RBO printed Vol5 No3
advertisement
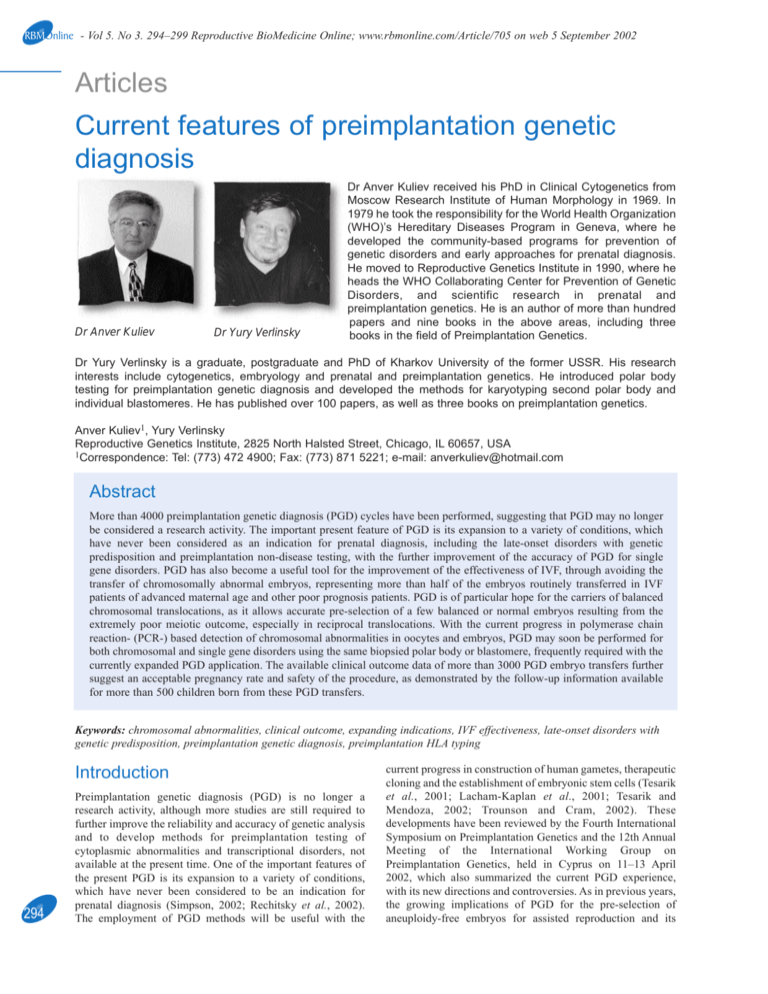
RBMOnline - Vol 5. No 3. 294–299 Reproductive BioMedicine Online; www.rbmonline.com/Article/705 on web 5 September 2002 Articles Current features of preimplantation genetic diagnosis Dr Anver Kuliev Dr Yury Verlinsky Dr Anver Kuliev received his PhD in Clinical Cytogenetics from Moscow Research Institute of Human Morphology in 1969. In 1979 he took the responsibility for the World Health Organization (WHO)’s Hereditary Diseases Program in Geneva, where he developed the community-based programs for prevention of genetic disorders and early approaches for prenatal diagnosis. He moved to Reproductive Genetics Institute in 1990, where he heads the WHO Collaborating Center for Prevention of Genetic Disorders, and scientific research in prenatal and preimplantation genetics. He is an author of more than hundred papers and nine books in the above areas, including three books in the field of Preimplantation Genetics. Dr Yury Verlinsky is a graduate, postgraduate and PhD of Kharkov University of the former USSR. His research interests include cytogenetics, embryology and prenatal and preimplantation genetics. He introduced polar body testing for preimplantation genetic diagnosis and developed the methods for karyotyping second polar body and individual blastomeres. He has published over 100 papers, as well as three books on preimplantation genetics. Anver Kuliev1, Yury Verlinsky Reproductive Genetics Institute, 2825 North Halsted Street, Chicago, IL 60657, USA 1Correspondence: Tel: (773) 472 4900; Fax: (773) 871 5221; e-mail: anverkuliev@hotmail.com Abstract More than 4000 preimplantation genetic diagnosis (PGD) cycles have been performed, suggesting that PGD may no longer be considered a research activity. The important present feature of PGD is its expansion to a variety of conditions, which have never been considered as an indication for prenatal diagnosis, including the late-onset disorders with genetic predisposition and preimplantation non-disease testing, with the further improvement of the accuracy of PGD for single gene disorders. PGD has also become a useful tool for the improvement of the effectiveness of IVF, through avoiding the transfer of chromosomally abnormal embryos, representing more than half of the embryos routinely transferred in IVF patients of advanced maternal age and other poor prognosis patients. PGD is of particular hope for the carriers of balanced chromosomal translocations, as it allows accurate pre-selection of a few balanced or normal embryos resulting from the extremely poor meiotic outcome, especially in reciprocal translocations. With the current progress in polymerase chain reaction- (PCR-) based detection of chromosomal abnormalities in oocytes and embryos, PGD may soon be performed for both chromosomal and single gene disorders using the same biopsied polar body or blastomere, frequently required with the currently expanded PGD application. The available clinical outcome data of more than 3000 PGD embryo transfers further suggest an acceptable pregnancy rate and safety of the procedure, as demonstrated by the follow-up information available for more than 500 children born from these PGD transfers. Keywords: chromosomal abnormalities, clinical outcome, expanding indications, IVF effectiveness, late-onset disorders with genetic predisposition, preimplantation genetic diagnosis, preimplantation HLA typing Introduction 294 Preimplantation genetic diagnosis (PGD) is no longer a research activity, although more studies are still required to further improve the reliability and accuracy of genetic analysis and to develop methods for preimplantation testing of cytoplasmic abnormalities and transcriptional disorders, not available at the present time. One of the important features of the present PGD is its expansion to a variety of conditions, which have never been considered to be an indication for prenatal diagnosis (Simpson, 2002; Rechitsky et al., 2002). The employment of PGD methods will be useful with the current progress in construction of human gametes, therapeutic cloning and the establishment of embryonic stem cells (Tesarik et al., 2001; Lacham-Kaplan et al., 2001; Tesarik and Mendoza, 2002; Trounson and Cram, 2002). These developments have been reviewed by the Fourth International Symposium on Preimplantation Genetics and the 12th Annual Meeting of the International Working Group on Preimplantation Genetics, held in Cyprus on 11–13 April 2002, which also summarized the current PGD experience, with its new directions and controversies. As in previous years, the growing implications of PGD for the pre-selection of aneuploidy-free embryos for assisted reproduction and its Articles - Current features of PGD - A Kuliev, Y Verlinsky wider application for the improvement of the effectiveness of IVF have been reviewed. A special consideration was given to the currently expanding indications for PGD, with the relationship to the ethical and social issues involved. These recent developments are presented below under four major topics: (i) future directions, summarizing the prospects for preimplantation testing of cytoplasmic and transcriptionally relevant abnormalities, the recent developments in micromanipulation techniques and the progress in understanding of the origin of aneuploidies; (ii) expanding indications for PGD; (iii) PGD in assisted reproduction; and (iv) PGD clinical outcomes. Future directions It is well known that the pre-selection of oocytes or embryos with the highest potential to implant and go to term cannot be achieved properly by testing only for nuclear abnormalities, requiring the evaluation of the cytoplasmic maturity of oocytes and embryos. For example, variation in mitochondrial content should affect the functionality of the gametes and embryos. Although significant progress in the analysis of cytoplasmic abnormalities and the evaluation of the cytoplasmic competence of oocytes and embryos has been achieved, no test is presently available to apply in clinical practice (Cohen and Malter, 2002). The same is true of transcriptional patterns of preimplantation development, suggesting similarities of embryonic and cancer cells in a global demethylation of DNA and genetic deprogramming to a proliferative stem cell state (Monk et al., 2002). It is obvious that the genetic expression is highly stage-dependent, so knowledge of the normal expression patterns may allow the performance of preimplantation screening for the expression of a range of imprinted genes, in order to identify the stage-specific expression anomalies. Nuclear abnormalities, the testing for which is currently a routine PGD practice, increase significantly with age, representing one of the major causes of reproductive failures in women of advanced maternal age. However, despite advanced maternal age remaining the only well-documented risk factor for maternal meiotic non-disjunction, the basic mechanisms of the maternal-age effect is still unknown. The alterations in maternal recombination rates in meiosis are the other identified risk factor for chromosome nondisjunction, although measurements of meiotic recombination have been made only indirectly, through the examination of DNA-polymorphism inheritance in families with trisomic livebirths or spontaneous abortions. Direct evidence of the relationship between reduced recombination and non-disjunction has recently been obtained in the analysis of human spermatozoa (Martin et al., 2002). By studying recombination in the pseudo-autosomal region in X and Y chromosomes, the lack of recombination in this region was established, with association to XY nondisjunction and production of aneuploid spermatozoa. The other direct study of meiotic crossovers was performed in human fetal oocytes, by staining for a mismatch-repair protein MLH1 (Tease et al., 2002). As the distribution of foci of this protein at pachytene matches that of chiasmata at metaphase I, representing an excellent marker for recombination, the number and distribution of the MLH1 foci were determined for chromosomes 13, 18, 21 and X. In addition to a sex-specific difference in control of recombination, it was shown that some chromosomes 18 and 21 lacked an MLH1 focus, representing a high risk of nondisjunction in the process of completion of meiosis, while neither chromosome 13 and X lacked this locus in any of the oocytes classified as normal. So the detection of the recombination-deficient oocytes may indicate an increased risk of meiotic chromosome nondisjunction and production of aneuploid ova. One recent development in micromanipulation and nuclear transfer was work on the construction of human gametes. This was attempted for creating both female and male gametes, demonstrating a strong morphological evidence for haploidization (Galat and Verlinsky, 2002; Lacham-Kaplan, 2001; Tesarik et al., 2001; Tesarik and Mendoza, 2002). However, no cytogenetic proof for haploidization has been presented, required also to ensure the normalcy of the resulting gametes, deriving from the somatic cell transfer into the matured oocytes. The nuclear transfer technique, by contrast, has been further used for visualization of blastomere chromosomes in PGD for translocations, demonstrating its clinical usefulness (Verlinsky et al., 2002a). The technique was applied in 52 PGD cycles for translocations, with a clinically acceptable rate of conversion of interphase nuclei of the blastomeres into metaphase. Of a total of 437 blastomeres tested, the technique was successful in 383 (88%), making possible the pre-selection of normal embryos or those with balanced chromosomal complement for transfer in 38 PGD cycles for translocations. A highly reproducible technique is presently available for the derivation of human embryonic stem cells and their directed differentiation into different cell types (Trounson and Pera, 2001; Trounson and Cram, 2002). A success rate in the establishment of human embryonic stem cells is approximately 66%. The directed differentiation of these cells, using factors produced from differentiating or somatic cells, was achieved for the following cell types: ciliated epithelia of the lung, secretary epithelia in the gut-like structures, neuronal cells and muscles, including cardiomyocytes. The aggregates of muscles were shown to beat 45–60 times per minute, evident for 11–21 days after initiation of the co-culture. In addition, a spontaneous differentiation of embryonic stem cells into insulin-producing beta cells was observed (Assady et al., 2001), as well as the production of hematopoietic precursor cells, following a co-culture of embryonic stem cells with a mouse bone marrow cell line (Kaufman et al., 2001). These developments provide an obvious potential for the therapeutic use of embryonic stem cells in clinical practice. Expanding indications for PGD Late onset disorders: Among the recent applications, PGD for inherited predisposition to late-onset disorders included cancer predisposition, presently offered to patients with predisposition to familial adenomatous polyposis, Von Hippel Lindau syndrome, retinoblastoma, Li-Fraumeni syndrome (determined by p53 tumour suppressor gene mutations), neurofibromatosis type I and II and familial posterior fossa brain tumour (Verlinsky et al., 2001a; Rechitsky et al., 2002). For the latter, overall 20 PGD cycles were performed, resulting in the pre-selection and transfer of 40 mutation-free embryos, which yielded five unaffected clinical pregnancies and four 295 Articles - Current features of PGD - A Kuliev, Y Verlinsky healthy children born by the present time. Despite the controversy of PGD use for late-onset disorders, such data demonstrate the usefulness of this approach as the only acceptable option for at-risk couples to avoid the birth of children with an inherited predisposition to cancer and to have a healthy child of their own. Perhaps one of the most unexpected applications of PGD was in the genetic predisposition for Alzheimer’s disease, which is an autosomal dominant familial predisposition to a presenile form of dementia (Verlinsky et al., 2002b). The disease is determined by a nearly completely penetrant autosomal dominant mutation in the amyloid precursor protein gene, for which no treatment is available, despite a possible predictive diagnosis. The results demonstrated the feasibility of PGD for early-onset Alzheimer’s, providing a non-traditional option for patients who may wish to avoid the transmission of the mutant gene predisposing to early Alzheimer’s in their potential children. For some patients, this may be the only reason for undertaking pregnancy, as the pregnancy may be established free from an inherited predisposition to Alzheimer’s from the very onset. HLA typing: Preimplantation human leukocyte antigen (HLA) matching has recently emerged as a tool for the pre-selection of potential donor progeny for bone marrow transplantation (Verlinsky et al., 2001b). Previously, this was applied to a case of Fanconi anaemia, in which the pre-selection and transfer of unaffected embryos with an HLA match with the affected sibling yielded a clinical pregnancy and the birth of a healthy carrier of the Fanconi anaemia gene, whose cord blood was transplanted to the affected sibling, resulting in a successful haemopoietic reconstitution. The method has currently been applied to HLA genotyping in 18 cycles (five for thalassaemia, six for Fanconi anaemia, one for Wiscott-Aldrich syndrome and six for leukaemia) from 11 couples overall, involving the testing of 197 embryos in combination with genetic disease, and to 86 embryos for HLA typing only. This resulted in the pre-selection of 37 (19%) HLA-matched embryos, including 21 (17.5%) in combination with pre-selection of unaffected embryos following mutation testing and 16 (22%) not involving mutation analysis. These HLA-matched embryos have been transferred back to patients, resulting in four clinical pregnancies and the birth of two HLA-matched children, one pending transplantation of the cord blood stem cells to the affected sibling with leukaemia (Verlinsky et al., unpublished data). 296 Dynamic mutations: The application of PGD has further expanded to dynamic mutations, with the largest series of PGD for these disorders performed as previously in the Brussels centre (Sermon, 2002). In addition to myotonic dystrophy, Huntington’s disease, and fragile X syndrome (FRAXA), PGD was performed for spinal and bulbar muscular atrophy and spino-cerebellar ataxia 7. Overall, 161 PGD cycles were performed for 72 patients, resulting in the transfer of unaffected embryos in approximately 85% of cycles and 20% clinical pregnancies per transfer. The majority of these cases was done for myotonic dystrophy and Huntington’s disease, including 94 cycles for myotonic dystrophy and 44 for Huntington’s disease, resulting in 80 and 38 transfers, and 18 and 7 clinical pregnancies, respectively. The accuracy of PGD has been further improved in this work with the application of fluorescence PCR (FL-PCR) with the expand long template (ELT) kit, which enabled the reduction of the allele dropout (ADO) rate from approximately 30% in both conventional PCR and FL-PCR to as low as 5% in the testing for myotonic dystrophy. The other attractive approach for improving the accuracy of PCR analysis in single cells involved the application of real-time PCR, which was found to reduce the ADO rate by half, compared with conventional PCR or FLPCR (Rechitsky et al., 2002). The application of these approaches, together with the simultaneous testing for the causative mutation and at least one or two linked markers, may avoid the risk of misdiagnosis completely in PGD for single gene disorders. PCR-based testing for chromosomal disorders: With the expanding PGD application, it is becoming current practice to test for single gene disorders together with chromosomal abnormalities, such as in cases of advanced maternal age or chromosomal translocations. So, ideally, the same single cell should be utilized for testing both genetic and chromosomal disorders. As previously demonstrated, one of the possible approaches for PCR-based testing for chromosomal aneuploidies is DNA fingerprinting, which is based on the patterns of alleles that uniquely identify an individual, relying on a multiplex FL-PCR of low template DNA. Using tetranucleotide microsatellite markers with a high heterozygosity index and broad allelic size distribution, the single cell DNA fingerprinting systems have been developed for detection of aneuploidies for chromosomes 13, 18 and 21, which showed 93% reliability, 94% accuracy, 6% ADO rate and 10% preferential amplification rate (Katz et al., 2002). This system has been applied for a combined testing of Down’s syndrome and cystic fibrosis in single cells. Further progress has been achieved in the development of comparative genome hybridization (CGH), which is another feasible PCR-based method for the testing of chromosomal abnormalities in a single cell. This method may enable the detection and exclusion from transfer of the aneuploid embryos, of which a sizable proportion could be misdiagnosed as normal by the commercially available five-colour probe (Wilton et al., 2001). The previously reported limitations of the CGH protocol, involving a 3-day duration of the procedure incompatible with the current laboratory framework for PGD, has presently been overcome either by performing the polar body CGH, or by accelerating the procedure to be completed in 38 h. The first practical application of CGH using the first polar body was attempted in a 40-year-old IVF patient and resulted in the detection of a single aneuploidy-free oocyte from the 10 available for testing. The transfer of the embryo resulting from this oocyte, however, yielded no clinical pregnancy (Wells et al., 2002). The follow-up fluorescence insitu hybridization (FISH) analysis of all the remaining embryos resulting from the nine aneuploid oocytes has confirmed a CGH-based diagnosis at day 3, suggesting that the procedure may be applied in clinical practice. Acceleration of the CGH procedure to be applied to blastomere biopsy was also achieved, using a specific protocol for the degenerate oligonucleotide primed-polymerase chain reaction CGH (DOP-PCR-CGH), applying different Taq polymerase and labelling methods (Ozen et al., 2002). In addition to shortening the procedure, this also yielded a three-fold greater DOP-PCR product. In the meantime, the standard CGH protocol, which takes 5 days to complete, has presently been applied in 20 Articles - Current features of PGD - A Kuliev, Y Verlinsky frozen cycles for poor prognosis IVF patients, resulting in the pre-selection and transfer of 19 aneuploidy-free embryos in 13 cycles, which yielded three unaffected clinical pregnancies (Wilton et al., 2002). For the first time, CGH was also performed for testing structural chromosomal rearrangements in single blastomeres, obtained from spare embryos that were diagnosed unbalanced [t(6;7)(p25;q11.2); t(10;11)(p11.2;q23.3); t(9;13)(q12;p13); and t(10;11)(q12;p13)] and therefore unsuitable for transfer (Malmgren et al., 2002). A total of 94 blastomeres from 28 human embryos have been analysed, confirming the diagnosis of the unbalanced translocations performed by FISH analysis. In addition, a high degree of numerical aberrations was found, including monosomies and trisomies for whole chromosomes or their parts. It is interesting that almost all the embryos appeared to be mosaic, containing more than one chromosomally distinct cell line, or even chaotic with different chromosomal contents in each blastomere. PGD in assisted reproduction As already mentioned, the most universal application of PGD has been the pre-selection of aneuploidy-free embryos for IVF patients of advanced maternal age (International Working Group on Preimplantation Genetics, 2001). The usefulness of PGD in assisted reproduction is obvious from the data on the prevalence of nuclear abnormalities in the oocytes of women of 35 years and older, which is further confirmed to be over 50% even by testing of only five chromosomes (chromosomes 13, 16, 18, 21 and 22) (Kuliev et al., 2002). These data are based on the FISH analysis of 6733 oocytes, obtained in 1297 PGD cycles performed in IVF patients of average age 38.5 years. A total of 3509 (52%) aneuploid oocytes was detected, originating comparably from the first and second meiotic divisions. Overall, 41.8% oocytes had errors in meiosis I, 30.7% errors in meiosis II, and 27.6% both meiotic division errors. In a total of 45.1% of the abnormal oocytes with complex errors, the same chromosome in both meiotic divisions was involved in 21.5% of cases, while different chromosomes were observed in 78.5% of oocytes. Of 3224 detected aneuploidy-free zygotes, 2587 were transferred in 1100 treatment cycles (2.35 embryos per transfer), resulting in 241 (21.9%) clinical pregnancies and 176 healthy children born, suggesting a positive clinical outcome following aneuploidy testing of oocytes in a group of IVF patients of average age 38.5 years. The above overall rates of nuclear abnormalities in oocytes are comparable to those detected in preimplantation embryos in PGD for aneuploidies at the cleavage stage, taking into consideration additional fertilization-related abnormalities and paternally-derived meiotic errors, which could also have been detected at this stage. In approximately the same number of PGD cycles performed for aneuploidy at the cleavage stage by the Saint Barnabas and SISMeR centres, the proportion of embryos with chromosomal abnormalities was as high as 60% (Munné, 2002; Gianaroli et al., 1999, 2002a). However, the types of anomalies in oocytes and embryos were significantly different, which is mainly attributable to a high frequency of mosaicism, comprising approximately half the chromosomal abnormalities at the cleavage stage. Although the origin of a high rate of mosaicism is still unclear, preliminary data indicate that the mosaicism may be of different nature. Some mosaic types are increased with maternal age (Munné et al., 2002b), while others are possibly attributable to the immaturity of the centrosome structures in spermatozoa, which may be the case in testicular sperm extraction (TESE) patients (Silber et al., 2002). It could be that a significant proportion of mosaic embryos originates from the oocytes that are aneuploid from the outset, through a process similar to that known as aneuploidy ‘rescue’. A possible high rate of further mitotic errors in cleaving embryos deriving from the oocytes with the complex aneuploidies may also explain a phenomenon of chaotic embryos, which make up almost half the embryos with mosaicism. The overall experience of using PGD for chromosomal disorders presently exceeds 3000 cases, confirming the positive impact on clinical outcome (Munné et al., 1999; Gianaroli et al., 1999), although there is a need to further quantify its impact in randomized controlled studies, which are currently in progress. Preliminary data from these studies confirm a previously suggested positive impact on implantation rate, which was found to double as a result of the pre-selection of chromosomally normal embryos for transfer (Gianaroli et al., 2002a; Staessen et al., 2002). It is obvious, however, that the improvement of the outcome of PGD may be expected only when the number of embryos biopsied is equal to or higher than the number of embryos expected to be replaced without PGD (Munné et al., 2002c). A clinical impact of aneuploidy testing, in terms of improved pregnancy and implantation rates, as well the improved outcome of pregnancies through the reduction of spontaneous abortions, has been further confirmed not only for IVF patients with advanced maternal age, but also for other poor prognosis patients, including those with repeated IVF failures, repeated spontaneous abortions and altered karyotypes (Gianaroli et al., 2002a). The latter group includes the carriers of balanced translocations, who have an extremely poor chance of having an unaffected pregnancy. It is therefore not surprising that PGD appeared to be highly efficient in assisting these couples to have an unaffected pregnancy and to deliver a child free of unbalanced translocation. More than 400 clinical cycles have been performed at the present time, resulting in at least 100 clinical pregnancies and births of unaffected children. The data are in agreement with previous reports, suggesting a considerable reduction of spontaneous abortion rate in PGD patients with balanced translocations (Munné et al., 2000a; Munné, 2002; Verlinsky et al., 2002a). Clinical outcome of PGD Data on clinical outcome are presently available from the single largest series of 1416 PGD embryo transfer cycles performed in the Chicago centre (Verlinsky et al., 2002a; Kuliev et al., 2002; Ginsberg et al., 2002) and from a sample of 1670 PGD transfer cycles collected from 25 different centres (ESHRE Preimplantation Genetic Diagnosis Consortium, 2002). These transfers resulted in 338 (23.9%) and 309 (18.5%) clinical pregnancies, respectively, and the birth of 539 unaffected children overall (260 and 269, respectively), with multiple pregnancies in approximately onethird of the cases. The overall congenital malformation rate was 5.4% and 6.6%, respectively, which is not different from 297 Articles - Current features of PGD - A Kuliev, Y Verlinsky population prevalence, of which only 2.25% and 3.9%, respectively, were attributable to the major abnormalities. Overall, more than 4000 PGD cycles has presently been performed, with further wider application not only in the USA and Western Europe, but also in the Eastern Mediterranean and Asian countries. For example, a network of six PGD centres has recently been established in China and has already performed 79 PGD cycles for different indications, resulting in 18 clinical pregnancies and the birth of 12 healthy children (Zhuang, 2002). Also, increasingly PGD is being performed for conditions that have never been subject to traditional prenatal diagnosis, such as preimplantation gender determination for social reasons, performed recently in India (Malpani et al., 2001) and Jordan (Kilani and Haj Hassan, 2002). However, the majority of PGD cycles are still performed for chromosomal disorders, with the ratio of PGD cycles for chromosomal and single gene disorders approximately 3:1, the latter group presently including lateonset disorders with genetic predisposition, the proportion of which is gradually increasing. More than 1000 PGD cycles have currently been performed for single gene disorders, with the outcome data available for more than 200 clinical pregnancies and births suggesting the acceptable accuracy of PGD, which may be further improved by the above-mentioned new developments in DNA analysis of single cells. In PGD for chromosomal disorders, the indications are also expanding, with further obvious interest in PGD for translocations because of a strong impact of PGD on reducing the spontaneous abortion rate in the carriers of balanced translocations. Almost half these cycles has been performed by the St Barnabas and Chicago centres (Fisher et al., 2002; Verlinsky et al., 2002a), with an increasing number of other centres, such as the Brussels (Van Assche et al., 2002), SISMeR (Gianaroli et al., 2002b), London (Braude, 2002) and Seoul (Lim et al., 2002) centres, performing a few dozen PGD cycles for translocations. The available results demonstrate a clear advantage of PGD over traditional prenatal diagnosis for translocations, attributable to a poor meiotic outcome, particularly in reciprocal translocations. As mentioned, the accuracy of PGD for translocations has recently been improved by the introduction of blastomere nucleus conversion to metaphase, which will allow a reliable testing for any complex chromosomal rearrangement. It is also true that the testing for translocations has to be considered in combination with aneuploidy analysis, even for the chromosomes not involved in the structural rearrangement, as there is presently evidence for considering chromosomal translocations as a risk factor for aneuploidy. This may in future be performed by PCR-based methods, which will soon provide the opportunity for simultaneous testing for single gene disorders, translocations and aneuploidies in the same biopsied cell. embryos to only two, and even to only one in blastocyst transfer, in an attempt to avoid complications due to multiple pregnancies, the pre-selection of the chromosomally normal embryos will soon become standard IVF practice; there is no way of deliberately transferring untested embryos, more than 50% of which are aneuploid, definitely compromising the outcome of IVF in a traditional setting. In the meantime, information on the availability of such options should be provided at least to poor prognosis IVF patients, so they can have the opportunity of improving their chances of becoming pregnant and avoiding the establishment of a pregnancy destined to be lost due to chromosomal aneuploidy. The clinical outcome is presently available in approximately 700 clinical pregnancies resulting from PGD for aneuploidies, supporting the above-mentioned observations on the positive impact of PGD on implantation and pregnancy rates and the improvement of pregnancy outcomes. In conclusion, PGD has become a practical tool for assisted reproduction and genetic services, providing an important option for couples with genetic risk to avoid the birth of an affected child and have a healthy child of their own. In addition, the application of the technique has been extended to non-disease testing, such as gender determination for social reasons and the pre-selection of HLA-compatible donor progeny. Although preimplantation testing was never intended to be applied without genetic diagnosis, the fact that thousands of individuals in need of haemopoietic stem cell transplantation still fail to find an HLA-matched donor for years, with many of them dying before they can find a match, led to the application of preimplantation HLA matching as a primary indication. This is highly relevant for those couples that have an affected child with bone marrow diseases and cancers, requiring cord blood or bone marrow transplantation. The strategy would clearly not be clinically acceptable through traditional prenatal diagnosis because of a possible clinical pregnancy termination after HLA matching. But these couples can now initiate an HLA-matched pregnancy from the outset with the intention of treating their existing child for whom no other treatment is available. Despite the need for further ethical considerations, preimplantation non-disease testing is clearly an important option for couples with an affected child in need of an HLA-matched bone marrow transplantation. This is obvious from the current increase of the acceptance of nondisease preimplantation testing by couples who are not at genetic risk but who would like to combine their planning for the next child with pre-selection of HLA-compatible progeny to be able to treat their affected child in need of transplantation therapy. These future applications will require a careful ethical consideration (Edwards, 2002). The next (Fifth) International Symposium on Preimplantation Genetics will be held in Antalya, Turkey, on June 5–7, 2003. References 298 Finally, there is further evidence to support the clinical usefulness of PGD for assisted reproduction, as more than half the preimplantation embryos are chromosomally abnormal from the outset and have to be excluded from transfer in IVF patients of advanced maternal age. It is evident that the further improvement of IVF efficiency will be unrealistic without the pre-selection of aneuploidy-free oocytes and embryos. With the current tendency for limiting the number of transferred Assady S, Maor G, Amit M et al. 2001 Insulin production by human embryonic stem cells. Diabetes 50, 1691–1696. Braude P 2002 Strategies and outcomes of the first 100 cycles of PGD for serious familial genetic conditions. Reproductive BioMedicine Online 4 (suppl. 2), 37 (abstr.). Cohen J, Malter H 2002 Cytoplasmic abnormalities. Reproductive BioMedicine Online 4 (suppl. 2), 11 (abstr.). Edwards R 2002 Social and ethical issues on PGD, cloning and gene Articles - Current features of PGD - A Kuliev, Y Verlinsky therapy. Reproductive BioMedicine Online 4 (suppl. 2), 36–37 (abstr.). ESHRE Preimplantation Genetic Diagnosis Consortium. 2002 Data collection III, May 2002. Human Reproduction 17, 233–246. Fisher J, Escudero T, Chen S et al. 2002 Obstetric outcome of 100 cycles of PGD of translocations and other structural abnormalities. Reproductive BioMedicine Online 4 (suppl. 2), 26 (abstr.). Galat V, Verlinsky Y 2002 Haploidization of somatic cell nuclei by cytoplasm of human oocytes. Reproductive BioMedicine Online 4 (suppl. 2), 48–49 (abstr.). Gianaroli L, Magli MC, Ferraretti AP, Munné S 1999 Preimplantation diagnosis for aneuploidies in patients undergoing in vitro fertilization with poor prognosis: identification of the categories for which it should be proposed. Fertility and Sterility 72, 837–844. Gianaroli L, Magli MC, Ferraretti AP 2002a Preimplantation genetic diagnosis for IVF patients with a poor prognosis. Reproductive BioMedicine Online 4 (suppl. 2), 25 (abstr.). Gianaroli L, Magli MC, Ferraretti AP et al. 2002b Robertsonian and reciprocal translocations. Reproductive BioMedicine Online 4 (suppl. 2), 26–27 (abstr.). Ginsberg N, Cieslak J, Rechitsky S et al. 2002 Reproductive BioMedicine Online 4 (suppl. 2), 31 (abstr.). International Working Group on Preimplantation Genetics 2001 Preimplantation genetic diagnosis – experience of 3000 clinical cycles. Report of the 11th Annual Meeting of International Working Group on Preimplantation Genetics, in association with 10th International Congress of Human Genetics, Vienna, May 15, 2001. Reproductive BioMedicine Online 3, 49–53. Katz MG, Mansfield J, Gras L et al. 2002 Diagnosis of trisomy 21 in preimplantation embryos by single-cell DNA fingerprinting. Reproductive BioMedicine Online 4, 43–50. Kaufman DS, Hanson ET, Lewis RL et al. 2001 Hematopoietic colony-forming cells derived from human embryonic stem cells. Proceedings of the National Academy of Sciences of the USA 98, 10716–10721. Kilani Z, Haj Hassan L 2002 Sex selection and preimplantation genetic diagnosis at the Farah Hospital. Reproductive BioMedicine Online 4, 68–70. Kuliev A, Cieslak J, Ilkevitch Y, Verlinsky Y 2002 Nuclear abnormalities in series of 6733 human oocytes. Reproductive BioMedicine Online 4 (suppl. 2), 11 (abstr.). Lacham-Kaplan O, Daniels R, Trounson A 2001 Fertilization of mouse oocytes using somatic cells as male germ cells. Reproductive BioMedicine Online 3, 205–211. Lim CK, Min JH, Song GJ et al. 2002 Reliability of PGD with FISH analysis in reciprocal or Robertsonian translocation carriers. Reproductive BioMedicine Online 4 (suppl. 2), 29 (abstr.). Malmgren H, Sahlén S, Inzunza J 2002 Single cell CGH analysis of human preimplantation embryos from PGD patients with balanced structural chromosome aberrations. Reproductive BioMedicine Online 4 (suppl. 2), 14–15 (abstr.). Malpani A, Malpani A, Modi D 2001 The use of preimplantation genetic diagnosis in sex selection for family balancing in India. Reproductive BioMedicine Online 4, 16–20. Martin R, Shil Q, Field LL, Rademaker A 2002 Reduced recombination and non-disjunction in human spermatozoa. Reproductive BioMedicine Online 4 (suppl. 2), 12 (abstr.). Monk M, Holding C, Goto T 2002 Embryo-specific gene expression in human preimplantation development and cancer. Reproductive BioMedicine Online 4, (suppl. 2), 12 (abstr.). Munné S 2002 Preimplantation genetic diagnosis of numerical and structural chromosome abnormalities. Reproductive BioMedicine Online 4, 183–196. Munné S, Magli C, Cohen J et al. 1999 Positive outcome after preimplantation diagnosis of aneuploidy in human embryos. Human Reproduction 14, 2191–2199. Munné S, Sandalinas M, Escudero T et al. 2000a Outcome of preimplantation genetic diagnosis of translocations. Fertility and Sterility 73, 1209–1218. Munné S, Sandalinas M, Escudero T et al. 2002b Some mosaic types increase with maternal age. Reproductive BioMedicine Online 4 (suppl. 2), 19 (abstr.). Munné S, Cohen J, Sable D 2002c Preimplantation genetic diagnosis for advanced maternal age and other indications. Fertility and Sterility 78, 234–236. Ozen S, Rechitsky S, Verlinsky Y 2002 Optimization of highresolution single cell comparative genomic hybridization to fit in PGD framework. Reproductive BioMedicine Online 4 (suppl. 2), 44 (abstr.). Rechitsky S, Verlinsky O, Chistokhina A et al. 2002 Preimplantation genetic diagnosis for cancer predisposition. Reproductive BioMedicine Online 5, 148–155. Sermon K 2002 Preimplantation genetic diagnosis for dynamic mutations. Reproductive BioMedicine Online 4 (suppl. 2), 24 (abstr.). Silber S, Sadowy S, Lehahan K et al. 2002 High rate of chromosome mosaicism but not aneuploidy in embryos from karyotypically normal men requiring TESE. Reproductive BioMedicine Online 4 (suppl. 2), 20 (abstr.). Simpson JL 2002 PGD as part of pre-pregnancy genetic screening. Reproductive BioMedicine Online 4 (suppl. 2), 10 (abstr.). Staessen C, Van Assche E, Platteau P et al. 2002 Ongoing implantation rate after blastocyst transfer with or without PGD for aneuploidy screening in women over 37 years (a randomized controlled trial). Reproductive BioMedicine Online 4 (suppl. 2), 18 (abstr.). Tease C, Hartshorne G, Hulten MA 2002 Patterns of meiotic recombination in human fetal oocytes. American Journal of Human Genetics 70, 1469–1479. Tesarik J, Mendoza C 2002 Reconstruction of oocytes from patient’s somatic cells. Reproductive BioMedicine Online 4 (suppl. 2), 22 (abstr.). Tesarik J, Nagy ZP, Sousa M et al. 2001 Fertilizable oocytes reconstructed from patient’s somatic cell nuclei and donor ooplasts. Reproductive BioMedicine Online 2, 160–164. Trounson AO 2002 Embryonic stem cells. Reproductive BioMedicine Online 4 (suppl. 2), 23 (abstr.). Trounson A, Pera M 2001 Human embryonic stem cells. Fertility and Sterility 76, 660–661. Van Assche E, Staessen C, Ogur G et al. 2002. PGD for reciprocal and Robertsonian translocations in 41 treatment cycles. Reproductive BioMedicine Online 4 (suppl. 2), 27 (abstr.). Verlinsky Y, Rechitsky S, Verlinsky O et al. 2001a Preimplantation diagnosis for p53 tumour suppressor gene mutations. Reproductive BioMedicine Online 2, 102–105. Verlinsky Y, Rechitsky S, Schoolcraft W et al. 2001b Preimplantation diagnosis for Fanconi anemia combined with HLA matching. Journal of the American Medical Association 285, 3130–3133. Verlinsky Y, Cieslak J, Evsikov S et al. 2002a Nuclear transfer for full karyotyping and preimplantation diagnosis for translocations. Reproductive BioMedicine Online 5, 300–305. Verlinsky Y, Rechitsky S, Verlinsky O et al. 2002b Preimplantation diagnosis for early onset Alzheimer disease caused by V717L mutation. Journal of the American Medical Association 287, 1018–1021. Wells D, Escudero T, Levy B et al. 2002 Comprehensive aneuploidy screening in human IVF embryos using CGH: protocol development and clinical application. Reproductive BioMedicine Online 4 (suppl. 2), 14 (abstr.). Wilton L, Williamson R, McBain J et al. 2001 Birth of healthy infant after preimplantation confirmation of euploidy by comparative genomic hybridization. New England Journal of Medicine 345, 1537–1541. Wilton L, Williamson R, McBain J et al. 2002 Preimplantation diagnosis of aneuploidy using comparative genomic hybridization. Reproductive BioMedicine Online 4 (suppl. 2), 13–14 (abstr.). Zhuang GL 2002 PGD: China’s experience. Reproductive BioMedicine Online 4 (suppl. 2), 39 (abstr.). 299