Magnetic resonance imaging of ligaments and membranes in the
advertisement

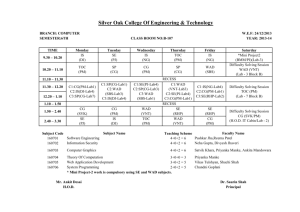
ORIGINAL ARTICLE ACTA RADIOLOGICA Magnetic resonance imaging of ligaments and membranes in the craniocervical junction in whiplash-associated injury and in healthy control subjects REIDAR DULLERUD1,2, ØIVIND GJERTSEN1 & ANDRÉS SERVER1 Department of Neuroradiology, Ullevål University Hospital, Oslo, Norway; 2Department of Radiology, Lovisenberg Diaconal Hospital, Oslo, Norway Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. 1 Background: The pathogenesis and imaging findings in whiplash-associated injury (WAD) are poorly understood and remain debatable. Purpose: To assess the ligaments and membranes in the craniocervical junction with magnetic resonance imaging (MRI) in patients with WAD and to compare them with healthy control subjects. Material and Methods: Twenty-eight patients with WAD were selected at random from a total number of 180 examined with MRI using 2-mm proton density (PD)-weighted images in three orthogonal planes at 1.5T. The patients were compared with 27 healthy control subjects without neck trauma. Results: High signal intensity of the alar and transverse ligaments was quite common and was reported at an average of about 50% both among patients and control subjects. The incidence of abnormalities of the tectorial and posterior atlantooccipital membranes was low in both groups. No statistically significant difference between control subjects and patients with WAD was revealed for any of the structures assessed. Additional fat-suppressed images seemed to reduce the number of reported anomalies. Conclusion: Due to lack of significant differences between patients with WAD and healthy control subjects, it is not recommended that MRI with the current technique and classification system be used in the routine workup of patients with WAD. Key words: Ligaments; MR imaging; spine; trauma Reidar Dullerud, Department of Radiology, Lovisenberg Diaconal Hospital, NO-0440 Oslo, Norway (tel. +47 23 22 56 01 / 92 68 42 58, fax. +47 23 22 56 03, e-mail. redu@lds.no) Submitted December 22, 2008; accepted for publication September 8, 2009 Whiplash-associated disorder (WAD) has become an increasingly important medical condition in recent decades (1–3). The incidence of reported WAD, and the amount of medicolegal issues associated with it, varies considerably between different countries (1, 3, 4). The pathogenesis of whiplash complaints is poorly understood. Most authors agree that it is multifactorial. Prognosis seems to be negatively influenced by female gender, low level of education, and pre-accident neck pain. Type of occupation and other personal, societal, and environmental factors are also possible predictors (2, 3, 5, 6); the severity of injury may influence the outcome as well (6). However, in an English study of subjects exposed to high-energy trauma, whiplash injury was not seen more frequently than neck pain in the general population (7). Treatment strategies in WAD range from conservative methods (8) to extensive surgical interventions with instrumental fixation from the occipital bone to the mid-cervical portion (9). In recent years, attention has been drawn toward imaging of the ligaments and membranes in the craniocervical junction. By magnetic resonance imaging (MRI), these structures can be well visualized (10–15, 16). The purpose of the present study was therefore to assess MRI signal alterations of the ligaments and loss of integrity of the membranes in the craniocervical junction in patients with WAD, and to compare them with uninjured control subjects. Material and Methods Twenty-eight patients, 17 females and 11 males, aged 19–59 years, median 38 years, were selected from a total number of 180 patients with WAD consecutively DOI 10.3109/02841850903321617 © 2010 Informa UK Ltd. (Informa Healthcare, Taylor & Francis AS) 208 R. Dullerud et al. Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. Fig. 1. Alar ligaments (arrows) with low signal intensity, grade 0: sagittal PD (A) and coronal PD (B). examined with MRI from 1 to 7 years after a whiplash injury. All patients were given a number from one to 186. From this list, a random sampling was performed. The patients were compared with 27 uninjured control subjects, 13 females and 14 males, aged 21–66 years, median 36 years. None of the control subjects had a history of severe neck pain or injury to the head or neck. All MRI examinations were carried out using continuous 2-mm interleaved sagittal, coronal, and axial fast spin-echo proton density-weighted (PD) images at 1.5 Tesla with a Siemens Sonata MR unit (Erlangen, Germany), as described by KRÅKENES et al. (11–14). In addition, sagittal images were repeated using PD fat suppression with the following parameters: repetition/ echo time (TR/TE) 2370/11 ms, number of excitations (NEX) 5, field of view (FoV) 230 mm, bandwidth 121 Hz/pixel, acquisition time 7:34 min, matrix 224⫻512 giving a pixel size of 0.6x0.4 mm, in order to differentiate between fat in the ligaments and high-signal alterations caused by edema or fibrosis. All examinations were assessed by three independent neuroradiologists blinded to the classification by their colleagues on a 4-point scale ranging from 0 (normal) to 3 (maximal pathologic change) (11–14). The classification was defined as follows. For alar ligaments, based on maximal cross-section involvement in sagittal images (11): grade 0, low signal throughout entire cross-section (Fig. 1); grade 1, high signal in 1/3 or less of cross-section; grade 2, high signal in 1/3–2/3 of cross-section; grade 3, high signal in 2/3 or more of cross-section (Fig. 2). For the transverse ligament (13): grade 0, ligament with low signal intensity, appearing dark; grade 1, slightly increased signal, well defined or slightly diffuse margins; grade 2, moderately increased signal intensity with or without diffuse margins (Fig. 3); grade 3, markedly increased signal intensity, identical to that of muscle tissue or higher, and ill-defined margins. For the tectorial membrane (12): grade 0, a membrane/dura mater complex thicker than the dura mater alone in all sagittal sections (Fig. 4); grade 1, only dura Acta Radiol 2010 (2) mater left in ⬍1/3 of transverse width1; grade 2, only dura mater left in 1/3 to 2/3 of transverse width; grade 3, only dura mater left in ⬎2/3 of transverse width. For the posterior atlantooccipital membrane (12): grade 0, smooth and well-defined membrane/dura mater complex; grade 1, thinning, minor discontinuity, or a dural hump in ⬍1/3 of transverse width (v. 5); grade 2, as grade 1, affecting 1/3–2/3 of transverse width1; grade 3, discontinuity with or without a dural flap in ⬎2/3 of transverse width. The alar ligaments and the tectorial and posterior atlantooccipital membranes were assessed both with and without fat suppression. In the transverse ligaments, however, the assessment according to the current classification (13) is to a greater extent based on coronal and axial images. Therefore, this ligament was classified based on images without fat suppression only. For the alar and transverse ligaments, interobserver variability was tested with the kappa value. In the tectorial and posterior atlantooccipital membranes, however, the frequency of abnormal findings was too low for a valid kappa-value calculation. Differences between patients and control subjects were calculated with the chi-square test (17). In cases where one of the expected values was below 5, the Fisher exact test was used (17). As the final result, the assessment by one of the authors (Ø.G.) was chosen (Table 1). Results Interobserver agreement was poor among all observers both for the alar ligaments (kappa: 0.05–0.40) and for the transverse ligament (kappa: 0.19–0.20). The classification of the ligaments and membranes of the craniocervical junction in WAD patients and control subjects appears in Table 1. 1 The transverse width was estimated by numbering all images in which the membranes could be appreciated. MRI of the craniocervical junction in WAD patients 209 Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. Fig. 2. Alar ligaments (arrows) with high signal intensity, grade 3 in a healthy control subject: sagittal PD (A) and coronal PD (B). In the alar ligaments, signal alterations were found in 27 of 56 ligaments in the WAD group and in 29 of 54 ligaments in control subjects. The proportion of high signal, including grades 2 and 3, was as high in control subjects as in patients. Imaging with fat suppression reduced the number of ligaments graded 2 and 3, leaving the grade 1 category essentially unchanged. Thus, with fat suppression, the proportion of normal ligaments increased both among patients and control subjects (Fig. 6). High signal or blurred margins were seen in about half of the transverse ligaments in both groups (Fig. 3). The vast majority of both patients and control subjects had normal tectorial membranes (Fig. 4). On imaging without fat suppression, as many as 12 of the atlantooccipital membranes were deemed to be grade 1, both among WAD and control subjects. In both groups, however, a majority of membranes with a discontinuity on imaging without fat suppression were Fig. 3. Transverse ligament (arrows) with grade 2 signal in axial PD of a control subject. well defined on fat-suppressed images. Some other membranes were graded 1 due to the presence of a dural hump (Figs. 4 and 5). Discussion The current MRI technique (14) allows good visual resolution of the ligaments and membranes of the craniocervical junction. All structures were easily recognized in all patients and control subjects. Alar ligaments Both KRÅKENES et al. (11) and MYRAN et al. (15) found satisfactory interobserver agreement in their assessment of the alar ligaments. This differs from our results, which indicate that observer variation may influence the interpretation of the examinations. Using an open Fig. 4. Normal tectorial membrane (arrows) and a posterior atlantooccipital membrane with a small dural hump (arrowheads): sagittal PD of a healthy control subject. Acta Radiol 2010 (2) 210 R. Dullerud et al. This assumption is supported by other studies of the alar ligaments in uninjured subjects demonstrating asymmetry (19) and high signal (18), respectively. Furthermore, biomechanical studies have not provided evidence of alar ligament involvement in whiplash injuries (20). Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. Transverse ligament In a previous study (13), the transverse ligament was deemed normal in 22 of 30 (73%) control subjects compared to only 32 of 92 (36%) in a whiplash group. In our study, however, the proportion of low-signal transverse ligaments was essentially equal and about 50% in both groups. Fig. 5. Dural hump of the posterior atlantooccipital membrane (arrows) in sagittal PD of a control subject. 0.5T MRI unit, ROY et al. (18) also noticed significant interobserver disagreement. In one study, an association between the exposure to whiplash injury and signal alterations of the alar ligaments has been observed (11). Compared to control individuals without a history of head or neck trauma, a higher proportion of WAD patients had high-signal alar ligaments. In the control group of that study, signal alteration grades 2 and 3 were never reported. This strongly differs from the results of MYRAN et al.(15) and our study, which conclude that high signal in the alar ligaments are as common in control subjects as in whiplash patients. Hence, high signal of the alar ligaments may belong to a spectrum of normal variation, and should not be linked to a certain type of trauma. Tectorial and posterior atlantooccipital membranes Significantly more lesions of these structures have been observed in patients than in control subjects in another investigation, as well as a higher overall incidence of abnormalities (12). Our results, however, indicate that lesions of the tectorial and posterior atlantooccipital membranes are rare in both groups. We consider a dural hump of the posterior atlantooccipital membrane, previously assumed to be a traumatic lesion (12), to be a normal variant, which is quite frequently seen on routine examinations of the head and neck in nontraumatized subjects (Figs. 4 and 5). Fat-saturated images Fat-saturated PD imaging is widely used in musculoskeletal MRI. Fat saturation facilitates the differentiation between fat, which is suppressed by this technique, and fibrosis or edema, which retain high signal (21). Table 1. Classification of ligaments and membranes of the craniocervical junction in whiplash-associated injury (WAD) and uninjured control subjects Structure Alar ligaments without fat saturation Alar ligaments with fat saturation Transverse ligament* Tectorial membrane without fat saturation Tectorial membrane with fat saturation Posterior atlantooccipital membrane without fat saturation Posterior atlantooccipital membrane with fat saturation Category 0 1 2 3 Total Chi-square P value WAD control WAD control WAD control WAD control WAD control WAD control WAD control 29 25 35 34 23 26 26 22 26 25 14 14 25 23 11 13 12 11 17 14 2 5 2 2 12 12 3 3 13 12 7 5 16 10 0 0 0 0 1 1 0 1 3 4 2 4 0 4 0 0 0 0 1 0 0 0 56 54 56 54 56 54 28 27 28 27 28 27 28 27 0.718 0.869 2.281 0.515 2.355 0.502 0.195 0.120 0.680 0.486 0.982 0.806 1.066 0.587 *The right and left aspects of the transverse ligament were assessed separately. Acta Radiol 2010 (2) Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. MRI of the craniocervical junction in WAD patients 211 Fig. 6. Sagittal PD of a high-signal alar ligament, grade 3 (arrows) without fat suppression (left). Signal loss on fat suppression (right). High signal of the alar ligaments may, in some cases, be due to fat in the ligaments (Fig. 6). Fat may be a normal component of a ligament, and is frequently seen in other locations, e.g., the anterior cruciate ligament of the knee and the deltoid ligament of the ankle (21). Infiltration by fat may also be caused by inactivity. Further, fat saturation allows for improved delineation of tendons, ligaments, and membranes. In the present study, this was particularly true for the posterior atlantooccipital membrane, which appeared normal using fat saturation in the vast majority of examinations deemed to be grade 1 injury without fat saturation (Table 1). The reduced number of high-signal alar ligaments on fat-suppressed images, and the improved delineation of the posterior atlantooccipital membrane, reducing the proportion of abnormalities reported for both structures, indicate that fat-suppressed sequences ought to be considered in future studies of the craniocervical junction. High MR signal using PD sequences may also be caused by the magic-angle phenomenon, which occurs when examining structures orientated at an angle of 55° to the axis of the magnetic field (21). This may be of relevance for the alar ligaments in some patients. Additional T2-weighted images, which are less prone to this artifact, can solve the problem in equivocal cases. The routine use of longer TE sequences ought to be considered in further studies in WAD. Imaging at 3T and administration of intravenous contrast material also have the potential to improve image quality. At present, a lack of association between exposure to whiplash injury and MR findings has been demonstrated in several studies (10, 15, 16, 18), of which a recent prospective study of the alar ligaments (15) strongly supports our results. In conclusion, we cannot recommend that MRI with the current technique and classification system be used in the routine workup of patients with WAD. References 1. Ferrari R, Obelieniene D, Russel A, Darlington P, Gervais R, Green P. Laypersons’ expectation of the sequelae of whiplash injury. A cross-cultural comparative study between Canada and Lithuania. Med Sci Monit 2002;8:728–34. 2. Hagan KS, Naqui SZ, Lovell ME. Relationship between occupation, social class and time taken off work following whiplash injury. Ann R Coll Surg Engl 2007;89:624–6. 3. Holm LW, Carroll LJ, Cassidy JD, Hogg-Johnsen S, Côte P, Guzman J, et al. The burden and determinants of neck pain in whiplash associated disorders after traffic collisions. Spine 2008;33 Suppl 4:S52–9. 4. Rebbeck T, Sindhusake D, Cameron ID, Rubin G, Feyer AM, Walsh J, et al. A prospective cohort study of health outcomes following whiplash associated disorders in an Australian population. Inj Prev 2006;12:93–8. 5. Berglund A, Bodin L, Jensen I, Wiklund A, Alfredson L. The influence of prognostic factors on neck pain intensity, disability, anxiety and depression over a 2-year period in subjects with acute whiplash injury. Pain 2006;125:244–56. 6. Pape E, Brox JI, Hagen KB, Natvig B, Schirmer H. Prognostic factors for chronic neck pain in persons with minor or moderate injuries in traffic accidents. Accid Anal Prev 2007;39:135–46. 7. Giannoudis PV, Metha SS, Tsiridis E. Incidence and outcome of whiplash injury after multiple trauma. Spine 2007;32:776–81. 8. Cassidy JD, Carroll LJ, Côte P, Frank J. Does multidisiplinary rehabilitation benefit whiplash recovery? Results Acta Radiol 2010 (2) 212 9. 10. 11. 12. Acta Radiol Downloaded from informahealthcare.com by McMaster University on 11/20/10 For personal use only. 13. 14. R. Dullerud et al. of a population-based incidence cohort study. Spine 2007; 32:126–31. Volle E, Montazem A. MRI video diagnosis and surgical therapy of soft tissue trauma to the craniocervical junction. Ear Nose Throat 2001;80:41–8. Karlsborg M, Smed A, Jespersen H, Stephensen S, Cortsen M, Jennum P, et al. A prospective study of 39 patients with whiplash injury. Acta Neurol Scand 1997;95:65–72. Krakenes J, Kaale BR, Moen G, Nordli H, Gilhus NE, Rorvik J. MRI assessment of the alar ligaments in the late stage of whiplash injury: a study of structural abnormalities and observer agreement. Neuroradiology 2002; 44:617–24. Krakenes J, Kaale BR, Moen G, Nordli H, Gilhus NE, Rorvik J. MRI of the tectorial and posterior atlanto-occipital membranes in the late stage of whiplash injury. Neuroradiology 2003;45:585–91. Krakenes J, Kaale BR, Nordli H, Moen G, Rorvik J, Gilhus NE. MR analysis of the transverse ligament in the late stage of whiplash injury. Acta Radiol 2003;44:637–44. Krakenes J, Kaale BR, Rorvik J, Gilhus NE. MRI assessment of normal ligamentous structures in the craniocervical junction. Neuroradiology 2001;43:1089–97. Acta Radiol 2010 (2) 15. Myran R, Kvistad KA, Nygaard OP, Andresen H, Folvik M, Zwart JA. Magnetic resonance imaging assessment of the alar ligaments in whiplash injuries: a case-control study. Spine 2008;33:2012–6. 16. Wilmink JT, Patijn J. MR imaging of alar ligament in whiplash-associated disorder. An observer study. Neuroradiology 2001;43:859–63. 17. Altman DG. Practical statistics for medical research. London: Chapman & Hall; 1991. p. 241, 253. 18. Roy S, Hol PK, Laerum LT, Tillung T. Pitfalls of magnetic resonance imaging of alar ligaments. Neuroradiology 2004;46:392–8. 19. Pfirrmann CWA, Binkert CA, Zanetti M, Boos N, Hodler J. MR morphology of alar ligaments and occipitoatlantoaxial joints. Study in 50 asymptomatic subjects. Radiology 2001;218:133–7. 20. Bitterling H, Stabler A, Bruckmann H. Mystery of alar ligament rupture. Value of MRI in whiplash injuries. Biomechanical, anatomical and clinical studies. Rofo 2007;11:1127–36. 21. Stoller DW. Magnetic resonance imaging in orthopaedics and sports medicine. Baltimore: Lippincott Williams & Wilkins; 2007. p. 1–28, 484.