Venous-Thromboembolism-In-Pregnancy-DrOD
advertisement
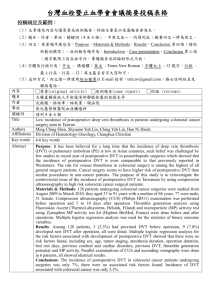
Venous Thromboembolism In Pregnancy By Prof.Osman Donia INTRODUCTION AND INCIDENCE • Pregnancy is a known hyper-coagulable state, with a five-fold risk of venous thromboembolism over the non-pregnant condition • 0.5 and 3 of every 1000 pregnancies are complicated by symptomatic deep venous thrombosis (DVT). • 25% may develop pulmonary embolism (PE), of which up to 15% are fatal. AETIOLOGY • • • • • Increase in the levels of coagulation factors VII, VIII, IX, and X. Increased fibrinogen levels. Increased platelet activation. Decreased protein-S and Antithrombin III concentrations. Venous stasis in the lower limbs due to pressure by the gravid uterus THROMBOPHILIA • Acquired thrombophilia • This is mostly associated with the antiphospholipid syndrome (APS). APS is the combination of lupus anticoagulant (LAC) with or without, anticardiolipin antibodies (ACA), with a history of recurrent miscarriage and or thrombosis. • • Inherited thrombophilias Protein-C, protein-S, and Antithrombin III deficiency. Risk factors for DVT / PE during pregnancy • • • • • • • • • • Maternal age > 35 years. Pre-pregnancy weight > 80 kg. Pre-existing Thrombophilia. Previous DVT. Severe varicose veins (V.Vs). Prolonged bed rest. Multi foetal pregnancies. Severe pre-eclampsia. Caesarean section delivery. Sepsis, especially pelvic. DEEP VEIN THROMBOSIS (DVT) • CLINICAL DIAGNOSIS • DVT usually presents clinically with pain in the calf muscles associated with varying degrees of redness, hotness, or swelling, especially unilateral oedema. DEEP VEIN THROMBOSIS (DVT) • INVESTIGATIONS • Colour Doppler Ultrasound: It allows assessment of the deep veins between the knee and the iliac veins and also allows for the dynamic assessment of femoral and iliac veins. It is currently the preferred first-line method for investigating a suspected case of DVT during pregnancy being an accurate, non-invasive procedure. • Venography: This allows excellent visualization of veins both below and above the knee. However it is an invasive procedure, requiring the injection of a contrast medium and the use of X-ray. This method is not preferable during pregnancy. DEEP VEIN THROMBOSIS (DVT) • MANAGEMENT • Anticoagulant therapy • 1. Heparin and LMW heparin derivatives: The preferred initial line of treatment, as they do not cross the placenta, are not teratogenic, and their effect can be stopped within hours by withholding further doses. Heparin prolongs the activated partial thromboplastin time (APTT), while calcium heparins affect factor X activity. • These drugs are regarded relatively safe; however prolonged therapy for more than 6 months may be associated with idiosyncratic reaction, thrombocytopenia and higher risk of osteoporosis. DEEP VEIN THROMBOSIS (DVT) 2. Oral anticoagulants: Warfarin prolongs the prothrombin time (PT). The drug crosses the placenta and can cause limb and facial defects in the first trimester, and fetal intracerebral haemorrhage in the third trimesters. Recently some centres use it in the 2nd trimester. DEEP VEIN THROMBOSIS (DVT) • Anticoagulant prophylaxis • Women with a history of DVT occurring during or following a previous pregnancy are given prophylactic LMW heparin derivatives during subsequent pregnancies at least in the last trimester that extends at least to the end of the puerperium. • Women with a history of DVT occurring in the nonpregnant state should be screened for thrombophilias, and offered anticoagulant prophylaxis at least starting from the second trimester. • Some women will require full anticoagulation throughout pregnancy as those with artificial heart valves and cases of APS with recurrent DVTs, or cases with a definite history of previous pulmonary embolism. PULMONARY EMBOLISM (PE) • PE is one of the fatal consequences of undiagnosed or improperly managed cases of DVT. • Clinical presentation • The most common presentation is mild breathlessness with inspiratory chest pain. • Associated tachycardia, hypoxia, pleural rubs and sometimes ECG changes will settle the clinical diagnosis. • A history of recent DVT event or the presence of clinical evidence of pelvic or lower limb DVT is an important clue for diagnosis and immediate management. PULMONARY EMBOLISM (PE) • Management • Once suspected, early intervention by full I.V. anticoagulant therapy may be life saving. Full I.V. heparinization is immediately started, with supportive oxygen therapy. • Definitive diagnosis is then required via ventilation / perfusion scan or pulmonary angiography. A positive diagnosis of PE will have a major impact regarding long-term anticoagulation.