Outpatient Disease Management of Deep Venous Thrombosis
advertisement

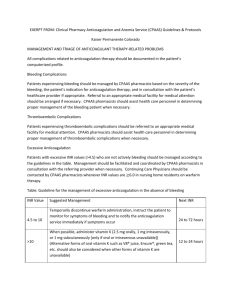
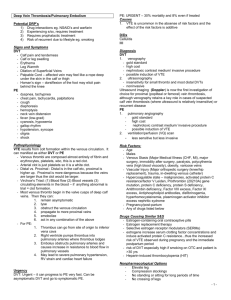
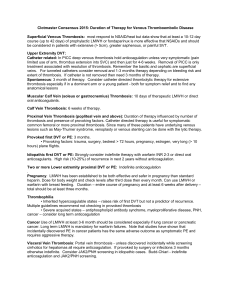
OHSU Outpatient Anticoagulation Guidelines Outpatient Disease Management of Deep Venous Thrombosis *Eligible population includes patients with diagnosis of DVT without contraindications to outpatient management. Relative contraindications include: respiratory instability, extensive clot burden, known potential for non-compliance, recent surgery/trauma, active bleeding, severe HTN, pregnancy, HIT, thrombocytopenia < 80,000 * Individual patient considerations and advances in medical science may supersede or modify these recommendations. Key Components Recommendations Diagnosis of acute DVT Risk/benefit assessment OAT selection Associated interventions Intensity of OAT Perform initial comprehensive history and physical considering conditions predisposing to DVT DVT confirmed by duplex ultrasonography or venography Assess risk for clotting (identify any provoking factors which will continue) Assess risk for bleeding (HAS-BLED, HEMORRHAGES, Outpatient Bleeding Risk Index) Start LMW or fondaparinaux Initiate concurrent warfarin therapy at 5 mg orally on day of DVT diagnosis; titrate to INR range of 2.0 – 3.0. Continue LMW (minimum of 5 days) until INR range 2.0 – 3.0 for ≥ 24 hours Consider rivaroxaban if LMW contraindicated or cost is prohibitive when FDA approved Consider dabigatran instead of warfarin if: age < 75, no renal disease, no history of GI bleeding and patient is taking full PO, and has no renal impairment (Cr Cl < 50 ml/min), cost is not an issue Compression socks 30 – 40 mmHG at ankle for 2 years Pain management: acetaminophen, narcotic if pain severe. Avoid NSAIDS if possible (if needed use salsalate or COX-II inhibitor). Target INR (range) 2.5 (2.0 – 3.0) Comments Initial or baseline lab work Testing/monitoring Duration of therapy/reevaluation Obtain baseline PT/INR, aPTT, CBC with plts Creatinine for elderly patients (>75yrs), those with Hx CHF or renal disease LFTs if Hx liver disease Hypercoagulability work up if unprovoked and patient is young, unusual site, or there is First INR day 3 after warfarin initiation Daily INRs thereafter while on LMW or fondaparinaux After sub Q medication discontinued INR testing every 2 – 3 times per week for the next 1 – 2 wks, weekly testing until stable, then every 4 weeks For indefinite therapy may check every 12 weeks if patient has stable INRs for 6 months or greater Superficial venous thrombosis: NSAID/heat till resolution of signs and symptoms at least of 10-12 day course of prophylactic LMWH or fondaparinux for patients with extensive (> 5cm), greater saphenous, or painful SVT Upper extremity DVT: Catheter related (esp PICC): remove catheter and hold anticoagulation unless very symptomatic (risk of bleeding with therapy can be as high as 25%) Spontaneous: 3 month of therapy. Muscular calf vein (soleus or gastrocnemius) Thrombosis: 10 days of LMWH. Calf Vein Thrombosis (tibial/peroneal): 6 weeks of therapy. Proximal vein thrombosis (popliteal vein and above): 3 months to indefinite. Duration of therapy influenced by number of thrombosis, provoking factors (surgery, pregnancy, etc.) and presence of hypercoagulable states Provoked first DVT: 3 months. • Provoking factors: trauma, surgery, bedrest > 72 hours, pregnancy, estrogen, very long (> 10 hours) plane flights. Idiopathic first DVT: At least 3 months then strongly consider indefinite therapy. High risk (10-25%) of recurrence in next 2 years without anticoagulation. • Risk groups for recurrence: Men, age > 65, postphlebitic syndrome, obesity, pulmonary embolism as event • Lesser risk of recurrence: women (esp. < 65) • Role of post-therapy D-dimer – controversial – strong risk factor for recurrence is positive (~9-10%/yr) but still 2.93.9%/yr risk with negative d-dimer Referral Two or more lower extremity proximal DVT: Indefinite anticoagulation Vascular surgery for catheter directed thrombolytic therapy for: 1) extensive UE thrombosis (especially if in a dominant arm or a young patient) or 2) very symptomatic common femoral or iliac thrombosis. Interventional Radiology for IVC filter removal (done with therapeutic INR) Hematology for hypercoagluable work up in patients with unusual DVT sites, idiopathic DVT Physical therapy for symptom relief Social worker/community services Interpreter services for language needs Patient education/Health literacy Management Model Specialty Populations Dietician for complicated dietary needs Primary Care Provider for health maintenance and nonanticoagulation related medical problems Teaching regarding: function of Anticoagulation Clinic, purpose of anticoagulation medications, importance of taking prescribed dosage, importance of regular blood testing, reporting of medication changes, reporting of change in tablet color, factors influencing anticoagulation (diet, ETOH, activity, health, OTCs, herbal remedies), notification of all providers/dentists, medications to avoid (ASA, NSAIDs, OTCs, herbal remedies, acetaminophen precautions), reporting signs of bleeding, contacting Anticoag Clinic staff, pregnancy risks and contraception needs. Health Literacy: baseline understanding (accurately able to explain reason for visit and relevant medical history, describe the alteration in self-care routines/abilities resulting from treatment, providers name and contact information, anticoagulation medication dosage and reason for taking anticoagulation medication, and verbalization of ability to adhere to proposed treatment plan for medication, blood testing, diet and activity), learning needs (disease/symptoms, medication administration, pain management, diet, drugfood interactions, diagnostic tests, safety and infection control) and barriers to learning (cognitive, physical, pain/comfort level, hearing/visual/speech limitation, cultural, emotional/fear, psychosocial, lack of desire/motivation, reading inability, financial, religious and language) Dedicated anticoagulation service Patient Self Testing if meets criteria Pregnancy: LMWH has been established to be both effective and safer in pregnancy than standard heparin. Dose for body weight and check levels after third dose then every month. Can use LMWH or warfarin with breast feeding. Duration – entire course of pregnancy and at least 6 weeks after delivery – total should be at least three months. Thrombophilia • Inherited hypercoagulable states – raises risk of first DVT but not a predictor of recurrence • Severe acquired states – antiphospholipid antibody syndrome, myeloproliferative disease, PNH, cancer – consider long term anticoagulation Cancer: Use of LMWH long term should be considered especially if lung cancer or pancreatic cancer. Long term LMWH is mandatory for warfarin failures. Incidentally discovered PE in cancer patients have the same adverse outcome as symptomatic PE and require aggressive antithrombotic therapy. General Reference: ACCP Conference on Antithrombotic and Thrombolytic Therapy. American College of Chest Physicians, 2012 (www.chestnet.org).