Working Effectively with Borderline Personality Disorder

Lisa Davies
Consultant Forensic Psychologist
Malta, October 2012
What is Borderline Personality Disorder
How to treat BPD effectively
Pink Elephants
Principles of Dialectical Behaviour Therapy
BPD is: a major health problem
Prevalent – severe, chronic and persistent
High mortality rate
10% of BPD patients will die by suicide
Much higher rate of suicide in the 36-65% who have attempted suicide or intentionally injured themselves in the past
The emotional costs are enormous
BPD individuals describe:
Anger, Emptiness, Depression and Anxiety
Extreme Frustration
They experience:
Brief psychotic episodes
They have:
Chaotic Relationships and Confused Identities
Suicidal ideation is common
Quality of Life ratings are low
Few treatments with proven efficacy
Emotional dysregulation
Inappropriate intense or uncontrollable anger
Affective Instability
Interpersonal dysregulation
A pattern of intense and unstable interpersonal relationships
Frantic Efforts to avoid abandonment
Self dysregulation
Identity disturbance
Emptiness
Behavioural dysregulation
Recurrent suicidal or para-suicidal behaviour
Impulsive behaviours
Cognitive dysregulation
Transient stress-related paranoid ideation
Severe dissociative symptoms
Biological and environmental factors account for BPD
BPD individuals are born with an emotional vulnerability
BPD individuals grow up in invalidating environments
Reciprocal influences between biological vulnerabilities and an invalidating environment lead to a dysfunction in the emotion regulation system.
High sensitivity to emotional stimuli – low threshold for an emotional response and quick reaction which results in responding to even low levels of stress
Emotional intensity – emotional reactions are seen to be extreme and difficult to regulate
Slow return to emotional baseline – emotional attention (to emotionally congruent information) and reactivation of memories.
The individual is told that they are wrong in both their description and reflections of their own experiences. In other words, their private experiences and expressions of emotions are not viewed as valid responses to events around them.
The environmental messages are that the individual feels something that they state they don’t, that they like something that state they don’t like or that they have done something which they state they haven’t.
Dialectics
Walking the middle path
Out of extreme ways of thinking and behaving
Things can both be true and not true
Achieving synthesis
See the validity in their statements
Search for the truth
I feel bad because I am ugly,
If I felt ugly I would feel bad too.
Therapists see suicide as a problem
Patients see suicide as the solution
Perceptions are diametrically opposed
Solutions in DBT include:
Solve the problem
Change your emotional reaction to the problem
Tolerate the problem
Stay miserable
Make things worse….
Behaviour Therapy
Behaviour is learned.
Basic principles of reinforcement or punishment
Define behaviour in behavioural terms
Shouted at me
Preparing to overdose by storing pills
Burst into tears when criticised
Vulnerability factors
Precipitating factors
Understanding the link
Explore consequences
Explore alternative solutions
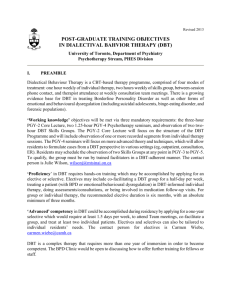
Stage 1 Therapy – Achieving behavioural control
Aim is to stabilise the client
Gain Commitment before entering therapy
Pro’s and cons
Devils Advocate
I’m going to ask you not to kill yourself whilst you are in this treatment. This is going to be difficult - so why would you do that?
Freedom to choose
You can choose not to do this, but will your life get better?
Highly structured
Group based Skills Training
Weekly individual therapy
Telephone consultation
Consultation Team Meeting for Therapists
do all members agree to be responsible for the outcomes of all patients treated by the team, not just the ones they treat individually?
Life threatening behaviours
Imminent treatment drop out
Team interfering behaviours
Who needs consultation?
Life threatening behaviour in our clients
Risk of imminent treatment drop out
Team interfering behaviours
lateness, not asking for help, lack of motivation,
What do I need from consult meeting?
A clearer case conceptualisation, help with a treatment plan?
Trouble finding empathy
Sharing successes
A feeling of dread when the phone rings
What’s getting in the way? What’s going well?
What can we do to help?
Dialectical Strategies
Core Strategies
Validation
Problem Solving
Stylistic Strategies
Irreverent communication
Reciprocal Communication
Case Management
Therapist supervision / Case consultation
Consultation to the patient
Environmental interventions
BPD clients often feel invalidated when:
Others focus on change (they feel blamed), but they also insist that their pain ends now
Or
When others try to get them to tolerate and accept their situation
BPD clients need to
build a better life and accept life as it is feel better and tolerate emotions better
Only striving for change is doomed to fail
The most caring thing a therapist can do is help clients change in ways that bring them closer to their ultimate goals
Clarity, precision and compassion are of the utmost importance in the conduct of DBT
The therapeutic relationship is a real relationship between equals
Principles of behaviour are universal
DBT therapists can fail
DBT therapy can fail even when therapists do not
Therapists treating borderline patients need support
Patients are doing the best they can
Patients want to improve
Patients need to do better, try harder, and be more motivated to change
Patients may not have caused all of their problems, but they have to solve them anyway
The lives of suicidal, borderline individuals are unbearable as they are currently being lived
Patients must learn new behaviours in all relevant contexts
Patients cannot fail in DBT.