Analysis of the evidence for the lower limit of systolic
advertisement

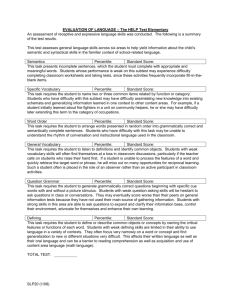
Continuing Medical Education Article Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children Ikram U. Haque, MD, FAAP; Arno L. Zaritsky, MD, FAAP, FCCM LEARNING OBJECTIVES On completion of this article, the reader should be able to: 1. Identify key factors that contribute to determining the optimal blood pressure goals for resuscitation of critically ill children. 2. Select appropriate blood pressure targets in critically ill children. 3. Recall the relationship between systolic, diastolic, and mean arterial blood pressure. Both authors have disclosed that they have no financial relationships with or interests in any commercial companies pertaining to this educational activity. Lippincott CME Institute, Inc., has identified and resolved all faculty conflicts of interest regarding this educational activity. Visit the Pediatric Critical Care Medicine Web site (www.pccmjournal.org) for information on obtaining continuing medical education credit. Objective: Systolic blood pressure (SBP) and mean arterial pressure (MAP) are essential evaluation elements in ill children, but there is wide variation among different sources defining systolic hypotension in children, and there are no normal reference values for MAP. Our goal was to calculate the 5th percentile SBP and MAP values in children from recently updated data published by the task force working group of the National High Blood Pressure Education Program and compare these values with the lowest limit of acceptable SBP and MAP defined by different sources. Design: Mathematical analysis of clinical database. Methods: The 50th and 95th percentile SBP values from task force data were used to derive the 5th percentile value for children from 1 to 17 yrs of age stratified by height percentiles. MAP values were calculated using a standard mathematical formula. Calculated SBP values were compared with systolic hypotension definitions from other sources. Linear regression analysis was applied to create simple formulas to estimate 5th percentile SBP and 5th and 50th percentile MAP for different age groups at the 50th height percentile. Results: A 9 –21% range in both SBP and MAP values was noted for different height percentiles in the same age groups. The 5th percentile SBP values used to define hypotension by different sources are higher than our calculated values in children but are M lower than our calculated values in adolescents. Clinical formulas for calculation of SBP and MAP (mm Hg) in normal children are as follows: SBP (5th percentile at 50th height percentile) ⴝ 2 ⴛ age in years ⴙ 65, MAP (5th percentile at 50th height percentile) ⴝ 1.5 ⴛ age in years ⴙ 40, and MAP (50th percentile at 50th height percentile) ⴝ 1.5 ⴛ age in years ⴙ 55. Conclusion: We developed new estimates for values of 5th percentile SBP and created a table of normal MAP values for reference. SBP is significantly affected by height, which has not been considered previously. Although the estimated lower limits of SBP are lower than currently used to define hypotension, these values are derived from normal healthy children and are likely not appropriate for critically ill children. Our data suggest that the current values for hypotension are not evidence-based and may need to be adjusted for patient height and, most important, for clinical condition. Specifically, we suggest that the definition of hypotension derived from normal children should not be used to define the SBP goal; a higher target SBP is likely appropriate in many critically ill and injured children. Further studies are needed to evaluate the appropriate threshold values of SBP for determining hypotension. (Pediatr Crit Care Med 2007; 8:138 –144) KEY WORDS: blood pressure; hypotension; infant; child onitoring blood pressure in critically ill or injured children is considered one of the mainstays for patient evaluation in the prehospital setting, pe- diatric emergency department, and intensive care unit (1–5). Studies in adults and children with trauma showed that systolic blood pressure (SBP) is a predictor of mortality (6) and that prehospital Assistant Professor (IUH), Professor and Chief (ALZ), Division of Pediatric Critical Care Medicine, Department of Pediatrics, University of Florida College of Medicine, Gainesville, FL. Copyright © 2007 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 138 DOI: 10.1097/01.PCC.0000257039.32593.DC hypotension is associated with an increased risk of mortality (7–10). The depth and duration of hypotension appear to have a direct relationship with adverse hospital outcome in emergency department patients with nontraumatic shock (11). Moreover, hypotension is used as a criterion for diagnosis of “decompensated” shock along with other features of poor perfusion in pediatric patients (1, 3). Most published guidelines define hypoPediatr Crit Care Med 2007 Vol. 8, No. 2 tension in children as an SBP below the 5th percentile for age. Table 1 is a summary of SBP values as used by the Pediatric Advanced Life Support (PALS) course, Brain Trauma Foundation (BTF), and International Pediatric Sepsis Consensus Conference to define hypotension in children. These guidelines for hypotension are reportedly derived from the reports of the task force on blood pressure control in normal healthy children (12, 13). Although age-related “norms” of blood pressure are published in most of the relevant pediatric emergency and critical care training manuals and textbooks, the evidence for these norms is usually not referenced and the publications do not report the confidence intervals for normal blood pressure or adjustments of these norms for gender or for height and weight of the child within an age group. Variation in the age-based range of blood pressure was observed in the recently published international consensus conference definitions of sepsis and organ dysfunction in children, which included a table of the lower limits of acceptable SBP (14). These guidelines reportedly were based on a review of published studies but appear to overestimate the lower limits of SBP in different aged children, as shown in Table 1. Hemodynamic treatment of shock is aimed at maintaining oxygen delivery above a critical threshold and increasing mean arterial pressure (MAP) to a level that allows appropriate distribution of cardiac output for adequate tissue perfusion (15). In adults, a MAP range from 60 to 90 mm Hg has been used as the desired target (16 –19) for therapeutic end points such as improved urine output and creatinine clearance (20). In children, several sources recommend early aggressive restoration of hemodynamic end points, which include normalization of MAP to age-appropriate values in pediatric shock states (1, 3, 21–23). Unfortunately, there is little objective evidence defining the target values of MAP in pediatric patients. Furthermore, no age-related MAP nomogram in children is available for clinicians to use as a reference. Neonatal studies have collected data on the normal values of blood pressure in very low birth weight infants (24 –26), but there are no pediatric studies of MAP from children in the pediatric intensive care unit. When mathematical integration of invasive arterial pressure measurements to calculate the MAP is not available, MAP is typically calculated by using the following formula, which assumes that one third of the cardiac cycle is spent in systole (27–29): MAP ⫽ diastolic pressure ⫹ ([systolic pressure ⫺ diastolic pressure]/3) [1] The aim of this study was to use a large published database of blood pressures in children to estimate the lower limits of systolic pressure and define normal mean arterial pressures using the preceding equation and to compare these estimates with those that are currently being used. To achieve our aim, we used data from the working group of the National High Blood Pressure Education Programs, which recently published updated guidelines on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents (30). We analyzed the data from this report using standard mathematical models to calculate the 5th percentile values of SBP and diastolic blood pressure for the entire pediatric population. Table 1. Definition of hypotension in children by different sources Hypotension Guidelines, mm Hg Age Group 0 days–1 wk 1 week–1 mo 1 mo–1 yr ⬎1–5 yrs 6–12 yrs 13–18 yrs Pediatric Advanced Life Support Brain Trauma Foundationa International Pediatric Sepsis Consensus Conferenceb ⬍60 ⬍60 ⬍70 70 ⫹ 2 ⫻ yrs 70 ⫹ 2 ⫻ yrs (up to 10 yrs) ⬍90 (⬎10 yrs) ⬍90 ⬍65 ⬍65 ⬍65 ⬍70–75 ⬍80–90 ⬍59 ⬍79 ⬍75 ⬍74 ⬍83 ⬍90 ⬍90 a Brain Trauma Foundation last accessed October 14, 2005 (http://www2.braintrauma.org/ guidelines/downloads/btf_guidelines_prehospital.pdf); b corrected values, letter to the editor, Goldstein et al. Pediatr Crit Care Med 2005; 6:500 –501. Pediatr Crit Care Med 2007 Vol. 8, No. 2 MATERIALS AND METHODS The updated blood pressure report is based largely on data collected by the National Center for Health Statistics with ⬎32,000 boys and ⬎31,000 girls including new data from the 1999 –2000 National Health and Nutrition Examination Survey. The blood pressures reported by the task force were obtained by auscultatory method in normal healthy children. The revised blood pressure tables now include the 50th, 90th, 95th, and 99th percentiles by gender, age, and height. The values for 50th percentile and 95th percentile of SBP and diastolic blood pressure were extracted from the task force data for all age groups across the range of height percentiles into tables for both boys and girls (30). We used simple mathematical calculations to derive the 5th percentile values of SBP from these data, assuming that the data in this large database are normally distributed so that the difference in pressure between the 95th and 50th percentile should be the same as the difference between the 5th percentile and 50th percentile. Tables for values of the 5th percentile SBP for different ages, genders, and height percentiles were generated. We then compared calculated values of SBP with currently used guidelines for defining hypotension from different sources. The published data and our calculated values of SBP and diastolic pressure at various percentiles of height for a given age were then used to estimate the MAPs for age, gender, and height percentile using the previously stated formula. We then used linear regression to determine the line of best fit and from that regression created simple mathematical formulas for clinicians to approximate values of the 5th percentile SBP and 5th and 50th percentile for MAP at the 50th height percentile for children 1–17 yrs of age. We also calculated the effect of height on the range of SBP values and derived simple estimates to adjust the SBP according to the height percentile. RESULTS The demographic information on the source of blood pressure data of the population was described in detail in the original report (30). Table 2 shows the 5th percentile values of SBP from age 1–18 yrs for males and females; the table also details the range of SBP for each age group ranging from the 5th percentile to 95th percentile for height. As seen in this table, the SBP in the same age group varies by approximately 8 –9 mm Hg between the 5th and 95th height percentile in males and by approximately 6 –7 mm Hg in females. Relative to the mean SBP, the magnitude of the difference between the 5th and 95th height percentile com139 Table 2. Calculated 5th percentile systolic blood pressure (mm Hg) according to height percentiles among boys (M) and girls (F) 1–18 yrs old Fifth Percentile Systolic Blood Pressure, Percentile for Height 5th 25th 50th 75th 95th Age, Yrs M F M F M F M F M F 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 62 67 68 70 72 73 74 77 77 79 81 83 87 88 92 93 97 66 68 68 71 71 74 76 78 78 80 82 85 87 89 90 91 91 65 70 71 73 76 76 77 80 80 83 85 86 88 91 95 96 98 68 70 71 73 74 76 78 78 81 83 85 87 89 89 92 93 93 67 70 73 75 78 78 79 82 82 85 87 89 90 94 95 98 100 68 71 71 74 76 77 79 81 83 85 85 87 90 92 93 93 93 70 72 76 78 78 81 81 82 85 85 87 91 92 96 97 101 102 71 71 74 74 77 79 79 82 84 86 88 90 92 93 93 96 96 72 74 77 79 80 83 83 84 87 89 89 93 94 98 99 103 104 73 73 76 76 79 81 82 84 86 88 90 92 92 95 95 98 98 pared with the 50th height percentile SBP by age was 7–14.9% in boys and 5.4 –11.1% in females. This variation is seen graphically in Figure 1. The calculated values for MAP at the 5th, 50th, and 95th percentiles stratified by different height percentiles in the same age group are shown in Table 3. A difference of approximately 5– 6 mm Hg is noted between 5th and 95th height percentiles for the same age group in both males and females. This results in a range of MAP across different heights of 8 –13% in girls and 9 –21% in boys. There is wide variation, however, in the normal MAP values across the 5th and 95th percentiles for a given height. Linear regression was applied to the 50th height percentile group for the 5th and 50th percentile values of SBP and the 5th and 50th percentile MAP (data not shown). Simplified formulas for estimating the 5th percentile SBP and the 5th and 50th percentile MAP for 50th percentile of height were derived from these values, as shown next. A simple calculation can be used to estimate 5th percentile SBP adjusted for height percentile for each quartile above or below 50th height percentile. Our calculations suggest that for males ⫾2 mm Hg for each height quartile and for females ⫾1.5 mm Hg for each quartile of height can approximate the 25th to 75th percentile SBP values. The line of best fit for MAP was exponential, but the linear equations produce estimates that are within the range of values across the range of height percentiles 140 and were chosen because they are easier to recall. SBP (5th percentile at 50th height percentile) ⫽ 2 ⫻ age in years ⫹ 65 [2] SBP (50th percentile at 50th height percentile) ⫽ 2 ⫻ age in years ⫹ 85 [3] MAP (5th percentile at 50th height percentile) ⫽ 1.5 ⫻ age in years ⫹ 40 [4] MAP (50th percentile at 50th height percentile) ⫽ 1.5 ⫻ age in years ⫹ 55 [5] The 5th percentile SBPs are plotted as shown in Figure 1 for both males and females along with the PALS, Brain Trauma Foundation, and International Pediatric Sepsis Consensus Conference definitions and our estimated formulas for SBP determined from regression analysis. The graph shows that systolic blood pressure limits defined by both PALS and Brain Trauma Foundation are high compared with our calculated values, and the PALS limit often exceeds the 5th percentile SBP even in children at the 95th percentile of height. Moreover, the graph illustrates that most normal healthy ad- olescents exceed the 90 mm Hg threshold for lower limit of acceptable blood pressure recommended in the PALS and Advanced Cardiac Life Support courses for adolescents. DISCUSSION The early detection and rapid treatment of hypotension are important in the management of critically ill and injured children. Moreover, MAP is often used as a therapeutic end point in shock management. Thus, it is important to define the normal ranges for both variables in children. These normal values represent a starting point for thinking about the desired blood pressure target, but the desired target blood pressure in a critically ill or injured child is likely higher than these lower limits of normal blood pressure obtained in healthy children. Although not evidence based, hypotension is typically defined as an SBP less than the 5th percentile for age. Since it is often difficult to recall blood pressure data listed in tables by age, various formulas have been used to estimate the lower limit of acceptable blood pressure. For example, the formula used in PALS training materials (1) states that the lower limit of acceptable SBP is 70 ⫹ 2 ⫻ (age in years) for children from 1 to 10 yrs of age. For children ⬍1 yr, the lowest acceptable SBP is 60 mm Hg up to 1 month and 70 mm Hg from 1 month to 1 yr. For children ⬎10 yrs of age, the lowest acceptable SBP is 90 mm Hg; the latter is consistent with Advanced Cardiac Life Support guidelines for defining hypotension in adults (31). A review of different sources revealed substantial variation in their definition of systolic hypotension, and current sources do not consider the variation in blood pressure due to height differences within an age group. Analysis of our derived data from the updated blood pressure data from the task force report does not agree with any of the recommended threshold blood pressures to define hypotension, making it difficult for the clinician to know which source to use and remember. Furthermore, it is interesting to note that the threshold blood pressure values used in the Paediatric Logistic Organ Dysfunction score are much higher than any of the current threshold blood pressure values that define hypotension Pediatr Crit Care Med 2007 Vol. 8, No. 2 Figure 1. Fifth percentile systolic blood pressure (BP) according to height (HT) percentiles plotted against Pediatric Advanced Life Support (PALS), Brain Trauma Foundation (Brain Trauma), and International Pediatric Sepsis Consensus Conference (Int Ped Sepsis) hypotension guidelines, and our new estimates based on linear regression R2 for boys ⫽ .99 (top) and for girls ⫽ .98 (bottom). Gray lines and the shaded area indicate the calculated values. Pediatr Crit Care Med 2007 Vol. 8, No. 2 141 Table 3. Calculated mean arterial blood pressure (mm Hg) according to height percentiles among boys (M) and girls (F) 1–18 yrs old Mean Arterial Blood Pressure for Boys and Girls, Percentile for Height Age, Yrs 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Percentile for Blood Pressure M F M F M F M F M F 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 5 50 95 30 49 69 35 54 73 39 58 77 42 61 79 45 63 82 47 66 84 51 67 83 50 69 87 51 70 88 52 71 90 54 72 91 54 73 92 56 75 93 59 75 91 58 77 96 60 79 98 63 81 100 35 53 71 39 57 75 42 60 78 45 63 80 46 64 82 49 66 84 50 68 85 52 70 87 53 71 89 54 72 90 55 73 91 57 75 92 58 76 94 60 77 95 61 78 96 61 79 96 61 79 96 33 52 70 38 56 75 41 60 78 43 63 82 47 66 84 49 67 86 50 69 88 53 71 89 53 72 91 55 73 92 56 74 92 57 75 94 57 76 95 59 78 96 61 79 98 62 81 99 63 83 102 37 54 72 41 58 76 44 61 79 46 64 82 48 66 83 50 68 85 51 69 87 52 70 88 54 71 89 55 73 90 56 74 92 58 75 93 59 77 94 60 78 96 61 79 97 62 80 98 62 80 98 34 53 72 39 57 76 42 61 80 46 64 83 49 67 85 50 69 87 52 70 89 54 72 91 55 73 92 56 75 93 57 75 94 58 77 95 59 77 96 61 79 97 62 80 99 63 82 101 65 84 103 37 55 73 42 59 77 44 62 80 47 65 83 49 67 85 51 69 86 52 70 88 54 71 89 55 73 90 56 74 92 57 75 93 58 76 94 60 78 95 61 79 97 62 80 98 63 81 99 63 81 99 36 54 73 40 59 77 44 62 81 47 66 84 49 68 87 52 70 88 53 72 90 55 73 92 56 75 93 56 75 94 58 76 95 60 78 96 60 79 97 62 80 99 63 82 100 65 83 102 67 85 104 39 57 74 42 60 78 46 64 81 47 65 84 50 68 86 52 69 87 53 71 89 55 72 90 56 74 91 57 75 93 59 76 94 60 78 95 61 79 97 62 80 98 63 81 99 63 82 100 65 82 100 37 56 74 41 60 79 45 64 82 48 67 86 51 69 88 53 71 90 54 73 92 56 75 93 58 76 94 59 77 96 59 78 96 61 79 98 61 80 99 63 82 100 64 83 102 66 85 104 69 87 106 40 58 76 44 62 80 47 65 83 49 67 85 52 69 87 54 71 89 55 72 90 56 74 91 57 75 93 59 76 94 60 78 95 61 79 97 62 80 98 64 81 99 64 82 100 66 84 101 66 84 101 5th (32). These empirically derived blood pressure values suggest that our current thresholds are too low. Our study analyzed a large database of blood pressures in children to provide objective evidence for the lowest acceptable SBP and MAP. Our data show that the definition of the 5th percentile SBP from all the currently used sources is often higher than the values calculated based on the largest available database of 142 25th 50th 75th blood pressure in children. Using a regression model, we developed new simple formulas that give a more accurate approximation of 5th percentile SBP for different age groups in normal children from 1 to 17 yrs of age: SBP (5th percentile at 50th height percentile) ⫽ 2 ⫻ age in years ⫹ 65 [6] 95th It is important for clinicians to know that there is a fairly large difference on a percentile basis between the lower limit of SBP for a short vs. a tall child. This variation has not previously been reported or used to adjust the goal for assessment or blood pressure target. We do not know the clinical or pathophysiologic significance of this observation. The estimated SBP for 25th and 75th percentile height children at a given age can be estimated by adding or Pediatr Crit Care Med 2007 Vol. 8, No. 2 subtracting 2 mm Hg for boys and 1.5 mm Hg for girls from the SBP estimate at the 50th percentile of height. Another important finding was that although the adult Advanced Cardiac Life Support guideline for hypotension uses 90 mm Hg beyond 12 yrs of age, the 5th percentile values for SBP in normal children in this age group were ⬎90 mm Hg. The clinical implication of this is not clear except that it suggests that clinicians may be accepting a lower SBP than appropriate. Moreover, using the lower limit of SBP as the definition of decompensated shock and hypotension and especially as the target for resuscitation may not be appropriate since these definitions are based on data in normal children and do not account for the stress response that occurs in seriously ill or injured children. For example, in a recent study, Dark et al. (33) followed a cohort of children admitted to the emergency department with blunt trauma and found that these patients presented with relative systolic hypertension compared with ageappropriate SBP as estimated by the guidelines. They speculated that apparently normal blood pressure in children with blunt trauma could represent relative hypotension. Another study evaluated the relationship between blood pressures and outcome after severe traumatic brain injury in pediatric patients (34). Poor outcome was associated with an SBP less than the ageadjusted 75th percentile even if the SBP was ⱖ90 mm Hg. White et al. (35) reported that the odds of survival increased 19-fold in pediatric severe traumatic brain injury patients with maximum SBP of ⬎135 mm Hg, also suggesting that supranormal blood pressures are associated with improved outcome in this patient population. These studies highlight that a higher SBP target may be particularly important in children with traumatic brain injury in whom cerebral perfusion is determined, in part, by maintenance of an adequate perfusion pressure when intracranial pressure is increased. It is noteworthy, however, that the Brain Trauma Foundation still uses an SBP ⬍90 mm Hg to define hypotension in adolescents even though a much higher SBP is needed to maintain cerebral perfusion pressure ⬎70 mm Hg if one assumes that intracranial pressure is 20 mm Hg. Since one of the major determinants of tissue perfusion pressure is MAP, it is typically used in shock states to estimate tissue perfusion pressure and thus blood flow. For example, cerebral perfusion pressure (CPP) is calculated by the following formula (36): Pediatr Crit Care Med 2007 Vol. 8, No. 2 CPP ⫽ mean arterial pressure ⫺ intracranial pressure [7] Hence, it is important for clinicians caring for critically ill children to know whether a child’s MAP is appropriate for his or her age. We calculated the values of MAP tabulated according to height percentile for different age groups. The optimal MAP to achieve adequate tissue perfusion pressure in shock is unknown and likely varies according to the type of shock. As noted, a higher MAP is likely needed in children with increased intracranial pressure. Conversely, in a child with cardiogenic shock treated with vasodilators, adequate tissue perfusion and improved myocardial performance may be achieved at a low MAP by maximizing vasodilator therapy since blood flow is proportional to MAP ⫼ systemic vascular resistance. As a starting estimate of adequate perfusion pressure, it may be appropriate to choose the 50th percentile MAP for age and height as a target based on the preceding observations that critically ill children often have elevated blood pressures. Using regression analysis, we created a formula that approximates the MAP for age in both males and females: MAP (5th percentile at 50th height percentile) ⫽ 1.5 ⫻ age in years ⫹ 40 [8] MAP (50th percentile at 50th height percentile) ⫽ 1.5 ⫻ age in years ⫹ 55 [9] Clinicians should recall that MAP values vary across the height percentile within the same age group, and this variation may need to be considered when caring for a very short or tall child. CONCLUSIONS We developed new estimates of the fifth percentile SBP for children 1–17 yrs of age from analysis of recently published blood pressure data from the Task Force on Hypertension. Most of the current guidelines use higher values for defining hypotension compared with our estimate from a large pediatric blood pressure database. Since the “normal” blood pressures are obtained from healthy children at rest, it is rational to use a higher threshold for defining hypotension in critically ill children than currently used. Furthermore, since there is a 5–15% variation in normal SBP from the 5th to 95th percentile height, the clinician may need to consider using a length-based system for determining the appropriate blood pressure target. Moreover, the clinician should recognize that automated blood pressure devices are not reliable when distal pulses are weak to absent, and other signs of poor perfusion should be used to define severe shock besides just a low SBP. Clearly, there is a critical need for studies to validate the appropriate blood pressure target and to better define hypotension in critically ill children. To avoid confusion among pediatric healthcare providers, we recommend using a consistent definition of hypotension by all professional groups developing guidelines for children. This consistent definition of hypotension, however, should not represent the target blood pressure goal. Instead, we recommend that the target blood pressure goal should be individually developed based on adequacy of organ perfusion measured by markers of tissue perfusion such as lactate and urine output and considering the etiology of the shock state. For example, epidemiologic studies in trauma patients suggest that a higher blood pressure target is appropriate, but this has not been tested prospectively. We also calculated normal values for MAP to be used as reference values while treating critically ill children. Further research is needed to identify appropriate SBP and MAP treatment goals in populations of critically ill and injured children, such as children with traumatic brain injury, to better determine the optimal therapeutic end point. REFERENCES 1. Hazinkski MF, Zaritsky A, Nadkarni VM, et al: Pediatric Advanced Life Support Provider Manual. Dallas, TX, American Heart Association, 2002 2. Dieckmann RAE, American Academy of Pediatrics: Pediatric Education for Prehospital Providers (PEPP). Sudbury, MA, Jones and Bartlett, 2000 3. Gausche-Hill MFS, Yamamoto LG: Advanced Pediatric Life Support: The Pediatric Emergency Medicine Resource. Fourth Edition. Sudbury, MA, Jones and Bartlett, 2004 4. Pigula FA, Wald SL, Shackford SR, et al: The effect of hypotension and hypoxia on children with severe head injuries. J Pediatr Surg 1993; 28:310 –314 5. Kokoska ER, Smith GS, Pittman T, et al: 143 6. 7. 8. 9. 10. 11. 12. 13. 14. 144 Early hypotension worsens neurological outcome in pediatric patients with moderately severe head trauma. J Pediatr Surg 1998; 33:333–338 MacLeod J, Lynn M, McKenney MG, et al: Predictors of mortality in trauma patients. Am Surg 2004; 70:805– 810 Shapiro NI, Kociszewski C, Harrison T, et al: Isolated prehospital hypotension after traumatic injuries: A predictor of mortality? J Emerg Med 2003; 25:175–179 Michaud LJ, Rivara FP, Grady MS, et al: Predictors of survival and severity of disability after severe brain injury in children. Neurosurgery 1992; 31:254 –264 Levin HS, Aldrich EF, Saydjari C, et al: Severe head injury in children: Experience of the Traumatic Coma Data Bank. Neurosurgery 1992; 31:435– 443 Luerssen TG, Klauber MR, Marshall LF: Outcome from head injury related to patient’s age. A longitudinal prospective study of adult and pediatric head injury. J Neurosurg 1988; 68:409 – 416 Jones AE, Aborn LS, Kline JA: Severity of emergency department hypotension predicts adverse hospital outcome. Shock 2004; 22: 410 – 414 Report of the Second Task Force on Blood Pressure Control in Children–1987. Task Force on Blood Pressure Control in Children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics 1987; 79:1–25 Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: A working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics 1996; 98:649 – 658 Goldstein B, Giroir B, Randolph A: Interna- 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. tional pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6:2– 8 Ince C, Sinaasappel M: Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 1999; 27:1369 –1377 Desjars P, Pinaud M, Potel G, et al: A reappraisal of norepinephrine therapy in human septic shock. Crit Care Med 1987; 15: 134 –137 LeDoux D, Astiz ME, Carpati CM, et al: Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med 2000; 28:2729 –2732 Rivers E, Nguyen B, Havstad S, et al: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345:1368 –1377 Dellinger RP: Cardiovascular management of septic shock. Crit Care Med 2003; 31: 946 –955 Redl-Wenzl EM, Armbruster C, Edelmann G, et al: The effects of norepinephrine on hemodynamics and renal function in severe septic shock states. Intensive Care Med 1993; 19: 151–154 Carcillo JA, Fields AI: Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 2002; 30:1365–1378 Han YY, Carcillo JA, Dragotta MA, et al: Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics 2003; 112: 793–799 Parker MM, Hazelzet JA, Carcillo JA: Pediatric considerations. Crit Care Med 2004; 32(11 Suppl):S591–S594 Emery EF, Greenough A, Yuksel B: Effect of gender on blood pressure levels of very low birthweight infants in the first 48 hours of life. Early Hum Dev 1993; 31:209 –216 25. Versmold HT, Kitterman JA, Phibbs RH, et al: Aortic blood pressure during the first 12 hours of life in infants with birth weight 610 to 4,220 grams. Pediatrics 1981; 67:607– 613 26. Watkins AM, West CR, Cooke RW: Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 1989; 19:103–110 27. Rogers MC, Helfaer MA: Handbook of Pediatric Intensive Care. Third Edition. Baltimore, Williams & Wilkins, 1999 28. Rogers MC, Nichols DG: Textbook of Pediatric Intensive Care. Third Edition. Baltimore, Williams & Wilkins, 1996 29. Fuhrman BP, Zimmerman JJ: Pediatric Critical Care. Second Edition. St. Louis, MO, Mosby, 1998 30. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114(2 Suppl 4th Report):555–576 31. Cummins RO, American Heart Association: Advanced Cardiac Life Support. Dallas, TX, American Heart Association, 1997 32. Leteurtre S, Martinot A, Duhamel A, et al: Validation of the paediatric logistic organ dysfunction (PELOD) score: Prospective, observational, multicentre study. Lancet 2003; 362:192–197 33. Dark P, Woodford M, Vail A, et al: Systolic hypertension and the response to blunt trauma in infants and children. Resuscitation 2002; 54:245–253 34. Vavilala MS, Bowen A, Lam AM, et al: Blood pressure and outcome after severe pediatric traumatic brain injury. J Trauma 2003; 55: 1039 –1044 35. White JR, Farukhi Z, Bull C, et al: Predictors of outcome in severely head-injured children. Crit Care Med 2001; 29:534 –540 36. Robertson CS: Management of cerebral perfusion pressure after traumatic brain injury. Anesthesiology 2001; 95:1513–1517 Pediatr Crit Care Med 2007 Vol. 8, No. 2