Outpatient Surgery Instructions - Los Olivos Women's Medical Group
advertisement

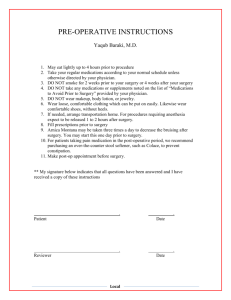
Outpatient Surgery Instructions Prior to your surgery Stop taking aspirin, ibuprofen or any of the non-steroidal anti-inflammatory medications that can inhibit blood clotting one week prior to your surgery. Using Tylenol until the time of surgery is acceptable. The pre-operative appointment is the time when your physician will answer all of your questions. Bring a current list of your medications and drug allergies to this appointment. Your surgeon will discuss the surgical procedure with the risks, benefits and alternatives to the surgery you will be undergoing. You will be asked to sign surgical consents. Additional consents are necessary for tubal ligation and hysterectomy if applicable. A copy of the consent will be provided for you to bring to the hospital. Consider taking a stool softener 2-3 days prior to your procedure and after your procedure. If you are taking pain medication (narcotics), constipation is a common post-operative complaint. Benefiber, Colace and Fibercon are common stool softeners. Ibuprofen (maximum dose 2400 mg/day) taken with narcotics will enhance pain relief without increasing the narcotic side effects (drowsiness, constipation). You can purchase ibuprofen without a prescription and start it when you are discharged. The evening before surgery Do not eat or drink anything eight hours before surgery unless directed by your surgeon or anesthesiologist. Take your usual medication in the morning with a sip of water. The anesthesiologist will call you on the night prior to your surgery to discuss your anesthetic. Be prepared to discuss your health history including any drug allergies, previous anesthetics and any medications you take. You can visit the anesthesiologist’s website at www.groupanesthesia.com. If you will not be home the night prior to surgery, please call their office during the day at (408) 354-2114 and leave an alternate phone number. Surgery The outpatient surgical centers request that you check in one hour prior to your surgery. The pre-operative area nurses will ask you your health history and take your vital signs. They will give you a special surgical gown. You will be asked to sign a facility surgical consent for your operation and for the anesthetic. The nurses will ask you to remove any dentures, hearing aids, contact lenses, wigs and jewelry that you may be wearing. Once the operation is over, you will be moved into the recovery area. This area is specially equipped for monitoring patients after surgery. With your permission, your surgeon will meet your family in the waiting area to discuss your health. You will not remember much about what you are told on the day of surgery due to medications that you are given both before and after the surgery. If you had a miscarriage or an ectopic pregnancy and are blood type Rh negative, you should have a Rhogam shot unless your partner is also Rh negative. Recovery at Home After outpatient surgery, you will probably be able to go home within 1-2 hours. It is recommended that you not drive for 24 hours after outpatient surgery. Take pain medication as needed. Ibuprofen (up to 2400 mg/24 hours) acts to enhance narcotics and may be recommended in addition to a narcotic. Tylenol may also be sufficient. Resume all of your usual medications as previously prescribed. Procedures involving abdominal surgery may cause post-operative gas pains and several days to recover normal bowel function. If you are constipated, use a Ducolax suppository or Fleets enema as a laxative. A stool softener (Colace, Benefiber and Fibercon) may also be helpful during recovery. Side effects of the narcotics include drowsiness, constipation and nausea. Anti-inflammatory medications decrease uterine cramping more than narcotic medications. Your doctor may recommend a special diet for recovery from some operations. A low fat, bland diet is best. Avoid highly spiced or acidic foods. Drink more water daily than you are used to drinking. Avoid carbonated beverages. Narcotics can cause constipation so increase natural fiber or consider a stool softener, as needed. Remove simple band-aids from incisions in 6-10 hours. There is no need to cover incisions unless they are oozing. A small amount of drainage or bleeding is normal. Pain and bruising around the incisions are normal after surgery. Steri-strips should be removed 3-5 days after surgery. If you had a laparoscopy and have visible sutures, make an appointment for suture removal in 3-5 days. Glue can be removed from incisions in 3-5 days. After a vaginal procedure, do not have intercourse or douche, and do not use tampons until bleeding has stopped (3-7 days). Some patients have no bleeding and this also is normal. You may shower or take a bath on the day following surgery. Do not use ointments, topical antibiotics, or peroxide on the wound unless you are directed to do so. If your skin folds over the incision, keep the skin separated with clean dry gauze or a peripad. You may also use a hair dryer to keep the incision dry. You may resume normal activity, unless otherwise directed. Use common sense. Do not drive while taking narcotics. Make a follow-up appointment with your physician one to two weeks after surgery. Warning signs Call the office for a temperature over 101 degrees, severe pain, nausea, vomiting, urinary burning, or increasing redness around the incisions. Do not hesitate to call Los Olivos (408) 356-0431 if you have any other questions.