Correction is highlighted
advertisement
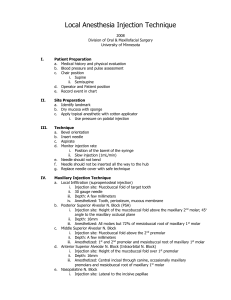
Canine and first premolar on the side of the injection You need to give a long buccal injection in order to extract the molars and second bicuspid. For operative procedures, a long buccal injection may not be needed for these teeth. The long buccal injection anesthetizes the soft tissue and periosteum buccal to the mandibular molar teeth. The needle is inserted in the mucous membrane distal and buccal to the most distal molar in the arch. To anesthetize the lingual nerve: When administering an inferior alveolar nerve block slowly withdraw the syringe, and when approximately half its length remains within tissues, reaspirate. If negative, deposit a portion of the remaining solution (0.1 ml) to anesthetize the lingual nerve. Incisors may need local infiltration for extractions. Other Techniques of Mandibular Anesthesia: • Mental nerve block: This nerve block is used when buccal soft-tissue anesthesia is necessary anterior to the mental foramen (around the second premolar) to the midline and skin of the lower lip and chin. The needle is inserted in mucobuccal fold at or just anterior to the mental foramen. Target area: mental nerve as it exits the mental foramen (usually located between the apices of the first and second premolars). • Vazirani-Alkinosi closed-mouth mandibular block: although this technique can be used whenever mandibular anesthesia is desired, its primary indication remains those situations in which limited mandibular opening (i.e., patients with trismus) precludes the use of other mandibular techniques. Nerves anesthetized: inferior alveolar, incisive, mental, lingual, mylohyoid nerves. Area of needle insertion: soft tissue overlying the medial (lingual) border of the mandibular ramus directly adjacent to the maxillary tuberosity at the height of the mucogingival junction adjacent to the maxillary third molar. Note: The injection is performed blindly because no bony endpoints exists, the needle is advanced 25 mm into tissue (for an averagesized adult). The distance is measured from the maxillary tuberosity. • The Gow-Gates technique: this technique is a true mandibular nerve block because it provides sensory anesthesia to virtually the entire distribution of V3 (inferior alveolar, lingual, mylohyoid, mental, incisive, auriculotemporal, and buccal nerves). Its primary use is when a conventional inferior alveolar nerve block is unsuccessful. Note: Patient must extend his or her neck and open wide for the duration of the technique (the condyle then assumes a more frontal position and is closer to the mandibular nerve trunk). Extraoral landmarks: corner of mouth, tragus of ear, and intertragic notch Area of needle insertion: the needle is positioned so that it is inserted just distal to the maxillary second molar at the height of its mesiolingual cusp. The needle is slowly advance until bone (neck of the condyle) is contacted. The average depth of softtissue penetration to bone is 25 mm. The needle tip is withdrawn 1 mm, aspirate, and slowly deposit solution.