No Slide Title
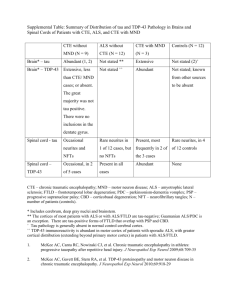
advertisement

Neuropathology in Chronic Traumatic Encephalopathy (CTE) with Motor Neuron Disease Compared to CTE and ALS Trever Symalla BS, Thor Stein MD/PhD, Christopher Leung MS, Lauren Ferrerosa MS, Anne McKee MD, Center for the Study of Traumatic Encephalopathy, Boston University School of Medicine Background Tau Scoring Scale Score Number of NFT’s * (20X field) Number of NFT’s (Amygdala/ Hippocampus) 0 0 0 1 1 1-9 2 2-5 10-19 3 6-9 20-29 4 10+ 30+ 0.80 CTE CTEM 0.60 0.40 0.20 0.00 * Sample Size: 9 CTEM cases, 16 CTE cases, matched for stage of CTE TDP-43 Positive Cases 1.00 ALS in Athletes: It has been shown that there is a significant increased incidence of ALS within athletes, especially professional football players. A recent study showed that there was a 4 times increased mortality from ALS and AD in professional football players. Stage 1 Stage 2 0.80 0.60 0.40 CTEM 0.20 0.00 Substantia Nucleus of Motor Anterior Nigra 12 Nucleus of Horn 10 CTE with Motor Neuron Disease (CTEM) is a subset of CTE patients that also meet the diagnosis of ALS. Normally, CTE doesn’t present with motor neuron disease but there are a significant number of individuals that have been diagnosed with CTE that also have motor neuron dysfunction. When looking at the gross pathology, these individuals show similar changes to those in ALS, particularly degeneration of the lateral cortical spinal tracts and loss of alpha motor neurons in anterior horn cells. Examine the distribution of tau and TDP-43 in CTEM and compare it to the distribution of tau in CTE and the distribution of TDP-43 in ALS. 1.00 * NFT: Neurofibrillary Tangles Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disease that is characterized by the loss of both upper and lower motor neuron function. ALS can be sporadic or have a genetic cause. While a variety of protein inclusions have been found in ALS, the most prevalent are TDP-43 inclusions. Objective Tau Positive Cases Percentage of Cases CTE Pathology is characterized by neurofibrillary tangles containing phosphorylated tau that accumulates in a characteristic pattern that is unique to CTE. The tau is found first in the depths of the sulci and perivascularly. The tau pattern is distinct from Alzheimer's disease (AD) and amyloid plaques are not present in CTE. Pathology that is more characteristic of other diseases has also been seen in subsets of individuals that have been diagnosed with CTE. These include TDP-43 inclusions seen in frontal temporal dementia (FTD) and ALS as well as Lewy bodies that are seen in Lewy body dementia and Parkinson’s disease. Scoring Method: Each brain is preserved and sectioned by specific brain regions. The slides where stained using immunohistochemistry for either phosphorylated tau or TDP-43. Each slide was examined using a light microscope in a 20X field and scored based on the scales below. Percentage of Cases Chronic Traumatic Encephalopathy (CTE) is a neurodegenerative disease that is caused by mild repetitive head trauma. This trauma is commonly seen in contact sports, such as football and boxing. CTE has also developed in military members exposed to blasts and autistic children who repetitively bang their heads on a wall. Clinically, CTE presents with memory difficulties, loss of concentration, mood changes that include aggression and erratic behavior, and suicidal thoughts and actions. Results Methods Conclusions Stage 3 Stage 4 TDP-43 Scoring Scale Score Number of Inclusions 0 0 1 1-2, or neurites 2 2-3 3 4-9 4 10+ The data clearly illustrates that, in the area’s selected, the tau pathology in CTE and CTEM are the same. This indicates that the disease process leading to the clinical picture of CTE in both CTE and CTEM demonstrates the same pathological processes. The next step is to obtain the TDP-43 profile for ALS cases and compare it to CTEM. If they align in the same matter, then it will appear that the same process was involved in each. If the pathologies differ, that would suggest that there is a link between the CTE and motor changes. References McKee AC, Gavett, BE, Stern RA,, Nowinski CJ,, Cantu RC, Kowall NW., Perl DP, Hedley-Whyte ET, Price B, Sullivan C, Morin P, Lee H, Kubilus CA, Daneshvar DH, Wulff M, Budson AE. (2010) J Neuropathol Exp Neurol 69(9), 918-29. Lehman EJ, Hein MJ, Baron SL, Gersic CM. (2012) Neurology 79, 1-5.