impact of the superficial tangential zone in cartilage on tissue
advertisement

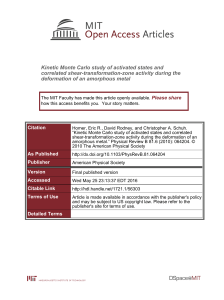
IMPACT OF THE SUPERFICIAL TANGENTIAL ZONE IN CARTILAGE ON TISSUE ENGINEERING EFFORTS *Owen, JR; +*Wayne, JS +*Orthopaedic Research Laboratory, Departments of Orthopaedic Surgery and Biomedical Engineering Virginia Commonwealth University, Richmond, Virginia jswayne@vcu.edu transplanted material with a quality STZ may provide an improved mechanical environment for appropriate mechanotransduction signals in the entire repairing region, even for repair tissue with inferior mechanical properties. A viable STZ may be critical in achieving the long-term survival of repairing cartilage. ISOTI REP 2 Negative Flow rate REPTI 2.5 E-02 µm/sec 1, 3 0 Figure 1: Radial effective fluid velocity after 30 sec of loading. Deformation scale factor = 1. Only a 6mm radius is shown. REP REPT I 0.12 8% 0.1 6% 0.08 0.06 4% 2% MPa ISOT I 10% Percent Compression INTRODUCTION: Much effort is being devoted to create replacement tissue for repair of defects in articular surfaces. While some success has been realized, the normal zonal characteristics of articular cartilage throughout its thickness, particularly the superficial tangential zone (STZ), and normal material properties have not been reproduced in vitro in scaffolds nor in vivo in repairing defects. Without sufficient quality, the fate of such transplanted scaffolds in vivo may be doomed mechanically from the outset. Removal of the STZ from normal cartilage has been shown to negatively affect the remaining cartilage’s ability to support axial loads and retain fluids [1-3]. Previous studies have modeled excessive axial deformation of repair cartilage [4-5]. Other studies have shown that modeling the STZ of normal cartilage as transversely isotropic provides better agreement with indentation experimental results than isotropic models [6-9]. This finite element study examines the role of transverse isotropy on the behavior of a normal and repaired articular surfaces under contact loading. METHODS: Using ABAQUS® (version 6.4) finite element analysis software, a 2D axi-symmetric model (2760 quadratic quadrilateral pore fluid/stress elements, 8808 nodes) was developed to represent a cartilage surface 12mm radius and 1mm thick. The model was divided into regions simulating naturally occurring zones (e.g. STZ=20%, middle and deep=80%). A 3mm radius region was created in the center to allow simulation of a repair cartilage plug for specific repair models. Mesh was refined in areas expected to have large gradients. Material properties comparable to those found in the literature [9] were assigned to the regions as dictated by the scenarios (Table 1). A 5N load was applied in ramp fashion over 0.5 sec to a 400mm radius impermeable rigid sphere (E=200GPa, ν=0.3), which transferred load to the center of the model’s articular surface. The load was then held constant for 30 sec to evaluate short-term creep. Zero axial fluid flow was prescribed in the contact region, while zero pore pressure was maintained on the articular surface outside of the contact area and along the outer radial surfaces to ensure unrestricted fluid flow. Three scenarios were investigated: ISOTI: Normal isotropic cartilage in the middle and deep zones. Normal transversely isotropic cartilage was modeled for the STZ. The plane of isotropy was parallel to the articular surface with a higher modulus in the radial direction. REP: Repair isotropic cartilage in a central 3mm radius region through the middle, deep, and STZ zones. Normal isotropic cartilage in the middle and deep zones outside of the repair area. Normal transversely isotropic cartilage in the STZ outside of the repair area. REPTI: Repair cartilage in a central 3mm radius region going only through the middle and deep zones. Normal isotropic cartilage in the middle and deep zones outside of the repair area. Normal transversely isotropic cartilage in the STZ, covering the entire geometry. RESULTS: Abnormal radial flow occurred in the repair region of REP. At the interface between normal and repair, negative radial flow occurred. The presence of a normal STZ in REPTI restored outward radial flow in the repair (Fig 1). Compared to ISOTI, REP (without STZ) resulted in a 32% increase in full axial compression, in more than doubling of compression in its’ STZ region (top 20%), in large reductions in von Mises stress on the center of the articular surface and immediately beneath the STZ region (64% and 87%, respectively), and a 26% reduction in fluid pressure at the bottom center of the model (Fig 2). As compared to REP, placing an STZ over the repair in REPTI improved surface and underlying stresses by a factor of 2.5 and 2.3, respectively. Fluid pressure improved by 21%, axial and STZ compressions were reduced by 20% and 69%, respectively. DISCUSSION: This analysis predicts a reduction in axial deformation, in von Mises stress on the articular surface and in underlying repair tissue, and an increase in repair pore pressure when a transversely isotropic STZ is in place over the region of repair. Previous studies that have emphasized the importance of the STZ in normal cartilage [1-3] support these findings. Prescribing unrestricted axial flow has indicated that strain-dependent permeability in the STZ is an important factor in protecting underlying tissues [10]. In-vivo conditions likely allow some axial flow out of the tissue. This study strongly suggests that 0.04 0.02 0% 0 Full ST Z Surface Repair Fluid Figure 2: Full thickness and STZ axial compression; von Mises stress on the articular surface and in the repair beneath the STZ; fluid pressure at the bottom of the repair region after 30 sec of creep. Material Normal Repair Normal Material Property Iso Iso Trans-Iso 0.46 0.1 5.8 E1 and E3 (MPa) 0.46 0.1 0.46 E2 (MPa) 0 0 0 νp (in-plane) 0 0 0 νtp (transverse) N/A N/A 2.9 Gp (MPa) N/A N/A 0.37 Gt (MPa) 5.1 10 5.1 k (x10-15m4/N-s) 4 4 4 Initial Void Ratio νp=ν13=ν31; νtp=ν21=ν23; νpt=ν12=ν32; Gp=G13; Gt=G12=G23 Table 1: Material properties assigned to respective regions. (Iso ≡ isotropic; Trans-Iso ≡ transversely isotropic) REFERENCES: [1] Glazer, C, et al, Osteoarthritis Cart, Feb; 10(2):83-99, 2002. [2] Torzilli, P, et al, Med Biol Eng Comput. Jul; 31 Suppl:S93-8, 1993. [3] Torzilli, P, et al, J. Biomech, 16(3):169-79, 1983. [4] Smith, C, et al, 47th Ann Mtg ORS, 2001. [5] Wayne, J, et al, Proc Inst Mech Eng, 205(3):155-62,1992. [6] Korhonen, R, et al, Med Eng Phys, 24, 99-108, 2002. [7] Mow, V, et al, 46th Ann Mtg ORS, 2000. [8] Gardner, T, et al, ASME Bioengr. Div. 2003 Summer Conf. [9] Cohen, B, 39th Ann Mtg ORS, 1993. [10] Owen, J and Wayne, J, ASME Bioengr. Div. 2005 Summer Conf. 52nd Annual Meeting of the Orthopaedic Research Society Paper No: 1436