2015 HTN ExecutiveOverview Final

2015 Executive Overview
An Independent Licensee of the Blue Cross and Blue Shield Association
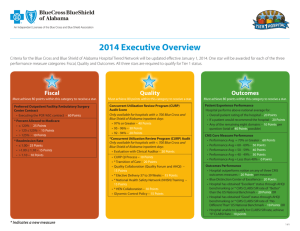
Criteria for the Blue Cross and Blue Shield of Alabama Hospital Tiered Network will be updated effective January 1, 2015. One star will be awarded for each of the three performance measure categories: Fiscal, Quality and Outcomes. All three stars are required to qualify for Tier 1 status.
Fiscal
Must achieve 80 points within this category to receive a star.
Preferred Outpatient Facility/Ambulatory Surgery
Center Contract
• Executing the POF/ASC contract – 60 Points
Percent Allowed to Medicare
• ≤ 120% – 25 Points
• > 120 ≤ 125% – 15 Points
• > 125% – 10 Points
Readmission Rate
• ≤ 1.00 – 25 Points
• > 1.00 ≤ 1.10 – 15 Points
• > 1.10 – 10 Points
Quality
Must achieve 80 points within this category to receive a star.
Concurrent Utilization Review Program (CURP)
Quality Improvement Process – 30 Points
CURP Audit
Only available for hospitals with ≥ 700 Blue Cross and
Blue Shield of Alabama inpatient days
≥ 92% or greater – 20 Points
CURP Audit Score
Only available for hospitals with < 700 Blue Cross and
Blue Shield of Alabama inpatient days
Evaluation with Clinical Auditor – 20 Points
• Transition of Care – 20 Points
• Quality Collaboration (Quality Forum and AHQI) –
15 Points
• Elective Delivery 37 to 39 Weeks – 15 Points
• * Participation in National Registries/Rural Quality
Network – 10 Points
• National Healthcare Safety Network (NHSN) Training
– 10 Points
• * Surviving Sepsis Campaign – 10 Points
* Indicates a new measure
Outcomes
Must achieve 80 points within this category to receive a star.
Patient Experience Performance
Hospital performs above national average for:
• Overall patient rating of the hospital – 20 Points
• If a patient would recommend the hospital – 20 Points
• Any of the remaining eight domains – 10 Points per question (total of 40 Points possible)
CMS Core Measure Performance
• Performance Avg = 70% or Greater – 40 Points
• Performance Avg = 60 - 69% – 30 Points
• Performance Avg = 50 - 59% – 20 Points
• Performance Avg = 40 - 49% – 10 Points
Outcomes Performance
• Hospital outperforms nation on any of three CMS outcomes measures – 20 Points per measure
• Hospital has obtained “Excellent” status through AHQI benchmarking or *CMS CLABSI or CAUTI SIR rate of
“Better” than the US National Benchmark – 20 Points OR
• Hospital has obtained “Good” status through AHQI benchmarking or *CMS CLABSI or CAUTI SIR rate of
“No Different Than” US National Benchmark – 10 Points
• Hospital Performance on CMS Outpatient Imaging and Emergency Room Measures
• Performance Avg = 70% or Greater – 30 Points
• Performance Avg = 60 - 69% – 25 Points
• Performance Avg = 50 - 59% – 20 points
• Performance Avg = 40 - 49% – 15 Points
• Blue Distinction Center of Excellence – 20 Points
1 of 6
Fiscal – 80 Points
Preferred Outpatient Facility/Ambulatory Surgery Center Contract – 60 Points Possible
The Preferred Outpatient Facility/Ambulatory Surgery Center (POF/ASC) contract has a fee schedule that reimburses select outpatient surgery procedures based on an Ambulatory Surgery Center grouping. It also has the standard contractual cost plus arrangement for other outpatient medical services.
Points awarded to hospitals that have executed the POF/ASC contract.
Percent Allowed to Medicare – 25 Points Possible
The Percent Allowed to Medicare is a ratio determined by comparing the Blue Cross Allowed Amount to the Medicare Allowed Amount. The estimated Medicare
Allowed Amount is calculated using Medicare’s Inpatient Prospective Payment System (IPPS) and Outpatient Prospective Payment System (OPPS) methodologies based on Medicare Severity Diagnosis Related Group (MS-DRG) and Ambulatory Payment Classifications (APC) systems, respectively, to compare corresponding Blue Cross
Allowed Amounts for the same Blue Cross claims. The profiled claims include Blue Cross and Blue Shield of Alabama primary claims incurred between July 1, 2013, through June 30, 2014, and processed through September 30, 2014. It does not include secondary claims or Blue Advantage claims.
Points awarded to hospitals are as follows:
• ≤120% – 25 points
• >120 ≤ 125% – 15 points
• >125% – 10 points
Readmission Rate – 25 Points Possible
The Severity Adjusted Readmission Index is calculated using a severity adjusting claims grouper called APR-DRG* to group inpatient claims into a single line item for each discharge. The APR-DRG grouper assigns each claim with a Severity of Illness (SOI) indicator, which takes into account the patient’s co-morbidities and other clinical information coded during the discharge. All eligible hospital discharges in the state are aggregated and the readmission rate is calculated for each APR-
DRG and SOI. This statewide calculation becomes the expected readmission rate for all patients with a given APR-DRG and SOI. The expected readmission rate is calculated for each provider by summing the benchmark rate for each of the provider’s discharges by APR-DRG and SOI indicators.
The profiled claims include Blue Cross and Blue Shield of Alabama primary claims incurred between July 1, 2013, through June 30, 2014, and processed through
September 30, 2014. It does not include secondary claims or Blue Advantage claims.
Points awarded to hospitals for Readmission Index are as follows:
• ≤1.00 – 25 points
• >1.00 ≤1.10 – 15 points
• >1.10 – 10 points
* Produced using proprietary computer software created, owned and licensed by the 3M Company. All copyrights in and to the 3M Software (including the selection, coordination and arrangement of all codes) are owned by 3M. All rights reserved.
2 of 6
Quality – 80 Points
CURP Quality Improvement Process – 30 Points Possible
Hospitals will receive points for submitting a CURP Quality Improvement (QI) Process to their assigned Blue Cross Clinical Auditor. To receive points, the QI process must be reviewed and approved by the Clinical Auditor by September 30, 2014.
CURP Audit Score (Only available for hospitals with ≥ 700 Blue Cross inpatient days) – 20 Points Possible
Audit scores from the fourth quarter of 2013 through the third quarter of 2014 are averaged. Points will be awarded for an average audit score of 92 or greater.
Hospitals scheduled for only one audit during the evaluation period may request a second audit to meet the standard.
CURP Review Audit (Only available for hospitals with < 700 Blue Cross inpatient days) – 20 Points Possible
A CURP hospital reviewer will participate with Blue Cross Clinical Auditors in a detailed review of 20 days, or no more than 10% of all inpatient days, to ensure medical necessity for inpatient admission and continued stay appropriateness as evidenced by the clinical record.
Transition of Care – 20 Points Possible
Transition of care is a critical step in ensuring quality outcomes once patients are discharged or transferred from a particular location. In 2014, Blue Cross introduced a focus on Transition of Care by encouraging hospitals to have documented policies and processes in place for all inpatients discharged to home (excluding home health, nursing home and emergency department) and a tracking effort designed to measure the effectiveness of that process. Transition of Care includes logistical arrangements, education of the patient and family, and coordination among the health professional involved in assisting patients.
Hospitals will receive points for achieving a ≥ 50% average on these four measures for all inpatients discharged to home (excludes home health, nursing home and emergency department):
• Medication reconciliation for all patients prior to discharge
• Scheduling of follow-up visits prior to patient’s discharge
• Providing discharge summary report to primary care physician (PCP) within three business days of discharge. If patient does not have a PCP, assist with identifying a PCP and send summary report
• Follow-up calls to patients with a high risk for admission (e.g., COPD, CAD, CHF, etc.) and a tracking effort designed to measure the effectiveness of that process
Quality Collaboration – 15 Points Possible
The Quality Forum and the Alabama Hospital Quality Initiative (AHQI) Best Practice Meetings are collaborations between Blue Cross and Blue Shield of Alabama, the
Alabama Hospital Association, CareFusion MedMined Services, the Alabama Quality Assurance Foundation, Alabama Department of Public Health and the Medical
Association of the State of Alabama.
Meeting Dates:
AHQI Webinars: January 14, 2014, and July 15, 2014
Quality Forum/AHQI Meetings: May 12, 2014, and October 21, 2014
Points Breakdown
Meetings refer to either AHQI Webinars or Quality Forum meetings.
• Attendance at four meetings – 15 points
• Attendance at three meetings – 10 points
• Attendance at two meetings – 5 points
3 of 6
Elective Delivery 37 to 39 weeks – 15 Points Possible
The American Congress of Obstetricians and Gynecologists (ACOG) recommend 39 completed weeks of gestation prior to delivery except when medically indicated.
Elective labor inductions and cesarean deliveries between 37 to 39 weeks gestation have dramatically increased over the last several years. A recent review of evidence shows that elective deliveries can cause unnecessary health risks for babies and increase the hospital length of stay for mothers. Eliminating non-medically indicated deliveries prior to 39 weeks is a national quality measure for Leapfrog, the National Quality Forum and the Joint Commission. Blue Cross is also concerned about the potential adverse patient outcomes due to elective deliveries between 37 to 39 weeks gestation.
A reported delivery rate of ≤ 3 percent for elective deliveries between 37 to 39 weeks gestation from July 2013 through June 2014. Note, the rate reported is meant to represent the following equation: (The number of elective deliveries occurring within 37-39 weeks)/(Total deliveries in the facility).
Participation in National Registries/Rural Quality Network – 10 Points
A registry collects and analyzes information on certain medical topics, conditions, or procedures for hospitals or other providers. The registry then provides the hospitals or providers with information to help them improve the care they provide. The Centers for Medicare & Medicaid Services (CMS) Hospital Inpatient Quality
Reporting (IQR) program includes structural measure questions with respect to participation in systematic databases for cardiac surgery, stroke care, nursing sensitive care and/or general surgery. Hospitals that participate in one of the registries considered by and reported to CMS or other identified registries or hospitals that do not submit information to a national registry but do participate with the Rural Quality Network may also receive points.
CMS-identified registries are listed below. Participation in other national registries will also be accepted. Use the checklist to identify.
• The Society of Thoracic Surgeons Cardiac Surgery Registry
• American Heart Association/America Stroke Association Get With the Guidelines Program
• Centers for Disease Control’s Paul Coverdell National Acute Stroke Registry
• American Nursing Association’s National database of Nursing Quality Indicators
• American College of Surgeons National Surgical Quality Improvement Program Registry
New
National Healthcare Safety Network (NHSN) Training - 10 Points Possible
The Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network is one of the nation’s most widely used healthcare-associated infection tracking systems. NHSN provides hospitals, State Public Health organizations, states, regions and the nation with data needed to identify problem areas and to measure progress for the efforts of prevention with the goal to eliminate healthcare-associated infections. The data is analyzed by the CDC as well as other entities to direct actions for healthcare hospital-associated infections prevention. CMS reporting requirements change from year to year so it is critical that infection preventionists understand the changes in order to provide the best, most accurate and timely reports.
Participate in one of the AQAF NHSN training sessions or provide evidence Infection Preventionist attended advanced NHSN training during 2014.
Surviving SEPSIS Campaign – 10 Points
The Surviving Sepsis Campaign (SSC), a quality improvement initiative to increase early recognition and treatment of sepsis in patients on hospital medical, surgical and telemetry units, has partnered with the Institute of Healthcare Improvement (IHI) to incorporate its “bundle concept” into the diagnosis and treatment of patients with severe sepsis and septic shock. The use of “bundles” is a selected set of elements of care from evidence-based guidelines that when implemented as a group has an effect on outcomes beyond implementing the individual elements alone. The goal of compliance with the severe sepsis bundle is to reduce mortality due to sepsis. Information about the Surviving Sepsis Campaign and Bundles can be found at http://www.survivingsepsis.org
or at
IHI, http://www.ihi.org/resources/Pages/Measures/ComplianceSevereSepsisBundles.aspx
.
New
Hospital will receive points for attesting that the facility has implemented either the three-hour or six-hour Sepsis Bundle.
4 of 6
Outcomes – 80 Points
Patient Experience Performance – 80 Points Possible*
Hospital performs at or above the national average based on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) questions.
• Overall patient rating of hospital – 20 points
• If a patient would recommend the hospital – 20 points
• Any of the remaining eight domains – 40 points possible (10 points per question)
CMS Core Measure Performance – 40 Points Possible*
CMS requires the reporting of hospital process of care measures, which include: heart attack care, heart failure care, pneumonia care and prevention of surgical infection.
Hospitals will receive points based on CMS Core Measure results based on the September 2014 data release for the time period of January through December 2013.
Your hospital’s score will be based on a performance average. To calculate your performance average, one point will be awarded for every measure that exceeds a score of 95%. For example: Your facility submits 20 measures to CMS. An example of the calculation:
15 (# of measures≥95% )
20 (# of measures submitted)
• Performance Average = 70% or greater – 40 points
• Performance Average = 60 - 69% – 30 points
= 75% (Performance Average)
• Performance Average = 50 - 59% – 20 points
• Performance Average = 40 - 49% – 10 points
Quality Outcomes and Infection Reduction Performance – 60 Points Possible (20 points per measure)
CMS Outcome Mortality – This measure allows for recognition of Alabama hospitals that are outperforming the national rate on CMS outcome-related measures. CMS released risk-adjusted measures that illustrate hospital mortality performance in relation to the U.S. National Rate. These measures are revised on an annual basis using a three-year time period. The next release is in July 2014 and will contain data from July 2010 through June 2013. Top performers are defined on these CMS outcomerelated measures.
Hospital outperforms the U.S. National Rate on any of the three CMS outcome mortality measures (Heart Failure, Pneumonia or Acute Myocardial Infection).
Infection Reduction Performance – 20 Points Possible
Hospital with AHQI Benchmarking
• “Excellent” status through AHQI benchmarking – 20 points
• “Good” status through AHQI benchmarking – 10 points
OR
Facilities without AHQI benchmarking
• CMS Central Line-Associated Blood Stream Infections (CLABSI) or Catheter-Associated Urinary Tract Infection (CAUTI) Standardized Infection Ratio (SIR) rate of “Better”
than the US National Benchmark – 20 points
• CMS CLABSI or CAUTI SIR rate of “No Different Than” the US National Benchmark – 10 points
5 of 6
Other Measures – 30 Points Possible*
CMS Emergency Department and Outpatient Imaging Efficiency Measures
As part of the Hospital Inpatient Quality Reporting (IQR) and Outpatient Quality Reporting Programs (OQR), CMS evaluates how hospitals treat patients who come to the hospital with medical emergencies and how often a hospital provides specific imaging tests for Medicare beneficiaries. Hospitals will receive points on the six combined
CMS Emergency Department measures and six Outpatient Imaging measures with “less than or equal to the national average” results based on the September 2014 data release for the time period of January through December 2013. Note, the measure “Outpatients who had a follow-up mammogram, ultrasound, or MRI of the breast within
45 days after a screening mammogram” is not compared to a national average; therefore, a score greater than zero and less than 14% is considered passing.
Your hospital’s score will be based on a performance average for combined measures. An example of the calculation:
6 (# of measures≥95% )
= 50% (Performance Average)
12 (# of measures submitted)
• Performance Average = 70% or greater – 30 points
• Performance Average = 60 - 69% – 25 points
• Performance Average = 50 - 59% –
• Performance Average = 40 - 49% –
20 points
15 points
New
Recognition as a Blue Distinction® Center+ or a Blue Distinction® Center – 20 points
* Rescore can be requested in subsequent quarter.
Note: Blue Distinction® Centers met overall quality measures for patient safety and outcomes, developed with input from the medical community. Blue Distinction® Centers+ also met cost measures that address consumers’ need for affordable healthcare. Individual outcomes may vary. National criteria is displayed on www.bcbs.com. A local Blue Plan may require additional criteria for facilities located in its own service area. To find out which services and providers (including hospital-based physicians) are covered under your policy, or to learn about local Blue Plan criteria, contact your local Blue Plan; and contact your provider before making an appointment to verify its current Network and Blue Distinction Centers status. Each hospital’s Cost Index is calculated separately, based on data from its local Blue Plan. Hospitals in portions of CA, ID, NY, PA, and WA may lie in areas served by two local Blue Plans, resulting in two Cost Index figures; and their own local Blue Plans decide whether all hospitals in these areas must meet Blue Distinction Centers+ national criteria for one or both Cost Index figures. Neither the Blue Cross and Blue Shield Association nor any Blue Plans are responsible for damages, losses, or non-covered charges resulting from Blue Distinction or other provider finder information or care received from Blue
Distinction or other providers. To find out more, contact your local Blue Plan.
6 of 6