nbrc-written-rrt-ex#247E706.ppt [Read
advertisement
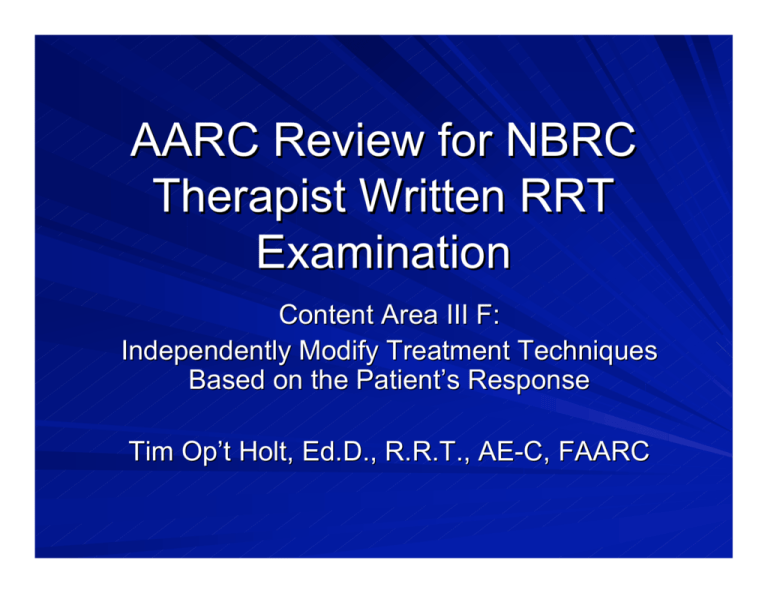
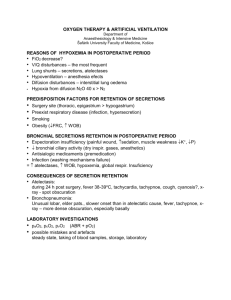
AARC Review for NBRC Therapist Written RRT Examination Content Area III F: Independently Modify Treatment Techniques Based on the Patient’s Response Tim Op’t Holt, Ed.D., R.R.T., AE-C, FAARC Goal Through patient scenarios and didactic information, the participant will be able to prepare for the NBRC Therapist Written RRT Examination content outline section III F: Independently Modify Treatment Techniques Based on the Patient’s Response Objectives The participant will be able to independently modify the following therapies, based on patient response: – Lung expansion therapy – Bland and medicated aerosol therapy – Gas therapy – Tracheobronchial hygiene, to include artificial airway care and suctioning – Maintenance of alarm settings and mechanical dead space during mechanical ventilation Section Outline 1. Lung expansion therapy 2. Bland and medicated aerosol therapy 3. Oxygen therapy 4. Gas therapy 5. Tracheobronchial hygiene, to include artificial airway care and suctioning 6. Maintenance of alarm settings and mechanical dead space during mechanical ventilation Section 1: Lung Expansion Therapy Resorption atelectasis – Associated with mucus plugging Passive atelectasis – Associated with decreased, monotonous tidal volume and postoperative inactivity – Alveoli shrink due to absence of periodic hyperinflation, tachypnea, and hypopnea – Surface tension increases to the point of alveolar collapse Section 1: Lung Expansion Therapy Clinical signs of atelectasis – Hypoxemia – Dyspnea – Decreased breath sounds and late inspiratory crackles – Bronchial breath sounds as atelectasis worsens – Tachycardia – Fever may be present, but not always Section 1: Lung Expansion Therapy Selection of appropriate technique – Indications for Incentive spirometry Atelectasis Conditions predisposing to atelectasis such as upper abdominal or thoracic surgery Restrictive lung defects associated with quadriplegia and/or dysfunctional diaphragm – Patient characteristics Able to cooperate and understand instructions Able to generate at least 33% of the predicted IC Section 1: Lung Expansion Therapy Selection of appropriate technique – Indications for IPPB Atelectasis not responsive to other therapies Patients unable to understand or participate in other therapy for atelectasis or administration of aerosol medications – Patient characteristics Obtundation, weakness Pain, incompletely controlled by analgesia, resulting in insufficient deep breathing Unable to generate at least 33% of predicted IC Section 1: Lung Expansion Therapy Modifying IPPB technique Patient response Modification/intervention Dizziness Leaks Ask the patient to slow their breathing rate Decrease goal pressure or volume Use a mouth seal or face mask Section 1: Lung Expansion Therapy Modifying IPPB technique Patient response Inspiratory time too short Inspiratory time too long Inadequate chest excursion Pain, discomfort Modification/intervention Decrease inspiratory flow Increase inspiratory flow Increase pressure or volume Decrease pressure or flow Section 1: Lung Expansion Therapy Modifying IPPB technique Patient response Modification/intervention Hypotension Sudden unconsciousness Onset of chest pain Hemoptysis Gastric distention Discontinue treatment and notify physician Assure adequate oxygenation and ventilation Decrease goal volume or pressure Section 1: Lung Expansion Therapy Modifying IS technique Patient response Modification/intervention Dizziness, tingling in fingers, fatigue Pain Ask the patient to slow their breathing rate Assist patient with splinting of operative site, assure adequate analgesia Section 1: Lung Expansion Therapy Modifying IS technique Patient response Modification/intervention Unable to achieve goal volume Assist patient with splinting of operative site Assure adequate analgesia Temporarily decrease goal volume, assure patient Section 1: Lung Expansion Therapy History and physical A 54-year-old previously healthy female was referred to a surgeon and presented with abdominal pain that had previously been treated medically without relief. Abdominal palpation revealed mid-abdominal pain. On admission the following information was available: T = 99.0°F P = 88/min R = 14/min SpO2 = 99% Height = 66” Weight = 78 kg (175 lbs) Section 1: Lung Expansion Therapy An exploratory laparotomy resulted in a large midline abdominal incision. The incision was closed and dressed. Following surgery, there was a small amount of serosanguinous drainage into the dressing. www.pvss.org/ Cases/renal/2.jpg Section 1: Lung Expansion Therapy The respiratory therapist was called to evaluate and treat the patient postoperatively. Three hours postoperatively, vital signs were: – – – – T = 100.8°F P = 98/min R = 20/min and shallow Room air SpO2 = 92%; 98% with 3L/min. nasal cannula Physical examination revealed the following: – Observation revealed an awake, drowsy female, with abdominal pain. Minimal abdominal excursion, fair chest wall excursion, unable to take a deep breath. Weak, dry cough. Section 1: Lung Expansion Therapy – Abdominal pain on palpation, no abdominal excursion, 2 cm. chest wall excursion. – Breath sounds clear and decreased to auscultation in the apices; crackles in the left base. – A chest radiograph revealed the following: http://www.meddean.luc.edu/lumen/meded/medicine/pulmonar/images/cxr2/80a.jpg Section 1: Lung Expansion Therapy The initial order was for incentive spirometry, q1° while awake Measured Inspiratory Capacity = 700 mL Section 1: Lung Expansion Therapy Question 1 Using the data given in this case scenario, what therapy should the therapist perform? A. Incentive spirometry, q1 hour. B. Chest physical therapy to the LUL and LLL C. IPPB with a goal volume of 2.0L D. IPPB with a pressure of 10 cm H2O Section 1: Lung Expansion Therapy Question 2 During IPPB, the patient complains of abdominal pain and states, ”the breath is too long.” The therapist’s most appropriate actions are to: I. Contact the nurse for an analgesic II. Increase the inspiratory flow III. Decrease the peak pressure IV. Use a mask to deliver the therapy A. I, II only B. II, III only C. III, IV only D. I, III only Section 1: Lung Expansion Therapy Question 3 During IPPB with a pressure-controlled ventilator, the therapist measures a volume of 1.0L. To obtain a volume of 1.5L, the therapist should increase the: A. tidal volume setting B. inspiratory flow C. inspiratory pressure D. trigger sensitivity Section 1: Lung Expansion Therapy Question 4 Thirty-six hours after surgery, the patient has an inspiratory capacity of 1.1L. What is the therapist’s most appropriate action? A. Increase the inspiratory pressure during IPPB B. Add chest physical therapy to the left chest C. Change therapy to incentive spirometry with a goal of 2.0L, q1 hour. D. Change therapy to coughing and deep breathing every hour. Section 1: Lung Expansion Therapy Question 5 The patient is performing incentive spirometry and complains of tingling in her fingers and dizziness. The therapist should: A. explain that this is a normal outcome of therapy. B. encourage the patient to slow her breathing rate. C. pause 5 seconds at the end of each inspiration. D. have the patient perform IS every 2 hours. Section 1: Lung Expansion Therapy KEY 1. C 2. D 3. C 4. C 5. B Section 1: Lung Expansion Therapy Question 1 analysis: If you answered C, you are right. Since the patient had an IC < 33% of predicted, IPPB was indicated. Answer A: IS would not have been effective.1 Answer B: CPT was not indicated, as the patient’s cough was dry and CPT would have been painful. Answer D: IPPB should be volume-oriented. Section 1: Lung Expansion Therapy Question 2 analysis: If you answered D, you are right. The patient was in pain and needed an analgesic. Also, the inspiratory time was too long. To make the breath more comfortable and decrease inspiratory time, the therapist should decrease the peak pressure. Increasing inspiratory flow would maintain an uncomfortable pressure. A mask was not indicated, as there was no mention of a leak. Section 1: Lung Expansion Therapy Question 3 analysis: If you answered C, you are right. Tidal volume will increase if the inspiratory pressure is increased.2,3 It is not possible to independently increase the tidal volume on a pressure-controlled ventilator. Increasing inspiratory flow or sensitivity will not increase tidal volume. Section 1: Lung Expansion Therapy Question 4 analysis: If you answered C, you are right. The patient has an adequate IC and can perform IS appropriately.4 More IPPB and coughing and deep breathing are possible, but not as effective as IS at this point. CPT is not indicated, as there is no evidence of secretions. Section 1: Lung Expansion Therapy Question 5 analysis: If you answered B, you are right. Tingling and numbness is caused by hyperventilation. Slowing the respiratory rate will relieve this.5 Hyperventilation is not a normal event during IS. Instituting an inspiratory pause is important, but not the answer. Decreasing frequency of therapy does not treat hyperventilation. Section 1: Lung Expansion Therapy References 1. Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:880. 2. Ibid:876. 3. White GC. Basic Clinical Lab Competencies for Respiratory Care: An Integrated Approach. Clifton Park, NY, Delmar;2003:335-337. 4. Reference 1:870. 5. Reference 1:868. Section 1: Lung Expansion Therapy Clinical Practice Guidelines AARC Clinical Practice Guideline: IPPB. http://www.rcjournal.com/contents/05.03/ 05.03.0540.asp AARC Clinical Practice Guideline: Incentive Spirometry http://www.rcjournal.com/online_resourc es/cpgs/ispircpg.html Section 2: IIIF3 Bland and Medicated Aerosol Therapy Bland aerosol therapy defined – An aerosol of sterile distilled water or hypotonic, isotonic or hypertonic saline – May be delivered to the upper airways (MMAD >5 _m), cool or warmed – Hypo-and hypertonic saline for sputum induction, MMAD1-5 _m – Bypassed upper airway, MMAD 2-10 _m, cool or warmed AARC CPG: Bland Aerosol Administration 2203 revision and update. RCJ May 2003;48(5):529-33. Bland Aerosol Therapy Equipment – Large volume aerosol generator (nebulizer) Pneumatically powered Control particle size by jet orifice size and baffling FiO2 is controlled by a variable air entrainment port Therapy is to be discontinued if the patient begins to wheeze due to particle reaction Bland Aerosol Therapy Equipment – Ultrasonic nebulizer Electrically powered Particle size 1/% signal frequency; MMAD 2.5 or 4-6 _m Mist density % signal amplitude; up to 7 mL/min. Blower delivers mist to the patient More frequently used for sputum induction with hypertonic saline Present an infection hazard unless frequently decontaminated (q 6 days) Discontinue therapy if patient begins to wheeze Bland Aerosol Therapy Airway Appliances – Aerosol mask and face tent for patients with intact upper airway – T-piece or Briggs adapter with reservoir for orally intubated patients – Tracheostomy mask for patients with a tracheostomy tube No traction, allows condensate to escape away from the airway Bland Aerosol Therapy Aerosol output – Large volume nebulizer Unheated, output is 26-35 mg H2O/L Heated, output is 33-55 mg H2O/L 2-3L/day depending on temperature and source gas flow – Ultrasonic nebulizer Mist density % signal amplitude; up to 7 mL/min. – Adjusted based on mucus viscosity, ease of suctioning, and patient subjective response Bland Aerosol Therapy Aerosol temperature – Unheated aerosol is cooler than ambient temperature Appropriate for patients breathing through native airway If patient complains that aerosol is too cold, a heater may be applied – Heated aerosol is ~ 88-95°F with a heater that warms liquid just prior to aerosolization Useful when upper airway is bypassed and for sputum induction Bland Aerosol Therapy History and physical A 55-year-old previously healthy male was referred to a thoracic surgeon due to a lung mass. Following surgery the patient developed pneumonia, which required an additional 10 days of antibiotic therapy and mechanical ventilation. On day 10, ventilator parameters were: Mode: VC-SIM/PSV FiO2: 0.4 Mandatory rate: 6/min PEEP: 5 cm H2O Set tidal volume: 700 mL PSV: 8 cmH2O Bland Aerosol Therapy Question 1 Since the patient could not be extubated, a jet nebulizer was used to deliver aerosol to the patient using a T-piece and 100 cc reservoir. Tenacious secretions made suctioning at -120 mm Hg difficult. The therapist should: A. replace the jet nebulizer with an ultrasonic nebulizer. B. attach a heater to the jet nebulizer. C. lengthen the reservoir tubing. D. make the suction pressure more negative. Bland Aerosol Therapy Question 2 This patient required a tracheotomy and was weaned from the ventilator. A T-piece and reservoir were used to deliver aerosol from a jet nebulizer. The nurses have had to adjust the aerosol tubing and change the dressing at the tracheotomy site frequently. The therapist should: A. clean the tracheotomy site with peroxide. B. contact the surgeon. C. replace the T-piece with a tracheostomy collar. D. attach a heater to the nebulizer. Medicated Aerosol Therapy Delivery of medications to the lower airways in the form of: – A liquid aerosol using a small volume gas powered nebulizer (SVN), vibrating mesh nebulizer, or other electrically-powered SVN – A liquid aerosol using a metered dose inhaler (MDI) with or without a valved holding device – A dry powder, using a dry powder inhaler (DPI) Medicated Aerosol Therapy Drug categories – Beta adrenergic agents (albuterol, pirbuterol, bitolterol, salmeterol) – Anticholinergic agents (ipratropium, tiotropium) – Corticosteroids (fluticasone, beclomethasone, budesonide, etc.) – Mucokinetics (acetylcysteine, DNAse) Small Volume Nebulizers Factors favoring SVN 50 psi @ 6-10 L/min source gas flow available Any breathing pattern or level of cooperation Any combination of liquid medication Variable dilution Mouthpiece or mask delivery with mouth breathing Factors limiting SVN MDI or DPI available for same drugs Ambulatory patient Drug only available as MDI or DPI (i.e salmeterol/fluticasone) Treatment time for SVN Increased cost of equipment for SVN Variation in SVN output/dependence on pressure and flow for optimal particle size Infection Metered Dose Inhalers Factors favoring MDI Short treatment time As effective as SVN Now the device of choice, assuming drug availability and patient cooperation Factors limiting MDI Technique-dependent Patient teaching time Often requires a valved holding chamber or spacer Several different drug MDIs may be required CFC propellants Need to prime/drug loss Valved Holding Chambers The MDI is actuated into the VHC to – slow the particles and allow propellant evaporation to improve airways deposition – decrease reliance on hand-breath coordination – decrease pharyngeal deposition The plastic VHC should be washed in soap and water at least monthly to clean and decrease electric charge A reservoir must be used when administering an MDI to a mechanically ventilated patient Dry Powder Inhalers Factors favoring DPI Short treatment time As effective as SVN Now the device of choice, assuming drug availability and patient cooperation No CFC Factors limiting DPI Humidity causes drug clumping Technique dependent – Patient must maintain a designated inspiratory flow Patient teaching time Drug Dilution The amount of diluent added to a liquid drug to be aerosolized does NOT decrease the dose delivered to the patient – It only increases the time for nebulization – The dose of active drug remains the same Decreasing the amount of drug WILL decrease the dose delivered to the patient – Such as using _ of a unit dose or using 0.25 mL of a 0.5% solution instead of a full unit dose or 0.5 mL Drug Dilution Pneumatic SVNs require at least 1 mL of solution to nebulize (dead volume) – Optimal total SVN volume is > 4mL Vibrating mesh nebulizers nebulize drops of solution (no dead volume) – Failure to dilute results in full mg dose delivered in a few seconds – May cause side-effects – Dilute conventionally Medicated Aerosol Therapy Question 3 An employed, ambulatory patient with COPD is to take treatments with albuterol and ipratropium QID following hospital discharge. What drug delivery method should the therapist teach to the patient? A. metered dose inhaler with valved holding chamber B. small volume nebulizer with compressor C. dry powder inhalation D. metered dose inhaler with closed-mouth technique Medicated Aerosol Therapy Question 4 A patient with mild persistent asthma returns to the clinic after a two-week trial of fluticasone (Flovent) 110, 1 puff BID. His symptom diary shows no improvement. What should the respiratory therapist do FIRST: A. Increase the fluticasone dose to 2 puffs BID. B. Switch the patient to budesonide (Pulmicort) by SVN. C. Have the patient demonstrate proper spacer cleansing. D. Check and reinforce proper MDI technique. Medicated Aerosol Therapy Question 5 A patient with steroiddependent COPD is receiving mechanical ventilation. She receives albuterol/ipratropium unit dose by SVN Q4 hours and 1 puff of Flovent (fluticasone) 220 BID using an MDI using the adapter shown here: Medicated Aerosol Therapy Question 5 continued Her flow-volume loop is shown here: What should the respiratory therapist do first? Flow L/min Vol. (L.) Medicated Aerosol Therapy Question 5 continued A. Replace the adapter with a chamber spacer for the fluticasone treatments. B. Contact the physician for an order to double the fluticasone. C. Contact the physician for an order to double the dosage of albuterol/ipratropium. D. Change the inspiratory flow pattern to decelerating ramp. Section 2: Bland and Medicated Aerosol Therapy Key 1. B 2. C 3. A 4. D 5. A Section 2: Bland and Medicated Aerosol Therapy Question 1 analysis If you answered B you are right. A heater will increase the temperature of the delivered gas and increase it’s water vapor content. This is supposed to increase water to the airway and make the inhalation of the aerosol more comfortable. A USN will also add water, perhaps too much, and it is difficult to adjust the FiO2. Lengthening the reservoir tubing helps stabilize FiO2. Making suction pressure more negative increases the chance of trauma to the airway. Section 2: Bland and Medicated Aerosol Therapy Question 2 analysis C is correct. A T-piece will pull on a tracheostomy tube, possible causing bleeding and inflammation. Always use a tracheostomy collar in this case. Cleaning the tracheostomy site only will temporarily make the site look better. The surgeon will tell the therapist to wait for his next visit, prolonging corrective action. A heater is indicated, but the tracheostomy collar is most important at this time. Section 2: Bland and Medicated Aerosol Therapy Question 3 analysis A is the best answer. MDIs with a spacer are the delivery device of choice for ambulatory patients, and these drugs are available as MDIs. A SVN and compressor tethers the patient to his home and is unnecessarily expensive. These drugs are not available as DPIs The closed mouth technique is suboptimal, as much of the medication is deposited in the oropharynx. Section 2: Bland and Medicated Aerosol Therapy Question 4 analysis D is the best answer. Because MDI therapy is dependent upon correct technique, this is the first and cheapest thing to check when the patient complains of therapy ineffectiveness. If technique is appropriate, the dosage may need to be increased. Changing therapy to another drug and increasing the cost, especially when the problem is inhaler technique, is unproductive. After only two weeks, it is unlikely that the spacer will have needed cleaning. Section 2: Bland and Medicated Aerosol Therapy Question 5 analysis A is correct. Narrow barrel and elbow adapters allow delivery of almost no drug and should always be replaced by a spacer chamber. The flow-volume loop shows air-trapping, characteristic of bronchospasm. Doubling the fluticasone with this administration device wastes the medication faster The dose of albuterol/ipratropium is already appropriate Increasing inspiratory time is appropriate, but will not solve the problem of poor drug delivery. Section 2: Bland and Medicated Aerosol Therapy References AARC Clinical Practice Guideline: Bland aerosol administration-2003 revision and update. RCJ 2003;48(5):529-533 AARC Clinical Practice Guideline: Selection of aerosol delivery device. RCJ 1992;37:891-897. Rau JL. Respiratory Care Pharmacology 6th ed. St. Louis, Mosby;2002:77-78. Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:751-755,766-782. Section 2: Bland and Medicated Aerosol Therapy Other resources AARC Professor’s Rounds: Getting the Most from the Mist: Current and Future Aerosol Delivery. http://www.aarc.org/education/professors_round s_05/ AARC Webcasts: Pneumatic aerosol devices: Past, present and future. Liquid aerosol drug delivery: Nebulization for the 21st century. AARC.org/education/webcast Section 3: IIIF4 Oxygen Therapy Changing the “mode” of oxygen administration – Changing from high to low flow therapy – Changing from low to high flow therapy – Changing devices within high/low flow categories – Changing from ambient oxygen therapy to continuous positive airway pressure Oxygen Therapy Changing from high to low flow therapy – Initial patient condition consists of an unstable ventilatory pattern or high minute ventilation, unstable vital signs, and/or unknown cause of mild-moderate hypoxemia – An air entrainment mask is often chosen to deliver an FiO2 to keep SpO2 > 92% FiO2 may be > 30% – After initial therapy, stable ventilatory pattern, vital signs, and FiO2 < 35%: therapy could be changed to a low flow device (nasal cannula) at 3-5 L/minute, concurrent with pulse oximetry to assure oxygenation Oxygen Therapy Changing from low to high flow therapy – Initial patient condition consists of a stable ventilatory pattern or normal minute ventilation, stable vital signs, and/or known cause of mild hypoxemia – A low-flow device (nasal cannula) is in use at 2-5 L/minute. – A sudden or gradual deterioration of vital signs and SpO2, ventilatory pattern instability: therapy should be changed to an air entrainment mask at an FiO2 > 0.4 concurrent with pulse oximetry to assure oxygenation Oxygen Therapy Changing high flow devices, beginning with the air entrainment mask – In the event of tracheostomy or intubation, without mechanical ventilation, use a heated air entrainment nebulizer with a tracheostomy collar or T-piece. – at an appropriate FiO2, as the FiO2 requirement increases, consider an open blending system to provide a greater total flow (> 60 L/minute) – In the event of inspissated secretions, an air entrainment nebulizer at the same FiO2 as the entrainment mask may be used. Oxygen Therapy Changing low flow devices, beginning with the nasal cannula – In sudden onset of respiratory distress, unstable vital signs, and SpO2 < 90%: change to a nonrebreather mask at >10 L/minute concurrent with pulse oximetry to assure oxygenation. This is usually short-term while determining necessity for intubation. – In mouth-breathing patients with mild-moderate hypoxemia and congested nasal airway: change to a simple mask at 5-8 L/minute, concurrent with pulse oximetry to assure oxygenation; usually short-term as it is uncomfortable. Oxygen Therapy Changing from ambient oxygen to CPAP – Hypoxemia refractory to ambient oxygen therapy with a nonrebreather mask – Impending or established hypoxemic respiratory failure – Heart failure, early ARDS, atelectasis unresponsive to ambient oxygen therapy – PaO2 < 50-60 mm Hg on > 50% oxygen – P/F ratio < 300 – Dyspnea Oxygen Therapy Adjusting flow and FiO2 – Flow is adjusted on low flow devices until the: desired SpO2 is achieved, or FiO2 delivery limits are reached, or mode or delivery device should be changed protocol is satisfied – Flow and FiO2 are adjusted on high flow devices until the: desired SpO2 is achieved, or FiO2 delivery limits are reached, or mode or delivery device should be changed protocol is satisfied Oxygen Therapy Air/Oxygen blenders – Provide 50 psi gas at an FiO2 of 0.21-1.0 at flows up to 180 L/minute – Used when high flow oxygen therapy is desired at flows in excess of the air entrainment mask or nebulizer 80% oxygen from an air entrainment mask has an air:oxygen entrainment ratio of 0.3:1. If the patient has a minute ventilation of 12 L/minute, the flow needed is 36 L/minute (flow needed = 3 x VE). Source gas flow would have to be 28 L/minute, beyond the operable range of most air entrainment nebulizers and masks. Oxygen Therapy Air/Oxygen blenders – Provide mixed gas for ambient or CPAP systems – In both open and closed systems (pictured here) an antiasphyxia valve must be in place, in the event of gas failure Oxygen Therapy Air/Oxygen blenders – FiO2 must be checked at least each shift – Unstable or incorrect FiO2 must be followed by exchanging the blender – Blender alarms indicate a loss of one source gas Assure connection to both oxygen and air Assure air and oxygen sources have pressures within specifications Test low air and oxygen source gas alarms by disconnecting each source Oxygen Therapy Liquid oxygen systems – 1 ft3 of liquid oxygen = 860 ft3 of gaseous oxygen – Storage unit is much like a thermos, with a liquid oxygen storage bottle suspended in a vacuum – Portable and in-home storage dewars Portable dewar Large storage dewar Oxygen Therapy Liquid oxygen systems – Oxygen supply company fills the large storage dewar as needed 45-100 lbs of liquid oxygen Up to 34,000 L gaseous oxygen – Patient may use oxygen from the large dewar, or from a portable dewar, refillable from the large dewar. 5-14 lbs. 5-8 hours of oxygen at 2 L/minute – Service pressure is 20-25 psi – Gas flow is metered by an adjustable flow restrictor, _ - 15 L/minute Oxygen Therapy Liquid oxygen systems Computing duration of flow – Size of dewar in lbs x fraction of full = lbs. available – lbs. available x 344 L gas/lb. = liters gas available – liters available/flow (L/min) = minutes available at that flow Oxygen Therapy Liquid oxygen systems Advantages Disadvantages Large volumes in a small space Low pressure system Refillable portable system allows ambulation Frequent deliveries necessary Oxygen is constantly venting when not in use (waste) Contact with liquid causes burns Potential difficulty when filling portable unit High cost Less likely to be covered by insurance Oxygen Therapy Oxygen concentrators – Electrically powered – Removes oxygen from the air by passing air through molecular sieves – O2 concentration 1-2 L/min: 92-95% 3-5 L/min: 85-93% – If FiO2 falls below 85%, sieve canisters are replaced by home care provider http://www.ucanhealth.com/graph/m400-410.jpg Oxygen Therapy Oxygen concentrators Advantages Disadvantages No waste or loss Low pressure system (15 psi) Cost-effective when in continuous use No oxygen deliveries Covered by insurance Require electrical supply, so backup oxygen cylinder is required FiO2 1/% flow Increased power costs Oxygen Therapy Question 1 The respiratory therapist is checking oxygen on an elderly patient with heart failure who is using a nasal cannula at 3L/min. The therapist notes that the patient’s pulse is weak, SpO2 is 83%, and the patient is poorly responsive. The therapist should: A. B C. D. Increase the oxygen flow to 4 L/min. Apply a nonrebreather mask at 12 L/min. Apply a 40% air entrainment mask Apply a simple mask at 8 L/min. Oxygen Therapy Question 2 A patient with lung cancer arrives on the medical unit from the ICU wearing a 50% air entrainment mask at 12 L/min. The patient’s color is good and his SpO2 is 100%. The therapist should: A. B. C. D. continue present oxygen therapy. apply a nonrebreather mask at 12 L/min. decrease the FiO2 to 35% apply a nasal cannula at 2 L/min. Oxygen Therapy Question 3 A 35-year-old male who crashed a motorcycle into a freeway overpass is seen by the respiratory therapist 36 hours after the crash. The patient is dyspneic and has an SaO2 of 85% on a 50% air entrainment mask. What is the optimal therapy at this time: A. mask CPAP. B. an increase in the FiO2 to 0.7. C. mechanical ventilation. D. a nonrebreather mask Oxygen Therapy Question 4 A patient’s liquid oxygen system holds 30 lbs. when full. It now reads _ full. How much longer will the supply last running at 4 L/min? A. B. C. D. 1.8 days 7.2 days 43 hours 645 minutes Oxygen Therapy Question 5 A patient with COPD is using an oxygen concentrator at 2 L/min. The respiratory therapist measures the FiO2 and finds that it is 0.85. The therapist should: A. B. C. D. increase the liter flow. have the sieves changed. note the FiO2 and continue with his checks. clean the air filter on the concentrator. Section 3: Oxygen Therapy KEY 1. B 2. C 3. A 4. D 5. B Oxygen Therapy Question 1 analysis Answer B is correct. The patient is severely hypoxemic, has a weak pulse, and decreased sensorium. While awaiting definitive medical therapy, the patient’s oxygenation status must be improved by greatly increasing FiO2. The other options are incorrect because they do not offer as high an FiO2 as the nonrebreather mask. Oxygen Therapy Question 2 analysis The correct response is C. Since the patient’s color and SpO2 are good, the FiO2 can be decreased using SpO2 as a guide. Responses A and B would increase the FiO2 which is not indicated. Response D represents a decrease in FiO2 that may be too great for the patient to tolerate at this time. Oxygen Therapy Question 3 analysis The correct response is A. The first 24-36 hours after trauma represents the latent period for ARDS. Once the patient becomes tachypneic and refractory hypoxemia is established, the only way to improve oxygenation is to implement CPAP, either by mask or artificial airway. Options B and D increase FiO2, but do nothing to increase alveolar surface area. Mechanical ventilation is a possibility, but may be more than the patient needs at this time. Oxygen Therapy Question 4 analysis – Size of dewar in lbs (30) x fraction of full (.25) = lbs. available (7.5 lbs.) – lbs. available (7.5) x 344 L gas/lb. = liters gas available (2580 L.) – liters available (2580 L.)/flow (L/min) (4L/min.) = minutes available at that flow (645 min.) The correct response is D. Oxygen Therapy Question 5 analysis The correct response is B. When the sieves become “full” of nitrogen, they are unable to filter out more nitrogen, so the zeolite in the sieve canisters must be replaced. The other responses do nothing to correct this problem. Failure to replace the zeolite will result in a further decrease in the FiO2 delivered by the concentrator. Section 3: Oxygen Therapy References Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:833-852,1254-1260. AARC Clinical Practice Guideline: Oxygen therapy for adults in the acute care facility-2002 revision and update. RCJ 2002;47(6):717-720. Selecting the Most Appropriate O2 Device for Your Patient. AARC Webcast. http://www.aarc.org/education/webcast/index.asp Section 4: IIIF5 Specialty Gas Therapy Helium/Oxygen (Heliox) therapy – Indications Large airway obstruction Dyspnea and tachypnea in COPD Acute upper airway obstruction Asthma with acute respiratory failure Anesthesia through small endotracheal tubes Postextubation stridor – Effects Decreases the work of breathing by carrying oxygen in a gas less dense than nitrogen Specialty Gas: Heliox Guidelines for Use – Always mix Helium with > 20% oxygen – Most common mixes are 80/20 and 70/30 Helium/Oxygen – Use for as long as necessary in postextubation stridor Treat concurrently with steroids and racemic epinephrine Specialty Gas: Heliox Modes of administration – Use a nonrebreathing system, simple mask, or nonrebreather mask – Always check the FiO2 of the cylinder before use, to assure the correct FiO2 – May be administered with a ventilator but it confounds the volume delivery systems of most ventilators, so should be used only with caution and experience – May be bled into the mask of an NPPV system Recent study does not demonstrate decreased intubation rate or ICU stay Specialty Gas: Heliox May be administered using a commercially available system (GE Aptaér Heliox Delivery System) Nonrebreathing system For spontaneouslybreathing patients http://www.gehealthcare.com/usen/respiratory_care/images/ac_80.jpg Specialty Gas: Heliox Modes of administration – During aerosol therapy Improves aerosol delivery: improves FEV1, PEF, decreases intubation rate Don’t let air into the system Run the nebulizer at 11 L HeO2/min. Aerogen nebulizer may also be used Specialty Gas: Heliox Adjusting Heliox flow – Correction factors for heliox use through an oxygen flowmeter 1.8 for 80/20 heliox 1.6 for 70/30 heliox For example, if 80/20 heliox is being delivered with an oxygen flowmeter set to 10 L/min., there are actually 18 L/min. of heliox. Adjusting Heliox concentration – Use 70/30 heliox in the treatment of airway obstruction with accompanying hypoxemia Specialty Gas: Heliox References Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:858-859. AARC Webcast: Heliox Therapy. http://www.aarc.org/education/webcast/ind ex.asp Specialty Gas: Nitric Oxide Indications – Disorders where blood flow to ventilated alveoli is decreased Effect is limited to the pulmonary arteries Approved only for use in neonates – Treatment of term and near-term neonates with hypoxic respiratory failure with pulmonary hypertension Specialty Gas: Nitric Oxide Mode of administration GE INOvent – – – – Adjustable [NO] Limits production of NO2 Monitors [NO] and [NO2] Adds NO to the inspiratory limb of the ventilator – Most effective when combined with HFOV – Scavenging unnecessary http://www.gehealthcare.com/usen/anesthesia/products/anelifesupport_inovent.html Specialty Gas: Nitric Oxide Adjustment of concentration and flow – Recommended initial dose is 20 ppm – < 14 days or until underlying oxygen desaturation has improved – Dose can often be reduced to 5 ppm after the initial 4 hours – Higher doses did not improve effect and increased the hazard of NO2 – starting at a high dose and working down is more effective than starting at a low dose and working up Specialty Gas: Nitric Oxide Withdrawal of therapy – Reduce concentration to lowest effective dose (< 5ppm) – Patient should be hemodynamically stable – Oxygenation should be stable with < 40% oxygen – Hyperoxygenate with 60-70% oxygen before removing NO – Prepare to provide hemodynamic support if needed Specialty Gas: Nitric Oxide References Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:855-858. AARC Webcast: Nitric oxide therapy. http://www.aarc.org/authenticate.asp?/edu cation/webcast/archives/nitric_oxide/index. asp Specialty Gas Question 1 What flow of Heliox should be used to power a small volume nebulizer for bronchodilator administration? A. 6 L/min. B. 8 L/min C. 11 L/min. D. 15 L/min Specialty Gas Question 2 What is the correct flow setting for an oxygen flowmeter to deliver a 70/30 heliox at 18 L/minute? A. 18 L/min. B. 11 L/min. C. 32 L/min. D. 29 L/min. Specialty Gas Question 3 A patient with asthma is inhaling 80/20 heliox with a simple mask. The SpO2 is 90%. The therapist should: A. increase the heliox to 70/30. B. deliver the heliox with a nonrebreather mask. C. decrease the heliox to 70/30 and use a nonrebreather mask D. decrease the heliox to 70/30 and use an air entrainment nebulizer set at 80% oxygen. Specialty Gas Question 4 What initial dose of nitric oxide should the therapist administer to an infant with pulmonary hypertension? A. 100 ppm B. 80 ppm C. 40 ppm D. 20 ppm Specialty Gas Question 5 An infant who is receiving 5 ppm nitric oxide has a stable hemodynamic status and a PaO2 of 60 mm Hg on an FiO2 of 0.38. What are the therapist’s most appropriate actions? I. Prepare to hyperoxygenate the infant. II. Turn the nitric oxide off. III. Decrease the FiO2 to 0.35 IV. Increase the nitric oxide to 8 ppm A. I, II only B. III, IV only C. I, IV only D. II, III only Specialty Gas Key 1. C 2. B 3. C 4. D 5. A Specialty Gas Question 1 analysis C is the correct response, according to Hess in the AARC Webcast on heliox. Lower or higher values decreased aerosol deposition. Specialty Gas Question 2 analysis The correct answer is B, 11 L/minute. If one wants an 18 L/min. flow of 70/30 heliox, the desired oxygen flowmeter setting = the quotient of the desired heliox flow/1.6: Flow = 18/1.6 = 11.25 L/min. Specialty Gas Question 3 analysis The correct response is C. The patient is hypoxemic and is receiving heliox using a less than optimal delivery device. The therapist should increase the FiO2 by obtaining a cylinder of 70/30 heliox and assure a higher concentration of source gas by using a nonrebreather mask. Specialty Gas Question 4 analysis The correct response is D. The other concentrations of NO are higher than the recommended dose and have not been shown to improve oxygenation index, survival, or less need for ECMO. Higher doses are also associated with an increase in nitrogen dioxide, a toxic byproduct of NO administration. Specialty Gas Question 5 analysis The correct response is A. This infant has an acceptable oxygenation status and is on the lower end of the NO dose range, so is ready to be weaned from NO. The therapist is to prepare for temporary hyperoxygenation and to discontinue the NO. Decreasing the FiO2 may cause hypoxemia. Increasing the [NO] is not indicated. Section 5: IIIF6, 7, 8 Bronchial Hygiene Therapy, Management of Artificial Airways, and Suctioning Patient positioning and duration of bronchial hygiene therapies Coordination of sequencing of bronchial hygiene therapies Management of artificial airways to: – – – – Change type of humidification equipment Initiate suctioning Control cuff inflation Perform tracheostomy care Section 5: IIIF6, 7, 8 Bronchial Hygiene Therapy, Management of Artificial Airways, and Suctioning Suctioning, related to – Altering the frequency and duration – Changing the type and size of catheters – Changing pressure – Use of irrigating solutions Bronchial Hygiene Therapy Refers to postural drainage therapy (CPT), cough techniques, PEP techniques, and HFCWO Altering patient position in unilateral lung disease – Poor oxygenation associated with a particular position, i.e. while lying on right side; would indicate atelectasis/consolidation on the right side. Lying on the left side may improve oxygenation. Altering patient position in ARDS – Prone positioning 1° for the purpose of improving oxygenation, 2° for postural drainage Bronchial Hygiene Therapy Altering patient position for secretion clearance or atelectasis – Indicated for any of the following in a lobe or segment not currently receiving CPT Radiographic indication of consolidation or atelectasis Coarse crackles Bronchoscopic evidence of secretions Rhonchial fremitus Bronchial Hygiene Therapy Duration of bronchial hygiene therapies – 3-15 minutes in each position, as tolerated – Total treatment time of 30-40 minutes – Reevaluate every 48-72 hours – Mechanical insufflation-exsufflation consists of five cycles followed by secretion removal Bronchial Hygiene Therapy Coordination of sequencing – Hygiene therapy follows medicated aerosol or may be concurrent with bland aerosol therapy – “secretion mobilization” phase is first CPT, Huffing, slow exhalation through PEP device Slow, deep breathing at tidal volume > normal through PEP device – “secretion elimination” phase follows Coughing Rapid exhalation through vibratory PEP device (FlutterTM or AcapellaTM) Bronchial Hygiene Therapy Reference Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:888-904. Artificial Airway Management Humidification equipment – Heated humidifier May be used during mechanical ventilation or while spontaneous breathing Delivers water vapor Require a high-flow of mixed gas (blender and flowmeter) if not used with a ventilator Constant airway temperature is maintained Can deliver 100% RH at body temperature Long-term mechanical ventilation (>96 hours) When the HME is contraindicated Artificial Airway Management Humidification equipment – Heated bland aerosol Air entrainment nebulizer Patients not receiving mechanical ventilation Aerosol temperature is controlled by a heater 33-55 mg H2O/L water output Delivers aerosol through a T-piece or tracheostomy collar Easy, from an equipment setup point-of-view Adjustable, stable FiO2, unless a high flow and high FiO2 are necessary Artificial Airway Management Humidification equipment – Heat and Moisture exchanger (HME) The two most efficient types are the hygroscopic condenser and hydrophobic condenser Contraindications: – – – – Thick, copious or bloody secretions Expired VT < 70% inspired VT (bronchopleural fistula) Body temperature < 32°C Spontaneous VE > 10L/min. Remove HME from circuit when administering aerosolized medications May be used for all mechanical ventilation unless contraindicated Artificial Airway Management Humidification equipment reference Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:741-753. Artificial Airway Management: Indications for Suctioning Coarse crackles Radiographic evidence of secretions Changes in monitored pressure/flow graphics Increased PIP (VCV) Decreased VT (PCV) Atelectasis or consolidation, consistent with secretions Visible secretions in the airway Observed increase in WOB Deteriorating ABGs Need to obtain a sputum specimen Need to maintain artificial airway patency Need to stimulate cough Artificial Airway Management: Cuff Care An increase in cuff pressure or volume may be indicated when: There is an audible leak There are bubbles at the mouth Exhaled VT < Inhaled VT Aspiration is suspected There is loss of PEEP A decrease in cuff pressure or volume may be indicated when: Cuff pressure is >25-30 cm H2O ***Always use the lowest inflation pressure needed to obtain a satisfactory seal*** Artificial Airway Management: Tracheostomy Care Cleaning the tracheostomy site: Daily When gauze or ties are soiled When there are visible secretions or blood around the site Replacing a tracheostomy tube: When plugged with blood clot or mucus When cuff is ruptured When a different size tube is indicated Artificial Airway Management: Tracheostomy Care Repositioning a tracheostomy tube is indicated if the distal end migrates into the pretracheal space – – – – Tube may be too short Neck may be too thick Postoperative swelling Insecure ties Pretracheal space Requires emergent reinsertion or placement of an ETT in the stoma http://um-jmh.org/images/healthlibrary/TRACH-1.gif Airway Management: Suctioning Altering frequency or duration of suctioning – Suction when any of the previously listed indications exist – Total suction time should be < 10-15 sec. Discontinue if bradycardia, arrhythmia, desaturation or hypotension is induced by suctioning Oxygenate the patient using 100% oxygen by resuscitator or ventilator Airway Management: Suctioning Changing size of catheter – Catheter size is determined by airway diameter; two methods Catheter size = ETT (mm) x 2, use the next size smaller catheter in Fr. Catheter size (Fr.) = ETT (mm) x 3 2 – Larger catheter will be more difficult to pass and may occlude the airway – Smaller catheter will not be as efficient in removing secretions – Once the optimal size is determined, it should not be changed Airway Management: Suctioning Changing type of catheter Four types available – Straight and Coudé catheters Used when a closed-system catheter is not available or seems ineffective Coudé may be useful to access the left mainstem, since it has an angled tip – Straight and Coudé closed-system catheters Generally used for all mechanically-ventilated patients Airway Management: Suctioning Indications for closed suction systems – High ventilator requirements PEEP > 10 cm H2O MAP > 20 cm H2O TI > 1.5 sec. FiO2 > 0.6 – Suctioning > 6times/day – Hemodynamic instability associated with ventilator disconnection – Ventilated patients with active TB – Nitric oxide or heliox in use Airway Management: Suctioning Negative pressures for suctioning – Adult: 100-120 mm Hg – Child: 80-100 mm Hg – Infant: 60-80 mm Hg If secretions are too thick to suction at the top of any negative pressure range – Evaluate effectiveness of humidifier – Consider instilling solution (see below) Do not exceed recommended ranges Airway Management: Suctioning Use of irrigating solutions – Routine use is not recommended – Efficacy of saline remains unclear; may make the airway and mucus “slipperier” – Instillates may increase nosocomial infection by washing bacteria from the airway wall into the trachea; have been demonstrated to cause desaturation – Instillates have included 3-5 mL normal saline, 2% NaHCO3, and 10% acetylcysteine; the latter two being mucolytics NO proven value! Artificial Airway Management References Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:655-659,681-685, 686-688. Bronchial Hygiene Question 1 Bronchoscopy has revealed mucus plugging of the right lower lobe bronchus in a patient with pneumonia who is receiving mechanical ventilation. Chest physical therapy is ongoing while the patient is lying on his right side in Trendelenberg. What is the therapist’s most appropriate action? A. Place the patient on his left side in Trendelenberg and continue chest physical therapy. B. Increase the frequency of suctioning. C. Instill 3-5 mL of 10% acetylcysteine and suction. D. Select a Coudé suction catheter and continue suctioning. Bronchial Hygiene Question 2 A patient with cystic fibrosis is receiving vibratory PEP therapy. After three secretion mobilization breaths, several secretion elimination breaths fail to produce any secretions. The therapist should: A. suggest postural drainage and percussion. B. have the patient take 8-10 secretion mobilization breaths. C. suction the patient. D. administer an aerosol with 5 mL of 10% acetylcysteine. Bronchial Hygiene Question 3 A patient is receiving mechanical ventilation through a hygroscopic condenser HME. Secretions are tenacious. There is continuous bubbling in the water seal chamber of the pleural drainage system. The therapist should: A. install a new hygroscopic condenser HME. B. install a hydrophobic condenser HME. C. instill 3 mL of 10% acetylcysteine and suction. D. replace the HME with a heated humidifier. Bronchial Hygiene Question 4 A patient is receiving mechanical ventilation in the PCV mode with 15 cm H2O above PEEP. Tidal volumes measured over the past 90 minutes are as follows: 1:00pm 450 mL 1:30pm 425 mL 2:00pm 415 mL 2:30pm 405 mL The therapist palpates an increase in rhonchial fremitus. The therapist should: A. increase the PCV level to achieve a tidal volume of 450 mL. B. switch to volume controlled ventilation with a VT of 450 mL. C. suction the patient. D. check the ventilator circuit for leaks. Bronchial Hygiene Question 5 A patient’s endotracheal tube cuff pressure is 30 cm H2O. The therapist determines that the seal is satisfactory with a pressure of 15 cm H2O. The therapist should: A. maintain a 30 cm H2O cuff pressure. B. maintain the cuff at minimal leak. C. increase cuff pressure to 34 cm H2O. D. set the cuff pressure at 15 cm H2O. Bronchial Hygiene Question 6 A patient is receiving mechanical ventilation through a tracheostomy tube. A leak is detected and the cuff will not seal with injection of additional air. The therapist’s most appropriate action is to: A. replace the tracheostomy tube. B. pack additional gauze into the stoma around the tube. C. clean around the tube and stoma with hydrogen peroxide. D. insert an endotracheal tube in the stoma. Bronchial Hygiene Question 7 An adult with an 8mm ID endotracheal tube is being suctioned through a 10 fr. catheter at -100 mm Hg. However, the thick secretions are not being effectively aspirated into the catheter. The therapist should: A. instill 3 mL normal saline and increase suction pressure to -140 mm Hg. B. increase suction pressure to -120 mm Hg and suction catheter size to 14 fr. C. increase suction catheter size to 16 fr. And maintain -100 mm Hg suction D. instill 3 mL normal saline and continue suctioning. Bronchial Hygiene Question 8 An adult with an 8 mm ID tracheostomy tube is being suctioned with a 14 fr. Catheter at -120 mm Hg. Secretions are thick and are not being aspirated effectively. Which of the following should the therapist consider? I. Increasing the airway temperature II. Installing an HME III. Instilling normal saline before suctioning IV. Increasing the size of the suction catheter A. I, II only B. II, III only C. I, III only D. II, IV only Bronchial Hygiene Key 1. A 2. B 3. D 4. C 5. D 6. A 7. B 8. C Bronchial Hygiene Question 1 analysis Answer A is correct because it alters the patient’s position to addresses the issue of mucus plugging in the right lower lobe. More frequent suctioning may help. The undirected instillation of acetylcysteine down the trachea has little or no effect. A Coudé suction catheter may be useful when one wants to suction the left lung. Bronchial Hygiene Question 2 analysis Answer B is correct. When using the Flutter or AcapellaTM, 8-10 secretion mobilization breaths precede secretion elimination breaths. If the patient uses these devices as directed, CPT and suctioning should be unnecessary. There is no documentation that aerosolized acetylcysteine is useful for any pulmonary condition. Bronchial Hygiene Question 3 analysis Since secretions are tenacious and there is bubbling in the water seal chamber (indicating that exhaled VT is < inhaled VT), any HME is contraindicated. Therefore, D, a heated humidifier, should be used in place of the HME. Instilled acetylcysteine would be hazardous and make no difference. Bronchial Hygiene Question 4 analysis Since the tidal volume is decreasing, there must be an increase in resistance. This is confirmed by the increased fremitus which indicates secretions. The answer is C, suction the patient. Increasing the pressure or changing to VCV could expose the patient to excessive pressure and would not correct the problem. If there was a leak, the ventilator would likely be time cycling and there would be an alarm. Bronchial Hygiene Question 5 analysis Always use the lowest inflation pressure needed to obtain a satisfactory seal. Therefore, D is the correct answer. Cuff pressure could be set to minimal leak, minimal seal, 30 or 34 cm H2O, but any of these may cause tracheal damage eventually. Bronchial Hygiene Question 6 analysis There is a leak in the cuff or in the pilot balloon line. The best fix is to replace the tube (A). There should always be a spare nearby. Cleaning and packing the tube does nothing in this case. Inserting an endotracheal tube in the stoma will restore ventilation, but is not the optimal procedure. Bronchial Hygiene Question 7 analysis Both the suction catheter size and vacuum pressure are inadequate and should be increased (B). Instillation of saline may help. An 18 fr. catheter is too big for an 8 mm airway. Bronchial Hygiene Question 8 analysis Increasing the gas temperature at the airway is correct, since the humidifier will provide more water vapor. Instilling saline may help my making secretions slipperier, which may help temporarily. An HME is contraindicated in the presence of thick secretions and the correct size catheter is already in use. Section 6: IIIF9 Mechanical Ventilation Monitoring and adjusting alarm settings – Volume – Pressure – Incompatible settings – FiO2 – Temperature – Apnea Mechanical dead space – A “dead” issue – No longer used or recognized Monitoring and Adjusting Alarm Settings Low exhaled tidal volume – Set 100 mL or 10-15%% below set VT Low exhaled minute volume – 2-5 L/min. or 10-15% below baseline VE Alerts personnel to the presence of a leak If VT or VE change or are changed appropriately, alarm tolerances should be adjusted accordingly When a volume alarm sounds, the patient should be manually ventilated until mechanical ventilation can be restored Monitoring and Adjusting Alarm Settings High exhaled minute volume – Set to 5L/minute or 10-15% above baseline minute volume – High volume alarm indicates tachypnea and/or hyperpnea and some level of patient distress – May indicate the patient is trying to meet metabolic demands by increasing ventilation (i.e. sepsis/metabolic acidosis) – May indicate patient discomfort or anxiety – If VE changes or is changed appropriately, alarm tolerances should be adjusted accordingly Monitoring and Adjusting Alarm Settings Low [peak] pressure – Set to 8 cm H2O or 5-10 cm H2O below PEEP – Indicates loss of pressure during inspiration – Usual cause is a leak at any circuit connection, at the endotracheal tube cuff, or in the humidifier – If tidal volume is adjusted in VC modes or pressure is adjusted in PC modes, the low pressure tolerance is adjusted accordingly. Monitoring and Adjusting Alarm Settings Low PEEP – Set to 3-5 cm H2O below PEEP – Some ventilators will attempt to compensate for this by increasing flow – Any condition causing a leak, leading to a low peak pressure alarm, may lead to a low PEEP alarm – As PEEP is changed, the low PEEP alarm is adjusted accordingly – In the event of a low pressure or PEEP alarm, manual ventilation is provided until the fault is corrected Monitoring and Adjusting Alarm Settings High pressure limit – Set to 50 cm H2O initially, then 10-12 cm H2O above PIP once PIP is established – Indicates an obstruction in the circuit, decreasing compliance, or increasing resistance Secretions, tube kink, coughing – In the event of repeated high pressure alarms, the patient should be manually ventilated while the cause is determined and remedied – If tidal volume or PIP are changed appropriately, then the high pressure limit is adjusted accordingly Monitoring and Adjusting Alarm Settings Incompatible settings – Part of the ventilator’s logic to prevent an inverse I:E ratio – Automatic, alerts the therapist to the incompatibility of requested settings and suggests an action – Example: the therapist sets a flow of 30 L/minute and a mandatory rate of 24 breaths/minute with a tidal volume of 800 mL. – This results in an inverse I:E, and a message suggesting an increase in flow Monitoring and Adjusting Alarm Settings FiO2 – Ventilators that incorporate an oxygen analyzer may allow the therapist to set high and low limits – Set to 5-10% above and below the desired FiO2 – If FiO2 is changed, the therapist adjusts the FiO2 limits accordingly Monitoring and Adjusting Alarm Settings Temperature – Set 2°C above and below set temperature at the airway – Some humidifiers allow this setting, for others it is automatic – Alerts the therapist if there is excess/loss of heat at the airway – Usually the result of a faulty heater, circuit wire, thermistor wire, or entire heater, usually requiring replacement of the wire at fault – In this event, it may be appropriate to place an HME until the problem is resolved Monitoring and Adjusting Alarm Settings Apnea – Alerts the therapist of apnea in spontaneous breathing modes or low-rate IMV – Set to a value < mandatory total cycle time or 20 seconds – Frequent apnea alarms may indicate loss of ventilatory drive or oversedation and require an increase in mandatory rate Mechanical Dead Space A length of ventilator circuit tubing inserted between the circuit Y and the endotracheal tube Provides for a measured amount of rebreathed volume in each breath equal to 50 mL/6” length of tubing inserted Used to normalize/increase a patient’s PaCO2 and decreased pH when a high minute volume is used No contemporary use of mechanical dead space, no reference in contemporary texts There are no written recommendations on changing mechanical dead space Mechanical Ventilation Reference Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care, 8th ed. St. Louis, Mosby; 2004:1031-1032. Mechanical Ventilation Question 1 A patient is receiving volume controlled ventilation. It is agreed that the patient’s ARDS is worsening. Ventilatory parameters are not being changed at this time. Which of the following adjustments may be required? A. B. C. D. increase the pressure limit increase the minute volume limit decrease the apnea interval decrease the tidal volume limit Mechanical Ventilation Question 2 A patient with COPD is receiving volume controlled ventilation. A bronchodilator treatment has provided significant relief from bronchospasm. An alarm sounds frequently after the treatment. The therapist will likely: A. increase the high pressure alarm limit B. decrease the minute volume limit C. increase the tidal volume alarm limit D. decrease the low pressure alarm limit Mechanical Ventilation Question 3 A patient awakens following coronary artery bypass grafting, and is receiving volume controlled ventilation. He appears restless and an alarm sounds on his ventilator. The therapist is most likely to: A. increase the high pressure alarm limit. B. increase the minute volume limit. C. decrease the tidal volume alarm limit. D. decrease the low pressure alarm limit. Mechanical Ventilation Question 4 A postoperative patient is receiving pressure support ventilation during the weaning process. After receiving medication for pain, an alarm sounds. The therapist will most likely have to: A. increase the high pressure alarm limit. B. increase the minute volume limit. C. decrease the low tidal volume alarm limit. D. decrease the low pressure alarm limit. Mechanical Ventilation Key 1. A 2. D 3. B 4. C Mechanical Ventilation Question 1 analysis Worsening or ARDS is characterized by a decrease in compliance. At a fixed tidal volume, this means that peak pressure will increase. The pressure limit will sound, indicating a limiting of both pressure and volume. For the patient to receive the same volume, the pressure limit will have to be increased, so the answer is A. Mechanical Ventilation Question 2 analysis Whenever bronchospasm is relieved, resistance decreases and so does peak pressure. If the peak pressure decreases below the previously set low pressure alarm limit, that alarm will sound. This necessitates a decrease in the low pressure alarm setting. The answer is D. Mechanical Ventilation Question 3 analysis When a patient awakens and is receiving mechanical ventilation, it is likely that he will be restless, or at least, move around some and increase his ventilation. Therefore, the minute ventilation should increase, which may result in a high minute ventilation alarm. Therefore, the therapist may have to increase the minute ventilation limit. The answer is B. Mechanical Ventilation Question 4 analysis When a patient receives a pain medication, ventilatory drive may be decreased, which, in PSV, may decrease tidal volume or minute ventilation. In this case, the tidal volume has likely decreased, which will trigger the low tidal volume alarm. The therapist will have to adjust the low tidal volume alarm and consider if it is necessary to implement a mandatory rate until the sedation has metabolized. C is correct.