Predictive Modeling for ACOs
December 2013
©2013 Walgreen Co. All rights reserved.
Agenda
•Introductions
•Walgreens Mission and Vision
•Walgreens ACO predictive models
•Predictive models for End-of-Life
©2013 Walgreen Co. All rights reserved.
2
Introductions
Ian Duncan FSA FIA FCIA MAAA. Vice President, Clinical Outcomes & Analytics and Head of Research, Walgreen Co. Chicago. Adjunct Professor at UC Santa Barbara and Adjunct Research Professor, Georgetown Dept. of Health Administration. Board member, Massachusetts Health Insurance Connector Authority (Exchange).
Author of several books and peer‐reviewed studies in healthcare management and predictive modeling. 2011 publication has chapter on Massachusetts Reform. Published 2008
New Edition December 2013
May 2011
Walgreens mission and vision
MISSION
To be the most trusted, convenient,
multi channel provider/advisor of
innovative pharmacy, health and
wellness solutions, and consumer
goods and services in communities
across America.
A destination where health and
happiness come together to help
people get well, stay well, and
live well.
VISION
To be “My Walgreens” for everyone
in America, the first choice for health
and daily living
©2013 Walgreen Co. All rights reserved. Confidential and proprietary; should not
be reproduced or redistributed.
4
Walgreens has a multichannel, national footprint with a
local presence
Nearly ⅔ of the US population live within 3 miles of a Walgreens
Specialty
Home Infusion/RT
Mail
Healthcare Clinics
Take Care Worksites
Health Systems
Pharmacy
Retail
Walgreens points of care as of August 31, 2011. Source: Walgreens 2011 Annual Report.
©2013 Walgreen Co. All rights reserved.
5
Transforming community pharmacy into an integrated
healthcare delivery system
• A premier provider of healthcare
and wellness services
• 75,000 affiliated healthcare
providers deliver high-quality
healthcare services
̶ Retail and specialty pharmacists
̶ RNs, LPNs, NPs, PAs
̶ Dietitians
̶ Health and wellness coaches
̶ Health and fitness trainers
̶ Case managers and referral assistance
©2013 Walgreen Co. All rights reserved.
6
Healthcare Retail Clinic Locations
• Open 7 days a week with 360+ locations in 31 markets, 19 states
• Online appointment scheduling available
WA
MT
ND
ME
MN
OR
VT
WI
ID
NY
0
7
SD
MI
WY
IA
NE
NV
0
13
CO
UT
0
13
CA
KS
0
15
IL
MO
10,909
53
IN
0
18
0
27
OK
NM
11,171
14
Covered lives data supplied by Health Leaders as
of January 2012.
Data include fully insured lives plus self insured lives.
©2013 Walgreen Co. All rights reserved. Confidential and proprietary; should not
be reproduced or redistributed.
0
18
OH
4,003
18
WV
VA
0
10
1,898
4
CT
4,408
DE
0
2
NC
SC
AR
LA
RI
NJ
MD
0 33
MS
TX
NH
MA
PA
KY
2,670
35
TN
AZ
25,347
0
2
AL
GA
13,597
24
= # of Covered Medicare Lives*
= # of Healthcare Retail Clinics
4,877
5
FL
63,542
48
7
Moving into the future: Walgreens Well Experience
250+ Well Experience stores brings primary healthcare services front and center.
©2013 Walgreen Co. All rights reserved.
8
Accountable Care Services:
Targeted, Coordinated and Connected
©2013 Walgreen Co. All rights reserved. Confidential and proprietary; should not be
re-produced or re-distributed.
9
Walgreens ACO Predictive Models
December 2013
©2013 Walgreen Co. All rights reserved.
The Challenge for ACOs
Mr Micawber's famous, and oft-quoted,
recipe for happiness:
"Annual income twenty pounds, annual
expenditure nineteen pounds nineteen
shillings and sixpence, result
happiness. Annual income twenty
pounds, annual expenditure twenty
pounds ought and six, result misery."
Charles Dickens, David Copperfield
©2013 Walgreen Co. All rights reserved.
11
Providers are not good at predicting re-admission risk
Assessed the predictions made by
̶ Physicians
̶ Case managers
̶ Nurses
“...none of the AUC values were
statistically different from chance”
Allaudeen N, Schnipper JL, Orav EJ, Wachter RM, Vidyarthi AR. Inability of providers
to predict unplanned readmissions. J Gen Intern Med. 2011;26(7):771-6
Current Predictive Models aren’t much better
“Most current readmission risk
prediction models perform
poorly…Efforts to improve their
performance are needed.”
Implications
A single, nationwide model
is unfeasible
Additional data points
may improve predictive accuracy –
possibly including pharmacy data
Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M,
Kripalani S. Risk prediction models for hospital readmission: a systematic review.
JAMA. 2011 Oct 19;306(15):1688-98.
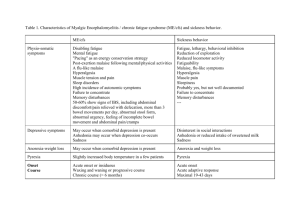
Overall membership distribution by condition
Membership Distribution
Members were
classified into 8
hierarchical categories:
• Nearly 25% of
members do not
have an identified
acute, chronic or
mental health
condition.
• 35.3% of the <65
segment do not
have an identified
condition
14
Condition
<65
65+
Overall
1) Acute MH Chronic
11.0%
11.9%
11.7%
2) Acute MH
5.8%
3.6%
4.1%
3) Acute Chronic
7.3%
17.6%
15.2%
4) Acute Only
6.5%
9.1%
8.5%
5) MH Chronic
7.8%
4.3%
5.1%
6) MH Only
10.3%
3.9%
5.4%
7) Chronic Only
8.8%
15.7%
14.1%
8) EHC
7.2%
13.8%
12.2%
No Condition
35.3%
19.9%
23.6%
Overall cost distribution by condition
Cost Distribution
When focusing on
costs…
• More than $4 of
every $10 dollars is
spent on most
complex members.
• Acute members with
chronic and mental
health comorbidities
account for nearly
76% of all spend –
care management is
critical for these
members
15
Condition
<65
65+
Overall
1) Acute MH Chronic
46.8%
41.3%
42.3%
2) Acute MH
10.8%
5.9%
6.8%
3) Acute Chronic
16.2%
29.2%
26.8%
4) Acute Only
6.2%
7.1%
6.9%
5) MH Chronic
8.0%
3.7%
4.4%
6) MH Only
5.5%
1.8%
2.4%
7) Chronic Only
3.9%
6.7%
6.2%
8) EHC
1.9%
3.6%
3.3%
No Condition
0.7%
0.8%
0.8%
Distribution for Aged and Disabled Population
Comparison between <65 members and >65 population.
Under 65 Population
100.0%
Over 65 Population
100.0%
11.0%
11.9%
90.0%
< 65
5.8%
80.0%
7.3%
70.0%
46.8%
7.8%
2) Acute MH
60.0%
3) Acute Chronic
10.3%
40.0%
10.8%
5) MH Chronic
6) MH Only
16.2%
30.0%
60.0%
No Condition
50.0%
4.3%
3.9%
40.0%
15.7%
35.3%
0.0%
% of Membership
16
5.5%
3.9%
0.7%
1.9%
Costs %
3) Acute Chronic
5.9%
4) Acute Only
5) MH Chronic
6) MH Only
29.2%
7) Chronic Only
8) EHC
30.0%
13.8%
No Condition
20.0%
7.1%
10.0%
19.9%
3.7%
1.8%
6.7%
0.8%
3.6%
% of Membership
Costs %
8.0%
10.0%
2) Acute MH
9.1%
7) Chronic Only
8) EHC
6.2%
1) Acute MH Chronic
70.0%
4) Acute Only
7.2%
20.0%
65 +
41.3%
17.6%
1) Acute MH Chronic
8.8%
3.6%
80.0%
6.5%
50.0%
90.0%
0.0%
Overview - How do the aims of the ACO drive strategy?
4x Aims of the ACO
©2013 Walgreen Co. All rights reserved.
ACO Strategies
17
Overview – Clinical Programs
High cost and/or
highly intervenable
patients
(a) Prevent over-medicalized End-Of-Life
(EOL) care.
(b) Prevent unplanned Transitions in care.
(c) Prevent Ambulatory-Care-Sensitive
(ACS) hospitalizations.*
(d) Improve decision-making for PreferenceSensitive Treatments (PST).
(e) Prevent over-medicalization of Chronic
Kidney Disease (CKD).
(f) Prevent Somatization - over-investigation
of medically unexplained symptoms.
*especially for patients with a combination of
acute + chronic + mental health issues.
18
Overview - The Role of Analytics
Analytics supports the goals of the ACO through the
following processes:
1.Conducting opportunity analysis to identify (and then quantify)
potential clinical programs;
2.Aggregating and warehousing data from multiple sources;
3.Predictive modeling/risk stratifying at the patient level for
implementation of clinical programs;
4.Identifying gaps in care at the patient level;
5.Developing baseline quality measures for outcomes reporting (33
quality measures);
6.Providing ongoing reporting for program management and outcomes.
©2013 Walgreen Co. All rights reserved.
19
Overview – The Value of Predictive Modeling
•Assists providers by stratifying patients and focusing resources;
it is not a substitute for clinical judgment.
•Harnesses the power of healthcare data, including CMS data that
providers do not have.
•Focuses ACO clinical programs on the portion of the patient
population with the greatest potential for improved outcomes
(Triple Aim).
•Focuses resources where they will have the greatest impact.
•Increases efficiency and impact of clinical programs.
©2013 Walgreen Co. All rights reserved.
20
Overview – Predictive Modeling Defined
Predictive models stratify the patient population according
to their likelihood of experiencing the target event. The
process includes:
1.Using a similar dataset, identify all potentially correlated independent
variables that predict the dependent (outcome) variable.
2.Derive scores for each patient (i.e. likelihood of experiencing the
event) under numerous combinations of variables.
3.Compare the actual outcomes to the scores, to determine the scenario
with the best positive predictive value. (PPV)
4.Operationalize the method for application to actual ACO data.
Develop a program to manage the targeted members.
©2013 Walgreen Co. All rights reserved.
21
Preventing over-medicalized
End-Of-Life care
22
End-of-Life
There is not a significant difference between the experience of members
with a hospice stay and those without (65+).
END OF LIFE - HOSPICE
END OF LIFE - NON-HOSPICE
< 65
65 +
Total
< 65
65 +
Total
Average Lives
1,035
15,091
16,126
2,752
18,139
20,892
% of Overall
0.1%
0.5%
0.4%
0.3%
0.6%
0.6%
Total Allowed
$ 7,322
$ 5,826
$ 5,922
$ 5,072
$ 5,550
$ 5,487
% of Overall
1.5%
3.9%
3.4%
2.8%
4.4%
4.1%
•Note: these lives represent 6 months of deaths; to derive the annual total double the
prevalence.
•These numbers represent 6 months of claims. To derive the last 12 months of claims, multiply
by 3.0.
©2012 Walgreen Co. All rights reserved.
23
End-of-Life
The most complex members are a significant portion of the end-of-life
population, and total cost.
Members
Costs
< 65
65 +
< 65
65 +
ALL
39.5%
46.9%
62.2%
60.1%
HOSPICE
43.8%
50.4%
56.2%
59.8%
NON‐HOSPICE
56.2%
58.9%
65.5%
61.2%
Overall, close to 60% of end-of-life costs are generated by the most complex
patients; because end-of-life accounts for 23% of all costs, the complex
patients generate about 14% of all costs.
©2012 Walgreen Co. All rights reserved.
24
End-of-Life (all)
The most complex members: Comparative Utilization.
Complex end of life patients
have a high frequency of
hospital admissions (2500
per 1000). Most of these
are for medical DRGs. Also
very high specialist visit
frequency.
Under 65 patients are an
even high-utilizing group.
< 65
3,788 OVERALL
65 +
33,230 Total
37,017 IP Admits ‐ Overall
Average IP Length of Stay ‐ Overall
IP 30 Days Re‐Admits ‐ Overall
Readmit % ‐ Overall
2,548 7.8 800 31.4%
1,929 7.2 421 21.8%
1,977 7.7 426 21.5%
3,136 8.5 998 31.8%
2,499 7.6 566 22.6%
2,555 7.7 604 23.6%
IP Admits ‐ Medical
Average IP Length of Stay ‐ Medical
IP 30 Days Re‐Admits ‐ Medical
Readmit % ‐ Medical
IP Admits ‐ Surgical
2,243 7.1 744 33.2%
305 1,682 6.7 379 22.5%
247 1,680 6.9 378 22.5%
297 2,691 7.5 901 33.5%
445 2,154 6.9 503 23.3%
345 2,201 7.0 538 24.4%
354 Average IP Length of Stay ‐ Surgical
13.1 10.6 12.1 14.5 12.1 12.4 LTC Admits 56 18.4%
‐
43 17.2%
0.1 48 16.1%
0.3 97 21.7%
‐
63 18.2%
0.4 66 18.6%
0.4 ER Visits OP Services 311 17,112 72 15,883 123 12,816 356 15,444 138 15,546 157 15,537 PCP Visits
2,448 2,605 2,744 3,457 2,927 2,973 Specialist Visits 6,818 4,989 4,850 6,539 4,718 4,878 CT Services MRI Services 3,750 844 2,726 482 2,626 433 4,003 718 3,261 489 3,326 509 10,352 7,916 9,365 15,796 12,251 12,563 Average Lives
IP 30 Days Re‐Admits ‐ Surgical
Readmit % ‐ Surgical
X‐Ray Services ©2012 Walgreen Co. All rights reserved.
1) Acute MH Chronic
< 65
65 +
Total
1,509 15,627 17,137 25
Preventing over-medicalized End-Of-Life care
Clinical Program:
•Education for physicians and
their staff on how to instigate
end-of-life conversations.3
•Program to encourage patients
to complete advance directives,
consisting of materials, a
helpline, and a registry.4
•Patient access to hospice and
palliative care.
•Symptom-focused case
management for very high-risk
patients.3
↑
Population
health
Reduction in
inappropriate
life-sustaining
treatments
within 6
months of
death,
including a
reduction in
ER visits.2
↓
Administrative
burden
Dedicated
case managers
to support
physicians in
caring for
complex
patients that
are at very
high risk of
overmedicalized
end-of-life care
as defined by
Barnato et al.2
↓
Per capita cost
↑
Patient
experience
Homehospice care
associated
with
significantly
lower average
costs ($12,434
versus $4,761
per year in
2007 dollars).5
Patients
receiving inhome
palliative care
report
significantly
higher
satisfaction
and quality of
life.6
Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Archives of Internal Medicine. 2009;169(5):480
Barnato AE, Farrell MH, Chang CC, Lave JR, Roberts MS, Angus DC. Development and validation of hospital "end-of-life" treatment intensity measures. Medical Care. 2009;47(10):1098-1105
3 Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment.
JAMA 2008; 300(14):1665-73
4 Nicholas L, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA 2011; 306(13):1447-53
5Shnoor Y, Szlaifer M, Aoberman AS, Bentur N. The cost of home hospice care for terminal patients in Israel. Am J Hosp Palliat Care. 2007 Aug-Sep;24(4):284-90
6 Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, McIlwane J, Hillary K, Gonzalez J. Increased satisfaction with care and lower costs: results of a randomized trial of in-home
palliative care. J Am Geriatr Soc. 2007 Jul;55(7):993-1000.
1
2
End of Life Predictive Model - Definition
Over-medicalized death is defined as:
¾ Chemotherapy for cancer patients within 14 days of
death;
¾ Unplanned hospitalization within 30 days of death;
¾ More than one emergency department (ED) visit
within 30 days of death
¾ ICU admission within 30 days of death; or
¾ Life-sustaining treatment within 30 days of death.
·
Ho, T. H., Barbera, L., Saskin, R., Lu, H., Neville, B. A., & Earle, C. C. (2011). Trends in the aggressiveness of
end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol, 29(12), 1587-1591.
doi:10.1200/JCO.2010.31.9897. Retrieved
from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3082976/pdf/zlj1587.pdf
· Earle, C. C., Park, E. R., Lai, B., Weeks, J. C., Ayanian, J. Z., & Block, S. (2003). Identifying potential indicators of
the quality of end-of-life cancer care from administrative data. Journal of Clinical Oncology, 21(6), 1133-1138. doi:
10.1200/jco.2003.03.059 Retrieved from http://jco.ascopubs.org/content/21/6/1133.long
27
End of Life Predictive Model - Scoring
•
An EOL risk score is calculated for each member.
•
Risk scores range in value from 0.0-1.0.
•
Model is based on the following member attributes (121 in all):
•
Age and gender;
•
Race;
•
Region
•
Clinical Grouper Flags (65 HCCs);
•
Baseline admission count(s)
•
Baseline readmission count(s)
•
Baseline ER visit count(s)
•
Baseline admission via ER indicator
•
Baseline dollars spent for healthcare resources
28
End of Life Predictive Model – Conditions
and Attributes that Add Most to Scores
1. Acute Myocardial Infarction
2. Acute Leukemia
3. Craniotomy with major device implant
4. Cardio-Respiratory Failure & Shock
5. Metastatic Cancer & Acute Leukemia
6. Lung, Upper Digestive Tract and Other Severe Cancers
7. Septicemia or Severe Sepsis
8. Number of Admissions
29
End of Life Predictive Model – Opportunity
as seen from Medicare 5% Database
Medicare Patients and Deaths (based on 50% of the 5% file)
Categories
Members
% of Total
Population
PMPM
Survivors
819,189
92.0%
$684.80
Deceased
71,059
8.0%
$4,323.73
Appropriate
22,989
2.6%
$2,249.62
Inappropriate
9,832
1.1%
$3,433.30
OverMedicalized
38,238
4.3%
$5,797.08
890,248
100.0%
$975.26
Total
The difference between over-medicalized and appropriate death
represents a financial and clinical opportunity. (Inappropriate death
also represents an opportunity, although a smaller one).
30
End of Life Predictive Model – Member
costs by category and risk score
The PMPMs for members in each category vary across the bands of
risk scores. The difference in the costs between those that experience
overmedicalized deaths versus those that experience appropriate
deaths is greatest in members with risk scores >.95.
31
End of Life Predictive Model – Performance
of Model on Medicare 5% Database
Out of a 10,000 attributed life group, we would expect 430
overmedicalized deaths (4.3%). Based on our model, approximately
46% of these members will have risk scores >.95.
32
End of Life Predictive Model – Performance
of Model on Medicare 5% Database
Distribution of members by risk score (10,000 life group)
Members
Risk Scores
Out of a 10,000 attributed life group, we would expect 341 members to
have risk scores >.95. Of these members, we expect 197 (57.9%) to
be “true positives”; that is, these are the members that represent an
opportunity to avoid an overmedicalized death.
33
End of Life Predictive Model - Targeting
Total OM
Deaths
(430 of
10,000)
Remaining
OM Deaths
(232)
True Positives
(197)
False Positives
(143)
Members
with
Risk Scores >.95
(341 of 10,000)
Focusing on members with risk scores >.95 allows us to target our
resources on only 3.4% of the population in order to “find”
nearly half of the members that represent our opportunity.
34
End of Life Predictive Model - Targeting
Intervention Costs Incurred on
All Targeted, Engaged Members
Total OM
Deaths
(430 of
10,000)
Remaining
OM Deaths
(232)
True Positives
(197)
False Positives
(143)
Members
with
Risk Scores >.95
(341 of 10,000)
Opportunity
for Savings
Thru Effective Interventions
The risk score “cut off” point is determined by evaluating the number of total
members above a given risk score with the number of “true positives” found
in that group. We will incur intervention costs on all members with risk scores
above the cut-off, but only have the opportunity to generate savings on the
“true positives” within that group.
35
End of Life Predictive Model - Financial
Scenario at 95% Risk Score Threshold
Based on Members with Risk Scores >.95
# of Members (out of 10,000)
% of Members (out of 10,000)
Over Medicalized Sensitivity
PPV (OM Deaths)
# of True Positives (out of 10,000)
# of False Positives (out of 10,000)
Estimated Gross Savings
# of True Positives (a)
Engagement Rate (b)
Effectiveness Rate (c )
Potential Savings per True Positive (d), (1)
Estimated Gross Savings (a x b x c x d)
Estimated Net Savings
# of Members with p>.95 (e )
Engagement Rate (b)
Cost of Case Management (f)
Total Cost (e x b x f)
Net Savings/(Costs)
341
3%
46.0%
57.9%
197
143
197
40%
50%
$ 15,981
$ 630,853
341
0%
$ 940.67
$ 128,234
$ 502,619
(1) Difference in costs between OM death and appropriate
death, over 6.5 months (PMPM*6.5).
36
Operationalizing the End of Life Predictive
Model
Process:
¾ Analytics team will apply EOL Predictive Model to the warehoused data
after each month’s additions to the data.
¾ Analytics team will produce list of members at high risk for an overmedicalized death within the next 6-12 months. (monthly report)
¾ Clinical team and providers will target the identified members for
application of the components of the EOL Clinical Program, for
example:
9Advanced Directives
9Access to Hospice and Palliative Care
9Complex-case Management
37
Contact Information
Clinical Outcomes & Reporting
Ian Duncan FSA FIA FCIA MAAA
Vice President
Ian.duncan@walgreens.com
(847) 964-6418
1415 Lake Cook Rd. / 4S / MS #L444
Deerfield, IL 60015
©2013 Walgreen Co. All rights reserved.
38
The power of a national footprint with the
reassurance of a personalized, local presence.