Psychiatric emergencies in med-surg patients
advertisement

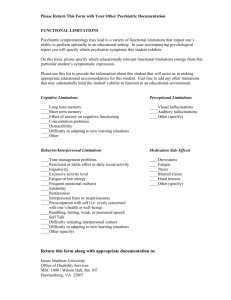
Psychiatric emergencies in med-surg patients: Are you prepared? All nurses—not just psych nurses— are likely to encounter patients experiencing psychiatric emergencies. By Marlene Nadler-Moodie, MSN, APRN, PMHCN-BC RODNEY, AGE 47, was admitted to the hospital 2 days ago with rib and femur fractures and facial contusions. He appears well nourished and well groomed. The previous shift’s report indicates he had a restless night, requested pain medications, and seemed anxious. His chart reveals a routine course with restlessness and anxiety throughout multiple shifts. Halfway through your shift, you observe that Rodney is restless, is moving about in bed, and has hand tremors. When you walk into his room, he is frantically brushing the bedsheets with his hands and arms in sweeping motions. Despite a reasonably cool room temperature, he’s sweating profusely. Toward the end of your shift, you find Rodney in a panic, trying to get out of bed. He complains of nausea and has vomited a small amount into an emesis basin. He is sobbing, and yells,“There are bugs all over the sheet!” He can’t stop shaking. You suspect he is in acute alcowww.AmericanNurseToday.com hol withdrawal and needs immediate intervention to manage his delirium tremens. Psychiatric disorders and related problems are common in med-surg patients, and scenarios like this one occur every day in acute-care hospitals. One source estimates that in 2007, 46% of the U.S. population experienced such mental-health disorders as anxiety, impulse control, and substance abuse. In 2006, psychosis was the third-highest-volume CE 1.7 contact hours L EARNING O BJECTIVES 1. Describe how to assess patients for potential psychiatric problems. 2. Identify signs and symptoms of common psychiatric emergencies on the med-surg unit. 3. Discuss appropriate interventions for common psychiatric emergencies. diagnostic-related group (DRG). This DRG (430) includes major personality disorders, such as schizophrenia, catatonia, bipolar affective disorders, and paranoia. People with psychosis or substance use disorders are at risk for the same health problems as any other population subset. What’s more, even patients without preexisting mental disorders may become anxious and apprehensive when hospitalized, which may alter their behavior. Consequently, aberrant social behaviors may increase in the hospital setting. Bottom line: You don’t have to be a psych nurse to encounter patients experiencing psychiatric emergencies. That’s why all nurses should have a basic knowledge of psychiatric nursing, regardless of the setting they work in. Identifying psychiatric emergencies On med-surg units, common psychiatric problems include psychosis, substance abuse and withMay 2010 American Nurse Today 23 Hallmarks of psychosis Psychosis is a state of being out of touch with reality. Key signs and symptoms include hallucinations and delusions. • Hallucinations manifest as reports of false sensory input, such as seeing visions, hearing voices, smelling and tasting various sensations, and tactile disturbances. In some cases they’re a hallmark of a frank psychiatric disorder. In others, they arise secondary to such conditions as infection, high fever, drug toxicity, and brain anomalies. • Delusions are false fixed beliefs with no basis in reality—for instance, the belief that “there’s a conspiracy against me.” A patient may claim that “all the doctors in this hospital want to experiment with my brain and send it to outer space for future dealings with aliens.” As with hallucinations, delusions can stem from a psychiatric disorder or result from delirium or medical-surgical complications. drawal, delirium, anxiety, aggression, bipolar disorder, personality disorders, and suicidal behavior or ideation. To ensure appropriate intervention, these problems need to be identified early and their cause must be determined. (See Hallmarks of psychosis.) Signs and symptoms of psychiatric problems cross over into many diagnostic categories. Nurses skilled in early assessment of these disorders are best prepared to intervene. During your assessment, seek corroboration from family members, look for a history of such problems in the patient’s medical record, or document the patient’s report that he or she has a known psychiatric disorder. Generally, psychiatric disorders are long-term problems with exacerbations and remissions. Knowing if your patient’s current psychotic symptoms are secondary to an ongoing psychiatric disorder can guide interventions. Medication reconciliation can yield valuable clues. Has the patient been taking psychiatric medications routinely? If so, which ones? Did she recently stop taking such drugs? If so, when? Is she taking the prescribed dosage at the prescribed frequency? Some psychiatric medications can be dangerous if they build up to a toxic blood level; for example, toxic levels of lithium exceed 1.5 mEq/L. Finding out if the patient’s 24 American Nurse Today taking too much or too little of a prescribed medication can help the healthcare team stabilize the drug regimen as soon as possible. If the patient has no known psychiatric disorder, continue to assess all aspects of the current situation to determine what might be causing the signs and symptoms. Alleviating the cause may resolve the problem. In other cases, short-term use of antipsychotic drugs can calm the patient and reduce agitation. General goals of care While each type of psychiatric emergency requires specific nursing interventions, these general care goals apply to all: • Assess the problem or potential problem early. • Maintain a safe environment. • Intervene appropriately using all available resources. • Ensure an appropriate followup plan, if needed. Know that good communication and interpersonal skills are crucial when dealing with patients experiencing psychiatric emergencies. (See Key communication tips.) Substance intoxication and withdrawal As with Rodney in the opening scenario, substance intoxication or withdrawal can pose a psychiatric emergency. Intoxication with various substances can cause aggres- Volume 5, Number 5 sive behavior. Especially during physical assessment, patients may believe you are going to harm them and may become combative or assaultive. Acute alcohol withdrawal is common in med-surg patients and must be treated. But be aware that some patients aren’t truthful about their alcohol intake. Alcohol withdrawal may not occur for 24 to 72 hours after the last drink, so withdrawal symptoms may come as a surprise to caregivers a few days after a patient’s admission. Alcohol withdrawal signs and symptoms include high blood pressure, tachycardia, fever, hand tremors, insomnia, nausea and vomiting, anxiety, generalized tonicclonic seizures, and transient visual, tactile, or auditory hallucinations. Progression to delirium tremens includes disorientation, delusions, severe agitation, profuse perspiration, and fever. The most serious phase of alcohol withdrawal, delirium tremens has a mortality of 5% to 30%. Intervention Alcohol withdrawal symptoms can be managed fairly easily with immediate and consistent care. Early, continuous treatment promotes rapid stabilization. Benzodiazepines, such as chlordiazepoxide or lorazepam, routinely are given every 4 to 6 hours; patients receiving these drugs should be monitored closely. A common, easy-to-administer tool for assessing alcohol withdrawal and guiding management is the Clinical Institute Withdrawal Assessment—Alcohol, Revised (CIWA-AR). It takes about 5 minutes to administer and yields a score indicating the severity of the patient’s withdrawal symptoms. To use it, the examiner asks specific questions or makes specific observations. The primary care goal for patients in acute alcohol withdrawal www.AmericanNurseToday.com Key communication tips Keep in mind that patients with behavioral or psychiatric problems may be unable to think clearly and may lack good judgment and decision-making skills. When speaking with them, use short sentences with short words, and avoid long or complicated messages. A rule of thumb is to use words with five or six letters in sentences containing five or six words. For example, “Stay calm and rest here” or “Please drink this water now, slowly.” Avoid arguing with a patient who has psychotic symptoms. If she is hallucinating or reports that others are conspiring against her, don’t state, “There are no bats flying around the room” or “There’s no conspiracy.” The patient’s reality tells her you’re wrong. Instead, say, “I believe you, but I don’t see the bats.” That way, you’re not suggesting the patient is lying or that you don’t believe her; you’re simply letting her know her reality isn’t your reality. This may give her reason to question whether her hallucinations are real. is to promote safe withdrawal without injuries or medical complications. Nursing care includes: • monitoring vital signs • maintaining a quiet, calm environment • offering support and reassuring the patient he or she is safe • instituting fall precautions • addressing pain caused by medical-surgical conditions (and not withholding analgesia) • promoting good hygiene • monitoring food and fluid intake • encouraging supportive family members and others to stay at the bedside • promoting use of relaxation techniques, such as soft music, controlled breathing, and visualization. Delirium Many med-surg patients experience delirium secondary to stroke, intracranial tumors, trauma, surgical complications, fever, infection, heart failure, substance toxicity or withdrawal, sedative drugs, or excessive or deficient stimuli. Among the elderly, delirium is common with or without mental illness. Whatever its cause, delirium may result in: • perceptual disturbances www.AmericanNurseToday.com • • • • • • • disorientation restlessness reduced level of consciousness disorganized thinking decreased attention span memory impairment sleep disturbances. Delirium resembles dementia to some extent. However, signs and symptoms of delirium tend to be labile (in some cases, unpredictably so) while those of dementia are less likely to fluctuate. (See Differentiating dementia and delirium.) Intervention The behavioral problems that can accompany delirium may interfere with routine nursing care, causing frustration for care providers. Also, patients with delirium may be unable to participate in their care. Nursing actions should include providing structure, as routines are helpful to patients with disorganized thinking. Maintain an orderly environment, keeping items in the same place and within the patient’s view. Because of fluctuating signs and symptoms, finding the right time for certain interventions can promote a better outcome. Be aware that you may have to repeat yourself when speaking to the patient. And sometimes you may need to back off and wait until the patient is calmer and more receptive. Also, finding distractions from the task at hand can be helpful if the patient is particularly disturbed or distraught by your interventions. Remember—if you don’t insist emphatically, the patient isn’t likely to resist. In light of the disorganized thinking caused by delirium, giving patients some space and options can help you gain their cooperation. Violent behavior Violent behavior may result from such problems as substance intoxication, disordered or paranoid thinking and beliefs, and anger. Violent patients are a threat to their own safety as well as that of staff members, other patients, and visitors. Generally, violent outbursts don’t occur suddenly without warning. For example, agitated patients experience an inner tension that may manifest as hyperactivity and behavioral disorganization. So stay alert for violent tendencies. Trust your own judgment and tell others of your concerns. Intervention If a patient becomes violent, maintaining the safety of everyone involved—the patient, yourself, other staff members and patients, and anyone else in the immediate area—takes priority. Don’t approach the patient alone. Ask colleagues to remain nearby; no one should be isolated or left in a vulnerable space with a potentially violent patient. Make sure you can’t be trapped away from an exit. Check the environment for dangerous objects. Stay out of the patient’s physical space while keeping the patient within view at all times. Many hospitals have an emergency procedure for managing violent persons. Nursing staff must receive training on how and when May 2010 American Nurse Today 25 Differentiating dementia and delirium Dementia is sometimes confused with delirium, but with adequate knowledge and assessment skills, you can differentiate the two disorders and help ensure appropriate intervention. Patients with dementia lack full cognitive capacity. Like those with delirium, their memory and judgment may be impaired. However, dementia signs and symptoms are less dramatic then those of delirium and are less likely to fluctuate. Also, dementia has a slow, steady insidious onset and progression, whereas delirium has a rapid onset. to initiate this procedure. Enacting periodic mock scenarios helps prepare staff for a true emergency. Staff members should use deescalation techniques and crisis communication to avert aggressive behavior. (See Managing a psychiatric crisis.) All healthcare facilities should implement and provide staff education in violence deescalation. Well-known programs include those from the Crisis Prevention Institute, Mandt System, and Pro-ACT. Some facilities have designed their own de-escalation programs. Early identification of and interventions for violent behavior promote appropriate care planning and improve communication among team members, who can share their perception of what works and what doesn’t. For instance, staff members can alert each other to potential violence triggers. Use of restraints Violent patients who pose an immediate danger to themselves or others may need to be physically restrained for a brief period until they can gain self-control. However, patient injuries and litigation risks associated with physical restraints are well documented, so restraints should be avoided whenever possible. Use them only as a last resort for the shortest time needed and in the least restrictive manner possible—and only if you’ve been trained in the proper application technique. The restrained patient should be moni26 American Nurse Today tored closely and appropriate interventions followed. Several regulatory agencies, such as the Centers for Medicare & Medicaid Services and the Joint Commission, have established guidelines for restraint use. Most likely, your facility has a policy and procedure that comply with these guidelines. All nurses applying restraints need to be familiar with these. Medications Medications may be given to calm a violent patient and promote selfcontrol. Work with the physician to identify the need for medication. Encourage the patient to ac- Suicidal patients Some med-surg patients have suicidal thoughts or exhibit suicidal behavior. Patients may be hospitalized after a failed suicide attempt, such as an intentional drug overdose, hanging, or a nonfatal gunshot wound. Other med-surg patients may become suicidal when hospitalized for other reasons. A 2007 Patient Safety Goal of the Joint Commission was to identify patients with suicidal ideation. Although that goal applies mainly to patients being treated for mental illness in psychiatric settings, acute-care general hospitals can adopt it to assess for this potential problem. Intervention For a patient with known or suspected suicidal tendencies, take appropriate precautions. Med-surg units can pose a danger to such a patient; even psychiatric units aren’t completely safe. As a rule of thumb, assume no place is completely safe. Patients can hang or strangle themselves with sheets, se de-escalation techniques and crisis communication to avert aggressive behavior. Some facilities have designed their own de-escalation programs. U cept the recommended drug, and administer it before the patient’s behavior escalates. Medications commonly used to reduce agitation include lorazepam (alone or in combination with haloperidol) and atypical antipsychotics, such as risperidone, olanzapine, and ziprasidone. These drugs are available orally; some can be given intramuscularly. Haloperidol (lactate form only) is available for I.V. use. Volume 5, Number 5 towels, bedclothes, tubing, or cords. They may take large doses of drugs (legal or illegal) that they have brought with them or saved up. Also, sharp objects abound in hospitals, and even plastic cutlery can prove dangerous to those intent on harming themselves. The best approach is to closely monitor the patient’s environment and behavior. Patients at high risk for suicidal behavior should receive www.AmericanNurseToday.com Managing a psychiatric crisis If your patient experiences a psychiatric crisis, use the following techniques to help de-escalate the situation. • Maintain a calm demeanor. • Speak in a soft, clear voice. • Convey empathy. For instance, ask, “How can I help you?” • Allow the patient to vent. • Listen to the patient; then reflect back what she has said so she knows you’ve been listening. This may make her more likely to be receptive to you. • Use appropriate problem-solving techniques. • Offer reassurance and support. Let the patient know you’re trying to ensure her safety. • Avoid a power struggle. • Don’t argue with the patient. • Keep your options open by avoiding definitive statements. one-on-one care. The staff member should stay within arm’s reach of the patient at all times and never leave, even for a break, until directly relieved by another staff member. Special skill sets If you work in a setting where many patients pose behavioral problems, consider obtaining further education in psychiatric problems and crisis management. For instance, emergency departments see more psychiatric emergencies than other hospital areas. Patients in intensive care units have a higher acuity and thus may require different approaches and interventions in psychiatric emergencies. If you work on a pediatric unit, you may require a specialized skill set to care for children and adolescents with psychiatric or emotional problems. A maternity nurse may encounter patients with severe postpartum psychiatric emergencies that call for interventions encompassing the mother, newborn, and family. Psychiatric emergencies can occur in any healthcare setting— acute-care, hospice, long-term care, and outpatient clinics as well as psychiatric facilities. Nurses caring for patients from all walks of life with any type of healthcare problem can expect to encounter patients who are at risk for or are experiencing a psychiatric crisis. Make sure you have a fundamental understanding of psychiatric problems, including their identification and intervention. ✯ Selected references Allen M, Currier GW, Hughes DH, Reyes- CE POST-TEST — Psychiatric emergencies in med-surg patients: Are you prepared? Instructions To take the post-test for this article and earn contact hour credit, please go to www.AmericanNurseToday.com/ContinuingEducation .aspx. Simply use your Visa or MasterCard to pay the processing fee. (Online: ANA members $15; nonmembers $20.) Once you’ve successfully passed the post-test and completed the evaluation form, you’ll be able to print out your certificate immediately. If you are unable to take the post-test online, complete the print form and mail it to the address at the bottom of the next page. (Mail-in test fee: ANA members $20; nonmembers $25.) www.AmericanNurseToday.com Harde M, Docherty JP. The Expert Consensus Guidelines™: Treatment of Behavioral Emergencies. A Postgraduate Medicine Special Report. New York, NY: McGraw-Hill; 2001. Fossett B, Nadler-Moodie M, Thobaben M. Psychiatric Principles and Applications for General Patient Care. 4th ed. Brockton, MA: Western Schools; 2004. Gilbert SB. Psychiatric crash cart: Treatment strategies for the emergency department. Adv Emerg Nurs J. 2009;31(4):298-308. Hermanns MS, Russell-Broaddus CA. “But I’m not a psych nurse!” RN. 2006;69(12):28-31. Kerrison SA, Chapman R. What general emergency nurses want to know about mental health patients presenting to their emergency department. Accid Emerg Nurs. 2007;15:48-55. Ramadan M. Managing psychiatric emergencies. Internet J Emerg Med. 2007;4(1). http:// www.ispub.com/ostia/index.php?xmlFilePath =journals/ijem/vol4n1/psycho.xml. Accessed March 10, 2010. Stokowski L. Alternatives to restraint and seclusion in mental health settings: Questions and answers from psychiatric nurse experts. Medscape Nurses. May 5, 2007. http:// www.medscape.com/viewarticle/555686. Accessed March 10, 2010. Sullivan JT, Sykora K, Sneiderman J, Naranjo CA, Sellars EM. Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWAAR). Brit J Addict. 1989;84:1353-1357. www3 .interscience.wiley.com/journal/119445441/ abstract. Accessed March 10, 2010. Marlene Nadler-Moodie is a clinical nurse specialist in psychiatry and mental health nursing at Sharp Mesa Vista Hospital and Scripps Mercy Hospital in San Diego, California. The planners and author of this CNE activity have disclosed no relevant financial relationships with any commercial companies pertaining to this activity. Provider accreditation The American Nurses Association Center for Continuing Education and Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. ANA is approved by the California Board of Registered Nursing, Provider Number 6178. Contact hours: 1.7 Expiration: 12/31/13 Post-test passing score is 75%. ANA Center for Continuing Education and Professional Development’s accredited provider status refers only to CNE activities and does not imply that there is real or implied endorsement of any product, service, or company referred to in this activity nor of any company subsidizing costs related to the activity. This CNE activity does not include any unannounced information about off-label use of a product for a purpose other than that for which it was approved by the Food and Drug Administration (FDA). May 2010 American Nurse Today 27 CE POST-TEST • Psychiatric emergencies in med-surg patients: Are you prepared? Earn contact hour credit online at www.americannursetoday.com/ContinuingEducation.aspx (ANT100501) Please circle the correct answer. 1. Which statement about psychiatric problems is correct? a. Psychiatric disorders in med-surg patients are rare. b. People with psychoses are at lower risk for health problems than other population subsets. c. Psychosis is the seventh-highest-volume diagnosticrelated group. d. Nearly half of Americans have experienced mentalhealth disorders. 2. Which strategy for early identification of psychiatric problems in med-surg patients is not appropriate? a. Seek corroboration from family members as needed. b. Determine if the patient is taking psychiatric medications. c. Assume that psychiatric disorders are short-term problems. d. Assess for possible causes if the patient has no known psychiatric disorder. 3. When communicating with patients with psychiatric problems who can’t think clearly or who lack good judgment and decision-making skills, you should: a. contradict the patient’s skewed view of reality. b. agree with the patient’s skewed view of reality. c. use words of 8 to 10 letters in sentences containing six to eight words. d. use words of five or six letters in sentences containing five or six words. 4. Which statement about hallucinations is accurate? a. They manifest as reports of false sensory input. b. They do not stem from such conditions as infection or drug toxicity. c. They involve beliefs that have no basis in reality. d. They manifest as reports of conspiracies against the patient. 5. Which statement about delusions is true? a. They are fixed beliefs with no basis in reality. b. They do not arise from a psychiatric disorder. c. They do not arise from med-surg complications. d. They manifest as seeing visions or hearing voices. 6. Alcohol withdrawal may not occur until how many hours after a person’s last drink? a. 6 to 10 hours b. 10 to 20 hours c. 24 to 48 hours d. 24 to 72 hours 7. A common, easy-to-administer tool for assessing alcohol withdrawal and guiding treatment is the: a. Clinical Institute Withdrawal Assessment—Alcohol, Revised. b. National Institute Withdrawal Assessment—Alcohol, Edited. c. National Alcohol Withdrawal Assessment—Revised. d. Clinical Alcohol Withdrawal Assessment—Edited. 8. Which of the following is a sign or symptom of alcohol withdrawal? a. Absence seizures b. Bradycardia c. High blood pressure d. Sleepiness 9. Which statement about dementia is accurate? a. Dementia has a rapid onset. b. Patients with dementia have full cognitive capacity. c. Patients with dementia lack full cognitive capacity. d. Dementia signs and symptoms are dramatic. 10. Which statement about delirium is accurate? a. Delirium does not impair the patient’s memory. b. Delirium has a rapid onset. c. Delirium signs and symptoms are not dramatic. d. Delirium progresses steadily. Evaluation form (required) 1. In each blank, rate your achievement of each objective from 1 (low/poor) to 5 (high/excellent). (1.) Describe how to assess patients for potential psychiatric problems. ____ (2.) Identify signs and symptoms of common psychiatric emergencies on the med-surg unit. ____ (3.) Discuss appropriate interventions for common psychiatric emergencies. ____ Purpose/goal: To help med-surg nurses identify and manage CE: 1.7 contact hours 11. Which intervention might be appropriate for a patient with delirium? a. Avoid an orderly environment for a patient with disorganized thinking. b. Avoid routine for a patient with disorganized thinking. c. Frequently change the location of items in the room. d. Distract a distraught patient from the task at hand. 12. To de-escalate a psychiatric crisis, you should: a. maintain a calm demeanor. b. speak in a firm, loud voice. c. prevent the patient from venting. d. interrupt to distract the patient. 13. Which strategy is appropriate when dealing with a patient who has become violent? a. Approach the patient alone. b. Don’t approach the patient alone. c. Ask colleagues to stay far away. d. Move into the patient’s physical space. 14. Which statement about the use of restraints for a patient with violent behavior is correct? a. Restraints rarely are associated with a risk of litigation. b. Once applied, keep restraints on the patient for at least 4 hours. c. Regulatory agencies typically don’t issue guidelines on restraint use. d. Restraints should be avoided whenever possible. 15. Patients at high risk for suicide should be: a. receiving one-on-one care. b. left alone for no more than 5 minutes. c. restricted from access to plastic cutlery. d. left alone for no more than 10 minutes. Also rate the following from 1 to 5. 2. The relatedness and effectiveness of the purpose, objectives, content, and teaching strategies. ____ 3. The author(s)’competence and effectiveness. ____ 4. The activity met your personal expectations. ____ 5. The application to and usefulness of the content in your nursing practice. ____ 6. Freedom from bias due to conflict of interest, commercial support, product endorsement or unannounced off-label use. ____ 7. State the number of minutes it took you to read the article and complete the post-test and evaluation. ____ psychiatric emergencies Comments: ______________________________________________________ ________________________________________________________________ P LEASE P RINT C LEARLY Home phone Name — — — — — — — — — — — — — — — — — — — — — — — — — — Business phone — — — — — — — — — — — — Mailing address — — — — — — — — — — — — — — — — — — — — — — — Fax City — — — — — — — — — — — — — — — — — — — — — — — — — — — E-mail — — — — — — — — — — — — — — — — — — — — — State — — ———————————— ———————————— Zip — — — — — - — — — — Method of payment (ANA members $20; nonmembers $25) ■ Check payable to American Nurses Association. ■ Visa ■ MasterCard PLEASE DO NOT SEND CASH Amount authorized $____________________________________ For credit cards: Mail completed evaluation, post-test, registration form, and payment to: ANA, PO Box 504410, St. Louis, MO 63150-4410 Expiration date _________________________ 28 American Nurse Today Volume 5, Number 5 Account # ■■■■■■■■■■■■■■■■■ Authorized signature__________________________________________ www.AmericanNurseToday.com