Powell Neurologic Exam PA-C Conf 2012 Black & White
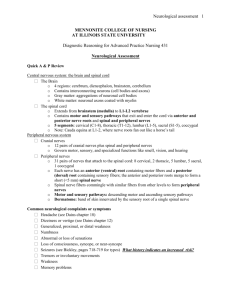
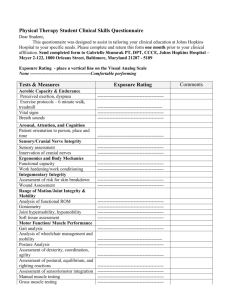
advertisement

Exam Documentation Neurological Exam • Neuro: WNL – We Never Looked • Neuro: Non Focal – The patient spoke in sentences, walked to the exam table without limping and was able to lift his shirt with both hands so that the heart could be auscultated. Tim Powell, M.D. Providence Epilepsy Center Spokane, WA Neurologic Exam • • • • • • • Mental Status Cranial Nerves Motor Sensory Cerebellar Gait Deep Tendon Reflexes • Neuro: Grossly Normal – No neuro exam took place. The patient looked O.K. to all superficial appearances and had no specific neurologic complaints. Folstein’s Mini Mental Status Exam http://www4.parinc.com/ 50 Test forms: $66 Mental Status Screen • • • • Orientation to person, place, time/date. Recall of Three Words (test of memory) Spell WORLD backwards (test of attention) Word Fluency: (Sensitive for Dementia) – “A” Test: Ask the patient to give as many words as possible b i i with beginning ith the th letter l tt "A" without ith t using i proper names.Well educated >8/min, poorly educated at least 6/min – “Animal” Test: Name as many animals as possible in 1 minute. Cranial Nerves I & II • I: Olfactory – Rarely tested. Always test in trauma – Test unilaterally with one nostril occluded • cinnamon, soap, vanilla (avoid noxious odors: stims V) • II: Optic – Pupillary Response: • M Monitor i size i andd symmetry • Direct vs. Consensual Response • Afferent pupillary defect – Visual Field testing • Confrontational testing If the patient has difficulty with any of the above, a full mental status examination is indicated. – Most sensitive to movement – Red object for testing color vision – Acuity: Eye Chart – Fundoscopic Exam 1 Pupillary Neuroanatomy Optic Tracts http://en.wikipedia.org/wiki/Retina http://www.aan.com/go/education/curricula/family/chapter2/section1 http://www.edoctoronline.com/medical-atlas.asp?c=4&id=21964 Grade I Papilledema Grade II Papilledema Grade IV Papilledema Cranial Nerves III, IV & VI • III: Oculomotor – Pupillary Response – Extraocular Movements (All directions except IV & VI) • Eye Alignment: Cover/Uncover test – Ptosis- Levator Palpebrae Muscle: principle eyelid opener • IV: Trochlear – Extraocular movements (Down and In) – Intorts the eye Normal – Pearls: The only cranial nerve contralateral to the end organ. – Most common CN affected by trauma • VI: Abducens – Extraocular movements (Lateral / Abduction) Optic Neuritis Ant. Ischemic Optic Neuropathy Emboli/Stroke Eye Muscles / Movements Superior Rectus Lateral Rectus Inferior Oblique 3 3 Cranial Nerves V & VII • V: Trigeminal – Motor: Muscles of mastication, Jaw jerk V3 – Sensory: Test PP, T, LT in all areas: V1, V2, V3 • Pearl: Innervation overlaps at midline • Corneal Response (afferent) 3 6 Clinical Neuroanatomy made Riduculously Simple, 1990 Medial Rectus • VII: Facial – Muscles of facial expression Inferior Rectus 4 3 Right Eye Bate’s Guides to Physical Examination, 2002, Lippincott Williams & Wilkins • Raise forehead, close eyes, show teeth, puff cheeks Superior Oblique – SYMMETRY! • Corneal Response (efferent) • Taste: Ant 2/3 of tongue. Clinical Neuroanatomy made Ridiculously Simple, 1990 http://www.fpnotebook.com/Neuro/Anatomy/CrnlNrv7.htm 2 Central VII Nerve Palsy Peripheral VII Nerve Palsy Bate’s Guides to Physical Examination, 2002, Lippincott Williams & Wilkins Bate’s Guides to Physical Examination, 2002, Lippincott Williams & Wilkins Cranial Nerves VIII, IX, X Cranial Nerves XI & XII • VIII: Vestibulocochlear – Nystagmus – Test high pitched sounds • XI: Spinal Accessory – Motor to Sternocleidomastoid: turns head to opposite side. Neck flexion when both sides contract. – Motor to Trapezius: Shoulder shrug. shrug Scapular winging if weak. • Finger Rub, Whisper • 512 hz tuning fork – Conductive hearing loss vs Nerve Deafness • IX: Glossopharyngeal – Gag – Palatal Elevation – Taste on posterior 1/3 of tongue • XII: Hypoglossal 512hz • X: Vagus – Tongue protruding. Deviates to the weak side – Palatal Elevation – Articulation- Palatal: “Ka” Guttural: “Ga” ?hoarse speech • Lateral push against tongue blade – Monitor tongue at rest inside mouth for fasciculation's (overcalled) Motor • Bulk: Atrophy/Hypertrophy • Abnormal Movements MRC Scale 0 No muscle movement. 1 Visible muscle movement, but no movement at the joint. 2 Movement at the joint, but not against gravity. – Spasticity: velocity dependent – Rigidity: velocity independent 3 Movement against gravity, but not against added resistance. • Continuous vs. Cogwheeling 4* Movement against resistance, but does not attain normal strength. 5 Normal strength. – Tremor / Fasciculation's – Seizure activity • Tone • Power: MRC Scale – Breakaway vs True weakness – Myotomes • Pronator Drift * Grades 4 - , 4 and 4+ maybe used to indicate movement against slight, moderate and strong resistance respectively 3 Myotomes Sensory • General Sensation (Examine distally to proximally) – Light Touch – Pin Prick – Vibration – Temperature – Position Sense • Cortical Sensation – Stereognosis 128hz – Graphesthesia – Two point Discrimination (nl 2-4 mm) – Double Simultaneous Stimulation (Extinction) • Romberg Aids to the Examination of the Peripheral Nervous System, 5e [Paperback] Michael O'Brien MD FRCP (Author) Patterns of Sensory Loss Sensory Dermatomes Peripheral Nerve: Loss of all sensation in the nerve distribution Sensory Root: Loss of all sensation in spinal segments involved Central Cord: Loss of pain and temperature in involved dermatomes Posterior Columns: Loss of position/vibration below the lesion Transection: Loss of position/vibration below the lesion on the involved side, loss of pain/temp below lesion on opposite side Thalamus: Decrease of all sensation on entire opposite body Sensory Cortex: Loss of discriminative sensation on opposite side Bate’s Guides to Physical Examination, 2002, Lippincott Williams & Wilkins Cerebellar • Rapid Alternating Movements – Finger tap, toe tap or hand flip (Don’t overcall the non-dominant hand) – Looking for Dysdiadochokinesia (inability to follow one movement with its opposite) • Point to Point testingg – Finger to Nose or Heel-Knee-Shin – Looking for Dysmetria (clumsy, unsteady, varying rate, movements that undershoot/overshoot target) Gait • Routine walking: check stride, stance, arm swing, symmetry, turning • Toe and Heel walking: Tests for plantar flexion and dorsiflexion strength and balance balance. • Tandem Walking: Sensitive for detecting ataxia. Age may begin to affect this ability >60 • Pearls: – Cerebellar deficits are ipsilateral to the lesion. – Motor weakness can mimic cerebellar dysfunction 4 Abnormalities of Gait Deep Tendon Reflexes • • • • • • • Ataxic / Cerebellar Hemiparetic / Stroke Shuffling / Parkinsonian Slap / Sensory ataxia Spastic / Scissoring Steppage / Foot drop Myopathic / Hip or Pelvic Girdle instability • Astasia-Abasia / Hysterical Bate’s Guides to Physical Examination, 2002, Lippincott Williams & Wilkins Deep Tendon Reflexes Common DTR’s • • • • • Biceps: C5, C6 Brachioradialis: C5, C6 Triceps: C6, C7 Patellar: L3, L4 Achilles / Ankle: L5, S1, S2 • • • • • Babinski Testing Grading of DTR’s 0 : Absent 1+ : Diminished 2+ : Normal/Average 3+ : Brisk,, Increased 4+ : Markedly increased, Often associated w/ clonus Pearl: In general, reflexes are not pathologic if they are symmetric, unless they are 4+ or truly absent Pearl: Babinski’s are either Present or Absent. There is no such thing as a positive or negative Babinski. http://zionmedicalstudent.blogspot.com/2010/07/how-to-check-babinski-sign-related-word.html Neuro Exam References Nerve Whiz App • http://icarus.med.utoronto.ca/NeuroExam/main.htm – Thorough, well done, video demonstration of the entire neuro exam 5 Case #1 History Neurological Exam • 45 y.o. male, drug rep, involved in a MVA and sustained cervical and rib fractures. He was noted to be unable to move his R UE. Case Studies Case #1: Exam Case #1 Potential Localization • Right Upper Extremity Weakness – L Motor Cortex – L Internal Capsule – Brainstem – Spinal Cord – R Brachial plexus / Peripheral Nerves – Mental Status: Oriented, in pain – Cranial Nerves: Pupils reactive, EOM intact, Face symmetric. – Motor: Complete inability to move the R UE, retained ability to move R LE and L side Sensory: Intact to touch and pinprick in all 4 extremeties – Cerebellar: FNF intact on the L – Gait: Normal toe, heel, tandem walking – DTR’s: 2+ & symmetric, except the R UE which is 3+. Babinski on R. Homunculus Case #1 Potential Localization • Right Lower Extremity Weakness – L Motor Cortex – L Internal Capsule – Brainstem-Very Brainstem Very hard to just affect entire arm and nothing else – Spinal Cord – Same thing – R Brachial plexus / Peripheral Nerves-Reflexes are present, and toe is upgoing Motor Sensory http://tmww.blogspot.com/2011/05/homunculus-of-touch.html 6 Case #2 History Case #1 Cortical Contusion Axial T2 FLAIR • 36 yo female, newscaster, noted by coworker to have mildly slurred speech and left facial weakness. Pt c/o left facial numbness, but had not noticed weakness. Coronal T1 Case #2 Exam Case #2 Potential Localization • • • • R Cortical Posterior limb R Internal Capsule Brainstem: L Pons L CN VII Case #2 Potential Localization • • • • – Mental Status: Oriented, Memory intact, naming and repetition normal, – Speech: Mild dysarthria – Cranial Nerves: EOMI, pupils equal, widened L palpebral l b l fissure, fi L facial f i l droop-upper d andd lower, l sensation intact, tongue midline, neck/shoulder 5/5. – Motor: 5/5 throughout, tone normal, PND absent – Sensory: Intact – Cerebellar: Intact DTR’s: 2+, toes downgoing – Gait: Normal Case #2 (Bells Palsy) R Cortical Forehead is not spared Posterior limb R Internal Capsule-Same Brainstem: L Pons-Maybe… L CN VII http://www.sciencephoto.com/media/251817/enlarge http://www.facebook.com/pages/Bells-Palsy-Support-Group/351858436387 http://meded.ucsd.edu/clinicalimg/neuro_central_cn7_palsy2.htm 7 Case #3 History • 28 yo male, works in landscaping, complains of chronic ‘numbness’ in his right hand. He is dropping tools now, and presented to his PCP The numbness sometimes wakes him PCP. up at night, but it does not bother him in the morning hours. Case #3 Exam Case #3 Potential Localization • • • • • L Cerebral cortex L posterior limb Internal Capsule Thalamus (Sensory component only) C8 root, T1 root, Brachial Plexus Peripheral Nerve-Ulnar vs Median vs Both Case #3 Exam – Mental Status: Normal – Cranial Nerves: Normal – Motor: Weak thumb opposition and abduction. Atrophy of the R thenar eminence. Hand g and wrist extension 5/5 intrinsics,, finger – Sensory: decreased pinprick in lateral/palmar aspect of R hand, Sensation above the wrist is normal. – Cerebellar: No dysmetria, RAM normal – Gait: Normal – DTR’s: +Tinels, otherwise 2+ http://cmapspublic.ihmc.us / http://drwolgin.com/carpaltunnel.aspx Case #3 Potential Localization • • • • L Cerebral cortex: Only 2 muscles involved L posterior limb Internal Capsule: Same Thalamus: Only explains sensory C8 root, T1 root, Brachial Plexus: Clinical Exam is too focal • Peripheral Nerve-Ulnar vs Median vs Both: Not Ulnar distribution Case #4 History • 48 yo female, homemaker, woke up with numbness “from the waist down,” and weakness of the L leg. Diagnosis Median Nerve compression at the wrist: Carpal Tunnel Syndrome 8 Case #4 Potential Localization • Right midline cortical lesion • Spinal Cord • Lumbar Polyradiculopathy Case #4 Potential Localization Case #4 Exam – Mental Status: Normal – Cranial Nerves: II-XII Intact – Motor: Diffuse L LE paresis – Sensory: Decreased Pinprick below the umbilicus on the R, decreased vibration below the umbilicus on the L – Cerebellar: Intact – Gait: Cannot stand without assistance – DTR’s: 3+ of the L LE, with a L Babinski, o/w 2+ throughout. Case #4 (T 10 lesion-myelopathy) • Right midline cortical lesion Sensory Level • Spinal Cord• Lumbar Polyradiculopathy- DTR’s are 3+ with i a Babinski i i Case #5 History • 63 yo accountant noticed sudden incoordination using his R hand on his calculator, followed within 30 seconds by intense vertigo, nausea and vomiting. He stood to run to the bathroom, but fell down and could not stand back up. Case #5 Potential Localization • Brainstem-Pons/Medulla • Cerebellum • Herniation syndrome 9 Case #5 Exam – Mental Status: Alert, too nauseated and vertiginous to cooperate with detailed testing – Cranial Nerves: Subtle nystagmus when looking to the right, face symmetric – Motor: Dyscoordination of the R UE – Sensory: Intact to pinprick and vibration, Romberg positive – Cerebellar: Dysmetria of the R UE, and R LE – Gait: Ataxic – DTR’s: Trace throughout. Toes downgoing Case #5 (Cerebellar Infarct) Case #5 Potential Localization • Brainstem-Pons/Medulla Dysmetria • Cerebellum • Herniation syndrome Case #6 History • 57 yo female, restaurant owner, slipped on the ice, falling on her back and hitting her head. She had sudden radiating pain down both legs, legs and inability to stand due to B leg weakness. She complains of a headache. Denies having loss of consciousness. Case #6 Exam Case #6 Potential Localization • Lower spine • Lumbar plexus • Midline hemispheric hemorrhage – Mental Status: A little slow in responses, but A&O x4, memory intact – Cranial Nerves: II-XII intact – Motor: L: 4+ Quads, 3+ Ant Tib. R: 3+ Gastroc. – Sensory: Decreased Pinprick in L lateral thigh & shin. Decreased Pinprick over the length of the posterior t i R leg l – Cerebellar: RAM/FNF intact – Gait: L Foot drop (can’t heel walk). Unable to Plantar flex the R foot (can’t toe walk). – Unsteady, radiating pain – DTR’s: Absent L patellar, Absent R Ankle, o/w 2+ throughout. Toes are downgoing 10 Case #6 Potential Localization Case #6 (Cauda Equina Syndrome) • Lower spine Asymmetric nerve distributions • Lumbar plexus- L4 (L) and S1 (R) nerves • Midline Hemispheric lesion Obviously Not • L4-L5 Disc Herniation http://www.netterimages.com/image/4808.htm Case #7 History • 75 yo male, retired Vet, with sudden onset of painless visual loss on the right side. Case #7 Potential Localization • • • • Case #7 Exam – Mental Status: A&O x 4, All Normal – Cranial Nerves: EOMI, Pupil is 4 mm on R and 3 mm on L. The direct pupillary response is absent on the R & intact on the L. The consensual pupillary response with the light shining in the R eye is absent, and with the light shining in the L eye is present. present Visual fields show monocular visual loss of the right eye. Vision field is intact on the left. Fundoscopic exam-no hemorrhage, mild papilledema on the right. Face is symmetric. All other cranial nerves are intact. – Motor, Sensory, Cerebellar, Gait, DTR’s: All intact and symmetric. Toes downgoing. L Occipital lobe L Optic radiations R Optic nerve R Retina/Eye Case #7 Potential Localization • • • • L Occipital lobe-Monocular Visual Loss L Optic radiations- Same R Optic nerveR Retina/Eye- Fundoscopic exam unremarkable except for papilledema 11 Case #7 Ischemic Optic Neuropathy Case #8 History • 67 yo female, retired truck driver, who had sudden onset of weakness of the entire Left side of the body, (face, arm and leg), causing h to her t fall. f ll Case #8 Potential Localization • • • • Right Cortex Right Internal Capsule Brainstem Cervical Cord Case #8 Potential Localization Case #8 Exam – Mental Status: Normal – Cranial Nerves: Left lower facial weakness, forehead spared, dysarthric, tongue midline, Facial sensation is intact and symmetric, EOMI, Pupils equal – Motor: Severe weakness of all muscle groups on the Left side. – Sensory: Intact pp/vib/temp throughout, symmetric – Cerebellar: Intact on the R, unable to test on L – Gait: L hemiparetic – DTR’s: 3+ on the L, 2+ on the R, Toe upgoing on L Case #8 Pure Motor Hemiparesis Lacunar Syndrome • Right Cortex: R MCA Stroke is usually Face &Arm > Leg. It would have to be a huge cortical infarct, or massive subarachnoid to affect the entire left body. body • Right Internal Capsule • Brainstem-R Ventral Pons/Basis Pontis • Cervical Cord? – (Arm and Leg, Yes…Face? No) 12 Case #9 History • 23 yo male with HIV presents one week after developing complaints of blurred vision, sometime seeing double. Case #9 Exam – Mental Status: Mild decrease in mentation according to S.O. – Cranial Nerves: Right eye will not abduct. Left eye will not deviate down and in. Left pupil is unreactive. There is nystagmus when looking to the right. right He is mildly dysarthric and has a mild L facial droop. – Motor: 5/5 throughout, Normal tone – Sensory: Intact pin prick/temperature/vibration Cerebellar: No dysmetria – Gait: Mildly ataxic – DTR’s: 2+, Babinski’s absent Case #9 Basilar Meningitis-Tb Case #9 Potential Localization • • • • Occipital cortex Brainstem CN III Globe Case #9 Potential Localization • Occipital cortex Visual Fields Intact • Brainstem – Cranial Nerves (R IV, R VI, R VIII, L III, L VII, IX ) • CN III Does not explain all findings • Globe No Case #10 History • 63 yo female, retired math professor, with sudden onset of inability to talk or move her right side Osborn, Diagnostic Imaging Brain 2004 13 Case #10 Potential Localization Case #10 Exam – Mental Status: Profound expressive aphasia, unable to follow commands – Cranial Nerves: Eyes deviated to the L, unable to cross the midline to the R with oculocephalic maneuvers, pupils reactive, R facial droop, absent gag. – Motor: No voluntary mvt of RUE, and no withdrawal to pinch. R lower extremity is externally rotated, and withdraws to pinch. – Sensory: As above. Withdraws briskly on the L – Cerebellar: L-reached for object w/o difficulty – Gait: Unable to test – DTR’s: 3+ on the right, R Babinski • Brain Case #10 Potential Localization Case #10 L MCA w/ hemorrhagic transformation • Brain-L Hemisphere Case #11 History • 46 y.o. male with onset of numbness and paresthesias in his distal lower extremities 2 weeks prior to admission. He also complained of his muscles feelingg “tired” in his legs g only. y • His symptoms have progressed to where he is now having trouble climbing stairs and complaints of paresthesias in his hands. Case #11 Potential Localization • Paresthesias – Peripheral nerves • Lower extremity weakness – Intrahemispheric mass lesion – Lumbar spinal cord – Conus Medularis (symmetric motor weakness) – Bilateral Lumbar Plexus / Peripheral nerves 14 Case #11 Exam – Mental Status: A & O x4 – Cranial Nerves: EOMI, face symmetric, speech normal, All intact – Motor: 4+/5 bilateral distal LE symmetric weakness – Sensory: Prominent stocking-glove gradient sensory loss to all modalities on all 4 extremities – Cerebellar: Intact – DTR’s: Absent throughout. Babinski’s absent – Gait: No ataxia or asymmetries, but appears labored Case #11 Guillain-Barre Syndrome Case #11 Potential Localization • Paresthesias – Peripheral nerves • Lower extremity weakness – Intrahemispheric I h i h i mass lesion l i Absent Ab DTR’ DTR’s – Lumbar spinal cord, Conus Medularis (symmetric motor weakness) Absent DTR’s – Bilateral Lumbar Plexus / Peripheral nerves Case #12 History Acute inflammatory demyelinating polyneuropathy (AIDP) • Exam and History are Classic • CSF revealed elevated protein of 53 without increased WBC’s (“albuminocytologic dissociation”) • Rx with IVIG • 21 yo Burmese refugee who immigrated to the US. By report, he has had seizures since the age of 16. Through an interpreter, the seizures start with tingling in his L hand. hand The symptoms can spread from there and result in a convulsion. http://www.childrenshospital.org/az/Site974/mainpageS974P0.html Case #12 Potential Localization • R Cortical Sensory Strip Case #12 Exam – Mental Status: Alert, follows commands. Memory 3/3 recall. Naming was unable to be tested. – Cranial Nerves: II- XII Intact – Motor: Strength is 5/5 throughout. Tone normal. – Sensory: Appears symmetric to touch. Difficult to test in detail due to language barrier. – Cerebellar: No dysmetria. – Gait: Nl toe, heel, tandem walking. – DTR’s: 2+ and symmetric with downgoing toes. 15 Case #12 Potential Localization Case #12 Neurocysticercosis • R Cortical Sensory Strip – Based on history only Case #13 History • 62 yo female, nurses aide, with a history of Epilepsy, who has noticed progressive difficultyy with balance and tingling/numbness in her hands and feet. Case #13 Exam – Mental Status: Alert and oriented. Memory Intact. Follows commands. – Cranial Nerves: Gaze evoked nystagmus, Saccadic dysmetria, Scanning Speech and mild dysarthria – Motor: Strength is 5/5 throughout. Tone is normal. Mild rubral tremor when testingg Pronator Drift. – Sensory: : Decreased vibration and PP in a stocking/glove fashion on all 4 extremities, LE>UE – Cerebellar: Dysmetria with Finger-to-nose and Heelknee-shin maneuvers – Gait: Ataxic – DTR’s: Absent throughout with downgoing toes Case #13 Potential Localization • Brain/cerebellum • Spinal cord (posterior columns) • Peripheral nerves Case #13 Potential Localization • Brain/cerebellum Distal/Proximal Gradient Sensory Loss • Spinal cord (posterior columns) Eye findings, speech tremor speech, tremor, Absent DTR’s DTR s & Absent Babinski’s • Peripheral nerve Eye findings, speech, tremor Findings cannot be explained with 1 focus/lesion 16 Case #13 Chronic Dilantin Therapy Cerebellar Atrophy and Peripheral Neuropathy 17