An Independent Licensee of the Blue Cross and Blue Shield Association
2014 Executive Overview
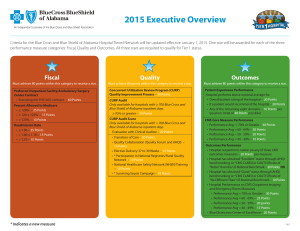
Criteria for the Blue Cross and Blue Shield of Alabama Hospital Tiered Network will be updated effective January 1, 2014. One star will be awarded for each of the three
performance measure categories: Fiscal, Quality and Outcomes. All three stars are required to qualify for Tier 1 status.
Fiscal
Must achieve 80 points within this category to receive a star.
Preferred Outpatient Facility/Ambulatory Surgery
Center Contract
• Executing the POF/ASC contract – 60 Points
* Percent Allowed to Medicare
• ≤ 120% – 25 Points
• > 120 ≤125% – 15 Points
• > 125% – 10 Points
* Readmission Rate
• ≤ 1.00– 25 Points
• >1.00 ≤ 1.10 – 15 Points
• > 1.10 – 10 Points
* Indicates a new measure
Quality
Outcomes
Must achieve 80 points within this category to receive a star.
Must achieve 80 points within this category to receive a star.
Concurrent Utilization Review Program (CURP)
Audit Score
Only available for hospitals with ≥ 700 Blue Cross and
Blue Shield of Alabama inpatient days
• 97% or Greater – 40 Points
• 95 - 96% – 30 Points
• 92 - 94% – 20 Points
*Concurrent Utilization Review Program (CURP) Audit
Only available for hospitals with < 700 Blue Cross and
Blue Shield of Alabama inpatient days
• Evaluation with Clinical Auditor – 20 Points
• CURP QI Process – 10 Points
• * Transition of Care – 20 Points
• Quality Collaboration (Quality Forum and AHQI) –
15 Points
• * Elective Delivery 37 to 39 Weeks – 15 Points
• * National Health Safety Network (NHSN) Training –
15 Points
• * HEN Collaboration – 10 Points
• Glycemic Control Policy – 15 Points
Patient Experience Performance
Hospital performs above national average for:
• Overall patient rating of the hospital – 20 Points
• If a patient would recommend the hospital – 20 Points
• Any of the remaining eight domains – 10 Points per
question (total of 40 Points possible)
CMS Core Measure Performance
• Performance Avg = 70% or Greater – 60 Points
• Performance Avg = 60 - 69% – 50 Points
• Performance Avg = 50 - 59% – 40 Points
• Performance Avg = 40 - 49% – 30 Points
• Performance Avg = Less than 40% – 0 Points
Outcomes Performance
• Hospital outperforms nation on any of three CMS
outcomes measures – 20 Points per measure
• Blue Distinction Center of Excellence – 20 Points
• Hospital has obtained “Excellent” status through AHQI
benchmarking or * CMS CLABSI SIR rate of “Better”
than the US National Benchmark – 20 Points OR
• Hospital has obtained “Good” status through AHQI
benchmarking or * CMS CLABSI SIR rate of “No
Different Than” US National Benchmark – 10 Points OR
• Hospital unable to qualify for CLABSI SIR rate, achieve
“0” CLABSI Rate - 10 points
1 of 6
Fiscal Efficiency – 80 Possible Points
Preferred Outpatient Facility/Ambulatory Surgery Center Contract
The Preferred Outpatient Facility/Ambulatory Surgery Center (POF/ASC) contract has a fee schedule that reimburses select outpatient surgery procedures based on
an Ambulatory Surgery Center grouping. It also has the standard contractual cost plus arrangement for other outpatient medical services.
• Points awarded to hospitals that have executed the POF/ASC contract – 60 points
Percent Allowed to Medicare
The Percent Allowed to Medicare is a ratio determined by comparing the Blue Cross Allowed Amount to the Medicare Allowed Amount. The estimated Medicare
Allowed Amount is calculated using Medicare’s Inpatient Prospective Payment System (IPPS) and Outpatient Prospective Payment System (OPPS) methodologies
based on MS-DRG and APC systems, respectively, to compare corresponding Blue Cross Allowed Amounts for the same Blue Cross claims. The profiled claims include
Blue Cross and Blue Shield of Alabama primary claims incurred between July 1, 2012, through June 30, 2013, and processed through September 30, 2013. It does not
include secondary claims or Blue Advantage claims.
• Points awarded to hospitals are as follows:
o ≤120% – 25 points
o >120 ≤125% – 15 points
o >125% – 10 points
New
Readmission Rate
The Severity Adjusted Readmission Index is calculated using a severity adjusting claims grouper called APR-DRG* to group inpatient claims into a single line item for
each discharge. The APR-DRG grouper assigns each claim with a Severity of Illness (SOI) indicator, which takes into account the patient’s co-morbidities and other
clinical information coded during the discharge. All eligible hospital discharges in the state are aggregated, and the readmission rate is calculated for each APRDRG and SOI. This statewide calculation becomes the expected readmission rate for all patients with a given APR-DRG and SOI. The expected readmission rate is
calculated for each provider by summing the benchmark rate for each of the provider’s discharges by APR-DRG and SOI indicators.
The profiled claims include Blue Cross and Blue Shield of Alabama primary claims incurred between July 1, 2012, through June 30, 2013, and processed through
September 30, 2013. It does not include secondary claims or Blue Advantage claims.
• Points awarded to hospitals for Readmission Index are as follows:
o ≤1.00 – 25 points
o >1.00 ≤1.10 – 15 points
o >1.10 – 10 points
New
* Produced using proprietary computer software created, owned and licensed by the the 3M Company. All copyrights in and to the 3M Software (including the selection, coordination and arrangement of all codes)
are owned by 3M. All rights reserved.
2 of 6
CURP Audit Score (Only available for hospitals with ≥ 700 Blue Cross inpatient days) – 40 Points Possible
Audit scores from the fourth quarter of 2012 through the third quarter of 2013 are averaged. Points will be awarded as follows:
• 97% or Greater – 40 points
• 95 - 96% – 30 points
• 92 - 94% – 20 points
Hospitals scheduled for only one audit during the evaluation period may request a second audit to meet the standard.
CURP Review Audit (Only available for hospitals with < 700 Blue Cross inpatient days) – 20 Points Possible
A CURP hospital reviewer will participate with Blue Cross Clinical Auditors in a detailed review of 20 days, or no more than 10% of all inpatient days,
to ensure medical necessity for inpatient admission and continued stay appropriateness as evidenced by clinical record.
New
CURP Quality Improvement (QI) Process – 10 Points Possible
Hospital will receive points for submitting either of the following to their assigned Blue Cross Clinical Auditor:
• Outcomes/improvements to CURP process as identified during current Quality Improvement Processes by September 30, 2013 – 10 points
OR
• Development and implementation of a new CURP QI process with initial results. Plan must be approved with the Blue Cross Clinical Auditor by September 1, 2013,
and initial results submitted by September 30, 2013 – 10 points
Transition of Care – 20 Points Possible
Transitional care is a critical step in ensuring quality outcomes once patients are discharged or transferred from a particular location. For 2014, Blue Cross would
encourage hospitals to have documented policies in place and a tracking effort designed to measure the effectiveness of the current process. Transition of Care
includes logistical arrangements, education of the patient and family, and coordination among the health professionals involved in assisting the patient.
Hospitals will receive points for attesting that the facility has continuity/transition of care processes outlined below for all inpatients released to home (excludes
home health, nursing home and emergency department) by September 30, 2013 – 15 points:
•
•
•
•
Medication reconciliation for all patients prior to discharge
Scheduling of follow-up visits prior to patient’s discharge
Providing discharge summary report to primary care physician within 3 business days of discharge
Follow-up calls to patients with a high risk for readmission (e.g., COPD, CAD, CHF, etc.)
Hospitals will receive additional points for sharing outcomes/measures of their Transition of Care processes (outlined below) by September 30, 2013, for the time
period of July 2012 through June 2013 – 5 points:
•
•
•
•
Percentage of patients with medication reconciliation performed prior to discharge
Percentage of patients with follow-up visits scheduled
Percentage of discharge summary reports to Primary Care Physician within 3 business days
Number of calls completed within 3 business days (percentage of population)
New
3 of 6
Quality Collaboration – 15 Points Possible
The Quality Forum and AHQI Best Practice Meetings are collaborations between Blue Cross and Blue Shield of Alabama, the Alabama Hospital Association,
CareFusion MedMined Services and the Alabama Quality Assurance Foundation.
Meeting Dates:
AHQI Webinars: January 28, 2013, and July 23, 2013
Quality Forum/AHQI Meetings: April 16, 2013, and October 15, 2013
Points Breakdown
Meetings refer to either Quality Forum meetings or AHQI Webinars.
• Attendance at four meetings – 15 points
• Attendance at three meetings – 10 points
• Attendance at two meetings – 5 points
Elective Delivery 37 to 39 weeks – 15 Points Possible
The American Congress of Obstetricians and Gynecologists (ACOG) recommend 39 completed weeks of gestation prior to delivery except when medically indicated.
Elective labor inductions and cesarean deliveries between 37 to 39 weeks gestation have dramatically increased over the last several years. Recent reviews of evidence
shows that elective deliveries can cause unnecessary health risks for babies and increase hospital length of stay for mothers. Eliminating non-medically indicated
deliveries prior to 39 weeks is a national quality measure for Leapfrog, the National Quality Forum and the Joint Commission. Blue Cross is concerned about the
potential adverse patient outcomes due to elective deliveries 37 to 39 weeks gestation.
New
• Hospital submits an attestation of an implemented policy by September 30, 2013, with data to support ACOG compliance for eliminating elective
non-medically indicated deliveries – 5 points
• A reported delivery rate of ≤ 5 percent for elective deliveries between 37 to 39 weeks gestation from July 2012 through June 2013. NOTE: Indicate when reporting
if the period is 1/1/2013 through 6/1/2013 – 10 points
National Health and Safety Network (NHSN) Training – 15 Points Possible
To standardize the reporting of infections, the CDC has developed five new self-study competency training courses for the Device–associated Module of NHSN. The
person responsible for infection prevention as it relates to NHSN must complete the course(s) with an 80% score and provide a copy of Certificate of Completion for
each course to Blue Cross. Hospitals may receive 5 points for each module successfully completed (up to 3) between 10/1/2012 through 9/30/2013.
These five courses are located under Patient Safety Component:
•
•
•
•
•
Introduction to the Device-Associated Module
Central Line-Associated Blood Stream Infection (CLABSI)
Ventilator-Associated Pneumonia (VAP) Surveillance
Catheter Associated Urinary Tract Infection (CAUTI)
Central Line Insertion Practices (CLIP) Adherence Monitoring
New
Links to the training are found on the Alabama Department of Public Health (ADPH) website, www.adph.org/hai, or directly at www.cdc.gov/nhsn/training.
4 of 6
Hospital Engagement Network (HEN) Collaboration – 10 Points Possible
Blue Cross would like to support the collaborative Hospital Engagement Networks (HENs) that are in place and encourage hospitals that are not involved in a HEN
to participate. HENs are working to identify solutions that reduce health-acquired conditions, establish ways to develop learning opportunities for hospitals, and
provide initiatives to improve patient safety. HENs seek to reduce avoidable re-hospitalizations with effective care coordination and transition of care. Additional
information can be found online at http://partnershipforpatients.cms.gov.
Blue Cross is partnering with the Alabama Quality Assurance Foundation (AQAF), Alabama’s Medicare Quality Improvement Organization (QIO), HEN participants and
other facilities in a statewide learning collaborative. The goal of this collaborative is to support the Partnership for Patients, the HEN initiatives and Centers for Medicare
& Medicaid Services (CMS) QIO goals of reducing 30-day rehospitalizations using the Institute for Healthcare Improvement’s (IHI) State Action on Avoidable
Rehospitalization (STAAR) Initiative evidence-based intervention.
The collaborative will include participation in AQAF conference calls, identification of an intervention, and sharing results.
The goals of the first phase of this collaborative are to:
• Identify the current HEN involvement in the state of Alabama.
• Identify facilities not currently in a HEN who are interested in joining a statewide initiative with the same goals.
• Participate in an AQAF conference call prior to September 30, 2013.
New
Points will be awarded to hospitals who complete all the following: (10 points)
• Complete the attestation form notating participation in a HEN or agreeing to participate in a similar statewide initiative with AQAF, and return attestation by July 15, 2013.
• Provide names of Quality Contacts for participation in the AQAF conference call.
• Participate in the initial AQAF conference call to be conducted prior to September 30, 2013.
Glycemic Control Policy in Place – 15 Points Possible
The IHI Map is an online tool that distills the best knowledge available from the key process improvements that lead to exceptional patient care. In 2011, hospitals
completed the IHI GAP Analysis Survey to help identify areas for improvement in their facilities. Opportunities for improvement were identified from the survey
through collaboration with the AlaHA Quality Task Force. In 2012, hospitals shared their policies and procedures and it was identified that there are gaps in policies
based on national standards. For the 2014 Hospital Tiered Network, hospitals must implement an improvement process on Glycemic Control for all non-critically ill
patients. This improvement process should include specific elements that can be measured within a set time frame. One example of an improvement process is the
IHI model, which includes a three-part measurement system to assess the adequacy of glucose control. The IHI model can be reviewed online at www.ihi.org.
Policies and procedures should allow hospitals to measure the following:
o
o
o
Percent of patients with blood sugars in the 60 to 180 mg/dL range
Percent of patients with blood sugars in the 0 to 59 mg/dL range
Percent of patients with blood sugars greater than 181 mg/dL
New
• Hospital will receive points for attesting that the facility has an implemented Glycemic Control Process Improvement Plan (PIP) for all non-critically ill patients,
excluding newborns, by September 30, 2013 – 10 points
• Hospital will receive points for reporting the results of the above components of the Glycemic Control PIP by September 30, 2013, for the time period between
July 2012 through June 2013 – 5 points
5 of 6
Patient Experience Performance – 80 Points Possible*
Hospital performs at or above the national average based on HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) questions.
• Overall patient rating of hospital – 20 points
• If a patient would recommend the hospital – 20 points
• Any of the remaining eight domains – 40 points possible (10 points per question)
CMS Core Measure Performance – 60 Points Possible*
CMS now requires the reporting of hospital process of care measures, which include: heart attack care, heart failure care, pneumonia care and prevention of surgical
infection. Hospitals will receive points based on CMS Core Measure results based on the September 2013 data release for the time period of January through
December 2012.
Your hospital’s score will be based on a performance average. To calculate your performance average, one point will be awarded for every measure that exceeds a score
of 95%. For example: Your facility submits 20 measures to CMS. An example of the calculation:
6 (# of measures≥95% )
20 (# of measures submitted)
• Performance Average = 70% or greater - 60 points
• Performance Average = 60 - 69% – 50 points
• Performance Average = 50 - 59% – 40 points
= 30% (Performance Average)
• Performance Average = 40 - 49% – 30 points
• Performance Average = Less than 40% – 0 points
Quality Outcomes and Infection Reduction Performance – 100 Points Possible
This measure allows for recognition of hospitals in the state that are outperforming the national rate on CMS outcome-related measures. CMS released risk-adjusted
measures that illustrate hospital mortality performance in relation to the U.S. National Rate. These measures are revised on an annual basis using a three-year time
period. The next release is in July 2013 and will contain data from July 2008 through June 2011. Top performers are defined on these CMS outcome-related measures.
• Hospital outperforms the U.S. National Rate on any of the three CMS outcome mortality measures (Heart Failure, Pneumonia and Acute Myocardial Infection) –
60 points possible (20 points per measure)
• Recognition as a Blue Distinction Center or Blue Distinction Center+ – 20 points
New
• Hospital has obtained “Excellent” status through AHQI benchmarking or a CMS CLABSI SIR (Standardized Infection Ratio) rate of “Better” than the
U.S. National Benchmark – 20 points OR
• Hospital has obtained “Good” status through AHQI benchmarking or a CMS CLABSI SIR rate of “No Different Than” the U.S. National Benchmark – 10 points OR
• For hospitals that are unable to qualify for a CLABSI SIR rate due to lack of volume, achievement of a zero (“0”) CLABSI rate during evaluation period - 10 points.
* Rescore can be requested in subsequent quarter.
Note: Blue Distinction® Centers met overall quality measures for patient safety and outcomes, developed with input from the medical community. Blue Distinction® Centers+ also met cost measures that address consumers’ need for affordable healthcare. Individual
outcomes may vary. National criteria is displayed on www.bcbs.com. A local Blue Plan may require additional criteria for facilities located in its own service area. To find out which services and providers (including hospital-based physicians) are covered under your policy,
or to learn about local Blue Plan criteria, contact your local Blue Plan; and contact your provider before making an appointment to verify its current Network and Blue Distinction Centers status. Each hospital’s Cost Index is calculated separately, based on data from its
local Blue Plan. Hospitals in portions of CA, ID, NY, PA, and WA may lie in areas served by two local Blue Plans, resulting in two Cost Index figures; and their own local Blue Plans decide whether all hospitals in these areas must meet Blue Distinction Centers+ national
criteria for one or both Cost Index figures. Neither the Blue Cross and Blue Shield Association nor any Blue Plans are responsible for damages, losses, or non-covered charges resulting from Blue Distinction or other provider finder information or care received from Blue
Distinction or other providers. To find out more, contact your local Blue Plan.
6 of 6