Dissection 30
advertisement

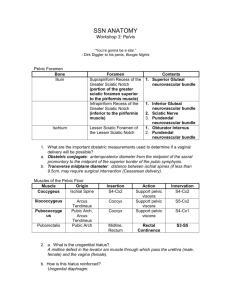
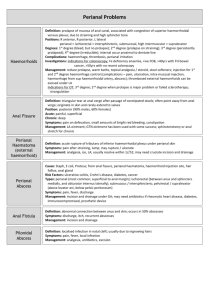
DISSECTION 30 The Perineum, Anal Triangle References: M1 402-406, 409-418, 453-459, 461-464, 567; N 340-346, 359-361, 363, 365-369, 376, 384-385, 391, 393, 477, 484-485; N352-359, 377-380, 382-386, 395, 404-405, 411, 413, 495, 502-503; R 338-341, 350-354 AT THE END OF THIS LABORATORY PERIOD YOU WILL BE RESPONSIBLE FOR THE IDENTIFICATION AND DEMONSTRATION OF THE STRUCTURES LISTED BELOW: 1. Bones and related features: symphysis pubis, inferior pubic ramus, ischial ramus, ischial tuberosity, ischial spine. 2. Features of external genitalia: scrotum and scrotal raphe, prepuce, frenulum, glans, body, external urethral orifice, perineal raphe, mons pubis, labium majus, anterior and posterior labial commissures, body of penis, body of clitoris, labium minus, vaginal vestibule, vaginal orifice. 3. Fasciae and spaces of the perineum: ischiorectal (ischioanal) fossa and its anterior recess, central tendon of the perineum. 4. Muscles: levator ani, gluteus maximus, external anal sphincter, obturator internus, piriformis. 5. Nerves: pudendal, posterior femoral cutaneous and its perineal branch, inferior rectal. 6. Vessels: internal pudendal, inferior rectal artery and vein. 7. Ligaments: sacrotuberous, sacrospinous. YOU SHOULD ALSO BE ABLE TO DO THE FOLLOWING THINGS: 1. Give the bony landmarks which delineate the perineum and divide it into anal and urogenital triangles. 2. Demonstrate on the cadaver the boundaries of the ischiorectal (ischioanal) fossa including its anterior and posterior recesses. 3. Identify on the cadaver the nerves and arteries passing through the ischiorectal fossa and passing in its walls. 4. Discuss the arterial supply and venous drainage of the rectum and anal canal. 5. Distinguish between internal and external hemorrhoids. Although the term perineum has two meanings, an anatomical and a clinical, it will be used here in the anatomical sense to mean the region external to the inferior pelvic outlet. This region is bounded by the arch and inferior rami of the pubic bones, the tuberosities of the ischia, medial borders of the gluteus maximus muscles, and the tip of the coccyx. Superiorly, it is bounded by the pelvic diaphragm and inferiorly by the skin between the thighs and buttocks. A line drawn transversely from one ischial tuberosity to the other divides the region arbitrarily into an anterior, urogenital triangle, and a posterior, anal triangle. The anal triangle is similar in the two sexes, but the urogenital triangle is different by reason of the associated Dissection 30, Perineum, Anal Triangle urogenital organs (G3.42; N363; N380). Before beginning the dissection of the perineum, identify the following features of surface anatomy: Male (N 365, 369; N382, 386) PENIS PREPUCE and its FRENULUM GLANS Page 2 Remove the skin from the perineum. In the male incise the skin in the midline along the scrotal raphe, and bluntly separate the right and left portions of the scrotum. An incision should encircle the anus to leave it in situ, with the vulvar region similarly treated in the female. Complete removal of the skin avoids bothersome flaps in this restricted area (G3.44, 54; N344, 346; N357, 359; A344, 346, 370). Since the anal triangle will be dissected first, it is well to finish the skin removal with the cadaver in the prone position. BODY EXTERNAL URETHRAL ORIFICE SCROTUM and SCROTAL RAPHE Female (N359; N377) MONS PUBIS LABIUM MAJUS (PLURAL, LABIA MAJORA) LABIAL COMMISSURES, ANTERIOR and POSTERIOR CLITORIS PREPUCE and its FRENULUM GLANS To better view important neurovascular structures entering the region of the anal triangle, begin with a superficial exposure of the gluteal region. Remove any remaining skin and tela subcutanea of the buttock laterally to the midaxillary line and inferiorly to include the skin of the upper thigh. In these regions the tela subcutanea can be reflected effectively only by sharp dissection. Cutaneous nerves need not be retained but be aware of them and note from atlas illustrations their wide origin -- superior cluneal nerves (posterior primary rami (L1, L2, L3), middle cluneal nerves (posterior primary rami S1, S2, S3) and inferior cluneal nerves (anterior primary rami S1, S2, S3) from the POSTERIOR FEMORAL CUTANEOUS NERVE. Find and preserve the POSTERIOR BODY LABIUM MINUS (PLURAL, LABIA MINORA) EXTERNAL URETHRAL ORIFICE VAGINAL VESTIBULE VAGINAL ORIFICE Male and Female (N 340-342; N352-354) FEMORAL CUTANEOUS NERVE (A426; G5.3B; N476, 477, 522; N494, 495, 540). It emerges from beneath the gluteal fold deep to the fascia lata (the deep muscle fascia of the thigh), which must be split to expose the nerve. The PERINEAL BRANCH of the POSTERIOR FEMORAL CUTANEOUS NERVE (N393; 485, N413, N503) contributes to the innervation of the cutaneous area of the perineum and is in a fascial plane that must be taken into account by gynecologists in effective anesthesia of this area. SYMPHYSIS PUBIS INFERIOR PUBIC RAMUS ISCHIAL RAMUS ISCHIAL TUBEROSITY PERINEAL RAPHE Complete the removal of fascia from the GLUTEUS MAXIMUS. Free its upper margin and transect the muscle through its middle at right angles to the direction of its fibers. Be careful not to damage the SACROTUBEROUS LIGAMENT (G5.15; N477, 485; N495, 503; A427). By blunt dissection reflect the muscle and separate it from Dissection 30, Perineum, Anal Triangle the gluteus medius. Use your scalpel to reflect the gluteus maximus from the surface of the sacrotuberous ligament (G5.24, 25; N477; N495; A430). Gluteal arteries and nerves entering the deep surface of the muscle may be detached and identified in detail in a later dissection. Identify the PIRIFORMIS MUSCLE, inferior to which many structures (including the large sciatic nerve) enter the gluteal region. Deep to the sacrotuberous ligament, locate the ISCHIAL SPINE and SACROSPINOUS LIGAMENT. Identify the PUDENDAL NERVE and INTERNAL PUDENDAL ARTERY where they cross the sacrospinous ligament (G5.25; N485; N503; A430). The pudendal nerve usually is located medial to the internal pudendal vessels. Start the dissection of the anal triangle by removing the fat of the superficial fascia from the ISCHIORECTAL (ISCHIOANAL) FOSSA (N344, 346; N357, 359). These fossae are bilateral spaces separated medially by the anus and lower end of the rectum, and by the anococcygeal raphe. Extend your removal of fat anteriorly to demonstrate a blind prolongation of the ischiorectal fossa superior to the urogenital diaphragm known as the ANTERIOR RECESS. Other boundaries are: superomedially, the LEVATOR ANI MUSCLE and its inferior fascial layer; posterolaterally, the GLUTEUS MAXIMUS MUSCLE; anteriorly, the body of the pubis; laterally, the obturator internus. As the fat is removed, watch for the INFERIOR RECTAL VESSELS and NERVES (N391, 393; N411, 413). When found, trace them to their site of emergence Page 3 from the lateral wall of the fossa, where they arise from larger, pudendal structures which traverse the pudendal (Alcock's) canal in the fascia of the OBTURATOR INTERNUS MUSCLE. Open the fascia of the pudendal canal and follow the pudendal nerve and internal pudendal vessels posteriorly to their emergence from deep to the sacrotuberous ligament. The pudendal canal ends anteriorly at the posterior border of the urogenital diaphragm and the PUDENDAL NERVE and INTERNAL PUDENDAL VESSELS pierce the fascia and enter the urogenital diaphragm. As they do so they give rise to superficial nerves and arteries to the perineum, named perineal nerves and arteries and posterior scrotal (or labial) nerves and arteries. Initially they are in the superficial perineal space between the superficial perineal fascia and the inferior fascia of the urogenital diaphragm. These fascial layers will be clarified in the next dissection of the urogenital triangle. Identify the EXTERNAL ANAL SPHINCTER (G3.46, 55; N344, 346; N357, 359; A344, 346, 370-371), a muscle that surrounds the anus at a subcutaneous level, and trace its posterior attachment to the coccyx. Note that its anterior attachment blends with a fibrous mass, called the CENTRAL TENDON OF THE PERINEUM or "perineal body". (The obstetrical definition of the term perineum is restricted to this structure.) Examine the thickened part of the smooth muscle that surrounds the inferior 2.5 cm of the anal canal, and which is in contact with the external sphincter. This band of muscle is the internal anal sphincter. This may be seen more clearly when the pelvis is split in dissection 33. ______________________________________________________________________________________________ STUDY QUESTIONS 1. What are the boundaries of the perineum? 1. The boundaries of the perineum are: 1) the symphysis pubis, 2) the inferior pubic rami, 3) the ischial rami, 4) the ischial tuberosities, 5) the sacrotuberous ligaments, and 6) the coccyx. Dissection 30, Perineum, Anal Triangle Page 4 2. What kind of muscle is the external anal sphincter skeletal or smooth? 2. It is skeletal muscle. 3. How is the external anal sphincter innervated? 3. It is innervated by the perineal branch of the fourth sacral nerve and by the inferior rectal nerves. The cell bodies of the motoneurons which supply it are located in the ventral gray column of the mid sacral spinal cord, especially S4. 4. From what artery does the inferior rectal artery arise? 4. Internal pudendal artery. 5. What other arteries supply the rectum? 5. The middle and superior rectal arteries. 6. What is the venous drainage of the rectum? 6. The venous drainage follows the arteries. A plexus of veins surrounds the rectum and drains chiefly into the superior rectal vein, which is a tributary to the inferior mesenteric vein. The paired middle and inferior rectal veins drain into the internal iliac veins. 7. What are hemorrhoids? 7 Hemorrhoids are varicose dilations of veins in the rectal submucosal venous plexus. Distinguish between internal and external hemorrhoids. Internal hemorrhoids lie above the pectinate line and drain into the superior rectal vein. External hemorrhoids are below the pectinate line and drain into the inferior rectal veins. 8. What are the boundaries of the ischiorectal (ischioanal) fossa? 8 Medially--levator ani Laterally--obturator internus Posteriorly--gluteus maximus and sacrotuberous ligament Inferiorly--urogenital diaphragm and skin 9. How far anteriorly does the anterior recess of the ischiorectal (ischioanal) fossa reach? 9. To the body of the pubis. 10. What is the pudendal canal? 10. A passageway for the internal pudendal artery and vein and the pudendal nerve in the obturator internus fascia on the lateral wall of the ischiorectal fossa (spine to tuberosity of ischium). Dissection 30, Perineum, Anal Triangle Page 5 11. Describe the course of the pudendal nerve and internal pudendal artery proximal to the pudendal canal. 11. The pudendal nerve and internal pudendal artery exit the pelvis and enter the gluteal region through the greater sciatic foramen inferior to the piriformis. They exit the gluteal region and enter the perineum by passing through the lesser sciatic foramen. In this course they pass superficial to the sacrospinous ligament and deep to the sacrotuberous ligament. 12. Consider some of the structures that could be damaged by an incision to drain an abscess in the ischiorectal fossa. 12. 13. What does the inferior rectal nerve supply? 13. External anal sphincter muscle and skin adjacent to anus. 14. What nerve supplies the levator ani? 14. Nerve to the levator ani on its superior surface direct from the sacral plexus (chiefly S4). 15. What nerves supply the scrotum? 15. Anterior scrotal nerves from the ilioinguinal nerve, posterior scrotal from the pudendal nerve; genital branch of genitofemoral supplies the cremaster muscle as well as the skin, and laterally the perineal branch of the posterior femoral cutaneous. 16. Do the two ischiorectal (ischioanal) fossae communicate? 16. Yes. The two fossae communicate with each other posterior to the anal canal above a part of the external anal sphincter that extends backward to attach to the coccyx. Here an abscess in one ischiorectal fossa may extend across to the other fossa. (M1 416 and H793-794). LJ:bh revised 06/19/09