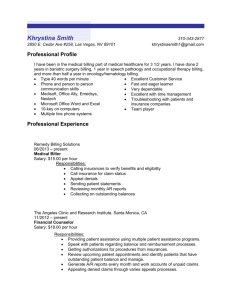
Example Medical Billing Skills
advertisement

MEDICAL BILLING/CODING SKILLS • Process insurance claim forms • Assign medical codes • Operate databases and medical billing software • Current on HIPAA regulations • Proper use of ICD-9, CPT and HCPCS codes • Receive and complete medical claim forms • Answer inquiries from doctors, patients and insurance companies • Collect medical information such as diagnosis, prognosis and dates of treatment from patient records • Understand insurance guidelines including Medicare and other government, private, self-insurance, and managed-care plans • Knowledgeable in medical terminology and hospital, clinic, or laboratory procedures • Schedule appointments and bill patients • Compile and record medical charts, reports, and correspondence • • • • • • • • • • • • Answer customer billing inquiries Explain billing policies to customers Maintain patient records Produce income & statistical reports Coordinate invoicing for 8 doctors Develop and implement billing policies and procedures Prepare accounting records Maintain patient records Answer customer billing inquiries Investigate customer complaints Coordinate invoicing for 6 doctors Submit insurance claim forms • Maintained patients’ documents and addresses • Maintained the patient's information, reports, income reports and statistics with balancing the daily schedule • Developed the forms and manuals and procedure of organization • Processed patient's billing, statements, reimbursement claims, post transaction and data • Handle inquiries and respond via telephone or in writing • Distribute reports, answer the telephone and generate bills • Prepared records of accounting, reports of registration, results of investigation etc • Maintained records of patients, billing instructions etc • Maintained the special bill's lists, customers account, etc • Answer customers’ inquiries, complaints and problems • Kept detailed records such as prepaid vouchers, overpayment and incorporate charges shown on customer account Member, American Academy of Professional Coders (AAPC), 2011 – present Member, Healthcare Billing & Management Association (HBMA), 2011 – present Job Descriptions Job 1: Works daily with patients and staff to ensure timely and accurate billing of patient charges to all types of payers public and private. Uses knowledge of the Federally Qualified Healthcare Clinic (FQHC) prospective payment system and "wrap-around" as well as sliding scales to bill effectively. Collects revenues as needed. Provides reports to management per schedule. Works with diverse populations and must consistently function well in an environment that includes varying and often unpredictable circumstances while exercising appropriate critical thinking and judgment skills. This is a high-attendance position requiring minimal absences, sick time and late arrivals. ESSENTIAL DUTIES AND RESPONSIBILITIES: Serves as a role model in action and word for the Organizations mission and beliefs. Maintains highest degree of confidentiality in patient, staff and management matters. Remains up to date on best practices relevant to the position; enhances personal skills. Provides courteous and timely assistance to patients and coworkers. Meets time and attendance requirements for the position and uses work hours productively and appropriately. This is a high-attendance position. Meets all safety protocols and medical practice standards. Must be able to communicate well with staff volunteers and clients. Perform as a team member fostering an environment of cooperation among team members. Conserves resources and materials. OTHER RESPONSIBILITIES: Bills Medi-Cal, Medicare, CHDP, FPACT and CDP and other payers. Processes billing to/from all payers in a timely manner as directed by SWO. Maintains accounts accurately and keeps them up to date. Generates reports accurately and timely. Reconciliation of all superbills and/or Encounters as directed by Standard Work Orders (SWO). Enter all reimbursements from the Explanation of Benefits forms into the Practice Management system. Keeps data entry for clinic current, accurate; provides monthly reports. Processes billing for BCEDP. Enter bills under the correct billing code. Post all accounts in a timely manner. Follows up with collections as needed. COMPUTER & EQUIPMENT SKILLS: Uses electronic medical record software (Allscripts) Uses Word, Excel, Outlook and Internet software proficiently Strong knowledge of computer operations, proficiently uses a keyboard and calculator Strong knowledge of medical terminology, ICD-9 and CPT codes EDUCATION and / or EXPERIENCE: At least three years of experience in high-volume and broad-based billing environment. High school diploma required; literacy and math skills at the 12-grade level. Certified biller coder. Fluent Spanish speaker REASONING and MENTAL ABILITY: Uses planning and evaluation skills to develop successful strategies and tactics. Uses critical thinking skills to interpret information furnished in written, oral, diagram, or schedule formMakes sound decisions and sets goals based on available information and evaluates situations and requirements to plan and adjust work accordingly. Projects accurate future occurrences based on current or historic data. Must be able to perform well under pressure in a very busy medical clinic. Needs to be very detailed oriented and punctual! Must be have a Positive attitude and great customer service skills. Job 2: Understand full cycle billing, and must be well versed in Government/Commercial insurances. Qualified candidates must have experience working Texas Medicaid accounts. Must be able to review Medicaid and Commercial payor denials and re-file claims as needed. Review payments to ensure accurate payments have been received. Job 3: Currently seeking a medical biller/coder. You must have ICD-9-CM/CPT coding experience. Experience in coding and abstracting, working knowledge of Diagnosis Related Groups (DRGs), Prospective Payment Systems, and Medicare coverage guidelines is required. Must have current certification credentials in coding. This is a fantastic opportunity for a dynamic individual that is looking for career growth! If this is what you are looking for...APPLY TODAY! We are an equal employment opportunity employer. Job 4: Hospital Medical Biller/Coder ... join a corporate casual company that will actually value your team involvement, diligence at details, independent focus and demand for accuracy. This deadline oriented environment will rely upon your Medical Billing/Coding knowledge ... Certified Medical Biller (or very close to completion) WITHOUT experience welcome to apply. This is a great opportunity to LEARN and GROW! Hours are either 7am-4pm or 8am-5pm, Monday-Friday. Earn up to $13/hour (depending on experience) and enjoy great benefits including major medical, vision, paid vacations/holidays, and quarterly performance bonuses. Hospital Medical Biller/Coder will: • • • • audit hospital bills submitted through Medicare, following up on all insurance claims for billing through final resolution ensure proper codes are listed in the claims; correct/reclassify coding in Excel if necessary and repost for billing identify and resolve discrepancies and claims delay issues that impact billing and collections prepare and submit medical claims electronically Requirements: Hospital Medical Biller/Coder requirements: • • • • • • • Medical Billing/Coding Certification (or very close to certification) an absolute must exposure to ICD-9, hospital coding and Medicare applications highly preferred ability to independently meet tight deadlines in a project based atmosphere dependable work ethics with excellent attendance good troubleshooting skills strong attention to details proficiency with Excel Transferrable Skills: (These are things that you may have done in other jobs that are transferrable to the job you are seeking) Clerical Organizational Computer Detail-Oriented