HYDROMORPHONE
advertisement

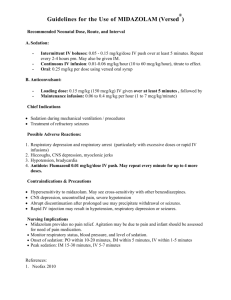
HYDROMORPHONE VIHA (South Island) EPIDURAL MONOGRAPH OTHER NAMES HYDROCHLORIDE *ELDER ALERT CLASSIFICATION Dilaudid Opiate agonist – Narcotic analgesic See Cautions INDICATIONS FOR EPIDURAL USE NON HEALTH CANADA APPROVED INDICATION BUT SUBSTANTIATED IN THE LITERATURE: • Management of pain following surgery or trauma.1,2 CONTRAINDICATIONS Hypersensitivity to hydromorphone.3 Cross hypersensitivity may occur with codeine, morphine, oxycodone or oxymorphone. CAUTIONS ∗ • Elderly: may be at increased risk of respiratory depression after the first dose.2 Very young1, debilitated or other poor risk patients (e.g. Addison’s disease), respiratory disease and patients with decreased respiratory reserve (e.g. obesity, kyphoscoliosis): increased risk of delayed respiratory depression.3 • Thoracic epidural administration: the risk of both early and delayed respiratory depression is increased.3 • Severe renal or hepatic impairment or patients with reduced metabolic rates: dose reduction may be required, due to decreased elimination.3 • Increased intracranial pressure, or head injury: respiratory depression or obscuring of clinical course may occur.3 DRUG INTERACTIONS: CNS depressants – additive effects increase the risk of respiratory depression.1,2 PREGNANCY/BREAST FEEDING: Contact pharmacy for most recent information. ADMINISTRATION MODE DIRECT WITHOUT CATHETER DIRECT VIA CATHETER YES YES Anaesthetist only Registered nurses with specialized skills – training in epidural administration WHO MAY GIVE Dilute 1 mL hydromorphone (2 mg/mL) to 10 mL with NS for 0.2 mg/mL. Discard excess hydromorphone from syringe & give prescribed dose slowly. ADULT/ PAEDIATRIC NEONATE REQUIREMENTS CONTINUOUS EPIDURAL INFUSION YES Registered nurses with specialized skills – training in epidural administration 10 mcg/mL – using 2 mg/mL solution add 1.25 mL to 250 mL NS. 20 mcg/mL – using 2 mg/mL solution add 2.5 mL to 250 mL NS. Limited information Limited information 0.22 micron epidural specific in-line filter Infusion device for continuous infusion. Apnoea monitors if less than 6 months old or paediatric with lung disease. IV line must be established prior to epidural therapy and be maintained for 18 hours following last epidural dose or end of infusion. MONITORING REQUIRED ADULTS – Non-Obstetrics Direct via Catheter: • Baseline RR and sedation scale, then q 1 h x 18 hours. Continuous Infusion: monitor during infusion and for 18 hours after the epidural infusion is stopped • Baseline RR, then q 1 h x 24 hours, then q 4 hours. • Baseline sedation scale, then q 1 h x 18 hours, then q 4 hours. ADULTS – Obstetrics • Monitoring as per prepared maternity epidural analgesia order. PAEDIATRICS • Monitoring as per prepared paediatric epidural analgesia order. RECOMMENDED • Fluid balance. Assess for bladder distension. RECONSTITUTION • None required. Available in a variety of concentrations and volumes. For preparation of standard solutions use hydromorphone 2 mg/mL – 1 mL ampoule. References available on the VIHA (South Island) Pharmacy Web site (http://intranet.viha.ca/clinical_support/pharmacy/si/) Rev Feb 2004 VIHA (South Island) EPIDURAL MONOGRAPH HYDROMORPHONE HYDROCHLORIDE COMPATIBILITY/STABILITY • • • • Dilute only with NS WITHOUT PRESERVATIVE. Compatible and stable in NS, with or without bupivacaine for at least 72 hours at room temperature and in the refrigerator. Pharmacy recommends all aseptically admixed products be stored in the refrigerator. 4 Compatible in a syringe with fentanyl for at least 15 minutes at room temperature.5 For additional drug-drug compatibility contact Drug Information. ADVERSE EFFECTS1, 2 RESPIRATORY • Respiratory depression: decreasing quality/depth of respirations may be the initial indication of respiratory depression. Will not occur without sedation, as higher doses are required to produce respiratory depression than to produce sedation. Treatment: naloxone IV and respiratory support. CNS • Sedation; most patients experience sedation at the beginning of therapy and whenever the dose is increased significantly. DERMATOLOGICAL • Pruritus (common); usually localised to the face, neck or upper thorax. More common in obstetric patients. Very rarely accompanied by a rash. Responds to a decrease in dose. If treatment is required: diphenhydramine or naloxone IV. • True allergy (very rare). It is important to determine the exact nature of the reaction in patients reporting an allergy, as many believe they are allergic after experiencing an exaggerated pharmacological response such as nausea, drowsiness or constipation.3 MISCELLANEOUS • Nausea, vomiting. Most common with the initial dose. Dose related. Slow and steady dose titration helps reduce nausea. • Urinary retention: may require catherization. DOSE • The following doses should only be considered as guidelines. Safe and effective doses for individual patients will vary considerably, depending on age, medical condition, site of catheter placement, type of pain, and other factors. • Using a combination of bupivacaine and hydromorphone will decrease the required dose of hydromorphone. • Onset of action 15-30 minutes, peak 45-60 minutes, duration up to 18 hours; based on a single bolus administration.2 • Duration of analgesia is dose dependent; the higher the dose the longer the duration. When steady state is reached by continuous infusion, hydromorphone, morphine and fentanyl differ little in terms of duration of analgesia.2 ADULT2 • Bolus dose: usual dose range; 0.8 – 1.5 mg. Frequency determined by patient’s clinical condition and response. • Continuous infusion: usual starting dose; 0.15 – 0.3 mg/hour. Dependent upon previous narcotic use. ELDERLY2 • Some recommend lowering the starting dose and increasing the interval between doses. Consider age-related renal impairment. PAEDIATRIC • Bolus dose: limited experience in paediatrics. Studies in adults would suggest a 3:1 to 5:1 epidural potency ratio to morphine.1 • Continuous infusion: 1 – 3 mcg/kg/hr.1 NEONATE • Limited information available at this time. RENAL IMPAIRMENT ADJUSTMENTS • Dosage reduction may be required; no guidelines currently available.3 HEPATIC IMPAIRMENT ADJUSTMENTS • Dosage reduction may be required; no guidelines currently available.3 HEMO/PERITONEAL DIALYSIS • No information available at this time. MISCELLANEOUS • When switching opioid-naïve patients from epidural to IV hydromorphone a conversion ratio of 1:5 has been used.2 References available on the VIHA (South Island) Pharmacy Web site (http://intranet.viha.ca/clinical_support/pharmacy/si/) Rev Feb 2004 HYDROMOPHONE EPIDURAL - REFERENCES 1. Polaner DM, Berde CB. Postoperative pain management. In: Cote CJ, Ryan JF, Todres ID, et al, eds. A practice of anaesthesia for infants and children. Philadelphia: Saunders; 1993:451-69. 2. Pasero C, Portenoy RK, McCaffery M. Opioid analgesics. In: Pain: Clinical manual. 2nd ed. McCaffery M, Pasero C, eds. St. Louis: Mosby; 1999:161-299. 3. Repchinsky C, ed. Compendium of Pharmaceuticals and Specialties. 38th ed. Ottawa, ON: Canadian Pharmaceutical Association; 2003:1197-9. 4. Lui W, Hyang Park M. Shelf-life of Baxter’s Pain Management admixtures. Baxter Corporation. Mississauga, ON. May 2002. (Letter) 5. Trissel LA, ed. Handbook of injectable drugs. 11th ed. Bethesda, MD: American Society of Hospital Pharmacists; 2001: 718. References available on the VIHA (South Island) Pharmacy Web site (http://intranet.viha.ca/clinical_support/pharmacy/si/) Rev Feb 2004