ARRA Stimulus Funding - Hewlett
advertisement
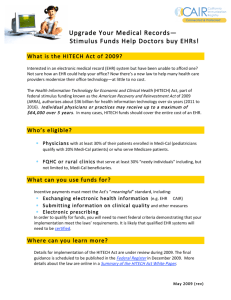
ARRA StimuluS Funding: A guide FoR the medicAl PRActice PhySiciAn Unprecedented economic funding means unexpected opportunities for medical practices. ARRA StimuluS Funding I. Stimulus Overview The American Recovery and Reinvestment Act of 2009 (ARRA) and the section of ARRA on promoting information technology, Health Information Technology for Economic and Clinical Health (HITECH) Act, are unique economic developments that have resulted in unprecedented opportunity for growing small and medium healthcare practices: the chance to update technology and jumpstart electronic health record (EHR) adoption through substantial incentive payments. Transitioning to an EHR platform and a new technology system might seem a bit overwhelming, which is why this informative guide aims to help you understand: • What is ARRA and the HITECH Act – and what are their impact on the healthcare industry; • What does this legislation mean for your practice; • Why it’s smart to update your practice’s technology infrastructure and make the transition to EHR adoption now – not later; • The penalties – and risks – of non-EHR adoption; • What defines “meaningful use” in terms of technology and your EHR systems; and • How to manage a smooth transition to an EHR system. The bottom line: ARRA and the HITECH act are a rare and time-sensitive opportunity for small to medium medical practices facing EHR adoption requirements to update technology – and receive incentive payments for doing so quickly. II. What is ARRA? Incentive Payments, big advantages Passed by Congress and signed into law by President Obama in February 2009, the American Recovery and Reinvestment Act (ARRA) is part of a targeted, strategic and far-reaching overall plan to jumpstart a sagging economy. Designed to help “create new jobs, preserve existing jobs, spur economic activity, and invest in long-term growth,” the Act is a $787 billion infusion of funds for a huge range of critical-need areas – including a $224 billion increase in federal funds for entitlement programs like unemployment, as well as for education and healthcare. Healthcare impact While much of the Act is certainly focused on boosting the economy, it also includes provisions for many basic infrastructure programs that are designed for the long-term economic impact and well-being of all Americans. For healthcare in particular, this funding marks an incredible opportunity to transform the industry – including helping to reduce medical errors, improve quality, and dramatically decrease overall healthcare costs. If overall operations run smoother, physician practices can better concentrate on what’s important: providing the best patient care possible. III. What is the HITECH Act? Change at the front lines The time for change is now – and ARRA is a transformative change agent that is designed to help, starting where it’s needed most – on the front lines, and at the physician/patient care level. ARRA has allocated approximately $36 billion for healthcare IT investments and upgrades alone – and most of that ($20 billion) is earmarked specifically to make it easier for small to medium practices to move toward required EHR adoption.1 Known as the Health Information Technology for Economic and Clinical Health (HITECH) Act, this critical portion of the ARRA bill includes financial incentives for EHR adoption that, in conjunction with HIPAA, will help further ensure patient privacy with more stringent data protection standards for the industry. And, those physicians and practices that implement and use eligible EHR systems according to HITECH guidelines sooner rather than later stand to reap substantial financial benefits. Critical need: Technology help There’s no question that, in a smaller medical practice, Information Technology (IT) is an ongoing expense and a time-intensive proposition. It’s hard enough to balance running a profitable business, providing the best in patient care and ensuring that you have a happy and productive staff without also having to worry about IT. But it’s a critical-need area that demands attention, diligence, compliance and quick response. The HITECH Act will help make that prospect a lot easier for medical practices by offering considerable financial incentives, if your practice acts now – not later. 1. SOURCE: Government Technology, “ARRA Stimulus Package: $20 Billion for Healthcare IT, $4.3 Billion for Smart Grid Technology,” March 2009 As you can see by the EHR Stimulus Timeline below, the longer physician practices wait to adopt a comprehensive EHR system, the less incentive money is available – not to mention that practices will start seeing penalties in 2015. It’s wise to start implementing now, not only to get the full financial benefits, but also to ensure your practice stays at the forefront of technological advancement. EHR STImuluS TImElInE FEbRuARy 17 2009 President Barack Obama signs the American Recovery and Reinvestment Act. Included in the act are the HITECH regulations which allocated $36 billion to healthcare providers who demonstrate meaningful use of EHRs. 2010 2011 Definition of Meaningful Use finalized; HITECH policy, education and plans for execution finalized. Providers and vendors should be assessing readiness, plan and implementation. Incentive payments begin for early adopters of EHR. Payments continue through 2015 for a total incentive payment of $44,000. Meaningful Use requirement in effect. 2012 2015 Tiered incentive payments continue for healthcare providers who adopt EHRs. 2015 Penalties begin for healthcare providers that fail to adopt and utilize Health Information Technology; Reduction in Medicare payments will be reduced gradually to a maximum of 3% reduction. 2016 Medicare and Medicaid payment incentives end. IV. What does this mean for your practice? Reimbursements for upgraded technology Small to medium physician practices stand to reap benefits of early EHR system adoption as indicated in the HITECH Act, which is offering incentive payments to help practices offset the cost of implementing qualified EHR systems. Providers with qualifying EHRs can start receiving HITECH Act incentive payments as early as 2011. In fact, your practice could receive up to $44,000 per practitioner when you adopt HITECH standards – and that’s a huge benefit. These payments will come directly from ARRA funds to those physicians whose practices include Medicare and Medicaid patients and, while there’s a year delay for reimbursement once the EHR system is implemented, these funds can significantly offset the cost of such a system. Better, faster technology infrastructure Besides the attractive financial incentive for adopting HITECH standards, the overall technology benefits of such an adoption for medical practices can be significant, including: • Increased data security; • Increased productivity; • Reduced maintenance costs because your practice has the latest systems; • Newer applications that are easier to use; and • Enhanced technical support. In short, updating your practice’s technology infrastructure and making the transition to EHR adoption sooner, rather than later, makes a lot of sense both financially and from an operations perspective. A newer system gives your practice the power of the latest technology, while also ensuring compliance – so that you can concentrate on growing your business and meeting patient and staff needs. What does this mean for your practice? Each section below explains the advantages of having a current technology infrastructure – giving you the edge for continued success. Less risk, more secure data There’s no doubt that the economic downturn affected businesses in every industry, and healthcare was no exception. As a result, many practices halted a large percentage of spending – and that included updating electronic and computer systems, software and hardware. Nearly 40 percent of the computers in small businesses are more than three years old, with many using older operating systems.2 2. SOURCE: TechAisle Whitepaper: “SMBs: The Case for Buying Modern PCs,” March 2010. However, not updating systems and technology infrastructure means potentially compromising data security – and that’s simply not an option for any healthcare practice. Because older PCs are more susceptible to hardware and software failures, viruses, spyware and malware attacks3, the risk of compromising essential data security and strict electronic compliance requirements because you’re using old technology is simply too great. Newer technology, increased productivity Beyond the risk of compromising or losing sensitive data, there’s also the issue of productivity. Newer PCs have 40 percent less downtime than older systems – that’s an average of 7 hours versus 10 hours with older PCs.4 What could your practice do with an extra three hours in a day? In an average small business, that’s a whopping 50 hours of downtime per PC per year.5 Your time – and your patient’s time – is worth much more than that. Cost savings, increased ROI Your practice will also save money with newer, up-to-date systems, especially when you consider that the maintenance costs of newer PCs is one-and-a-half times less than older machines, including the cost of replacing hard drives, graphics cards and the like, as well as paying for someone to service the systems. The faster processors, improved graphics, more energy-efficient attributes and seamless communication abilities of newer hardware means faster patient processing, more accurate and reliable diagnostic data, and lower overall cost of IT operations. It’s clear that this stimulus incentive money will go a long way toward easing the stress of cost pressures for many smaller practices implementing an EHR system. After all, it’s innovation that makes small businesses agile and competitive. Having an IT system you can rely on and that meets EHR requirements is not only essential, but also will contribute greatly to the overall success of your practice in the long run – including at the operational, clinical, and administrative levels. V. understanding the Penalties – and Risks – of non -EHR Adoption Adopt now, or pay the price later Clearly, the financial incentive to adopt qualifying EHR systems soon is self-evident. That’s because these unique, one-time, “use it or lose it” incentive payments are on a strict schedule of diminishing returns for practices – implement now, and get more incentive money. Many practices are starting to embrace that kind of thinking, citing financial incentives as a significant motivator. In an Ingenix survey of more than 1,000 physicians and physician practice administrators about their attitudes toward EHR technologies and how federal incentives might affect purchasing decisions, a whopping 82 percent say they are “more likely” to adopt an EHR system if they are reimbursed for their investment, including 34 percent who would be “much more likely” to do so. However, if your practice waits, or you choose to ignore the stimulus fund incentive opportunity altogether, the cost will be staggeringly high. As you can see below, according to the HITECH Act Physician Reimbursement Plan, incentive money decreases dramatically if practices don’t act soon; by fiscal year 2014, that potential overall payment of $44,000 will have decreased by almost half. HITECH ACT: PHySICIAn REImbuRSEmEnT PlAn AdoPtion 2011 AdoPtion 2012 AdoPtion 2013 AdoPtion 2014 AdoPtion 2015+ 2011 $18,000 $0 $0 $0 $0 2012 $12,000 $18,000 $0 $0 $0 2013 $8,000 $12,000 $15,000 $0 $0 2014 $4,000 $8,000 $12,000 $12,000 $0 2015 $2,000 $4,000 $8,000 $8,000 $0 2016 $0 $2,000 $4,000 $4,000 $0 totAl $44,000 $44,000 $39,000 $24,000 $0 health Prof. Shortage Area $48,400 $48,400 $42,900 $26,400 $0 How to get the maximum financial benefit As you can see from the timeline, incentive payments start for early EHR adopters in 2011 – which means that the time to implement an EHR system is now – to get the full practice benefit of $44,000. Practices who implement early will get staggered and partial payments each year through 2015, including: $18,000 in 2011; $12,000 in 2012; $8,000 in 2013; $4,000 in 2014; and $2,000 in 2015 for a total of $44,000 – the maximum incentive payment. After that, the financial incentives drop dramatically. For example, if your practice doesn’t have a qualifying EHR system in place by 2013, your overall incentive payment drops $5,000 to $39,000. Wait until 2014 and the total benefit drops to $24,000. After 2015, ARRA/HITECH Act adoption incentives end completely. Ignore EHR adoption – and compromise your Medicare payments However, non-adoption goes far beyond getting government stimulus incentive payments to help pay for EHR systems. Practices who don’t adopt EHR standards are at risk of also having their Medicare payments reduced for each year of non- adoption. And it’s not a small percentage. Penalties include a gradual, but significant, 3 percent reduction in Medicare and Medicaid payments over a period of three years. No practice can afford that kind of financial hit, and that’s a powerful source motivation for many. In the Ingenix survey, 77 percent of physician practices say that penalties for not adopting EHR technology by 2014, as prescribed by the provisions of ARRA, are likely to motivate them to implement the technology. The bottom line? Start the EHR adoption process now, and your organization can mitigate the risk of penalties later. VI. meaningful use Understanding what’s “meaningful” As part of the HITECH Act, practices must meet specific guidelines for EHR systems that are designed to further information exchange and increase data security. Known as “Meaningful Use,” these requirements will be enacted in stages over the next five years. While final comprehensive guidelines are still in development, Stage 1 EHR guidelines will generally include the following categories/requirements6: Capturing the Right Data: All Stage 1 data must focus on specific elements, including field entries specific to the provider, such as Clinical Decision Support (CDS) rule parameters and specialty performance measure metrics. Your practice’s EHR system needs to have structured fields for each criteria, and the ability to acquire and load content databases; configure data-entry templates that help and remind users to enter the correct data; and the ability to design/develop methods to download eligibility, test results and other data from other systems. There’s also a training component – training physicians and/or other users on how to accurately enter patient data. Establishing Effective Workflows to Reinforce Data Entry (Including Medication Reconciliation): This means developing teams and assigning roles to ensure the right data is entered and captured. Everyone in your practice can play an active role in medication reconciliation by asking patients about medications and gathering medication information from patient transition records and notifications. Encouraging Provider Involvement in EHR Adoption: Providers must become committed EHR users to meet the definition of “meaningful use.” So, to make sure your practice has consistent data, every provider must consistently use the system – and that requires a team and overall practice commitment. u.S. congress. house. American Recovery and Reinvestment Act 0f 2009. h.R. 1. 111th cong., 1st sess. (February 10, 2009). http://edocket.access.gpo.gov/2010/e9-31217.htm (tables 22 and 23, accessed June 2010). NOTE: An additional incentive payment of 10% is available for eligible professionals who provide services in a geographic area designated as a Health Professional Shortage Area (HPSA.) These traditionally underserved areas are designated by the Health and Human Resources Secretary due to shortages of primary medical care, dental or mental health providers and may be geographic, demographic or institutional in nature. Source: http://edocket.access.gpo.gov/2010/E9-31217.htm 3. SOURCE: TechAisle Whitepaper: “SMBs: The Case for Buying Modern PCs,” March 2010. 4. SOURCE: TechAisle Whitepaper: “SMBs: The Case for Buying Modern PCs,” March 2010. 5. SOURCE: TechAisle Whitepaper: “SMBs: The Case for Buying Modern PCs,” March 2010 6. SOURCE: Report on “Meaningful Use for Eligible Professionals: The Top Ten Challenges,” CSC, 2010. IT assessment for adoption success A mature IT function in the medical practice facilitates a more seamless EHR adoption. But what does that mean? While every practice is unique, evaluating the following four core areas is instrumental in gaining a better understanding of your organizations IT status, including areas of strength and weakness. • Network/Infrastructure: This is the most important part of your technology roadmap, since almost every function in your practice is supported by the network, including your EHR system, HR, finance, and security. • Technical Support: This is the most important part of your technology roadmap, since almost every function in your practice is supported by the network, including your EHR system, HR, finance, and security. • Database: The key “meaningful use” standards under the HITECH Act require proper data management, collection and organization, making this a critical component for any medical practice. • Technology Management: Many practices rely on IT reactively, but it should be a proactive, mindful initiative that can effectively lead your practice – and help you deliver the best patient care possible. Establishing Computer-Based Provider Order Entry (CPOE): This applies to all orders, including laboratory, radiology, referral, medication, physical therapy and other services. And, each qualified order has to be directly entered by the authorizing provider. So, in a practice setting, every ordering provider needs an understanding of how CPOE works, how to use it, and how to enforce its use. Adopting E-Prescribing Now: Now’s the perfect time to start e-prescribing, since this is one area where practices have full control, including configuring the EHR with an e-prescribing module; subscribing to networks that help with transmittal; training users; and ensuring consistent use of the system. Many providers are already e-prescribing; according a report by Superscripts, which operates an e-prescribing network, the number of prescriptions routed electronically grew from 68 million in 2008 to 191 million in 2009.7 Managing Clinical Decision Support (CDS): Stage 1 meaningful use requirements include five CDS rules that each eligible professional must demonstrate. In multi-specialty and multi-provider practices, this may mean implementing a separate subset of rules for each specialty and/or provider, because those five rules also have to be relevant to the specialty, or a high clinical priority. Implementing Patient Health Information Exchange Workflows: Patient health information exchange criteria requires communication with patients based on and using the EHR, like patient notifications and sharing care information such as visit summaries and test results. Formulating a Provider Health Information Exchange Strategy: This includes allowing for “testing of a certified EHR technology’s capacity to electronically exchange key clinical information.” So, EHR system exchange functions and features need to be installed, configured and ready to go. Complying with Privacy and Security Requirements: An extension of HIPAA, this guideline makes sure that practices identify and address potential workflow security and other weaknesses, such as password protection of electronic patient records distributed via mobile media. Initiating EHR-Based Quality Performance Measurement Support: The key to successfully meeting quality performance metrics is in capturing the data, so practices must make sure that every data element is captured or stored in the appropriate format. There’s no question that transitioning to updated technology is essential for EHR compliance – and, while it’s also an intensive process, moving your practice to EHR adoption sooner rather than later has many benefits. VII. How do you manage the transition? Any sort of technology adoption or transition can be a daunting prospect for a smaller practice. In fact, in the Ingenix survey, 74 percent of those surveyed ranked disruption of workflow as one of the top three risks of EHR deployment. However, implementing an EHR solution can greatly streamline workflow, save time, increase accuracy, and result in better patient care. The first step is to assess where your practice is now with a basic technology infrastructure. Knowing where you are now will help you make sound and practical decisions when it comes to choosing the right EHR system for your needs – and the one that will have the most benefit to your medical practice. Part of that assessment process is gauging your organization’s level of “IT Maturity” – a mature infrastructure means that you have all the necessary technology pieces in place so that your practice runs smoothly; increases your practice’s overall efficiency, productivity and effectiveness; and delivers value – to you, and to your patients. 7. SOURCE: “More Doctors are E-Prescribing,” Pharmalot.com, March 2010. Must-have EHR project management Managing a successful transition to your EHR system – or any technological upgrade – also requires following key project management guidelines, including: • Detailing and implementing a project plan so that everyone stays on track and understands what needs to happen and when; • Assigning roles and responsibilities so that everyone in your practice is on board and committed to the success of the implementation process – and the practice’s overall success; • Allowing for practice downtime, and planning for it in advance to minimize disruption; and • Ensuring that everyone in your practice has access to the right training and development to ensure a smooth transition to your EHR system. With a wealth of knowledge and support at your fingertips, the right technology partners on your team, and an understanding that better, current technology is the key that will take your practice to the next level of success, you can rest assured that you’ll implement an EHR system your practice can afford – and that your patients will appreciate. VIII. Conclusion Given the urgent timeline for taking advantage of incentive recovery funds, it’s critical for practices to take action for the future and implement EHR sooner, not later. The benefits far outweigh the risks, and stimulus funds through the HITECH Act are there to help defray your practice’s overall financial investment. The evolution of your practice should include technology that gives you: • Increased data security; • Increased productivity; • Reduced maintenance costs; • Newer applications; • Enhanced technical support; and • An EHR system that’s compliant – and that works for your practice. It’s important to have a trusted, reliable, technology partner that gives you access to proven industry systems and platforms – the right EHR solution that meets the needs of your practice and puts the most innovative and cost-effective systems in place now – when you need them most. As an early EHR system adopter, your practice will reap the full benefits of ARRA/HITECH stimulus dollars, as well as an updated and efficient technology infrastructure. IX. Resources medicAl oRgAniZAtionS: AMA: http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/health-information-technology/hit resources-activities.shtml ADA: http://www.ada.org goVeRnment oRgAniZAtionS: Health Information Technology: http://healthit.hhs.gov/portal/server.pt Centers for Medicare and Medicaid Services: http://www.cms.gov/ ARRA Site: http://www.recovery.gov/Pages/home.aspx hP & intel linKS: HP SMB Healthcare: http://www.hp.com/sbso/solutions/healthcare Intel: http://www.intel.com/healthcare/ ARRA Site: http://www.recovery.gov/Pages/home.aspx common AcRonymS: ARRA American Recovery and Reinvestment Act BCMA Bar Code Medication Administration CCHIT Certification Commission for Healthcare Information Technology CDSS Clinical Decision Support Systems CPOE Computerized Physician Order Entry EHR Electronic Health Record EMR Electronic Medical Record FQHC Federal Qualified Health Centers HIE Health Information Exchange HIPAA Health Information Portability and Accountability Act HITECH Health Information Technology for Economic and Clinical Health OIG Office of the Inspector General ONCHIT Office of the National Coordinator of Health Information Technology PHI Protected (or Personal) Health Information PHR Personal Health Record PMRI Patient Medical Record Information RHIO Regional Health Information Organization X. About HP in Healthcare HP is the largest provider of business process management services for the healthcare and managed care markets and has long been an informed and trusted technology partner in the healthcare industry. In fact, more healthcare organizations depend on HP for healthcare technologies and services than any other vendor. Ninety-six percent of U.S. hospitals run on HP servers; HP supports and maintains healthcare IT for the Department of Veterans Affairs, the world’s largest healthcare integrated network system; and HP systems are an indispensable part of leading medical institutions including HCA, Inc., Kaiser Permanente, Mayo Clinic, Scripps and many others. HP brings to the healthcare landscape a 50-year history of innovation; end-to-end, tailored solutions based on best-in-class technology; and rock-solid IT that delivers the high reliability, security and manageability that healthcare environments demand. HP’s strategic partnerships with selected software partners offer options for flexible, tailored healthcare solutions, and HP is committed to helping the healthcare industry make a smooth and successful transition toward EHR adoption. Except ional Ca re Through E xc ept iona l IT. © 2010 Hewlett - Packard Development Company, L.P. The information contained herein is subject to change without notice. HP shall not be liable for technical or editorial errors or omissions contained herein. July 2010 HP Restricted. 4AA1- 4833ENUS, July 2010