Chapter 3
advertisement
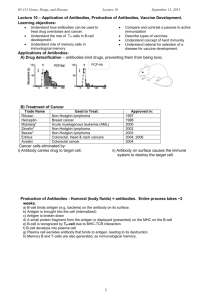
Chapter 3 Immunity and how vaccines work A Practical Guide to Immunisation 3.1 Objectives: • • • • • • • • To understand and describe the immune system and how vaccines produce immunity To understand the differences between Passive and Active immunity To understand what Antigens and Antibodies are and how they contribute to immunity To understand how vaccines work To understand the importance of different components of vaccines including suspension fluids, preservatives, stabilisers and antimicrobial agents and thiomersal To understand the differences between inactivated vaccines, toxoids and live vaccines To understand what is meant by the term “vaccine failure” To understand why it is necessary to leave time intervals between vaccinations. 3.2 The immune system Immunity can be defined as the ability of the human body to protect itself from infectious disease. The body has its own specific mechanism for protection e.g. physical barriers (skin and mucous membranes), chemical barriers (gastric and digestive enzymes) and immunological barriers (phagocytes, macrophages and complement system) that help to protect us. The characteristic feature of these mechanisms of protection is that no “memory” of protection exists afterwards. 3.3 Active and Passive Immunity Immunity to illness can be acquired through passive or active mechanisms. Passive immunity is the mechanism whereby protection is provided by the transfer of antibodies from people who have immunity to those that do not. The most common form of passive immunity is the transfer of antibodies from mother to baby across the placenta. Other less common forms of passive immunity include transfer of antibodies through transfusion of blood or blood products including immunoglobulin. This protection is temporary. Active immunity can be acquired through contact with a disease and the development of antibodies to that disease or through vaccination. Vaccines are designed to provide immunity similar to natural disease but without the side effects or complications of the disease. Vaccination helps to stimulate and strengthen the immune system and generate long lasting immunity. Active immunisation involves the administration of all, or part of, a micro-organism or a modified product of that micro-organism (e.g. toxoid, purified antigen, or an antigen produced by genetic engineering) to provoke an immune response in the recipient. Some vaccines provide life long protection against disease, some provide partial protection and some must be re-administered at regular intervals to provide protection. 3.4 What do antibodies contribute to the immune system? Antibodies neutralise toxins, block adhesion/cell entry of the antigen and kill the antigen by producing complement. Different types of antibody are produced at different time periods and by different body systems. Antibodies are antigen specific and cannot cross protect e.g. measles antibody cannot protect against meningococcal disease etc. There are five different types of antibodies namely IgM, IgG, IgA, IgD and IgE antibodies, of which IgM and IgG are the most important (Figure 3.1). Page 22 Chapter 3: Immunity and how vaccines work A Practical Guide to Immunisation Figure 3.1: Immune Response following exposure to antigen. The primary immune response develops in the weeks following exposure to an antigen and is mainly IgM antibody. It is made by cells in lymph nodes, spleen and bone marrow and circulates in the blood and lymphatic system. IgM antibodies activate the complement system. IgM antibodies have a short half-life (5 days). The secondary immune response is faster and more powerful and is predominantly IgG antibody. It is made in lymph nodes, spleen and bone marrow. The IgG antibody is smaller than IgM and its half life is about 3 weeks. It also passes through the placenta from mother to baby giving the baby antibodies to which the mother is immune. Active immunity can be divided into antibody and cell mediated responses. 3.4.1 Antibody mediated immunity Antibody mediated responses are produced by B lymphocytes (B cells) and plasma cells. When a B cell encounters an antigen that it recognises, the B cell is stimulated to proliferate and produce large numbers of lymphocytes, secreting antibody to the antigen. Replication and differentiation of B cells into plasma cells is regulated by contact with the antigen and by interactions with T cells, macrophages and complement. The antibodies produce immunity through neutralising toxins, blocking adhesion and cell entry by organisms, neutralising and preventing viral replication or complement-mediated killing. 3.4.2 Cell mediated immunity Cell mediated immunity is controlled by a subset of lymphocytes called T lymphocytes or T cells. T cells stimulate B cells to produce antibodies and play an inhibitory role and control the level and quality of the immune response. Cytotoxic T cells recognise and destroy infected cells and activate phagocytes to destroy pathogens that they have taken up. 3.5 How do vaccines work? Vaccines work by inducing active immunity and by providing immunological memory. Immunological memory allows the immune system to recognise and respond rapidly to natural infection when exposed at a later stage and to prevent or modify the effect of that disease. Antibodies can be detected in blood or serum but, even if undetectable, memory usually still exists. Vaccines are made from inactivated (killed) or attenuated live organisms, secreted products, recombinant components or components of cell walls. Vaccines must contain sufficient antigenic mass to stimulate a desired response. The components of vaccines are listed in Table 3.1. Chapter 3: Immunity and how vaccines work Page 23 A Practical Guide to Immunisation Table 3.1: Types of Vaccines Vaccine Name Type BCG Live attenuated Diphtheria Toxoid Tetanus Toxoid Pertussis Inactivated bacteria Polio Inactivated virus MMR Live attenuated Meningococcal Conjugate Hib Conjugate Hepatitis B Conjugate Pneumococcal Conjugate 3.6 Vaccine components Other components of vaccines include: 3.6.1 Conjugating agents There are carrier proteins which when combined with antigens enhance the type and magnitude of the immune response. Examples include Haemophilus influenzae B (Hib) and Meningococcal C vaccine. 3.6.2 Suspension fluid The suspension fluid could simply be water for injection or saline solution. It may also be a tissueculture mixture containing proteins or other components from which the vaccine is produced (e.g. egg antigen, gelatine or cell culture derived antigens). 3.6.3Preservatives, stabilisers and antimicrobial agents. Trace amounts of preservatives and antimicrobial agents (e.g.neomycin or streptomycin sulphate) may be included in some vaccines and immunoglobulin products to maintain stability. An allergic reaction can occur if the recipient is sensitive to one or more of these additives. 3.6.4 Thiomersal Thiomersal (also known as thimerosal) is a mercury-containing compound added to some vaccines to prevent bacterial and fungal growth. Thiomersal has been used since the 1930s in the manufacture of some vaccines and other medical products. Thiomersal is also used as an inactivating agent in the very early stages of production of some killed vaccines. Only minuscule amounts of thiomersal used for this purpose remain after the manufacture is completed. Recently there was concern that thiomersal could be associated with neurological problems. There is now strong evidence to show that thiomersal in vaccines does not cause adverse neurological effects. As part of a global goal to reduce exposure to mercury from avoidable sources in general, European and American regulators recommended in 1999 that vaccine manufacturers phase out use of thiomersal wherever possible as a precautionary measure. Manufacturers are actively developing research programmes to eliminate, substitute or reduce thiomersal in vaccines, following the European recommendations. Further information is available on the National Immunisation Office website www.immunisation.ie. Page 24 Chapter 3: Immunity and how vaccines work A Practical Guide to Immunisation 3.6.5 Adjuvants An aluminium salt is used in varying concentrations to increase immunogenicity for vaccines containing inactivated micro-organisms or their products. Examples include Hepatitis B vaccine, and diphtheria and tetanus toxoids. 3.7 Live attenuated vaccines Live attenuated vaccines usually are created from the virus or bacterium itself. Viruses and bacteria are weakened (or attenuated) by growing them over and over again in a laboratory under nourishing conditions called cell culture. The process of growing a virus repeatedly serves to lessen the disease-causing ability of the virus. Vaccines are made from viruses whose disease-causing ability has been weakened from multiple passages. Live attenuated viral vaccines produce a long lasting immune response after one or two doses. The live organism grows in the body and stimulates the immune system to react as it does to natural infection. As the vaccine is an attenuated live vaccine it does not cause the disease itself but can cause a mild form of the disease (e.g. fever and rash 6-10 days after MMR). 3.8 Inactivated vaccines and toxoids Inactivated vaccines and toxoids injected into a person who does not have prior exposure to the antigen produce a primary antibody response. IgM antibody is produced initially followed by IgG antibody. Two or more injections are usually required initially with the need for booster doses at longer time intervals. Even if antibody levels are undetectable immunological memory will persist and will be called upon in response to antigen exposure. Inactivated vaccines cannot cause the disease that they have been designed to protect against. Polysaccharide vaccines are not as effective in stimulating the immune system as toxoids. This means that the polysaccharide vaccines do not provide life long immunity and the response in children can be poor. The vaccines can be made more effective by conjugation as described above. Some inactivated vaccines contain adjuvants such as aluminium phosphate or aluminium hydroxide to enhance the immune response. 3.9 What is vaccine failure? When a person who has been fully vaccinated develops the disease against which they have been vaccinated, it is referred to as vaccine failure. In the vast majority of cases, however, it is not the vaccine that has failed, but an inadequate immune response to the vaccine has occurred. Vaccine failure can be primary or secondary Primary vaccine failure occurs when the recipient does not produce enough antibodies when first vaccinated. Infection can therefore occur at any time post vaccination. This can occur in about 10% of those who receive the MMR vaccine. Secondary vaccine failure occurs when an adequate number of antibodies are produced immediately after the vaccination, but the levels fall over time. The incidence of secondary vaccine Chapter 3: Immunity and how vaccines work Page 25 A Practical Guide to Immunisation failure therefore increases with time after initial vaccination and booster doses are required. This is a feature of many of the inactivated vaccines. 3.10 Why it is necessary to leave time intervals between vaccinations? Gaps between deliveries of vaccines are needed to allow the immune response to develop. If another live vaccine is given whilst the immune system is making a primary immune response, the activation of the immune system may neutralise the second live vaccine so that it does not work. A gap of four weeks is therefore required between the administration of any two live vaccines. If immunoglobulin has been given, it is necessary to leave a gap of three months before a live vaccine can be administered. The antibodies in the immunoglobulin could neutralise any live vaccines. 3.11 Useful resources American Academy of Paediatrics. 2006 Report of the Committee on Infectious Diseases – The Red Book http://aapredbook.aappublications.org/ Department of Health UK. November 2006. Immunisation against infectious disease. http://www. dh.gov.uk/en/Policyandguidance/Healthandsocialcaretopics/Greenbook/DH_4097254 Health Protection Surveillance Centre, Ireland. www.hpsc.ie Irish Pharmaceutical Healthcare Association Medical Compendium. http://www.medicines.ie. Irish Medicines Board. http://www.imb.ie National Immunisation Office. Health Service Executive, Ireland. http://www.immunisation.ie. Royal College of Physicians of Ireland. Immunisation Guidelines for Ireland. Available at www.hpsc.ie Page 26 Chapter 3: Immunity and how vaccines work