Early Ambulation After Acute Deep Vein Thrombosis

Early Ambulation After Acute Deep Vein
Thrombosis: Is It Safe?
Marilyn Slavin Blumenstein, MSN, RN
The number of thrombotic events in children, although significantly less than that in adults, is increasing as a result of therapeutic advances in primary illnesses that were previously fatal. When a patient, adult or pediatric, develops a deep vein thrombosis and anticoagulation therapy is initiated, many health professionals ask, “When should this patient have physical therapy and/or ambulate?”
Fear of causing a pulmonary embolism with increased activity drives this question. Often, an order for bed rest is prescribed based more on tradition than on evidence-based medicine. A review of the literature has provided an evidence-based answer to the question, and although the studies are all of adult populations, the results have been extrapolated for use with comparable pediatric populations. The majority of studies agree that early ambulation does not increase an anticoagulated patient’s risk for pulmonary embolism. Moreover, most studies report that early ambulation carries benefits such as decreased pain and swelling and fewer postthrombotic syndrome symptoms.
Key words: deep vein thrombosis, ambulation, physical therapy, pulmonary embolism, children
R ecently, a pediatric physical therapy manager asked me for practice recommendations for her staff when they are working with children with deep
© 2007 by Association of Pediatric Hematology/Oncology Nurses
DOI: 10.1177/1043454207308896 vein thrombosis (DVT). Her staff had 4 questions:
(1) Is it correct to hold ambulation/out-of-bed orders if there is a suspected DVT or if an ultrasound result is pending? (2) Once a DVT is diagnosed and the patient is placed on anticoagulant therapy using enoxaparin (Lovenox®), how long until the patient is out of bed and/or ambulating? (3) With DVTs, are bed exercises on the unaffected limbs allowed? (4)
Who is the point person for questions related to ambulation and physical therapy for patients with
DVTs? Questions like these are also asked by other health care providers who are responsible for the dayto-day supervision and coordination of patient activities. One-size-fits-all answers to these questions are unhelpful and potentially dangerous. The attending physician responsible for the patient, sometimes in collaboration with a hematologist, is in the best position to direct the patient’s care. Our pediatric physical therapy manager was advised to continue to collaborate with the patient’s attending physician. In addition, I conducted a literature search and evaluated the evidence-based clinical research concerning ambulation in the setting of acute DVT. Those results were used to inform our practice and are offered here so that other pediatric nursing and physical therapy groups can inform their practices too.
Marilyn Slavin Blumenstein, MSN, RN, is a thrombosis program nurse coordinator at the Children’s Hospital of Philadelphia. Address for correspondence: Marilyn Slavin Blumenstein, MSN, RN, 34th and Civic
Center Boulevard, Hematology, Philadelphia, PA 19101; e-mail:
Blumenstein@email.chop.edu.
309 Journal of Pediatric Oncology Nursing, Vol 24, No 6 (November-December), 2007; pp 309-313
Blumenstein
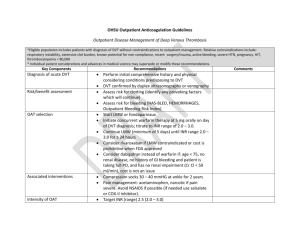
Table 1.
List of Treatment Options for DVT
Observation with serial imaging and without anticoagulation
Thrombolysis with or without balloon angioplasty or Angiojet
Inferior vena cava filter placement (temporary or permanent) with or without anticoagulation
Anticoagulation
Unfractionated heparin
Low molecular weight heparin (eg, enoxaparin/Lovenox ® )
Vitamin K antagonist (eg, warfarin/Coumadin
®
)
Direct thrombin inhibitors (eg, hirudin, argatroban)
Gradient compression therapy
Table 2.
Inherited/Congenital Risks for Thrombosis Organized Using Virchow’s Triad
Alterations in Flow Vascular Endothelial Injury
May-Thurner syndrome
Thoracic outlet syndrome
Hyperhomocysteinemia (?)
Hypercoagulability
Factor V Leiden mutation
Prothrombin gene mutation
Antithrombin deficiency
Protein C deficiency
Protein S deficiency
Elevated lipoprotein (a)
Hyperhomocysteinemia
Dysfibrinogenemia
Case 1
Joann is a 16-year-old female who has a body mass index in the 90th percentile, is using estrogencontaining oral contraception pills, and has just returned to the United States from a school-sponsored trip to
Australia. She presented to the emergency department with a red, hot, swollen, and painful left leg. Doppler ultrasound demonstrated an occlusive DVT in her left superficial femoral and external iliac veins; the inferior vena cava was open. Oral contraception pills were stopped and anticoagulation with enoxaparin was initiated. Joann wants to get out of bed and walk around. Is it safe?
Case 2
Dillan, an 11-month-old infant born at 30 weeks gestation, was noted to have significant swelling in his right leg at his wellness check by his primary care provider. Imaging studies revealed an occlusive thrombosis of his infrarenal inferior vena cava and right iliac vein. His parents reported noticing a slight difference in leg size recently and attributed it to his new skill of standing and cruising while holding onto furniture. Dillan’s medical history included an umbilical cord line placed during his neonatal intensive care unit stay. Anticoagulation with enoxaparin was started. Results of Dillan’s thrombophilia workup were normal except for factor V Leiden. He is heterozygous for the mutation. Dillan wants to crawl and cruise! Is it safe?
To help you answer this safety question, the following sections provide a definition for DVT, a list of treatment options (Table 1), a list of risk factors associated with the development of DVTs (Tables 2 and
3), an introduction to postthrombotic syndrome
(PTS), and results of a literature review focused on finding practice recommendations regarding early ambulation after acute DVT.
Deep Vein Thrombosis
A DVT is a blood clot in any vessel of the body’s deep venous system. DVTs can be partially or completely occlusive, can be fixed or embolic, and can
310 Journal of Pediatric Oncology Nursing 24(6); 2007
Early Ambulation After Deep Vein Thrombosis
Table 3.
Common Acquired Risks for Thrombosis Organized Using Virchow’s Triad
Alterations in Flow Vascular Endothelial Injury
Central lines
Immobilization
Trauma
Surgery/anesthesia
Cancer
Dehydration
Cardiac disease
Prosthetic valves
Thrombocytosis
Polycythemia vera
Central lines
Increasing age
Systemic lupus
Crohn’s disease
Ulcerative colitis
Diabetes mellitus
Infection
Trauma
Surgery
Cancer
Obesity
Smoking
Hypercoagulability
L-asparaginase
Heparin-induced thrombocytopenia
Estrogen/pregnancy
Antiphospholipid antibodies
Renal disease
Cancer develop suddenly or gradually. Patients with DVTs often have inherited/congenital and/or acquired risk factors that contribute to their development. More than 140 years ago, Rudolf Virchow described thrombosis as the result of alterations in blood flow, vascular endothelial injury, or alterations in the constitution of the blood (hypercoagulability) (Ennis, 2005).
When blood flow is sluggish in any of the body’s vessels for many hours, as happens when patients are confined to bed rest or are under general anesthesia for long operating room procedures, the first part of this triad, alterations in blood flow, occurs. Stasis allows blood coagulation to be completed at the initial site of thrombus formation (Hoffbrand, Moss, &
Pettit, 2006). When intravascular clotting starts, it often grows, mainly in the direction of the slowly moving venous blood. Untreated, about 1 clot in 10
(in adults) breaks loose and travels through the right side of the heart into pulmonary arteries, causing a pulmonary embolism (PE) (Guyton & Hall, 2006).
The practice of prescribing bed rest after acute DVT stems from fear that patients will develop PEs.
In pediatrics, the second component in Virchow’s triad, endothelial damage, is most often incurred when a central venous catheter is placed. These lines are thrombogenic because they damage vessel walls and disrupt blood flow. Although central lines are essential for the medical management of pediatric patients, they are associated with significant morbidity (
>
90% of
DVTs in neonates and 60% of DVTs in children are associated with central lines) and, occasionally, mortality (Andrew, Monagle, & Brooker, 2000).
The third part of Virchow’s triad consists of alterations in the constitution of the blood, causing hypercoagulability. Several congenital abnormalities in hemostasis have been identified, and strategies for prevention and treatment of DVT in both adults and children vary. Andrew et al. (2000) reported that without an additional acquired risk for thrombosis, it is rare for a child who inherits a single gene defect for thrombophilia to develop a DVT. However, children who are homozygous for a defect or are double heterozygous often present with symptoms of DVT in the newborn period or as children (Andrew et al.,
2000). Tables 2 and 3, organized using Virchow’s triad, list the more common inherited/congenital and acquired risks for thrombosis, respectively.
Literature Review
Fear of causing serious or fatal PE and a belief that pain and swelling would be improved faster by immobilization drive the traditional recommendation of bed rest in combination with anticoagulation
(Partsch, 2005). In 1944, William Dock, writing in the Journal of the American Medical Association , warned physicians about the hazards of complete bed rest. His article, “The Evil Sequelae of Complete Bed
Rest,” alerts readers to the dangers of this “highly unphysiologic and definitely hazardous form of therapy” (p. 1084). Fear of dislodging thrombi, especially in the lower extremities, has prompted many physicians to disregard Dock’s advice, ignore their knowledge
Journal of Pediatric Oncology Nursing 24(6); 2007 311
Blumenstein that immobility promotes stasis, and order lengthy bed rest for patients with acute DVTs. This practice is without evidence-based studies demonstrating that bed rest with anticoagulation is superior in reducing the risk of PE for patients. “Bed rest has obviously more risks concerning thrombus propagation and lifethreatening complications, especially in old patients, and does not prevent pulmonary embolism” (Partsch,
2001, p. 202).
Buller and colleagues (2004), reporting at the 7th
American College of Chest Physicians Conference, strongly recommended that patients with DVTs ambulate as soon as possible and as much as tolerated. A prospective, observational study of 2650 patients with acute, symptomatic DVTs or pulmonary embolism, all of whom were treated with low molecular weight heparin, was reported (Trujillo-Santos et al., 2005). Bed rest was prescribed for 54% of the patients, whereas the others had early ambulation.
Patients in the bed rest group tended to be sicker at baseline than the ambulation group, which is a limitation of this study. Over a 15-day period, 9 patients treated with bed rest and 6 of those ambulating developed clinically evident and radiographically confirmed PEs. The authors concluded that there was no apparent association between early ambulation and new, symptomatic PEs (Trujillo-Santos et al., 2005).
Partsch (2001) reported on 1289 consecutive patients admitted for acute DVT, all treated with low molecular weight heparin, early ambulation, and gradient compression therapy. The study, which identified 5 endpoints, concluded that the low incidence of recurrent and fatal PE in this series affirms the value of early ambulation with leg compression therapy.
Reporting on the findings of several adult studies,
Partsch (2001) concluded that bed rest is potentially harmful. Starting therapeutic doses of anticoagulation and encouraging patients to walk as soon and as much as possible with good compression therapy for lower extremity DVT are associated with better outcomes (decreased pain, decreased swelling, and decreased occurrence/severity of postthrombotic syndrome) (Partsch, 2001).
Although postthrombotic syndrome (PTS) is not a focus of this article, I want to provide some information about it because several studies cited in this article identified a reduction in PTS incidence and/or severity as an important study outcome or end point.
The clinical features of PTS are pain, swelling, visible collateral vein formation, and skin abnormalities that range from hyperpigmentation and induration to stasis ulcers (Manco-Johnson, 2006). Citing 4 studies in her article “How I Treat Venous Thrombosis in
Children,” Dr Manco-Johnson reported a PTS occurrence rate in children of 10% to 60% following DVT
(2006). The pathophysiology of PTS begins with venous hypertension caused by blood flow obstruction (by the thrombus) and/or refluxed blood flow attributable to incompetent venous valves damaged by the clot or mechanical therapies directed at breaking up the clot (eg, Angiojet system, Possis, Minneapolis,
MN) (Manco-Johnson, 2006). Therapies that reduce the incidence and severity of PTS, such as anticoagulation with early ambulation and gradient compression therapy, have important implications for long-term morbidity, especially for children with DVT because they might expect to have 5 to 8 decades of life after
DVT (unlike most adults with DVT).
The literature review can be summarized as follows: study populations were adults, often elderly, with no infants or children studied. All studies recommended the initiation of anticoagulation before ambulation or physical therapy. Some studies recommended immediate ambulation as tolerated, whereas others suggested a 48- to 72-hour waiting period before ambulating regularly. Most studies involved
DVT of the lower extremities and also recommended gradient compression therapy with ambulation
(Aschwanden, Labs, & Engel, 2001; Ciccone, 2002;
Partsch, 2000; Schellong et al., 1999). All studies reviewed for this article concluded that early ambulation with anticoagulation does not increase risk for patients for pulmonary embolism. Most studies reported improved outcomes on pain, swelling, and incidence of PTS with early ambulation.
Conclusions and Implications for Nursing Practice
Early ambulation and physical therapy are of particular importance to pediatric patients at risk for loss of range of motion, skin breakdown, or joint contracture if physical therapy or ambulation orders are held as a consequence of the development of a DVT. There are no published studies evaluating the safety and benefits of early ambulation and physical therapy in pediatric patients with acute DVTs. Clearly, this is an
312 Journal of Pediatric Oncology Nursing 24(6); 2007
Early Ambulation After Deep Vein Thrombosis issue nurses should study in children. In the interim, pediatric nurses and other health care providers are encouraged to consider the findings from the adult literature on this topic to matched pediatric patients.
Early ambulation and physical therapy, as tolerated, should be encouraged once anticoagulation is instituted. In addition, there were no reports that physical therapy, such as active or passive range of motion exercises, performed with the unaffected limbs caused any morbidity or mortality in patients with acute
DVT on anticoagulation therapy. Furthermore, the addition of gradient compression therapy for patients with lower extremity DVTs seems to further improve patient outcomes (Partsch, 2001). Early ambulation is not associated with an increased risk for pulmonary embolism in anticoagulated patients with acute deep vein thromboses.
References
Andrew, M., Monagle, P. T., & Brooker, L. (2000).
Thromboembolic complications during infancy and childhood . Hamilton, ON: B.C. Decker.
Aschwanden, M., Labs, K. H., & Engel, H. (2001). Acute deep vein thrombosis: Early mobilization does not increase the frequency of pulmonary embolism. Journal of Thrombosis and
Haemostasis , 85 , 42-46.
Buller, H. R., Agnelli, G., Hull, R. D., Hyers, T. M., Prins, M. H.,
& Raskob, G. E. (2004). Antithrombotic therapy for venous thromboembolic disease: The seventh American College of
Chest Physicians’ Conference on antithrombotic and thrombolytic therapy. Chest , 126 (Suppl.), 4015-4285.
Ciccone, C. D. (2002). Does ambulation immediately following an episode of deep vein thrombosis increase the risk of pulmonary embolism? Physical Therapy , 82 , 84-88.
Dock, W. (1944). The evil sequelae of complete bed rest. Journal of American Medical Association , 125 , 1083-1085.
Ennis, R. S. (2005). Deep venous thrombosis prophylaxis in orthopedic surgery. Retrieved September 15, 2007, from: http://www.emedicine.com/orthoped/topic600.htm.
Guyton, A. C., & Hall, J. E. (2006). Textbook of medical physiology . Philadelphia: Elsevier Saunders.
Hoffbrand, A. V., Moss, P. A. H., & Pettit, J. E. (Eds.). (2006).
Essential haematology . Malden, MA: Blackwell.
Manco-Johnson, M. (2006). How I treat venous thrombosis in children. Blood , 107 , 21-29.
Partsch, H. (2000). Compression and walking versus bed rest in the treatment of proximal deep venous thrombosis with low molecular weight heparin. Journal of Vascular Surgery , 32 ,
861-869.
Partsch, H. (2001). Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Journal of Vascular Diseases , 30 , 195-204.
Partsch, H. (2005). Immediate ambulation and leg compression in the treatment of deep vein thrombosis. Disease a Month , 51 ,
135-140.
Schellong, S., Schwarz, T., Kropp, J., Prescher, Y., Beuthein-
Baumann, B., & Daniel, W. (1999). Bed rest in deep vein thrombosis and the incidence of scintigraphic pulmonary embolism. Thrombosis and Haemostasis , 82 , 127-129.
Trujillo-Santos, J., Perea-Milla, E., Jimenez-Puente, A., Sanchez-
Cantalejo, E., del Toro, J., Grau, E., et al. (2005). Bed rest or ambulation in the initial treatment of patients with acute deep vein thrombosis or pulmonary embolism: Findings from the
RIETE registry. Chest , 127 , 1631-1636.
Continuing Education Credit
The Journal of Pediatric Oncology Nursing is pleased to offer the opportunity to earn pediatric hematology/oncology nursing continuing education credit for this article online. Go to www.aphon.org and select “Continuing Education.” There you can read the article again or go directly to the posttest assessment. The cost is $15 for each article. You will be asked for a credit card or online payment service number.
The posttest consists of 11 questions based on the article, plus several assessment questions (e.g. how long did it take you to read the article and complete the posttest?). A passing score is 8 out of 11 questions correct on the posttest and completion of the assessment questions yields one hour of continuing education in pediatric hematology/oncology nursing for each article.
The Association of Pediatric Hematology/Oncology Nurses is accredited as a provider of continuing nursing education by the American Nurses
Credentialing Center’s Commission on Accreditation.
Journal of Pediatric Oncology Nursing 24(6); 2007 313