nursing care related to the gastrointestinal and urinary
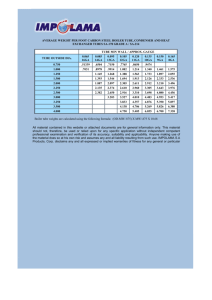
advertisement

U.S. ARMY MEDICAL DEPARTMENT CENTER AND SCHOOL FORT SAM HOUSTON, TEXAS 78234-6100 NURSING CARE RELATED TO THE GASTROINTESTINAL AND URINARY SYSTEMS SUBCOURSE MD0918 EDITION 100 DEVELOPMENT This subcourse is approved for resident and correspondence course instruction. It reflects the current thought of the Academy of Health Sciences and conforms to printed Department of the Army doctrine as closely as currently possible. Development and progress render such doctrine continuously subject to change. ADMINISTRATION For comments or questions regarding enrollment, student records, or shipments, contact the Nonresident Instruction Section at DSN 471-5877, commercial (210) 2215877, toll-free 1-800-344-2380; fax: 210-221-4012 or DSN 471-4012, e-mail accp@amedd.army.mil, or write to: COMMANDER AMEDDC&S ATTN MCCS HSN 2105 11TH STREET SUITE 4192 FORT SAM HOUSTON TX 78234-5064 Approved students whose enrollments remain in good standing may apply to the Nonresident Instruction Section for subsequent courses by telephone, letter, or e-mail. Be sure your social security number is on all correspondence sent to the Academy of Health Sciences. CLARIFICATION OF TRAINING LITERATURE TERMINOLOGY When used in this publication, words such as "he," "him," "his," and "men" are intended to include both the masculine and feminine genders, unless specifically stated otherwise or when obvious in context. . TABLE OF CONTENTS LESSON PARAGRAPH INTRODUCTION....................................……… 1 NURSING CARE RELATED TO THE GASTROINTESTINAL SYSTEM Section I. Section II. Section III. Section IV. Section V. Section VI. Section VII. Section VIII. Exercises 2 1-1--1-12 1-13--1-19 1-20--1-24 1-25--1-39 1-40--1-48 1-49--1-54 1-55--1-64 1-64--1-76 NURSING CARE RELATED TO THE URINARY SYSTEM Section I. Section II. Section III. Section IV. Exercises MD0918 Anatomy and Physiology…………………….. Nursing Assessment…………………………. Diagnostic Procedures………………………. Gastrointestinal Intubation……………….….. Gastrostomy, Colostomy, Ileostomy….…….. Gastrointestinal Disorders…………………… Hepato-Biliary Disorders…………………….. Diabetes………………………………………. Anatomy and Physiology………………….… Nursing Assessment and Diagnostic Procedures......................……………….…… Catheterization and Drainage………………. Urinary Disorders…………………………….. i 2-1--2-8 2-9--2-14 2-15--2-23 2-24--2-40 SUBCOURSE MD0918 NURSING CARE RELATED TO THE GASTROINTESTINAL AND URINARY SYSTEMS INTRODUCTION A patient is not a passive object on which we perform nursing care procedures. A patient should never be thought of, or discussed, as merely a condition or injury. It is not acceptable to think of, or refer to, your patient as "the gallbladder" or "the fractured hip" or "the bleeding ulcer." A patient is much more than the condition that brought him to the hospital. A patient is a human being, possessing physical and emotional needs and wants. The relationship between the patient and the nursing staff is extremely dynamic and personal. The patient places his trust in the nursing staff and they, in return, must utilize all their knowledge and skills to ensure the patient's well-being and assist in his return to good health and independence. This is accomplished by developing a therapeutic relationship between the patient, his family, and the health care professionals. The nursing paraprofessional relates very closely with the patient and his family by virtue of his participation in providing nursing care and his presence at the bedside. It is often the nursing paraprofessional who makes the initial observation that something is not as it should be. Nursing paraprofessionals who are responsible, educated, and observant are assets to the therapeutic environment necessary for patient recovery. To help foster this therapeutic environment, the nursing paraprofessional must do the following: Assess the patient's ability to express himself. Assess the patient's mechanisms for coping. Assess the patient's level of understanding about his condition and the teaching provided by the health care professionals. Assist the patient to establish a trusting relationship with the health care providers. Utilize the nursing process to provide the best possible care. Continue to pursue his education in order to sustain and enhance professional knowledge and skills. MD0918 ii The purpose of this subcourse is to enhance your knowledge of medical surgical nursing care related to the gastrointestinal and urinary systems and the role of the nursing paraprofessional in providing that care. Subcourse Components: This subcourse consists of two lessons. The lessons are: Lesson 1, Nursing Care Related to the Gastrointestinal System. Lesson 2, Nursing Care Related to the Urinary System. Credit Awarded: To receive credit hours, you must be officially enrolled and complete an examination furnished by the Nonresident Instruction Section at Fort Sam Houston, Texas. Upon successful completion of the examination for this subcourse, you will be awarded 12 credit hours. Procedures for Subcourse Completion: It is necessary for you to have a working knowledge of medical terminology to fully understand this text. If you do not, complete MED010, Basic Medical Terminology, before you attempt this subcourse. It is suggested that you also have a medical dictionary available. Additionally, it is necessary for you to have a basic knowledge of general nursing procedures in order to fully understand this text. If you do not, it is best to complete MED911, Nursing Fundamentals I (previously entitled General Nursing Procedures), and MED912, Nursing Fundamentals II, before attempting this subcourse. You can enroll by going to the web site http://atrrs.army.mil and enrolling under "Self Development" (School Code 555). A listing of correspondence courses and subcourses available through the Nonresident Instruction Section is found in Chapter 4 of DA Pamphlet 350-59, Army Correspondence Course Program Catalog. The DA PAM is available at the following website: http://www.usapa.army.mil/pdffiles/p350-59.pdf. MD0918 iii LESSON ASSIGNMENT LESSON 1 Nursing Care Related to the Gastrointestinal System. TEXT ASSIGNMENT Paragraphs 1-1 through 1-76. LESSON OBJECTIVES After completing this lesson, you should be able to: 1-1. Describe the processes of digestion. 1-2. List the organs of the digestive system, to include the accessory organs. 1-3. Describe the function of each digestive organ. 1-4. Describe the nursing assessment of a gastrointestinal patient. 1-5. Identify the abdominal quadrants. 1-6. Describe the nursing actions to be taken when performing a physical examination of the abdomen. 1-7. State the nursing implications associated with an X-ray that utilizes contrast medium. 1-8. List the nursing implications associated with an endoscopy. 1-9. State the purposes for gastrointestinal intubation. 1-10. Differentiate between the types of N/G tubes used. 1-11. List the steps for inserting a nasogastric tube. 1-12. List the nursing implications associated with care of a patient with diabetes. 1-13. State the nursing action taken for obstruction of a nasogastric tube. 1-14. Define the relationship between glucose and insulin. 1-15. List the steps for irrigation of a nasogastric tube. MD0918 1-1 1-16. List the steps for administering a gavage feeding. 1-17. State the purposes for gastric lavage. 1-18. List the steps for performing gastric lavage. 1-19 State the procedure for changing a gastrostomy dressing. 1-20. List the causes, symptoms, and nursing management of diabetic ketoacidosis. 1-21. Describe the anatomical and physiological differences between colostomy and ileostomy. 1-22. List the steps for performing a colostomy irrigation. 1-23. List the causes, symptoms, and nursing management of "insulin shock." 1-24. State the nursing care objectives for a patient with gastrointestinal ulcers. 1-25. List the nursing implications associated with appendicitis. 1-26. List the nursing implications associated with intestinal obstruction. 1-27. Describe the symptoms of intestinal obstruction. 1-28. State the guidelines used for accuracy when measuring abdominal girth. 1-29. Differentiate between diverticulosis and diverticulitis. 1-30. Differentiate between the types of hepatitis. 1-31. Explain the relationship between cirrhosis, portal hypertension, and esophageal varices. 1-32. List the nursing implications related to cirrhosis. SUGGESTION MD0918 After studying the assignment, complete the exercises at the end of this lesson. These exercises will help you to achieve the lesson objectives. 1-2 LESSON 1 NURSING CARE RELATED TO THE GASTROINTESTINAL SYSTEM Section I. ANATOMY AND PHYSIOLOGY 1-1. DIGESTION a. The intake of food is necessary for life because the foods we eat provide essential nutrients. Nutrients are substances necessary for growth and repair of tissue and for maintenance of normal body functioning. A "nutritionally adequate" diet will contain all the essential nutritive substances in the amounts and proportions required to maintain life and health. These essential nutrients are carbohydrates, proteins, fats, minerals, vitamins, and water. (1) Carbohydrates, proteins, and fats are the basic fuels for cellular activity. (2) Minerals are inorganic substances that help to regulate body processes. Some work with the enzymes, some act as catalysts, and some work within the buffer systems. (3) Vitamins are organic nutrients that function to regulate physiological processes such as growth and metabolism. (4) Water is an important nutrient with many functions. It acts as a coolant, a lubricant, a suspending medium, and as a reactant in chemical processes. b. Since the food we eat cannot be used for fuel in its consumed form, it must be broken down (digested) to the molecular level. In molecular form, the chemicals can be transported and absorbed through the cell membranes for utilization by the body cells. This process of digestion consists of both mechanical breakdown and chemical breakdown. (1) defecation. Mechanical digestion includes chewing, swallowing, peristalsis, and (2) Chemical digestion is the enzymatic breakdown of the food- stuffs into chemically simple molecules that can be absorbed and utilized by the cells. c. Carbohydrates, also known as sugars and starches, are organic compounds that provide the most ready source of energy to the body. Carbohydrates are broken down to their simplest form, called a monosaccharide, to be absorbed from the digestive tract. Carbohydrates consist of three major groups: monosaccharides, disaccharides, and polysaccharides. MD0918 1-3 (1) Monosaccharides are called the "simple sugars" because they cannot be further broken down into simpler molecules. The monosaccharide glucose is the major carbohydrate used for fuel by the cells. (2) Disaccharides are two monosaccharides that are joined chemically. (3) Polysaccharides are a group of five or more monosaccharides that are joined chemically. d. Proteins are complex molecules of chemically linked chains of amino acids. Proteins are essential components of all cells in the body and have many functions within the human body. Some proteins function as enzymes, some as antibodies, and some are used for nutrition. The diet must contain sufficient protein to replace the protein broken down during normal body functions and growth. Proteins are broken down into their constituent amino acids to be absorbed from the digestive tract. These amino acids are transported to the body's cells, where they are recombined to form (synthesize) new protein molecules. (1) All proteins are synthesized from combinations of the naturally occurring amino acids. A great variety of proteins are made possible with only a limited number of amino acids because a different protein is created with each variation in the number and arrangement of the amino acids. This can be likened to the alphabet and words. The letters (amino acids) can be combined in a multitude of ways to form different words (proteins). (2) Ten of these amino acids are termed "essential" amino acids. This is due to the fact that these amino acids cannot be synthesized within the body, but must be consumed as food for growth and survival. Other amino acids can be synthesized within the body from other molecules present within the cells. A food protein that contains all the essential amino acids is referred to as a "complete" protein. e. Fat is primarily an energy source. In addition to its value as an energy source, fat serves as a carrier for the fat-soluble vitamins (A, D, E, and K) and adds flavor to the diet. Fats are emulsified in the intestine and split into fatty acids and glycerol for absorption. If not used as immediate energy sources, fatty acids are resynthesized into body fat and stored in the many fat cells of the body for future use. 1-2. METABOLISM Metabolism refers to all the chemical activity within the body. All chemical reactions either release or require energy. Metabolism has two phases: an energygenerating process called catabolism and an energy-requiring process called anabolism. Both processes occur simultaneously within the cells, but they are regulated independently. For this reason, the body's metabolism can be thought of as energy balancing. MD0918 1-4 a. Catabolism is a degenerative, energy-generating process. Complex molecules of proteins, carbohydrates, and fats are systematically broken down into simpler, smaller molecules by the body's cells. The bonding energies that hold the atoms of a complex molecule together are released as the molecule is broken down. Much of this energy released by catabolism is captured and stored by the cells in the form of a chemical molecule known as ATP. Digestion is a catabolic process because the breakdown of the food releases energy. b. Anabolism is a building, energy-requiring process. New, more complex molecules are synthesized from simple molecules. These larger molecules form the body's structural and functional components. This synthesis requires the expenditure of the cellular energy generated by the cell's catabolic activities. 1-3. THE DIGESTIVE SYSTEM a. The digestive system is made up of the alimentary canal (food passageway) and the accessory organs of digestion. The products of the accessory organs help to prepare food for its absorption and use by the tissues of the body. The main functions of the digestive system are: (1) To ingest and carry food so that digestion can occur. (2) To eliminate unused waste material. b. The alimentary canal is approximately 28 feet long in the adult and extends from the lips to the anus. It is composed of the organs listed below. (1) Mouth (and associated glands). (2) Pharynx. (3) Esophagus. (4) Stomach. (5) Small intestine (and associated glands). (6) Large intestine. (7) Rectum. (8) Anal canal and anus. c. Refer to figure 1-1, an illustration of the digestive system, as you continue to read about the structure and function of each component. MD0918 1-5 Figure 1-1. The digestive system. MD0918 1-6 1-4. THE MOUTH The mouth, or oral cavity, is the beginning of the digestive tract. Here food taken into the body is broken into small particles and mixed with saliva so that it can be swallowed. a. Teeth. (1) A person develops two sets of teeth during his life, a deciduous (or temporary) set and a permanent set. There are 20 deciduous teeth and these erupt during the first 3 years of life. They are replaced during the period between the 6th and 14th years by permanent teeth. There are 32 permanent teeth in the normal mouth: 4 incisors, 2 cuspids, 4 bicuspids, and 6 molars in each jaw. Each tooth is divided into two main parts: the crown, that part which is visible above the gums; and the root, that part which is not visible and which is embedded in the bony structure of the jaw. The crown of the tooth is protected by enamel. Tooth decay is from the outside in; once the protective enamel is broken, microorganisms attack the less resistant parts of the tooth. (2) The primary function of the teeth is to chew or masticate food. The teeth also help modify sound produced by the larynx to form words. b. Salivary Glands. These glands are the first accessory organs of digestion. There are three pairs of salivary glands. They secrete saliva into the mouth through small ducts. One pair, the parotid glands, is located at the side of the face below and in front of the ears. The second pair, the submandibular glands, lies on either side of the mandible. The third pair, the sublingual glands, lies just below the mucous membrane in the floor of the mouth. The flow of saliva is begun in several ways. Placing food in the mouth affects the nerve endings there. These nerve endings stimulate cells of the glands to excrete a small amount of thick fluid. The sight, thought, or smell of food also activates the brain and induces a large flow of saliva. About 1,500 ml. of saliva are secreted daily. The saliva moistens the food, which makes chewing easier. It lubricates the food mass to aid in the act of swallowing. Saliva contains two enzymes, chemical ferments, which change foods into simpler elements. The enzymes act upon starches and break them down into sugars. c. Tongue. The tongue is a muscular organ attached at the back of the mouth and projecting upward into the oral cavity. It is utilized for taste, speech, mastication, salivation, and swallowing. d. Taste Buds. Located on the tongue and at the back of the mouth are special clumps of cells known as taste buds. Taste buds are sensitive to substances that are sweet, sour, bitter, and salty. MD0918 1-7 1-5. PHARYNX The pharynx is a musculomembranous passage that leads from the nose and mouth to the esophagus. The passage of food from the pharynx into the esophagus is the second stage of swallowing. When food is being swallowed, the larynx is closed off from the pharynx to keep food from getting into the respiratory tract. 1-6. THE ESOPHAGUS The esophagus is a musculomembranous passage about 10 inches long, lined with a mucous membrane. It leads from the pharynx through the chest to the upper end of the stomach. Its function is to complete the act of swallowing. The involuntary movement of material down the esophagus is carried out by the process known as peristalsis, which is the wavelike action produced by contraction of the muscular wall. This is the method by which food is moved throughout the alimentary canal. 1-7. THE STOMACH The stomach is an elongated pouch-like structure lying just below the diaphragm, with most of it to the left of the midline. It has three divisions: the fundus, the enlarged portion to the left and above the entrance of the esophagus; the body, the central portion; and the pylorus, the lower portions. Circular sphincter muscles that act as valves guard the opening of the stomach. (The cardiac sphincter is at the esophageal opening, and the pyloric sphincter is at the junction of the stomach and the duodenum, the first portion of the small intestine.) The cardiac sphincter prevents stomach contents from reentering the esophagus except when vomiting occurs. In the digestive process, two important functions of the stomach are: a. It acts as a storehouse for food, receiving fairly large amounts, churning it, and breaking it down further for mixing with digestive juices. Semiliquid food is released in small amounts by the pyloric valve into the duodenum, the first part of the small intestine. b. The glands in the stomach lining produce gastric juices (which contain enzymes) and hydrochloric acid. The enzymes in the gastric juice start the digestion of protein foods, milk, and fats. Hydrochloric acid aids enzyme action. The mucous membrane lining the stomach protects the stomach itself from being digested by the strong acid and powerful enzymes. 1-8. SMALL INTESTINE a. The small intestine is a tube about 22 feet long. The intestine is attached to the margin of a thin band of tissue called the mesentery, which is a portion of the peritoneum, the serous membrane lining the abdominal cavity. The mesentery supports the intestine, and the vessels that carry blood to and from the intestine lie within this membrane. The other edge of the mesentery is drawn together like a fan; the gathered MD0918 1-8 margin is attached to the posterior wall of the abdomen. This arrangement permits folding and coiling of the intestine, so this long organ can be packed into a small space. The intestine is divided into three continuous parts: duodenum, jejunum, and ileum. b. Most of the absorption of food takes place in the small intestine. Muscular contraction of the intestinal walls produces the wave-like motion called peristalsis, which propels the contents through the length of the intestines. The walls of the intestines are covered with small, fingerlike projections called villi, which provide a larger surface area for absorption. After food has been digested, it is absorbed into the capillaries of the villi and carried to all parts of the body via the circulatory system. c. The small intestine receives digestive juices from three accessory organs of digestion: the pancreas, liver, and gallbladder (figure 1-2). (1) Pancreas. The pancreas is a long, tapering organ lying behind the stomach. The head of the gland lies in the curve of the small intestine near the pyloric valve. The body of the pancreas extends to the left toward the spleen. The pancreas secretes a juice that acts on all types of food. Two enzymes in pancreatic juice act on proteins. Other enzymes change starches into sugars. Another enzyme changes fats into their simplest forms. The pancreas has another important function, the production of insulin. (2) Liver. The liver is the largest organ in the body. It is located in the upper part of the abdomen with its larger (right) lobe to the right of the midline. It is just under the diaphragm and above the lower end of the stomach. The liver has several important functions. One is the secretion of bile, which is stored in the gallbladder and discharged into the small intestine when digestion is in process. The bile contains no enzymes, but it breaks up the fat particles so that enzymes can act faster. The liver performs other important functions. It is a storehouse for the sugar of the body (glycogen) and for iron and vitamin B. It plays a part in the destruction of bacteria and worn out red blood cells. Many chemicals such as poisons or medicines are detoxified by the liver; others are excreted by the liver through bile ducts. The liver manufactures part of the proteins of blood plasma. The blood flow in the liver is of special importance. All the blood returning from the spleen, stomach, intestines, and pancreas is detoured through the liver by the portal vein in the portal circulation. Blood drains from the liver by hepatic veins that join the inferior vena cava. (3) Gallbladder. The gallbladder is a dark green sac, shaped like a blackjack and lodged in a hollow on the underside of the liver. Its ducts join with the duct of the liver to conduct bile to the upper end of the small intestine. The main function of the gallbladder is the storage and concentration of the bile when it is not needed for digestion. MD0918 1-9 1-9. LARGE INTESTINE (COLON) a. The large intestine is about 5 feet long. The cecum, located on the lower right side of the abdomen, is the first portion of the large intestine into which food is emptied from the small intestine. The appendix extends from the lower portion of the cecum and is a blind sac. Although the appendix usually is found lying just below the cecum, by virtue of its free end it can extend in several different directions, depending upon its mobility. Figure 1-2. Stomach, duodenum, and the accessory organs. b. The colon extends along the right side of the abdomen from the cecum up to the region of the liver (ascending colon). There the colon bends (hepatic flexure) and is continued across the upper portion of the abdomen (transverse colon) to the spleen. The colon bends again (splenic flexure) and goes down the left side of the abdomen (descending colon). The last portion makes an S curve (sigmoid) toward the center and posterior of the abdomen and ends in the rectum. c. The main function of the large intestine is the recovery of water and electrolytes from the mass of undigested food it receives from the small intestine. As this mass passes through the colon, water is absorbed and returned to the tissues. Waste materials, or feces, become more solid as they are pushed along by peristaltic movements. Constipation is caused by delay in movement of intestinal contents and MD0918 1-10 removal of too much water from them. Diarrhea results when movement of the intestinal contents is so rapid that not enough water is removed. 1-10. THE RECTUM AND ANUS The rectum is about 5 inches long and follows the curve of the sacrum and coccyx until it bends back into the short anal canal. The anus is the external opening at the lower end of the digestive system. It is kept closed by a strong sphincter muscle. The rectum receives feces and periodically expels this material through the anus. This elimination of refuse is called defecation. 1-11. DEFECATION The passage of feces is called defecation. It is begun voluntarily by contraction of the abdominal muscles. At the same time, the sphincter muscles of the anus relax, and there is a peristaltic contraction wave of the colon and rectum. Feces are expelled as a result of all these actions. Feces consist of undigested food residue, secretions from the digestive glands, bile, mucus, and millions of bacteria. Mucus is derived from the many mucous glands that pour secretions into the intestine. Bacteria are especially numerous in the large intestine. They act upon food material, causing putrefaction of proteins and fermentation of carbohydrates. Although the bacteria normally in the large intestine serve a useful purpose internally, they are contaminants outside the intestine. 1-12. TIME REQUIRED FOR DIGESTION Within a few minutes after a meal reaches the stomach, it begins to pass through the lower valve of the stomach. After the first hour the stomach is half-empty, and at the end of the sixth hour none of the meal is present in the stomach. The meal goes through the small intestine, and the first part of it reaches the cecum in 20 minutes to 2 hours. At the end of the sixth hour, most of it should have passed into the colon; in 12 hours, all should be in the colon. Twenty-four hours from the time when food is eaten, the meal should reach the rectum. However, part of a meal may be defecated at one time and the rest at another. Section II. NURSING ASSESSMENT 1-13. GENERAL The vague nature of many gastrointestinal symptoms makes diagnosis of GI problems quite difficult. A complete patient history and an adequate physical examination are necessary in order to gather as much information as possible. Although this is routinely done by the admitting physician, a nursing assessment must be completed as well. Patients will quite often neglect to mention facts, which they consider insignificant, unimportant, or irrelevant. A detailed nursing interview may elicit previously unmentioned, valuable information. MD0918 1-11 1-14. THE NURSING HISTORY a. When obtaining the nursing history of a gastrointestinal patient, a detailed interview should be conducted. Nursing personnel should question the patient about his dietary habits, his bowel habits, and his GI complaints (signs and symptoms). b. Obtaining a history of dietary habits will provide valuable information. Question the patient about the following: (1) The number of meals ate per day. (2) Meal times. (3) Food restrictions or special diets followed. (4) Changes in appetite. Increased? Decreased? No appetite? (5) What foods, if any, have been eliminated from the diet? Why? (6) What foods are not well tolerated? (7) Alterations in taste. (8) Medications used. Dosage and frequency. c. Information about bowel patterns, especially a change in bowel patterns, can provide clues that will aid in the diagnosis of the problem. Question the patient about the following: (1) Frequency of bowel movements. (2) Use of laxatives and/or enemas. (3) Changes in bowel habits. (4) Stool Description. (a) Constipation. (b) Diarrhea. MD0918 (c) Blood in stool. (d) Mucous in stool. 1-12 (e) Black, tarry stools. (f) Pale or clay colored stools. (g) Foul smelling stools. (h) Pain with stool. d. Ask the patient to describe any complaints not yet discussed in the interview. For example. (1) Nausea. Frequency? Duration? Associated with meals? Relieved by? (2) Vomiting. Frequency? Character of emesis? Relieved by? (3) Heartburn/indigestion. Frequency? Duration? Associated with specific foods? Relieved by? (4) Relieved by? Gas (belching and flatus). Frequency? Associated with specific foods? (5) Pain. Location? Frequency? Duration? Character of the pain? (6) Weight loss. How much? In what time period? 1-15. PHYSICAL ASSESSMENT a. Perform a brief, general head-to-toe visual inspection of the patient. Are height and weight within normal range for the patient's age and body type? b. Observe the skin for the following: MD0918 (1) Color (pale, gray, ruddy, jaundiced). (2) Bruises. (3) Rashes. (4) Lesions. (5) Turgor and moisture content. (6) Edema. 1-13 c. Examine the mouth and throat. (1) Look at the lips, tongue, and mucous membranes, noting abnormalities such as cuts, sores, or discoloration’s. (2) Observe the condition of the teeth. Note any discolored, cracked, chipped, loose, or missing teeth. (3) Observe the gums. Are they healthy and pink? Note the patient's breath for unusual odors (fruity, foul, alcohol, and so forth). 1-16. EXAMINATION OF THE ABDOMEN a. Physical examination of the abdomen involves visual inspection, auscultation, and palpation. It is best to perform this examination while the patient is resting in a supine position, knees slightly flexed to relax the abdominal muscles. b. In order to facilitate the referencing of location, the abdomen is viewed as four quadrants or nine regions. The quadrant division is the most commonly used by nursing personnel. Refer to figure 1-3. The abdomen is divided by a vertical midline and a horizontal line through the navel. Note the organs located in each quadrant. Figure 1-4 illustrates the regional method of division. Again, note the organs underlying each region. 1-17. VISUAL EXAMINATION Begin the abdominal examination by visually inspecting the abdomen. Observe the following: a. Color. Pale? Jaundiced? Ruddy? b. Pigmentation. Even? Note blotches or lines of pigmentation. c. Contour. Symmetrical? Flat? Rounded? Sunken? Distended? d. Presence of: Petechiae? Scars? Rash? Visible blood vessels? e. Hair growth patterns. MD0918 1-14 Figure 1-3. Abdominal quadrants. MD0918 1-15 Figure 1-4. Abdominal regions. MD0918 1-16 1-18. AUSCULTATION Next, auscultate the abdomen. Move the stethoscope in a symmetrical pattern, listening in all four quadrants. a. Listen for bowel sounds. The best location is below and to the right of the umbilicus. b. Describe the sounds heard according to location, frequency, and character of the sound. c. Abnormalities include absent bowel sounds and the peristaltic rush of a hyperactive bowel. 1-19. PALPATION After auscultation, palpate the abdomen. Palpation is used to detect muscle guarding, tenderness, and masses. Gently palpate the abdomen, moving in a symmetrical pattern and covering all four quadrants. Record any of the following findings, noting the location. a. Rigidity or Guarding. This is the inability to relax the abdominal muscles. (Rigidity may be caused by nervousness or fear. Encourage the patient to breathe deeply and regularly to promote relaxation.) b. Pain or Tenderness. Ask the patient to describe the pain if palpation elicits a painful or tender area. c. Rebound Pain. This is pain felt upon release of pressure, as opposed to application of pressure. d. Masses. Organs can be palpated for size and contour by a trained examiner. Additionally, masses and irregularities in and around the abdominal organs may be detected. Section III. DIAGNOSTIC PROCEDURES 1-20. RADIOLOGIC a. General. The digestive tract can be outlined by x-rays by utilizing the administration of a contrast medium. The contrast medium is swallowed by the patient in order to visualize the upper GI tract. These procedures are referred to as "barium swallow," "upper GI," or "small bowel follow-through." To visualize the lower GI tract, the contrast medium is instilled rectally. This procedure is called a "barium enema." MD0918 1-17 b. Pre-Procedural Nursing Implications. (1) For upper GI examinations, the patient is normally held NPO after midnight the day before the exam in order to empty the upper GI tract. Additionally, gum chewing and smoking should be discouraged the morning of the exam, as this stimulates gastric action. (2) For lower GI tract examinations, the patient's large intestine must be free of stool. This is normally accomplished through the use of laxatives and cleansing enemas. The patient is held NPO after midnight the day before the exam. (3) The patient must be educated about the procedure, the significance of the preparation, and any significant post-procedural sequelae. (4) Many procedures require that the patient sign a permit. Check with your local military treatment facility (MTF) standard operating procedure (SOP). c. Post-Procedural Nursing Implications. (1) Many patients experience constipation as a side effect of the contrast medium. If so, mineral oil or a laxative may be required to relieve constipation. (2) Observe the patient for any signs of abdominal or rectal discomfort. Check vital signs in accordance with (IAW) the ward SOP. (3) Resume diet and medications as directed by ward SOP. 1-21. GASTRIC ANALYSIS a. General. Examination of gastric contents and gastric juice provides information used in diagnosis. For example, the following may be determined: (1) The presence, amount, or absence of hydrochloric acid. (2) The presence of cancer cells. (3) The types and amounts of enzymes present. b. Pre-Procedural Nursing Implications. (1) The patient must be educated about the procedure, the significance of the preparation, and any significant post-procedural sequelae. (2) Many procedures require that the patient sign a permit. Check with your local MTF SOP. MD0918 1-18 (3) The physician may require the patient to be nothing by mouth (NPO) for 8-10 hours prior to the test. (4) Gastric analysis requires the insertion of a gastric tube for the purpose of withdrawing a specimen. General care and precautions associated with gastric intubation should be implemented. (Refer to Section IV, Gastrointestinal Intubation.) (5) lab analysis. If ordered by the physician, withdraw the stomach contents and save for (6) The patient should be allowed to rest for 20 to 30 minutes after insertion of the tube before beginning the test. This allows time for the patient's body to return to a rested, basal state. c. Procedural Nursing Implications. (1) Obtain the specimens as directed by the physician or local SOP. (2) Label each specimen with the amount and the time collected in addition to the patient identification. (3) Note and report the presence of the following: (a) Undigested food. (b) Blood. (c) Fecal odor. (4) Assess the patient's tolerance to the procedure by monitoring blood pressure and pulse. (5) Some gastric analysis tests require the administration of drugs to stimulate gastric secretion. It is necessary to have an emergency cart available in these cases. d. Post-Procedural Nursing Implications. MD0918 (1) Monitor the patient's vital signs in accordance with the ward's SOP. (2) Observe for signs of throat irritation secondary to tube placement. (3) Observe for signs of bleeding from the throat or stomach. (4) Resume diet and medication IAW the physician's orders or ward SOP. 1-19 1-22. STOOL EXAM a. General. Stool samples can be examined on the ward and in the laboratory to determine the presence of substances that aid in diagnosis. For example: (1) On the ward, nursing personnel can determine the color, consistency, and amount of stool. The presence of unseen blood (occult) can be determined with a simple test. (2) In the laboratory, tests can be performed to determine the presence of fat, urobilinogen, ova, parasites, bacteria, and other substances. b. Nursing Implications. (1) Nursing personnel should consider the following information when assessing and documenting information related to a patient's bowel movements. (a) Small, dry, hard stools may indicate constipation or fecal impaction. (b) Diarrhea may indicate fecal impaction or fecal mass, or it may be the result of a disease process (such as colitis or diverticulitis) or a bacterial infection (such as dysentery). (2) Nursing personnel should consider the patient's diet when assessing and documenting the character of a patient's stool. (a) Black, tarry stools may be the result of upper GI bleeding, iron supplements, or diet selection (eating black licorice, for example). (b) Reddish colored stools may be the result of bleeding in the lower GI tract or diet selection (eating carrots or beets, for example). 1-23. ENDOSCOPY a. General. Endoscopy is a visual examination of the interior through the use of special instruments called endoscopes. In relation to the digestive system, the term endoscopy is used to describe visual examination of the inside of the GI tract. There are many different types of endoscopes, each designed for a specific use. Generally, the scope consists of a hollow tube with a lighted lens system that permits multi-directional viewing. The scope has a power source and accessories that permit both biopsy and suction. b. Pre-Procedural Nursing Implications. (1) Endoscopic procedures are invasive, and therefore require a formal, signed consent form. MD0918 1-20 (2) The patient must be educated about the procedure, the significance of any preparation, and any post-procedural sequelae. (3) Upper GI endoscopy (esophagoscopy, gastroscopy) requires that the patient be fasting. Sedatives are administered prior to the procedure to relax the patient and facilitate passage of the scope. (4) If the patient wears dentures, have a denture cup available. The physician may require the removal of the dentures prior to oral insertion of the scope. (5) Colon endoscopy (proctoscopy, sigmoidoscopy, and colonoscopy) requires that the bowel be free of stool to enhance visualization. This is normally accomplished with laxatives and cleansing enemas. c. Post-Procedural Nursing Implications. (1) Accidental perforation of the esophagus or colon may occur during endoscopy. If pain or bleeding occur following the procedure, notify the professional nurse. Note the following: (a) Mouth or throat pain. (b) Rectal pain. (c) Abdominal pain. (d) Bleeding from rectum. (e) Bleeding from mouth or throat. (2) Withhold foods, fluids, and p.o. medications until the patient is fully alert and gag reflex has returned. (3) Take vital signs per ward SOP. 1-24. BLOOD TESTS a. General. There are many blood tests that can be used to assist in the identification and measurement of gastrointestinal disorders. For example: (1) Impaired glucose utilization may be detected by abnormal blood glucose levels. Tests used are the fasting blood glucose, post-prandial blood glucose, and glucose tolerance test. MD0918 1-21 (2) Elevated blood levels of cholesterol and triglycerides (fats) are indicative of the need for patient education in dietary habits, allowing for modification before serious disease occurs. (3) Measuring levels of serum enzymes can provide information about the liver, the pancreas, and the patency of the biliary system. Enzymes tested include amylase, lipase, alkaline phosphatase, SGOT, SGPT, and LDH. b. Nursing Implications. (1) It is a nursing responsibility to ensure that the patient has had the appropriate preparation. For example: a special diet or fasting. (2) It is a nursing responsibility to be aware of the normal and abnormal ranges of blood tests, in order to understand the significance of the test results. Section IV. GASTROINTESTINAL INTUBATION 1-25. INTRODUCTION a. Gastric and intestinal intubation is the process of passing a tube through the nose or mouth, through the esophagus, and into the stomach or intestine. A patient is intubated for one or more of the following purposes: (1) To obtain specimens of gastric and intestinal contents for laboratory analysis. (2) To relieve distention of the stomach or intestine, or to keep an obstructed bowel empty. (3) To gavage (tube feed) or to administer drugs to unconscious or extremely weak patients. (4) To lavage (wash out) the stomach prior to surgery, in the case of poisoning, and some types of gastric disorders (bleeding, for example). b. The intubation procedure is usually done by the professional nurse or physician. Under conditions specified by local Department of Nursing policy, the nursing paraprofessional may be authorized to intubate a patient. 1-26. TYPES OF TUBES There are many different tubes with different names for different purposes. The tube required for a specific treatment is ordered by the doctor. Since gastrointestinal tubes are inserted into nonsterile body cavities, sterile technique is usually not required MD0918 1-22 for insertion, although the tubes are sterilized before use. The nursing paraprofessional should be familiar with the general characteristics and uses of each; the different types are usually ordered by name; for example: a. Levin Tube. The Levin tube is flexible with soft walls, and is about four feet long. It is available in sizes 12 French (small) to 18 French (large). It has a rounded tip with multiple holes and is marked by single circular rings at 10cm. (4 inch) intervals, the first being 45cm. (18 inches) from the tip. The Levin tube is used primarily for longcontinued gastric drainage and for gavage feeding. It is also used for diagnostic purposes. Its advantages are that it can be inserted either nasally or orally and that it is firm enough to be passed into an unconscious patient, but flexible enough so there is little danger of producing injury. The chief danger in passing this tube is the possibility of it entering the trachea rather than the esophagus. Care must also be taken to avoid injury to the mucous membrane. b. Gastric Sump Tube. The gastric sump tube (salem, ventrol) is a flexible, double lumen tube. It is routinely used for continuous suction. One lumen is used for aspiration and irrigation. The smaller lumen provides a "vent" to the atmosphere. The advantage of this tube is the presence of the venting lumen, which decreases the occurrence of the tube obstruction. c. Stomach Tube (Ewald). The stomach tube is a large caliber, heavy-walled, fairly stiff tube with a rounded tip and several large holes at one end. A funnel is attached to the other end to facilitate introducing large amounts of fluid into the stomach. It is used only for washing out the stomach (lavage). It is stiff enough to be readily inserted through the mouth into an unconscious or poorly cooperative patient or one with a hypersensitive gag reflex. The chief danger lies in its stiffness, which makes it capable of doing severe damage to the larynx or perforating the esophagus or stomach during insertion; therefore, the procedure should be done only under direct medical supervision. d. Miller-Abbott Tube. The Miller-Abbott tube is a 10-foot long double lumen tube that is equipped with a small balloon near the metal tip at the distal end of the tube. One lumen is used for aspiration and irrigation; the other is used for inflating the balloon. Air, water, or mercury (4 to 5 ml) accomplishes inflation. This intestinal tube is used for small bowel suction. The two openings are independent of each other and are clearly marked. Preferably, this tube is inserted nasally; however, it can be used orally. Position of the tube is determined by aspiration first. X-ray may be used to determine the position in the small intestine. Peristaltic action carries the balloon and the tube through the intestine. When the first mark on the tube is at the patient's nose, suction is started. The doctor inflates the balloon after the tube has passed through the pylorus. e. Cantor Tube. This is a 10-foot long, single-lumen tube used for intestinal decompression. The Cantor tube has a mercury-weighted rubber tab attached to its MD0918 1-23 perforated tip to help carry the tube through the stomach and intestine. The mercury is placed in the bag with a syringe and needle before the tube is inserted nasally by the doctor. f. Sengstaken-Blakemore Tube. Also referred to as a Blakemore tube, this tube is a three lumen, esophageal-gastric balloon tube that is used in the treatment of bleeding esophageal varices. One lumen is used to inflate the esophageal balloon, one lumen is used to inflate the gastric balloon, and the third lumen is used for decompression and irrigation of the stomach. 1-27. NASOGASTRIC INTUBATION Gastric intubation is done to obtain a specimen of stomach contents, to lavage the stomach, to gavage a patient, or to allow for drainage of stomach contents by suction apparatus. Nasogastric intubation is preferred over orogastric intubation. 1-28. PROCEDURE a. Assemble the following clean items on a tray and place the tray on the patient's bedside stand. (1) Nasogastric (NG) tube of size and style specified by physician. (2) Sponge basin containing ice p.r.n. (Use ice to chill a rubber tube, to stiffen it and make insertion easier. Do not chill a plastic tube.) (3) Catheter tip style syringe, 30ml--50ml. (4) Emesis basin. (5) Paper tissues. (6) Water soluble lubricant. (7) Glass of water and straw. (8) Stethoscope. (9) Bath towel or chux pad. (10) Clamp for tubing. (11) Adhesive tape. b. Explain the procedure to the patient. Provide privacy. Position the patient sitting upright in bed or in a chair. MD0918 1-24 c. Place a towel or Chux pad around the patient's neck as a "bib”. d. Place the tissues and the glass of water convenient to the patient's hand. Tell him that small sips of water will help him to swallow during the procedure and that he can expect tears and flow of nasal secretions. CAUTION: Do not emphasize the possibility of gagging or vomiting, but place the emesis basin convenient to your hand. e. Measure the correct length of tubing to be inserted by following the steps below. (This is done to ensure passage of the tube into the stomach.) (1) nose, plus: Use the tube to measure from the patient's ear lobe to the tip of his (2) The distance from the tip of the nose to the bottom of the xiphoid process (tip of breastbone). Mark this distance with a piece of adhesive tape. f. Lubricate the tip of the tube with water-soluble lubricant to prevent injury to the nasal mucosa. g. Insert the tube. (1) Instruct the patient to tilt his head back and insert the tube into one of the nares. Advance slowly. (2) When you feel the tube begin to curve down in to the pharynx, instruct the patient to tilt his head forward slightly. This position facilitates passage of the tube by closing the trachea and opening the esophagus for ease of swallowing. (3) Unless contraindicated, instruct the patient to swallow sips of water. Continue to advance the tube to the desired distance as the patient swallows. (4) Advance the tube the measured distance. CAUTION: Discontinue insertion immediately if the patient coughs or chokes. Remove the tube completely. Allow the patient to rest for a few minutes before attempting reinsertion. Discontinue the procedure again if coughing, choking, or excessive gagging occurs. Report two unsuccessful attempts to the professional nurse. h. Test for placement of tube in stomach. (Tube may be lightly taped to avoid movement during placement testing.) MD0918 1-25 (1) One method is to aspirate with a syringe. Fit the syringe tip snugly into the end of the tube. Aspirate slowly and observe the barrel of the syringe for gastric content return. (2) Another method is to place a stethoscope over the epigastric area and inject 5 ml of air into the tube. Air can be detected by a whooshing sound entering the stomach rather than the bronchus. (3) Test to make sure the tube is not in the trachea. As the patient exhales, immerse the end of the tube momentarily in water. No bubbles should appear. If they do appear on exhalation, pinch off and remove the tube immediately. (4) If it is certain that the tube is in the stomach but no secretions have been aspirated, wait a minute or so. Encourage the patient to relax. Try aspiration again. The tube sometimes becomes kinked or momentarily plugged with mucus or a food particle. i. Following successful aspiration, clamp the tube until you are ready to begin the procedure for which the tube was inserted. j. Tape tube in place at nostril, using strips of hypoallergenic tape. Split one 3inch length of tape halfway down its length. Wrap one split end around the tube at the nostril entry point. Center the tube in the nostril to prevent pressure on either side. With the two free ends, anchor the tube to the bridge of the nose. k. Report the completion of the procedure to the professional nurse, and record the procedure on the nursing notes. 1-29. TUBE REMOVAL Nasogastric tubes must be removed quickly and smoothly to prevent choking or gagging. a. Clamp or pinch off the tube. b. Remove tape or safety pins securing the tube. c. Hold some tissues at the patient's nose, and withdraw the tube quickly and smoothly, catching the end in the tissues as it emerges from the nose. d. Immediately after removal of the tube, encourage the patient to gently blow his nose. e. Assist the patient to rinse his mouth and wash his face. f. Change any soiled bedding or pajamas. Position the patient for comfort. MD0918 1-26 g. Remove all unnecessary equipment from the bedside. h. Wash your hands. i. Document the procedure and the patient's tolerance in the nursing notes. 1-30. SUCTION Suction drainage by means of a mechanical drainage apparatus may be ordered by the physician. These suction devices are designed to provide controlled, lowpressure suction to avoid injury to mucous membranes. Two commonly used electric powered pumps are the Gomco and Emerson pumps. Be certain to read the manufacturer's instructions and local SOP before attempting to use this equipment. In hospital areas such as a recovery room or intensive care area, a special suction device may be available for use with a wall suction outlet. 1-31. SUCTION PROCEDURE a. Test the suction equipment by aspirating water through the drainage tubing. Clamp the tubing. b. Connect the nasogastric tube to the drainage tubing. c. Unclamp both the drainage tubing and the N/G tube. Observe for drainage in the tubing. d. Support the drainage tubing by anchoring it to the bottom bed sheet. (1) Use a rubber band or cloth tape looped around the tubing and pin the rubber band or tape it to the sheet. (2) Allow sufficient length of tubing to prevent pull on the tube when the patient moves or turns. e. Document the procedure in the nursing notes. f. Check the operation of the suction equipment frequently. Observe the following: MD0918 (1) Machine operation. (2) Connections should be properly fitted and airtight. (3) Tubing should not be kinked. (4) Drainage in the tubing. 1-27 (5) Drainage in the collection bottle. g. If no drainage is observed to be moving through the tube, and all equipment is operational, the tube may be obstructed. Failure to drain may be due to mucous clogging the tube or due to the end of the tube adhering to the wall of the stomach. If this is the case, attempt to clear the obstruction by one of the following nursing measures. (1) Change the patient's position by turning him or by raising or lowering the head of the bed. (2) Reposition the nasogastric tube. Loosen the tape and withdraw the tube about an inch. (3) If neither. of the above methods are successful notify the professional nurse The physician may order irrigation of the tube to clear the obstruction. 1-32. DISCONTINUE SUCTION To discontinue suction, complete the following steps. a. Clamp off the nasogastric tube. b. Turn off the suction apparatus. c. Protect the open end of the nasogastric tube by covering loosely with a gauze dressing. d. Take the suction equipment to the utility room. e. Measure the drainage. Record on I&O worksheet. f. Dispose of used equipment per local ward SOP. g. Record the procedure in the nurse’s notes. Note the color, character, and amount of drainage. h. Do not remove a nasogastric tube unless specifically ordered. 1-33. INTESTINAL DECOMPRESSION Intestinal decompression accomplished by intubation and application of suction is similar in many respects to gastrointestinal suction drainage with a nasogastric tube. Important differences include the following considerations: a. Intubation is done by the medical officer. MD0918 1-28 b. The Miller-Abbott (or Cantor) tube is not taped to the patient's face following intubation. Since the tube is designed to advance through the stomach into the small intestine by gravity and peristalsis, taping or otherwise securing the outside length could interfere with the desired advancement. The long, distal length of tube is coiled loosely at the head of the bed unless otherwise ordered. c. Position and activity of the patient following intubation contribute to the advancement rate of the tube. The nursing staff must know the position, the sequence, and the time interval ordered for each change in position, and modify other patient care measures accordingly. For example, after the tube has been introduced into the stomach, placing the patient on his right side with the foot of the bed elevated for a specified time interval facilitates the passage of the tip of the tube into the pylorus. Once the tube starts to advance, subsequent positions may be ordered: on the back, in Fowler's position; and finally, left lateral recumbent, with the bed flat; followed by ambulation. NOTE: Explaining to the patient and securing his full cooperation is very important, but the patient may be too ill to understand instructions or to realize that the tube is anything more than a constant source of annoyance and discomfort. 1-34. CARE AND HANDLING OF DRAINAGE DURING TREATMENT a. Observe frequently the color and amount of drainage. Report any changes immediately to the professional nurse. Cloudy, pale-yellowish drainage is characteristic when the tube is in the stomach; bile-colored (greenish) drainage is characteristic when the tube is in the duodenum. In gastrointestinal drainage, blood varies in color--it may be dark red when fresh, dark brownish-red or in brown particles ("coffee ground drainage") if it has been partially digested. Fecal odor of the drainage is noticeable in intestinal obstruction. Note your observations in the patient's nurse’s notes. b. Measure the contents and empty the drainage bottle at the hours ordered by the physician, when the drainage bottle is two-thirds full or when suction is discontinued. c. Procedure for emptying the drainage bottle. (1) Clamp the nasogastric tube. Remove stopper of drainage bottle. Place stopper in emesis basin. Take bottle to utility room. (2) Measure and record amount of drainage. Dispose of measured drainage by flushing into hopper or toilet. (3) Rinse the bottle with cold water. Wash thoroughly with prescribed detergent solution. Rinse and drain. (4) Reconnect clean bottle, replacing the stopper securely. Release clamp. Observe for effective renewal of suction drainage. MD0918 1-29 1-35. NASOGASTRIC TUBE IRRIGATION a. Introduction. (1) Irrigate only on order by the physician. (The type and amount of solution and frequency of irrigation must be specified.) (2) Measure amounts of irrigating solution accurately and record on the I&O (Intake and Output) worksheet as specified by local Department of Nursing SOP. (3) Do not use the syringe to aspirate back the irrigating solution unless ordered to do so; ordinarily, all solution used to irrigate and clear the tube will be returned in the suction drainage. (4) Do not use a Luer-type syringe unless so ordered. An asepto (bulb) syringe or catheter-tip syringe is recommended for use because less pressure is exerted. b. Equipment. (1) Irrigation kit (or solution bowl, emesis basin, and a 30-50 ml syringe). (2) Solution ordered (at room temperature, unless otherwise specified). (3) Rubber-shod hemostat forceps, 2. c. Procedure. (1) Pour solution into bowl. (2) Clamp drainage tubing. (3) Place emesis basin under connecting tip between nasogastric tube and drainage tubing. (4) Clamp N/G tube (or pinch off with fingers) and disconnect N/G tube from the drainage tubing. NOTE: If suction drainage is not in use, it will be necessary to check the placement of the nasogastric tube by other means. Gentle aspiration with a syringe to check for stomach contents will verify that the tube is in the stomach. (5) Fill syringe, insert syringe tip into N/G tube, and unclamp tube. Gently inject a small amount of solution. If fluid flows in freely, the tube is open. Continue to irrigate until the prescribed amount has been injected. MD0918 1-30 CAUTION: Do not use force. (6) Clamp nasogastric tube and remove syringe. (7) Reconnect nasogastric tube to the drainage tubing. (8) of suction. (9) Release clamps and observe for flow of drainage upon reestablishment Record time, amount, and type of solution used on the I&O worksheet. d. Care of Irrigation Equipment. (1) Following a one-time irrigation, remove equipment. Dispose of used equipment properly. (2) If equipment is kept at the bedside for repeated irrigation at scheduled intervals, rinse syringe in tap water, and keep syringe and solution bowl between folds of the wrapper. Replace with clean equipment daily. 1-36. ADMINISTRATION OF MEDICATION THROUGH A NASOGASTRIC TUBE a. Pour required liquid medication into medicine cup. (Pills must be crushed and capsules opened.) b. Unless contraindicated, add 15-20 ml of water. Stir thoroughly, using a clean tongue blade. c. Place medication, tongue blade, a cup of water, and a 30-50 ml catheter tip syringe on a tray, and take to the patient's bedside. d. Clamp the drainage tubing and the nasogastric tube. Disconnect the nasogastric tube from the drainage tubing. NOTE: If suction drainage is not in use, it will be necessary to check the placement of the nasogastric tube by other means. Gentle aspiration with a syringe to check for stomach contents will verify that the tube is in the stomach. e. Remove the plunger from the syringe. Insert the syringe tip into the nasogastric tube and pour the medication into the syringe. Release the clamp, allowing the medication to flow into the nasogastric tube. f. Follow the medication with 30 ml of water to clear the tube. Replace clamp. MD0918 1-31 g. Reconnect the nasogastric tube to the drainage tubing, leaving the clamps in place. Unless otherwise ordered, the nasogastric tube should remain clamped for at least one hour to allow absorption of the medication. h. Record the time, medication type and amount, and the amount of water administered on the I&O worksheet. Also note the time the tube was clamped and the time it is to be unclamped. 1-37. GAVAGE Gavage, or tube feeding, is used to provide nourishment to a patient who is unconscious, unable to swallow, or too weak to eat. A liquid formula is ordered by the physician and provided by food service. Formula provided by food service must be marked with the patient's name and the date prepared. A nasogastric tube or a small caliber feeding tube must be in place for feedings. Local Department of Nursing procedure will specify the frequency with which the tube must be changed when the patient is receiving gavage feeding for a prolonged period of time. a. Equipment. (1) Syringe. (2) Liquid feeding of type and amount prescribed. (3) Feeding set (bag or bottle). (4) Cup of water. (5) Chux pad. b. Procedure. (1) Assemble the necessary equipment and prepare the feeding by pouring the prescribed amount into the feeding set. Do this in a clean work area, never in the dirty utility room. (2) If permissible, position the patient in an upright sitting position or modified Fowler's position. (3) If clamped, unclamp the nasogastric tube and check the tube for placement. Attach the syringe and aspirate gently to ensure that the tube is in the stomach. Reclamp the nasogastric tube. (4) Suspend the filled feeding set from an IV pole or irrigating stand. Unclamp the tubing and allow the feeding to advance to the end of the tubing, expelling MD0918 1-32 all air. Attach the adapter at the end of the tubing to the nasogastric tube. Place a chux pad under this connection. (5) Adjust the flow rate to deliver the required number of ml per minute. This can be done by adjusting the clamp located below the drip chamber. If precise control of feeding is required, the feeding may be controlled by use of an infusion pump such as IMED or IVAC. If pump control is not used, the patient must be observed at frequent intervals during feeding to prevent the feeding from being administered too quickly. (6) When the required feeding has been administered, clamp the feeding tube and disconnect it from the nasogastric tube. (7) Clear the nasogastric tube of feeding residue by instilling 30-50 ml of plain water. Clamp the tube. (8) Record the type and amount of feeding, along with the amount of water given, on the I&O worksheet. (9) Record the procedure and the patient's tolerance in the nursing notes. (10) Dispose of used equipment properly. Local Department of Nursing policy will specify the length of time a feeding set may be used before being exchanged. 1-38. LAVAGE a. Introduction. Gastric lavage is the washing out of the stomach via a nasogastric tube or stomach tube. Lavage is ordered to wash out the stomach (after ingestion of poison or an overdose of medication, for example) or to control gastrointestinal bleeding. If the patient does not have a nasogastric tube in place already, the physician will order the insertion of the appropriate tube. For a stomach wash, the physician will probably order the insertion of an Ewald stomach tube or a large lumen nasogastric tube. To control gastrointestinal bleeding, a large lumen Levine tube or Salem sump tube will be inserted. In the event of severe bleeding, as in the case of esophageal varices, a Sengstaken-Blakemore tube will be inserted. A large lumen tube is preferred, since particles of food or other material may occlude the lumen of a small tube. The tube must be checked to verify proper placement in the stomach prior to proceeding with lavage. b. Equipment. Gather the following equipment and take to the patient's bedside. MD0918 (1) Syringes, 2 or more, 50cc catheter tip. (2) Washbasins, 2 (to collect used solution). 1-33 (3) Bath towels. (4) Chux pads. (5) Emesis basin. (6) Paper tissues. (7) Graduated container for measuring. (8) Prescribed lavage solution (usually, normal saline solution). (9) Suction equipment readily available. c. Preparation. Prior to beginning the procedure, check to be certain that you have prepared everything you will need. (1) In most gastric lavage procedures, the physician's order will be to lavage "until clear." This means that the lavage procedure will be repeated until the stomach contents that are returned are clear, that is, nothing returned except the irrigating solution itself. This requires that you be prepared with at least 6 liters of solution. You may not need to use it all, but you should have it available at the bedside. (2) If the lavage procedure is being done to control gastrointestinal bleeding, the order will probably be "ice lavage." Chilling the solution with ice will promote constriction of the blood vessels, thereby helping to control bleeding. Again, you will need to have quite a bit of iced solution on hand and ready for use. (3) Position of the patient for lavage will depend upon the patient's tolerance and the physician's preference. Lavage may be done with the patient sitting or lying. Placing the patient on his left side with the HOB elevated 15 degrees will allow the tip of the tube to lie in the greater curvature of the stomach. d. Lavage Technique. There are two basic techniques used in performing gastric lavage. The technique used depends upon the reason for the procedure and the physician's preference. Check the doctor's orders to see which method is specified. If the physician does not specify the technique, consult with the professional nurse. The two techniques used are as follow. (1) Solution is instilled and aspirated 50cc at a time, using a catheter tip syringe. The procedure is repeated until the stomach contents return clear, the entire amount of prescribed solution has been used, or otherwise directed. (2) Solution is slowly poured into the tube through a funnel, allowing the solution to enter the stomach by gravity. Up to 500cc of solution may be instilled at a time, depending upon the size and tolerance of the patient. The tube is then lowered MD0918 1-34 below the level of the patient, allowing the solution to drain out of the stomach by gravity. When using this technique to lavage, it is imperative that the patient be assessed carefully for abdominal distension. Repeat the procedure until the stomach contents return clear, the entire amount of solution has been used, or otherwise directed. e. Procedure. (1) Assemble the necessary equipment. (2) Identify the patient and explain what is to be done. (3) Position the patient and place an emesis basin and paper tissues within (4) Drape the patient with towels or paper chux to absorb any drainage. (5) Verify tube placement by aspirating stomach contents. reach. (6) Place the stomach contents in a labeled specimen container for examination by the physician and/or laboratory analysis. (7) Instill lavage solution, using one of the techniques described above. (8) Remove the lavage solution, using one of the techniques described above, as appropriate to the method of administration. (9) Continue to lavage until stomach contents return clear, the prescribed amount of solution has been used, or as otherwise directed. (10) Continually observe the patient for cyanosis, increased respiration’s, gagging, and attempts to vomit. If the patient vomits, support his chin in hyperextension to keep the airway open and prevent aspiration. (11) When lavage is completed, clamp the tube if it is to remain in place. (12) If the tube is to be removed, clamp or pinch off the tube and withdraw it quickly and smoothly. Place it in a basin or chux. (13) Remove all used equipment from the bedside. (14) Measure the total lavage return. Estimate the amount of stomach contents by subtracting the known amount of solution used from the total. Record on the I&O worksheet. (15) Discard lavage solution. MD0918 1-35 (16) Dispose of equipment in accordance with local SOP. (17) Record the procedure in the patient's Nursing Notes. Note the following information. (a) Type and amount of lavage solution used. (b) Appearance, odor, color, and amount of gastric return. (c) Patient's tolerance to procedure. (d) Disposition of specimens. 1-39. NURSING CARE OF THE PATIENT WITH A NASOGASTRIC TUBE a. Provide good oral hygiene at regular and frequent intervals. Offer water or mouthwash to rinse the mouth every hour. Assist the patient to brush his teeth at least every 4 hours. b. Keep the nostrils free of accumulations of dried secretions. c. If permissible, apply lubricant such as Vaseline to the lips and nostrils for the patient's comfort. Patients may wear lipstick. d. Encourage the patient to swallow saliva naturally; the tube is a constant source of annoyance and the patient may have a tendency to expectorate excessively. The physician may allow chewing gum or hard candy to help maintain mouth moisture and to encourage normal swallowing of saliva. Only conscious, responsive, alert patients should be given these items. CAUTION: Remind the patient to remove gum or candy before mouth care and sleep. e. Report complaints and signs of nose or throat irritation (excessive mucus, sore throat, or hoarseness). f. Encourage the patient to change position frequently, using care not to pull on the tube and not to lie on the drainage tubing. g. Follow diet orders exactly. If water or clear fluids are allowed by mouth, be sure to check on amount to be given at one time. Know exactly whether or not the tube is to be clamped when fluids are given and at what time interval in relation to oral intake. For example, the order may be to clamp the drainage tube for 1 hour after intake to allow some absorption. MD0918 1-36 h. Keep accurate intake and output records. Large amounts of fluid and electrolytes are lost during continuous suction drainage. Information on all in-take and all output is used by the doctor in planning fluid replacement. i. Observe the patient frequently when he is asleep, noting the tube marking at the nostril. The patient may have unknowingly pulled the tube out partially or completely. If partially out, advance the tube to the required point and check for drainage. Tape securely. If the tube has been accidentally removed, notify the nurse or doctor. Reinsert only on order. Section V. GASTROSTOMY, COLOSTOMY, ILEOSTOMY 1-40. NURSING CARE OF THE PATIENT WITH A GASTROSTOMY a. A gastrostomy is a surgical opening into the stomach, made through an incision in the left, upper abdomen. The anterior gastric wall is sutured to the abdomen, preventing leakage of gastric contents into the abdominal cavity. The gastrostomy procedure is done when disease or injury of the esophagus makes gastric intubation by way of the esophagus impossible. At the time of surgery, the gastrostomy tube, with usually a size 20 to 26 catheter, is inserted into the stomach through the incision. The distal end is clamped to prevent leakage, and the tube is secured at the incision with one or two sutures. As healing of the wound takes place, a stoma (artificial opening) is formed, and the catheter can then be removed and reinserted. Some patients are fitted with a plastic prosthesis instead of the catheter. The prosthesis remains in place and a catheter is inserted through its lumen for feeding. A screw cap or plug seals off the prosthesis opening when the catheter is not in use. b. Special attention must always be paid to the skin area around the tube since there may be some leakage of gastric secretions and, unless the skin is kept clean and dry, it will soon become very irritated. When the nursing paraprofessional does the gastrostomy feeding, he must also know how to carry out the prescribed skin care and dressing procedure. c. For the patient's morale, his feeding procedure should resemble as much as possible a normal meal procedure and not be an activity incidental to the dressing and skin care routine. For example, dressing and skin care materials should not be assembled on the same tray with his feeding set. When the time intervals for doing all required procedures coincide, plan to do the dressing and skin care procedures first so that the patient is as clean, comfortable, and relaxed as possible for his meal. d. The teeth and mouth of a patient with a gastrostomy must be kept in optimum condition by frequent oral hygiene measures. e. If permissible, chewing gum may be given to stimulate the flow of saliva and keep the mouth moist. If the patient is unable to swallow the saliva, a covered, MD0918 1-37 disposable sputum container should be provided and changed frequently. Measurement of expectorated saliva should be recorded on the I&O worksheet. f. The physician may allow the patient to chew food and spit it out. This will stimulate salivation and exercise the gums. This measure should only be entrusted to reliable, compliant patients. 1-41. GASTROSTOMY DRESSING After the original surgical incision has healed, the dressing procedure for the stoma is routinely done by the nursing personnel in accordance with the physician's orders. Generally, a minimal number of dry, sterile, gauze compresses are placed around the tube. The clamped end of the gastrostomy tube may be coiled on top of the dressing. A semipermeable surgical dressing such as OpSite may also be used to protect the skin from breakdown. a. Equipment. (1) Basin of warm, soapy solution. (2) Basin of warm water. (3) Chux pads. (4) Wash cloth. (5) Towel. (6) Paper bag or Chux pad (for discarded materials). (7) Sterile 4 x 4 gauze compresses, or a surgical dressing such as OpSite. (8) OpSite or similar surgical dressing. b. Procedure. (1) Assemble the equipment. (2) Explain the procedure to the patient and screen the patient for privacy. Assist the patient into a comfortable position in bed. Turn the bed covers back to hip level and open the pajamas to expose the gastrostomy dressing. (3) Place a paper bag or Chux pad at the foot of the bed. Place a Chux pad at the upper left side of the patient. (4) MD0918 Wash your hands. 1-38 (5) While supporting the gastrostomy tube with one hand to prevent tension on the tube, remove the old dressing. Inspect it for character, color, and odor of drainage before discarding it into the paper bag. (6) breakdown. Inspect the skin around the stoma (peristomal) for irritation or (7) Wash the peristomal area with the washcloths and soap solution. Rinse thoroughly and pat dry with a towel. Note any complaints from the patient of soreness or tenderness in the peristomal area. (8) Apply a dry dressing. OpSite or sterile 4 x 4 gauze compresses may be used. NOTE: If using gauze dressings, use surgical net or montgomery straps instead of tape to secure the dressing. Frequent application and removal of tape will cause skin breakdown. (9) Coil the clamped end of the tube on the surface of the dressing. Be sure there is no tension on the tube. (10) Make the patient comfortable. (11) Remove dressing equipment and discard waste. Wash hands. (12) Record procedure, observations of skin condition, and patient tolerance in the Nursing Notes. 1-42. GASTROSTOMY TUBE FEEDING A gastrostomy tube feeding should be treated as a normal meal. The procedure must never be rushed, and the atmosphere should be pleasant and relaxing for the patient. The prescribed feeding may be a commercially prepared formula or a special preparation from the hospital food service. The procedure for administration of a gastrostomy tube feeding is as follows. a. Review the patient's clinical record to verify physician's order for the amount and type of tube feeding. b. Wash your hands. c. Collect the necessary supplies and equipment. MD0918 (1) Feeding solution, as prescribed. (2) Large bulb syringe or catheter tip 50cc syringes. 1-39 (3) Tap water. (4) Graduated container for measuring. d. Prepare the tube feeding, as ordered. (1) For 1/4, 1/2, or 3/4 strength feeding, mix the solution with the appropriate amount of water to obtain the desired strength. (2) Always check the label of a commercially prepared formula for expiration (3) When mixing a feeding formula, label with date, time, and initials. (4) Warm solution to room temperature to prevent cramps and gas date. formation. e. Approach and identify the patient and explain procedure. f. Provide for patient privacy. g. Place patient in semi-fowler's position in bed to promote digestion. h. Fold top linen down to expose gastrostomy tube and protect area with towel. i. Attach the syringe to the clamped gastrostomy tube. (1) Remove plunger if using a 50cc catheter tip syringe. (2) Remove bulb from bulb syringe. j. Check patency of the tube by pouring a small amount of water from the graduated container into the syringe. (1) Remove clamp. (2) If water flows freely, the tube is patent. (3) If water does not flow freely, notify the professional nurse. k. Pour feeding solution into the syringe. (1) As solution flows into the stomach, tilt the syringe to allow air bubbles to (2) Add more solution to the syringe when about one quarter of it remains. escape. MD0918 1-40 (3) Increase or decrease the flow rate by raising or lowering the syringe. (4) Depending upon the solution's consistency, and the amount, feeding may take 10 to 20 minutes. l. After administering the ordered amount of feeding solution, flush the tube with 30 ml of water to clear the feeding solution residue. m. Clamp or plug the tube to prevent leakage. n. Instruct patient to remain in a sitting position for 30 minutes to enhance normal digestive process. o. Record feeding on intake and output record. Record procedure and the patient's tolerance in the nursing notes. p. Check back with the patient. He should not feel overly full or nauseated. Report these symptoms to the professional nurse at once. Gastric distress may require adjustment of feeding schedule. 1-43. COLOSTOMY a. A colostomy is a surgically created, artificial opening (stoma) into the colon through the abdomen. It may be temporary or permanent. b. A temporary colostomy is normally made for diversion of fecal material. Fecal diversion is utilized in order to rest a portion of the colon following intestinal surgery, in preparation for further surgery, or in cases of severe inflammatory disease (such as diverticulitis). c. A permanent colostomy serves as an artificial anus for the remainder of the patient's life. This procedure is done in conjunction with the removal of the lower bowel and rectum. Although there is no sphincter muscle control at the stoma, bowel movements may be controlled by a daily routine that encompasses diet, physical activity, and colostomy irrigation’s. Consistency of the bowel movements generally depends upon the location of the colostomy (see figure 1-5), but can be manipulated by the patient's choice of diet. d. Whether temporary or permanent, a colostomy can be very distressing to the patient. Patients with colostomies require encouragement, understanding, and assistance in overcoming the negative emotions associated with a colostomy, and in learning independence and self-sufficiency in living with a colostomy. e. Colostomy "training" should begin as soon as possible, with the permission of the physician, after surgery. The ease and skill with which the nursing personnel care for the patient with a colostomy are important in helping the patient physically and MD0918 1-41 emotionally. The patient and his family will learn that a colostomy can be effectively managed to allow a full and active life. f. There are several different surgical procedures that create different types of colostomies. The procedure used will depend upon the nature of the disease, the desired end result (temporary or permanent), and the physician's preference, among other things. For example: Figure 1-5. Colostomy sites. (1) Two stoma openings can be created at the abdominal surface (double barrel). One serves as a temporary artificial anus for the functioning part of the gastrointestinal tract, discharging feces, and flatus. The second opening leads to the nonfunctioning part of the colon and rectum. Mucous or serous secretions are normally discharged from this opening. This opening may also be utilized for irrigation of the resting colon. This procedure would be utilized when the colostomy is temporary. Later surgery would involve closing the stomas with re-anastomosis of the bowel. (2) A single colostomy may be done at one of the sites illustrated in figure 15. The site chosen normally depends upon the portion of the bowel that must be removed. The colostomy site is created at a section of healthy bowel. The bowel distal to the colostomy is removed and the rectum surgically closed. MD0918 1-42 1-44. GENERAL NURSING IMPLICATIONS a. It is the responsibility of the nursing staff to help the patient become independent and self-sufficient in the care of his colostomy. However, do not permit colostomy care and teaching to dominate the nursing interaction. Take an interest in the patient and treat him, as a person-who just happens to have a colostomy. This will discourage the patient from dwelling on the idea that he is somehow "different" or "abnormal" because of his colostomy. b. To promote self-sufficiency and return to normal living, follow these nursing guidelines. (1) When the patient is ready, encourage participation in colostomy care. (2) To promote a relaxed atmosphere, ensure complete privacy for the patient if desired. (3) To emphasize return to normal bowel evacuation habits, perform colostomy irrigations in the bathroom while the patient is seated on the toilet. (4) Unless contraindicated, eliminate the use of gloves during irrigation and dressing changes. This will discourage the patient from feeling that colostomy care is a "dirty" procedure. (5) Encourage the patient to learn and perform good care. This will promote a clean, odor-free stoma and prevent excoriation of the peristomal skin. (6) Follow and assist the patient as he progresses to a normal diet. (a) Diet will aid in establishing regularity. (b) The patient should experiment with different foods and food combinations, as each individual responds differently to various foods. (There are no set rules about foods to avoid.) (c) By experience, the patient will discover which foods cause gas, loose stools, distention, or discomfort. (Chewing slowly with the mouth closed may help to reduce gas.) 1-45. COLOSTOMY IRRIGATION a. Irrigation should be done at the same time each day in order to establish regularity of bowel evacuation. Unless contraindicated or otherwise ordered by the physician, it is best to establish a routine of daily irrigation in accordance with the patient's former bowel habits. For example, if the patient has always moved his bowels MD0918 1-43 after breakfast, establish the irrigation routine for that time, rather than some other arbitrary schedule. b. Review the procedure with the patient, if necessary. c. Wash your hands. d. Assemble the necessary equipment (Equipment can be kept at the patient's bedside or in the bathroom.) (1) Irrigation kit (irrigation bag with clamp and tubing, cone-tip irrigation catheter, irrigation drain pouch). (2) Water soluble lubricant. (3) IV pole (or other suspending hook). (4) Soap and water. (5) Washcloth and towel. (6) Ostomy appliance. (7) Waste receptacle. (8) Prescribed irrigating solution, usually 500-1000cc warm (100º--105ºF) tap water. e. Provide for privacy. f. If the patient is ambulatory, have the patient sit on the toilet or on a chair facing the toilet. If the patient is bedridden, elevate the HOBº 45-90ºand position Chux around the patient. g. Fill the irrigation bag with the prescribed solution and hang it on the IV pole or hook. (1) The bottom of the bag should be at the patient's shoulder level when he is seated to prevent fluid from entering the bowel too rapidly. (2) The bottom of the bag should be placed 18 to 20 inches above the stoma when the patient is in bed. h. Open the clamp on the irrigation tubing and allow the solution to fill the tubing. Reclamp. (This prevents the administration of air into the intestines.) MD0918 1-44 i. As necessary, prepare to begin the colostomy irrigation (see figure 1-6). (1) Remove the ostomy pouch, if applicable, and place the irrigation drain pouch over the stoma. (Attach stoma belt if required.) (2) Place the bottom, open end of the irrigation drain pouch in the toilet (or bedpan) to facilitate drainage by gravity. (3) Connect the cone-tip catheter to the tubing and flush with solution. Figure 1-6. Colostomy irrigation. j. Lubricate the cone with the water-soluble lubricant to avoid irritating the mucous membranes. k. Gently insert the cone into the stoma so that the stoma is occluded. l. Unclamp the irrigating tubing and allow the water to flow in slowly. (1) Allow water to enter the colon over a period of 10 to 15 minutes. (2) If cramping occurs, slow down the flow rate and ask patient to deep breathe until cramps subside. Cramping during irrigation may indicate that: (a) MD0918 The bowel is ready to empty. 1-45 (b) The water is too cold. (c) The flow is too fast. (d) The tube contains air. m. Clamp the catheter and remove from the stoma. Fold down the top opening of the irrigation drain pouch and secure it in the closed position. n. Have the colostomy patient sit on or near the toilet for about 15 to 20 minutes so the initial colostomy returns can drain into the toilet. (If the patient is on bed rest, allow the colostomy to drain into the bedpan.) o. Close the colostomy irrigation drain pouch with a rubber band or pouch clip, then ambulate the patient, or return him/her to bed. (1) Ambulating stimulates elimination, producing improved irrigation return. (2) Have the non-ambulatory patient lean forward or massage his/her abdomen to stimulate return. p. Wait approximately 1 hour for the rest of the colostomy return, then remove the irrigation drain pouch from the patient. q. Gently clean the area around the stoma with mild soap and water. (1) Be careful not to rub the skin. (2) Rinse and dry the area with a towel. r. Apply a clean pouch or dressing, as applicable. s. Provide for the patient's comfort; remove and dispose of used supplies. t. Record the procedure and significant nursing observations in the patient's clinical record and report it to charge nurse. (1) Note color and condition of stoma and peristomal skin. (2) Record color, consistency, and amount of drainage. (3) Note amount of irrigating solution used. u. As recovery progresses, the nursing personnel should gradually assume a more passive role in colostomy care, allowing the patient to assume the active role. MD0918 1-46 1-46. ILEOSTOMY a. An ileostomy is a surgically created, artificial opening (stoma) into the small bowel (ileus) through the abdomen. The stoma is located low on the abdomen (lower quadrants.) Most ileostomies are performed because of inflammatory bowel disease. b. An ileostomy may be temporary or permanent. If temporary, the bowel is left intact. In a permanent ileostomy, the colon is removed. c. Unlike a colostomy, an ileostomy cannot be regulated. The fecal contents of the ileum are fluid, and drain continuously. For this reason, an ileostomy patient must always wear an appliance. d. New surgical techniques are being used to create what is called a "continent" ileostomy. In these procedures, a portion of the ileum is used to create a pouch with a nipple valve. Pressure from feces entering the pouch causes the valve to close, preventing leakage of gas or feces from the stoma. The pouch can be easily emptied by insertion of a catheter and gravity drainage. Because the pouch is continent, the patient does not need to wear an appliance. 1-47. NURSING IMPLICATIONS FOR THE PATIENT WITH AN ILEOSTOMY a. There are many commercial ileostomy appliances available. Each patient should be fitted with the style that is most comfortable and convenient for that patient's lifestyle. Appliances should be applied, removed, and cleaned in accordance with the manufacturer's directions. b. The appliance worn over the stoma of a conventional, or "incontinent," ileostomy must be drained several times daily. (1) For convenience, this can be done at the same time the patient urinates. (2) Pouches are equipped with an emptying spout at the bottom, allowing the contents of the pouch to be drained directly into the toilet. c. An appliance can normally be left in place for 2-4 days before being changed. A regular schedule for changing the appliance should be established to avoid leakage. d. Each time the appliance is changed, the peristomal skin should be washed with soap and water and inspected for irritation or breakdown. (1) Although each patient will develop his own routine for changing the appliance, it is best to perform this care when the ileostomy is quiet. For example: before a meal, 2 hours after a meal, or at bedtime. MD0918 1-47 (2) If desired, the patient may remove the appliance, shower, or bathe, and then apply a clean appliance. e. The stoma should be covered to absorb drainage and prevent excoriation of the peristomal skin while changing appliances. (1) A gauze dressing may be used to cover the stoma. (2) A small vaginal tampon may be gently inserted into the stoma. 1-48. DIETARY CONSIDERATIONS FOR THE PATIENT WITH AN ILEOSTOMY a. Most physicians do not recommend dietary restrictions once the patient has recovered from surgery and is released from the hospital. However, foods that cause discomfort, gas, or diarrhea should be omitted. b. Hard to digest foods should be avoided if they cause discomfort. Examples are celery, popcorn, berries, and high-fiber foods. c. Odor-causing foods include cabbage, onions, fish, and eggs. These foods should be tested individually to determine if they can be tolerated. d. Spinach, parsley, yogurt, and buttermilk act as deodorizers on the intestinal tract. e. All foods ingested will normally pass through the ileostomy within 4-6 hours. Section VI. GASTROINTESTINAL DISORDERS 1-49. GASTRITIS/GASTROENTERITIS a. Acute gastritis is the irritation and inflammation of the stomach's mucous lining. Gastritis may be caused by a chemical, thermal, or bacterial insult. For example, drugs such as alcohol, aspirin, and chemotherapeutic agents may cause an attack of gastritis. Likewise, hot, spicy, rough, or contaminated foods may bring about an attack. Management involves symptomatic treatment measures after removal of the causative agent. b. Gastroenteritis, or inflammation of the stomach and intestines, is generally caused by bacteria and viruses. Other causes include parasites, food allergens, drug reactions to antibiotics, and ingestion of toxic plants. Treatment is the same as for gastritis, with the addition of anti-microbial drugs for severe cases. c. Signs and symptoms of both include pain, cramping, belching, nausea, and vomiting. Severe cases may include hematemesis. Diarrhea may occur with gastroenteritis. MD0918 1-48 d. Nursing implications. (1) Stop all P.O. intakes until symptoms subside. (2) Assess the patient's symptoms and administer the prescribed symptomatic relief medications such as antacids and antiemetics. (3) Monitor intake and output closely. Excessive vomiting or diarrhea may result in severe electrolyte depletion that will require replacement therapy. (4) Administer and monitor IV therapy when ordered to replace lost fluids. (5) Weigh daily to monitor weight loss. (6) Encourage the prescribed diet to maintain nutrition. 1-50. GASTROINTESTINAL ULCERS a. A gastrointestinal ulcer is a break in the continuity of the mucous lining. Ulcers may occur in any part of the GI tract that comes in contact with the gastric juices. Ulcers commonly occur in the lower esophagus, the stomach, and the duodenum. b. In addition to mucosal deterioration by hydrochloric acid and pepsin secretion, other factors may be implicated in the development of ulcers. (1) Emotional stress. (2) Prolonged physical stress associated with trauma, surgery, burns, and (3) Hereditary factors. so forth. (4) Certain drugs and medications. For example: alcohol, caffeine, aspirin, corticosteroids, and chemotherapeutic agents. c. The primary symptom of ulcers is pain. It is described as a burning, cramping, aching, or gnawing pain in the stomach area between the xiphoid process and the umbilicus. The severity of the pain is generally an indication of the extent of the ulceration. Likewise, ulcer pain is normally localized, the patient being able to indicate the area of the pain by pointing one finger. Radiating pain indicates a severe or perforated (ruptured) ulcer. d. Nursing implications are usually twofold. The focus of treatment and nursing care for the patient with ulcers is twofold. The first objective is to promote gastric rest. The second objective is prevention of further ulceration. Both of these objectives may be accomplished by utilizing the following measures: MD0918 1-49 (1) Encourage physical and emotional rest by using relaxation techniques and prescribed medications (such as sedatives and tranquilizers) to reduce anxiety, restlessness, and insomnia. (2) Practice prophylaxis (prevention) by use of antacids and avoidance of irritants such as aspirin, alcohol, caffeine, and spicy foods. (3) Dietary management aids in control of pain and prevention of ulcers. Meals should be frequent, regular, and small to moderate in size. Foods not well tolerated should be eliminated. Daily intake should be of sufficient caloric and nutritive value to maintain health. (4) When ulceration is in the acute stage, diet should be modified to consist of bland, low-fiber, non-gas-producing foods. Foods that are mechanically, chemically, and thermally nonirritating to the stomach. e. Observe for signs and symptoms such as nausea, vomiting, blood in emesis or stool, abdominal rigidity, or abdominal pain. These symptoms may indicate the presence of bleeding, rupture, or obstruction at the ulcer site. 1-51. APPENDICITIS a. Definition. Appendicitis is the inflammation of the vermiform appendix. The appendix fills with food and empties regularly. Because its lumen is quite small, it empties irregularly and is prone to obstruction. The obstruction sets off an inflammatory process that may lead to infection, necrosis, and perforation. b. Signs and Symptoms. (1) Generalized abdominal pain that localizes in the right lower quadrant. (2) Anorexia. (3) Nausea and vomiting. (4) Abdominal rigidity or guarding. (5) Rebound tenderness. (6) Fever. (7) Elevated white blood cell count. c. Nursing Implications. (1) MD0918 Administer IV fluids as ordered to maintain hydration. 1-50 (2) Keep the patient NPO until symptoms subside and/or surgery is ruled out. (3) Position the patient in Fowler's or semi-Fowler's position. This position relaxes the abdominal muscles and reduces pain. (4) Never apply heat to the abdomen, as this may cause the appendix to (5) Analgesics are normally withheld since they mask symptoms. rupture. d. Treatment. Treatment of choice is surgical removal of the appendix, especially if rupture is suspected or imminent. (1) If the appendix can be removed before it ruptures, the post-op course is generally uncomplicated. The wound is closed and the patient is usually discharged within a week. (2) If rupture has occurred, the wound is often left open to drain. The patient must be observed for signs and symptoms of obstruction, peritonitis, hemorrhage, or abscess. 1-52. PERITONITIS a. The peritoneum is the serous membrane that lines the abdominal cavity and covers the visceral organs. Peritonitis is inflammation of the peritoneum. Inflammation may be generalized throughout the peritoneum, affecting the visceral and parietal surfaces of the abdominal cavity, or may be localized in one area as an abscess. b. Peritonitis occurs as a result of leakage of contents from an abdominal organ into the abdominal cavity. Generally, this disorder results from perforation of the GI tract, allowing bacterial contamination of the peritoneum. Peritonitis may also occur as a result of chemical irritation, and subsequent infection, caused by rupture of an organ. (For example, the ovaries, spleen, or urinary bladder.) c. Signs and symptoms. (1) Diffuse pain that eventually localizes in the area of the underlying (2) Abdominal tenderness. (3) Abdominal muscle rigidity. (4) Rebound tenderness. (5) Nausea and vomiting. process. MD0918 1-51 (6) Paralytic ileus. (7) Fever. (8) Rapid pulse rate. (9) Elevated WBC. d. Nursing implications. The objectives of medical treatment are to identify and eliminate the cause, treat the infection, and maintain fluid and electrolyte balance, while promoting patient comfort. To promote patient comfort, the nursing personnel should do the following: (1) Observe for signs of hypovolemia and shock. These conditions may result from loss of fluids and electrolytes into the abdominal cavity. (2) Strictly monitor I&O and vital signs. (3) Observe safety precautions, since fever and pain may cause the patient to become disoriented. (4) Administer prescribed medications and intravenous fluid replacement. 1-53. INTESTINAL OBSTRUCTION a. Intestinal obstruction is defined as any hindrance to the passage of intestinal contents through the small and/or large bowel. Obstruction may be partial or complete. Severity depends upon the area of bowel affected, the degree of blockage, and the degree of vascular impairment. b. Intestinal obstruction is divided into two basic categories: mechanical and non-mechanical. (1) Mechanical obstruction results from obstruction within the lumen of the intestine or mural obstruction from pressure on the walls of the intestines. Causes include: (a) Foreign bodies such as fruit pits, parasitic worms, or gallstones. (b) Volvulus. (c) Intussusception. (d) Hernia. (e) Cancer. MD0918 1-52 (f) Adhesions. (g) Strictures. (2) Non-mechanical obstruction is the result of physiological disturbances. Causes include: (a) Electrolyte imbalances. (b) Neurogenic disorders (such as spinal cord lesions). (c) Paralytic (adynamic) ileus, developing as a result of abdominal surgery, trauma, or infection. c. Signs and symptoms of small bowel obstruction. (1) Small bowel obstruction is characterized by colicky pain, constipation, nausea, and vomiting. (2) If the small bowel obstruction is complete, the peristaltic waves become quite vigorous, assuming reverse direction and propelling intestinal contents toward the mouth rather than the rectum. The patient vomits stomach contents first, then the bilious contents of the duodenum, and finally the fecal contents of the ileum. (3) In later stages, dehydration and plasma loss result in hypovolemic shock. (As much as 10 liters of fluid can collect in the small bowel, causing a drastic reduction in plasma volume.) d. Signs and symptoms of large bowel obstruction. (1) Symptoms of large bowel obstruction differ from those of small bowel obstruction because the colon is able to absorb its fluid contents and distend well beyond normal size. (2) Constipation may be the only symptom for several days. (3) Eventually, the distended colon loops will be visible on the abdomen. (4) Nausea and cramps, abdominal pain will occur. (5) Vomiting is absent at first, but when obstruction becomes complete, fecal vomiting will occur. (6) If the obstruction is only a partial one, any of the above symptoms may occur in a less severe form. Additionally, liquid stool may leak around the obstruction. MD0918 1-53 e. Nursing implication for intestinal obstruction. (1) Abdominal girths should be measured daily. For accuracy of comparison, follow these suggested guidelines: (a) Use the same measuring tape each time. (b) Place the patient in the same position each time. (c) Ensure that the tape measure is placed in the same position each time. This can be done by drawing small tic marks on the patient's abdomen to indicate position for the tape. (d) Measure the patient at the same time each day. (2) occult blood. (3) Note the color and character of all vomitus. Test for the presence of Any stool passed should be tested for the presence of occult blood. (4) Monitor vital signs closely. Elevations of temperature and pulse may indicate infection or necrosis. (5) Monitor I&O closely. Fluid and electrolyte losses must be replaced. 1-54. DIVERTICULAR DISEASE a. Definition. Diverticula are bulging dilatations or "out-pouchings" of the gastrointestinal walls. Common sites are the sigmoid colon, duodenum, and the distal ileum. However, diverticula can occur anywhere along the GI tract, from the esophagus to the anus. b. Diverticulosis. The presence of asymptomatic diverticula is called diverticulosis. Diverticulosis is sometimes the source of LLQ pain that is relieved by defecation or flatulence. Constipation or diarrhea may also occur. Diverticulosis generally requires no treatment other than dietary modification to prevent irritation of the bowel. c. Diverticulitis. When diverticula become inflamed or infected, the condition is referred to as diverticulitis. Food and bacteria lodge and harden in the diverticular sac. Inflammation results, followed by infection. Complications include abscess, obstruction, perforation, peritonitis, and hemorrhage. (1) Symptoms include low grade fever, nausea, gas, abdominal pain, and abdominal rigidity. MD0918 1-54 (2) Treatment of mild cases of diverticulitis includes antibiotics, antispasmodics, stool softeners, and liquid diet. (3) Severe cases of diverticulitis, or cases that involve perforation, obstruction, fistula, or peritonitis may require surgical intervention. Colon resection may be necessary to remove the diseased portion of the bowel. A temporary or permanent colostomy may be indicated. d. Nursing Implications. (1) Reinforce patient education regarding dietary modification. Increased roughage in the diet may prevent intestinal contents from lodging in the diverticula. Roughage includes grains, fruits, vegetables, and fiber. (2) When symptoms occur, the patient should immediately alter his diet to one that is bland and nonirritating. (3) Diet should include adequate fluid intake to avoid constipation. Constipation encourages inflammation of the bowel. (4) Vital signs and I&O should be monitored closely. (5) Observe stools for color and consistency. (6) If surgery becomes necessary, observe routine preoperative and postoperative nursing care procedures. Section VII. HEPATO-BILIARY DISORDERS 1-55. HEPATITIS Hepatitis is inflammation of the liver with destruction of liver cells. Hepatitis may be viral or non-viral in origin. a. Viral hepatitis includes: (1) Type A hepatitis virus (infectious hepatitis). (2) Type B hepatitis virus (serum hepatitis). (3) Type non-A/non-B hepatitis virus. b. Non-viral hepatitis includes: MD0918 (1) Toxic hepatitis (acute liver cell necrosis). (2) Drug induced hepatitis. 1-55 1-56. VIRAL HEPATITIS a. Type A hepatitis virus, also called infectious hepatitis, is a highly contagious form of hepatitis. Modes of transmission include: (1) Oral ingestion of contaminated materials such as water, milk, or shellfish from contaminated waters. (2) Fecal/oral contamination from poor sanitation. (3) Person-to-person contamination from blood, saliva, or feces. (4) Blood transfusions are RARELY, if ever, a source of Type A hepatitis virus. b. Type B hepatitis virus, known as serum hepatitis, is the type that poses a threat to health care workers. Type B hepatitis virus is spread through: (1) Contact with contaminated body secretions. (2) Parentally, through contact with contaminated needles, syringes, blood, and blood products. (3) By transmission from mothers to babies. c. A third type of hepatitis virus is identified as type non-A/non-B. Although the cause for this type of hepatitis is unclear, its mode of transmission appears to be bloodborne. Type non-A/non-B hepatitis virus is responsible for 80 percent—90 percent of all the post transfusion cases of hepatitis. It is associated with: (1) Blood transfusions and transfusion products. (2) Parenteral drug abusers. (3) Personnel associated with renal transplant and dialysis units. (4) Institutions with long-term residents. d. Refer to Table 1-1 for a comparison of the types of viral hepatitis. 1-57. NURSING IMPLICATIONS ASSOCIATED WITH VIRAL HEPATITIS a. Rest. Patients with viral hepatitis experience fatigue and malaise during all phases of the infection. (1) MD0918 Bed rest should be encouraged during the acute phase of the illness. 1-56 (2) During convalescence, the patient should be encouraged to alternate periods of rest with periods of activity. b. Diet. Nonspecific GI symptoms such as anorexia, nausea, and abdominal pain occurs in-patients with hepatitis. (1) tolerances. Diet should be modified to conform to individual symptoms and (2) The patient should be encouraged to eat the prescribed diet to maintain an optimum balance of nutrients and to promote healing. (3) Nursing personnel should note and document what the patient eats. If the patient is unable to tolerate the prescribed diet, the physician may order an alternate form of nutrition therapy. c. Emotional Support. Viral hepatitis is a prolonged illness, often requiring lengthy hospitalization. The patient may become discouraged with the course of treatment and depressed because of separation from family. (1) Make an effort to stop and visit with the patient whenever you have a few extra minutes. Allow the patient time to ventilate feelings. (2) Arrange with occupational therapy or the facility Red Cross volunteers to provide books, cards, games, and other diversional activities. (3) Allow time for visiting with family members. d. Infection Control. Isolation and infection control procedures should be implemented IAW the local infection control SOP. (1) Alert the hospital infection control nurse when a patient with hepatitis is admitted. (2) Consult the infection control SOP for the procedures to be implemented for that particular type of hepatitis. e. Referrals. It may be necessary to consult with other activities. (1) The preventive medicine activity may be required to make a health investigation in certain cases of hepatitis. (2) The community health nurse may be required to provide follow-up home visits. MD0918 1-57 Mode of Transmission Incubation Period Prodromal Phase (Preicteric) Icteric Phase Post-Icteric Phase Type A Hepatitis Virus Type B Hepatitis Virus (Infectious Hepatitis) (Serum Hepatitis) Fecal-oral contamination Body secretions of infected persons Person-to-person contaminated Water-borne needles, syringes food borne mothers to babies 2-6 weeks Mean: 30 days Generally asymptomatic at first with abrupt onset of flu-like symptoms: headache, malaise, fever, lassitude, and nonspecific GII symptoms such as anorexia, nausea, upper abdominal disconfort and vomiting Jaundice Dark urine Pale stools Tender and enlarged liver Pruritis 4-24 weeks mean: 90 days Insidious onset of variable symptoms: Includes same symptoms as Type A. Arthralgias Uticarial skin rashes Prolonged acute phase with anorexia, malaise and abdominal pain Jaundice may or may not occur When jaundice reaches its peak usually within two weeks, symptoms tend to subside 2-6 weeks convalescence Prolonged convalescence of 36 months Type non-A/non-B Hepatitis Virus Transfusions Transfusion products Personnel in Renal and Dialysis units Institutions with long-term residents 2-15 weeks mean: 60 days Isidious onset of symptoms Similar to type B, but less severe Similar to Type B, but less severe Most cases are without jaundice Prolonged convalescence Probability of a carrier state Table 1-1. Types of viral hepatitis. (3) Consult the local SOP or infection control nurse for guidance. f. Blood Donation. Patients who have had viral hepatitis should be instructed that it is unsafe for them to donate blood. They may contaminate a potential recipient. 1-58. NONVIRAL HEPATITIS a. Toxic hepatitis (acute liver cell necrosis) is caused by ingestion, inhalation, or injection of certain chemicals (hepatotoxins) that have a poisonous effect on the liver. MD0918 1-58 Examples include carbon tetrachloride, phosphorus, chloroform, vinyl chloride, and poisonous mushrooms. (1) Signs and symptoms include anorexia, nausea, vomiting, jaundice, and hepatomegaly. (2) Liver damage occurs within 24-48 hours, depending on the dose of the toxin. (3) as possible. For recovery to occur, the toxin must be identified and removed as soon b. Drug induced hepatitis is an idiosyncratic reaction to a drug due to hypersensitivity. Examples include sulfonamides, isoniazid, and halothane. (1) Symptoms may appear any time during or after exposure to the drug, but usually appear after 2-4 weeks of therapy. (2) Onset is generally abrupt, with chills, fever, anorexia, nausea, rash, and pruritis. Jaundice and hepatomegaly may occur later. (3) Symptoms subside when the offending drug is removed. c. Nursing implications. (1) Care is symptomatic and supportive in nature. (2) Patient education should be reinforced regarding proper handling of chemicals, cleaning agents, solvents, and so forth, as applicable. (3) Nursing personnel, pharmacists, and physicians should alert patients to medication side effects. If fever, rash, or pruritis result from any medication, it should be stopped at once and the prescribing physician consulted. (4) anesthetic. Patients with known liver disease should not receive halothane as an 1-59. CIRRHOSIS a. Cirrhosis is a chronic disease of the liver characterized by destruction of the parenchyma (functional) cells, with fibrotic tissue replacement. This degeneration causes impaired blood and lymph flow, which results in hepatic insufficiency. The major causes of cirrhosis are alcohol abuse and chronic hepatitis. b. Cirrhosis has a long, latent period with vague gastrointestinal symptoms including anorexia, indigestion, nausea, vomiting, constipation, and diarrhea. MD0918 1-59 c. The latent period ends with the abrupt appearance of abdominal swelling and pain, hematemesis, and dependent edema. Skin turgor is poor, with accompanying dryness and pruritis. d. The condition advances to include symptoms that are a result of hepatic insufficiency, portal HTN, and hepatic encephalopathy. Such symptoms include: (1) Ascites. (2) Jaundice. (3) Bleeding tendencies (nosebleeds, bleeding gums, easy bruising). (4) Bleeding esophageal varices (2º portal HTN). (5) Limited thoracic expansion that interferes with gas exchanges (2 ascites). (6) Central nervous system disorders (2º hepatic encephalopathy) to include lethargy, slurred speech, mental changes, and peripheral neuritis. 1-60. DIETARY MANAGEMENT FOR THE PATIENT WITH CIRRHOSIS Nursing care of patients with cirrhosis requires careful assessment and monitoring of the patient's nutritional status. The nutritional therapy ordered by the physician must be strictly enforced in order to maintain an optimum physiologic state that will facilitate recovery. a. The diet should be high in calories. Total food intake should not be used to replace energy requirements. (1) The patient should be kept at a level of minimum activity to conserve (2) Nutrient consumption is necessary for the healing process to take place. energy. b. The amount of protein in the diet should be limited to that which the liver is able to handle. (1) The liver is the body's major organ of protein catabolism. (2) Protein catabolism yields ammonia, which is normally converted by the liver to the nontoxic substance called urea. (Urea is carried by the blood from the liver to the kidneys, where it is excreted in the urine.) MD0918 1-60 (3) Ammonia that cannot be converted to urea by the diseased liver will escape into the circulatory system. Excess blood ammonia can be very toxic to the brain. (4) Blood ammonia levels are monitored by the physician, who determines dietary protein allowances accordingly. c. The patient should be instructed to avoid table salt, salted butter and margarine, salty foods, and processed foods, which are generally high in sodium. (1) "Salt substitutes" such as lemon juice, herbs, and spices should be used to enhance food flavor. (2) being used. Commercial salt substitutes must be approved by the physician before d. If fluid retention (manifested by edema or ascites) occurs, the physician may order dietary restrictions such as: (1) Sodium restrictions. (2) Fluid restrictions. e. Intake of substances that are toxic to the liver must be stopped. (1) Alcohol. (2) Drugs. f. A patient with cirrhosis will experience anorexia, and will require encouragement and even enticement to eat the prescribed, well-balanced diet. (1) Consider individual patient preferences, and ask the dietician to use preferred foods in the menu. (2) Small, frequent meals may be better tolerated than three large meals. (3) Make meal times as pleasant and leisurely as possible. g. Ensure that the patient takes the prescribed supplementary vitamins. A diseased liver cannot effectively store or activate vitamins. Supplementary vitamins prescribed may include the following: (1) Vitamin K. Vitamin K, known as the anti-hemorrhagic vitamin, is a fatsoluble vitamin normally stored in the liver. It is essential for the synthesis of prothrombin, a substance necessary for normal blood clotting. MD0918 1-61 (2) Thiamine. Thiamine, also known as vitamin B1, is a water-soluble vitamin not stored in the body. It must be consumed in food or in supplement form. Thiamine is required for normal carbohydrate metabolism and nerve conduction. Deficiencies lead to the syndromes of beriberi and polyneuritis. (3) Folate. Folate (folic acid) is a water-soluble vitamin necessary for the normal production of white and red blood cells. Folate deficiency anemia is the usual result of insufficient folic acid. (4) Iron. Although iron is a mineral and not a vitamin, it is included in this discussion because it is often prescribed along with folic acid to combat anemia inpatients with cirrhosis. (5) Vitamin C. The exact mechanisms of vitamin C are not fully understood, but it has been proven that vitamin C is effective in helping the body to fight infection and to speed healing. 1-61. NURSING IMPLICATIONS FOR THE PATIENT WITH CIRRHOSIS a. Assess for Fluid Retention. (1) Weigh daily. (2) Measure abdominal girth daily. (3) Observe and record accurate intake and output. (4) Observe for the presence of edema. b. Observe for Bleeding Tendencies. (1) Monitor vital signs frequently. (2) Assess for anxiety, weakness, or abdominal fullness that may indicate internal bleeding. (3) Observe and test stool, urine, and emesis for the presence of blood. (4) Observe the gums for evidence of bleeding. (5) Observe the skin for petechiae and bruising. c. Manage Bleeding Tendencies. (1) MD0918 Provide a safe environment to prevent injuries. 1-62 (2) Implement the use of a soft bristle toothbrush. (3) Implement the use of an electric razor for shaving instead of a blade (4) Use small gauge needles for drawing blood and starting IVs. (5) Caution the patient against forceful nose blowing to prevent epistaxis. razor. d. Provide Skin Care. (1) Use gentle cleansers to decrease skin irritation. (2) Use soothing lotions to control the itching that occurs as a result of bile salt retention. (3) Administer prescribed medications for pruritis. (4) Keep the patient's fingernails short to prevent scratching the skin. e. Observe and Assess for Indications of Hepatic Encephalopathy. (1) Arouse the patient at intervals and assess level of consciousness and orientation to place and time. (2) Observe for personality changes or mental changes. (3) Observe for signs of increasing lethargy. (4) Observe for signs of neuromuscular dysfunction. (5) Observe for evidence of hallucinations. f. Provide Emotional Support. (1) The patient will experience fatigue and malaise as a normal consequence of the illness. Assure him that this is normal and will eventually resolve. (2) Educate the patient and his family about the nature of the illness so that they will be better able to cope. 1-62. PORTAL HYPERTENSION AND ESOPHAGEAL VARICES a. Portal hypertension (elevated pressure in the portal vein) is a result of the increased resistance in blood flow through the portal venous circulation. This disorder is almost always the result of cirrhosis. MD0918 1-63 b. All blood returning to the heart from the spleen, stomach, pancreas, and intestines is detoured through the liver by the portal vein. Branches of the portal vein carry the blood into the functional units (lobules) of the liver. Here, poisons are extracted by the hepatic cells to be stored or detoxified. Nutrients just absorbed from the intestines are extracted and stored or utilized in anabolism. c. As portal pressure increases, blood backs up into the spleen and bypasses the liver, returning to the right atrium via collateral circulation. The result is splenomegaly, ascites, and varicosities of the collateral veins (esophageal and gastric varices). d. Esophageal and gastric varices are dilated, tortuous veins in the submucosa of the esophagus and stomach. Prone to rupture, esophageal varices may require immediate emergency treatment to control hemorrhage and prevent shock and death from hypovolemia. e. Nursing Implications. A patient with bleeding esophageal varices is to be considered in critical condition. Nursing management is aimed at assisting the physician in controlling bleeding and preventing shock and death. (1) Monitor V.S. closely and assess level of consciousness frequently. (2) Observe for signs of hypovolemic shock. (3) Measure and record I&O. (4) Administer IVF's and blood, as ordered. (5) Initiate balloon tamponade, as ordered. (Refer to figure 1-7 and para 1-26f, Sengstaken-Blakemore Tube.) (6) Administer iced saline lavage, as ordered. (Refer to para 1-38, Lavage.) (7) Offer reassurance and moral support to the patient and his family. (a) Assess the patient's mental status and coping mechanisms. (b) Reinforce teaching and explanations. (c) Report to the professional nurse any observations about the needs of the patient and his family. MD0918 1-64 Figure 1-7. Sengstaken-Blakemore tube. 1-63. GALLBLADDER DISEASE a. Cholelithiasis, the presence of calculi or stones in the gallbladder, is the cause of 90 percent of gallbladder disease. Their presence indicates some dysfunction of the gallbladder. Gallstones are composed of cholesterol, calcium, bilirubin, and inorganic salts. b. Cholecystitis, inflammation of the gallbladder, is usually associated with gallstones. c. Biliary colic, or a "gallbladder attack," is the result of contracture of the gallbladder. Stimulated by fat (from a meal), the gallbladder attempts to release bile, but is unable to do so because of some obstruction. In most cases, this obstruction is due to gallstones. Symptoms of the classic gallbladder attack include the following: (1) MD0918 Acute RUQ pain. Pain may radiate to the chest or the upper back. 1-65 (2) Nausea and vomiting. (3) Diaphoresis. (4) Chills. (5) Low-grade fever. d. Nursing implications. (1) Dietary modifications that decrease fat consumption are used to prevent attacks. (Fatty foods are likely to precipitate an attack.) (2) Surgery (usually cholecystectomy) is the treatment of choice. Nursing care will therefore focus on postoperative care and observation. Section VIII. DIABETES 1-64. DEFINITION a. Diabetes mellitus is a metabolic disorder in which the body loses its ability to properly oxidize carbohydrates. It is caused by a deficiency in the production of insulin by the pancreas. Insulin is a hormone produced by the beta cells of the Islets of Langerhans within the pancreas. b. The body gets its supply of energy from glucose, a product of carbohydrate metabolism. Normally, glucose is stored in the liver, in the form of glycogen, and released into the blood stream when the level of glucose in the circulating blood decreases. c. Insulin regulates glucose metabolism. Without insulin, blood glucose cannot pass through the capillary membrane to be used by the cells for energy, nor can it be stored by the body. When the body's cells are unable to use glucose, it accumulates in the blood (hyperglycemia) and spills over into the urine (glycosuria). When the body cannot store glucose for release when required, blood glucose deficiency (hypoglycemia) will occur. 1-65. CLASSIFICATION Diabetes mellitus is categorized according to the type of diabetes and the intensity of the carbohydrate intolerance. a. Type I: Insulin Dependent Diabetes Mellitus. (1) Insulin Dependent Diabetes Mellitus (IDDM) is characterized by onset in youth (age 20 or younger), although it may occur at any age. Insulin Dependent Diabetes Mellitus has previously been referred to as "juvenile diabetes." MD0918 1-66 (2) Insulin Dependent Diabetes Mellitus is characterized by low serum insulin levels due to an insulin deficiency. (3) Treatment consists of parenteral administration of insulin along with diet therapy. b. Type II: Non-Insulin Dependent Diabetes Mellitus. (1) Non-Insulin Dependent Diabetes Mellitus (NIDDM) is characterized by onset after the age of 40, although it may occur in younger persons as well. Non-Insulin Dependent Diabetes Mellitus is also known as "adult onset diabetes mellitus" (AODM). (2) or elevated. (3) Insulin production does not stop, but insulin levels may be low, normal, Sixty to 90 percent of Type II diabetics are overweight or obese. (4) Treatment consists of diet therapy, weight control measures, and the use of oral hypoglycemic medications if necessary. 1-66. SYMPTOMS Diabetes mellitus may be discovered during a physical examination when the patient complains of any of the following symptoms: a. Visual disturbances. b. Weakness and fatigue. c. Unexplained weight loss. d. Recurrent infections. e. Polyuria (excessive urination). f. Polydipsia (excessive thirst). g. Polyphagia (excessive eating). h. Symptoms of peripheral vascular disease. MD0918 (1) Diminished or absent pulses. (2) Skin that is thin and shiny. (3) Loss of hair on the dorsum of the foot. 1-67 (4) Decreased skin temperature. (5) Decreased capillary and venous filling. (6) Thick and ridged toenails. 1-67. DIAGNOSIS Simple screening tests that determine blood and urine glucose levels are used to aid in the diagnosis of diabetes mellitus. a. Fasting Blood Sugar. The fasting blood sugar (FBS) test measures the amount of sugar present in the blood after a patient has been fasting for a prescribed amount of time (generally 6-8 hours). An elevated fasting blood sugar level indicates the possibility of diabetes and the need for further investigation. b. Two-Hour Post-Prandial Blood Sugar. The two-hour post-prandial blood sugar (two percent ppBS) is a common diagnostic test to determine how well sugar is metabolized by the body. A patient remains fasting for 6-8 hours, a fasting blood specimen is drawn, and the patient is given a high carbohydrate meal. The meal contains a measured amount of carbohydrates. The patient must eat the entire meal within 15 minutes. Two hours after completion of the meal, another blood sugar level is drawn. In a person with normal metabolism, the blood sugar level has returned to normal range within two hours after the meal. An elevated blood sugar level indicates the possibility of diabetes and the need for further investigation. c. Glucose Tolerance Test. The glucose tolerance test (GTT) test is performed when a patient is found to have an elevated blood sugar level or sugar in the urine. This test is used to evaluate the body's use of glucose. During this test, blood and urine specimens are collected at timed intervals following the ingestion of a measured amount of glucose. The test normally proceeds in this manner: (1) The patient may be required to follow a prescribed high carbohydrate diet for three days prior to the test date. (2) The patient must fast for the required period of time prior to the start of the test, normally 6-12 hours. (3) Blood and urine are collected while the patient is fasting. (4) The patient is given a measured amount of glucose solution to drink, which must be consumed quickly. (5) Blood and urine are collected at timed intervals after the ingestion of the glucose drink. Intervals are normally at 1/2 hour, 1 hour, 2 hours, and even up to 6 hours following the ingestion of the glucose drink. MD0918 1-68 (6) The patient is permitted to take water only during the duration of the test. This is done to make the patient more comfortable and to facilitate voiding for the urine specimen collection. d. Urinalysis. Urine tests are used to detect the presence of glucose or acetone in the urine. Normally, urine contains no sugar or acetone. When excess sugar accumulates in the blood, it "spills over" into the urine during filtration of the blood by the kidneys. Urine must be tested for sugar and acetone on a regular schedule. This is normally done IAW ward SOP or the physician's orders. Common times are prior to each meal and at bedtime. (1) Urine. Always use freshly voided urine for testing. Stale urine will not provide accurate results. Do not use urine that has been standing in a urinary drainage bag. (2) Double Void. For complete accuracy, the "double void" method should be used when testing urine. Instruct the patient to empty his bladder, wait 15-30 minutes, and void again. Test the urine from the second voiding. (3) Clinitest tablets. Place 10 drops of water into a test tube. Add 5 drops of fresh urine. Drop in one of the clinitest tablets. Wait 15 seconds and compare the color of the solution in the test tube to the appropriate color chart (enclosed in the kit) to determine the concentration of sugar present. (a) This chemical reaction is heat producing. Always use a test tube rack to hold the tube. Never hold it in your hand. (b) Document the test results in the patient's record. (4) Acetest tablets. Place one drop of fresh urine onto an acetest tablet. If the tablet turns purple, the test is positive for the presence of acetone. Document the test results in the patient's record. (5) Ketodiasti x. Test strips measure glucose and acetone at the same time. Dip one ketodiastix quickly in the fresh urine. Time the readings according to the instructions provided and use the color chart on the ketodiastix bottle to determine the presence of acetone and the concentration of glucose. Document the results in the patient's record. 1-68. DIET a. Since diabetes is a disorder of the body's metabolism, the diabetic must maintain a carefully balanced routine of diet, exercise, and medication (insulin or oral hypoglycemic agents). Diet is the most important factor in the control of diabetes. MD0918 1-69 (1) Diet is calculated by the patient's physician and is based on the age, sex, health, activity level, and dietary habits of the patient. (2) Diet consists of controlled amounts of carbohydrate, protein, and fat calories. (3) Dietary allowances are normally divided among 3 meals and one or more snacks. For example: breakfast, lunch, dinner, and an evening snack. b. The American Diabetic Association (ADA) has devised a diet using six "exchange lists" that outline equivalent foods that may be exchanged for one another. This allows the patient a variety of food selections and menu choices in meal planning. (1) Foods may be exchanged within each list, but foods cannot be exchanged from one list to another. (2) The six exchange lists are: (a) Milk. (b) Vegetables. (c) Fruits. (d) Breads. (e) Meats. (f) Fats. c. Illness, injury, infection, pregnancy, stress, overexertion, and strenuous exercise are all capable of disrupting the metabolic balance of the diabetic. Therefore, alterations in dietary requirements and medication dosages will be necessary. The status of the hospitalized diabetic patient should be evaluated regularly, as the metabolic balance may get out of control rapidly. Evaluation is routinely accomplished by scheduled testing of the patient's urine, and occurs as a part of daily nursing care. d. Nursing implications. (1) Test urine on schedule and use the correct procedure. (Refer to para 1-1-67d.) (2) Reinforce dietary instruction provided by the dietician. Emphasize the consequences of deviation from the prescribed diet. MD0918 1-70 (3) Note and document what the patient has eaten at each meal. Failure to consume the full meal provided will result in a metabolic imbalance that could lead to a hypoglycemic reaction. (4) Do not permit the patient to eat anything other than his prescribed diet. Extra, unauthorized food may precipitate a hypoglycemic reaction. 1-69. ORAL HYPOGLYCEMIC AGENTS a. Oral hypoglycemics act by stimulating the pancreatic beta cells to produce more insulin or by increasing the effectiveness of existing insulin. b. Oral hypoglycemics are NOT a form of oral insulin. Oral hypoglycemic agents require a pancreas with functional beta cells. This is why oral hypoglycemics do not work for all patients with diabetes. c. Oral hypoglycemics act within an hour after ingestion and last for 24 hours. d. Examples of oral hypoglycemic agents include Orinase, Diabinese, and Tolinase. 1-70. INSULIN a. When insulin is present within the blood, glucose is able to pass through the capillary membrane and into the body's cells to be utilized for energy. b. Insulin is measured in units. The most common strength of insulin is "U-100." This means that 1 ml of the solution contains 100 units of insulin. U-100 syringes (fig. 1-8) are designed specifically for the administration of U-100 insulin. Use of other syringes, not calibrated in units, is a dangerous practice that allows for medication error. c. Insulin is routinely refrigerated to prolong shelf life, but should be at room temperature when administered to prevent irritation of skin tissue. d. Insulin is classified according to its action. (1) Rapid-acting insulin includes regular and semilente. (a) Onset of action occurs 1/2 to 1 hour after administration. MD0918 1-71 Figure 1-8. Insulin syringe. (b) Peak of action occurs 2 to 4 hours after administration. (c) Duration of action is relatively short (about 6 hours for regular and about 14 hours for semilente). (2) Intermediate-acting types are NPH and lente. (a) Onset of action occurs 2 hours after administration. (b) Peak of action occurs 6 to 12 hours after administration. Lente peaks several hours later than NPH. (c) Duration of action is of medium length (24 to 28 hours for NPH and 24 to 48 hours for lente). (3) Long-acting types are protamine zinc and ultra lente. (a) Onset of action occurs 6 to 7 hours after administration. MD0918 (b) Peak of action occurs 16 to 24 hours after administration. (c) Duration of action is long, about 36 hours. 1-72 1-71. INSULIN "COVERAGE" a. When a diabetic is hospitalized, the combination of illness, stress, and change in routine may cause an insulin imbalance. Therefore, the patient will normally have routine urine (or blood) testing for sugar and acetone. If sugar is "spilled" into the urine, additional insulin ("insulin coverage") is given in addition to the patient's regular dose. b. This coverage is commonly ordered on a "sliding scale." That is, the physician will order additional insulin in correlation with the amount of sugar present in the urine. For example: no sugar = no insulin, 1+ sugar = 5 units regular insulin, 2+ sugar = 10 units regular insulin, 3+ = 15 units regular insulin, 4+ = 20 units regular insulin. As you see, the additional coverage is increased as the amount of sugar in the urine increases. 1-72. NURSING IMPLICATIONS FOR ADMINISTRATION OF INSULIN a. Be certain to give the correct type of insulin. b. Prepare the correct dosage. Have another nurse double-check the dose before you administer the injection. c. Use the correct syringe. Never use a regular syringe for insulin. Use a syringe calibrated in "units." d. Before drawing up the insulin, gently "roll" the bottle between your palms to mix and warm the solution. e. Eliminate all air bubbles from the syringe. One small air bubble may displace 2 or 3 units of insulin. f. Cleanse the skin with alcohol and allow to dry. This helps avoid pitting of the skin. g. Give the injection subcutaneously. Rotate the injection site with each dose. (Rotating the sites prevents tissue necrosis.) Refer to figure 1-9 for injection sites. h. Always check to see whether the patient is and has been eating his normal diet. (1) Administration of the regular dosage of insulin when the patient's intake of food has been decreased or withheld could cause the blood sugar level to drop too much. MD0918 1-73 Figure 1-9. Sites for injection. (2) A patient who is experiencing vomiting will require adjustment of the insulin dosage. (3) A patient who is being held NPO for procedures or tests should not receive his regular insulin dosage. This could precipitate a hypoglycemic reaction. Notify the physician for instructions. Routinely, insulin is withheld until the procedure is completed and the patient is permitted to eat. 1-73. HYPOGLYCEMIA a. Hypoglycemia, also referred to as insulin reaction or insulin shock, is caused by too little sugar in the blood (in relation to the amount of insulin in the blood). This situation may be caused by any of the following: MD0918 1-74 (1) Missed or delayed meals and/or snacks. (2) Over exertion or strenuous exercise. (3) Excessive vomiting. (4) Insulin overdose. b. Signs and symptoms of hypoglycemia include the following. Onset may be quite sudden. (1) Pale, cool, clammy skin. (2) Cold sweat. (3) Nervousness, trembling. (4) Dizziness. (5) Weakness, fatigue. (6) Tachycardia. (7) Hypertension. (8) Hunger, often quite sudden. (9) Low blood sugar level. (10) Small urine output (oliguria). (11) Urine frees of sugar and acetone. c. Pathophysiology. (1) The symptoms of hypoglycemia are a reflection of the effects of a low blood glucose level upon the central nervous system, along with the release of epinephrine. (2) Decreasing uptake of glucose by the CNS and lowered utilization of oxygen by the brain will result in permanent damage to CNS neurons. (3) The primary factor in prevention of the problems of hypoglycemia is early recognition of the symptoms. Initiation of treatment can eliminate the reaction and its consequences. MD0918 1-75 d. Nursing management. (1) Administer glucose immediately. (a) A conscious patient may be given some form of sugar by mouth. (Table sugar, orange juice, cola, honey, syrup, jelly, or candy.) (b) An unresponsive patient may be given "instant glucose," a form of rapidly absorbed glucose that is squeezed out of a tube into the patient's mouth for oral absorption. (c) An intravenous infusion of dextrose in water should be initiated if possible. (2) Have the patient stop all activity and rest to conserve energy. (3) Notify the physician. (4) Draw blood for a glucose level. (5) Monitor vital signs and level of consciousness carefully. (6) Document all information in the patient's clinical record. 1-74. HYPERGLYCEMIA AND KETOACIDOSIS a. Hyperglycemia and ketoacidosis (also referred to as diabetic coma) result from too much sugar in the blood (in relation to the amount of insulin). This situation can be caused by eating more food than allowed, taking too little or no insulin, illness, or infection. Remember that insulin regulates glucose metabolism and that insufficient insulin will cause an inability to utilize the glucose. Glucose accumulates in the blood (hyperglycemia) and is unable to be used as a source of energy due to the lack of insulin. When glucose cannot be utilized, the body must break down fats and proteins for energy. If too many by-products of fat and protein metabolism (ketones) accumulate in the body, an acid-base imbalance will occur. This condition is called acidosis, or ketoacidosis. If this condition is left undetected or untreated, coma and death will result. b. Signs and symptoms of diabetic ketoacidosis include the following. Onset is gradual, occurring over several hours to several days. MD0918 (1) Hot, dry, flushed skin. (2) Absence of sweating. (3) "Fruity" odor to breath (acetone). 1-76 (4) Slow and labored respirations, air hunger. (5) Anorexia and nausea. (6) Tachycardia. (7) Hypotension. (8) Polydipsia (excessive thirst). (9) Large and frequent urine output (polyuria). (10) Presence of sugar and acetone in the urine. (11) High blood sugar level. c. Pathophysiology. (1) As mentioned above, when glucose cannot be utilized, fats and proteins are broken down for energy. Their by-products (ketones) accumulate in the blood. Ketone bodies are strong acids that can lower blood pH, producing metabolic acidosis (ketoacidosis). (2) Electrolyte disturbances occur as a result of polyuria, dehydration, and the alteration in pH. (3) Hypothermia and a lack of pyrexial response (fever) to infection may occur. (4) Level of consciousness will begin to alter (probably due to diminished brain perfusion of oxygen), resulting in coma and death if the condition is left untreated. d. Nursing management. (1) Administer insulin. (The physician will usually order administration of a low dose of regular insulin intravenously.) MD0918 (2) Draw blood for a glucose level. (3) Monitor vital signs and level of consciousness carefully. (4) Force fluids (usually IV). (5) Insert a retention catheter to monitor urine output. (6) Observe for respiratory changes. 1-77 (7) Observe accurate I & O. (8) Document all information in the patient's clinical record. 1-75. EDUCATION OF PATIENT AND FAMILY The goal of education is to aid the patient and his family in understanding the nature of the disease, the control of the disease, and the prevention of complications. a. The patient must understand that diabetes is a life-long disease that is controlled, not cured. (1) Explain normal and abnormal physiology of glucose metabolism in a manner that is understandable to the patient. (2) Explain the signs and symptoms that occur, and why they occur. b. The patient must understand and comply with diet therapy and weight control. (1) Explain the relation between obesity and diabetes. (2) Explain the effects of a controlled and uncontrolled diet on blood sugar (3) Explain the purpose of a regulated diet in relation to blood sugar. level. (4) Teach the patient how to utilize the food exchange lists within his prescribed diet. (5) Caution the patient about the consequences of deviation from the prescribed diet. c. The patient must understand the importance of exercise and activity in relation to blood sugar level. (1) Explain that activity/exercise requires fuel (glucose) and will lower the blood sugar level. (2) Activity or exercise that is more strenuous than the patient's normal routine may cause blood sugar to drop dangerously low. (3) Extra activity or exercise should be planned for in advance. Insulin dosage may need to be decreased, or food intake increased. (4) MD0918 Explain that regular exercise improves circulation and general health. 1-78 d. The patient must understand the purpose, actions, and side effects of prescribed medication (insulin or oral hypoglycemic agents). (1) Explain the type, action, dosage, route and times of administration, and side effects of the medication prescribed. (2) Demonstrate and discuss the proper procedures for storage and administration of medications. e. The patient must understand the importance of regular urine testing. (1) Explain that the purpose of regular urine testing is to detect the presence of glucose and/or ketones "spilled over" into the urine. (2) Demonstrate and discuss the correct procedure for collecting and testing a urine specimen. (3) Explain how to interpret the test results, along with actions to be taken for the different results. (4) Stress the importance of documentation of the results and actions taken. Encourage good record keeping. f. The patient must be made aware of the complication of diabetic neuropathy. (1) Neuropathy is a common complication of diabetes that causes impaired sensation in the extremities, especially the feet. (2) Damaged nerves lose their ability to adequately conduct impulses. Because of this, the diabetic may not feel an injury. (3) Instruct the patient to be cautious due to the decreased sensation. Emphasize the following: (a) Wear only well fitted shoes. (b) Never walk bare-footed. (c) Do not use heating pads or hot-water bottles. The patient could sustain a heat injury due to decreased sensation. g. The patient must be made aware of the complication of peripheral vascular disease (PVD). (1) Another common complication of diabetes, PVD causes impaired circulation, which results in decreased oxygen perfusion to body tissues. MD0918 1-79 (2) Teach the patient to recognize the signs and symptoms of PVD. (a) Decreased skin temperature. (b) Decreased venous and capillary filling. (c) Diminished or absent pulses. (d) Skin that appears thin and shiny. (e) Loss of hair on the back of the hand or dorsum of the foot. (f) (3) Thick and ridged toenails. Discuss methods of promoting good circulation. (a) Daily exercise to improve circulation. Walking is the best exercise. (4) (b) Keep feet warm. Use socks, blankets, etc. (c) Do not sit or lie with legs crossed. (d) Do not use stockings or garters with tight elastic bands. Instruct patient to thoroughly inspect and properly care for his feet. (a) Soak feet for about five to ten minutes each day to keep the skin and nails soft. (b) Dry feet thoroughly and apply lotion. (c) Inspect the feet for cuts, scrapes, sores, blisters, or other skin changes. (d) Emphasize that no foot problem should be self-treated. The patient must always seek the care of a physician. h. The patient must be made aware of the complication of infection. (1) Impaired circulation and decreased oxygen to body tissue results in slow and lengthy healing times as well as an increase in the likelihood of serious infection. MD0918 (2) Teach the patient to observe for signs of infection. (3) Teach the patient to prevent infection. 1-80 (a) Never self-treat open sores. (b) Use extreme care and proper technique when performing nail care. Use only a proper nail clipper and cut straight across the nail. (c) Never pick at sores, scabs, cracked skin, or ingrown nails. (4) Explain that the fever of an infection will cause an increase in the metabolic rate, which will cause a change in caloric requirements. The patient with fever should always consult with his physician. i. The patient and his family must be aware of the signs and symptoms as well as emergency treatment for the diabetic emergencies of ketoacidosis and insulin shock. As discussed in paragraphs 1-73 and 1-74, reinforce the following: (1) Causes. (2) Signs and symptoms. (3) Emergency treatment. (4) Prevention. 1-76. CONCLUSION a. This lesson has introduced the basic nursing care techniques and procedures involved in the nursing care related to the gastrointestinal system. b. Review the lesson objectives once again. If you feel confident that you have achieved the lesson objectives, complete the exercises at the end of this lesson. c. If you do not feel that you have met the lesson objectives, review the necessary material before you attempt the end of lesson exercises. Continue with Exercises MD0918 1-81 EXERCISES, LESSON 1 INSTRUCTIONS: Answer the following exercises by marking the lettered response that best answers the question, by completing the incomplete statement, or by writing the answer in the space provided at the end of the question. After you have completed all of these exercises, turn to "Solutions to Exercises" at the end of the lesson and check your answers. For each exercise answered incorrectly, reread the material referenced with the solution. 1. The mechanical portion of digestion includes chewing, ____________________, __________________, and ___________________. 2. ______________________ is the major carbohydrate used for fuel. 3. The first accessory organ that enters the digestive process is the _____________________ . 4. The wavelike action produced by contraction of the muscular wall of the alimentary canal is called ___________________. 5. The 3 parts of the small intestine are the ________________________________, ______________________________, and ______________________________. 6. Most of the absorption of food takes place in the __________________________. 7. Bile is secreted by the __________________________ and stored in the ________________________. 8. Water and electrolytes are absorbed in the ______________________________. 9. Physical examination of the abdomen involves ____________________________ ______________________________, and ______________________________. MD0918 1-82 10. The sigmoid colon is located in which abdominal quadrant? ________________ __________________________. 11. The hepatic flexure of the colon is located in the _________________________ quadrant. 12. When examining the abdomen, which should be done first palpation or auscultation? ______________________ . 13. Inability to relax the abdominal muscles is called _________________________. 14. A side effect of the use of contrast medium is ____________________________. 15. _________________________ is a potential complication of endoscopic procedures. 16. Gavage, lavage, and relief of distention are all reasons for__________________ _________________. 17. A 10-foot long, double lumen, single balloon, gastrointestinal tube used for small bowel suction is the _______________________________________________. 18. The tube used in the treatment of esophageal varices is the__________________ ________________________. 19. When inserting a nasogastric tube, the patient should first tilt his head __________________, then move it __________________ as the tube curves into the pharynx. 20. When inserting a nasogastric tube, if the patient coughs or chokes, you should _________________________. MD0918 1-83 21. Changing the patient's position and repositioning the nasogastric tube are nursing measures used to __________________________________________________. 22. Before irrigating a nasogastric tube, you must_____________________________ _________________________________________________________________ 23. To clear a feeding tube after administering a gavage feed, you should________ ___________________________________. 24. When a physician orders "lavage until clear," he means ___________________ ____________________________________. 25. In a patient with a transverse colostomy you would expect the usual feces to be: a. Solid. b. Mushy. c. 26. Fluid. Unless contraindicated, colostomy irrigation should be done: a. In the morning. b. After dinner. c. At the same time of day the patient used to move his bowels. 27. Most ileostomies are performed because of _____________________________ 28. You should never apply heat to the abdomen of a patient with appendicitis because _________________________________________________________. MD0918 1-84 29. When measuring the abdominal girth of a patient, you should do what to maintain consistency and accuracy? _________________________________________________________________ _________________________________________________________________ _________________________________________________________________ 30. Inflammation of the liver with destruction of the liver cells is called _____________________________. Check Your Answers on Next Page MD0918 1-85 SOLUTIONS TO EXERCISES, LESSON 1 1. Swallowing, peristalsis, defecation. (para 1-1b) 2. Glucose. (para 1-1c(1)) 3. Salivary glands. (para 1-4b) 4. Peristalsis. (para's 1-6, 1-8b) 5. Duodenum, jejunum, ileum. (para 1-8a) 6. Small intestine. (para 1-8b) 7. Liver, gallbladder. (para 1-8c(2)) 8. Large intestine. (para 1-9c) 9. Inspection, auscultation, palpation. (para 1-16a) 10. LLQ. (figure 1-3) 11. RUQ. (figure 1-3) 12. Auscultation. (para's 1-18, 1-19) 13. Rigidity or guarding. (para 1-19a) 14. Constipation. (para 1-20c(1)) 15. Accidental perforation of tissue. (para 1-23c(1)) 16. Gastrointestinal intubation. (para 1-25a) 17. Miller-Abbot tube. (para 1-26d) 18. Sengstaken-Blakemore tube. (para 1-26f) 19. Back, forward. (para 1-28g(1), (2)) 20. Remove the tube. (para 1-28g) 21. Clear an obstruction in an N-G tube. (para 1-31g) MD0918 1-86 22. Check tube placement to be sure it is in the stomach. (para 1-35c) 23. Instill 30-50 ml of plain water. (para 1-37b(7)) 24. Lavage until stomach contents returns clear. (para 1-38c(1)) 25. b (figure 1-5) 26. c (para 1-45a) 27. Inflammatory bowel disease. (para 1-46a) 28. It may cause the appendix to rupture. (para 1-51c(4)) 29. Use same tape measure, same patient position, same body location, and do it at same time each day. (para 1-53e(1)) 30. Hepatitis. (para 1-55) End of Lesson 1 MD0918 1-87 LESSON ASSIGNMENT LESSON 2 Nursing Care Related to the Urinary System. TEXT ASSIGNMENT Paragraphs 2-1 through 2-40. LESSON OBJECTIVES After completing this lesson, you should be able to: 2-1. State the functions of the urinary system. 2-2. List the anatomical parts of the urinary system. 2-3. Identify the anatomical parts of the kidney. 2-4. Name the functional unit of the kidney. 2-5. Define polyuria. 2-6. Define oliguria. 2-7. Define anuria. 2-8. Define dysuria. 2-9. Define hematuria. 2-10. List two nursing implications associated with the care of a patient undergoing a cystoscopy. 2-11. List the steps for collection of a clean-catch urine specimen. 2-12. List the steps for collection of a 24-hour urine specimen. 2-13. List five purposes for cauterization of the urinary bladder. 2-14. List three general nursing implications associated with the insertion of a urinary catheter. 2-15. List the steps for insertion of a retention catheter. MED918 2-1 2-16. State the purpose of a closed urinary drainage system. 2-17. List the steps for collecting a sterile urine specimen from an indwelling catheter. 2-18. List three purposes for continuous bladder irrigation. 2-19. List the steps for performing a continuous bladder irrigation. 2-20. State the route of entry of bacteria in most urinary tract infections. 2-21. List three nursing implications associated with care of a patient with a urinary tract infection. 2-22. Define pyelonephritis. 2-23. List three factors, which may precipitate urolithiasis. 2-24. List the symptoms associated with urolithiasis. 2-25. Define glomerulonephritis. 2-26. List at least three nursing implications associated with the care of a patient with glomerulonephritis. 2-27. Explain the purpose of restricting dietary protein in patients with renal disease. 2-28. Define renal failure. 2-29. List at least three nursing implications associated with care of a patient with renal failure. SUGGESTION MED918 After studying the assignment, complete the exercises at the end of this lesson. These exercises will help you to achieve the lesson objectives. 2-2 LESSON 2 NURSING CARE RELATED TO THE URINARY SYSTEM Section I. ANATOMY AND PHYSIOLOGY 2-1. INTRODUCTION a. The primary function of the urinary system is to control the composition, volume, and pressure of the body's fluids by regulating excretion of water and solutes. b. Circulating blood is filtered by the kidneys, where nonessential solutes are removed or "cleared" from the blood. Essential chemicals and water are restored to the blood in accordance with the body's homeostatic requirements. c. Metabolic waste products, foreign substances, and water are removed from the body in the form of urine. d. The urinary system consists of two kidneys, two ureters, one urinary bladder, and one urethra (figure 2-1). Figure 2-1. The urinary system. MED918 2-3 2-2. THE KIDNEYS a. The kidneys (figure 2-2) are a pair of bean-shaped organs about four inches long, two inches wide, one-inch thick, and weighing four to six ounces each. b. One kidney is located on each side of the body. They are pressed against the posterior abdominal wall at about the level of the first lumbar vertebrae. c. The medial side of each kidney is concave and has a central notch called the hilum. Here, the renal artery enters the kidney, and the renal vein and ureter exit the kidney. Nerves and lymphatic vessels also pass through the hilum. d. The kidneys are enclosed by the renal capsule. Directly beneath the capsule lies a reddish area called the renal cortex. The cortex contains millions of microscopic filtration plants called nephrons. Nephrons are the functional units of the kidney. Figure 2-2. The kidney. MED918 2-4 e. Beneath the cortex is a reddish-brown area called the renal medulla. Within the medulla are striated areas called the renal pyramids. Urine collecting tubules within the pyramids cause the striated appearance. f. The collecting tubules terminate at the pyramid's point, emptying the urine into the renal pelvis. Along the edges of the renal pelvis are cup-like projections called the minor and major calyces. Each minor calyx collects urine from the pyramid and empties it into a major calyx. The major calyces empty into the renal pelvis. 2-3. URETERS The pelvis of each kidney is drained by a ureter, a muscular tube extending from the hilum to the posterior portion of the urinary bladder. Ureters are smooth muscle structures, and urine is passed through each ureter by peristalsis. Drop by drop, urine passes into the bladder. Ureters are about 15 to 18 inches in length and about 1/5 inch in diameter. 2-4. URINARY BLADDER The urinary bladder, a muscular sac located in the lowest part of the abdominal cavity, stores urine. Normally it holds 300 to 500 ml. The bladder is emptied by contraction of its muscular walls that force urine out through the urethra. 2-5. URETHRA The urethra is the tube that carries urine from the urinary bladder to the external opening, the urinary meatus. a. In the male, the urethra will vary in length. Including the portion within the body, it is approximately 6 to 7 1/2 inches in length. It is divided into three areas: the prostatic area, which passes through the prostate gland; the membranous area, beneath the prostate; and the penile area, which passes through the penis. b. The female urethra, about 1 1/2 inches long, extends from the bladder to the meatus, which is located above the vaginal opening. 2-6. URINATION Urination is the discharge or voiding of urine. It is done by a contraction of the bladder and relaxation of the sphincters. In the adult, the act of voiding, although dependent on involuntary reflexes, is partly under voluntary control. Voluntary contraction of abdominal muscles usually accompanies and aids urination. MED918 2-5 2-7. URINE FORMATION a. Urine is formed by the kidneys in millions of tiny filtration plants called nephrons. The nephrons receive and filter all the blood in the body about once every 12 minutes. b. Each nephron (figure 2-3) is composed of 3 parts: the glomerulus, the capsule, and the tubule. Each part is essential in the filtration, re-absorption, and excretion processes. Figure 2-3. The kidney nephron. MED918 2-6 c. Circulating blood enters the cluster of capillaries known as the glomerulus. Water, electrolytes, and small organic molecules are filtered from the capillary blood and pass into the capsule. Blood cells and large protein molecules cannot pass through the glomerulus into the capsule. d. The "filtrate" (water and solutes filtered from the blood) passes from the capsule into the tubule. In the tubule, water and usable chemical products are reabsorbed. e. The final waste product, urine, drains from the last loop of the nephron's tubule into a collecting tubule for drainage into the renal pelvis. 2-8. CHARACTERISTICS OF URINE a. Composition. Normal urine is composed of about 95 percent water and 5 percent solutes. Normal solutes found in urine include: (1) Urea. (2) Creatinine. (3) Uric acid. (4) Ketone bodies. (5) Potassium. (6) Sodium. (7) Chloride. b. Specific Gravity. The specific gravity of urine depends upon the amount of solutes present. The greater the concentration of solutes, the higher the specific gravity. Normal range for specific gravity is from 1.008 to 1.030. c. Appearance. Urine is a transparent (clear) fluid. Color varies from pale yellow to dark amber, depending upon its concentration. (Concentration is the ratio of solutes to water.) (1) Dilute urine may be pale, straw colored, or even appear colorless. (2) Concentrated urine appears highly colored (for example, bright yellow or deep amber). (3) Turbid (cloudy) urine is usually considered abnormal. It may be the result of blood, pus, sperm, or bacteria present in the urine. MED918 2-7 d. Odor. Normal, freshly voided urine has a faint aromatic odor. Old, stale urine develops a strong ammonia odor from chemical breakdown. (1) A strongly offensive odor may indicate the presence of bacteria. (2) Diet selection can alter normal odor. Asparagus is a good example. (3) Some medications may alter the normal odor of urine. Ampicillin is one example. e. Amount. The average, normal adult will excrete approximately 1,500 to 2,000 ml of urine each day (every 24 hours). This will vary with fluid intake and fluid loss. Fluid losses other than urination include fluid lost through vomiting, diarrhea, and "insensible" losses. Insensible fluid loss is that which is not perceptible or appreciable. Such loss includes that fluid which is lost through respiration, evaporation from the skin, and fecal content. Section II. NURSING ASSESSMENT AND DIAGNOSTIC PROCEDURES 2-9. NURSING ASSESSMENT When performing a nursing assessment of a patient with a suspected disorder of the urinary system, it is important to question the patient about urinary output and changes in voiding patterns. a. Urinary Output. (1) During the act of micturition (urination), the bladder contracts and urine is expelled from the body through the urethra. The average urine output for a normal adult is considered to be about 1500-2000ml/24 hours. This, of course, will vary with fluid intake and other fluid losses (as discussed in Section I). (2) Polyuria is the passage of a large volume of urine in a given period of time. Polyuria is seen with diabetes. It may also occur with excessive fluid intake. (3) Oliguria is the passage of a small amount of urine in a given period of time. This is generally considered to be 100-500 ml/24 hours. Oliguria may indicate renal failure, shock, dehydration, or a fluid and electrolyte imbalance. (4) Anuria is the absence of urine. Passage of less than 50 ml/24 hours is considered to be anuria. This condition indicates a serious renal dysfunction and requires emergency medical intervention. b. Changes in Voiding Patterns. When interviewing the patient, ask about changes in their normal voiding pattern. Identification of signs and symptoms is a MED918 2-8 valuable tool in diagnosis of the condition. The following symptoms are significant and should be recorded in the nursing assessment. (1) Frequency. Voiding that occurs more often than usual (in comparison to the patient's regular pattern). (2) Urgency. A strong desire (or urge) to urinate. (3) Hesitancy. Undo difficulty or delay in initiating voiding. (4) Incontinence. Involuntary loss of urine. (5) Stress incontinence. Intermittent leakage of urine is caused by sudden (6) Nocturia. Excessive urination at night. strain. (7) Enuresis. Involuntary voiding during sleep. Bedwetting is considered abnormal after the age of three. (8) Dysuria. Painful or difficult urination. (9) Hematuria. The presence of blood in the urine. (10) Retention. Accumulation of urine within the bladder caused by the inability to urinate. 2-10. URINALYSIS a. Urinalysis is the examination and analysis of urine. It is routinely performed to detect abnormalities. The results of urinalysis are used by the physician in diagnosis of urinary conditions. b. Basic principles for collecting urine specimens include the following: (1) The first morning urine specimen is the most concentrated and would be required for tests where identification of specific elements is required (hormones, for example). (2) Never leave urine standing at room temperature. It will begin to breakdown, preventing accurate analysis. (3) Urine specimens should be collected using "clean-catch" technique (see paragraph 2-11). MED918 2-9 (4) When collecting a 24-hour specimen, ensure that the patient fully understands the collection procedure. If the patient fails to collect all the urine voided in a 24-hour period, the resulting evaluation will be erroneous. (5) If a "sterile" sample of urine is required, it should be obtained by catheterization. Such a sample might be necessary for a urine culture and sensitivity test. Catheterization is discussed in Section III. 2-11. COLLECTING A CLEAN CATCH URINE SPECIMEN a. Review patient's clinical record to verify physician's order for a clean catch urine specimen. b. Assemble the necessary equipment. (1) Antiseptic towelettes. (2) Disposable gloves for nurse if assisting a female patient. (3) Sterile specimen container. c. Approach and identify the patient. d. Explain the procedure to the patient. Patient will be asked to collect a virtually uncontaminated midstream urine specimen. (This is commonly referred to as a "clean-catch" urine specimen.) Because the urethra orifice is colonized by bacteria, urine readily becomes contaminated during voiding. e. Instruct the male patient in the steps of collecting a clean-catch urine specimen. (1) Instruct the patient to expose glands and cleanse area around meatus. Wash area with a mild antiseptic solution (towelettes). (2) Allow the initial urinary flow to escape into toilet or urinal. (3) Collect the midstream urine specimen in a sterile container. (4) Avoid collecting the last few drops of urine. (Prostatic secretions may be introduced into urine at the end of the urinary stream.) f. Instruct the female patient in the steps of collecting a clean catch urine specimen. MED918 2-10 (1) Ask the patient to separate her labia to expose the urethra orifice. Keeping the labia separated prevents labial or vaginal contamination of the urine specimen. (2) Cleanse the area around the urinary meatus with antiseptic towelettes. (3) While the patient keeps her labia separated, instruct her to void forcibly. This helps wash away urethra contaminants. (4) Allow initial urinary flow to drain into bedpan (toilet) and catch the midstream specimen in a sterile container. g. Instruct the patient to repeat the steps of the procedure. Correct misinformation/understanding as needed. h. Instruct patient to obtain the required specimen. (Assist as necessary.) i. Send the specimen to the laboratory immediately. j. Record the procedure in the patient's clinical records and report significant observation to the Charge Nurse. 2-12. COLLECTING A TWENTY-FOUR HOUR SPECIMEN a. Review the patient's clinical record to verify the physician's order and identify the purpose of the 24-hour specimen. (1) Urine is routinely collected for 24 hours in order to obtain a substantial quantity of urine for measuring solutes that are normally excreted in small amounts (such as hormones, proteins, and electrolytes). (2) Urine is also collected for 24 hours in order to test excretion rates in one day's function. b. Some tests require dietary restrictions prior to and/or during the exam. Be certain these restrictions are followed. c. Assemble the necessary equipment. (1) Twenty-four hour urine collection container. (Container should have required chemical preservatives inside, as appropriate for test.) MED918 (2) Urine collection pan/urinal. (3) Intake and output worksheet. 2-11 (4) Signs stating "twenty-four hour urine collection in progress." (5) Urine specimens cup (if initial specimen is required). d. Approach and identify the patient. e. Explain the procedure and its purpose to the patient. Be certain the patient understands what must be done. f. At the designated time on the designated day, begin the collection. (1) A twenty-four-hour collection normally begins in the early morning, at the time of the patient's first morning void. (2) Instruct the patient to empty his bladder. (Sometimes, a specimen is collected at this time. If not required, discard the urine.) (3) Record the time the patient emptied his bladder in the patient's chart and on the twenty-four hour collection container. This is the start time. g. Instruct the patient that all urine voided for the next 24 hours must be saved and placed into the twenty-four hour collection container. (1) Provide the patient with a urine collection pan or urinal, as appropriate. (2) Instruct the patient to notify the nursing staff each time he urinates into the collection pan, so the urine can be measured and added to the twenty-four hour collection container. (3) Record each voiding on the I & O sheet, if required. h. Post signs saying " twenty-four hour urine collection in progress" on the patient's chart, the bed, the door, and in the bathroom, as appropriate. i. Once the first urine specimen has been placed into the twenty-four hour collection container, the container must be kept on ice or in a specimen refrigerator (never, a food refrigerator). j. The following day, at the same time the test was initiated, ask the patient to void one last time. This specimen is added to the twenty-four hour collection container. k. Record date and time of completion on the container and in the patient's chart. Remove "24-hour urine collection in progress" signs. l. Complete the appropriate laboratory request slips and transport the specimen to the laboratory within 30 minutes of completion. MED918 2-12 m. Record the procedure and significant nursing observations in the patient's clinical records. 2-13. RADIOLOGIC EXAMS The two radiographic procedures used most frequently to aid in diagnosis of urinary disorders are the kidneys, ureters, and bladder (KUB) and Intravenous pyelogram (IVP). a. A flat plate X-ray of the abdomen to visualize the KUB. (1) It is used to show the size, shape, and positioning of the kidneys. (2) It serves as a baseline reference for follow-up X-rays. (3) It is used to visualize the size and position of urinary tract calculi (stones). b. Intravenous pyelogram is the intravenous introduction of a contrast medium that concentrates in the urine. This visualizes the KUB. (1) the exam. It is customary to keep the patient N.P.O. for 8-10 hours prior to (2) Laxatives are given the evening prior to the exam to eliminate fecal matter from the GI tract. (3) The patient should not be overly hydrated, as this will dilute the contrast medium and reduce visualization. 2-14. CYSTOSCOPY a. Cystoscopy is the direct visualization of the urethra and bladder by means of a special device called a cystoscope. The lighted, tubular, scope is inserted into the urethra. It is used to: (1) Inspect the urethra and bladder. (2) Remove calculi from the urethra, bladder, and ureters. (3) Allow insertion of catheters for removal of specimens. b. Preparation is minimal and involves: (1) MED918 Administration of prescribed medications and anesthetic. 2-13 (2) Patient education about the procedure. c. Nursing implications. (1) The patient will experience some burning and passage of blood when urinating following the procedure. This is due to irritation of the mucous membrane. (2) If urinary retention occurs, it may be necessary to insert an indwelling catheter (on physician's order only). Section III. CATHETERIZATION AND DRAINAGE 2-15. INTRODUCTION Catheterization is the procedure of introducing a catheter through the urethra into the urinary bladder. The procedure may be ordered by the physician for any of the following reasons: a. To relieve distention of the bladder due to inability to void. Distention is caused by retention of urine. Retention can occur with cystitis (inflammation of the bladder), with paralysis, or following surgical procedures. b. To obtain a sterile specimen of urine for laboratory analysis and culture. c. To determine residual urine. (Residual urine is defined as that amount of urine remaining in the bladder after voiding.) d. To provide continuous drainage of the bladder. e. To irrigate or instill liquid medications into the bladder. Medications and fluids for irrigation are prescribed by the physician. 2-16. GENERAL NURSING IMPLICATIONS Because both the bladder and the urethra are easily injured and highly susceptible to infection, it is important to stress several precautions in the performance of the procedure. a. Aseptic Technique. Each catheterization is a potential source of infection if not carried out properly. Most cases of cystitis and other urinary tract infections, which develop after catheterization, are usually caused by improper technique. b. Lubricated Catheter. The catheter must be well lubricated prior to insertion to reduce friction and trauma to the mucous membrane lining of the urethra and the bladder. The disposable catheterization kits used today contain sufficient lubricant within the kit. MED918 2-14 c. Gentle Insertion. The catheter is inserted only far enough to enter the bladder. Use only mild pressure during insertion. Never force a catheter if resistance is met. Stop the procedure and inform the professional nurse. 2-17. RETENTION CATHETERS A retention (indwelling) catheter is ordered to permit continued drainage of the urinary bladder without repeated catheterization. The catheter commonly used is a selfretaining urethra catheter (Foley type). This tube has a double lumen: one lumen is for drainage and the other is for inflation of the retention device (a small balloon at the tip of the catheter). The retention balloon is inflated with a measured amount of sterile water following its placement in the bladder. When a retention catheter is used, provision is usually made for bladder drainage by means of drainage tubing connected to a plastic drainage bag. Following insertion of the catheter, it is a nursing responsibility to set up and maintain the drainage system. Aseptic technique in maintaining urinary drainage is required since the patient is exposed to a source of chronic irritation from the indwelling catheter and is therefore more susceptible to any source of infection. 2-18. SUPPLIES AND EQUIPMENT a. Disposable sterile catheterization set, containing: (1) Catheter (straight or indwelling). (2) Gloves, sterile. (3) Sterile detergent-disinfectant solution, for cleansing skin, as prescribed. (4) Water soluble lubricant, sterile. (5) Protective, sterile drapes. (6) Chux pads. (7) Sterile specimen container. b. Specimen label and appropriate laboratory request forms. c. Floor lamp, adjustable. d. Portable screen (according as circumstances may require (p.r.n.)). e. Kelly forceps (p.r.n.). f. Adhesive tape. MED918 2-15 g. Waste receptacle. **If inserting an indwelling (retention) catheter, you will also need: h. Sterile water (usually included in kit). i. Sterile syringe (10 cc) (usually included in kit). j. Sterile urine drainage bag with collecting tubing. 2-19. CATHETERIZING THE FEMALE PATIENT a. Preparatory Phase. (1) Check physician's order. (2) Approach and identify the patient and explain the procedure. (3) Place patient in supine position with knees bent and feet resting flat on the bed about two feet apart. Drape the patient. (4) Position moisture-proof pad under patient's buttocks. (5) Place waste receptacle in accessible place. (6) Direct light for visualization of genital area. (7) Wash hands. (8) Open catheter kit using aseptic technique. (9) Squeeze lubricant into plastic tray. (10) Pour cleansing solution over cotton balls or open swab packet. (11) Wash hands and put on sterile gloves. **If inserting retention catheter, you must also: (12) Inspect catheter for defects. Test the balloon by injecting 10 cc of sterile water into the balloon. Allow water to drain back into syringe. N OTE: If there is a leak in the balloon, the catheter must be discarded and replaced. (13) Connect the catheter to the connecting tubing on the drainage bag. Maintain sterility of catheter and drainage bag. MED918 2-16 b. Performance Phase. (1) Using your non-dominant hand, separate the labia, so that the urethra meatus is visualized. This hand maintains separation of the labia until catheterization is finished. This helps prevent labial contamination of the catheter. NOTE: This glove is no longer sterile. (2) With dominant sterile hand, pick up cotton ball (with forceps) or one swab stick. With downward stroke, from anterior to posterior, cleanse the labia farthest from you. DO NOT RETRACE. (3) Repeat the procedure to cleanse the labia closest to you. (4) Repeat the procedure a third time to cleanse the area between the two labia. Stroke from top to bottom, cleansing the urinary meatus. Discard cotton balls or swabs. (5) Grasp the catheter about 3 inches from the tip and lubricate it, keeping the remainder coiled in the palm of the hand. (6) Gently insert the catheter about 2 inches into the urethra or until urine begins to flow. Aim the catheter downward and to the back. NOTE: If the catheter is accidentally introduced into the vagina, remove the catheter and discard it. Obtain another sterile catheter and begin the procedure again. (7) Allow the urine to flow into the catheter tray (drainage bag, if retention catheter). **If inserting a retention catheter, skip steps (8) through (11) and go to step (12). (8) Collect a sterile specimen (if ordered) in the sterile specimen cup contained in the kit. NOTE: Never allow more than 1000 cc of urine to drain from the bladder at one time. Clamp the catheter and wait about 15 minutes before allowing the remainder of the urine to drain. (9) When the urine has stopped flowing, pinch off the catheter and gently remove it. (10) Dry the patient and leave her in a comfortable position. Replace any soiled linen. MED918 2-17 (11) Wash hands. Skip steps (12) through (18) and go to follow-up phase (item c). (12) When urine is observed moving through the collecting tubing, advance the catheter another 1/2 inch. (This will ensure that the catheter tip is fully within the bladder.) (13) Inflate the balloon with 10 cc of sterile water. (14) GENTLY pull on the catheter to ensure that it is properly placed, and then gently push back into the bladder about 1/4 inch. (15) Secure catheter in place with adhesive tape. Anchor the catheter to the skin of the inner thigh. (16) Dry the patient and leave her in a comfortable position. (17) Wash hands. (18) If collection of a sterile specimen is ordered, you may collect it from the urinary drainage bag at this time. (Closed system is sterile until opened.) NOTE: This is the ONLY time it is acceptable to collect urine from the drainage bag for testing purposes. c. Follow-Up Phase. (1) Remove all equipment from the patient's bedside. Discard disposable items and return other equipment to the appropriate storage areas. (2) Measure the urine. Send the sterile specimen to the laboratory with the appropriate request slips. (3) Record the procedure in the Nursing Notes: include the date, time, amount and appearance of urine obtained, whether specimen was sent to the lab, and the patient's tolerance. 2-20. CATHETERIZING THE MALE PATIENT a. Preparatory Phase. MED918 (1) Check physician's order. (2) Approach and identify the patient and explain the procedure. (3) Place the patient in a supine position with legs extended. 2-18 (4) Place a sterile moisture proof drape across upper thighs. (5) Place waste receptacle in accessible place. (6) Direct light for visualization of genital area, if necessary. (7) Wash hands. (8) Open catheter kit using aseptic technique. (9) Squeeze lubricant into plastic tray. (10) Pour cleansing solution over cotton balls or open swab packet. (11) Wash hands and put on sterile gloves. **If inserting a retention catheter, you must also: (12) Inspect catheter for defects. Test the balloon by injecting 10 cc of sterile water into the balloon. Allow the water to drain back into the syringe. NOTE: If there is a leak in the balloon, the catheter must be discarded and replaced. (13) Connect catheter to the connecting tubing on the drainage bag. Maintain sterility of catheter and bag. b. Performance Phase. (1) Using your non-dominant hand, grasp penis, raising it almost straight up. (This maneuver straightens the urethra and facilitates catheterization.) Maintain grasp on penis until procedure is completed. NOTE: This glove is no longer sterile. (2) With dominant sterile hand, pick up cotton ball (with forceps) or one swab stick. Cleanse urethra meatus in a circular motion. Repeat as required, using a new swab or cotton ball each time. DO NOT RETRACE. Discard swabs/cotton balls. (3) Grasp the catheter about three inches from the tip and lubricate it, keeping the remainder coiled in the palm of the hand. (4) Gently insert the catheter into the urethra until urine begins to flow (6-9 inches). The catheter may be held with Kelly forceps rather than the gloved hand, if preferred. MED918 2-19 (5) Allow the urine to flow into the catheter tray (drainage bag, if retention catheter). **If inserting a retention catheter, skip steps (6) through (9) and go to step (10). (6) Collect a sterile specimen (if ordered) in the sterile specimen cup contained in the kit. NOTE: Never allow more than 1000 cc of urine to drain from the bladder at one time. Clamp the catheter and wait about 15 minutes before allowing the remainder of the urine to drain. (7) When the urine has stopped flowing, pinch off the catheter and gently (8) soiled linen. Dry the patient and leave him in a comfortable position. Replace any remove it. (9) Wash hands. Skip steps (10) through (16). Go to follow-up phase (item c). (10) When urine is observed moving through the collecting tubing, advance the catheter another 1/2 inch. (This will ensure that the catheter tip is fully within the bladder.) (11) Inflate the balloon with 10 cc of sterile water. (12) GENTLY pull on catheter to ensure that it is properly placed, and then gently push back into the bladder about 1/4 inch. (13) Secure catheter in place with adhesive tape. Anchor the catheter to the skin of the abdomen, with the penis pointing toward the patient's head. (14) Dry the patient and leave him in a comfortable position. (15) Wash hands. (16) If collection of a sterile specimen is ordered, you may collect it from the drainage bag at this time. (Closed system is sterile until opened.) NOTE: This is the ONLY time it is acceptable to collect urine from the drainage bag for testing purposes. c. Follow-Up Phase. MED918 2-20 (1) Remove all equipment from the patient's bedside. Discard disposable items and return other equipment to the appropriate storage areas. (2) Measure the urine. Send the sterile specimen to the laboratory with the appropriate request slips. (3) Record the procedure in the Nursing Notes: include the date, time, amount and appearance of urine obtained, whether specimen was sent to the lab, and patient's tolerance. 2-21. FOLLOW-UP NURSING CARE FOR RETENTION CATHETER AND CLOSED DRAINAGE SYSTEM The retention catheter and drainage system may be continued for days, weeks, or indefinitely. As a general rule, the retention catheter is changed in accordance with the infection control standard operating procedure (SOP). Daily, continuing care of the patient and the equipment includes the following essentials: a. Maintain an accurate intake and output record. Unless otherwise ordered, encourage the patient to drink at least 3000 ml of fluids daily to provide an effective "internal irrigation" system for the bladder, catheter, and drainage tubing. b. Observe the tubing and catheter connections frequently for kinks. Make sure the patient is not lying on the tubing since this both obstructs drainage and causes undue pressure on the skin. c. Maintain cleanliness and protect the urethral meatus. This requires direct observation and specific hygiene measures. Wash the perineal area carefully, from front to back. Remove secretions of mucus and other discharge gently but thoroughly to help reduce irritation and possible infection. Follow infection control SOP for guidance on frequency of catheter care and choice of antiseptic/antimicrobial cleansers to be used. d. Measure and record the collected output in accordance with (IAW) local SOP. Never permit the drainage bag to become more than three-fourths full in order to prevent any possibility of the tubing outlet becoming immersed in the draining urine. e. Do not disconnect tubing from drainage bag. f. Keep the collecting bag below the level of the bladder, but never allow it to touch the floor. g. Provide continued gravity drainage for the ambulating patient. Check to see that the tubing is not excessively long or looped below the level of the bag when he is standing upright. MED918 2-21 h. DO NOT separate connecting tube and catheter. Obtain a urine specimen without disrupting the closed system. A needle and syringe is used to aspirate urine from a special port on the collecting tubing. i. Change the catheter as ordered or IAW local infection control policy. The order may be to remove the catheter and then to replace it following several hours interval to relieve pressure on the urethra. Remember: (1) Always deflate the balloon of a self-retaining catheter before removal. (2) Use aseptic techniques for any procedure involving the urethra and bladder. Each catheterization is a potential source of injury and infection if not performed properly. 2-22. COLLECTING A URINE SPECIMEN FROM AN INDWELLING CATHETER a. Review the patient's clinical record to verify the physician's order and determine the reason for collection of the urine specimen. b. Assemble the necessary equipment. (1) Rubber band or screw clamp. (2) Sterile syringe. (3) Sterile 20-gauge needle. (4) Alcohol sponge. (5) Sterile specimen collection container. (6) Identification labels and laboratory request slips. c. Wash your hands. d. Approach and identify the patient. e. Explain the procedure to the patient. f. Provide for privacy. g. Wash your hands. h. Clamp the drainage tubing directly below the aspiration port with a rubber band or clamp to ensure a sufficient amount of pooled urine for a specimen. Fifteen minutes is generally sufficient. MED918 2-22 NOTE: Remember, a urine specimen collected from an indwelling catheter bag is not acceptable for laboratory testing unless it is the first urine drained into a new sterile bag. i. Place a sign above the patient's bed "Urine Tubing Temporarily Clamped." j. When sufficient urine has accumulated in the tubing, cleanse the aspiration port with an alcohol swab. k. Expel all air from the syringe. l. Insert the needle into the aspirating port. m. Withdraw the desired volume of urine. (1) The amount of urine needed will vary, depending on the laboratory testing methods. (2) Refer questions to your laboratory technician. n. Withdraw the needle and transfer the urine from the syringe into the sterile specimen container. o. Remove the rubber band or screw clamp so urine can drain freely into the drainage bag once again. p. Remove the sign placed above the patient's bed. q. Complete the appropriate laboratory request slips. r. Label urine specimen and send it to the laboratory within 30 minutes of collection. s. Dispose of the needle and syringe in the appropriate location. t. Record procedure in patient's clinical record. Report significant observations to professional nurse, as appropriate. 2-23. CONTINUOUS BLADDER IRRIGATION a. Preparatory Phase. (1) Review the patient's clinical record to verify physician's order and to become familiar with reason(s) for performing continuous bladder irrigation. Irrigation of the bladder is done for the following reasons: MED918 2-23 (a) To help prevent urinary tract obstruction by flushing out small blood clots that form after prostate or bladder surgery. (b) To create mild tamponade that may help prevent venous (c) To treat an irritated, inflamed, or infected bladder lining. hemorrhaging. (2) Check the patient's medication history for hypersensitivity to antibiotics, and report significant findings to professional nurse. (3) Wash your hands. (4) Collect the equipment needed. (a) Two containers of irrigating solution (usually 1,000 ml containers of normal saline or prescribed amount of antibiotic solution). (b) Y-type IV tubing. (c) Sterile alcohol or povidone-iodine sponge. (d) Catheter kit with a triple lumen catheter. NOTE: A three-way or triple lumen catheter has three separate openings. One lumen inflates the balloon holding the catheter in place. The second lumen allows for the outflow of urine and the outflow of drainage solution. The third lumen allows for the inflow of irrigating solution (antibacterial rinse) into the bladder (figure 2-4). (e) (5) Closed drainage system. Approach and identify the patient and explain the procedure. b. Performance Phase. (1) Attach catheter to the drainage apparatus before inserting the catheter into the urethra. Catheterize the patient according to the steps previously mentioned. (2) To prevent the introduction of organisms where the catheter enters the urethral meatus, apply an antimicrobial ointment. (3) Begin irrigation. (a) Provide for privacy and drape as necessary. (b) Insert one spike of the Y-type tubing into each container of irrigating solution. (c) Squeeze the drip chamber on each spike of the tubing. (d) Open the flow clamps to remove air from the tubing. Close them when the fluid reaches the end of the tubing. MED918 2-24 (e) Hang the two containers of irrigating solution on an IV pole. Figure 2-4. Continuous bladder irrigation. (f) Clean the opening to the inflow lumen of the catheter with the sterile alcohol or povidone-iodine sponge. MED918 2-25 (g) Insert the distal end of the I.V. tubing securely into the inflow lumen of the catheter. (The outflow lumen should already be attached to tubing leading to the drainage collection bag.) (h) Open the flow clamp on one of the containers of irrigating solution and set the drip rate as ordered. (4) Switch to the reserve container when the first container of irrigating solution is nearly empty. (a) To prevent air from entering the system, do not allow the primary container to empty completely. Simultaneously close the flow clamp on the nearly empty container and open the flow clamp on the second container. (b) Adjust the drip rate, as ordered. (c) Disconnect the tubing from the nearly empty container with a twisting motion, being careful not to contaminate the tubing. (d) Hang a new reserve container on the IV pole and insert the tubing, maintaining asepsis. (e) Discard the empty container appropriately. (f) As the irrigating solution containers become nearly empty, repeat the exchange procedure in order to maintain a constant flow of irrigation solution. c. Follow-Up Phase. Observe special considerations while performing continuous irrigations: (1) Always have a second container of irrigating solution available to replace the one that's nearly empty. (2) Check the inflow and outflow lines periodically for kinks, to make sure the solution is running freely. (3) Measure the outflow volume correctly. (a) Outflow volume should equal or, allowing for urine production, slightly surpass inflow volume. (b) If inflow volume exceeds the outflow volume, suspect bladder rupture or renal damage, and notify the professional nurse immediately. (4) MED918 Assess outflow for blood clots and/or changes in appearance. 2-26 (5) Empty drainage collection bags frequently. (6) Document in the patient's clinical record. Record procedure, significant nursing observations, and amount of fluid instilled and drained. Report same to professional nurse. Section IV. URINARY DISORDERS 2-24. URINARY TRACT INFECTIONS a. Urinary tract infections (UTI) are caused by the presence of pathogenic microorganisms in the urinary tract. In most urinary tract infections, bacteria enter through the urethra and ascend to the bladder. Once established within the bladder, the bacteria are able to ascend through the ureters to the kidneys. Contamination of the urinary tract can occur in the following ways: (1) Reflux of urine from the bladder, into the urethra, and back up into the (2) Reflux of urine from the bladder into the ureters. (3) Fecal contamination of the urinary meatus. (4) Introduction of instruments for examination or catheterization. bladder. b. Urinary tract infections may occur in the urethra (urethritis), the urinary bladder (cystitis), the prostate gland (prostatitis), and the kidney (pyelonephritis). (1) Cystitis is more common in females because the female urethra is short and in close anatomical proximity to the vagina and rectum. The male urethra is longer, and the prostatic secretions have an antibacterial property that discourages passage of bacteria. (2) Urethritis may be associated with cystitis, may occur as a result of trauma from a catheter or cystoscope, or may be sexually transmitted. If urethral discharge is present, with or without other symptoms, a urethral smear should be sent to the laboratory for analysis along with the standard urine culture. (3) Pyelonephritis is an infection of the kidney's renal pelvis, tubules, or interstitial tissue. It may occur as an acute or chronic condition. Pyelonephritis can result in renal insufficiency, which may lead to renal failure. (4) Prostatitis is inflammation of the male prostate gland. Inflammation of the prostate commonly occurs without the presence of infection. However, bacterial invasion of the prostate may occur as a result of bacteria descending from the kidney or bacteria ascending from the urethra. MED918 2-27 c. Certain factors predispose the urinary tract to infection: (1) Urinary stasis. (2) Obstructions to urine flow such as strictures or stones. (3) Systemic infection, which may enter the kidney through the blood or (4) The presence of other renal disease. lymph. 2-25. SIGNS AND SYMPTOMS OF URINARY TRACT INFECTIONS Infections of the urinary tract may occur with or without symptoms. When symptoms do occur, they may include the following: a. Lower urinary tract infections (cystitis, urethritis). (1) Dysuria. (2) Hematuria. (3) Frequency. (4) Urgency. (5) Nocturia. (6) Bacteria/pus in urine. (7) Back pain. (8) Sensation of "bearing down" or spasm in suprapubic region. (9) Urethral discharge (urethritis). b. Upper urinary tract infections (pyelonephritis). MED918 (1) All the symptoms of a lower UTI, plus: (2) Flank pain. (3) Fever. (4) Chills. 2-28 2-26. NURSING IMPLICATIONS a. Successful treatment of UTI involves a urine culture to identify the bacteria present and a sensitivity test to determine the most effective antibiotic. Nursing personnel must ensure that proper technique is used during collection of the specimen in order to prevent contamination of the specimen. Contamination by other substances will result in an inaccurate test. b. Fluids should be encouraged in order to "flush" the system of the bacteria. c. Frequent voiding should be encouraged to prevent urinary stasis. d. I.V. fluids and antibiotics should be administered as ordered. 2-27. UROLITHIASIS a. Urolithiasis is the presence of stones in the urinary system. These stones are formed by the deposit of crystalline substances excreted in the urine. (1) Variations in sizes range from sand-like granules to stones the size of a (2) Most stones are combinations of calcium and phosphate. baseball. (3) Different stone compositions develop in association with the pH of the urine. For example: (a) Phosphate, oxalate, and carbonate stones form in alkaline urine. (b) Uric acid, urate, and cystine stones form in acid urine. b. Factors that precipitate stone formation include: MED918 (1) Infections. (2) Urinary stasis. (3) Excess calcium. (4) Vitamin deficiencies (especially vitamin A). (5) Dehydration. 2-29 2-28. CLINICAL MANIFESTATIONS OF UROLITHIASIS Signs and symptoms will vary according to the size and location of the stone. Symptoms also vary with the presence of infection and/or obstruction. a. General symptoms include: (1) Pain. (2) Diarrhea. (4) Vomiting. (5) Abdominal discomfort. b. Renal colic, associated with kidney stones, is manifested by: (1) Acute renal area pain, radiating anteriorly and downward. (2) Nausea. (3) Vomiting. (4) Loin tenderness. c. Ureteral colic, associated with stones in the ureters, is manifested by: (1) Acute, colicky pains radiating to genital area and down the thigh. (2) Frequent desire to void, with little urine passed. (3) Hematuria. 2-29. NURSING IMPLICATIONS Nursing care of patients with urolithiasis involves: a. Controlling Pain. (1) Administer pain medications as prescribed and assess patient frequently, as this pain can be excruciating. (2) Hot bath or moist heat to painful area. b. Relief of Obstruction. MED918 2-30 (1) Encourage fluids. (2) Observe strict I & O. (3) Assist physician in catheterization or cystoscopy, as ordered. c. Determine Stone Type. (1) Strain all urine. (2) Send stones to laboratory for identification. d. Diet Modification. (1) Implement diet modifications as ordered. (2) Alter the pH of the urine to reduce stone formation. (a) To acidify urine, give citrus juices or ascorbic acid (vitamin C). (b) To alkalinize urine, give sodium bicarbonate. e. Prepare Patient for Surgery. Surgical intervention is indicated if the stone is causing: (1) An obstruction that cannot be relieved. (2) Infection that is not responsive to treatment. (3) Unrelenting pain. (4) Damage to the urinary system. 2-30. GLOMERULONEPHRITIS a. Glomerulonephritis is an inflammatory disease of the kidneys. The inflammatory process is thought to be a result of an immune system response. Antigenantibody reactions form molecule complexes that move through the circulatory system. Some of these complexes become lodged in the glomeruli, initiating the inflammatory response. The inflammation causes thickening of the glomerular filtration membrane, resulting in scarring and loss of filtering surface. Fibrous tissue forms and the kidney cannot function normally. b. Repeated occurrences of mild glomerulonephritis may cause damage that goes unchecked for years because the patient is asymptomatic. Even the insidious MED918 2-31 onset of symptoms may go unnoticed. The condition is often diagnosed during a routine physical exam or eye examination, when the patient may be found to have: (1) Mild hypertension. (2) Pedal edema. (3) Vascular changes or hemorrhages in the eyes. (4) Abnormal urinalysis. c. An acute attack may be manifested by: (1) Scanty amounts of bloody, cloudy, sediment filled urine. (2) Headache. (3) Malaise. (4) Flank pain. (5) Swollen, congested kidneys. (6) Edema, facial and extremity. (7) Increased blood levels of urea and creatinine. (8) Hypertension. (9) Pulmonary edema. (10) Congestive heart failure. (11) Renal failure. 2-31. NURSING IMPLICATIONS Nursing care of patients with glomerulonephritis involves observing for complications and protecting the kidneys from further damage. Nursing personnel should do the following: a. Monitor vital signs. b. Encourage bedrest. c. Observe strict I & O. MED918 2-32 d. Check weight daily. e. Observe for signs of impending renal failure. (1) Lethargy. (2) Nausea and vomiting. (3) Oliguria or anuria. f. Implement and enforce ordered fluid and diet modifications. (1) Protein restriction (for impaired renal function). (2) Sodium restriction (if edema is present). (3) Fluid restriction (if edema is present). (4) Increased dietary carbohydrate (to provide energy and reduce the metabolism of protein). 2-32. CHRONIC RENAL FAILURE a. Chronic renal failure is a progressive deteriorization of renal function. Renal insufficiency progresses to renal failure, ending in uremia and its complications. Uremia is the accumulation, in the blood, of substances ordinarily filtered by the kidneys and excreted in the urine. b. As renal function declines, the kidneys become increasingly unable to remove (filter) the body's metabolic wastes. The products of protein metabolism accumulate in the blood and other body fluids, causing disruption and imbalances throughout the body. Such alterations include: (1) Gastrointestinal: anorexia, nausea, vomiting, and diarrhea. (2) Hematological: anemia, bleeding tendencies. (3) Integumentary: skin discoloration, pruritis. (4) Skeletal: osteomalacia, uremic bone disease. (5) Sexual/reproductive: decreased libido, impotence, amenorrhea. (6) Cardiovascular: HTN, pulmonary congestion, pulmonary edema, and congestive heart failure. MED918 2-33 (7) Neurological: anxiety, personality changes, delusions, hallucinations, and convulsions. (8) Metabolic: water retention, sodium retention, potassium retention, and metabolic acidosis. c. Chronic renal failure may be caused by: (1) Chronic glomerulonephritis. (2) Pyelonephritis. (3) Uncontrolled hypertension. (4) Nephrotoxic agents (drugs/toxins). (5) Dehydration. d. Onset of symptoms begins with generalized weakness, lethargy, headache, and mild GI complaints, such as anorexia, nausea, and vomiting. If not diagnosed and treated, uremia will progress to a state of total body involvement. The patient will become increasingly somnolent. An ammonia odor will be evident on the breath, and respirations will become Kussmaul in character. "Uremic frost," a powdery substance composed of uric acid salts, will appear on the skin. Muscle twitching is followed by convulsions, coma, and death. 2-33. MEDICAL TREATMENT The basis of care in managing a patient with chronic renal failure is to: a. Assist the diseased kidneys to maintain homeostasis for as long as possible. b. Prepare the patient for dialysis/transplant when conservative, symptomatic treatment is no longer effective. (1) When the patient can no longer manage a normal lifestyle with conservative treatment, dialysis is indicated. (2) When end-stage renal failure occurs and the patient is facing imminent death, kidney transplant is indicated. 2-34. NURSING IMPLICATIONS Nursing management of the patient with chronic renal failure includes the following: MED918 2-34 a. Gastrointestinal. (1) Symptomatic treatment for nausea, vomiting, and diarrhea. (2) Encourage a nutritious, appetizing diet of the patient's preferred foods to combat anorexia and improve nutritional status. b. Hematological. (1) Administer vitamin and mineral supplements as ordered. (2) Observe skin and mucous membranes for evidence of bleeding or (3) Implement the use of soft bristle toothbrush and electric razor. bruising. c. Integumentary. (1) Use mild cleansers to avoid further skin irritation. (2) Apply soothing lotions (p.r.n.). (3) Administer prescribed antipruritics to combat itching. d. Cardiovascular. (1) Administer prescribed medications for control of hypertension, pulmonary edema, and congestive heart failure. (2) Monitor vital signs. (3) Observe for dependent edema. (4) Auscultate lungs for the presence of fluid. e. Metabolic. (1) Observe strict I & O. (2) Monitor blood levels of electrolytes. (3) Check weight daily and assess for fluid retention. (4) Implement prescribed dietary modifications. (a) Sodium restriction to decrease water retention. MED918 2-35 (b) Limited protein to decrease protein metabolism (protein metabolism will result in more nitrogenous wastes that cannot be filtered by the kidneys). (c) Any dietary protein allowed must be of high biological value to provide the essential amino acids. (d) High carbohydrate diet to provide energy and decrease protein metabolism. (e) Potassium restrictions to avoid hyperkalemia (cellular potassium is released during protein metabolism. Hyperkalemia, or potassium intoxication, can cause severe cardiac arrhythmia’s). f. Neurological. (1) Frequent assessment of level of consciousness. (2) Observation for mental status changes. (3) Encourage family to report noted personality changes. (4) Administer prescribed medications to manage muscle spasms and convulsive seizures. 2-35. ACUTE RENAL FAILURE a. Acute renal failure is the sudden and severe loss of kidney function. As in chronic renal failure, all body systems become disrupted by the inability of the kidneys to filter metabolic wastes. b. Acute renal failure may be the result of one of the following: (1) Trauma. (2) Nephrotoxic drugs. (3) Transfusion reaction. (4) Cardiopulmonary bypass. (5) Hypovolemic hypertension (as a result of hemorrhage or burns, for (6) Dehydration. (7) Sepsis. example). MED918 2-36 (8) Obstruction of the renal arteries. (9) Mechanical obstruction of the urinary tract (stones, strictures, tumor). c. Clinical manifestations. (1) Clinical manifestations are the same as for chronic renal failure, except that the onset of symptoms is not insidious as in chronic renal failure. An abrupt cessation of renal function will bring about rapid changes as the body struggles to maintain its homeostatic environment. (2) Blood analysis will reveal a rise in serum levels of elements normally excreted by the kidneys. (a) Urea. (b) Uric acid. (c) Creatinine. (d) Potassium. 2-36. MEDICAL TREATMENT a. Effective treatment depends upon identification and treatment of the underlying condition responsible for the failure of the kidneys. b. Along with treatment of the primary condition, normal homeostasis must be restored and maintained in order to restore kidney function and allow for tissue repair. 2-37. NURSING IMPLICATIONS a. Nursing care considerations are the same as for a patient with chronic renal failure, remembering at all times that changes in status may occur very rapidly. For this reason, intense and vigilant nursing observation is required. b. Fluid replacement therapy will be based on the patient's weight, urinary output, and insensible losses. I & O must be accurate in order for the physician to prescribe the correct amount of IV fluids and P.O. intake. c. The patient must be continually assessed for fluid retention. MED918 (1) Auscultate lungs for the presence of fluid. (2) Observe for dependent edema. 2-37 d. Assess for circulatory overload to avoid damage to the heart and lungs. Observe for: (1) Distended neck veins. (2) Dyspnea. (3) Orthopnea. (4) Pulmonary congestion. (5) Tachycardia. (6) Hypertension. 2-38. BLADDER TRAUMA a. Trauma to the bladder includes contusions, rupture, or urethral injuries. b. Causes include blunt trauma and penetrating injuries to the lower abdomen, fractures of the pelvis or symphysis pubis, and "seatbelt" rupture. (A full bladder can be ruptured by the force of impact in a collision when the seatbelt is worn snugly.) c. Signs and symptoms of an injured or ruptured bladder include: (1) Hematuria. (2) Blood at the urinary meatus. (3) Failure to void. (4) Rigid abdomen. (5) Shock. (6) Hemorrhage. d. Nursing implications. MED918 (1) Treat shock and hemorrhage. (2) Maintain strict I & O. (3) Catheterize as ordered. (4) Prepare for surgical repair of the bladder if indicated. 2-38 2-39. RENAL TRAUMA a. Trauma to the kidneys includes contusions, lacerations, and rupture. Because the kidneys are very vascular organs, receiving about one half the blood flow from the abdominal aorta, even a small laceration can cause massive hemorrhage. b. Any blunt or penetrating injury to the back, flank, or abdomen may bruise, lacerate, or rupture a kidney. c. Signs and symptoms of kidney trauma include: (1) Nausea and vomiting. (2) Back pain. (3) Flank pain. (4) Abdominal tenderness. (5) Hematuria. (6) Palpable mass (indicating internal bleeding). (7) Shock. d. Nursing implications. (1) Treat shock and hemorrhage. (2) Avoid administration of narcotic analgesics, as they mask symptoms that will indicate the onset of complications. (3) Observe vital signs closely. (4) Evaluate frequently for changes in status. (5) Monitor hemoglobin and hematocrit for signs of internal bleeding. (6) Maintain and monitor urinary drainage. (7) Enforce strict bedrest. (8) In cases of a severe or penetrating injury, surgical intervention is indicated. Prepare the patient for surgical repair or nephrectomy, as indicated. MED918 2-39 2-40. CONCLUSION a. This lesson has introduced the basic nursing care techniques and procedures involved in nursing care related to the urinary system. b. Review the lesson objectives once again. If you feel confident that you have achieved the lesson objectives, complete the exercises at the end of the lesson. c. If you do not feel that you have met the lesson objectives, review the necessary material before you attempt the end of lesson exercises. Continue with Exercises MED918 2-40 EXERCISES, LESSON 2 INSTRUCTIONS: Answer the following exercises by marking the lettered response that best answers the question, by completing the incomplete statement, or by writing the answer in the space provided at the end of the question. After you have completed all of these exercises, turn to "Solutions to Exercises" at the end of the lesson and check your answers. For each exercise answered incorrectly, reread the material referenced with the solution. 1. The primary function of the urinary system is ____________________________ ________________________________________________________________. 2. The renal cortex contains millions of ___________________________________. 3. Along the edges of the renal pelvis are cup-like projections called the__________ ________________ and ________________ ____________________________. 4. Urine is passed through each ureter by _________________________________. 5. The male urethra is how long? ________________________________________. 6. The female urethra is how long? ______________________________________. 7. Water and organic molecules are filtered from the blood in the _____________________________. 8. Water and usable chemicals are reabsorbed into the blood in the _____________________________. 9. Normal urine is composed of ___________________ and _______________. 10. The passage of a small amount of urine in a given period of time is called ____________________________________. MED918 2-41 11. Anuria is considered to be the passage of ____________________ ml of urine in a 24-hour period. 12. The presence of blood in the urine is called _____________________________. 13. When collecting a clean-catch urine specimen, cleansing the urinary meatus is necessary because ________________________________________________. 14. Once the first urine specimen has been placed in the 24-hour collection container, you must _________________________________________________________. 15. A KUB is an X-ray of the ______________________, _____________________ and __________________________. 16. List 4 reasons for insertion of a catheter. a. ____________________. b. ____________________. c. ____________________. d. ____________________. 17. Why must a catheter be lubricated prior to insertion?_______________________ ________________________________________________________________. 18. When inserting a retention catheter, you must inspect the catheter, ____________ _____________________________________________________, and connect the catheter to the drainage system, before insertion. 19. When is it acceptable to collect a urine specimen from the urine drainage bag? ______________________________________________________ ______________________________________________________. 20. Where should the retention catheter for a male patient be taped? ___________ _________________________________. MED918 2-42 21. In most urinary tract infections, bacteria enters through _____________________. 22. Cystitis is more common in females because ____________________________ ________________________________________________________________. 23. Why are fluids encouraged in-patients with a urinary tract infection? __________ ________________________________________________________________. 24. Infection of the renal pelvis, tubules, or interstitial tissue is called_____________ _________________________________. 25. Urinary stasis, infections, and dehydration may precipitate__________________ ________________________________________________________________. 26. Why should dietary protein be restricted in-patients with renal disease? ________________________________________________________________ ________________________________________________________________. 27. The sudden loss of kidney function is called ____________________________. 28. The basis of care in managing a patient with chronic renal failure is to_________ ________________________________________________________________ and ____________________________________________________________. 29. A high carbohydrate diet is prescribed for patients with renal insufficiency/renal failure because it _________________________________________________ and ___________________________________________________________. 30. What disease is associated with scarring and loss of glomerular filtering surface? _______________________________________________________________. Check Your Answers on Next Page MED918 2-43 SOLUTIONS TO EXERCISES, LESSON 2 1. To control the composition, volume, and pressure of the body's fluids by regulating excretion of water and solutes. (para 2-1a) 2. Nephrons. (para 2-2d) 3. Minor and major calyces. (para 2-2f) 4. Peristalsis. (para 2-3) 5. Approximately 6-7 1/2 inches. (para 2-5a) 6. Approximately 1 1/2 inches. (para 2-5b) 7. Glomerulus. (para 2-7c) 8. Tubules (of the nephrons). (para 2-7d) 9. Water (95 percent); solutes (5 percent). (para 2-8a) 10. Oliguria. (para 2-9a(3)) 11. Less than 50. (para 2-9a(4)) 12. Hematuria. (para 2-9b(9)) 13. The urethral orifice is colonized by bacteria. (para 2-11d) 14. Keep container "on ice" or in a refrigerator. (para 2-12i) 15. Kidneys, ureters, bladder. (para 2-13a) 16. A correct answer consists of any four of the following: a. b. c. d. e. To relieve distention. To obtain a sterile specimen of urine. To determine residual urine. To provide continuous drainage of the bladder. To irrigate or instill medications. (para 2-15a-e) 17. To reduce friction and trauma. (para 2-16b) 18. Inflate the balloon to test it, then deflate. (para 2-19a(12)) MED918 2-44 19. Only when collecting the initial specimen from a new, sterile bag after inserting the catheter. (para 2-19b(18)) 20. To the abdomen. (para 2-20b(13)) 21. The urethra. (para 2-24a) 22. The urethra is in close anatomical proximity to the vagina and rectum. (para 2-24b(1)) 23. To "flush out" the bacteria. (para 2-26b) 24. Pyelonephritis. (para 2-24b(3)) 25. Stone formation (urolithiasis). (para 2-27b) 26. To decrease protein metabolism, which produces nitrogenous wastes that cannot be filtered by the kidney. (para 2-34e(4)(b)) 27. Acute renal failure. (para 2-35a) 28. Assist the kidneys to maintain homeostasis; prepare the patient for dialysis or transplant. (para 2-33a,b) 29. Provides energy; decreases protein metabolism. (para 2-34e(4)(d)) 30. Glomerulonephritis. (para 2-30a) End of Lesson 2 MED918 2-45