP pathway when requirement for NADPH is more than for ribose 5-phophate
(Source: Berg et al, 2002, fig 20.24)
A 6-C unit (equivalent of glucose 6-P) is completely oxidised to CO2 by repeated passages
through the HMP. Both oxidative and non-oxidative branches of HMP take place, followed by
53
channeling of fructose 6-P and glyceraldehyde 3-P into gluconeogenesis to give more glucose 6-P
for continuing HMP. The overall stoichometry of the sequence is:
6 Glucose 6-P + 12 NADP+ + 7 H2O à 5 Glucose 6-P + 6 CO2 + 12 NADPH + 12 H+ + Pi
2. Need for ribose 5-P more than for NADPH (e.g. skin)
Fig 5.4.10b Mode of HMP pathway when requirement of ribose 5-phophate is more than for NADPH
(Source: Berg et al, 2002, fig 20.24)
Most of the glucose 6-P is processed by glycolysis to give fructose 6-P and glyceraldehyde 3-P,
following which the reverse reactions of transaldolase and transketolase convert these
intermediates to ribose 5-P. The oxidative part of the pathway is not involved. This occurs in
rapidly dividing tissue.
5 Glucose 6-P + ATP à 6 Ribose 5-P + ADP + H+
3. Requirement for NADPH and ribose 5-P is balanced
Fig 5.4.10c Mode of HMP pathway when requirement of ribose 5-phophate balances that for NADPH
(Source:Berg et al, 2002, fig 20.24)
The oxidative part of HMP is predominant over the non- oxidative part and generates NADPH and
ribose 5-P.
Glucose 6-P + 2 NADP+ + H2O à Ribose 5-P + 2 NADPH + 2 H+ + CO2
54
4. NADPH required but ribose 5-P is not needed
Fig 5.4.10d. Mode of HMP pathway when only NADPH is required (Source: Berg et al, 2002, fig 20.24)
Glyceraldehyde 3-P and fructose 6-P, produced by transaldolase and transketolase reactions, enter
glycolysis and undergo complete oxidation; ATP is generated.
3 Glucose 6-P + 6 NADP+ + 5 NAD+ + 5 Pi + 8 ADP
à
5 Pyruvate + 3 CO2 + 6 NADPH + 5 NADH + + H+ + 8ATP + H2O
SIGNIFICANCE OF HMP
•
Provides NADPH for syntheses of fatty acids, steroids, amino acids, nucleotides and
neurotransmitters
•
NADPH protects RBC from oxidative damage and hemolysis caused by H2O2. The
peroxide is eliminated by a tripeptide, reduced glutathione, which gets oxidized in the
process. NADPH enables regeneration of reduced glutathione. A hereditary lack of glucose
6-phosphate dehydrogenase causes hemolytic anemia, particularly if anti-malarial
drugs are administered.
Fig 5.4.11a. Reduction of glutathione (Source: Murray et al, 2003, p 167 fig 20-3)
55
Fig. 5.4.11b. RBC showing Heinz Bodies (dark particles) which are clumps of denatured protein formed due to
deficiency of glucose 6-phosphate dehydrogenase (Source: Berg et al, 2002, fig 20.25)
•
NADPH is required for detoxication of cytochrome P450 monooxygenases
•
NADPH is required for bactericidal activity of polymorphonuclear leucocytes
•
Ribose 5-P is used in nucleotide synthesis (for RNA, DNA, ATP, NAD+, FAD and CoA)
•
Excess pentose sugars in the diet can enter mainstream glucose metabolism
•
Fructose 6-P and glyceraldehyde 3-P can enter glycolysis or gluconeogenesis
SUMMARY 5.4: HEXOSE MONOPHOSPHATE PATHWAY
The hexose monophosphate pathway partially oxidizes glucose in the cytosol. Its main purpose is
to reduce NADP to NADPH. for fatty acid synthesis in tissues. It also provides ribose for nucleic
acid synthesis but does not generate ATP.
The pathway involves irreversible oxidative and reversible non-oxidative phases. The oxidative
phase decarboxylates glucose to ribulose and reduces NADPH. The non-oxidative phase carries
out a series of recombinations finally yielding fructose 6-phosphate and glyceraldehyde 3phosphate that can enter glycolysis, undergo reversal of reaction sequences to produce ribose or
glucose.
Chapter 5 Section 5
GLYCOGEN METABOLISM
The large reservoir of glycogen in the liver and muscle is a readily moblizable source of glucose
for the body in the periods between meals and at times of increased muscular activity. This form
of storage energy scores over fat stores on two major counts viz. speed of mobilization, and both
aerobic and anaerobic utilization. In addition, glycogen is a source of essential glucose to those
organs that cannot use lipids as energy fuel e.g. RBC and nerve cells. On the other hand, when
blood glucose levels go up after a carbohydrate meal, the excess glucose is trapped by glycogen
synthesis to be used later when required.
56
Fig 5.5.1. Glycogen granules in the cytoplasm of a hepatic cell (Source: Berg et al, 2002, fig 21.2)
The synthesis and degradation of glycogen is well co-ordinated so that blood glucose is
maintained at the steady levels vital for all organs. Both processes occur in the liver and muscle,
but there is a fundamental difference between them: the liver responds to the levels of glucose in
systemic circulation, while the muscle responds to its own need of glucose.
We pursue our study of glycogen metabolism under three sub-sections:
•
Glycogenolysis – the catabolic process of breakdown of glycogen to glucose
•
Glycogenesis – the anabolic process of synthesis of glycogen from glucose
•
Reciprocal regulation of glycogenolysis and glycogenesis – which enables control of
blood glucose levels
For the first time in your perusal of regulatory mechanisms, you will encounter in this section
details of the influence of hormones on metabolism. Remember that hormones are secreted by
endocrine glands on stimulation by external /internal factors. They trigger cellular signals to
integrate metabolism with the needs of the body. Epinephrine, glucagon and insulin play a major
role in glycogen metabolism, sensitizing it to the internal and external environment.
In this section you will also learn about enzyme cascade systems. The binding of specific
hormones to membrane receptors on target cells can initiate a sequence of enzyme-catalyzed
reactions, in which catalysts (i.e. enzymes) successively activate other catalysts (also enzymes).
The purpose is to ensure a large amplification of the initial signal. The binding of a few
molecules of hormone (e.g epinephrine) is the primary signal and it precipitates a massive
chemical response (e.g. glycogenolysis) by acting through enzymes that amplify the response at
each intermediate step. The process generally involves second messengers in hormone action like
cyclic 3’,5’-AMP (cAMP) or inositol 1,4,5-triphosphate (IP3).
57
Fig 5.5.2. Enzyme cascade systems (on left) amplify signals that stimulate glycogenolysis and provide large
quantities of glucose for energy (Source: Berg et al, 2002, p 866)
Section 5.5.A
GLYCOGENOLYSIS
Glycogen is stored as cytosolic granules in association with the enzymes and regulatory proteins
that catalyze both its degradation and synthesis. Recall that the glycogen molecule is a highly
branched homoglycan in which glucose molecules are linked by α-glycosidic bonds to form linear
(1:4) and branched (1:6) chains. Glycogenolysis is initiated at the non-reducing ends of linear
chains that are exposed to the exterior. The structure of the molecule ensures that glycogenolysis
can start simultaneously at many such ends.
Fig 5.5.3.
Schematic diagram of a glycogen molecule, showing non-reducing terminal glucosyl residues that are
targeted by glycogen phosphorylase (Source: Berg et al, 2002, fig 21.1)
Steps of glycogenolysis
Glycogenolysis occurs in the cytosol and glucose is liberated by the sequential action of 3-4
enzymes:
•
Phosphorylase – cleaves 1:4 α-glycosidic bonds
•
“Debranching” enzyme – with two enzymatic functions in the same molecule viz.:
58
* oligo (α-1:4à α-1:4) glucan transferase – transfers a trisaccharide moiety from
one glycosidic chain to an adjacent chain
* α -1:6 glucosidase – cleaves 1:6 α-glycosidic bonds
•
Phosphoglucomutase – transforms Glucose 1-P to Glucose 6-P
•
Glucose 6-phosphatase – removes phosphate group from Glucose 6-P
The first three enzymes are functional in both muscle and liver, but the last enzyme is found only
in the liver.
Step 1: The breakdown of glycogen is initiated by phosphorylase. The enzyme cleaves 1:4 αglycosidic bonds, starting from the non-reducing ends of the molecule. Recall from Chapter 2
Section 1 that each glycogen molecule has several peripheral and easily accessible non-reducing
ends.
Fig 5.5.4. Schematic flow diagram of the steps in glycogenolysis. Two linear chains of the glycogen molecule
(CORE) have been shown, connected by a branch-point. Phosphorylase action starts from the free, nonreducing end of each chain (Source: Berg et al, fig 21.4)
Phosphorylase enables Inorganic phosphate to split the 1:4 bond by phosphorolysis, resulting in
the release of one molecule of glucose 1-phosphate from each terminal residue attacked. Pyridoxal
phosphate (PLP) is an essential co-factor for the enzyme and participates in the transfer of the
phosphate group.
In terms of energetics, phosphorolysis is more advantageous than hydrolysis, since glucose is
released as Glucose 6-P and does not require ATP to enter the glycolytic pathway.
59
Fig 5.5.5. Removal of a terminal glucose residue as glucose 1-phosphate from a linear chain of glycogen by the
action of glycogen phosphorylase
Phosphorylase catalyzes step-wise removal of glucose units from linear portions of the glycogen
molecule until it approaches within four units of α-1:6 branch points. Phosphorylase cannot cleave
the 1:6 α-glycosidic bonds and its action stops near such branch-points. Hence, phosphorylase per
se can degrade only about 55% of the glycogen molecule, leaving a highly-branched residue
called “limit dextrin”.
Step 2: The oligo (α-1:4à α-1:4) glucan transferase activity of the “de-branching enzyme” now
targets the partially degraded chains. A trisaccharide unit, attached to the 1:6-linked glucose
molecule of each partially degraded chain, is transferred to the non-reducing end of a different
chain. The single glucose unit (shaded green in Fig 5.5.4.) at the 1:6 branch-point of the donor
chain is thus exposed, while the 2nd chain is lengthened by more 1:4 α-glycosidic bonds on which
phosphorylase can continue its action.
Step 3: The exposed glucose unit at the 1:6 position is removed hydrolytically by the α -1:6
glucosidase activity of the “de-branching enzyme”. Note that glucose and not glucose 1-P is
released by this action.
Step 4: The major product of glycogenolysis at this stage is glucose 1-P (and some free glucose),
which can neither enter glycolysis directly, nor leave the cell. The action of phosphoglucomutase
transforms glucose 1-P to glucose 6-P and enables its entry into glycolysis in both liver and
muscle (See Chapter 5 Section 1). Glycogenolysis thus provides skeletal muscle with a local
supply of glucose as energy fuel to support muscular contractions.
Step 5: occurs only in the liver. To fulfill its obligation of supplying glucose to other tissues of the
body, the liver uses another enzyme, glucose 6-phosphatase, to detach the phosphate group from
60
Glu 6-P and release free glucose into the blood. This enzyme is present only in the cells of the
liver (and kidney) but not in muscle, brain and adipose tissue. Consequently, the liver can make
glucose available from its stores to other tissues of the body but the muscle cannot do so.
Glucose 1 - P
phospho glucomutase
Glucose 6 - P
glucose
6 - phosphatase
H2 O
GLUCOSE
To BLOOD
Pi
It is interesting to know how the hepatic cell compartmentalizes and separates the action of
glucose 6-phosphatase and phosphohexose isomerase (the next enzyme in glycolysis) on the same
substrate i.e. glucose 6-phosphate. The isomerase is in the cytosol while the phosphatase is an
integral membrane protein of the endoplasmic reticulum (ER) with its catalytic surface facing the
ER lumen. A series of specific membrane transporters are brought into play. Glucose 6-P is
carried from the cytosol into the ER lumen by a transporter (T1), hydrolyzed there, returned to
cytosol by another transporter (T2), and then carried across the plasma membrane of the
hepatocyte to the blood by the transporter GLUT2.
Fig 5.5.6. Schematic diagram to show the hydrolysis of glucose 6-phosphate in a hepatic cell and release of glucose
into the blood (Source: Nelson and Cox, 2005, p 564 fig 15-6)
Fates of Glucose 6-phosphate
As indicated in the text so far, glucose 6-P can be directed into many routes of carbohydrate
metabolism. Glycolysis yields pyruvate and ATP from glucose 6-P, while the HMP pathway
produces pentose phosphate and NADPH. Glucose 6-P can be used in the syntheses of glycogen,
other sugars and glycocojugates. On the other hand, the action of glucose 6-phosphatase
hydrolyzes glucose 6-P to liberate free glucose into the blood for uptake by extra-hepatic tissues.
61
Fig 5.5.7. Fates of glucose 6-phosphate produced by glycogenolysis in liver and muscle.
(Source: Berg et al 2002, fig 21.3)
REGULATION OF GLYCOGENOLYSIS
Glycogen phosphorylase (PL) is the target enzyme for regulation of glycogenolysis. It is a
dimer, composed of two identical sub-units. One serine residue (Ser14) on each sub-unit can
undergo reversible phosphorylation. The structure of the subunits is rather unique. Each subunit
has four sites: a glycogen-binding (‘docking’/‘storage’) site, a catalytic site which is about 30
Angstroms away, an allosteric site and a cofactor (PLP)-binding site. The narrow crevice which
forms the glycogen-binding site, can accommodate only a linear chain of 4-5 glucose residues.
This explains why the enzyme is unable to act on the branched portions of the glycogen molecule.
At the same time the ‘docking’ of many glucosyl residues ensures better catalytic efficiency since
the substrate need not be completely associated or dissociated between catalytic cycles.
62
Fig 5.5.8. A ribbon diagram of glycogen phosphorylase. The two sub-units are shown in black and yellow. Each
catalytic site includes the cofactor PLP (pyridoxal phosphate). The yellow circle is the binding region
for Pi (inorganic phosphate). (Source: Berg et al 2002, fig 21.6)
Phosphorylase (PL) can exist in two forms:
i.
Phosphorylase ‘a’ – which is phosphorylated and is the active form
ii.
Phosphorylase ‘b’ – which is dephosphorylated and relatively inactive
Phosphorylation is brought about by the action of kinases viz. protein kinase and phosphorylase b
kinase, and utilizes ATP. Dephosphorylation is catalyzed by protein phosphatase-1 (PP-1) and
uses water.
Both phosphorylase a and b can adopt two different conformations:
i.
‘R’ or “relaxed’ conformation which is catalytically active
ii.
‘T ’or “tense” conformation which is catalytically inactive
63
Fig 5.5.9. Schematic diagram of the T (inactive) and R (active) forms of phosphorylase b and a, and the factors that
favor their existence. (Source: Voet and Voet, 1995, p 494 fig 17-9)
The R state of PL a (i.e active enzyme) is generally favored, unless glucose levels are high, while
PL b is mostly in the T state, unless AMP is high.
The activity of phosphorylase in liver and muscle is controlled by two mechanisms:
•
Hormonal: epinephrine and glucagon act through a cAMP-dependent enzyme cascade
pathway to activate PL by phosphorylation (i.e. covalent modification). This is the
preferred mode of regulation of PL under physiological conditions. The adrenals secrete
epinephrine, (for ‘fight or flight’), when the organism is under stress. The pancreas
secretes glucagon when blood levels of glucose are low, and insulin, when blood glucose
levels are high.
•
Allosteric: local ions/molecules (viz. AMP, Ca2+, glucose) in the cell bind to specific
allosteric sites and cause conformational changes that alter the activity of phosphorylase
Muscle and liver phosphorylases are isozymes and exhibit some differences in their regulatory
properties. We will, therefore, consider the regulation of phosphorylase activity separately in these
two organs.
1. Regulation of phosphorylase in the muscle
The activation of muscle phosphorylase is synchronized with muscle contraction. The hormonal
mechanism of regulation is initiated by epinephrine which is released when there is a need for
sudden and strong muscle activity. The action of one molecule of the hormone epinephrine (i.e.
the primary signal), finally leads to the activation of several molecules of the target enzyme,
phosphorylase. Such a mechanism is an enzyme cascade pathway.
64
Refer to Fig 5.5.9 as we trace the steps in the cascade mechanism for activation of glycogen
phosphorylase in the muscle.
Fig 5.5.10. Regulation of glycogen phosphorylase in the muscle by a cAMP-mediated enzyme cascade mechanism
Other factors in regulation of the target enzyme have also been shown. (Source: Murray et al, 2003, p 149 fig 18-6)
Step 1: Epinephrine binds to β-receptors on the cell membrane of myocytes to trigger a cAMPmediated cascade pathway for activating phosphorylase
Step 2: The binding of epinephrine activates a membrane-bound enzyme adenylyl cyclase, which
converts ATP to cyclic 3’,5’-AMP.
Step 3: Cyclic AMP binds to the enzyme protein kinase and activates it by removing its
regulatory subunits.
65
NH2
N
N
N
N
O
5'
CH2
O
H
H
O
P
O-
3'
O
H
H
OH
Fig 5.5.11. Structure of 3’,5’-cyclic AMP
Fig 5.5.12. The mechanism of activation of protein kinase by cyclic AMP: On left is the inactive holoenzyme, R2C2,
in which R and C are regulatory and catalytic sub-units respectively. In the inactive R2C2 complex, the
catalytic site of C is occupied by a ‘pseudosubstrate’, i.e. a pentapeptide sequence of the R chain which
prevents entry of the substrate. Allosteric binding of cAMP moves this sequence away so that C is now
free for binding and catalytic activity. (Source: Berg et al, 2002, fig 10.28)
Step 4: Active cAMP-dependent protein kinase (PKA) performs two functions:
• phosphorylates and fully activates phosphorylase kinase
• phosphorylates a small regulatory protein, inhibitor-1 which inactivates protein
phosphatase-1 (PP-1) This ensures that PP-1 cannot dephosphorylate and inactivate
both phosphorylase kinase and phosphorylase a. (In absence of active PKA, PP-1 will
dephosphorylate and inactivate both the enzymes).
Thus, both activation and inactivation of phosphorylase depend on presence or absence of cAMP
It is important to also note in Fig 5.5.9 that the enzyme phosphodiesterase can hydrolyze cAMP to
5’AMP and thus terminate hormone action within a cell.
Step 5: Activated phosphorylase kinase phosphorylates PL b to the active form, PL a, which then
starts the process of glycogenolysis.
66
Fig 5.5.13. Schematic representation of the phosphorylation of glycogen phosphorylase by phosphorylase kinase
and dephosphorylation by protein phosphatase-1. Organ-specific stimulatory effects (see text) of
epinephrine, glucagon, calcium ions and AMP on phosphorylase kinase have also been shown.
(Source: Nelson and Cox, 2003, p 584 fig 15-24)
The step-wise process of activation of phosphorylase depicted in Fig 5.5.12 (below) will now
enable you to understand the enzyme cascade mechanism. Notice that there have been 4
amplification steps in phosphorylase activation. Adenylate cyclase, protein kinase, phosphorylase
kinase and phosphorylase actions have followed in sequence, with each enzyme activating the
next enzyme in the sequence. Follow the estimated number of molecules shown at each step in the
figure. Remember that since an enzyme is a catalyst, every molecule of the enzyme is available
again for action at the end of every reaction. Notice also that only the enzymes per se have
undergone activation and remember that this is a reversible phenomenon.
67
Fig 5.5.14. The amplification of a primary hormonal signal by an enzyme cascade mechanism: An estimate of the
number of molecules produced at each step in the cascade has been shown. One molecule of
epinephrine finally activates 1,0000 molecules of the target enzyme, glycogen phosphorylase.
(Source: Nelson and Cox, 2003, p 585 fig 15-25)
Superimposed on the hormonal regulation of muscle phosphorylase is faster allosteric regulation
by:
•
AMP – During muscle contraction, the breakdown of ATP increases [AMP]. An allosteric
site in phosphorylase b attaches AMP and the enzyme is activated by a conformational
change without conversion to phosphorylase a.
•
Ca2+ – Calcium release is the signal for muscle contraction. Binding of Ca2+ activates
dephosphorylated phosphorylase kinase. The muscle enzyme is represented as (αβγδ)4.
Serine residues on the α and β subunits are phosphorylated by PKA. The δ subunit is
calmodulin and it binds four Ca2. The enzyme is fully active only when both
phosphorylation and Ca2+-binding have taken place
68
A.
B.
C.
Fig 5.5.15. Schematic diagram of the activation of phosphorylase kinase: the enzyme is only partly activated
by covalent modification (A: phosphorylation) or allosteric modulation (B: attachment of Ca2+ ).
Full activation requires both the mechanisms of activation (C) to occur simultaneously.
(Adapted from Berg et al, 2002, fig 21.13)
•
Glucose 6-P and ATP – High cellular concentrations of glucose 6-P and ATP inhibit PL
b: they prevent conformational change of PL b by attaching to its AMP-binding site.
Thus, regulation of phosphorylase ensures that at times of increased muscle activity,
glycogenolysis is stimulated and provides glucose. When muscle is at rest, ATP levels are
adequate and glycogenolysis is not required.
2. Regulation of Phosphorylase in the Liver
The mechanism of activation of phosphorylase in the liver is similar to that in the muscle with the
following differences that are in keeping with the role of the liver in carbohydrate metabolism:
•
Glucagon, secreted by the pancreas when blood glucose falls, can also initiate the cAMPdependent enzyme cascade pathway to activate phosphorylase. This ensures that hepatic
cells release essential glucose into the blood when the nutritional state is low. Glucagon is
ineffective in the muscle.
•
Vasopressin, oxytocin, angiotensin II and epinephrine stimulate glycogenolysis
through a phosphoinositide cascade pathway. The hormones bind to an α1-adrenergic
receptor in the plasma membrane and activate a G protein that stimulates phospholipase C.
The resulting increase in inositol 1,4,5-triphosphate (IP3) induces Ca2+ mobilization from
ER stores to the cytosol and activates phosphorylase kinase.
•
Allosteric regulation of phosphorylase is by glucose and not by AMP. When blood glucose
is high, glucose uptake in the hepatic cell is also increased. Glucose now binds to an
allosteric site on PL a, causing a conformational change that results in dephosphorylation
and inactivation of the enzyme by PP-1. When blood glucose falls, the allosteric inhibition
is removed and glycogenolysis starts again. Thus PL a is a “glucose sensor” in liver cells.
Fig 5.5.16. Schematic diagram of the conformational change in phosphorylase a caused by allosteric binding of
69
glucose. (Source: Nelson and Cox, 2003, p 585 fig 15-26)
•
Insulin, secreted by the pancreas when blood glucose is high, stimulates PP-1, which
inactivates both phosphorylase kinase and PL a. Insulin also increases the action of
phosphodiesterase so that cAMP is hydrolyzed. Thus insulin action is antagonistic to that
of glucagon.
Section 5.5.B
GLYCOGENESIS
Glycogenesis is the synthesis of glycogen from glucose. After a meal when the levels of blood
glucose are high and insulin is present, cells of the liver and muscle take up glucose to replenish
their glycogen stores. The reactions of glycogenesis are cytosolic, well-regulated and co-ordinated
with glycogenolysis.
Glycogen synthesis essentially involves step-wise attachment of glucose residues to a pre-existing
“glycogen primer” so that it increase in size. De novo synthesis of the glycogen molecule requires
a protein “primer” called glycogenin. The reactions are essentially similar in liver and muscle
though their regulation differs in detail in the two organs.
A. Steps in the synthesis of Glycogen by enlarging a “glycogen primer”
A “glycogen primer” is essentially a pre-existing α-1,4 glucan (i.e. amylose chains). There are
three steps in expanding this structure to obtain the highly branched glycogen molecule:
GLUCOSE
hexokinase /
glucokinase
ATP
Glucose 6 - P
phospho glucomutase
Glucose1- P
A DP
2 Pi
pyrophosphatase
UTP
pyrophophorylase
H O
2
PP i
U DP - Glucose
GLYCOGEN( n )
( primer )
glycogen synthase
UD P
GLYCOGEN( n + 1 )
( expanded primer )
Fig 5.5.17. Summary of the synthesis of glycogen from glucose by using ‘glycogen primer’.
Step 1: Conversion of glucose to UDP-glucose
Glucose is phosphorylated to Glucose 6-P by hexokinase /glucokinase (as in glycolysis) and then
isomerised to Glucose 1-P by phosphoglucomutase. The next enzyme, UDP-glucose
70
pyrophosphorylase, activates glucose by attaching UDP from UTP to Glucose 1-P. The reaction
products are UDP-glucose (UDPG) and pyrophosphate.
O
HN
CH O H
2
H
HO
O
H
OH
H
H
OH
O
H
O
O
P
O-
N
O
O
P
O
O-
CH2
H
O
H
H
H
HO
OH
Fig 5.5.18. Structure of UDP-Glucose (UDPG).
Rapid hydrolysis of pyrophosphate by pyrophosphatase keeps the overall equilibrium in favor of
UDPG formation, even though both mutase and pyrophosphorylase reactions are reversible. This
also prevents glycogenolysis from occurring by a reversal of the route of glycogenesis.
UDP-glucose serves as the donor of a glucosyl residue in the next step of glycogenesis.
Step 2: Attachment of UDPG to “glycogen primer”
Fig
5.5.19. Attachment of UDP-Glucose (orange) to the non-reducing end of a “glycogen primer” (yellow)
(Source: Lodish et al, 2003, p 548 fig 13-16)
This step is catalyzed by glycogen synthase, the main enzyme of glycogenesis. It transfers the
glucosyl residue from UDPG to the non-reducing end of a linear chain in the “glycogen primer”.
The attachment is by a 1:4 α-glycosidic bond and increases the linear chain-length by one glucosyl
residue. UDP is released and re-phosphorylated to UTP by nucleoside diphosphate kinase, using
ATP. Thus more glucose residues can be attached as in Step 1.
71
The net reaction at this stage is:
Glucose + (Glucose)n + 2ATP à (Glucose) n+1 + 2ADP +2 Pi
Glycogen synthase continues step-wise addition of more glucose residues on all linear chains of
the pre-existing “primer”. Physical proximity of glycogen synthase to the enlarging molecule
facilitates this attachment.
Step 3: Branching of linear chains
Fig 5.5.20. Schematic diagram of glycogenesis, showing detachment of an oligosaccharide unit from a newly
synthesized linear chain and re-attachment by an 1:6 α-glycosidic bond to form a branch-point.
(Source: Nelson and Cox, 2005, p 569 fig 15-9)
After a linear chain of at least 11-13 glucose residues has been formed, a terminal oligosaccharide
unit of 6-7 residues is detached and transferred to a more internal position on the same or a nearby
chain. The attachment is by an 1:6 α-glycosidic bond, thus creating a branch point. The enzyme
catalyzing this reaction is amylo 1:4à 1:6 transglycosylase or “branching” enzyme. The new
branch point is created at least 4 glucosyl residues away from any pre-existing branch point.
Glycogen synthase can now continue to add more glucosyl residues by 1:4 α-glycosidic bonds to
two non-reducing ends.
The final size of the glycogen molecule is attained by continued linear increase with 1:4 αglycosidic bonds and branching with 1:6 α-glycosidic bonds.
B. De novo synthesis of glycogen
Glycogenin is a protein “primer which initiates synthesis of a new glycogen molecule. It is a 37
kDa, self-glycosylating protein that first attaches a glucosyl residue from UDPG to the hydroxyl
group of a specific Tyrosine residue in its own peptide chain. Glycogenin then continues its
glucosyltransferase activity till a linear chain of 8 glucosyl residues, joined by 1:4 α-glycosidic
bonds, is obtained. The “primed” glycogenin can now be acted on by glycogen synthase and the
“branching” enzyme to obtain the final glycogen particle.
72
Fig 5.5.21. De novo synthesis of glycogen: a Tyrosine residue in the protein glycogenin (represented by the blue
oval) attaches glucosyl residues borne by UDP. Subsequently glycogen synthase and the branching
enzyme help to produce the final product, glycogen (green oval).
Fig 5.5.22. Initial interaction between a molecule of UDP-Glucose and Tyrosine residue of glycogenin
(Source: Nelson and Cox, 2005, p 570 fig 15-11)
73
Fig 5.5.23. Ribbon model of glycogenin: The red ball-and-stick structure represents the substrate, UDP-Glucose.
(Source: Nelson and Cox, 2005, p 569 fig 15-10)
Glycogen synthase is catalytically active only as long as it is in contact with glycogenin; this
restricts the size of the final glycogen molecule
REGULATION OF GLYCOGENESIS
Glycogen synthase (GS) is the target enzyme for regulation of glycogenesis. The enzyme can
exist in two forms (cf phosphorylase):
i.
Glycogen synthase ‘a’ – non-phosphorylated and active
ii.
Glycogen synthase ‘b’ – phosphorylated and relatively inactive
Notice that glycogen synthase is activated by dephosphorylation and inhibited by
phosphorylation. This is in contrast to. phosphorylase.
The mechanisms of regulation are both hormonal and allosteric, and operate in response to blood
and cellular levels of glucose:
Hormonal – reversible phosphorylation of glycogen synthase is the key to its control (cf
phosphorylase). The effective hormones are insulin and epinephrine/glucagon.
Allosteric – by Glc 6-P, Ca2+ and possibly glycogen itself
74
Fig 5.5.24. Cascade mechanism for activation/inactivation of glycogen synthase. Refer to the text for details.
(Source: Murray et al, 2003, p 150 fig 18-7)
GS is unique in that it can be phosphorylated i.e. inactivated (GSa à GSb) on several serine
residues by at least eleven different kinases! The most important among them is glycogen synthase
kinase-3 (GSK3), which strongly inhibits glycogen synthase by phosphorylating three Ser residues
near the carboxy-terminal end of the enzyme. GSK3 acts after prior “priming” of GS by another
protein kinase, casein kinase II.
The kinases that phosphorylate GSa, are in turn regulated by small local molecules like cAMP,
Ca2+ and DAG (diacylglycerol). High glycogen in tissues decreases GSa but the mechanism is not
understood.
75
Fig 5.5.25. Phosphorylation of glycogen synthase by GSK3 and its dephosphorylation by PP-1. The effect of
hormones on these two enzymes is also shown (Source: Nelson and Cox, 2005, p 586 fig 15-27)
In the liver, GS is dephosphorylated i.e. activated (GSb à GSa), by protein phosphatase-1 (PP1), which removes the same three phosphoryl groups attached by GSK3. The catalytic activity of
PP-1 is facilitated by allosteric binding of Glc 6-P. Association with a glycogen-targeting protein,
GM, brings PP-1 into close proximity with glycogen synthase and helps in catalysis. G M can be
phosphorylated in two different sites (1 and 2), and its action depends on which of these sites has
been phosphorylated.
In the muscle, a different phosphatase performs this function of dephosphorylating and activating
glycogen synthase.
Insulin stimulates glycogenesis by promoting dephosphorylation of GS in two ways:
•
binds to a membrane receptor, tyrosine kinase, and triggers a cascade involving protein
kinase B (PKB) to phosphorylate and inactivate GSK3
76
Fig 5.5.26. Mechanism of insulin-induced activation of GSK3 and consequent inactivation of glycogen synthase.
(Source: Nelson and Cox, 2005, p 587 fig15-29)
•
acts through an insulin-sensitive kinase to phosphorylate GM at site 1 so that it associates
with the glycogen particle and activates PP-1; subsequently PP-1 dephosphorylates and
activates glycogen synthase
Fig 5.5.27. Association of GM with enzymes in the glycogen particle: insulin (1) promotes association while
epinephrine (2) causes dissociation of GM and PP-1 (Source: Nelson and Cox, 2005, p588 fig 15-30 )
77
Epinephrine/Glucagon inhibits glycogen synthesis by favoring phosphorylation of GS in two
ways:
•
•
binds to a β-adrenergic membrane receptor to initiate a cAMP-mediated cascade that
stimulates protein kinase (PKA) (cf. phosphorylase regulation) (see Fig 5.5.22.).
Subsequently, PKA inactivates GS by:
phosphorylating GSa
phosphorylating inhibitor-1, which in turn inhibits PP-1
phosphorylating GM at sites 1 and 2, so that PP-1 dissociates from the glycogen
particle and GS remains inactivated
binds to an α-adrenergic membrane receptor, triggering release of IP3, DAG
(diacylglycerol) and Ca2+, which inhibit GS. DAG, together with Ca2+, activates protein
kinase C to phosphorylate and inactivate glycogen synthase
78
Fig 5.5.28. Inhibition of glycogen synthase by IP3, diacylglycerol (DG) and Ca2+ in a hepatocyte. Note the
antagonistic action of epinephrine and glucagon in glycogen metabolism.
(Source: Voet and Voet, 1995, p 508 fig 17-22)
GLYCOGEN STORAGE DISEASES
The hereditary lack of any of the enzymes of glycogen metabolism may result in deposition of an
abnormal type or quantity of glycogen in tissues. These disorders called “glycogenoses” may have
serious consequences on health and even survival.
79
TABLE 5.5.1 GLYCOGEN STORAGE DISEASES
(Source: Murray et al, 2003, p 152 18-2)
Section 5.5.C
RECIPROCAL REGULATION OF GLYCOGENESIS AND GLYCOGENOLYSIS
Synthesis and breakdown of glycogen are co-ordinated in such a way that when one is stimulated
the other is inhibited. In this way steady levels of glucose are maintained both within the cell as
well as in the body.
Regulatory mechanisms in glycogenolysis and glycogenesis respond to:
•
Blood levels of glucose – which depends on the nutritional/metabolic state
•
Muscular activity – which may suddenly demand energy fuel several hundred times that
of the resting level
A balance in the activities of the two main enzymes viz. glycogen phosphorylase and glycogen
synthase, is crucial in regulation of glycogen metabolism. From the preceding sub-sections you
must have already realized that the actual controlling factors for glycogen synthase and
phosphorylase are almost the same. It is therefore reasonable to assume that if a factor stimulates
glycogenesis it should inhibit glycogenolysis synchronously and vice-versa.
In order to understand the reciprocal regulation of glycogenolysis and glycogenesis, it is useful
to bear some fundamentals in mind:
•
sites of glycogen metabolism are muscle and liver
•
glycogen provides glucose as energy fuel when energy state of cell is low
[ATP]:[AMP]↓)
•
surplus glucose needs to be stored as glycogen
80
(i.e.
•
regulation of the pathways is by reversible covalent modification (phosphorylation) and
allosteric modulation of key enzymes
•
key regulatory enzymes are glycogen phosphorylase and glycogen synthase
•
enzymes common to both pathways are phosphorylase kinase A and protein phosphatase-1
•
key hormones are epinephrine, glucagon and insulin; their secretion depends on the
[blood glucose]
•
second messengers in hormone action are cAMP, IP3, and DAG
•
enzyme cascades which amplify the primary signal are
phosphoinositide
•
other cellular molecules linked to both pathways are glucose, Ca2+, AMP and ATP
mediated by cAMP and
Recall too the salient features in regulation of PL and GS:
•
There is a basic difference in the effect of phosphorylation on PL and GS. Phosphorylation
activates PL and inactivates GS
•
PKA is the key enzyme in phosphorylation of PL and GS; it favors glycogenolysis and
inhibits glycogenesis
•
PP-1 is the main enzyme in dephosphorylation of PL and GS; it favors glycogenesis and
inhibits glycogenolysis
•
Cyclic AMP-mediated cascade simultaneously stimulates PKA and inhibits PP-1
•
Epinephrine and insulin act on both muscle and liver; glucagon action is only on liver
81
Fig 5.5.29. Reciprocal regulation of glycogenolysis and glycogenesis. See text for details.
(Source: Murray et al, 2003, p 151 fig 18-8)
We can now summarise the reciprocal regulation of glycogenolysis and glycogenesis as follows:
1.
2.
3.
4.
Epinephrine/Glucagon
glycogenesis:
stimulate
glycogenolysis
but
simultaneously
suppress
Epinephrine/Glucagon à bound to β receptor on cell membrane à ↑ [cAMP] à
activates PKA à phosphorylation promoted à PL activated; GS inhibited
Active PKA à inactivates PP-1 à dephosphorylation preventedà PL active; GS
inactive
Epinephrine à bound to α receptor on cell membrane à phospholipase C active
à ↑ [IP3] à cytosolic
↑ [Ca2+] à activates phosphorylase kinase à PL active
Phospholipase C activeà ↑ ([DAG] +↑ [Ca2+]) à activate protein kinase C à
phosphorylation favored à GS inactive
Insulin stimulates glycogenesis but simultaneously suppresses glycogenolysis:
Insulin à ↑Glucose entry à ↑ [Glc 6-P]à inhibits phosphorylase kinase and
activates PP-1à dephospohrylation favored à GS active; PL inactive
Insulin à inactivates GSK3 à dephosphorylation promotedà GS active
Insulin à activates PP-1 à dephosphorylation promoted à GS active; PL inactive
[Ca2+] stimulates glycogenolysis and simultaneously suppresses glycogenesis:
Muscle: the release of Ca2+ is the signal for muscle contraction and it
simultaneously stimulates glycogenolysis to provide glucose as energy fuel
Neural/electrical stimulation of muscle à cytosolic ↑ [Ca2+] à stimulates
phosphorylase
kinase and à phosphorylation promoted à PL activated; GS
inactive
Liver: Vasopressin, epinephrine etc.à ↑ [IP3] à cytosolic ↑ [Ca2+]
phosphorylation promoted à PL activated; GS inactive
à
[Glucose]: increased availability of glucose favors glycogenesis:
•
↑ [Glc 6-P] à allosteric binding to PL b à dephosphorylation favored à PL inactive
•
↑ [Glucose]à allosteric binding to PL a à dephosphorylation by PP-1 à GS active;
PL inactive
{Index: ↑ = increase; ↓ = decrease; GS = glycogen synthase; PL= phosphorylase; PKA
= protein kinase A; PP-1 = protein phosphatase -1}
82
SUMMARY 5.5: GLYCOGEN METABOLISM
Glycogen metabolism occurs primarily in the liver and muscle. It is constituted by two separate
pathways viz. glycogenolysis and glycogenesis.
Glycogenolysis releases glucose from the glycogen stores in the liver for provision to extrahepatic
tissues when blood glucose is low. Glycogenolysis in muscle provides glucose for its own
immediate energy needs. Cyclic AMP-linked enzyme cascade systems ensure an amplified
response to the hormonal signals which trigger glycogenolysis. Glycogenesis synthesizes
glycogen from glucose for storage purposes when blood glucose is high. A protein, glycogenin, is
essential for de novo synthesis of glycogen
Both processes are strictly regulated so that they do not occur simultaneously.
Chapter 5 Section 6
GLUCONEOGENESIS
Gluconeogenesis is the synthesis of glucose from non-carbohydrate precursors. There is
always a basal requirement of glucose per se in the body even when fats are available to meet
most of the body’s needs for energy.
Tissues like the brain and RBC use glucose as primary energy fuel and need a continuous supply.
Skeletal muscle performing strenuous exercise, needs glucose for anaerobic glycolysis. Glucose is
also a precursor for the synthesis of triglyceride in adipose tissue and lactose in the mammary
glands.
It is estimated that the average daily requirement of glucose in a typical adult is 160 gms, of which
the brain utilizes 120 gms! The available glucose in the blood and from glycogen reserves is
sufficient to meet our glucose needs only for a day. Hence a source of glucose is essential,
particularly during a long period of starvation or during sudden and intense muscular activity.
At such times the liver (and to a much lesser extent, the renal cortex) again comes to the rescue. It
carries out gluconeogenesis and converts pyruvate to glucose by reversing several of the steps of
glycolysis. Additionally, the process also serves to clear metabolic products of other tissues e.g.
lactate (muscle, RBC) and glycerol (adipose tissue). The main precursors for gluconeogenesis
are 3-C compounds like lactate, propionate, glycerol and alanine. The energy required for
gluconeogenesis is provided by oxidation of fatty acids.
Section 5.6A
PATHWAY OF GLUCONEOGENESIS
Gluconeogenesis, which converts pyruvate to glucose, shares several common steps with
glycolysis, which converts glucose to pyruvate. However, a simple reversal of glycolysis does not
enable gluconeogenesis, since the thermodynamic equilibrium of glycolysis strongly favors
conversion of glucose to pyruvate.
The energy barriers preventing a simple reversal are due to the three irreversible reactions of
glycolysis (refer Section 1) viz.:
• Glucose + ATP à Glucose 6-P + ADP (catalyzed by hexokinase/glucokinse)
• Fructose 6-P + ATP à Fructose 1,6 BP + ADP (catalyzed by phosphofructokinase-1)
• Phosphoenolpyruvate + ADP à Pyruvate + ATP (catalyzed by pyruvate kinase)
The energetically unfavorable reversal of glycolysis is converted to a favorable one with the help
of four “gluconeogenic” enzymes viz pyruvate carboxylase, phosphoenolpyruvate
83
carboxykinase, fructose 1,6-bisphosphatase-1 and glucose 6-phosphatase. Six high-energy
phosphate bonds from ATP and GTP are also utilized for every molecule of glucose synthesized
from pyruvate.
Fig 5.6.1. Overview of steps in the conversion of pyruvate to glucose.
(Adapted from: Hames and Hooper, 2000, p 291 fig 1)
The three irreversible reactions of glycolysis are circumvented in the following way to enable
gluconeogenesis:
84
Reaction 1: Pyruvate à Phosphoenolpyruvate
This reaction has two main steps, linked by an intermediate metabolite, OAA. The 1st step occurs
in the mitochondrion and is catalyzed by pyruvate carboxylase (PC). Pyruvate produced in the
cytosol, enters the mitochondrion using a pyruvate transporter, and is carboxylated by PC to yield
oxalacetate (OAA).
The enzyme is a tetramer of 4 identical subunits, each of which has biotin as a co-factor to
transfer activated CO2. The enzyme requires Mg2+.
Fig 5.6.2. Schematic representation of the domain structure of pyruvate carboxylase.
(Source: Berg et al, 2002, p 680 fig 16.25)
The ATP-binding domain of the enzyme transfers COO- group derived from bicarbonate- to its
biotin-binding domain. COO- is attached to pyruvate in the central domain. The overall reaction
here is as follows:
Enz-biotin +CO2 +ATP à Enz-biotin-COO- + ADP + Pi
Enz-biotin-COO- + Pyruvate à Enz-biotin + OAA
Fig 5.6.3. Ball-and-stick model of carboxy-biotin (C atoms = black; O atoms = pink; H atoms = white; N atoms =
blue; S atoms = yellow) Biotin is attached through a specific Lysine residue to a long flexible arm of
pyruvate carboxylase (Source: Berg et al, 2002, fig 16.27)
In the 2nd step, PEP-carboxykinase (PEP-CK) simultaneously decarboxylates and phosphorylates
OAA to produce phosphoenolpyruvate (PEP). This enzyme also requires Mg2+.
The ease in conversion of OAA to PEP depends on the location of PEP-CK within the cell.
Depending on the species, PEP-CK is present in the cytosol and/or mitochondrion. If the enzyme
is in the mitochondrion (e.g. rabbit), OAA can be directly converted to PEP which then goes out
into the cytosol for subsequent reactions. In humans, PEP-CK is more or less equally distributed
between the two compartments, and the activity of the mitochondrial isozyme is predominant
when the gluconeogenic precursor is lactate.
85
However, if PEP-CK is in the cytosol (e.g.rat), the malate shuttle (refer Section1) is used to
transport OAA across the mitochondrial membrane to the cytosol for subsequent conversion to
phosphoenolpyruvate.
Fig 5.6.4. The two routes for conversion of pyruvate to phophoenolpyruvate: the location of the enzyme PEP
carboxykinase determines whether the formation of PEP is in the cytosol or in the mitochondrion.
(Source: Nelson and Cox, 2005, p 547 fig14-19)
Cytosolic and mitochondrial isozymes of malate dehydrogenase (MDH) are used in the malate
shuttle. OAA is first reduced to malate by an NADH-linked, mitochondrial MDH. Malate crosses
the inner mitochondrial membrane and is re-oxidised to OAA by cytosolic MDH.
C O OHO
C
H
CH 2
C O O-
N A D+
N A D H. H
ma la te
d e h y d r ogena s e
malate
+
C O OC =O
CH 2
C O O-
oxaloacetate
The malate shuttle thus generates cytosolic NADH required to reverse the glyceraldehyde 3-P
dehydrogenase reaction of glycolysis, so that glucose can be synthesized.
Transaminases also enable a transfer of OAA to the cytosol, this time in the form of aspartate.
Overall Reaction
PYRUVATE + ATP + GTP + HCO3- à PEP + ADP + GDP + Pi + CO2
86
Notice that two high-energy phosphates have been used. Though ∆G’o is 0.9 kJ/mol for Reaction
1, the actual ∆G under cellular conditions is -25 kJ/mol and this makes the reaction irreversible.
Reaction 2:
Fructose 1,6-bisphosphate à Fructose 6-phosphate
6
6
C H OP
2
1
O
H
H
C H OP
2
HO
OH
H O
2
C H OP
2
Pi
O
fructose 1 6 '
bisphosphatase
OH
H
H
HO
OH
H
fructose 1,6-bisphosphate
CH O H
2
OH
H
fructose 6-phosphate
∆G’o = -16.3kJ/mol
The phosphate group at C-1 of fructose 1,6-bisphosphate (Fru 1,6-BP) is removed hydrolytically
by fructose 1,6-bisphosphatase-1 (FBPase-1) in an exergonic reaction that yields Fru 6-P. This key
enzyme is present in the liver and kidney but not in adipose tissue. It is an allosteric enzyme with
ATP as positive and AMP as negative modulators.
Reaction 3:
Glucose 6-phosphate à Glucose
6
6
C H OH
2
H
HO
O
H
OH
H
H
H
OH
C H OP
2
H2O
Pi
glucose 6 phosphatase
H
HO
OH
glucose 6-phosphate
O
H
OH
H
H
OH
H
OH
glucose
∆G’o = - 13.8 kJ/mol
Glucose 6-phosphatase (Glc 6-Pase) hydrolyzes glucose 6-phosphate (Glc 6-P) to glucose in the
lumen of the ER and releases glucose and Pi (as explained in glycogenolysis). The enzyme is
present in the liver, kidney and intestine but not in muscle and adipose tissue. Hence the liver is
the chief supplier of glucose formed by gluconeogenesis to the blood.
All the other reactions of gluconeogenesis are common with glycolysis and occur by a simple
reversal of the glycolytic reactions. We can now link all the reactions and view the composite
picture of the gluconeogenic pathway.
87
Fig 5.6.5. A composite view of the pathway of gluconeogenesis and its relationship to glycolysis.
(Source: Nelson and Cox, 2003, p 544 fig 14-16)
OVERALL REACTION OF GLUCONEOGENESIS:
2 Pyruvate + 4 ATP + 2 GTP + 2 NADH + 2 H+ + 4 H2O à
GLUCOSE + 4 ADP + 2 GDP + 6 Pi + 2 NAD+
88
MAJOR PRECURSORS OF GLUCONEOGENESIS
1. Lactate:
Approximately 80% of lactate produced by anaerobic glycolysis in the muscle and other tissues is
converted to glucose by gluconeogenesis in the liver. Reversal of the lactate dehydrogenase
reaction of anaerobic glycolysis converts lactate to pyruvate and funnels it into gluconeogenesis.
C O OHO
C
N A D+
N A D H. H
H
CH3
+
C O OC =O
lac t a t e
d e h y d r ogena s e
lactate
CH3
pyruvate
The processing of lactate between the muscle and liver is known as the Cori’s cycle. Lactate from
the muscle is carried by blood to the liver where it undergoes gluconeogenesis. The glucose
produced is transported back to the muscle for glycolysis. Tissue-specific distribution of the
isozymes of LDH enables ready conversion of lactate to pyruvate by the hepatic cells.
Fig 5.6.6.
Representations of the Cori’s cycle and the glucose-alanine cycle between muscle and liver. The Cori’s
cycle processes lactate while the glucose-alanine cycle processes alanine.
(Source: Murray et al, 2003, p 159 fig 22-13)
2. Alanine:
During starvation, slow breakdown of muscle produces glucogenic amino acids among which
alanine is predominant. Alanine is also released into the hepatic portal vein during protein
digestion in the GIT.
89
The blood transports Ala from muscle to the liver where transamination converts it to pyruvate for
gluconeogenesis. The glucose formed is transferred back to the muscle as energy fuel. The
glucose-alanine cycle thus results in a net transfer of Nitrogen from muscle to liver, and of energy
from liver to muscle.
The TCA cycle also provides a route for passage of other “glucogenic” amino acids into the
gluconeogenic pathway; Subsequent transfer to cytosol for gluconeogenesis is via malate. The
major intermediates that link the amino acids to gluconeogenesis are:
PYRUVATE - Ala, Cys, Gly, Ser, Threo, Try
α-KETOGLUTARATE - Arg, Glu, Gln, His, Pro
SUCCINYL CoA - Ileu, Met, Threo, Val
FUMARATE - Phe, Tyr
OAA - Asp, Asn
3. Glycerol:
Glycerol is a product of lipolysis in adipose tissue, both from stored triglycerides and from
lipoprotein complexes cleaved at the level of the capillary walls. Free glycerol diffuses out into
the blood and is taken up by the liver and kidney.
Fig 5.6.7. Conversion of glycerol to the glycolytic intermediate dihydroxyacetone phosphate, which can enter
gluconeogenesis as shown in Fig 5.6.5. (Source: Murray et al, 2003, p 198 fig 24-2)
Glycerol is first phosphorylated to glycerol 3-P by glycerokinase, an enzyme present mainly in the
liver and kidney but not in adipose tissue. This is followed by dehydrogenation to
dihydroxyacetone phosphate, which now makes a lateral entry into the pathway of
gluconeogenesis.
4. Propionate:
Propionate is a product of lipid digestion in ruminants, and of β-oxidation of fatty acids (with an
odd number of carbon atoms). Propionate is activated to propionyl CoA by acyl-CoA synthetase
and then carboxylated to a 4-C intermediate, methylmalonyl CoA. This compound can be
isomerised to succinyl CoA, an intermediate of the TCA cycle. Subsequent entry into
gluconeogenesis is via malate.
90
Fig 5.6.8. Route for conversion of propionate to succinyl-CoA which enters the gluconeogenic pathway via malate
(Source: Murray et al, 2003, p155 fig 19-2)
There is no net conversion of fatty acids to glucose in mammals even though oxidation of fatty
acids directly provides acetyl-CoA to the TCA cycle. The PDH reaction, which converts pyruvate
to acetyl-CoA, cannot be reversed by any “by-pass” step. The enzymes that release pyruvate from
citrate, viz. “malic” enzyme and citrate lyase, are more involved in lipogenesis than in
gluconeogenesis.
REGULATION OF GLUCONEOGENESIS
The rate of gluconeogenesis depends on the activities of its key enzymes and the availability of its
precursors.
The key regulatory enzymes in gluconeogenesis are:
•
pyruvate carboxylase
•
phosphoenolpyruvate carboxykinase
•
fructose 1,6-bisphosphatase-1
•
glucose 6-phosphatase.
The activities of these enzymes are low when blood glucose is high (as in carbohydrate-feeding)
and high when blood glucose is low (as in starvation and diabetes). Their regulation of these
enzymes is by both allosteric and hormonal mechanisms.
Acetyl-CoA is an allosteric activator of pyruvate carboxylase, The concentration of acetyl CoA
increases on consumption of a high fat diet (owing to increased β-oxidation of fatty acids); hence
such a nutritional state favors gluconeogenesis.
Citrate, which is a product of the condensation of acetyl-CoA with OAA, stimulates FBPase-1
allosterically.
ADP and AMP increase in concentration when the energy state of the cell is low and this is not
conducive to gluconeogenesis. ADP inhibits both pyruvate carboxylase and PEP-CK, while AMP
and fructose 2,6-bisphosphate inhibit FBPase-1.
The hormones, glucagon, epinephrine and glucocorticoids, are inducers of the synthesis of all
the gluconeogenic enzymes, while insulin is a repressor.
91
The availability of precursors also affects gluconeogenesis. Conditions in extrahepatic tissues
that increase the production of lactate and alanine are conducive to gluconeogenesis in the liver.
A high rate of anaerobic glycolysis in active muscle increases lactate production, while starvation
increases breakdown of muscle proteins to release alanine. High levels of Ala also inhibit pyruvate
kinase in the liver so that glycolysis is decreased. Glucagon increases lipolysis in adipose tissue
and makes glycerol available for gluconeogenesis while insulin has the opposite effect.
Ethanol inhibits gluconeogenesis. The oxidation of ethanol in the liver increases [NADH] and
shifts the LDH/MDH reactions to favor lactate/malate over pyruvate/OAA respectively. It is
therefore unwise to consume liquor on an empty stomach!
Section 5.6B
RECIPROCAL REGULATION OF GLYCOLYSIS AND GLUCONEOGENESIS
The hepatic cells have a triple access to glucose supply viz from the blood, by glycogenolysis and
by gluconeogenesis. Since the liver provides glucose as energy fuel to other tissues in preference
to its own self, a tight regulation is required on its ability to degrade glucose by glycolysis and
synthesize glucose by gluconeogenesis. At any point in time, the pathway favored depends on the
levels of blood glucose and on the energy state of the hepatic cells. Conditions that favor
gluconeogensis concomittantly suppress glycolysis, and vice- versa.
Both pathways have many common and reversible steps. Hence, regulation is excercised on the
enzymes catalyzing those reactions which are distinct for each pathway.
The key enzymes for glycolysis are pyruvate kinase (PK), phosphofructokinase-1 (PFK-1) and
glucokinase/hexokinase (GK/HK). The key enzymes for gluconeogenesis are pyruvate
carboxylase (PC), phosphoenolpyruvate carboxykinase (PEP-CK), fructose 1,6-bisphosphatase
(FBPase-1) and glucose 6-phosphatase (Glu 6-Pase). They are regulated reciprocally by allosteric
or hormonal control of their activity or transcriptional control of their quantity.
(It would be advisable here to revise the regulatory mechanisms explained for glycolysis in
Section 1 of this chapter. In the discussion below, we have used the color blue for glycolytic
enzymes and orange for gluconeogenic enzymes).
Allosteric regulation
Concentrations of critical local molecules cause allosteric modulation of the activities of PFK-1 vs
FBPase-1 and PK vs PC and they play a primary role in determining whether glycolysis or
gluconeogensis will take place.
The allosteric modulators affect the pathways as follows:
a. [ATP]/[AMP]
When the energy state of the cell is low, [AMP] is high and the synthesis of ATP is required.
Since AMP activates PFK-1 and inhibits FBPase-1, and ADP inhibits PC, hence glycolysis is
favored and gluconeogenesis is suppressed to make more ATP available to the cell.
Conversely, when the energy state of the cell is high, increased levels of ATP inhibit PFK-1 and
PK, while low [AMP] does not inhibit FBPase-1; hence gluconeogenesis is favored over
glycolysis. During processes that consume energy, a small change in [ATP] causes a large
change in [AMP]. This enables PFK-1 to respond even to small changes in the energy status of the
cell and thereby control glycolysis.
92
•
•
Fig 5.6.9. Allosteric modulators of the glycolytic and gluconegenic enzymes involved in reciprocal regulation
of the two pathways. (Source: Berg et al, 2002, fig 16.30)
b. Acetyl-CoA
Increased β-oxidation of fatty acids occurs under conditions of starvation, high-fat diet or diabetes.
The consequent increase in [acetyl-CoA] activates both PC and FBPase-1 allosterically,
stimulating gluconeogenesis but suppressing glycolysis:
•
↑ β-oxidation of fatty acids à ↑ [acetyl-CoA] à ↑ PC activity à ↑ OAA formation à ↑
[citrate] à stimulates FBPase-1 activity à gluconeogeneis ↑
•
↑ [citrate] à inhibits PFK-1 à glycolysis ↓
Increased [acetyl-CoA] provides more ATP as energy to facilitate gluconeogenesis, but the same
high cytosolic levels of ATP inhibit PFK-1 and also PK (by decreased formation of Fru 1,6 BP) to
suppress glycolysis. High [acetyl -CoA] also inhibits PDH, reducing pyruvate oxidation i.e. the
metabolic fate of pyruvate changes in the liver and kidney on transition from “well-fed” to starved
state.
c. Fructose 2,6-bisphosphate
Fru 2,6-BP is the most potent allosteric effector of PFK-1 and inhibitor of FBPase-1 in liver. It
relieves inhibition of PFK-1 by ATP and increases affinity for Fru 6-P. It inhibits FBPase-1 by
increasing Km for Fru 1,6-BP.
93
Fig 5.6.10. Reciprocal regulation of glycolysis and gluconeogenesis by Fructose 2,6-bisphosphate .
(Source: Nelson and Cox, 2003, p 582 fig 15-23)
The concentration of Fru 2,6-BP in the cell depends on the activity of the bifunctional enzyme,
(PFK-2 + FBPase-2) which we encountered earlier in the regulation of glycolysis.
When [blood glucose] is highà ↑ [Fru 6-P]à inhibits FBPase-2 à ↑ [Fru 2,6-BP] à stimulates
PFK-1 and inhibits FBPase-1 à hence glycolysis ↑ and gluconeogenesis ↓
The dominance of kinase vs phosphatase activity of the bifunctional enzyme depends on allosteric
and hormonal factors.
d. Glucose 6-phosphate
Accumulation of glucose 6-P in cells (by decreased activity of PFK-1) causes allosteric inhibition
of hexokinase and decreased uptake of glucose in extrahepatic tissues like muscle. The situation is
different in the liver where. glucokinase is inhibited by reversible binding of a regulatory protein
specific to the liver (refer Fig 5.1.16).
When blood glucose is high, efficiency of GLUT2 transporter ensures that cytosolic glucose levels
in the hepatic cells equilibrate with blood levels, glucokinase is freed from inhibition, and Glc 6-P
continues to be formed. However, if [blood glucose] falls below optimal levels, Fru 6-P causes
binding of the regulatory protein to glucokinase and formation of Glc 6-P is inhibited. This
ensures that liver does not compete with other tissues for glucose.
2. Hormonal regulation
Hormones like glucagon, epinephrine and insulin control the activity of the key enzymes either by
covalently modifying them or inducing or repressing their synthesis
GLUCAGON covalently modifies PKA and sets off a chain of reactions that finally increases
gluconeogenesis:
On starvation à ↓ [blood glucose] à GLUCAGON secretion ↑ à triggers cAMP-dependent
enzyme cascade in hepatic cell à activates PKA à activates FBPase-2 à ↓ [Fru 2,6-BP] à
FBPase-1 not inhibited and PFK-1 not stimulatedà hence gluconeogenesis ↑ and glycolysis ↓
The effects of INSULIN are opposite to those of glucagon but the mechanism is not well-defined:
In well-fed state à ↑ [blood glucose] à INSULIN released --à ↑ [Fru 2,6-BP] à strongly
stimulates PFK-1; FBPase-1 inhibited à hence glycolysis ↑ and gluconeogenesis ↓
Insulin, which rises on feeding, increases the synthesis of all key enzymes of glycolysis. On the
other hand glucagon, epinephrine and glucocorticoids, which rise on starvation, increase the
synthesis of gluconeogenic enzymes. A high glucagon/insulin ratio in the blood also increases
synthesis of transaminases that in turn affect the availability of gluconeogenic precursors. Both the
hormones act via separate signal cascades to affect transcription.
94
SUMMARY 5.6: GLUCONEOGENSIS
Gluconeogenesis is an anabolic process which synthesizes glucose from non-carbohydrate
precursors like lactate, alanine, glycerol and pyruvate. The process occurs in the liver when levels
of blood glucose are low. Its purpose is to provide glucose as energy fuel to tissue like the RBC
where continuous glucose supply is critical.
Gluconeogenesis is essentially a reversal of the steps of glycolysis, with by-pass enzymatic
reactions circumventing three energy barriers that prevent easy reversal.
Gluconeogenesis and glycolysis are reciprocally regulated by allosteric and hormonal factors,
Chapter 5 Section 7
REGULATION OF BLOOD GLUCOSE
The maintenance of stable levels of blood glucose is an excellent example of homeostasis in our
body. The elucidation of the mechanisms of glucose metabolism that enable this steady state, has
been an outstanding achievement in biochemistry. The doggedness and brilliant analytical skills
with which scientists have worked to understand the pathways and their regulations, are worthy of
respect and admiration. No wonder so many of them (Warburg, Meyerhoff, Krebs, the Coris,
Sutherland…the list goes on) have been awarded the Nobel Prize!
Fig 5.7.1.
Sources of blood glucose (dietary source of glucose has not been shown)
(Source: Vander et al, 2001, p 596 fig 18-2)
The sources of glucose in the blood are dietary intake, and hepatic glycogenolysis and
gluconeogenesis. All tissues take in glucose from the blood, though the extent to which they
95
depend exclusively on glucose as energy fuel are different. As mentioned earlier, the brain and
RBC need continuous and adequate supply of glucose.
The concentration of blood glucose varies before and after meals. In a normal adult, blood glucose
levels in the post- absorptive state are maintained between 4.5-5.5 mmol/L. However, a
carbohydrate meal can increase these levels to 6.5-7.2 mmol/L (hyperglycemia), while starvation
can decrease it to 3.3-3.9 mmol/L (hypoglycemia). Hyperglycemia may also be due to metabolic
disorders like diabetes mellitus. Hypoglycemia may be caused by vigorous muscle excercise,
pregnancy, or drugs. A sudden drop in the concentration of blood glucose causes convulsions and
may be fatal, but a more gradual decrease can enable metabolic adaptations to some extent.
The primary organ in maintaining stable levels of glucose in the blood is the liver. At normal
levels of blood glucose, the liver is a net producer of glucose. We have already seen that hepatic
glycogenolysis and gluconeogenesis release glucose into the blood, while glycogenesis stores
excess glucose as glycogen. As levels of blood glucose rise (as in hepatic portal vein after a meal)
the liver switches its enzymatic machinery from production to uptake of glucose. It helps that,
unlike extrahepatic tissues, the liver has the requisite glucose transporter for rapid uptake of
glucose from the blood when the levels are on the rise. When blood glucose is low, the liver shifts
its own metabolism from utilization of glucose for energy to the oxidation of fatty acids. Under
conditions of hypoglycemia, the increased use of fatty acids and ketone bodies as energy fuels,
also has a “sparing” effect on blood glucose essential to the RBC and neural tissues.
The ability of the liver to adjust its glucose metabolism with the levels of blood glucose, is largely
due to the hormones insulin and glucagon. Both hormones are produced by the pancreas; the αcells of the islets of Langerhans secrete glucagon while the β-cells secrete insulin.
Fig 5.7.2. Relation between the levels of plasma glucose and the secretion of glucagon and insulin.
(Source: Vander et al, 2001, p 604 fig 18- 9)
96
Low blood glucose shifts the ratio of [insulin]/[glucagon] in the blood in favor of glucagon, while
high blood glucose favors insulin over glucagon. We have already learnt how glucagon stimulates
hepatic glycogenolysis and gluconeogenesis in order to boost blood glucose levels. On the other
hand, the rise in [insulin] parallels that of [glucose] in the blood, and stimulates hepatic
glycogenesis and glycolysis. Additionally, insulin increases entry of glucose into extrahepatic
tissues for glycolysis, into muscle cells for glycogenesis, and into adipose tissue for triglyceride
synthesis. All these events tend to lower [blood glucose].
Fig 5.7.3.
Blood levels of glucose, glucagon and insulin after moderate exercise
(Source: Vander et al, 2001 p 607 fig 18-11)
Fig 5.7.4. The activities of hepatic glycogen phosphorylase and glycogen synthase in the liver after infusion
of glucose (Source: Berg et al, 2002, fig21.21)
The adrenal catecholamines and glucocorticoids tend to raise levels of blood glucose when there
is increased demand for glucose in muscle and other tissues. Epinephrine is secreted by the
adrenal medulla, and also by the sympathetic nerve endings, in response to stressful stimuli like
fear, excitement, hemorrhage and hypoglycemia. This causes increased glycogenolysis in both
muscle and liver.
97
Fig 5.7.5.
Interaction between the levels of plasma glucose and the secretion of epinephrine
(Source: Vander et al, 2001 p 602 fig 18-10)
Cortisol from the adrenal cortex is permissive to gluconeogenesis. Adenohypophyeal hormones
like STH and ACTH are also anti-insulinic in action.
Fig 5.1.6. Comparison of the blood
levels of glucose in normal and diabetic
individuals at different time intervals
in a glucose tolerance test . (Source:
Murray et al, 2003, p,161 fig19-6)
By now it would be apparent to
you that insulin is essential for
glucose entry into tissues, as
well as for its storage as glycogen in the liver. The deficiency of insulin causes diabetes mellitus,
a disorder with devastating effects throughout the body if left undetected and untreated. High
blood levels of glucose between meals and low readings in a “glucose tolerance” test are
indicative of the disorder. Drugs are used to stimulate insulin secretion in Type 2 diabetes
(NIDDM i.e. non-insulin dependent diabetes mellitus), while insulin per se has to be administered
in Type 1 diabetes (IDDM i.e. insulin dependent diabetes mellitus).
98
SUMMARY
Carbohydrate metabolism is constituted by anabolic, catabolic and amphibolic pathways, most of
which deal with glucose or its metabolic products.
Glycolysis is a major catabolic pathway of glucose which occurs in the cytosol. It provides energy
to cells under both aerobic and anarobic conditions. Glucose is degraded to pyruvate, which
results in a small yield of ATP under anaerobic conditions, but a much larger yield when
processed aerobically. Pyruvate is reduced to lactate under anaerobic conditions, but is oxidatively
decarboxylated to acetyl-CoA under aerobic conditions. NADH is also produced in glycolysis.
Shuttle systems enable transfer of reduced equivalents to the mitochondrion.
The citric acid cycle is a major amphibolic pathway which occurs in the mitochondrion and
accounts for the final oxidation of carbohydrate, lipid and protein. Acetyl-CoA, a common endproduct in intermediary metabolism, condenses with oxalacetate and enters the cycle as citrate. In
every turn of the cycle, a series of dehydrogenases degrade a citrate molecule, oxidizing two
carbon atoms to carbon dioxide and reducing the co-enzymes NAD+ and FAD. OAA is
regenerated to continue the cycle. The reduced co-enzymes yield ATP when passed through the
electron transport chain.
The hexose monophosphate pathway partially oxidizes glucose in the cytosol. Its main purpose is
to reduce NADP+ to NADPH.H+ for fatty acid synthesis in tissues. It also provides ribose for
nucleic acid synthesis but does not generate ATP.
Glycogen metabolism occurs primarily in the liver and muscle. It is constituted by two separate
pathways viz. glycogenolysis and glycogenesis. Glycogenolysis releases glucose from the
glycogen stores in the liver for provision to extrahepatic tissues when blood glucose is low.
Glycogenolysis in muscle provides glucose for its immediate energy needs. Glycogenesis
synthesizes glycogen from glucose for storage purposes when blood glucose is high. Both
processes are strictly regulated so that they do not occur simultaneously.
Gluconeogenesis is an anabolic process in the liver which synthesizes glucose from noncarbohydrate precursors like lactate, alanine, glycerol and pyruvate. The process occurs when
levels of blood glucose are low and serves to provide glucose as energy fuel to tissue like the RBC
where its requirement is critical. The process is essentially a reversal of the steps of glycolysis,
with by-pass enzymatic reactions circumventing those energy barriers that prevent easy reversal.
Gluconeogenesis and glycolysis are reciprocally regulated.
The pathways of glucose metabolism are well regulated so that blood levels of glucose are
maintained at a steady state.
SUMMARY 5.7: REGULATION OF BLOOD GLUCOSE
All the pathways of glucose metabolism are well regulated to maintain the blood levels of glucose
at a steady state.
Dietary and hormonal factors determine the levels of glucose in the blood. The glucose tolerance
test enables an assessment of the ability of the body to regulate glucose levels. Hyperglycemia and
hypoglycemia are both harmful to the body.
99
Credits for illustrations in Chapter 5
1.
Murray, R.K., Granner, D.K., Mayes, P. A. and Rodwell, V.W.: Harper’s Illustrated
Biochemistry, 26th edition,
2. International edition, 2003, The McGraw-Hill Companies Inc.
3.
Nelson, D.L. and Cox, M.M.: Lehninger’s Principles of Biochemistry, 4th edition, 2005, W.H.
Freeman and Co.
4.
Voet, D. and Voet, J.G.: Biochemistry, 2nd edition, 1995, John Wiley and Sons, Inc.
5.
Berg, J.M., Tymoczko, J.L. and Stryer, L.: Biochemistry, 5th edition, 2002, W.H. Freeman and
Co.
6.
Lodish, H, Berk, A., Matsudaira, P., Kaiser, C.A., Kreizer, M., Scott, M. and Darnell, J.:
Molecular Cell Biology,
7.
5th edition, 2003, W.H. Freeman and Co.
8.
Vander, A., Sherman, J. and Luciano, D.: Human Physiology: The Mechanisms of Body
Function, 8th edition,
9. 2001, International edition, The McGraw-Hill Companies Inc.
10. Boyer, R.: Concepts in Biochemistry, 1999, Brooks/Cole Publishing Company
11. Hames, B.D. and Hooper, N.M.: Instant Notes Biochemistry, 2nd edition, 2000, BIOS Scientific
Publishers Ltd.
100