Delusions vs. Delirium
advertisement

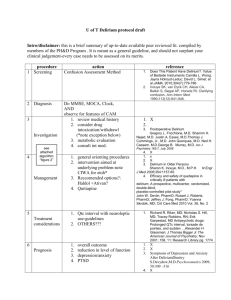
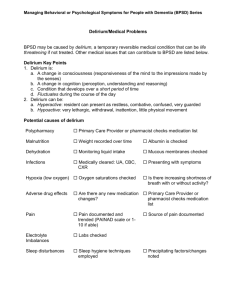
Riverside County Regional Medical Center Education Services Delusions vs. Delirium Confusional States in the Medically Ill Patient Jesse McDonald, CCRN The thin Caucasian man was barely able to sit still on the examining table due to agitation. He had multiple excoriations on his legs, arms, and abdomen. During the examination he dug “a bug” out of his skin. Showing his empty hand he exclaimed, “I got a good one”. The bugs began crawling about a month before and he was slightly frustrated that his wife could not share his observations. His wife said that he had not slept well in weeks and was even keeping her up at night, scratching himself until he bled. An MRI had been done as part of an evaluation for dementia and he was scheduled for a urology consult due to decreased urination. His medications included: ?? Cetirizing 10 mg daily ?? Furosemide 40 mg daily ?? Doxepin 25 mg at night He also was taking some over the counter anti-itch and cold medications. All medications were stopped and his delusions resolved overnight. He remained symptom-free during the six months prior to this report (4). [From a report by J.S Reichenberg] This report illustrates not only the importance of recognizing the effects of polypharmacy, especially anticholinergic side effects, but also how easily delirium can be mistaken for dementia. Confusion or altered mental state is a frequent finding in the medically ill. It is also a frequently missed finding (5-7). Shofield points out that what we call “delirium” in the United States is called “Acute Confusional State” or “Toxic Confusional State” in other countries (7). It is absolutely critical that medical etiologies be aggressively sought when faced with a patient who manifests behavioral or psychiatric symptoms. Manfredi (8) is an emergency department physician who pointed out, “all psychiatric patients will eventually die from a non-psychogenic disease” . Distinguishing between altered mental states manifested by delirium, mental illness, or dementia can be difficult due to the fact that each of these overlap or manifest an atypical presentation. Delusions and Hallucinations may be seen in both medical and psychiatric patients (1;3;9-14). Hallucinations are perceptions of reality that do not have a specific counterpart in reality. The patient may appear to be responding to internal events and talk to non-existent people. Delusions most often result from misapprehension of reality. The objects may exist but are perceived differently by the deluded person than others. Delusions may be defined as a belief that is patently bizarre, causing significant distress, or excessively pre-occupies the patient, especially if the person is subsequently unswayed by counter-evidence or reasonable arguments (13). An example of both of these distortions may be seen in the award-winning movie “A Beautiful Mind” in which director Ron Howard tells the story of Dr John Nash. Nash is the only schizophrenic to receive the Nobel prize in mathematics. Howard cuts between reality as experienced by Nash and by those around him. This allows the viewer to realize how real these are to the affected person. When we encounter a patient with an altered level of consciousness we need a way to quickly screen them for the presence of delirium. Delirium may be defined as an acute confusional state or syndrome. It is caused by severe physical or mental illness, or any process which interferes with normal metabolic function of brain (1) and represents a global brain dysfunction (5). It is characterized by a rapid onset accompanied by lucid intervals (5) and is associated with high morbidity and mortality approaching 76% in some patients (3;9). Wise describes delirium as a sign of glo bal cerebral dysfunction similar to the significance of angina in cardiac patients. He describes it as having a rapidly fluctuating course, lucid intervals, Sleep Wake disturbances, disorganized speech and thought, Disorientation, Altered perceptions, and Emotional lability (3). Dementia is a progressive decline in mental functioning that is associated with impaired memory, attention, language and problem solving. It has a gradual onset and is rarely reversible (9;14). Distinguishing delirium from dementia or mental illness is important. Patients with delirium are exhibiting the clinical signs of organ dysfunction (5). Ely states that in non-ICU Delirium is a Medical Emergency E.J. Griffin(2) patients it has been associated with a 25-33% in hospital mortality. It is also a frequently missed clinical sign, being unrecognized in up to 86% of patients (5). Since delusion is such a prominent part of delirium, it is difficult to distinguish them. Delirious patients commonly present with delusions, often involving small animals or distortions of environmental stimuli. Overt hallucinations are also commonly seen in delirium, such as talking with dead friends who are clearly visualized. Patients may be very hesitant to reveal these distortions and seek indirect evidence that they may or may not be valid. This indirect probing can easily be missed by staff members that do not recognize the context (7). Angina of the Brain Delirium is the tangible sign of cerebral insufficiency just as angina is a sign of cardiac insufficiency (3) As in angina, the most effective treatment is aimed at finding and correcting the underlying causes. And delirium is often multifactorial (3-5;9;15-17). Given the association with significant increases in mortality in medically ill patients who develop delirium, the mnemonic described by Wise is a grim reality: I WATCH DEATH. The 3 month mortality I WATCH DEATH is about 30%(3). M.G. Wise(3) Delirium, dementia, and psychiatric illness may all be associated with an altered mental state, may exhibit delusions or hallucinations, and may present with hypoactive, hyperactive, or mixed motor activity (35;7;17). It is often misdiagnosed by both nurses and physicians due to a lack of knowledge and active screening for this common syndrome (6). Because delirium has a strong association with clinical complications and morbidity we need to do a better job of screening our patients for this marker. It is possible to recognize this “Angina of the Brain” by closely observing the cognitive function of our patients (6). Angina has certain characteristics that help distinguish it from other forms of “Chest Pain”. Delirium also has a classic presentation. Classically Lucid I-Infectious W-Withdrawal A-Acute metabolic T-Trauma C-CNS pathology H-Hypoxia D-Deficiencies E-Endocrinopathies A-Acute vascular T-Toxins/Drugs H-Heavy metals One feature that should immediately suggest delirium is a relatively rapid onset (over hours or days) together with a fluctuating mental status. There will frequently be periods of lucidity alternating with worsening mental function, especially at night (3;5;7;9;17). Recognition of this may require the examiner to know the baseline mental status (1). When a patient is admitted with an altered mental status the nurse or physician should ask the family or caregiver about the patient’s normal functioning. The question “When was the last time they were acting normally?” may shine a spotlight on delirium. Dementia is commonly confused with delirium. Both When is the last may present with an altered mental status and perceptual distortion including hallucinations (16time they acted 18). In addition to having a progressive normally? neurodegenerative onset (9), dementia (such as Alzheimer’s Disease) does not commonly affect the motor or sensory function (2;19) while these are commonly disturbed in delirium. Two simple tests are available to help distinguish between these presentations. Alzheimer’s patients often have difficulty recalling common objects. Ask the patient to name as many “Zoo Animals” or grocery store items they can in 1 minute. The mean number is 18 while lists of less than 12 indicate a severe problem (2). Delirium is clinical indication of global cerebral dysfunction. Dysgraphia is one of the most sensitive indicators of delirium. Look for tremor to illegible scribble, spatial -- letter and line malalignment, misspelling and linguistic errors. Constructive apraxia is a sensitive indicator of confusional state. Look for an inability to draw a clock showing a particular time or 3-D cube (3). Delirium is a CLINICAL diagnosis Ultimately however, delirium is a clinical diagnosis. There are no tests that define it (1;6;9). Just as chest pain in a patient with cardiac risk factors is presumed to be cardiac angina until proved otherwise, so should an acute confusional state in a medically ill patient be considered delirium until ruled out. The presence of delusions, illusions, and hallucinations can lead to a presumption of psychiatric etiology. Shofield addressed this in a study of hospitalized patients who had recovered from delirium. Both illusions (distortion of reality) and hallucinations (distortion of internal stimuli) were common and vivid. Many patients described visits from friends (some dead) and there were frequent visual hallucinations of small animals (7). The author recalls an elderly woman who had a form UTI is a very of delirium often referred to as “ICU Psychosis” (5). During her delirium she believed she was in a “zoo” common cause and begged the staff to let her see the animals. The of delirium in staff thought she was delusional. Upon discharge, however, with her mental status restored she again the elderly (1) mentioned her disappointment that she could not see “the animals you kept talking about: the lions, and the bears, and the kangaroos”. From her room she could hear talk about ‘central lines’, ‘kangaroo’ pumps, and ‘bear’ ventilators! The information was distorted through her delirium but represented more illusion than delusion. Screening for Delirium According to the DSM IV criteria, there are four distinct features of delirium. A finding of delirium requires BOTH feature 1 and 2 together with feature 3 OR 4. This allows the design of a simple screening tool to rapidly screen patients for delirium (20). Called the “CAM-ICU” since it was designed for screening ICU patients, the tool is also useful for screening ANY patient who is able to respond to voice commands. The key to feature 1 is to ask: “Is the patient at their mental status baseline AND have they been at baseline for the past 24 hours?” If the patient has been continuously at baseline for the past 24 hours they do not have delirium now. If they do have an acute mental status change or fluctuating mental status THEN we ask “Do they show inattentiveness?” An easy way to demonstrate this is to ask the patient to squeeze your hand every time you say the letter “A”. Say the phrase ‘SAVEAHAART’ one letter at a time. The patient scores a point for each “A” they squeeze on AND a point for every letter that is NOT “A” that they DO NOT squeeze on. A total score less than 8 shows inattentiveness and feature 2 would be scored “Positive”. If EITHER feature 1 OR feature 2 is negative the patient DOES NOT have delirium and you may stop screening them for this. If the patient has BOTH feature 1 and feature 2, THEN we ask “Do they have EITHER disorganized thinking OR a currently altered level of consciousness?” If EITHER is present the patient DOES have delirium. If the patient has NEITHER feature 3 or feature 4 they do not have delirium now. Summary Mental status is a sensitive indicator of cerebral function. An acute confusional state in a medically ill patient is a medical emergency that carries a serious risk of complication or death. The Society of Critical Care Medicine has recommended that all mechanically ventilated patients be monitored daily for delirium (5). Treatment involves an aggressive search for treatable correctable causes and removal of all unnecessary medications. Mechanical restraints should be avoided whenever possible (3-5;9;16;17). Reference List 1. Wikipedia 2007 Delirium. 2. Griffin E.J. 2005 When Does Memory Loss Indicate Alzheimers Disease? 3. Wise M.G., Cassem N.H. 1988 Behavioral Disturbances in the ICU. In: Civetta J.M., Taylor R.W., Kirby R.R., eds. Critical Care. Philadelphia PA: J. B. Lippincott; 1595-1604 4. Reichenberg J.S., Magid M., Drage L.A. 2007 A Cure for Delusions of Parasitosis. JEADV1 5. Ely E.W. 2006 The Delirium Dilemma -- Advances in Thinking about Diagnosis, Management, and Importance of ICU Delirium. GE Medical Healthcare 6. Ohki t., Matsushima E., Shibuya M., Sunamori M. 2006 An Evaluation strategy for the early detection of postoperative delirium. Psychiatry and Clinical Neurosciences 60:277-282 7. Schofield K. 1997 A Small Exploratory Study of the Reaction of Older People to an Episode of Delirium. Journal of Advanced Nursing 25:942-952 8. Manfredi A. 1990 Psychiatric Patients in the ED. 9. Burton J. 2007 Dementia and Delirium. 10. David A.S. 1999 On the impossibility of defining delusions. Philosophy, Psychiatry and Psychology 6:17-20 11. Scott L.K. 2005 Sepsis-associated Encephalopathy. 12. Univ of Iowa 2007 Delirium. 13. Wikipedia 2007 Delusion. 14. Wikipedia 2007 Dementia. 15. Francis J., Martin D., Kapoor W.N. 1990 A prospective study of delirium in hsopitalized elderly. JAMA 263:1097-1101 16. Palmer T.R. 2006 Delirium Was Likely Due to Multiple Factors, Rather than Gatifloxacin Induced. JAGS 54:159 17. Rabins P.V. 1999 Mental Illness in the Elderly: Principles and Common Problems. In: Barker L.R., Burton J.R., Zleve P.D., eds. Principles of Ampulatory Medicine. 5 ed. Baltimore MD: Williams & Wilkins; 190-196 18. McCusker J., Cole M., Abrahamowicz M., Han L., Podoba J.E., Ramman-Haddad L. 2001 Environmental Risk Factors for Delirium in Hospitalized Older People. JAGS 49:1327-1334 19. Hayden M., Rowett D.L. 2005 Alzheimer's Disease. Healthwise 20. Ely E.W 2007 Delirium Training for Professionals (video) available at www.icudelirium.org DEMENTIA versus DELIRIUM Delusions, Delirium and Dementia in the Medically Ill Patient DEMENTIA ?? Is often the result of progressive neurodegenerative disease (Alzheimer’s Disease) ?? Patient experiences altered mental status ?? Patient has difficulty recalling common objects ?? Perceptual distortions in the form of hallucinations ?? Motor and sensory functions may not be affected DELIRIUM ?? Is a medical emergency ?? A sign of global cerebral dysfunction ?? Sign of cerebral insufficiency ?? Often multifactorial ?? Treatment is to find and correct the underlying cause ?? Patient may experience hallucinations ?? Patient may experience illusions ?? Causes include: o Infection o Withdrawal o Acute metabolic o Trauma o CNS pathology o Hypoxia o Deficiencies o Endocrinopathies o Acute vascular o Toxins / drugs o Heavy metals ?? Onset may be rapid over hours or days ?? Mental status fluctuates moment to moment, day to day OBSERVATIONS TO MAKE & QUESTIONS TO ASK Observe the cognitive status of the brain: Do they seem to improve at times? What is the patient’s baseline cognitive status? What were they like before this hospitalization? When was the last time they acted normally? Recognizing Delirium No Is the patient fully alert and oriented? When was the patient last fully oriented? Less than Hours or Days? More than Hours or Days? Yes Monitor for ALOC Probably not delirium. Monitor for periods of lucidity. If Seen, Consider Delirium Review Risk Factors I– Infection W- Withdrawal Watch for Lucid Intervals Document Assessment Notify Physician Review Labs Review Medications A- Acute Metabolic T- Trauma C- CNS Pathology H- Hypoxia