baby: hisa yoshi osa wa/getty ima ges
advertisement

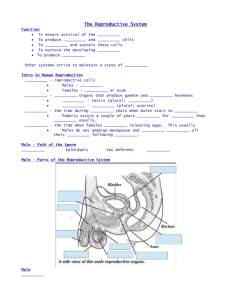
21 How babies might be made: Create eggs from stem cells // add sperm // place favorite embryo into uterus // pass the next nine months debating ethical issues Hard to Conceive by anita slomski // baby: hisayoshi osawa/getty images O n December 28, 1981, two days before his 71st birthday, gynecologic surgeon Howard Jones wrote a news release he hoped he wouldn’t have to use. The first baby created by in vitro fertilization in the United States was scheduled to be born by caesarean section that morning, and Jones and his wife, reproductive endocrinologist Georgeanne Jones, feared that the small size of the baby’s head meant a tragic defect had occurred, possibly as a result of the IVF procedure they had performed on schoolteacher Judy Carr, whose three ectopic pregnancies had destroyed her fallopian tubes. Jones left a blank space in the release for whatever anomaly had doomed the child. More than 15 years earlier, Jones had collaborated with British physiologist Robert Edwards from the University of Cambridge in England to fertilize a human egg in a cell culture dish. Then, in 1980, Jones founded the first IVF clinic in the United States at Eastern Virginia Medical School in Norfolk. But the work was controversial, with Jones and his wife under constant attack for what critics described as their unethical, morally indefensible medical experimentation. No less a luminary than Nobel Prize winner James Watson, who with Francis Crick had discovered the structure of DNA, told Edwards and Jones in 1971 that infanticide was a likely outcome of IVF. “What are we going to do with the mistakes?” Watson asked. But Elizabeth Jordan Carr, born at 7:46 a.m. that December day, was perfectly healthy, and in 2010, Robert Edwards, with whom Jones had collaborated, would be awarded the Nobel Prize in Physiology or Medicine for developing IVF. Jones, now 101, believes the recognition would have come sooner save for religious opposition. Of Edwards, who died in April, Jones notes that “the world has lost a true pioneer.” And even though assisted reproductive technologies have resulted in more than five million births since 1978, challenges to their legitimacy continue. In Personhood Revisited: Reproductive Technology, Bioethics, Religion and the Law, published late last year, Jones takes on opponents who want to pass laws asserting that personhood begins with fertilization—a major threat to IVF, he says. Yet ongoing debate about IVF and other assisted reproductive technologies hasn’t kept science from further expanding the boundaries of human reproduction. Last year, two major scientific studies raised the possibility that women whose egg supply has dwindled because of age or exposure to agents that damage egg cells may one day be able to use their own stem cells to revitalize their ovaries with new eggs. That could reduce the need for IVF, and some researchers envision a time in which a woman might freeze sufficient numbers of primitive egg cells to become pregnant whenever she wants. Meanwhile, scientists have for the first time sequenced the entire genome of a fetus. The combination of having an unlimited supply of eggs and the ability to manipulate genes in utero could someday enable a couple to choose from among dozens or even hundreds of their own embryos to create a healthy, genetically desirable child. The ethical issues that would pose are only beginning to be Spring 13 // protomag.com 22 explored. Of more immediate concern is new research from Australia that finds higher rates of birth defects in offspring conceived by assisted reproductive methods. “These technologies have opened doors for countless people who would never have had a chance at pregnancy,” says Thomas Toth, director of the Vincent In Vitro Fertilization Unit at Massachusetts General Hospital. “However, as the field evolves, we’re realizing that we need to perturb nature as little as possible.” W omen, like other female mammals, are born with all of the eggs they’ll ever have, as accepted scientific thinking goes. A fetus in the womb has seven million immature egg cells called oocytes. A genetically controlled process of cell deletion winnows that to one million by the time she’s born and to 200,000 at puberty. By menopause, the supply is virtually exhausted. “We think oocyte death is part of an audition process to ensure that only the best egg ovulates during each cycle,” says Jonathan Tilly, investigator in the Vincent Center for Reproductive Biology at MGH. Typically, only one egg matures when a woman ovulates, and that egg then allows only one sperm to fertilize it. But if pregnancy doesn’t occur naturally, IVF may be called in to help. With IVF, injected hormones spur the production of multiple eggs. Using ultrasound to gauge when the ripening eggs are about to emerge from the ovarian follicles that house them, surgeons use a hollow needle to remove the eggs, which are then combined with sperm in the lab. Usually after a few days, the resulting embryo or embryos are transferred into the uterus, and if all goes well, one (or sometimes more) attaches itself to the uterine wall and a viable pregnancy results. But IVF could be more effective—or might not even be needed—if women could produce new oocytes, and controversial research by Tilly suggests that it might be possible. In 2004, he published a paper asserting that he’d found oocyte precursor cells—stem cells—in mouse ovaries that could change into oocytes. He had suspected that might be the case, he says, because when he counted the number of follicles— the ovarian structures that house oocytes—in mice at various stages during their lives, he realized they were losing far too many follicles too fast to sustain reproduction. That, along with several other experimental observations, convinced him the mice must be making new oocytes. But the scientific community was skeptical. “At least 30 editorials claimed that our interpretations were wrong,” says Tilly. Since that initial paper, however, several other labs around the world have confirmed and extended Tilly’s observations. Last year, Tilly stirred new controversy when he announced in a paper published in Nature Medicine that he had isolated oocyte stem cells in women using the same procedure that helped him discover egg precursor cells in mice. Using fragments of frozen human ovaries from women in Japan who had undergone gender reassignment surgery, Tilly separated the stem cells from the immature oocytes in the ovaries, and when he examined the isolated cells under a microscope, the hair on his arms stood up. “These stem cells have a size and shape like no other,” he says. “They are very small—about 6 to 8 microns in diameter—and they’re perfectly round. These cells also had the specific gene pattern we expected to see. I The Trouble With Older Fathers // As men age, genetic mutations in their sperm multiply, raising risks for their offspring. As science has attempted to accommodate women’s desire to prolong their childbearing years, men have tended to worry much less about the ticking of their biological clocks. But new research from Iceland suggests older men don’t get a free pass. In the largest study to date, whole genome sequencing was performed on 78 nuclear families—father, mother and child—to find genetic mutations that appear only in the child. Spontaneous mutations that occur at the time of conception—known as de novo mutations—are important in natural selection, helping delete the function of genes that may be disadvantageous to the species. But about 10% of de novo mutations are considered protomag.com // Spring 13 harmful, giving offspring a higher risk of autism, schizophrenia and other disorders and diseases. Fathers pass on nearly four times as many de novo mutations as do mothers, and the older the father is, the more mutations the child receives. Because men make approximately 200 million sperm a day, the precursor stem cells that turn into sperm are continually dividing—and creating opportunities for mutations to arise. According to the Icelandic study, the mutation rate doubles with every 16.5 years of age and increases eightfold in 50 years. “One out of 30 people is born with a de novo mutation that results in the loss of the function of a gene,” which is bound to have some impact on that person’s traits, says neurologist Kari Stefansson, chief executive of deCODE Genetics in Reykjavik and an author of the study. Given that half of all human genes affect the brain, coding errors in DNA are particularly likely to contribute to neuropsychiatric disorders such as autism and schizophrenia. Stefansson notes that people with those largely inherited disorders tend to have few children, so logically the diseases should become less and less common. “Yet autism is on the rise today, and the prevalence of schizophrenia has remained the same for the past 100 years,” he says. “There must be a very significant contribution by de novo mutations.” knew right then what I was looking at.” Tilly marked the cells with a fluorescent green protein so he could track them. Then he injected them back into the human ovarian tissue and grafted that tissue into immunocompromised female mice. Within two weeks, he found glowing green oocytes in the grafted tissue—proof, he says, that the human stem cells had differentiated themselves into human oocytes. Tilly’s critics say he has simply found immature egg cells, not stem cells. But Tilly says you only have to watch the cells proliferate in culture dishes to know that they are egg precursor cells, which can make more of themselves, rather than immature egg cells or oocytes that are unable to proliferate. This is because oocytes and sperm undergo a unique process called meiosis, losing half their DNA as they divide. That happens so that when sperm and egg are joined as an embryo, there won’t be twice the normal number of chromosomes. “Not only can you make more of these cells outside the body; if you put them back in the body, at least in mouse studies, they will commit to meiosis and make eggs that fertilize and develop into healthy embryos and offspring,” says Tilly. vladimir godnik/getty images M itinori Saitou, professor of anatomy and cell biology at Kyoto University in Japan, has used a different type of stem cell to create mouse eggs that have produced two generations of mouse pups. Saitou found a new source for eggs in stem cells he obtained from fetal mice and from pluripotent stem cells (primordial cells that can be coaxed to differentiate into specialized cells, such as eggs), also from fetal mice. Using cytokines and growth factors, Saitou programmed the fetal cells to become primordial germ cells that started to differentiate into oocytes in a lab dish. To get the cells to mature and function as oocytes, Saitou mixed them with other fetal ovarian cells to make “reconstituted ovaries,” which he transplanted into immune-deficient adult female mice. After four weeks, Saitou removed the ovaries, isolated the oocytes, fertilized them with mouse sperm and transferred the embryos to surrogate mice, which gave birth to seemingly healthy pups that were also fertile. The research shows that it is possible to create functional eggs using stem cells, but Saitou cautions that we are a long way from producing eggs from an adult woman’s skin cells (a potential source of induced pluripotent stem cells). The stem cells Saitou used were embryonic, and the signaling they required to turn into functional oocytes came from the fetal ovarian tissue into which they were transplanted. That process isn’t possible for human reproduction because it would mean destroying human embryos. “We have to understand what these embryonic stem cells are doing to create germ cells before we can develop a strategy to induce human primordial germ cells,” says Saitou. Tilly, however, says his stem cells are ready for in-depth testing. One of Tilly’s fiercest initial critics—Evelyn Telfer, a reproductive biologist at the University of Edinburgh—is now collaborating with Tilly to coax oocyte stem cells obtained from women undergoing cesarean sections into mature eggs outside the body. If this is possible, the team plans to fertilize them and see whether they’re functional. (Generating human embryos for experimental purposes is illegal in the United States, but it’s permitted in the United Kingdom under tight regulation.) If the research is successful, there could be many applications, Tilly says. Because these oocyte stem cells can proliferate, a snip of ovarian tissue might yield hundreds of cells that could be frozen for later use. A woman whose ovaries have been damaged by chemotherapy, for example, might get an infusion of her own stem cells to restore her egg pool. The stem cells could also make IVF more efficient by generating many more than the six to eight eggs that can usually be retrieved today. With an endless supply of cells to work with, researchers might Spring 13 // protomag.com ”It’s unthinkable that there should be any area of scientific investigation set off limits,” said IVF pioneer Howard Jones in 1971. 24 also add hormones or drugs to discover the right environment for inducing cells to make more eggs in the ovaries. Perhaps the earliest clinical application of this research would be to use stem cells to re-energize old eggs and improve the odds of successful IVF. Older eggs often lack the energy to divide to make a good quality embryo, causing a higher rate of miscarriage and chromosomal abnormalities. In the 1990s, Dutch embryologist Jacques Cohen attempted to rejuvenate old eggs by transferring mitochondria—a cell’s energy source— from the cytoplasm of the egg cells of younger women. That procedure, known as cytoplasmic transfer, led to higher fertilization rates and the birth of 30 children before the Food and Drug Administration banned it in 2001, citing potential danger to offspring that received DNA from two women as well as the father. (Jones says he saw no reason why the procedure should not have been tried.) OvaScience, a public company co-founded by Tilly, has started a clinical trial with women ages 38 to 42 who have failed to conceive after two to five tries with conventional IVF. Their eggs will be injected with mitochondria obtained from their own egg cells, thereby avoiding the problem of foreign DNA from donor eggs. “If you start with better embryos,” says Tilly, “then you may only need to transfer a single embryo back into the patient’s uterus, which would eliminate the risk of multi-gestational births in a single pregnancy.” A lmost a third of pregnancies through assisted reproduction in the United States do indeed result in twins or triplets, and in part because those children are likely to be born prematurely, they have an elevated risk of developmental disorders and other problems. And those aren’t the only potential perils of assisted conception. Last year, an Australian study that analyzed more than 300,000 births from 1986 through 2002 found that the rate of birth defects was higher when conception was achieved with IVF and intracytoplasmic sperm injection (ICSI) than for naturally occurring pregnancies. Compared with a 5.8% rate of birth protomag.com // Spring 13 defects in the general population, women who used assisted reproductive technologies to get pregnant had an 8.3% risk of delivering a baby with problems ranging from holes in the heart to bowel malformation. But how much of that increased risk is attributable to reproductive technologies and how much relates to the characteristics of the women who turn to assisted reproductive techniques? Women seeking fertility assistance tend to be older, heavier and more likely to have hypertension and metabolic disorders such as diabetes and polycystic ovary syndrome, all of which are risk factors for birth defects. Indeed, when researchers for the Australian study factored in such characteristics, they found that IVF added little to the risk of birth defects. Moreover, embryos that were first frozen and then thawed before being inserted into the uterus actually had a belownormal rate of defects. “Developmentally compromised embryos don’t survive the frozen-thawed cycle,” says Michael Davies, associate professor at the University of Adelaide’s School of Paediatrics and Reproductive Health. Freezing embryos also allows IVF to be done after a woman’s body has had time to recover from the drugs she must take to spur ovulation. “After ovulation has been induced, the endometrium is more compromised, so it’s not the ideal circumstance for an embryo to implant and grow properly,” says Davies. “The frozen cycles of IVF seem to produce remarkably healthy embryos.” But the story is different for ICSI, which involves injecting sperm directly into the egg. Davies found that almost 1 in 10 children born using ICSI and nonfrozen embryos had birth defects. That statistic is particularly troubling to Davies because of the technology’s rising popularity. In the past, ICSI was used only when there were problems with sperm that made them unable to penetrate an egg on their own. Now, however, many couples elect to have ICSI instead of IVF because ICSI’s pregnancy rate is a third higher than the rate for IVF, according to Davies. ICSI accounts for 70% of assisted reproduction in Australia. ICSI’s higher risk of birth defects may happen because the procedure bypasses natural selection by fertilizing an egg with a sperm that might not have otherwise had a chance to fertilize an egg in a woman’s body. The DNA damage causing the male infertility that led to the treatment may also be a contributing factor. But Davies acknowledges that the risks associated with assisted conception may have declined since the study’s end in 2002, thanks in part to advances in embryology. erproductions ltd/getty images W hether or not today’s assisted reproductive technologies increase the risk that a child will have problems, there’s a growing perception that, soon enough, parents will be able to create super-healthy kids by genetically screening embryos. The news last year that scientists at the University of Washington and Stanford University School of Medicine sequenced the entire genome of a fetus for the first time only added to such expectations. Yet that vision of the future may not be realistic. “The genetics field is not on a trajectory where you’ll be able to customize your children any way you want,” says Mark Daly, chief of the Analytic and Translational Genetics Unit at MGH. “We cannot prenatally predict diabetes, schizophrenia or autism, which involve hundreds of genes—most of which haven’t been discovered—as well as environmental factors and chance.” And if those problems were solved, there would still be many ethical questions to answer. Suppose that, many decades in the future, a reproductive geneticist could scan computer readouts of the genomes of, say, 100 embryos a couple has produced. The prospective patients might then select one with the smallest susceptibility to a familial disease such as Alzheimer’s or depression, says Ronald Green, director emeritus of the Office of Genome Ethics at the National Human Genome Research Institute. But they might also make choices not just to avoid disease but to make better babies by “improving their genetic endowment,” says Green. Helped by prenatal genetic engineering, children might be born with greater resistance to disease, physical traits parents deem desirable and perhaps even enhanced intelligence. If such genetic tools become available and safe, some parents may be unable to resist the promise of creating disease-free and problem-free offspring. “As long as the demand is there, this technology will be difficult to regulate,” says Green. As assisted reproductive technologies expand around the world at a pace far beyond what Jones envisioned in 1981, the field will continue to inspire ethical and scientific debate. Yet he argues against putting any predetermined constraints on those explorations. “It’s unthinkable that there should be any area of scientific investigation set off limits,” he said in 1971, chiding medical peers for their hostility toward a technology that would give hope to desperate couples wanting a child. That bold approach may continue to shape a young field that has already changed the world. 25 Dossier 1. Pandora’s Baby: How the First Test Tube Babies Sparked the Reproductive Revolution, by Robin Marantz Henig (Houghton Mifflin Co., 2004). Henig tells the story of the physicians who pioneered IVF and how they endured the contempt of scientists who claimed that test-tube babies would launch science down the slippery slope toward genetic engineering and human cloning. 2. “The Next (Re)Generation of Ovarian Biology and Fertility in Women: Is Current Science Tomorrow’s Practice?” by Dori C. Woods and Jonathan L. Tilly, Fertility and Sterility, June 2012. A case for the existence of stem cells in the ovaries of reproductive-age women, a discovery that will bring stem cell–based approaches for treating infertility “one significant step closer to reality,” according to the authors. 3. Babies by Design: The Ethics of Genetic Choice, by Ronald M. Green (Yale University Press, 2007). Green lays out the future capabilities of genomic science in allowing parents to genetically modify their offspring to free them of disease and enhance them with desirable traits—raising ethical questions that should be asked now, he urges. Spring 13 // protomag.com