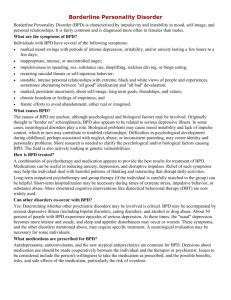
Borderline Personality Disorder: Keys to Effective Management
advertisement
Dialectical Behavior Therapy – Adaptation for Family Physicians Shelley McMain, PhD, C. Psych Head, BPD Clinic Centre for Addiction and Mental Health and Department of Psychiatry University of Toronto UNIVERSITY OF TORONTO Objectives Be familiar with DBT’s biosocial theory of BPD Identify two core DBT strategies used to effectively engage individuals with BPD Be familiar with strategies to reduce burnout and enhance self care BPD: Diagnosis Personality Disorder: enduring pattern of inflexible and maladaptive traits which causes impairment or distress arbitrary cutoff between BPD and traits: 5/9 utility of diagnosis diagnosis not made by your own reaction to the patient Dialectical Behavior Therapy “Standard DBT” is a comprehensive, multimodal treatment originally developed for people with BPD DBT has been adapted for various patient populations and across a variety of settings Any professional can implement selected strategies Vignette #1 • • • 42 year old single woman with chronic suicidal and self harm behavior Tx history includes numerous psychotropic medications, lengthy hospital stays and repeated ER visits, lengthy history of psychosocial treatments Patient frequently presents in a state of emotional – often angrily demanding more time and additional appointments Clinical Consideration How do you understand this patient’s problems? If you believe that this patient meets criteria for BPD, should you discuss the diagnosis? How should you engage this patient? Etiology of BPD: DBT’s Bisosocial Theory High Emotion Vulnerability Emotion Modulation Deficits Problematic Behaviours (e.g. suicide, substance use) DBT’s Biosocial Theory Fruzzetti et al. (2005) Emotion Vulnerability Heightened Emotional Arousal Pervasive History of Invalidating Responses Inaccurate/Extreme Expression Invalidating Responses from Others Fruzzetti et al, 2005 Educate Patients about BPD diagnosis • • • • Helps to de-stigmatize diagnosis Helps to increase hopefulness about possibility for change Encourages active participation in treatment planning Education about the diagnosis has been shown to reduce symptoms (Zanarini,2008) Adopt a Clear Treatment Structure Establish a treatment contract – clarify your roles, responsibilities, treatment goals Clarify structure of appointments – frequency of appointments, expectations about attendance Be clear about your limits and availability Anticipate and plan for crises APA, 2001 Guidelines on Concomitant Treatments Treatment by more than one clinician is viable however good collaboration is essential (APA, 2001). Someone should be identified as the primary clinician (APA, 2001; Oldhman et la., 2001; Gabbard, 2000; Gunderson, 2001; Linehan, 2003; Kernberg, ). Clinical Vignette #2 “I’ll kill myself if you don’t get me admitted to the hospital for the weekend” Patient’s parting words to therapist who indicated that she didn’t think that hospitalization would be helpful Clinical Considerations Is this client being manipulative? How should you respond? If you attend to the suicide threat will you reinforce this behavior? Should she be hospitalized? Functions of Self-injurious Behaviour Function % of patients To feel physical pain – to overcome psychic pain 59 To punish self for being “bad” 49 To control feelings 39 To exert control 22 To express anger 22 To feel-to overcome numbness 20 Gunderson, 2001 adapted from Shearer, 1994b Opt For the Least Restrictive Safe Treatment Setting Hospitalization may be iatrogenic Hospitalization should be viewed as a vehicle for maintaining safety Hospitalization should be considered if the risk of suicide outweighs the risk of inappropriate hospitalization Focus on helping patients cope in their natural environment Validate and Emphasize Patient Control Move flexibly from validating kernal of truth and helping patient take responsibility (APA, 2001) Don’t rush in and “take care of” patient” Don’t reinforce dysfunctional behavior with extra attention (i.e., avoid scheduling extra appointments in response to self-harm) Validate patients capability of behaving reasonably Validation Why Validate? an essential need of people with BPD the only way to build alliance reduces distress reduces polarization a prerequisite for cooperation How to Validate? listen, reflect make educated guesses at what she’s not saying (read her thoughts and emotions) normalise remember where she’s coming from find what is valid, right or understandable Encourage Effective Coping Always start by validating AND then paradoxically 1. Cheerlead - validate her strength and ability to cope/survive 2. Reinforce progress towards goal - reinforce the small steps 3. Negotiate - offer the options you are willing to offer and have clear limits 4. Suggest alternatives to the behaviour if possible Vignette #3 Thinking of your patient or seeing your patient evokes the following response: hope that she’ll get admitted to hospital relief when she cancels daydreaming about transferring her care Wish that you’d chosen another career feeling angry or irritated with her (comments to office staff) Reducing Burnout Validate yourself since stress is understandable Validate your patient – remind yourself of why she is doing the best she can Seek support from colleagues Assume responsibility for observing your personal limits Observing Your Personal Limits Monitor your limits with your patients Be honest with yourself and clear with your patients about your limits Observing limits is different than setting boundaries When your client exceeds your limits, validate and problem-solve negotiate a better arrangement for yourself (more resources for the patient?) Summary DBT’s biosocial theoretical model can increase understanding of symptoms. Educate patients about the diagnosis Treatment should be well structured Emphasis on validation in addition to helping the client control behavior Observe your limits and get support