Blood Vessels
advertisement

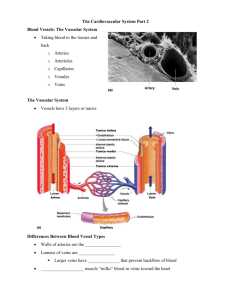
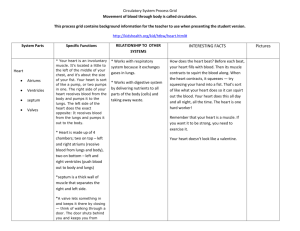
Chapter 19: The Cardiovascular System: Blood Vessels Dr. Renata Uribe Shenzhou University December 2015 FuncEons of the Peripheral CirculaEon • • • • • Carry blood Exchange nutrients, waste products, and gases Transport of hormones Regulate blood pressure Direct blood flow What are Blood Vessels? • Arteries (oxygenated) – Carry blood away from the heart – Branch/diverge – ElasEc, Muscular, Arterioles (into capillaries) • Capillaries – InEmate contact with Essue cells – Exchanges between blood and Essue • Veins (deoxygenated) – Carry blood toward the heart – Merge/converge – Venules, Small Veins, Medium or Large Veins Structure of blood vessel walls } Three disEnct layers (tunics) surrounding the lumen } Tunica in8ma (in8mate with the blood) } Deepest layer } Contains the endothelium (squamous epithelium) } Tunica media } Middle layer } Circularly arranged smooth muscle: maintaining blood pressure– respond to nerve supply à vasodilaEon/vasoconstricEon } Composed of circular smooth muscle allowing constricEon and dilaEon } Tunica externa (adven88a, outer most) } Superficial layer } Composed of collagen fibers loosely arranged } ProtecEon, anchoring it to surrounding structures } In large arteries the tunica externa contains ‘vasa vasorum’ (vessels of the vessels), that nourish the vessel wall. ElasEc Arteries • • • • Largest arteries (Aorta) Walls relaEvely thin – more elasEc Essue than muscle FuncEon as PRESSURE RESERVOIR Help propel blood forward while ventricles relaxing, also known as CONDUCTING ARTERIES – conduct blood to medium-­‐sized arteries MUSCULAR ARTERIES MUSCULAR ARTERIES • • Tunica media contains more smooth muscle and fewer elasEc fibers than elasEc arteries • Capable of vasoconstric8on/vasodila8on to adjust rate of blood flow • Also called distribuEng arteries – directs blood to different areas of the body • Anastomoses • Union of the branches of 2 or more arteries supplying the same body region • Provide alternate routes – collateral circulaEon • • • • ARTERIOLES Transport blood from small arteries to capillaries Smallest arteries where the 3 tunics can be differenEated Like small arteries – capable of vasoconstricEon and dilaEon Resistance vessels – help to maintain blood pressure Arterial System • Elas8c artery – Thick walls arteries near the heart with low resistance – Contain more elasEn than other arteries – Pressure reservoirs: expand and recoiling as blood is ejected from the heart, to make sure that blood flows conEnuously and to protect smaller vessels from high pressure. • Muscular artery – – – – • Merge from elasEc arteries Deliver blood to body organs Have thickest tunica medias, Less distensible Respond by constricEon ad dilaEon Arteriole – Few elasEc layers – Respond to hormonal and neural control to constrict and dilate controlling flow into the capillary bed – Are responsible for distribuEon of blood flow – Tunica media is smooth muscle with a few elasEc fibers Capillaries • The smallest blood vessels • Capillary wall = endothelial cells (simple squamous epithelium) • Just a thin tunica inEma • Some spider-­‐shaped smooth muscle-­‐like cells (pericytes) stabilize the capillary wall and help control permeability • Direct acces to nearly every cell • Exchange of materials between blood and intersEEal fluid • Substances move through capillaries by diffusion – Lipid-­‐soluble vs water soluble substances – RBCs to pass though capillary single file ConEnuous Capillaries • Most common, found in skin and muscles • Uninterrupted endothelial lining (Eght juncEons) • JuncEons leave intercellular clegs allowing limited passage of fluids and small solutes • In the brain the Eght juncEons are complete – Blood-­‐brain barrier Fenestrated Capillaries • Some of endothelial cells have oval pores • Much more permeable, larger gaps • Found in the kidney, where blood is filtrated Sinusoids • • • • Highly modified leaky capillaries Liver, bone marrow Fenestrated, allowing large molecules and blood cells to pass Phagocytes are ogen located just outside to pick up material Capillary Beds: MicrocirculaEon • Arterial capillaries conEnue into venous capillaries • Capillary networks are more extensive in highly metabolic Essues like lungs, cardiac muscle, liver, kidneys, skeletal muscle • Precapillary sphincters (in metarterioles) composed of smooth muscle cells regulates blood flow -­‐ At the root of the capillary there is a precapillary sphincter, serving as a valve to regulate blood flow and distribuEon • Example: ThermoregulaEon in skin Venous System • Venules – Are formed where capillaries unite – Very porous: fluid and white blood cells move through the walls. – Composed of mainly endothelium with one to two small layers of smooth muscle – Venules drain into small veins Venous System VEINS: Structural changes not as disEnct as in arteries In general, very thin walls in relaEon to total diameter Same 3 layers: – Tunica interna – thinner than arteries – Tunica media – thinner with lihle smooth muscle – Tunica externa – thickest layer • Not designed to withstand high pressure • Valves – folds on tunica interna forming cusps – Aid in venous return by prevenEng backflow • • • • Valves • Folds in inEma form 2 flaps that overlap • More valves in veins of lower extremiEes than in veins of upper extremiEes (Why?) • Varicose veins (defecEve valves) • Phlebi8s (inflammaEon of veins) VARICOSE VEINS in lower limb; causes • Occur due to incompetent valves include pregnancy, prolonged standing on hard floors, right sided heart failure Aging of the Arteries • Arteriosclerosis: General term for degeneraEon changes in arteries making them less elasEc; hardening of the arteries; increases resistance to blood flow causing increased BP and increased work to heart • Atherosclerosis: deposiEon of fahy plaque on walls Atherosclerosis • A form of arteriosclerosis (hardening of arteries) • In atherosclerosis the artery wall thickens as the result of deposit of fahy materials • Responsible for most heart ahacks and strokes • Risk factors: – Advanced age, male sex, family history, diabetes, tobacco smoking, hypertension, obesity, stress Atherosclerosis 1. The endothelium is injured causing an inflammatory process 2. Lipids (cholesterol) accumulate and oxidize in the tunica inEma, this ahracts macrophages which transform into lipid-­‐ laden foam cells forming a fahy streak. 3. Smooth muscle cells proliferate and a fibrous cap covers the fahy material: atheroscleroEc plaque 4. Plaque becomes unstable: enlarges, the core dies, calcium deposiEon. Vessel is constricted, the walls ulcerate, the rigidity leads to hypertension. Atherosclerosis DIFFUSION • • MOST IMPORTANT METHOD SUBSTANCES MOVE DOWN THEIR CONCENTRATION GRADIENT (from high to low) – O2 and nutrients diffuse from blood to intersEEal fluid to body cells – CO2 and wastes diffuse from body cells to intersEEal fluid to blood • Can cross capillary wall through intracellular clegs, fenestraEons through endothelial cells – Most plasma proteins cannot cross – except in sinusoids (proteins and even blood cells leave) BULK FLOW • Passive process in which large numbers of ions, molecules, or parEcles in a fluid move together in the same direcEon • Based on pressure gradient • Diffusion is more important for solute exchange • Bulk flow more important for regulaEon of relaEve volumes of blood and intersEEal fluid • Filtra8on – from capillaries into intersEEal fluid 8pressure inside the blood vessels • Reabsorp8on – from intersEEal fluid into capillaries Physiology of CirculaEon • Blood Flow: volume of blood flowing trough a vessel/organ or enEre circulaEon in a given period of Eme (ml/min) • Blood Pressure: force per unit area exerted on a vessel wall by the contained blood (mmHg), differences in blood pressure are the driving force for flow. – Systemic arterial blood pressure in the largest arteries near the heart • Resistance – opposiEon to flow, measure of the amount of fricEon blood encounters as it passes through vessels – Blood viscosity – thickness of fluid – Blood vessel length – longer the vessel, greater the resistance – Blood vessel diameter – smaller the diameter, greater the resistance RelaEonship Between Flow, Pressure and Risistance • Flow (F) in ml/min • Difference in Pressure (ΔP) • Resistance (R) • Blood flows from a higher to a lower pressure, the bigger the difference, the higher the flow • The higher the resistance, the lower the flow • Resistance is more important because it’s less stable. HydrostaEc and OsmoEc Pressure • Hydrosta8c Pressure: the force exerted by a fluid pressing against a wall – When capillary hydrostaEc pressure > intersEEal hydrostaEc pressure, fluid will flow out of the capillary into the intersEEal space – However, since lymph vessels constantly withdraw intersEEal fluid, the capillary hydrostaEc pressure is always higher • Colloid Osmo8c Pressure – Nondiffusable molecules ahract water – Capillary colloid osmoEc pressure: dependent on plasma proteins – IntersEEal fluid contains few proteins. Pressure in the capillary beds • AT ARTERIAL END – HydrostaEc pressure is greater than osmoEc pressure – Net movement of fluid out of capillary • AT VENOUS END – HydrostaEc pressure is less than osmoEc pressure Net FiltraEon Pressure • So how does it work? – The difference between capillary and intersEEal HydrostaEc Pressure – The difference between capillary and intersEEal Colloid OsmoEc Pressure • When NFP>0 the direcEon of flow is out of the capillary into the intersEEal fluid and vice versa. Systemic Blood Pressure • • • • • • Closer blood to heart à greater pressure ContracEon of ventricles generates BP Reflects two factors – Artery compliance – stretchability – Volume of blood Systolic pressure – Measured as leg ventricle contracts expelling blood into the aorta – Average 120mmHg – Highest pressure ahained in arteries during systole Diastolic pressure – Measured as the aorEc SL valve closes and ventricles relaxes – Aorta recoils to maintain enough pressure to push blood to capillaries, when the heart is not ejecEng but being filled – Average 70-­‐80 mmHg – Lowest arterial pressure during diastole Pulse pressure -­‐ The difference between the two. – Throbbing pulsaEon in an artery – Occurs as blood forced into elasEc arteries during ventricular contracEon Systemic Blood Pressure • Pressure falls progressively with distance from leg ventricle AlteraEons in Blood Pressure • Hypertension (>140/90): Dangerous disease, damages heart and vessels (atherosclerosis). “Silent Killer” – Primary (90%): heredity, diet, obesity, age, diabetes, stress, smoking – Secondary (10%): due to idenEfiable disorders (kidneys, endocrine disorders) • Hypotension (systolic <100): Associated with old age free of cardiovascular illness – OrthostaEc hypotension: dizziness when suddenly rising – Chronic hypotension: poor nutriEon, hypothyroidism Sites to take the pulse