Comparison of Dietary Phosphate Absorption After
advertisement

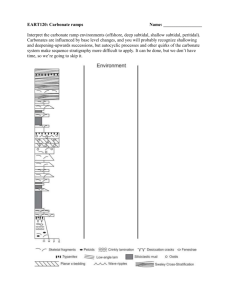
Original Investigation Comparison of Dietary Phosphate Absorption After Single Doses of Lanthanum Carbonate and Sevelamer Carbonate in Healthy Volunteers: A Balance Study Patrick Martin, MD,1 Phillip Wang, PhD,1 Antoine Robinson, MSN, CRNP,1 Lynne Poole, MSc,2 Jeffrey Dragone, MS,1 Michael Smyth, FRCS, MRCGP,2 and Raymond Pratt, MD1 Background: Lanthanum carbonate and sevelamer carbonate are noncalcium phosphate binders used to treat hyperphosphatemia in patients with chronic kidney disease. This is the first study to compare phosphate absorption from a standardized meal ingested with a typical clinical dose of these binders. Study Design: Randomized open-label crossover study. Settings & Participants: Healthy volunteers were confined to a clinical research center during 4 study periods. Of 31 volunteers randomly assigned, 19 completed all treatments and 18 were analyzed in the pharmacodynamic set (1 was excluded because of vomiting). Intervention: Participants were assigned in random order to meal alone, meal plus lanthanum carbonate (1 tablet containing 1,000 mg of elemental lanthanum), and meal plus sevelamer carbonate (three 800-mg tablets). The gastrointestinal tract was cleared, the meal was ingested (⫾ treatment), and rectal effluent was collected. In a fourth period, volunteers repeated the study procedures while fasting. Outcomes: The primary end point, net phosphate absorption, was analyzed using a mixed-effect linear model. Measurements: Phosphorus content of effluent and duplicate meal samples were measured using inductively coupled plasma– optical emission spectroscopy. Results: The standard meal contained ⬃375 mg of phosphate, 75% of which was absorbed (net absorption, 281.7 ⫾ 14.1 mg [adjusted mean ⫾ standard error]). Lanthanum carbonate decreased net phosphate absorption by 45% (net absorption, 156.0 ⫾ 14.2 mg) compared with 21% (net absorption, 221.8 ⫾ 14.1 mg) for sevelamer carbonate (P ⬍ 0.001). Lanthanum carbonate bound 135.1 ⫾ 12.3 mg of phosphate, whereas sevelamer carbonate bound 63.2 ⫾ 12.3 mg, a 71.9-mg difference (95% CI, 40.0-103.8; P ⬍ 0.001). Per tablet, this equates to 135 mg of phosphate bound with lanthanum carbonate versus 21 mg with sevelamer carbonate. Limitations: A single-dose study. Conclusions: In healthy volunteers, 1,000 mg of lanthanum carbonate decreased phosphate absorption by 45% compared with a 21% decrease with 2,400 mg of sevelamer carbonate. Am J Kidney Dis. xx(x):xxx. © 2011 by the National Kidney Foundation, Inc. INDEX WORDS: Chronic kidney disease; clinical trial; lanthanum carbonate; phosphate binder; sevelamer carbonate. A n increased serum phosphorus level is associated with increased morbidity and mortality in patients with chronic kidney disease (CKD), including those not yet requiring dialysis.1,2 Patient management strategies to decrease serum phosphorus levels include dietary phosphate restriction and provision of adequate dialysis when renal replacement therapy is required. A cohort study showed that sustained control of serum phosphorus levels to 3.5-5.5 mg/dL is a strong predictor of improved survival in patients new to dialysis therapy.3 Unfortunately, dietary phosphate restriction and dialysis often are insufficient to control serum phosphorus to guideline levels, such as those recommended by KDOQI (ie, the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative) and the KDIGO (Kidney Disease: Improving Global Outcomes) group, which are 3.5-5.5 mg/dL and ⬍4.6 mg/dL, respectively.4,5 Approximately 40% of patients on dialysis therapy still have serum phosphorus levels ⬎5.5 mg/dL.6 Am J Kidney Dis. 2011;xx(x):xxx There may be risks associated with trying to improve hyperphosphatemia through dietary restriction. Data from patients on dialysis therapy have shown that increasing protein intake while decreasing serum phosphorus level is associated with a lower risk of mortality compared with concurrent increases or decreases in both parameters or a decrease in protein From 1Shire Pharmaceuticals, Wayne, PA; and 2Shire Pharmaceuticals, Basingstoke, UK. Received July 13, 2010. Accepted in revised form November 17, 2010. Trial registration: ClinicalTrials.gov; study number: NCT00875017. Address correspondence to Patrick Martin, MD, Shire Pharmaceuticals, 725 Chesterbrook Blvd, Wayne, PA 19087-5637. E-mail: pmartin@shire.com © 2011 by the National Kidney Foundation, Inc. 0272-6386/$36.00 doi:10.1053/j.ajkd.2010.11.028 1 Martin et al intake with an increase in serum phosphorus level.7 KDOQI recommends protein intake of 1.2 g/kg of body weight per day for hemodialysis patients.8 Based on an average phosphate content of 10-12 mg/g of protein, a 70-kg patient consumes 84 g of protein and 840-1,008 mg/d of phosphate.5 Because 60%-80% of ingested phosphate is absorbed from the gastrointestinal (GI) tract,9 a typical dialysis patient may absorb at least 3,500 mg/wk of phosphate. Because thriceweekly hemodialysis typically removes 2,400 mg of phosphate,5 a net positive phosphate balance of at least 1,000 mg/wk may occur. It therefore is very difficult to maintain a net neutral balance or induce a net negative phosphate balance without dietary protein restriction or pharmacologic intervention. The use of efficacious dietary phosphate binders may be desirable to treat increased serum phosphorus levels because they would allow patients on dialysis therapy to maintain adequate protein intake and neutral phosphate balance. Several phosphate binders are available for use by patients with CKD. Calcium-based agents commonly are prescribed for patients on dialysis therapy, but high daily doses often are required, potentially increasing calcium load and the risk of vascular calcification.10,11 The current alternatives, non–calcium-based lanthanum carbonate (Fosrenol; Shire Pharmaceuticals, www.shire.com) and sevelamer (Renagel and Renvela; Genzyme Corp, www.genzyme.com), may be associated with a lower risk of vascular calcification,12-14 and studies have shown an association with improved survival when they are used compared with calcium-based agents in a subset of patients on dialysis therapy who are older than 65 years.15,16 Knowledge of a patient’s dietary phosphate intake and dialysis regimen combined with information about the phosphate-binding capacity of phosphate binders may allow tailoring of prescriptions to achieve decreases in serum phosphorus level and phosphate load while maintaining adequate protein intake. Assessments of the relative phosphate-binding capacities of lanthanum carbonate and sevelamer have been limited to in vitro and animal studies17,18 and indirect clinical comparisons versus the hydrochloride salt of sevelamer using 24-hour urinary excretion of phosphorus to estimate decreases in phosphate absorption.19,20 The binding capacities of aluminum- and calcium-based phosphate binders have been examined directly in a previous study by Sheikh et al.21 In their study, measurement of phosphorus in rectal effluent enabled direct assessment of dietary phosphate absorption and the phosphate-binding capacities of these agents. Use of healthy volunteers allowed assessment of phosphate absorption without interference from physiologic factors associated with CKD and its treatment. 2 Using methods similar to that of Sheikh et al,21 the study reported here directly compared the decrease in dietary phosphate absorption and binding capacities of lanthanum carbonate and sevelamer carbonate. METHODS Study Design This open-label randomized crossover study was conducted in the United States in accordance with International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Good Clinical Practice guideline E6,22 consistent with the Declaration of Helsinki. The study was conducted on behalf of Shire Pharmaceuticals by an independent study unit. Healthy male and female volunteers aged 19-45 years with body mass index of 20.0-29.9 kg/m2 and serum 1,25dihydroxyvitamin D3 level ⬎30 pg/mL were included in the study. Nonpregnant women of childbearing potential were required to use appropriate methods of contraception during the study. Written informed consent was obtained from all individuals. The eligibility of volunteers was confirmed during a 28-day screening period and reconfirmed at the start of each of 4 study periods when participants underwent assessment of vital signs, safety laboratory parameters, electrocardiography, and urinalysis. Women of childbearing potential had to have had a negative pregnancy test result. At the start of study period 1, participants were randomly assigned using a computer-generated list with a block size of 6 to 1 of 6 treatment sequences, each consisting of 4 periods separated by a 7- to 14-day washout (Fig 1). In each of the first 3 periods, participants received a meal standardized for phosphate content, the standard meal plus lanthanum carbonate (a single tablet containing 1,000 mg of elemental lanthanum), or the standard meal plus sevelamer carbonate (2,400 mg; three 800-mg tablets). Participants repeated the study procedures while fasting in the fourth period. Five days after completion of the fasting period or early withdrawal from the study, individuals were followed up to report any ongoing concomitant medications or adverse events (AEs) and any new AEs or serious AEs. Because studies suggesting a required dosage for sevelamer carbonate are sparse, doses were chosen based on those typically used in clinical trials of sevelamer hydrochloride and lanthanum carbonate.11,14,23,24 The carbonate and hydrochloride forms of sevelamer have been shown to be bioequivalent for the decrease in serum phosphorus levels.25 Doses were consistent with the prescribing information.26,27 Dosing and Sample Collection After admission to the clinical research center at the start of each study period, participants received a clear-liquid dinner (broth, Jell-O [Kraft Foods, www.kraftfoodscompany.com], and juice) and then fasted (with access to only deionized water) until lunchtime of the following day, when they received the standardized meal with or without phosphate-binder treatment. During the fasting period, participants underwent the same procedures, but did not consume the meal or phosphate binders. Four hours before ingestion of the meal, the GI tract was cleared by flushing with mannitol solution (3-4 L of solution D as described by Davis et al,28 administered using a nasogastric tube at 20-30 mL/min) until the stool was clear of solid material, confirmed visually by research center staff. During the assigned periods, participants were administered lanthanum carbonate or sevelamer carbonate with 250 mL of deionized water (containing 10 g of the nonabsorbable marker Am J Kidney Dis. 2011;xx(x):xxx Phosphate Absorption: Lanthanum vs Sevelamer Figure 1. A randomized open-label crossover study comparing absorption of dietary phosphate after doses of lanthanum carbonate (LC; 1,000 mg of elemental lanthanum) or sevelamer carbonate (SC; 2,400 mg). Abbreviation: R, randomization. polyethylene glycol) halfway through ingestion of the standard meal. The meal was consumed within a 30-minute period. Approximately 10 hours were allowed for digestion of the meal, after which a second 4-hour GI wash was performed and the rectal effluent was collected. No liquids other than deionized water were consumed during treatment. Because participants underwent dosing and sample collection under the close supervision of the study investigator, visual inspection of rectal effluent was deemed sufficient to confirm that the GI tract had been cleared. Given methods similar to the study by Sheikh et al,21 which showed 99%-100% recovery of polyethylene glycol, analysis of polyethylene glycol levels in rectal effluent was thought to be unnecessary. Care was taken to avoid contamination of the rectal effluent with urine. Participants were required to remain resident in the research center until 24 hours after dosing. Standardized Meal The standardized meal consisted of a broiled ground beef patty (80 g; 90% lean meat, 10% fat) with Swiss cheese (30 g) and french-fried potatoes (100 g). This meal was expected to contain ⬃429 mg of phosphate, based on reference data.29 Identical duplicate meals were analyzed independently to determine the actual phosphate content of meals. Sample Preparation Meal samples were ground and digested with concentrated nitric acid (70%; 1 mL/1 g of sample) on a hot plate for 0.5-1.0 hours. The resulting suspension was diluted with mannitol/electrolyte solution and the final volume was recorded. Rectal effluent samples were filtered and the residue was digested with concentrated nitric acid (as per the meal samples) before being recombined with the filtrate. The final volume (calculated based on weight and density measurements) was recorded. Processed samples were frozen (nominal ⫺20°C) in 50-mL aliquots for subsequent analysis. Quantification of Phosphorus The colorimetric technique for detection of phosphorus30 used by Sheikh et al21 was unsuitable for use with lanthanum because the assay can measure only free phosphate in solution. Although the acid treatment used as part of the colorimetric assay effectively dissociated the aluminum-phosphate complex, allowing accurate assessment of phosphorus in the study by Sheikh et al,21 the same procedure applied to lanthanum-containing samples resulted in lower than expected phosphorus recovery. This may occur because the lanthanum-phosphate complex is poorly soluble in acidic solution. This is reflected by the low dissociation constant of lanthanum phosphate calculated in previous in vitro studies.17 Am J Kidney Dis. 2011;xx(x):xxx Therefore, an alternative method was validated to ensure accurate measurement of phosphorus in rectal effluent samples. Phosphorus concentrations were analyzed using an inductively coupled plasma–optical emission spectroscopy (ICP-OES) assay. This assay was able to accurately measure phosphorus in the presence of the lanthanum-phosphate complex with recovery of ⬃100%. All samples, including those from meal-only and mealplus-sevelamer-carbonate treatments, therefore, were analyzed using ICP-OES. Inductively Coupled Plasma–Optical Emission Spectroscopy Processed samples were analyzed for phosphorus using ICPOES in a mannitol/electrolyte matrix. Samples (3 mL) were digested in concentrated nitric acid (2.5 mL) at 110°C for 1.5 hours followed by concentrated hydrochloric acid (⬃38%, 2.5 mL) at 100°C for 30 minutes and then diluted to 50 mL using mannitol/ electrolyte solution. Scandium was added as an internal standard and the suspension was vortexed before being introduced into the ICP-OES system (4300 DV Optima Inductively Coupled Plasma– Optical Emission Spectrometer; Perkin-Elmer, www.perkinelmer. com). Calibration standards and quality control samples in mannitol/ electrolyte solution were digested and processed using the same procedure as for study samples. Phosphorus and scandium were monitored at wavelengths of 214.91 and 361.38 nm, respectively. Phosphorus concentrations were obtained using the instrument software. The amount of phosphorus was calculated from the measured concentration and final volume recorded in the initial preparation step. Investigators who assayed samples for phosphorus were blinded to treatment allocation. Objectives The primary objective was to compare the absorption of dietary phosphate after a single dose of either lanthanum carbonate or sevelamer carbonate. The primary end point to assess this objective was net phosphate absorption. Secondary objectives included comparison of the dietary–phosphate-binding capacity of typical clinical doses of lanthanum carbonate and sevelamer carbonate, and assessment of the safety and tolerability of lanthanum carbonate and sevelamer carbonate. The safety set consisted of individuals who received at least 1 dose of study drug and had at least 1 postdose safety assessment. The pharmacodynamic set consisted of all individuals in the safety set who provided all rectal effluent collections and completed all study periods. Individuals who vomited during any of the study periods were excluded from the pharmacodynamic set. 3 Martin et al Net phosphate absorption and phosphate-binding capacity were calculated according to the following equations. Net phosphate absorption ⫽ phosphorus measured in standardized meal – (phosphorus measured in rectal effluent following meal only or meal with binder administration – phosphorus in rectal effluent following fasting). Phosphate-binding capacity ⫽ phosphorus measured in rectal effluent following meal with binder administration ⫺ phosphorus measured in rectal effluent following meal only. Statistical analyses were performed using SAS, version 9.2 (www.sas.com). Data were analyzed using a standard mixed-effect linear model with adjustment for sequence group, period, and treatment as fixed effects; subject within sequence was included as a random effect. The analysis used the pharmacodynamic set. Fifteen volunteers were required to complete the study to ensure 80% power to detect a 42-mg difference in phosphate absorption between lanthanum carbonate and sevelamer carbonate at the 5% significance level (2 sided) assuming a standard deviation of 50 mg. The study was not designed or powered to assess differences in the safety or tolerability profiles of lanthanum carbonate and sevelamer carbonate. RESULTS Thirty-one individuals were randomly assigned, 28 of whom received a dose of study drug and were included in the safety set. Eighteen participants were included in the pharmacodynamic set; reasons for exclusion are shown in Fig 2. Most participants were white (61%) and men (78%); mean age of the pharmacodynamic set was 26 ⫾ 6.8 (standard deviation) years (Table 1). Table 1. Participant Demographics for the Pharmacodynamic Set Parameter Value Sex Men Women 14 (78) 4 (22) Race White Black 11 (61) 7 (39) Ethnicity Hispanic or Latino Not Hispanic or Latino 4 (22) 14 (78) Age (y) Weight (kg) BMI (kg/m2) 26 ⫾ 6.8 73 ⫾ 8.4 25 ⫾ 2.3 Note: Values shown as number (percentage) or mean ⫾ standard deviation. Abbreviation: BMI, body mass index. Mean phosphorus content of the meal and rectal effluent samples after lanthanum carbonate or sevelamer carbonate treatment and fasting are listed in Table 2. Net phosphate absorption (adjusted mean ⫾ standard error) after receiving the meal without a phosphate binder was 281.7 ⫾ 14.1 mg of phosphorus (Fig 3). Net phosphate absorption was significantly lower with lanthanum carbonate (156.0 ⫾ 14.2 mg of phosphorus) than with sevelamer carbonate (221.8 ⫾ 14.1 mg of phosphorus); the difference in adjusted mean values was ⫺65.8 mg of phosphorus (95% confidence interval, ⫺96.0 to ⫺35.5; P ⬍ 0.001; Fig 3). Lanthanum carbonate (1,000 mg of elemental lanthanum) bound 135.1 ⫾ 12.3 mg of phosphate (as phosphorus), whereas sevelamer carbonate (2,400 mg) bound 63.2 ⫾ 12.3 mg, a difference in adjusted mean values of 71.9 mg (95% confidence interval, 40.0103.8; P ⬍ 0.001; Fig 4). Safety and Tolerability Treatment-emergent AEs during the meal-only study period were limited to nausea, vomiting, headache, and dizziness. AEs were similar during fasting, with the addition of a single case of pruritic rash. During sevelamer carbonate treatment, 1 participant had 2 treatment-emergent AEs (an arthropod sting and pruritus). No treatment-emergent AEs occurred during lanthanum carbonate treatment. Figure 2. Participant disposition. [Number] signifies treatment period (including the subsequent washout period). Abbreviations: AE, adverse event; GI, gastrointestinal. 4 DISCUSSION Previous assessments of the relative phosphatebinding capacities of lanthanum carbonate and sevelamer hydrochloride have been limited to in vitro investigations,17 animal studies,18 and indirect cliniAm J Kidney Dis. 2011;xx(x):xxx Phosphate Absorption: Lanthanum vs Sevelamer Table 2. Phosphorus Content of Samples Meal (mg) Rectal Effluent (mg) Study Period Mean ⴞ SE Range Mean ⴞ SE Range Meal only Meal plus lanthanum carbonate (1,000 mg of elemental lanthanum) Meal plus sevelamer carbonate (2,400 mg) Fasting 374.3 ⫾ 4.0 377.1 ⫾ 3.1 349.8-401.4 349.8-401.4 151.0 ⫾ 7.5 279.7 ⫾ 17.6 105.0-206.2 141.0-405.3 375.0 ⫾ 4.0 — 349.8-401.4 212.4 ⫾ 9.3 60.9 ⫾ 4.1 144.0-285.4 31.3-94.4 Note: N ⫽ 18. Conversion factor for phosphorus in mg to mmoles, ⫻0.0323. Abbreviation: SE, standard error. cal comparisons using 24-hour urinary excretion of phosphorus to estimate phosphate absorption.19,20 This is the first study in humans to directly compare the effects of lanthanum carbonate and recently introduced sevelamer carbonate on dietary phosphate absorption and allowed calculation of their in vivo phosphate-binding capacities. These results validate measurement of urinary phosphorus excretion as a biomarker reflecting the effect of phosphate binders.19,20 The balance study reported by Sheikh et al21 directly assessed the phosphate-binding capacities of aluminum carbonate and the citrate, acetate, and carbonate salts of calcium by measuring net phosphate absorption after ingestion of a standardized meal along with these phosphate binders. That study found that aluminum carbonate and calcium acetate had higher phosphate-binding capacities than calcium carbonate and calcium citrate. The method used by Sheikh et al21 and in this study is most appropriate for direct assessment of the binding capacities of phosphate binders because it measures phosphorus bound to the binder (and hence removed in the rectal effluent). We intended to use the same assay as Sheikh et al21 to directly compare the phosphate-binding capacities Figure 3. Lanthanum carbonate significantly decreased net phosphate absorption compared with sevelamer carbonate. *P ⬍ 0.001 versus meal only; †P ⬍ 0.001 versus sevelamer carbonate. N ⫽ 18. ‡Containing 1,000 mg of elemental lanthanum. ** Measured as phosphorus. Conversion factor for phosphorus in milligrams to millimoles, ⫻0.0323. Am J Kidney Dis. 2011;xx(x):xxx of lanthanum carbonate and sevelamer carbonate.26,27 However, the colorimetric method for detection of phosphorus30 used by Sheikh et al21 was not suitable for quantification of phosphorus bound to lanthanum because of the high affinity of lanthanum for phosphate, as shown previously in vitro.17 After further in vitro investigation, an ICP-OES method that allowed accurate assessment of phosphorus content of samples was developed and validated. Analysis of duplicates showed that the standardized meal contained ⬃375 mg of phosphate, lower than anticipated from reference data, but corresponding to about one third of typical daily intake in the average American diet in 2007.31 Consistent with the results of Sheikh et al,21 ⬃75% of this phosphate was absorbed (net absorption, 281.7 ⫾ 14.1 mg from the meal only; Fig 3). As expected, phosphate absorption was decreased significantly by ingestion of a phosphate binder during the meal. A typical clinical dose of lanthanum carbonate, containing 1,000 mg of elemental lanthanum, decreased phosphate absorption by 45% (net absorption, 156.0 ⫾ 14.2 mg), and a typical 2,400-mg dose of sevelamer carbonate decreased phosphate absorption by 21% (net absorption, 221.8 ⫾ 14.1 mg). Calculation of phosphate-binding capacity showed that a 1,000-mg dose of lanthanum (a single lantha- Figure 4. Lanthanum carbonate binds significantly more phosphate than sevelamer carbonate. *P ⬍ 0.001 versus sevelamer carbonate. N ⫽ 18. †Containing 1,000 mg of elemental lanthanum. **Measured as phosphorus. Conversion factor for phosphorus in milligrams to millimoles, ⫻0.0323. 5 Martin et al num carbonate tablet) bound 135 mg of phosphate, consistent with estimates of 79-156 mg calculated using urinary phosphorus excretion in phase I studies.20 A 2,400-mg dose of sevelamer carbonate bound 63 mg of phosphate (equivalent to 21 mg of phosphate per 800-mg tablet). Calculations based on urinary phosphorus excretion suggest that sevelamer hydrochloride binds 18-29 mg of phosphate per 800-mg tablet.19 The study by Sheikh et al21 indicated that a dose of calcium acetate containing 1,000 mg of elemental calcium bound 177 mg of phosphate, equating to 30 mg of phosphate per 667-mg tablet. This study used healthy volunteers because of the extended study time and nature of the investigative procedures. The study could have used patients with CKD not yet on dialysis therapy, but phosphate absorption may not have remained constant during the times involved because of the consequence of disease or its treatment on vitamin D levels. Although phosphate absorption may be slightly lower in patients with CKD than in healthy people,32 this does not alter the relative phosphate-binding capacities of the binders under the conditions examined. Therefore, we would not expect the choice of population to greatly influence results. A limitation of this study was use of single doses of the phosphate binders, rather than dosing to steady state. However, this design along with the use of healthy volunteers allowed indirect comparison with the historical results of Sheikh et al.21 The new KDIGO clinical practice guidelines recommend a decrease in serum phosphorus levels toward the reference range in an attempt to decrease the high mortality associated with increased serum phosphorus levels in patients with CKD.4 Sustained control of serum phosphorus levels to the target range of 3.5-5.5 mg/dL, previously recommended by KDOQI, is associated with a decrease in mortality risk in patients new to dialysis therapy.3 Restriction of dietary phosphate intake may be associated with protein malnutrition, the risk of which may outweigh the benefit of controlled serum phosphorus levels and may even increase mortality.7 Increased protein intake with a concurrent decrease in serum phosphorus levels has been associated with lower mortality than decreases in both parameters; efficacious phosphate binders, particularly those that do not increase calcium load or tablet burden, may be beneficial to decrease dietary phosphorus absorption without protein restriction.7 The data presented here may be used with knowledge of a patient’s dietary phosphate intake and dialysis regimen to predict the decrease in phosphate load achieved with the use of a phosphate binder. In the future, this may allow better tailoring of phosphatebinder prescriptions to the individual patient’s needs. A typical dose of lanthanum carbonate containing 6 1,000 mg of elemental lanthanum binds more than twice as much phosphate as a typical 2,400-mg dose of sevelamer carbonate. This translates into a lower tablet number to achieve the same decrease in serum phosphorus levels as sevelamer carbonate in clinical practice. In summary, lanthanum carbonate is an effective noncalcium phosphate binder that binds significantly more phosphate than sevelamer carbonate. Efficacious phosphate binders may help to achieve sustained control of serum phosphorus at the lower levels suggested for patients with CKD by the new KDIGO clinical practice guidelines, while allowing adequate protein intake. ACKNOWLEDGEMENTS We thank Apinya Bee Vutikullird (West Coast Clinical Trials, Cypress, CA), Heather Van Heusen (Shire Pharmaceuticals, Wayne, PA), Michael Emmett (Baylor University Medical Center, Dallas, TX), Peter Grohse (RTI Int, Research Triangle Park, NC), and Ping Qiu (formerly of Shire Pharmaceuticals, Wayne, PA) for valuable contributions to this study. Support: Clinical research was funded by Shire Pharmaceuticals, which markets lanthanum carbonate. Paul Farrow, PhD, an employee of Oxford PharmaGenesis Ltd, provided writing assistance to the authors. Editorial assistance in the form of proofreading, copy editing, and fact checking also was provided by Oxford PharmaGenesis Ltd. These services were funded by Shire Pharmaceuticals. Patrick Martin, Phillip Wang, Antoine Robinson, Lynne Poole, Jeffrey Dragone, and Michael Smyth are employees of Shire Pharmaceuticals. Raymond Pratt was an employee of Shire Pharmaceuticals at the time of the study and during manuscript development. Financial Disclosure: Aside from those reported in the previous section, the authors declare that they have no relevant financial interests. REFERENCES 1. Block GA, Klassen PS, Lazarus JM, et al. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208-2218. 2. Kestenbaum B, Sampson JN, Rudser KD, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol. 2005;16:520-528. 3. Danese MD, Belozeroff V, Smirnakis K, Rothman KJ. Consistent control of mineral and bone disorder in incident hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:1423-1429. 4. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int. 2009;76(suppl 113):S1-130. 5. Eknoyan G, Levin A, Levin NW. Bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42:1201. 6. Dialysis Outcomes and Practice Patterns Study Investigators. Serum phosphate (categories), by DOPPS country and cross-section. 2009 Annual Report of the Dialysis Outcomes and Practice Patterns Study: Hemodialysis Data 1999-2008. Ann Arbor, MI: Arbor Research Collaborative for Health. http://www.dopps.org/annualreport/ html/qphosphmgdl_c_TAB2009.htm. Accessed June 17, 2010. 7. Shinaberger CS, Greenland S, Kopple JD, et al. Is controlling phosphorus by decreasing dietary protein intake beneficial or Am J Kidney Dis. 2011;xx(x):xxx Phosphate Absorption: Lanthanum vs Sevelamer harmful in persons with chronic kidney disease? Am J Clin Nutr. 2008;88:1511-1518. 8. National Kidney Foundation. Kidney Disease Outcomes Quality Initiative. Guideline 15. Dietary protein intake (DPI) in maintenance hemodialysis (MHD). Clinical Practice Guidelines for Nutrition in Chronic Renal Failure (2000). http://www.kidney.org/ professionals/kdoqi/guidelines_updates/nut_a15.html. Accessed May 27, 2010. 9. Ramirez JA, Emmett M, White MG, et al. The absorption of dietary phosphorus and calcium in hemodialysis patients. Kidney Int. 1986;30:753-759. 10. Sperschneider H, Gunther K, Marzoll I, Kirchner E, Stein G. Calcium carbonate (CaCO3): an efficient and safe phosphate binder in haemodialysis patients? A 3-year study. Nephrol Dial Transplant. 1993;8:530-534. 11. Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815-1824. 12. Kalil RS, Flanigan MG, Stanford W, Haynes WG. The effect of lanthanum carbonate (LC) (Fosrenol®) on coronary artery calcification (CAC) and endothelial function (FMD) in hemodialysis (HD) patients. A pilot, prospective study [ASN abstract F-PO1252]. J Am Soc Nephrol. 2009;20:399A. 13. Russo D, Miranda I, Ruocco C, et al. The progression of coronary artery calcification in predialysis patients on calcium carbonate or sevelamer. Kidney Int. 2007;72:1255-1261. 14. Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245-252. 15. Suki WN, Zabaneh R, Cangiano JL, et al. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients. Kidney Int. 2007;72:1130-1137. 16. Wilson R, Zhang P, Smyth M, Pratt R. Assessment of survival in a 2-year comparative study of lanthanum carbonate versus standard therapy. Curr Med Res Opin. 2009;25:3021-3028. 17. Autissier V, Damment SJ, Henderson RA. Relative in vitro efficacy of the phosphate binders lanthanum carbonate and sevelamer hydrochloride. J Pharm Sci. 2007;96:2818-2827. 18. Hutchison AJ. Improving phosphate-binder therapy as a way forward. Nephrol Dial Transplant. 2004;19(suppl 1):i19-24. 19. Burke SK, Slatopolsky EA, Goldberg DI. RenaGel, a novel calcium- and aluminium-free phosphate binder, inhibits phosphate absorption in normal volunteers. Nephrol Dial Transplant. 1997;12: 1640-1644. 20. Finn W, Kingma-Johnson I. Urinary phosphorus excretion is a valuable measure of total body phosphorus burden in patients Am J Kidney Dis. 2011;xx(x):xxx with CKD stages 3 and 4 [ASN abstract TH-PO931]. J Am Soc Nephrol. 2008;19:320A-321A. 21. Sheikh MS, Maguire JA, Emmett M, et al. Reduction of dietary phosphorus absorption by phosphorus binders. A theoretical, in vitro, and in vivo study. J Clin Invest. 1989;83:66-73. 22. International Conference on Harmonisation Expert Working Group. International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. Topic E6 Guideline for Good Clinical Practice 2002. Geneva, Switzerland: International Conference on Harmonisation. http:// www.ema.europa.eu/docs/en_GB/document_library/Scientific_ guideline/2009/09/WC500002874.pdf. Accessed June 17, 2010. 23. Hutchison AJ, Maes B, Vanwalleghem J, et al. Long-term efficacy and tolerability of lanthanum carbonate: results from a 3-year study. Nephron Clin Pract. 2006;102:c61-71. 24. Qunibi WY, Hootkins RE, McDowell LL, et al. Treatment of hyperphosphatemia in hemodialysis patients: the Calcium Acetate Renagel Evaluation (CARE Study). Kidney Int. 2004;65:19141926. 25. Delmez J, Block G, Robertson J, et al. A randomized, double-blind, crossover design study of sevelamer hydrochloride and sevelamer carbonate in patients on hemodialysis. Clin Nephrol. 2007;68:386-391. 26. Shire Pharmaceuticals. Fosrenol (lanthanum carbonate) prescribing information (2009). http://pi.shirecontent.com/PI/PDFs/ Fosrenol_USA_ENG.pdf. Accessed July 13, 2010. 27. Genzyme Corp. Renvela (sevelamer carbonate) prescribing information (2007). http://www.renagel.com/docs/renvela_pi.pdf. Accessed July 13, 2010. 28. Davis GR, Santa Ana CA, Morawski SG, Fordtran JS. Development of a lavage solution associated with minimal water and electrolyte absorption or secretion. Gastroenterology. 1980;78: 991-995. 29. US Department of Agriculture. Agricultural Research Service. USDA National Nutrient Database for Standard Reference, release 21. Beltsville, MD: US Department of Agriculture; 2008. 30. Fiske C, Subbarow Y. The colorimetric determination of phosphorus. J Biol Chem. 1925;66:375-400. 31. Hruska KA, Mathew S, Lund R, Qiu P, Pratt R. Hyperphosphatemia of chronic kidney disease. Kidney Int. 2008;74:148-157. 32. Davis GR, Zerwekh JE, Parker TF, et al. Absorption of phosphate in the jejunum of patients with chronic renal failure before and after correction of vitamin D deficiency. Gastroenterology. 1983;85:908-916. 7