primary health care nursing in new zealand - ResearchSpace
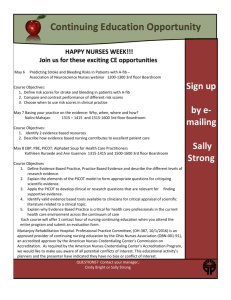
advertisement

MAPPING A NEW FUTURE: PRIMARY HEALTH CARE NURSING IN NEW ZEALAND Nicolette Fay Sheridan A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy, The University of Auckland, 2005 Thesis Consent Form This thesis may be consulted for the purpose of research or private study provided that due acknowledgement is made where appropriate, and that the author’s permission is obtained before any material from the thesis is published. I agree that The University of Auckland Library may make a copy of this thesis for supply to the collection of another prescribed library, on request from that library; and I agree that this thesis may be photocopied for supply to any person in accordance with the provision of Section 56 of the Copyright Act 1994. Signed: Date: Abstract The aim of the study was to determine the practice of nurses employed in integrated care projects in New Zealand from late 1999 to early 2001. Integrated care was a major health reform strategy that emphasised primary health care as a means to improve service provision between the health sectors. An investigation of nurses’ practice sought to determine the extent to which primary health care principles had been adopted in practice, as a comprehensive primary health care approach has been advocated globally in the management of chronic conditions; the leading cause of disability throughout the world and the most expensive problems faced by health care systems. The philosophical basis of the research was postpositivism. The study employed a quantitative non-experimental survey design because it allowed numeric descriptions of the characteristics of integrated care projects to be gained for the purpose of identifying nurses’ practice. The unit of inquiry was the integrated care project, and 80 comprised the study population. Data were obtained on projects from expert informants (n=27) by telephone survey using a structured interview questionnaire developed by the researcher. Data obtained from interviews were statistically analysed in two stages. First, data were produced to comprehensively describe the characteristics of integrated care projects and nurses practice. The ‘Public health interventions model’ was used as a framework to analyses the interventions (activities) and levels of population-based practice of nurses. Following this, the social values embedded in nurses’ practice were determined using ‘Beattie’s model of health promotion’ as a framework for analysis. A strong association was found between nurses’ practice in projects and strategies used in integrated care, such as information sharing, guideline development and promotion, and case management, and projects with an ethnic focus, low income focus, chronic condition focus, and well-health focus. Whilst nurses undertook interventions most frequently at the individual practice level they were also strongly i associated with the small proportion of interventions that were undertaken at the community level. The majority of interventions by nurses reflected the health promotion value of health persuasion, indicating a paternalist and individual-oriented philosophy. Nurses were engaged in two interventions that indicated a collectiveoriented philosophy - coalition building and community development, the latter reflecting health promotion values of negotiation, partnership and empowerment. The study demonstrated that nurses’ practice in projects was predominantly centred on individual-focused population-based practice suggesting the need for a framework to assist nurses to transition their practice to include more activity at the community and systems levels. Without a reorientation of practice, nurses will remain limited in their ability to achieve health gains for populations. In response to this conclusion, and drawing on research results and reviewed literature, a new model, The ‘Primary Health Care interventions model’ was constructed. Recommendations include advocacy for the acceptance of the model by the health funder, professional nursing bodies, health organisations, educational institutions, nurses, communities, and individuals. ii Dedication To my mother and father who taught me to care and reason, and whose experiences of illness gave new insights into the emerging model, with love iii Acknowledgements During the years that led up to this thesis, I have drawn often and long upon the time, advice, wisdom and good will of Jennifer Hand. Margaret Horsburgh has also provided significant help, and I thank both sincerely. For similar favours granted at more select points in time warm thanks go to Paul Brown, Barbara Smith, Val Grey, Warren Jones, Wendy Diamond, Sarah Lovell and Ivana Nakarada-Kordic. I owe a depth of gratitude to Lorraine Nielsen for her enduring kindness and generosity, and to Mary Finlayson who encouraged and believed in me. I am likewise grateful to Matthew Parsons and work colleagues who provided good cheer. Marjorie Schaffer, Linda Olson Keller, Sue Strohschein and Ron Labonte provided gracious hospitality and ready knowledgeable assistance; without them this would be a lesser work. Thanks also go to the New Zealand Ministry of Health for assisting with scholarship funding and Judy Kilpatrick, School of Nursing, University of Auckland who graciously allowed me to organise my days to complete this project. I am obliged to these institutions for their assistance. For all kinds of things having to do less directly, but no less essentially with this thesis completion, my fondest appreciation goes to Vicki Newton, friends and family. Finally, my gratitude extends to all those participants who stimulated my understanding of health and care; and how we, as nurses and health professionals, can assist clients in meeting their needs for health and wellness in a rapidly changing society. iv Table of Contents ABSTRACT I DEDICATION III ACKNOWLEDGEMENTS IV TABLE OF CONTENTS V LIST OF TABLES XIII LIST OF FIGURES XV INTRODUCTION XVI 1Chapter 1 Public health and generations of health reform 1 1.1 Introduction 1 1.2 Public health in context 1 1.3 Health systems and health reform 5 1.3.1 Three generations of health system reform 8 1.3.1.1 First generation health system reform 1.4 9 1.3.1.2 Second generation health system reform 10 1.3.1.3 Third generation health system reform 11 Public health developments intersect generations of health reform 14 1.4.1 Era of indigenous control (pre-colonisation) 14 1.4.2 Colonial era (1840 to 1890) 16 1.4.3 Nation-building era (1890 to 1940) 17 1.4.4 Affluence, medicine and infrastructure (1950s to early 1970s) 18 1.4.5 Life-style era (late 1960s to mid-1980s) 20 1.4.6 New public health (1980 to 2005 and beyond) 22 2Chapter 2 Health promotion theory 27 2.1 Introduction 27 2.2 Health promotion and nursing 28 2.3 Beattie’s model of health promotion 30 2.3.1 Health persuasion 32 2.3.2 Personal counselling 33 2.3.3 Legislative action 34 v 2.3.4 Community development 34 2.3.5 Beattie’s model: Health promotion values in practice 36 2.4 Health promotion: Social theories and models 37 2.4.1 Social theories 37 2.4.2 Models of health education and health promotion 38 2.5 Beattie’s model: An analytic framework for use in the NICPS 40 2.6 In conclusion 41 3Chapter 3 Chronic Conditions 43 3.1 Introduction 43 3.2 Chronic conditions challenge the health care system 44 3.2.1 Categorising countries 46 3.2.2 The reasons chronic conditions are escalating in New Zealand 46 3.2.2.1 Demographic trends and population ageing 47 3.2.2.2 Consumption patterns and life-style changes 49 3.2.3 Economic impact 51 3.2.3.1 New Zealand: Health care costs 3.2.4 3.3 Impact on the poor 55 Changing the systems of care 3.3.1.1 57 Community resources and policies 60 3.3.1.2 Health system organisation of care 60 3.3.1.3 Self-management support 60 3.3.1.4 Delivery system design 61 3.3.1.5 Decision support 61 3.3.1.6 61 Clinical information systems Risk prevention 3.4.1 3.5 53 Current health systems are not designed for chronic problems 3.3.1 3.4 52 62 Government responsibility for health 64 In conclusion 65 4Chapter 4 Primary health care nursing 67 4.1 Introduction 67 4.2 The current PHC nursing workforce 68 4.2.1 Primary health care and community survey 2001 69 vi 4.2.2 4.3 Education preparation 70 Nursing groups in communities 71 4.3.1 Community nurses in early New Zealand 71 4.3.2 District Nursing 72 4.3.3 Public Health Nursing 73 4.3.4 Plunket Nursing 74 4.3.5 School Nursing 75 4.3.6 Practice Nursing 77 4.3.7 Other community nursing groups and new strategies 79 4.3.8 The historical legacy of community nursing 79 4.4 Contemporary PHC nursing developments 82 4.4.1 Background 82 4.4.2 PHC Nursing scholarships and innovative models of practice 83 4.4.3 Nurse Practitioner scope of practice 85 4.5 A model for PHC Nursing: The public health interventions wheel 4.5.1 87 Describing the Public Health Intervention Wheel 89 4.5.1.1 Population-based 90 4.5.1.2 Individual and family, community, and systems levels of practice 91 4.5.1.3 Seventeen public health interventions 93 4.5.2 Validated and evidence-informed 96 4.5.2.1 Findings of the review of the intervention wheel 4.6 96 In conclusion 97 Chapter 5 5 Integrated Care 99 5.1 Introduction 99 5.2 Recent background 100 5.3 Central problem: Fragmentation between services 101 5.4 Integrated care: Different definitions and meanings 104 5.4.1 NICPS definition of integrated care 105 5.4.2 Perspectives of Ministers, advisors and purchasers 107 5.4.3 Types of integrated care 109 5.4.4 Strategies for integrated care 110 5.4.4.1 Collaboration 5.4.4.2 Case management 110 111 vii 5.4.4.3 Guideline development 5.4.5 5.5 Implications of integrated care for Maori New Zealand integrated care demonstration pilot projects 112 113 116 5.5.1 Conceptual development 116 5.5.2 Potential risks in integrated care 118 5.5.3 Implementation: What actually happened? 119 5.5.4 Evaluation findings 123 5.6 In conclusion Chapter 6 6 Methods: Nurses in integrated care projects study 125 127 6.1 Introduction 127 6.2 Research questions 128 6.3 A framework for the study design 129 6.3.1 6.4 Quantitative and descriptive: The survey Study Methods 6.4.1 Study population 132 133 133 6.4.1.1 Eligibility 133 6.4.1.2 Sampling 134 6.4.1.3 Procedures for the recruitment of projects 135 6.4.2 Ethical considerations 136 6.4.3 Data collection 136 6.4.3.1 Interview questionnaire 136 6.4.3.2 Question form and content 139 6.4.3.3 Pilot-testing the instrument 141 6.4.3.4 Reliability and validity 142 6.4.3.5 The role of the interviewer 6.4.4 Organising the data for analysis 6.4.4.1 Constructing a code and assigning to survey data 144 147 147 Ethnic group 152 Low income 153 Age group 153 Disease or condition 154 6.4.4.2 Data entry 157 6.4.4.3 Coding and data reduction as a source of errors 158 6.4.5 Data analysis 158 viii 6.4.5.1 Stage one analysis 159 6.4.5.2 Stage two analysis 160 Chapter 7 7 Results: Nurses in integrated care projects study 162 7.1 Introduction 162 7.2 Study results 162 7.2.1 Survey respondents 162 7.2.2 Integrated care projects 163 7.2.3 Organisational structure 163 7.2.4 Funding 165 7.2.5 Type of service integration 165 7.2.6 Strategies for integration 166 7.2.7 Project level of population-based practice 167 7.2.8 Age group 168 7.2.9 Ethnic group 168 7.2.10 Low income 169 7.2.11 Disease, condition, or other focus 169 7.2.12 Non-nursing personnel 171 7.2.13 Nursing 171 7.3 Projects employing nurses 7.3.1 177 Planning a new health service and delivering an existing health service differently by projects employing nurses 177 7.3.2 Funding by projects employing nurses 178 7.3.3 Type of service integration by projects employing nurses 178 7.3.4 Strategies of integration by projects employing nurses 178 7.3.5 Project level of population-based practice by projects employing nurses 180 7.3.6 Age group by projects employing nurses 180 7.3.7 Ethnicity by projects employing nurses 181 7.3.8 Low income by projects employing nurses 181 7.3.9 Disease, condition or other by projects employing nurses 182 7.3.10 Chronic or acute condition, well-health, or other by projects employing nurses 183 7.3.11 Non-nursing personnel by projects employing nurses 183 7.4 Chronic or acute condition, well-health, or other 7.4.1 Health service by chronic or acute condition, well-health, or other 183 183 ix 7.4.2 Project level of population-based practice by chronic or acute condition, well-health, or other 184 7.4.3 Age group by chronic or acute condition, well-health, or other 185 7.4.4 Age group by disease, condition or other 186 7.4.5 Ethnicity by type of disease, condition or other 187 7.5 Age group 187 7.5.1 Ethnicity by age group with and without disease or condition 187 7.5.2 Income by age group, with or without disease or condition 188 7.6 Nursing interventions 189 7.7 Social values embedded in the practices of nurses employed in projects 192 7.8 Summary of study results 195 Chapter 8 8 Discussion 199 8.1 Introduction 199 8.2 Which characteristics of integrated care are more strongly associated with projects that employ nurses? 200 8.2.1 Organisation 200 8.2.1.1 Delivering an existing service differently and planning a new service 200 8.2.1.2 Health care services provided by projects 201 8.2.1.3 Incentives and costs for general practice to be a project partner 203 8.2.1.4 Material incentives to clients 204 8.2.1.5 Incentives and costs for the hospital to be a project partner 205 8.2.2 Funding 206 8.2.3 Type of service integration 207 8.2.4 Strategies for integrated care 208 8.2.4.1 Information sharing 208 Building relationships 209 Peer advice, education and referral 210 Client education 210 Development of a database 211 8.2.4.2 Guideline development and promotion 211 8.2.4.3 Case management 212 8.2.4.4 New coordination strategies 214 8.2.5 Level of population-based practice approach of projects 214 x 8.2.6 Age group focus 217 8.2.7 Ethnic group focus 219 8.2.8 Low income focus 221 8.2.9 Health, disease, condition or other focus 222 8.2.10 Non-nursing personnel 8.3 Population-based interventions and levels of practice undertaken by nurses in integrated care projects 225 227 8.3.1 Intervention: Surveillance 228 8.3.2 Intervention: Disease and health event investigation 228 8.3.3 Intervention: Outreach 229 8.3.4 Intervention: Screening 230 8.3.5 Intervention: Referral and follow-up 231 8.3.6 Intervention: Case management 231 8.3.7 Intervention: Delegated functions 232 8.3.8 Interventions: Health teaching 232 8.3.9 Intervention: Counselling 233 8.3.10 Intervention: Consultation 234 8.3.11 Intervention: Collaboration 234 8.3.12 Intervention: Coalition building 235 8.3.13 Intervention: Community organising 236 8.3.14 Intervention: Advocacy 236 8.3.15 Intervention: Social marketing 237 8.3.16 Intervention: Policy development and enforcement 238 8.4 What underlying values are made explicit when interventions undertaken by nurses are analysed? 238 8.4.1 Beattie’s model of health promotion 239 8.4.2 The four approaches to Beattie’s model 239 8.4.2.1 Authoritative or negotiated modes of interventions 241 8.4.2.2 Individual and collective focus of interventions 242 8.4.2.3 The challenge for nursing 242 8.5 Study findings provide new insights and direction 244 8.6 The Primary Health Care Interventions Model 245 8.6.1 Strengths of the PHCI model 250 xi Chapter 9 9 Conclusion: Mapping a new future 252 9.1 Introduction 252 9.2 Strengths and limitations of the study 253 9.2.1 Study design 253 9.2.2 Study population 255 9.2.3 Questionnaire design 256 9.2.4 Data collection procedures 257 9.2.4.1 The interview 9.2.5 Data analysis procedures 257 258 9.2.5.1 Organising data analysis 258 9.2.5.2 Data analysis 258 9.3 Implications of the PHCI Model for nursing practice 259 9.4 Recommendations 262 9.5 Conclusion 264 References 266 Appendices 303 Appendix 1 Structure of the New Zealand Health and Disability Support Sector 1999 304 Appendix 2 Structure of the New Zealand Health and Disability Support Sector 2005 306 Appendix 3 Questionnaire 308 Appendix 4 Interventions undertaken by nurses in integrated care projects: Frequency tables 315 xii List of Tables Table 1: New Zealand public health developments and health reforms 25 Table 2: Studies addressing costs related to chronic conditions 52 Table 3: New Zealand studies addressing costs related to chronic conditions 53 Table 4: Milestones for PHC nursing development 87 Table 5: Definitions of public health interventions 95 Table 6: Risks 119 Table 7: Integrated care demonstration pilot projects 121 Table 8: Research approach to the Nurses in Integrated Care Projects Study 132 Table 9: Variables, research questions and items on the survey 138 Table 10: Question form of items on the survey 141 Table 11: Interviewer approaches to contacting respondent 145 Table 12: Codes assigned to questions 1 to 3 148 Table 13: Codes assigned to questions 4 to 9 149 Table 14: Codes assigned to question 10 150 Table 15: Codes assigned to questions 11 and 12 150 Table 16: Codes assigned to questions 13 to 15 152 Table 17: Codes assigned to question 17 154 Table 18: Codes assigned to question 18 155 Table 19: Codes assigned to questions 19 to 23 156 Table 20: Codes assigned to question 24 157 Table 21: Codes assigned to question 25 and 26 157 Table 22: Total interventions and levels of population-based practice by wedge undertaken by nurses in projects 176 Table 23: Project level of population-based practice by projects employing nurses 180 Table 24: Disease or condition or other by projects employing nurses 182 Table 25: Health service by chronic and acute condition, well-health, or other 184 xiii Table 26: Project level of population-based practice by chronic or acute condition, well-health, or other 185 Table 27: Age group by chronic or acute condition, well-health, or other 186 Table 28: Ethnicity by age group with or without disease or condition 188 Table 29: Health teaching intervention undertaken by nurses in projects 190 Table 30: Community organising intervention undertaken by nurses in projects 190 Table 31: Coalition building intervention undertaken by nurses in projects 191 Table 32: Surveillance intervention undertaken by nurses in projects 191 Table 33: Summary of research questions and evidence informed responses 195 xiv List of Figures Figure 1: Beattie’s model of health promotion 31 Figure 2: The Chronic Care Model 59 Figure 3: The Public Health Interventions Wheel 89 Figure 4: Population-based systems level of practice 91 Figure 5: Population-based community level of practice 92 Figure 6: Population-based individual and family level of practice 93 Figure 7: Knowledge claims, strategies of inquiry, and methods leading to approaches and the design process 130 Figure 8: Incentives to clients and project partners and new costs to hospitals and general practices 165 Figure 9: Organisational relationships based on vertical and/or horizontal integration 166 Figure 10: Strategies for integration 167 Figure 11: Project level of population-based practice 168 Figure 12: Projects by specific disease or condition 169 Figure 13: Chronic or acute condition, well-health or other 171 Figure 14: Total interventions undertaken by nurses in projects 172 Figure 15: Total interventions and levels of population-based practice undertaken by nurses in projects 173 Figure 16: Total interventions and levels of population-based practice by wedge undertaken by nurses in projects 174 Figure 17: Interventions and levels of population-based practice undertaken by nurses in projects 192 Figure 18: An adaptation of Beattie’s model of health promotion situating total interventions by nurses in projects 194 xv Introduction The task is not so much to see what no one else has seen, but to think what no one yet has thought, about that which everyone sees. (Arthur Schopenhauer, 1788-1860, Philosopher) Nurses are the largest health professional group working in the New Zealand health sector and have the potential to make an extensive and profound contribution to reducing health inequalities. Over the last 50 years, average life expectancy at birth has increased globally by almost 20 years (World Health Organization, 2003). However, there are major disparities in the health of people within New Zealand and between countries, as these disparities continue to grow (Ministry of Health, 2001c; Pomare et al., 1995; World Health Organization, 2003). Primary health care nursing in New Zealand is a new specialty area of practice that combines many different nursing groups who have traditionally worked in communities. These nurses have a central role in health promotion driven by primary health care principles, such as, social justice, equity and community participation. In 2004, primary health care nurses represented 10.6 per cent (n=3672) of the registered nursing workforce in New Zealand (New Zealand Health Information Service, 2004). The New Zealand Ministry of Health is investing in primary health care as a health reform strategy and nursing has received NZ$8.1 million for workforce development (A. King, 2005). The New Zealand Primary Health Care Strategy (Ministry of Health, 2001c) signposted the way forward, but as yet a national framework to guide primary health care (nursing) practice has not been articulated. The purpose of this thesis is to establish the current position of primary health care nursing in New Zealand, and to identify areas for future nursing development in line with the PHC Strategy. This thesis has produced a unique and innovative model for implementing primary health care nursing practice, developed from public health and nursing literature, health promotion theory, and research on nurses’ practice. The research investigated the practice of nurses employed in 80 New Zealand integrated care projects in the late 1990s during the third generation of health reform. xvi Primary health care is not a new concept and has been promoted in two earlier generations of health reform occurring within the period 1940 to 1980 (see p. 9-11, 25) as a way to provide health care to the majority of the world’s poor. This approach failed on both occasions because the care was “primitive rather than primary” (World Health Organization, 2000, p. 15). Health workers did not have the requisite skills, resource allocation was insufficient to meet the need, and health services had a prorich bias due to the disproportionate use of hospital services by the well off. The current generation of health reform in New Zealand and globally, is adopting primary health care for a third time. There is now a greater likelihood for success as a consequence of previous experience and learning, better knowledge about health and its determinants, improved information systems, ‘consumer voice’, and integrated approaches to health promotion. Today, a primary health care approach advocates a balanced system of treatment and disease prevention, through affordable, accessible and appropriate services. At the same time, there is recognition that health services alone are not the answer, and that a major re-orientation is needed in the way that health is considered, and health issues are acted upon (Talbot & Verrinder, 2005). Pressure also exists on all health systems to develop a response to the escalation of chronic conditions, which by 2020 will contribute to more than 60 per cent of the global burden of disease and be the leading cause of disability throughout the world (World Health Organization, 2001a; World Health Organization). In New Zealand, demographic transitions, population ageing, changing life-styles, consumption patterns, and risk behaviours are clear determinants of this trend. Internationally, chronic conditions disproportionately affect the poor, economically challenge families and governments, and jeopardise the sustainability of health care systems. Chronic conditions are lengthy and require continuity of care, demonstrating a mismatch with current health care systems that provide episodic acute care. A comprehensive health care system that assures ongoing support for chronic conditions is essential, as technological advances alone will not stop conditions such as heart disease, acquired immune deficiency syndrome, diabetes and depression (World Health Organization, 2000). Successful chronic care management requires the same fundamental changes as health systems, that is, a shift to effective prevention strategies. This has not been core xvii business, as the focus has traditionally been strongly placed upon curing people. Improving health requires a major emphasis on intervention in the chain of disease causation, with the underlying risks to health addressed, in addition to the treatment of established diseases. Almost half the global mortality and much of the burden of disease are attributed to the top 20 risk factors (World Health Organization, 2002b). Tackling major risk has the potential to reduce inequalities worldwide, and governments have a leading role in this risk reduction. Contemporary health promotion and public health theory can play a significant part in repositioning the focus from the medical ethics of the individual to one that considers the social ethics of the population (Lamm, 1994). Beaglehole and Bonita (1997) argue that “Public health is the collective action taken by society to protect and promote the health of entire populations; in contrast, clinical medicine deals only with the problems of individuals” (p. xiii). Accordingly, health care systems and health workers have tended to take a narrow view of what contributes to health, and focused on health service issues. Nurses who have historically provided care to sick individuals in bed-based institutional settings are being challenged to practice in new ways (Porter-O'Grady, 1999). The Ministry of Health in New Zealand has funded scholarships for postgraduate nursing education and the development of ‘innovation projects’ in an attempt to build a primary health care nursing workforce. However, situating various nursing groups under the umbrella title of primary health care does little to facilitate a primary health care philosophy linked to ideas of social justice and equity. At present, there is no commonly agreed core knowledge attributed to the specialty of primary health care nursing. The diverse range of interventions undertaken by the different nursing groups has not been well-defined, nor has the level/s at which nurses undertake population-based practice (individual and family, community, system). For nursing to take a leading role in “reducing health inequalities, achieving population health gains and promoting and preventing disease” (Ministry of Health, 2003b. p. vii), work with communities and systems has the potential to achieve greater improvements in population health than work exclusively focused on individuals and families (Keller, Strohschein, Lia-Hoagberg, & Schaffer, 2004a). An analysis of New Zealand nurses’ in integrated care projects actual practice can identify the particular interventions and xviii levels of practice that need to be strengthened, “as interventions at each level of practice contribute to the overall goal of improving population health” (Keller et al., 2004a, p. 457) . Integrated care was considered a major public sector reform strategy initiated from central government (Wells, 1998) that engaged health professionals, including nurses, in efforts to improve the coordination of care between health sectors and strengthen primary health care. The thesis research, ‘Nurses in integrated care projects study’ was conducted during this period. The study design was quantitative and the philosophical basis of the research was postpositivism (see pp. 130-131). The research aimed to describe the characteristics of integrated care projects to create a context within which nurses’ practice could be situated. Nurses’ practice was then assessed to determine the range of interventions and related levels of population-based practice routinely undertaken, and the health promotion values embedded within this practice were identified. Finally, the research findings in combination with the literature provided the basis for the construction of a model to guide the implementation of future primary health care nursing practice. The model provides a strong framework to develop primary health care practice, and nurses whose work impacts on health, can use this framework in a manner that both strengthens the relevance of health promotion work, and allows them to be accountable for their practice. Enabling insights for practitioner development at a personal level, the model can also be used by the nursing profession as an analytic framework to assess overall primary health care nursing practice, and inform national strategic direction. xix 1 Chapter 1 Public health and generations of health reform 1.1 Introduction “Public health is an approach that aims to promote health, prevent disease, treat illnesses, prolong valued life, care for the infirm and to provide health services” (Laverack, 2005, p. 1). Historically, public health centred on preventing the spread of infection and protecting the general population. Today, public health is also committed to reducing inequalities in health, and the development of health public policy is an essential component of this approach (Baum, 1998). With such a broad focus, it is not surprising that the term ‘public health’ is used to cover a wide range of specialist areas that include water supply and sanitation, environmental health, nursing and health promotion. Predictably, public health remains a contested and disputed area of practice knowledge, priorities, and the services it claims to deliver. This chapter describes the past and present public health developments and accompanying perspectives, as a basis for understanding and situating the practice of nurses in community settings. Section 1.2 highlights the various conceptions of public health and introduces the ‘new public health’ agenda. Sections 1.3 and 1.4 describe three generations of health care reform, and six distinct periods of public health identifying the dominant ideologies and interventions of each era. The tensions that exist in public health philosophy and practice are discussed. Laverack (2005) claims these tensions belong principally to people employed in the health sector who have vested interests in “conceptual models, professional legitimacy and resources” (p. 1). The chapter concludes with a summary table (see p. 25) that demonstrates where public health developments intersect generations of health reform. 1.2 Public health in context Definitions of public health have changed and evolved since the nineteenth century when the main concern was the interface between the body and the environment, and 1 public health efforts sought to prevent the transmission of disease (D. Armstrong, 1988). In the early twentieth century Last (1998) suggests a greater emphasis was placed upon the individual and on personal hygiene. The New Zealand Public Health Association defines public health according to the Acheson Report1 as “the art and science of preventing disease, prolonging life, and promoting the health of the population through the organised efforts of society” (N. Holt, personal communication, June 14, 2005). In New Zealand there may be confusion over the term public health because it is often used to refer to the publicly funded health service. Baum (1998) maintains public health exists to make people and their communities healthier through change, a definition that is consistent with the concept that “public health is the collective action taken by society to protect and promote the health of the entire population” (Beaglehole & Bonita, 1997, p. xiii). In contrast, clinical medicine deals only with the problems of individuals and tends to take a narrow focus on health service issues. Beaglehole and Bonita argue that the predominance of a narrow medical focus by health systems is the reason for the failure by public health to achieve its potential to improve the public’s health. They believe that until health in a broad sense becomes a central concern of the policy making process, this situation will not change. In most countries a narrow disease focused route prevails under the influence of current social and economic ideology, and health is taken to be the absence of disease attained by life-style changes that reduce an individual’s risk of disease. In this approach the main public health activities are disease prevention, targeting high-risk populations, and the emphasis in epidemiology is on method, and on clinical and molecular studies that produce short-term benefits and do not address fundamental threats to global health. The general social climate of the 1980s shifted away from the notion that medical progress would eventually cure most diseases (McKeown, 1979), and that individuals were responsible for making life-style changes to advance health (Hetzel, 1976), to a 1 In 1988, the Department of Health and Social Security published ‘Public Health in England’, a report of the Committee of Inquiry into the future development of the public health function. Sir Donald Acheson chaired the Committee and the report was commonly referred to as the ‘Acheson Report’. 2 focus on ‘health for all by the year 2000’, promoting primary health care2 (World Health Organization, 1978). This idea tied health improvement to overall social and economic development, and primary health care stressed the importance of equity in access to community-based services, encouraging a comprehensive, sustainable approach to improving health. Such an approach, however, was soon replaced by selective and targeted strategies to control disease, a major departure from the original ‘health for all’ concept (Rifkin & Walt, 1986). Selective primary health care emphasised medical interventions above measures such as housing, education and nutrition, and resulted in a focus on particular diseases that once resolved were simply replaced by another, as the underlying causes of ill health had not been dealt with (Tarimo & Webster, 1994). Recognition that major health problems cannot be solved by medical care (J. Ashton & Seymour, 1988; Lalonde, 1974) led to the most recent3 introduction of the term ‘new public health’. The world’s first international conference on health promotion was held in Canada in the mid-1980s and resulted in the development of the Ottawa Charter (World Health Organization, 1986). Baum (1998) pointed out that ‘health for all’ had not been adopted by wealthy countries, and the life-style and behavioural approaches were increasingly being seen limited and requiring a new conceptualisation for health promotion. She stressed that health budgets continued to grow in the 1980s and the prospect of reducing these by improving the health of populations was of interest. The Ottawa Charter approach to health promotion plays down the life-style (health education) approach to health and emphasises the importance of social structures and policy as key health determinants. Five areas for action include: building healthy public policy; creating supportive environments; strengthening community action; developing personal skills, and re-orienting health services. Green and Raeburn (1988) characterised two approaches to health promotion, the ‘individual’, and the ‘system’, “observing that these views led to divided ideology and theoretical perspectives on health promotion” (p. 35). Despite this, they suggested that in practice, viewpoints were often more integrated. The life-style approach was not 2 The Joint WHO/UNICEF International Conference on primary health care held at Alma Ata, USSR (now Almaty, Kazakhstan) in 1978, adopted primary health care as the strategy for achieving ‘health for all’. 3 The term ‘new public health’ was first used in 1916 and its original use referred to a narrow view of public health based on bacteriology (Hill, 1916). 3 rejected, but rather integrated under the ‘development of personal skills’ as one of many strategies. The Ottawa Charter, based on the understanding that peace, shelter, education, food, income, a stable ecosystem, social justice and equity are requisite for health, sought a multi-pronged, multilevel health promotion strategy. New public health overlapped and integrated with other health movements of the 1960s and 1970s, such as health promotion, primary health care, women’s health, Maori health, worker’s health, and health education. The new public health movement set out an agenda for public action, initiating more social interventions, community participation and policy change, in line with the activities of health promotion (Downie, Fyfe, & Tannahill, 1990). Contemporary approaches to health promotion: disease prevention; health education; healthy public policy; environmental4 protection, and community empowerment, are central to the practice of public health. Yet despite new public health and the central strategy of health promotion, which challenged the idea that health was just a medical issue and stressed socio-environmental aspects, the mainstream debate of the 1980s focused on the requirements of the curative services5. The 1990s have been a period of international economic uncertainty and coincided with less proactive public health action. Health promotion as a discrete activity has met with limited success, although many have argued that it should have been central to the development of social and economic policies. Free market thinking and neoconservative ideology have dominated making it difficult to advance strategies that considered the determinants of health. Only by directing attention towards the socioenvironmental threats to health can the increasing inequality between and within countries be addressed. Interestingly, however, there is also the risk of a shift in public health interest to the potential of the human genome project and molecular and genetic approaches to disease control (Beaglehole & Bonita, 1997). A lack of attention to the major factors required to create healthy populations is of great concern. The major contributions to the determination of overall population 4 The term ‘environmental’ refers to more than physical factors and is inclusive of social, cultural, and economic factors. 5 Governments continued to be preoccupied with hospital issues, such as the size of waiting lists. 4 health status arise from public health measures aimed at the prevention of disease, illness, disability, and the lowering of death rates, as opposed to the function of health care (Frenk, 1993). Beaglehole and Bonita (1997) suggest the integration of medical care under the public health umbrella would facilitate the process of setting broad health goals and targets, and encourage resources to flow to prevention. As the concept of population health becomes understood in policy decisions and there is a major shift in focus to environmental sustainability, equity, and community, the potential of public health may be realised. Equity in health care has not been achieved by health services and narrowly defined disease prevention and health promotion activities. Recent estimates of the global burden of disease, the ageing of the world’s population, and better knowledge of the determinants of health are influencing the way countries are reforming health systems (World Health Organization, 2002a). A reintegration of the Ottawa Charter for health promotion and life-style approaches beginning with a people centred approach (Raeburn & Rootman, 1997) sought to build self-reliant local communities linked into a global system (World Health Organization, 1992). A recent international health promotion conference attempted to build new alliances for health, and included private sector partners (World Health Organization, 1997). Future debates about the impact of globalisation, including the growing influence of multinational companies and the declining influence of nation states is important to public health development. At present, addressing socio- environmental factors poses a huge challenge, but also makes the new public health agenda a more relevant guide for action (Baum, 1998). 1.3 Health systems and health reform A health system includes “all the activities whose primary purpose is to promote, restore or maintain health” (World Health Organization, 2000, p.5). This includes the provision of professional medical attention, interventions by traditional healers and home care of the sick, which is how 70-90 per cent of all sickness is managed (Gwatkin & Guillot, 2000). Traditional public health activities such as health promotion, health education, and disease prevention, and other interventions that 5 promote health like environmental safety improvement are also included. Today, the most fundamental objectives of the health system are: improving the health of the population they serve (attainment); responding to people’s expectations (responsiveness and fairness), and providing financial protection against the costs of ill-health (performance) (World Health Organization, 2000). Governments have become central to social policy and health care because to meet such objectives requires decision making in managing resources equitably and ultimately, the “responsibility for the overall performance of a country’s health system lies with government” (World Health Organization, 2000, p. xiv). Unfortunately, nearly all of the information about health systems refers only to the ‘health care system’, and describes either the provision of, or investment in health services, such as preventative, curative, and palliative interventions provided to individuals or populations. Despite this more limited definition, health systems represent one of the largest sectors in the world economy, with global spending on health care in 1999 about $1.2 trillion, up 5.6 per cent from the previous year, and 13 per cent of world gross domestic product. A moderate acceleration in spending growth of 6.5 per cent is expected from 2002 until 2010 (Heffler et al., 2001). The health system represents governments’ formal commitment to the health of the population, and commonly attempts to create and sustain the greatest good for the largest group of people. There is, however, wide variability in the extent to which this goal is achieved because diverse approaches are taken by governments in response to needs or demands, and numerous programmes compete for government funding. In addition, there is no single way to organise government departments, and these structures often determine priorities. Political interest groups and consumers impact on the strategic activities undertaken within the health system with regard to decision making, where they place pressure on decision-makers to allocate resources (McMurray, 2003). McMurray suggests tradition has a significant part to play in the way health systems are shaped. For example, two very different models are demonstrated in the health systems of the United Kingdom and the United States. In the United Kingdom, the national health services model is characterised by a government-financed and operated system, whereas in the United States an entrepreneurial market model driven by the private sector controls health care. By 6 contrast, New Zealand has a mix of public and private health services, and the extent to which services are privatised represents another political element (Boyd & Sheridan, 2000). In health care, commercial partners expect returns on their investments and this can conflict with the interests of other health professionals, who may perceive limits to education, career advancement, and improved employment conditions. Health systems have undergone overlapping generations of reform in the past one hundred years, and this is discussed more extensively in section 1.3.1. In summary, health reforms have included the founding of national health care schemes, the extension of social insurance schemes, and the promotion of primary health care as a route to achieving universal coverage - the goal of health for all. In the last decade there has been a gradual shift towards ‘new universalism’, the delivery of high quality essential care to all people (World Health Organization, 2000). However, at the national level in New Zealand, the ongoing debate about health reform has been narrowly focused on medical care services and has not embraced the need for a reemphasis on public health services (Beaglehole & Bonita, 1997). This appears to be the situation in most countries and the political motivations for reforming health systems remain contradictory. Opinions on the drivers of health reforms include: concern over inefficiencies in service delivery, which a devolved regional system is considered better able to resolve, though this remains uncertain (Lomas & Rachlis, 1996; Reamy, 1995); concern over the ineffectiveness of many medical interventions fuelling health system and academic collaborations to develop a more evidence-based approach to resource allocation (Lomas, Woods, & Veenstra, 1997); a desire to shift services from institutional to community settings, such as early discharge programmes, outpatient day surgeries, and community based chronic care management; for cost efficiency reasons; to provide more responsive services, and a desire to increase individual and community participation in health decision making and self-management (Lewis, 1997; Lomas, 1997; Lomas et al., 1997). Betkowski (1996) maintains health reform should be based on asking whether there is a way to get better value out of the money we spend on health, whilst Wilson (1996) argues that the aim of reform has frequently been to accommodate to reduced government funding. 7 In New Zealand, the government assumes a major part of the responsibility for health care provision. Davis and Ashton (2001) described the New Zealand health reforms during the 1990s as radical, ongoing and pervasive. According to Ashton (2005), the most notable and most radical of the health reforms occurred in 1993 when marketlike incentives were introduced into the system. Public purchasers tended service contracts to private and public providers who were then required to compete. Beaglehole and Bonita (1997) agree the main drivers of the early 1990 reforms were the introduction of the market into health services and separating the purchasers of services from the providers. In 2000 health reforms led to the establishment of 21 district health boards and the recombined roles of purchasing and providing services. The move to devolve to a regional system was a result of a labour-led coalition government elected to power in 1999, and the waning of the market model. Health policy began to reflect centre-left ideology and the emphasis was placed upon ‘patients not profit’, and cooperation rather than competition. Today, more information is available for services that require funding, new alliances have been formed, and different styles of service provision have emerged (T. Ashton, 2001). In the last decade Ashton contends strategies for improving health care provision have included integrated care, evidence-based medicine, a greater reliance on democratic and consultative processes, and an emphasis on primary health care with each embodying specific values and bringing unanticipated problems. 1.3.1 Three generations of health system reform Traditional practices and systems of promoting health have existed for thousands of years and coexist today with organised health systems in the modern sense, which have developed only over the last hundred years. The health system plays a more influential role than ever before, affecting peoples’ lives and livelihoods throughout the lifespan. Perceived failures in health and the pursuit for greater efficiency, fairness and responsiveness to people’s expectations of the health system have prompted reforms. According to Frenk (1994) the course of reform determines “the deeper meaning of the social effort to care for health….the health system can reproduce inequalities, or it can assume a leading role in offering everyone an equal opportunity to confront the challenges of life….reforms imply options” (p. 32). The 8 World Health Organisation (2000) describes three overlapping generations of health system reform beginning in the twentieth century and moving into the twenty first. 1.3.1.1 First generation health system reform The first generation of reforms saw the founding of national health care systems and the extension to middle income nations of social insurance systems, mostly in the 1940s and 1950s in richer countries, and later in poorer countries (World Health Organization, 2000). Rising costs placed stress on systems in the 1960s as the volume and intensity of hospital-based care increased in all countries. The wealthy used health services more heavily than the poor who were underserved by systems that were technically universal in coverage. The World Health Organisation (2000) reported that too many people continued to depend upon their own resources to pay for health services and could often get only ineffective or poor quality care. Indigenous populations were frequently excluded from health services. Countries like Africa, under British administration, implemented a European model of health care intended for colonial administrators and expatriates, with second class or no provision made for indigenous peoples. In New Zealand, John Hinds reported on a six year study of bronciectasis (often a consequence of pertussis) in 1958, which demonstrated a higher incidence in the indigenous Maori, “who were also less likely to receive treatment” (Dow, 1995, p. 196). This was despite the British Crown and New Zealand Maori signing the Treaty of Waitangi6, which conferred citizen rights to Maori and should have afforded some protection. In former colonies and poor countries, the health system was unable to deliver the most basic services to people in rural areas. In most wealthy countries, major urban hospitals received around two- thirds of all government health budgets and delivered care to less than 20 per cent of the population (Barnum & Kutzin, 1993). Barnum and Kutzin also contended that 50 per cent of hospital inpatient funding went on treating conditions such as diarrhoea, malaria, and tuberculosis, which could have been managed by ambulatory care. 6 The Treaty of Waitangi was signed in 1840 and provided for a transfer of sovereignty, and a confirmation of existing property rights, in addition to conferring citizen rights to Maori (Boyd & Sheridan, 2000). 9 1.3.1.2 Second generation health system reform A second generation of radical reform introduced primary health care as the route to achieving affordable universal coverage, as concerns centred on the need to make systems more cost efficient, equitable, and accessible. Newell (1975) suggests that this approach built on the experiences of disease projects in the 1940s7, and in some countries, life expectancy at birth increased up to 20 years in a span of two decades. The emphasis was placed upon “public health measures relative to clinical care, prevention relative to cure, essential drugs, and education of the community by community health workers” (World Health Organization, 2000, p. 14). Primary health care sought to bring basic health care to all people. The term ‘primary’ acquired many meanings including: first contact with the health system; first level of care; simple treatments by untrained providers; interventions acting on primary diseases, and was also associated with political activity involving multisectoral action and community involvement. This is arguably why no single model of primary health care exists. Many primary health care programmes were funded inadequately, workers did not focus on prevention and community outreach, training and equipment was insufficient, and the care was often “primitive rather than primary” (World Health Organization, 2000, p. 15). For example in India, community workers were placed in over 100,000 health posts to deliver basic primary health care to two-thirds of the population. Primary care was better integrated into the whole system in wealthy countries. In New Zealand primary care was associated with general medical practice, and a reliance on general practitioners has remained central in current third generation reform. The second generation health reform approach, emphasised in the primary health care movement, gave too much attention to peoples’ demand for health care, instead of concentrating on their presumed needs (World Health Organization, 2000). Systems fail when these two concepts do not match, because the supply of services cannot align with both demand and need. Poverty is one of a number of reasons that needs 7 These countries included “South Africa, the Islamic Republic of Iran, and former Yugoslavia…also built on the successes and experiments of China, Cuba, Guatemala, Indonesia, Niger, the United Republic of Tanzania, and Maharashtra State in India” (World Health Organization, 2000, p. 14). 10 may not be expressed in demand. Both first generation and second generation reform have been supply-oriented. Primary health care has achieved an unprecedented degree of international consensus since the Alma Ata Conference of 1978 (Frenk, 1994), although poor organisation of programmes during the second generation of reform often led to failure. Aligned with the concept of new universalism (see p. 7), primary health care was characterised by the principle of ‘cost-effectiveness for everyone’, as opposed to all possible care for the whole population, or only the simplest and most basic care for the poor (World Health Organization, 2000). An emphasis was placed on public funding, though delivery of services could be both public and private, and rationing services was considered necessary as long as whole groups of the population were not excluded. In general, it was easier to define interventions that would benefit the poor if applied to the whole population, than to assure that the poor benefited, or that most of the beneficiaries were poor (World Health Organization, 2000). Publicly funded health services targeted to reach the poor were more often used by the rich, and this pro-rich bias was due largely to the disproportionate use of hospital services by the well off. Gwatkin (1998, as cited in World Health Organization, 2000) argues that “the distribution of primary care is almost always more beneficial to the poor than hospital care is….the poor sometimes obtain less of the benefit of primary care than the rich” (p. 16). The poor obtain much of their personal ambulatory care from private providers. This accounts for the bulk of their use of the health system and is paid for by out-of-pocket expenditure (Berman, 2000). 1.3.1.3 Third generation health system reform Current third generation reform is responding more to demand. Efforts to improve access for the poor, and the provision of subsidies, rather than just service provision within the public sector characterise third generation reform. There is a move away from allocating providers budgets to determine ‘supposed needs’ to reforms that attempt to make the money follow the patient. Third generation reform throughout the 1990s saw a greater shift to new universalism, and an understanding that assessing needs alone does not provide a sound basis for planning and purchasing health 11 services, when the severity or priority of needs cannot be ascertained (Petrou, 1998). The political focus accompanying this bottom up approach is to establish clear indications of financial limitations, particularly in light of a potentially infinite demand for care. The World Health Organisation (2000) maintains that if services are to be provided to all, then not all services can be provided. Third generation reform has been motivated by a number of reasons (see p. 7) and includes more experimentation in approach. There has been increased reliance on the market since the 1980s, with the promotion of competition, more explicit rationing criteria, and a reduction in government regulation and control. In addition, individual choice and responsibility have been emphasised. Focusing on the commercial performance of government-owned organisations in New Zealand was balanced ahead of the millennium by the government promoting provider and community cooperation in the interests of more effective services. The new centre left government merged central agency roles, promoted local collaborative and accountability cultures, as well as community involvement in decision making through district health boards. The overarching objective was to reduce inequalities (Boyd & Sheridan, 2000). Globally, governments attempted to establish realistic expectations about what they should do with general revenues within their financial capacity (World Health Organization, 2000). These changes have impacted on health systems, and one consequence has been an increase in insurance mechanisms. In New Zealand, a country with universal coverage, over one third of the population is covered by private health insurance, “which has a history of meeting the cost of services outside the taxpayer-funded health system” (Boyd & Sheridan, 2000, p. 309). Universal health insurance has been introduced to varying degrees in the Republic of Korea, Malaysia, Singapore, and China and reforms to extend or merge insurance coverage for greater risk sharing have also occurred in Argentina, Chile, Colombia, and Mexico (World Health Organization, 2000). A mix of insurance and out-ofpocket health care has replaced much of the public system throughout the former communist countries. In New Zealand, general practitioners as gatekeepers to the health system have been made accountable for their patient’s health and resource usage when prescribing 12 interventions. This role was formalised in New Zealand through budget holding for general practitioners in Independent Practitioner Associations. Similarly in the United Kingdom, general practice fund holding occurred, and in the United States, Health Maintenance Organisations acted as the vehicle for budget holding (Wilton & Smith, 1998). In the United States, there has also been a “shift in power from providers to insurers, who now largely control the access of doctors and patients to one another” (World Health Organization, 2000, p. 17). Third generation reforms have required countries like New Zealand to rethink the demands, issues and incentives that drive health service priorities. Emphasis is being placed on population health policies to improve the health of all New Zealanders, especially the poor, as it is no longer assumed that delivering personal health services will result in population health (Marmor & Mashaw, 2001). A paradigmatic change of this nature creates tension between the medical ethics of the individual and the social ethics of the health system and population (Lamm, 1994). Participating communities, self-management, and effective primary health care are the bases of such a model. To support community knowledge and self-determination, nurses, dieticians, physiotherapists, occupational therapists, counsellors, traditional healers, community workers and clients may increasingly be included in primary health care teams. There are currently opportunities for more appropriate utilisation of nurses. Government subsidies of NZ$30 million a year for nurses who work with general practitioners were expected to better align incentives for collaborative practice (Boyd & Sheridan, 2000). Seamless care for clients entering the health care system has been identified as an important area in which to improve quality. Strengthening partnerships between providers and investing in integrated information systems were recognised first steps. At the end of the 1990s the government invested NZ$4 million on trials of health information systems to support integrated providers (Boyd & Sheridan, 2000). All major providers are currently engaged in the ongoing development of effective information systems, and leadership in this area “could ensure national standards, appropriate methods, and commonality among clinical computing systems, electronic records, and clinical messaging” (Boyd & Sheridan, p. 312), although privacy issues are a major concern. 13 1.4 Public health developments intersect generations of health reform Section 1.4 draws attention to the importance of the linkages between public health and health system reform in order to establish a context within which contemporary and future developments can be placed. Whilst cost affects the kind of health care system a country can afford, the impact of politics and culture is of no less importance (Lassey, Lassey, & Jinks, 1997). Prevailing social and economic ideology has bearing on the emphasis given to health promoting strategies, and recurrent themes in the history of public health, such as collective responsibility for health, population focus, primary prevention, and government action play an important part in the debate about health system reform. All current challenges have historical antecedents and there are many lessons for this century. Contemporary public health practice in New Zealand reflects six distinct periods of development since the time of British colonisation and settlement. The most recent era ‘new public health’, represents the contribution of the past, and also a departure from it (Baum, 1998). To track this development, six periods of public health thinking and practice are outlined separately, although in reality these are overlapping eras of practice. The six periods are: the era of indigenous control; the colonial era; the nation-building era; the era of affluence, medicine and infrastructure; the life-style era, and the era of new public health8. It is interesting that the three most recent periods of public health development are in step with the three generations of health system reform. Health reform, placed within a public health context, can be considered in relation to particular dominant policies, ideologies and typical (health) interventions. Table 1 provides a summary of this information (see p. 25). 1.4.1 Era of indigenous control (pre-colonisation) The era of indigenous control is estimated to be in excess of 700 years in New Zealand (M. King, 2004). In history, many forms of collective public health activity 8 Baum (1998) identifies these six eras in relation to public health development in Australia. These periods, along with dominant ideology and policies, and typical intervention models have been applied to public health developments in New Zealand. 14 have been identified in diverse societies (Brockington, 1975; Rosen, 1958; W. Wilkinson & Sidel, 1991). Examples include: the isolation of people with leprosy (ngerengere) by Maori in New Zealand (Buck, 1949); the regulation of prostitution in Ancient Rome and Greece, and inoculation against smallpox in India and China before the common era (Baum, 1998). Maori in New Zealand recognised the importance of healthy communities and a public health system evolved, based on values that reflected the relationship between people and the natural environment. Health for early Maori was integral to survival and therefore demanded a united approach to every-day existence. Society was communal, families lived together and the natural environment was a source of food, shelter, clothing and identity (Durie, 1998). The “underlying philosophical basis for public health was linked to a division of people, places or events as either tapu or noa” (Durie, 1998, p. 7). Tapu is a sacred state or condition in which a person, place or thing is set aside by dedication to the gods and thereby removed from common use (Marsden, 1975). Conferring tapu was a measure of protection that invoked caution and warned of danger, in contrast to noa, which implied no restriction or scarcity, but rather safety, freedom and abundance. The work of the tohunga (traditional healer)9 depended on drawing distinctions between tapu and noa and re-establishing balance between the two. The concepts tapu and noa are embodied in separating clean from unclean, replacing a dangerous situation with a safe one, and distinguishing pure water from contaminated water. These are all recognisable as public health practices. Brockington (1975) points out religions may also be seen as public health measures as they encourage sobriety, cleanliness, isolation of people with infectious disease, and ritual abstention from food likely to convey parasites. 9 Traditional Maori communities recognised two classes of leaders, rangatira and tohunga. Within both classes hereditary and ascribed roles were important, and together they covered political, spiritual, and professional dimensions. Rangatira were the political leaders, while tohunga were the professional experts in a variety of pursuits including agriculture, warfare, weaving, decorative arts, fishing, environmental conservation, and healing. From an early age tohunga were immersed in tribal ritual and tradition, and inevitably became the carriers of tribal culture, science, and technology (Durie, 1998). 15 Durie (1998) maintains there is a failure to appreciate the transcultural nature of health and the shared experiences of most tribal and urban cultures. He suggests the major differences between traditional Maori and scientific, western approaches to health, is related as much to time and to balance as to irreconcilable belief systems. The dominant ideologies of the indigenous era include strong links with land, traditional healers, an emphasis on spirituality, and the integration of health and life (Baum, 1998). 1.4.2 Colonial era (1840 to 1890) The colonial era focused public health effort on the control of infectious disease in order to create healthier environments. Whilst New Zealand was portrayed to prospective emigrants as a society free from disease, sanitation and water supply caused concern in towns and smaller settlements. New Zealand’s geographic isolation afforded the greatest protection from infectious disease coming ashore, and the vigilance of quarantine officials, and good fortune played a lesser role (Dow, 1995). New Zealand’s public health legislation was inspired by the fear of cholera (1842), smallpox (1872), plague (1900) and influenza (1920) (MacLean, 1964). Dow noted other factors, such as the impact of chronology, financial considerations, local rivalries and developments beyond New Zealand as also playing a part in public health legislation. New Zealand was significantly influenced by Britain with regard to the establishment of quarantine acts, public health acts, and the provision of clean water and sanitation. The Public Health Act of 1872 sought to organise a system of public health. Central boards of health in each province networked with local boards, before the abolition of provinces in 1876 and a new Act that required one central board to be established (Dow, 1995). The Board however, met infrequently, dealt with matters of quarantine on rare occasions, and provided little support for local boards. The result was that almost nothing was done to improve public health in the colony prior to 1900 (MacLean, 1966). 16 Colonisation saw the introduction of measles, influenza, whooping cough, typhoid, scarlet fever and mumps, which had devastating consequences for Maori who had no ‘population’ immunity. This was compounded by Maori relocating from hill top kainga and pa (settlements) to live in coastal areas where there were opportunities for trade, education and employment. As new settlements frequently lacked public health amenities such as clean water, sanitation10 and drainage, the health of Maori declined. 1.4.3 Nation-building era (1890 to 1940) Public health promoted nation-building in line with an overarching government intention to strengthen the nation, which was seen as possible by improving the health and fitness of white citizens (Powles, 1988). ‘Improving the race’ was linked to eugenics, and consistent with the notions of vitality, efficiency, purity and virtue. Powles contended that the period of nation-building was characterised by two main ideas. The first, ‘progressivism’, sought to modify the effects of capitalism, motivated by Utopian views that governments were responsible for improving peoples’ health. The second idea, ‘national efficiency’, was based on the assumption that strong nations were essential for national protection. The pursuit of a ‘pure race’ became part of the public health agenda, demonstrating the influence of dominant political and social attitudes. While the concept of nation-building was evolving, public health efforts in New Zealand in the early 1900s concentrated on poor nutrition, inadequate sanitation, tuberculosis11 and infectious diseases. Maori Councils12 developed links between Iwi (tribes) and the government, and were attributed with a 70 per cent vaccination uptake of the entire Maori population. Maori community health workers improved housing, sanitation, and water supplies until the positions were disestablished in 1909, and 10 Old hill top sites with organised sanitation were abandoned and indiscriminate defecation on the lowlands led to the pollution of pools and springs (Buck, 1949). 11 Tuberculosis was the main cause of disease in New Zealand in 1900 (Dow, 1995). 12 Maori Councils established in 1900 delivered government prevention and health promotion programmes but were unable to introduce Maori policy perspectives, limiting their ability to improve Maori health. 17 district nurses were recruited to work in Maori communities with typhoid and other acute illnesses (Dow, 1995). Despite a number of community based approaches, in 1909 the Department of Public Health amalgamated with the Department of Hospitals, and an emphasis was placed on hospital services, rather than the health of the entire population. The Tohunga Suppression Act of 1907, two years earlier, also gave a clear indication that the government intended to base health care services on solely western concepts. Smallpox, the influenza epidemic of 1918, and campaigns for cancer detection assumed priority at the end of this period. Within the third era the health of citizens became a legitimate concern of governments, who also promoted the individual’s responsibility for their own health. Raising the standard of child health assumed a priority, and the New Zealand government funded routine medical examinations of schoolchildren, and also selected ‘squads of children’ to participate in special physical exercises (Dow, 1995). Internationally, comparisons were made between the average height and weight of schoolchildren throughout the first half of the century, as improving national physique was a common priority in all wealthy countries. Accompanying this focus were interests in dental health and diet. Dow describes experimental programmes such as ‘toothbrush drill’ (schoolchildren brushed, rinsed and spat in unison), and ‘open-air schools’ (classrooms maximised fresh air and sunlight) being implemented in multiple sites. These activities benefited children in the main centres who were nearly all European. It is not surprising that the focus of public health activities differed for Maori and non-Maori/European in light of the ideology linking health to pure race. It is even less surprising that many ‘White Australians’ (and New Zealanders) believed their civilised role was to smooth the pillow of the dying race (Baum, 1998). 1.4.4 Affluence, medicine and infrastructure (1950s to early 1970s) In this post war period, economic affluence and government intervention in health, housing and education aimed to improve the quality of life of the population. Clinical medicine was associated with new technologies, such as organ transplants. This was the golden age for medicine, with finance available for medical research on the prevention of disease and illness, fuelled by the belief that medicine would 18 conquer disease. Investments in hospitals grew and health budgets expanded. The growth of medicine coincided with a period of affluence, rising living standards and life expectancy13. Consistent with first generation reforms, “a social security scheme launched in 1939 provided New Zealanders with free medicines, free hospital care, and a universal subsidy for primary care physician visits for over twenty years” (Boyd & Sheridan, 2000, p. 305). Public health developments in New Zealand were closely aligned with health care services and focused on selected diseases and technological solutions, consistent with the approaches taken in other wealthy countries during this era (Beaglehole & Bonita, 1997). Planning and constructing hospitals saw costs escalate, and the idea of ‘capping costs’ was not strongly held. Efforts to stop escalating costs included domiciliary care advocated as an alternative to hospitalisation, and the amalgamation of psychiatric and general hospitals (Dow, 1995). Dow suggests these diversionary strategies had little impact on reducing overall hospital sector costs. Maori health problems were related to under privilege at a time when most had ‘plenty’ (Dow, 1995). Maori did not receive necessary care and in many cases were excluded from care, a common experience shared by other indigenous peoples (see p. 9) and a driver for the first generation of health reform. In 1951, life expectancy at birth was 14 - 17 years less for Maori than non-Maori, and Maori infant mortality was also much higher than that of non-Maori. The incidence of preventable conditions, such as bronchiectasis was higher in Maori (see p. 9), who also suffered disproportionately from tuberculosis, after it had been largely eradicated from the non-Maori population (Dow, 1995). “By the 1960’s, public hospital waiting lists were long, and medical insurance schemes grew to help people pay for private hospital admissions, particularly for nonacute surgery” (Boyd & Sheridan, 2000, p. 305). Hospital care continued to dominate, and like other wealthy countries, New Zealand’s health costs increased more rapidly than the gross domestic product. Scepticism about the cost and promise 13 The greatest gains in life expectancy were made in an earlier period before medical therapies were available. Changes to social, economic and environmental conditions appear to have had a much greater effect on mortality rates (McKeown, 1979). 19 of medicine was growing with McKeown (1979) challenging the notion that scientific medicine was responsible for extending the average life expectancy and others describing the limits of medicine’s contribution to health (Powles, 1973). Health education gained momentum through public exhibits, print, film, public meetings, and radio broadcasts. During this period the first anti-smoking campaign was launched and nurse training transferred from hospital schools to technical institutes, making it education-based rather than service-based14. The era of affluence, medicine and infrastructure that coincided with first generation reforms, which sought to address inequalities in access to health services for the poor, failed both in New Zealand and globally. Hospital care predominated, health system costs rose as the volume of hospital care increased, and efforts to reach the poor were either non-existent or very limited. 1.4.5 Life-style era (late 1960s to mid-1980s) The life-style era saw public health developments focus on the effects of affluence, in terms of chronic disease. Highly individual, behavioural approaches to life-style diseases such as diabetes, cancer and cardiovascular disease drew almost exclusively on psychological theory15 and had little regard for individuals’ social and economic circumstances, despite an increasing awareness of the structural causes of illness. The notion of primary health care (World Health Organization, 1978) was embraced, but unfortunately, selectively applied to the management of specific diseases (see p. 3). This encouraged the view that medical interventions are the most crucial to health, usually to the detriment of other measures such as housing, sanitation, education and food production (Rifkin & Walt, 1986). Termed ‘selective primary health care’ (Walsh & Warren, 1979), this approach was criticised by advocates of a more comprehensive community development approach for not addressing the root causes of illness (Rifkin & Walt, 1986; Werner, Sanders, Weston, Babb, & Rodriguez, 1997). 14 This action was intended primarily to reduce the high withdrawal among trainee nurses, which ran at 45 per cent (Dow, 1995), to support the new technical Institute movement (M. Brown, Masters, & Smith, 1997), and to encourage a community focus (M. Horsburgh, personal communication, July 15, 2005). 15 Theories developed in this decade included the health belief model (Becker, 1974), the theory of reasoned action (Ajzen & Fishbein, 1980), social learning theory (Bandura, 1977) and in the next decade, the stages of change model (Prochaska & DiClemente, 1984). 20 Targeted national public health programmes based on behavioural theories attempted to persuade people to stop smoking, improve their nutrition, practise breast selfexamination - exercise and health were deemed the individual’s responsibility. Programmes, such as these, focusing solely on individual behaviour change were widely criticised for ignoring the lack of opportunities for people who were disadvantaged to be healthy (Crawford, 1977; J. French & Adams, 1986; Naidoo & Wills, 1994; Rodmell & Watt, 1986; Tesh, 1988; B. Tones, 1986). Disease focused associations, such as the Heart Foundation, were active in their campaigns to change risk factors and population surveys of risk factors were commonly conducted. Prevention was rediscovered in an attempt to control health costs. Economic rationalism became a central discourse in New Zealand political life. The cost of medicine was questioned as New Zealand hospitals simultaneously succeeded in gaining a larger proportion of the health budget. The cost of health care increased during the 1960s, with a comparison of spending for the years 1961 and 1972 revealing an increase of 45 per cent (Dow, 1995). Consistent with second generation reforms, attempts to make efficient use of the reduced health budget throughout the 1980s focused on the transition to a population-based formula and an emphasis on primary care, synonymous in New Zealand with general medical practice. General practitioners “function as independent, fee-for-service practitioners receiving some government subsidies” (Boyd & Sheridan, 2000, p. 305) and provide clinical care, cure relative to prevention, and essential drugs. During the life-style period ‘Maori identity’ was asserted beyond the marae and into areas such as law, medicine and education. A resurgence of interest in Maori language and culture combined with new insights into the Treaty of Waitangi as a living social document relevant to contemporary life. An important earlier report on the Department of Maori Affairs examined issues such as land, housing, and education, concluding that integration should replace the former policy of assimilation, and differences based on inequality or discrimination should be eliminated (Hunn, 1961). While these findings had direct implications for health, nearly two decade passed before State sector reform in the 1980s reactivated the formal recognition of the Treaty and its integration into health services. Health 21 became a topic for discussion on the marae, rivalling land as the central focus of Maori concern. Maori health models were developed and articulated, reaffirming spirituality as a basis for health and well-being (Durie, 1998). Statistical information on socio- economic, self-esteem and cultural factors noted a further narrowing of the gap between Maori and non-Maori health, with differences attributed in part, to the monoculturalism of health services (Pomare et al., 1995). The life-style period was not discrete, and significant developments, such as indigenous peoples’ health movements and women’s health movements, coincided, contributing to the evolution of ‘new public health’. Second generation reform overlapping the life-style era, was as unsuccessful as the first generation of reform had been in improving the health of the poor. 1.4.6 New public health (1980 to 2005 and beyond) The most recent era, new public health, is based on the Ottawa Charter (see p. 3) and seeks to direct resources into a positive approach to health, placing a greater emphasis on health promotion. Baum (1998) suggests the driving forces behind the Charter result from the limited effectiveness of the ‘health for all by the year 2000’ strategy in wealthy countries, and the limitations of the life-style and behavioural approaches, requiring a new notion for health promotion. New public health has developed strategies that are integrative, combining some elements of past strategies and new ideas. Previous eras focused on physical infrastructure in order to provide clean water and sanitation, whilst new public health complements this focus also advocating social support, and behaviour and life-styles approaches. Legislation and policy, key mechanisms in the nineteenth century were rediscovered as important tools for modern public health. Intersectoral action is recognised as crucial to success, a shift from the time when medicine had centre place. Current philosophy promotes community participation, whereas ‘experts’ drove public health during the twentieth century. New public health considers many methodologies to be legitimate, not just epidemiology and is concerned with all 22 threats to health, including chronic conditions, and the sustainability of the physical environment. This is in contrast to earlier public health concerns that focused predominantly on infectious disease. New public health has established an agenda for action and policies are influenced by notions of poverty and social justice (Baum, 1998). The Healthy Cities programme in 1986 (J. Ashton, 1992; Tsouros, 1995) was a collaboration between different sectors of government and communities to create an environment conducive to good health. This early initiative saw cities as the units for public health planning, rather than individuals. Healthy cities varied between and within countries, although common aims included: promoting equity and reducing inequities in health status; recognising the importance of the determinants of health; fostering intersectoral collaboration; aligning with new public health thinking; partnering with community, and encouraging innovation. The healthy cities programme attempted to tackle complex public health issues at city, community and regional levels. Baum (1993) maintained that by focusing on individual cities, wider social, economic and political factors were ignored. Whilst this criticism may be justified, the healthy cities programme was an innovative experiment that led the healthy settings approach, which saw hospitals, schools and workplaces become centres for health promotion. The importance of policy as a tool of public health was agreed at the second international health promotion conference where the theme was healthy public policy. The purpose of healthy public policy is to create the preconditions for healthy living through: closing the health gap between social groups and between nations; broadening the choices of people to make the healthy choice the easier and most possible, and ensuring supportive social environments (Mahler, 1988). Implementing primary health care policy in New Zealand is necessary, partly because the community care sector has long been neglected, and policies of de-institutionalisation and changes to hospital procedures (day surgery, shorter average lengths of stay) have increased the demand for care in the community. New Zealand does not have a universal primary medical care system free at the point of use, and this circumstance 23 led to the development of third sector16 primary care (Crampton, Dowell, & Woodward, 2001). Successive governments have sought to improve access to primary medical care for low-income families by manipulating the primary care subsidy scheme, and attempts to limit the amount charged by general practitioners have failed (M. Brown & Crampton, 1997; Health Benefits Review, 1986). Experimental funding mechanisms such as capitation and budget-holding sought to increase control over demand-driven expenditure in the early 1990s (Malcolm & Shalowitz, 1997). Third sector primary care organisations - union health clinics, tribally based Maori health providers, and community-based primary care providers, established a formal network in 1994, Health Care Aotearoa, to serve populations that were largely non-European and lived in deprived areas. Population approaches to funding and service provision were consistent with the intention of integrated care (see p. 106), whereas projects in the late 1990s targeted defined populations, for example with chronic conditions. Since 2001 primary health organisations comprising collective groups of general practices and other primary care providers have sought to deliver population-based services to enrolled populations. Opportunities exist for primary health organisations to work in innovative ways with consumers to address inequalities in health and health care service provision. The linking of national strategies provides the opportunity for New Zealand public health to become more innovative, as patchy innovation has been evident throughout developments in community health. The Primary Health Care Strategy (PHC Strategy) seeks to tackle inequalities in health and emphasises population health, the role of community, health promotion, and preventive care. However, the continued reliance on goals and targets and measurable health outcomes as a means of monitoring (forcing a focus on disease), and the investment in general practice rather than broader primary health care services, strongly suggest a continued medical and behavioural focus. In New Zealand the debate between selective and comprehensive primary health care approaches mirrors that of other wealthy countries (Baum & Saunders, 1995). 16 The term third sector has been adopted internationally to describe organisations that are nongovernment and non-profit. 24 Table 1: New Zealand public health developments and health reforms Era Dominant policies and ideologies Typical intervention model Era of indigenous control (estimated in excess of 700 years ) Strong links with land, traditional healers, emphasis on spirituality and health was integral to life. Maori public health concepts – tapu and noa Public health practice was part of accepted culture, Maori knowledge was transferred through oral tradition. Tohunga protected Iwi survival. Colonial era (1840 to 1890s) Control of infectious disease, public health was strongly influenced by British settlers. Emphasis on sanitation. Maori re-settlement saw increased illness/death Quarantine Acts. Public Health Acts in colonies. Provision of clean water and sanitation. Nation-building era (1890 to 1940) Government action to strengthen the nation through health and fitness ‘Improve the (white) race’. Health linked to ideas of vitality, efficiency, purity and virtue. The focus was national protection and progress Medical inspections and organised exercise programmes aimed to improve the national physique of schoolchildren. Maori health received limited attention. Hygiene advice was given to the population Economic affluence sees governments committed to improving quality of life (post war). Investment in clinical medicine aligned with the belief ‘medicine would conquer disease’ Government involved in housing, education, and health. Hospitals and budgets expand. First organ transplant. Public health is linked to health services and disease prevention Affluence, medicine, and infrastructure (1950 to early 1970s) Life-style era (late 1960s to mid-1980) New Public Health era (1980 to 2005 and beyond) Chronic disease focus – effects of affluence. Economic rationalism. Individual responsibility. Epidemiological methods. Assertion of Maori identity in the professions, health models are developed Selective primary health care – illness causes not addressed. Individual behavioural approaches to care. Life-style projects. Population surveys. Treaty of Waitangi impacts health system Ottawa Charter: collective action; healthy public policy, and health promotion. Issues of poverty, social justice, equity, effect policies. Market economies, competition, reduced government expenditure Healthy public policy – ie. smoking legislation. Innovative healthy cities approach. Intersectoral action with community participation. Creating supportive social and physical environments Generation of health reform st 1 generation 1940s to 1950s Health care to the underserved/poor (indigenous/Maori) Hospital care had a pro-rich bias. In New Zealand free hospital care, medicines, subsidies for all nd 2 generation 1960s to 1980s Primary health care strategy sought to bring basic health care to all people. Supply-driven rd 3 generation 1980 and beyond Demand-driven. Better access, services/subsidies. Experimentation. Less regulation by government. Interest in health insurance mechanisms 25 It is ironic that during the new public health era, the World Health Organisation was advocating a broader agenda for public health, and simultaneously promoting a methodology that was essentially reductionist. The mismatch of philosophy and strategy (the broad social, economic and environmental agenda set by the Ottawa Charter) and the mechanism to achieve this mismatch (mainly behavioural and medically defined goals and targets) encapsulated the tensions and forces within public health itself. Medicine and epidemiology were, and remain, dominant professional groupings within public health, and the approaches of these groups dealt best with the behavioural and medical aspects. Third generation reform has not yet demonstrated sustainable improvement in the health and well-being of the poor. However, as this generation of reform continues, both the challenge and opportunity to improve population health through advocating health promotion exist. Chapter two introduces health promotion theory in order to shed light on the ways in which public health can be improved. “Health and its promotion…(must be) built into the consciousness of the public and professionals in order that change and improvement can be continually effected” (Downie et al., 1990, p. vi). The following chapter proposes that health promotion should be considered an important and crucial element of contemporary public health. As health promotion has acquired many meanings, Beattie’s model of health promotion (Beattie, 1991)17 provides a useful framework to explore underlying values. 17 Beattie’s model also provides a framework for analysing the NICPS results that determine the health promotion values embedded within nurses’ practice (see p. 192, chapter seven). 26 2 Chapter 2 Health promotion theory 2.1 Introduction Section 2.1 explicates a central model of health promotion from a variety of others, establishing the theoretical perspective for the study (see p. 127). Health promotion theory is discussed in a separate chapter to distinguish it from other public health literature, although it is clearly a logical extension of the former discussion. This approach also isolates health promotion theory from other components of the research process enabling the reader to better identify and understand the theory base and its use in the thesis research, the ‘Nurses in integrated care projects study’ (NICPS). Attempts to conceptualise health promotion have given rise to a range of different models and approaches. For the purpose of this thesis, health promotion is defined as any activity that encourages health (B. Tones, 1986) including chronic care management. Although Tones and Tilford (1994) have more recently suggested health promotion is health education and healthy public policy, and taken account of the concept of empowerment, the earlier definition is less bounded and therefore allows for a wider range of possible activities. The inclusion of chronic condition management, with its emphasis on disease reduction, prevention and health protection to maximise positive health, as an adjustment to this definition is becoming less contentious. The continuing debate over territory, challenging the nature of health promotion activities, is a feature of the history of health promotion. French (1990) has questioned why disease management should not be included, whereas Downie et al. (1990) explicitly removed curative and acute services from definitions of health promotion. Chapter 2 is presented in four parts. First, section 2.2 health promotion and nursing, is briefly discussed to establish a context for the professions’ approach to health promotion practice. Beattie’s model of health promotion is then described, and other models and related conceptions of health promotion are compared and contrasted in sections 2.3 and 2.4, respectively. Beattie’s model provides the framework for the analysis of study results in order to identify the health promotion values embedded 27 within nurses’ practice in section 2.5. Finally, summary comments draw together the central and related ideas expressed in chapters one and two. 2.2 Health promotion and nursing Health promotion is a contested area. This is partly because it is a very broad field of action, its focus has changed over time, and terms used such as ‘health education’ and ‘health promotion’ have shifted their meaning. There is no easy consensus about the ideas that underpin health promotion and protagonists hold very different views about priorities and strategies, which reflect their underlying values (Downie et al., 1990; J. French, 1990; J. French & Adams, 1986; B. Tones, 1986; K. Tones & Tilford, 1994). Nursing as a profession has contributed to the individualisation of health, views the client as a victim of his or her behaviour, and “encourages a form of health promotion which focuses on the individual and ignores or decontexualizes social problems” (Caraher, 1994, p. 465). Attempts to link health with structural or social issues were met with resounding disapproval in the 1980s (Beattie, 1991) at a time when health status focused on individuals and their beliefs (W. Rogers, 1991). Caraher (1994) pointed out that “viewing the individual as the focus of interventions is not in itself an inappropriate approach, depending on the context within which this happens” (p. 466). However, if the focus is solely on the individual and their behaviour it can lead to ‘victim-blaming’ (Crawford, 1977). Even within a health-promoting environment, which attempts to make healthy choices easier (World Health Organization, 1985) victim blaming can occur and people may choose to behave in ways determined as unhealthy. Hamilton and Bhatti (1996) maintain a population health promotion model that calls for action on the full range of factors that determine health shifts the focus away from victim blaming individuals. The way health is viewed influences the interventions undertaken. Factors causing disease, such as germs, were considered external to the individual and treated with antibiotics. The emphasis has moved towards individuals taking control over health and disease, “now, the healthful behaviour is the accepted standard and the unhealthful behaviour [excessive drinking and smoking] is socially 28 deviant….concepts about health, physical fitness, and personal responsibility have been fused with popular culture” (Guidotti, 1989, p. 402). The focus on individuals having control of their health, as opposed to social and economic factors, individualised the problem and poverty for example, became an issue individuals had to manage. This is given further emphasis by the claims of nursing to a health promotion capability. As Beattie (1991) contended The established and mainstream professions have become increasingly interested and involved in health promotion at a time when independently of one another, each of the professions has been vigorously examining and seeking to consolidate their own knowledge base, their definitions of professional competence…(p. 185). The nursing profession engaged in the development of individual practitioner’s skills, initially focusing on communication for the purpose of health teaching (Beattie, 1990; Coutts & Hardy, 1985; Gott & O'Brien, 1990). This proved to have limited effectiveness because nurses could advise, inform, and direct, but changing a client’s behaviour was something only the client could do. This realisation resulted in a shift to personal counselling as a more effective method of achieving health behaviour change (Wilson-Barnett, 1988). Personal counselling, like health persuasion, focuses on the individual and encourages them to be responsible for their own health. Nurses and other health professionals continue to use the strategies of health persuasion and personal counselling in efforts to encourage individuals to change their life-styles. Caraher (1994) contends “links between health and social structure are relegated to a position of areas we must use in targeting groups in society” (p. 467) with groups often deemed vulnerable to their own behaviour and not vulnerable to social and structural elements, such as occupation, social class and income. Any personal counselling intervention by nurses that teaches individuals to cope with their circumstances and to accept structural limitations can create victims and in itself can be a cause of ill health. Increasingly the social and economic determinants of health are identified in New Zealand national strategies as areas of focus in the interests of improving population health (Ministry of Health, 2001c). There is a strong argument that it will prove 29 difficult to advance health promotion practice unless an understanding of how broader social, political and cultural values are developed and this knowledge is translated into health promotion practice. For this reason Beattie’s model of health promotion was selected to make explicit the values in nurses’ practice when employed in integrated care projects (see p. 194, chapter seven). 2.3 Beattie’s model of health promotion Beattie’s analytical model of health promotion allows the foundation for practice to be investigated. By making explicit the links between core values and different practices a greater understanding of the philosophy and priorities of health promotion can be derived (Naidoo & Wills, 1994). Beattie’s model is not bounded by current practice and can describe a vision of health promotion practice not yet in operation. In this sense, theory may drive practice leading to new discoveries. Adapted from an earlier framework (Beattie, 1986), the dimensions of the crossclassification are adapted in figure 1 to examine the theoretical underpinnings of health promotion (Beattie, 1991). Beattie’s model is explicit in saying that health promotion is embedded within wider social and cultural practices, in ideologies and political struggles that include power, control, autonomy and authority. Various accounts of health promotion are positioned within a broad socio-cultural dimension, making this the most important feature of the model. Beattie’s model provides a range of approaches that may comprise an intervention: health persuasion, a traditional health education practice; personal counselling where individuals are assisted to find solutions to their health issues; legislative action, which develops activities to protect the public’s health, and community development, enabling groups of people to identify and meet their needs through education, support, or services. The specific approach to an intervention depends upon “bipolar dimensions namely ‘mode of intervention’ and ‘focus of intervention” (Beattie, 1991, p. 167) that invoke two well-known and established dichotomies in the analysis of social policy. 30 Figure 1: Beattie’s model of health promotion From “Knowledge and control in health promotion: A test case for social policy and social theory” by A. Beattie, 1991, p.162-202. In The Sociology of the Health Service. Chapter 7. Eds J. Gabe, M. Calnan, and M. Bury. Copyright 1991 by Routledge: London. Reprinted with permission of the author. Mode of intervention results from views about power and control. The authoritative mode is characterised by ‘top-down’ forms of interventions, led by experts who encourage individuals or communities to adopt behaviours perceived as good for them reflecting paternalism and prescription. This versus the negotiated mode characterised by ‘bottom-up’ forms reflecting participation, where health workers act as facilitators and people themselves lead, identifying their own needs. Beattie (1986; 1991) among others (Hardy, 1981; Room, 1979), has shown how top down and bottom up health interventions come to be polarised by degrees within the authority/negotiation dimension. Focus of intervention results from views about the causes of ill health, improving the health of individuals versus the health of communities or entire populations. “The individual/collective dimension stands in its own right as one of the most stable and enduring axes of conflict in social theory and social policy” (Taylor-Gooby & Dale, 1981, p. 168). 31 2.3.1 Health persuasion Beattie’s model assists us to reflect upon the social and political perspective underlying health promotion approaches and to recognise related social values. The ‘conservative’ model of health persuasion, for example, is based on a bio-pathological model of health. Health persuasion “has long historical roots, including temperance campaigns in the nineteenth century, anti-venereal disease propaganda at the time of the 1914 - 18 war and better-eating campaigns on the ‘home front’ during the 1939-45 war” (Beattie, 1991, p. 168). The strategy is associated with clinical preventative medicine, individual subjects, and a system of care primarily concerned with illness views health promotion as attempting to repair weaknesses or deficits and solve problems. The health persuasion strategy relates to individual responsibility, topdown authority by a health professional or outside agent and has been described by Crawford (1977) as paternalistic, favouring a culture of victim blaming. The health persuasion strategy has reinforced the idea of risk factors to health and “concepts about health, physical fitness, and personal responsibility have been fused with popular culture, so that the message is continually reinforced by peer pressure, advertising and the approval of the medical community” (Guidotti, 1989, p. 402). On the surface this social intervention appears straightforward to plan, such as a review of medical literature about the risks related to behaviour before delivering a message targeting a specific audience using selected media. However, the effectiveness of the health persuasion strategy has repeatedly been shown to be unsuccessful on its own in bringing about life-style changes (Gatherer, Parfit, Partner, & Vessey, 1979). Beattie (1991) contends “the dubious and discredited strategy of health persuasion regularly finds enthusiastic champions in Parliament” (p. 170) suggesting that many in governmental positions with power have ignored the lack of scientific justification for health persuasion campaigns and have even suppressed evidence of ineffectiveness. Gradually new knowledge has led to personal counselling being considered a more effective way of working with individuals to change their behaviour (Beattie, 1990; 1991; K. Tones, Tilford, & Robinson, 1990; Wilson-Barnett, 1988). 32 2.3.2 Personal counselling The realisation that bio-medicine with its emphasis on treatment and care was labourintensive and high cost led to an increased interest in an approach that persuaded individuals to change their life-styles (Guidotti, 1989). Personal counselling adopted counselling, group-work techniques and personal development programmes for the purpose of health promotion. The theories and models associated with this work have their origins in psychodynamic and post-Freudian humanistic psychology and social psychology, emerging within the context of the mental health movement. This strategy was apparent in biographical medicine within psychiatry, general practice, psychiatric nursing (D. Armstrong, 1979); pupil-centred education in schools and subsequently in personal tutoring (Walkerdine, 1984), and individual case work among social workers, probation officers, marriage guidance counsellors, hospital chaplains and other therapists (A. Campbell, 1984). Like health persuasion, the focus is on the individual, but in this situation does not necessarily imply paternalism. Personal counselling is client-led, relies on the health worker acting as a facilitator rather than an expert, and involves creating autonomy so that the client can make informed choices. The central precept in much personal counselling is ‘self-empowerment’ and the nondirective and client-orientation of the process is valued by its proponents (C. Rogers, 1969). Blackham (1978) suggests clients favour this strategy because it promises personal autonomy and self-determination. Criticisms of personal counselling include: the invasion of a private domain; professionals not expert in techniques (Halmos, 1965); emphasis on self-conscious verbalisation and disclosure; futureoriented life planning; the premium placed on middle-class values, potentially creating problems of access for the client who is poor (Bernstein & Henderson, 1974), and raising hopes which cannot be met within the present context of the client’s life (Radical Therapist-Rough Times Collective, 1974). Beattie (1991) argues the “emphasis is clearly and almost exclusively on helping individuals to learn to cope (rather than to change their circumstances)” (p. 175) and in this respect does not escape the charge of victim blaming (Pattison, 2000; Pearson, 1973). Both health persuasion and personal counselling approaches to health promotion place the 33 responsibility on the individual, and the health professional is not held accountable for any subsequent outcome. 2.3.3 Legislative action The social change approach of Ewles and Simnett (2003) assumes a concomitant philosophy of collective (or community) action, whilst Beattie’s model demonstrates that collective action can be participative and community-based or paternalistic and state directed. Beattie’s framework for analysis helps to tease out some of the complexities underlying health action. Legislative action seeks to direct behaviour towards achieving health at a macro-level using a top-down process to improve health. This strategy has a lengthy history, which includes environmental interventions, such as clean water, sanitation, improved diet, and better housing (Beattie, 1991), air pollution legislation (Scarrow, 1972), seat belt regulation, and smoke-free legislation in public places. Improving health by enforcing legislation has been argued with increasing force (Doyal & Pennell, 1979; Draper, Best, & Dennis, 1977; Kennedy, 1983) and recent evidence of the growing social and economic inequalities in health support this case (National Health Committee, 1998). Garside (1987) argued the need to understand the cultural and ethical issues related to legislative action, pointing out the “dangers of ‘collectivist authoritarianism’ in social reform focused too exclusively on health itself (as against ‘the problems of the community at large’)” (p. 173), an issue of no less importance today. Legislative action is a strategy led by professionals, intended to protect communities. This topdown approach, however, may be viewed as inappropriate or irrelevant by communities because of the limited or non-existent input they have had into processes that determine health promotion interventions directed at them. 2.3.4 Community development Community development is a more recent health promotion strategy that has been termed self-help health, community-oriented health education, health outreach, and community health action (Somerville, 1984). Like personal counselling, it has 34 emerged in different contexts with some similarities of ideas, such as selforganisation, mutual assistance within the group, and expertise external to the group being a less urgent requirement (Beattie, 1986). Groups form to discuss common concerns, establish mutual issues, clarify options and work collectively. Underlying a community development strategy are assumptions about empowerment, equity and the mobilisation of communities to work together to change their environment using a bottom-up process. The concept of empowerment in health promotion began with the emergence of the community health movement, which tried to stem the flow of authoritarianism and individualism that had come to dominate the political agenda (Beattie, 1991). The World Health Organisation (1986) acknowledged that health developments in communities should not only be developed for the people, but rather by the people. Tones (1990) and others (Hamilton & Bhatti, 1996) argue that if root causes of ill health are not addressed, an individually-oriented approach leading to victim blaming may occur. The role of the health worker in community development may include: identifying potential groups through community surveys or consultation processes; facilitating a group coming together; assisting the process of debate; mobilising community resources; linking the group with key people in positions of power; advocating for the group to wider audiences, and networking to bring the group together with others who can act as resources (Chaplin & Adams, 1986; Laverack, 2005). Beattie (1991) suggests community development has often been misunderstood as a way of getting prescribed health agendas and messages to groups considered hard-to-reach (health persuasion) through health and welfare services (personal counselling), made available at the local level (legislative action). In such a context, community development is assimilated into another health promotion strategy and that has assumed priority. Community development has an explicit purpose, to bring about social and political change, and can be supported by partnerships with health workers. John Raeburn (personal communication, April 30, 2003) suggests it is necessary for health workers, such as nurses, involved in community development to be able to make distinctions between the different models of partnership, a requirement for community 35 development. For example, a community involvement model is applied when the nurse determines the agenda and attempts to get the community on side, a community participation model is applied when the nurse gives the major role of the programmes design and implementation to the community but remains in control, and a community controlled action model is applied when the nurse acts as a guide and educator of community members who learn skills to undertake their own (health promotion) programme. Community controlled action is concerned with empowerment and can “support the community in the identification of issues that are important and relevant to their lives” (Laverack & Labonte, 2000, p. 256). Laverack & Labonte view community empowerment as more than a means to an end of health behaviour change, and recommend the goals of community empowerment are considered in parallel to the goals of top-down18 health promotion programmes. This idea prevents the assimilation of community empowerment into other health promotion agendas, by clarifying the criteria for its attainment. Programmes negotiated with well established communities may require a commitment of only six to 12 months, whilst nonestablished communities have been reported as taking no less than two years and up to seven years to develop (Raeburn, 1996). According to Laverack and Labonte “too short a programme time frame runs the real risk of initiating healthy community changes, only to end before such changes have reached some degree of sustainability” (p. 258). Examples of community development programmes designed and managed in negotiation with communities range from anti-poverty or housing development programmes to community gardens, and advocacy support (Labonte, 1996). 2.3.5 Beattie’s model: Health promotion values in practice Foucault (2002) recognised the importance of trying to understand the relationship between values (ways of thinking) and practice (ways of doing). Beattie’s model enables practitioners to identify the values and assumptions underlying different 18 Top-down programmes are conventional, solve a problem or deficit, focus on individual responsibility, are controlled by an outside agency and have low community ownership (Laverack & Labonte, 2000). 36 forms of practice and to assess practice from the point of view of others, such as policy makers and clients. Health professionals, including nurses, are influenced by socialisation into a family, a social class, a cultural group, and through values developed in professional training and experience. If for example, nurses’ values are not congruent with their professional role, or interventions overlap quadrants, the model may reveal only some of the formulation. However, as Beattie’s model is abstract and highly complex, it is anticipated that changing social values will be identified in the analysis of health promotion practice. 2.4 Health promotion: Social theories and models Health promotion has come to refer to a movement that challenged the medicalisation of health, stressing the importance of socio-environmental aspects to health and wellbeing. The theoretical base was derived principally from social and philosophic theory, with other contributions from the behavioural and educational sciences, epidemiology and clinical practice. In this section, social theories are outlined and links are drawn to behavioural psychology and education, amongst other disciplines. Health education and more comprehensive health promotion models are discussed as descriptive or analytical, and compared in relation to Beattie’s model. 2.4.1 Social theories Health promotion has drawn on perspectives found in sociology and social policy (Bunton, 1992), adopting a structural analysis that focuses on the physical and social influences, including relationships, that impact health and inequalities in health (Townsend, Phillimore, & Beattie, 1988). The social change or healthy public policy approach, synonymous with the period of new public health, owes much to a political economy analysis of how ill health is generated by poverty, poor housing and work environments, pollution, discrimination and unemployment (Doyal & Pennell, 1979). Health promotion has also adopted a post-modern notion of fragmentation, in the sense that it has attacked the objective, science-driven model of medicine and 37 embraced the diversity of lay accounts of health, subjectivity, social movements, community action and empowerment (Kelly & Charlton, 1995). Social policy has provided analytical frameworks for thinking about policy-making and policy-change. Examining shifts in policies for health, and wider political ideologies such as New Right perspectives on the sovereign consumer helps to explain recent shifts in health promotion. Other theories and models adopted by health promotion from social psychology and education include: locus of control; reasoned action; health belief, and behavioural change (Ajzen & Fishbein, 1980; Becker, 1974; Prochaska & DiClemente, 1984; Rotter, 1966). Sociologists have argued that health promotion, embedded in contemporary society, emerged as a persuasive discourse about risk, change, life-style and consumption, and its messages reflect fundamental shifts in the ways of seeing and practising health care. For example in India, rapid social change has led to an expanding human immunodeficiency viral epidemic (J. Armstrong, 1995). This is an important justification for developing analytic models such as Beattie’s model of health promotion that attempt to represent the tensions and oppositions by demonstrating the ways in which health promotion is embedded in wider social and cultural practices and political struggles. 2.4.2 Models of health education and health promotion Health education was a central health promotion activity undertaken in the 1980s and models proliferated, although there was no consensus on core activities (Downie et al., 1990). Health education activities, such as teaching attitude and behaviour change, informing and educating people about health issues, and empowering clients to set their own agendas, were undertaken alongside medical interventions that persuaded people to seek early treatment and approaches focused on changing the physical and social environment (Ewles & Simnett, 2003). The different approaches had distinctive priorities and reflected different views of clients. Unlike Beattie’s model these frameworks did not demonstrate what motivated health professionals to select one approach over another, and could only describe current practice. Descriptive models of health education and promotion activities can highlight issues, 38 but do not provide reliable models of real practice, and are not necessarily transferable to other settings. Describing how health promotion occurs rather than analysing the values and conflicts that underpin it does little to help practitioners reflect upon the approaches they adopt within their practice. French and Adams (1986), in contrast to Ewles and Simnet (2003) identified collective action, self-empowerment and behaviour change, as social values underpinning different approaches. Like Beattie (1991) others identified collective action and empowerment as effective and desirable concepts in health promotion (J. French & Adams, 1986; K. Tones & Tilford, 1994), proposing that through health education, communities and health professional bodies could influence public policy to address health inequalities and improve health (K. Tones & Tilford, 1994). Downie et al. (1990) identified traditional, transitional and modern approaches to health education. The first two approaches do not address positive health, life skills, self-esteem, participation, constraints to freedom of choice and collective dimensions of health and behaviour. In the modern or contemporary approach, health promotion work does not focus on prevention and disease reduction or on structural and social change, exclusively. Instead, this model offers combinations of approaches, and when compared to Beattie’s model does not make explicit the political or social values underlying each approach, or reveal the author’s preferences as to methods. Other models have attempted to link health promotion to social and political structures and to frameworks of social knowledge. Caplan and Holland plotted theories of knowing (conflict or consensual) against ways of knowing about the social world (subjective or objective) (Caplan, 1993). Collins (1993) has attempted to link a micro model of a person’s health beliefs, constraints and actions to a macro model, which analyses health promotion at a societal level. Like Beattie, these authors agree that when practitioners do not make their assumptions explicit they have not acknowledged the political nature of health promotion practice. Beattie’s definitive model assists the reflective practitioner to go beyond description to analysis (Schon, 1983). 39 The health promotion models discussed are not mutually exclusive, and being either descriptive or analytical, can demonstrate diversity and its potential conflicts. Diversity may be, but is not always, explained by trends and changing ideas over time. Conversely there are considerable differences between an approach based on bottom-up negotiation, one that utilises a regulatory framework and legislative changes, and one that relies on professional dominance. The increasing development of analytical models in health promotion suggests a greater awareness of the importance of making explicit the values within the society in which health promotion is undertaken. Models such as these present new possibilities for improving practice and provide opportunities to review ideas and actions. However, it is interesting that older, seminal work by Beattie (1991) is more relevant for the contemporary analysis of nurses’ practice than other models developed more recently. 2.5 Beattie’s model: An analytic framework for use in the NICPS Section 2.5 presents Beattie’s model of health promotion as a framework to both understand health promotion and analyse health promotion values within practice. Downie et al. (1990) argue health promotion reflects the values of society, which must be widely shared for the continuance of that society. Beattie’s model is firmly oriented towards advancing health promotion practice because it makes explicit the assumptions within the society (or profession) in which activities are undertaken. Of the health promotion models and theories that have been more generally discussed (see section 2.4), none provide the broad theoretical perspective that allows systematic analysis, as Beattie’s does. For this reason, Beattie’s model was adopted to investigate the health promotion interventions undertaken by nurses in integrated care projects (see p. 160). Alongside the investigation of types of investigations such as case management, there was a place for a more theoretical inquiry into the health promotion (social) values embedded within this practice. Beattie’s model, because of its cross-classification matrices is a highly suitable tool for such an analysis. The consensus values of health promotion within the era of new public health (see section 1.4.6) are represented in the model, as are the principles of primary health care (see p. xiv). The analysis of 40 interventions undertaken by nurses, using Beattie’s model will establish whether these values and principles are embedded within nurses’ actual practice. In addition, because the model is conceptual and therefore not bounded by existing practice, desired values for future primary health care nursing can be contemplated and in this sense, theory may transform contemporary practice leading to new discoveries. 2.6 In conclusion This chapter has shown that all current challenges have historical antecedents. Consideration of history, crucial philosophies, and practices that have been representative of public health are important in assisting an understanding of contemporary public health. New public health has been described as both a continuation of the past and a departure from it (Baum, 1998). The claim to be ‘new’ derives from having pulled together numerous, diverse movements into a cohesive whole that has the potential to radically define the future direction of public health. Combining many methodologies has also served to make health promotion, a key strategy of public health, a legitimate and respectable part of the wider health scene. Commentators like Alan Beattie have sought to develop models of health promotion that portray the differing philosophies embedded within understandings of what health is, and how health can be best promoted. Beattie’s classic model has made explicit the theoretical propositions embodied in public health practice, which can be assessed in any health system context. Beaglehole and Bonita (1997), among other observers of the historical and contemporary health system in New Zealand, agree that more emphasis should be placed on public health and primary health care activities. There is practically no disagreement in the literature on this view, yet achieving it is proving difficult in the face of an intransigently curative health system. Since the millennium, New Zealand has advocated primary health care as a central approach underpinning health reform. National strategies, restructuring, and an accompanying investment in the health workforce herald fundamental change in the culture of the health system. Even though in many countries public health practice has been reduced to a series of specific interventions far removed from the broad social movements that historically 41 have had the greatest effect on the public’s health, rethinking health promotion and primary health care has been apparent in all three generations of reform. Decreased interest in the broader agenda established by the Ottawa Charter is partially a consequence of a tight fiscal environment, and a return to the earlier core business of ‘curing people’. Cost containment is clearly a key motivation of third generation reform. The resources devoted by government to public health services in all countries are only a fraction of those spent on medical care, whilst the costs of medical care inspired by technological developments, the ageing population, and epidemics of non-communicable diseases (Evans & Stoddart, 1990) are the critical concern of governments. These issues are outlined in the next chapter, which discusses the pressure on health systems to respond to the global burden of disease, caused by an escalation of chronic conditions. 42 3 Chapter 3 Chronic Conditions 3.1 Introduction Most New Zealanders now die from chronic conditions, which are increasing globally. People are living longer with chronic illnesses and with more complex comorbidities (National Health Committee, 2005). Unhealthy life-style choices such as tobacco and excessive alcohol consumption, physical inactivity, and unhealthy nutrition are known risk factors for heart disease, diabetes, and stroke (cerebrovascular disease). By 2020 chronic conditions will be the leading cause of disability throughout the world and the most expensive problems faced by health care systems (World Health Organization, 2002a). At present, health care systems around the world are organised to provide acute illness care, despite the global disease burden having shifted towards chronic conditions. Health care services are fragmented, focus on acute and emergent symptoms, and often provide care without the benefit of complete clinical information. The client’s role in management is not emphasised, follow-up care can be sporadic, and community services tend to be ignored. There is pressure on all health systems to develop a response to the escalation of chronic conditions, which has grown as a result of demographic transitions and ageing, changing life-styles, consumption patterns and urbanisation (World Health Organization, 2002a). Action taken today can prevent and reduce the leading risks to health and avoid the burden of disease in future decades. The purpose of this chapter is threefold. Section 3.2 presents the challenge chronic conditions pose to countries from a health and economic standpoint, the reasons for this rapid growth, and the bi-directional relationship between chronic conditions and poverty. Section 3.3 considers the deficits in the New Zealand acute health care system when faced with managing chronic conditions, and introduces the ‘Chronic Care Model’, as a blueprint for a more comprehensive system of care. Section 3.4 outlines the risks to health and discusses risk prevention. Actions to lower the burden of disease, the role of government’s in tackling major risks, and promoting health are identified. 43 3.2 Chronic conditions challenge the health care system The importance of chronic conditions to the health of society has been of international concern since the 1940s (Commission on Chronic Illness, 1957) and primary prevention in chronic condition management was emphasised in the 1970’s (Benjamin & Newcomer, 1997). Chronic conditions are persistent health problems that never completely resolve and require differing degrees of health care management over time. Considered from this perspective, chronic conditions cover a wide spectrum of different health concerns. Persistent communicable (e.g., human immunodeficiency virus (HIV) / acquired immunodeficiency syndrome (AIDS) and tuberculosis (TB)) and non-communicable (e.g., cardiovascular disease, cancer and diabetes) diseases, specific mental disorders (e.g., depression and schizophrenia), and ongoing impairments in structure (e.g., amputations, blindness and joint disorders) are defined as chronic conditions (World Health Organization, 2002a). Persistent pain problems are also included within the chronic conditions category. Chronic conditions can be effectively managed for years, may be more severe at times, and require life-style changes. No longer considered in isolation, similar management strategies are effective across chronic conditions. Non-communicable conditions accounted for almost three-quarters (32 million) of the deaths among adults aged 15 years and over in 2002, nearly four times the number of deaths caused by communicable disease and maternal, perinatal and nutrition conditions combined (8.2 million, or 18% of all causes) (World Health Organization, 2003). Non-communicable diseases kill nine out of 10 people in wealthy countries compared with poor countries like Africa, where approximately one in three adult deaths result. In Latin America, Asia, and the Western Pacific Region three in four deaths are caused by non-communicable disease, “reflecting the relatively advanced stage of the epidemiological transition achieved in these populations and the emergence of the double burden of disease” (World Health Organization, 2003, p. 13). The burden of non-communicable diseases is increasing and accounts for almost half of the global burden of disease (all ages), a 10 per cent increase from estimated levels in 1990. The proportion of burden from non-communicable diseases in wealthy 44 countries remains stable at over 80 per cent in adults aged 15 years and over, while in middle-income countries it has already exceeded 70 per cent, and in poor countries almost 50 per cent of the adult disease burden is now attributable to noncommunicable diseases. Cardiovascular diseases account for 13 per cent of the disease burden among adults over 15 years of age. The two leading causes of mortality and disease burden among older adults (over age 60) are ischaemic heart disease and stroke. These two diseases are responsible for 36 per cent of all deaths in wealthy countries (World Health Organization, 2003). “Ischaemic heart disease and stroke…are two of the three leading causes of burden of disease in adult males globally. HIV/AIDS is the leading cause for males and the second leading cause for females, accounting for around 6% of the global burden of disease. Unipolar depressive disorders are the leading cause of burden for females, reflecting their higher prevalence in women” (World Health Organization, 2003, p. 14). Of the 7.1 million cancer deaths estimated to have occurred in 2002, 17 per cent were attributable to lung cancer alone and of these, three-quarters occurred among men (Shibuya, Mathers, Boschi-Pinto, Lopez, & Murray, 2002). An increase of nearly 30 per cent over the preceding 10 years reflected the emergence of the tobacco epidemic in low and middle income countries. Stomach cancer causes 850,000 deaths yearly, followed by liver and colon/rectal cancers, the third and fourth leading causes of cancer deaths, with over half of the liver cancer deaths occurring in the Western Pacific Region. Breast cancer is the leading cause of cancer among women, with breast cancer survival rates improving where there is coverage and access to secondary prevention. Globally, neuro-psychiatric conditions19 account for 19 per cent of disease burden among adults. 19 “More than 150 million people suffer from depression at any one point in time; nearly 1 million commit suicide every year; and about 25 million suffer from schizophrenia, 38 million from epilepsy, and more than 90 million from an alcohol or drug use disorder” (World Health Organization, 2003, p. 190). 45 3.2.1 Categorising countries Globally, the health of people is variable between, and to a lesser extent, within countries. Differing classification systems are used to group countries, but no system is fully satisfactory. The World Bank (1993) categorises countries according to their gross national product and by eight demographic regions. The regional categories can be divided into the former socialist economies of Europe and the established market economies where uniform age distributions are leading to older populations, and the other six regions where the age distributions are younger. “These latter countries correspond to the low and middle income countries and contain 85 per cent of the world’s population” (Beaglehole & Bonita, 1997, p. 5). The terms ‘developed’ and ‘less developed’ or ‘developing’ are used by the United Nations, and falsely allude to a continuum. However, developing countries will not inevitably follow the wealth generation of the small number of developed countries. Other terms include ‘North’ and ‘South’, ‘First World’ and ‘Third World’ countries, ‘industrialised’, ‘non-industrialised’, and ‘newly industrialising’ and are also unsatisfactory because within broad groups of countries there is enormous diversity in social, economic and health characteristics. Instead, the terms ‘rich’ or ‘wealthy’, and ‘poor’, have been adopted throughout this thesis because they emphasise an important distinction and remind us that “rich countries have achieved and maintained their position largely at the expense of poor countries” (Beaglehole & Bonita, 1997. p. 6). 3.2.2 The reasons chronic conditions are escalating in New Zealand Despite the decrease in the number of communicable diseases, the rise in noncommunicable conditions and mental disorders has far-reaching implications. In New Zealand chronic conditions make up the major health burden and reasons for this rapid growth include demographic trends, population ageing, consumption patterns and life-style changes (World Health Organization, 2002a). 46 3.2.2.1 Demographic trends and population ageing Populations are living longer due to nutrition, public health developments during the last one hundred years, and advances in science and technology (World Health Organization, 2002b). Average life expectancy at birth has increased globally almost 20 years in the last 50 years (World Health Organization, 2003). In 2005 life expectancy at birth for New Zealand males is 76.7 years and for New Zealand females 81.2 years (Statistics New Zealand, 2005a). Despite major improvements for Maori over the last 40 years, life expectancy is lower than the New Zealand average, although the gap in life expectancy at birth between Maori and non-Maori, reduced by 0.6 years in the five years to 2000-2002 (Ministry of Social Development, 2004). Ethnic differences in death and disease rates are associated with differences in the socio-economic status of the different groups (National Health Committee, 1998). Similar to other wealthy countries, New Zealand is experiencing changes in the age structure of its population characterised by fewer children and an increase in the older population. Projections indicate that the New Zealand population will increase from 4.06 million in 2004 to 5.05 million by 205120 (Statistics New Zealand, 2004) and there will be 1.14 million people aged 65 years and over, representing an increase of 166 per cent since 1996. People aged 85 and over will number 290,000 in 2051, a six-fold increase since 2000 (Khawaja & Thomson, 2000). Fertility levels will continue to decrease for New Zealand women until 2010 and will then level off to 1.9 children on average. The population under 15 years is expected to continue to decline, with children comprising 22 per cent of the population in 2004, and 16 per cent, in 2051 (Statistics New Zealand, 2004). There were 57,630 live births registered in New Zealand in the March 2005 year, 1.8 per cent higher than the annual average over the last decade (56,630), although this is, as in other wealthy countries, below the level required for a population to replace itself without migration (Statistics New Zealand, 2005a). A net migration gain of 5000 people each year (the average annual level for the last 100 years) will comprise approximately 4000 Asian 20 This is based on the medium projection series, which assumes medium fertility, medium mortality and a net gain from migration of 5,000 people per year over the intervening period. 47 people and 1000 Pacific people each year from 2000 until 201621 (Khawaja & Dunstan, 2000; Ministry of Health, 2002d; Statistics New Zealand, 2005b). The age structure of the New Zealand population will undergo significant changes in the future, because like other wealthy countries, the New Zealand population is ageing. People aged 65 and over will make up one-quarter of the population in 2039, compared with 12 per cent in 2004. The median age of the population is projected to rise from 35 years in 2004 to 45 years by 2045, reflecting the combined impact of sub-replacement fertility, increased longevity, and the transition of baby boomer22 cohorts into the older ages (Statistics New Zealand, 2004). Increasing longevity does not inevitably mean higher rates of chronic conditions, as there is growing evidence that successive cohorts of older people are living longer than their predecessors and are also healthier. Considerable debate surrounds whether increasing life expectancy will be largely healthy, with ill health and disability compressed into the last years of life. A ‘selective survival effect’ reported in very old people, is associated with health status in earlier years (Grundy, 1997). However, the sheer increase in numbers of older people in New Zealand will lead to an increase in chronic conditions and associated disability. Future increases in the incidence and prevalence of chronic conditions will be strongly influenced by the approaches to prevention that are undertaken by the New Zealand government today. Health expectancy is a summary measure of population health that captures the quantity and quality dimensions of physical health and is defined as the number of years a person could expect to live independently, without functional limitation and requiring assistance. In 2001, ‘independent life expectancy at birth’23 was 64.8 years for New Zealand males and 68.5 years for New Zealand females. There were large differences between Maori and non-Maori in their probability for living a long and healthy life (Ministry of Social Development, 2004). 21 Actual population numbers will depend on fertility and migration decisions that have not yet been made, and on mortality patterns that may be subject to change. 22 The baby-boom era refers to the post-war increase in fertility rates. Spanning from 1946 to 1965, New Zealand experienced the longest and most intense baby boom amongst wealthy countries. 23 Independent life expectancy at birth is a measure that reflects changes in social and economic conditions, life-style changes, medical advances and better access to health services. 48 3.2.2.2 Consumption patterns and life-style changes Life-style and behaviour are primary determinants of conditions such as heart disease, diabetes, and many cancers, and have the potential to prevent, initiate, or advance chronic conditions and their associated complications. Major causes and risk factors for chronic conditions are life-styles that adopt unhealthy behaviours such as tobacco use, physical inactivity, excessive alcohol use, unmanaged stress, and prolonged and unhealthy nutrition. The consumption of cigarettes, other tobacco products, and exposure to tobacco smoke is the world’s leading preventable cause of death, responsible for five million deaths a year (World Health Organization, 2003). Tobacco smoking is a well recognised risk factor for many cancers and respiratory and cardiac conditions, as well as exposure to environmental tobacco smoke (particularly maternal smoking), an identified risk factor for Sudden Infant Death Syndrome (SIDS) and respiratory problems in children. Brundtland (2001) contends “Tobacco will cause more of them to die than any other single reason - and health systems will not be able to afford the long and expensive care in its wake” (p. 14). In a 2001 comparison of adult smoking prevalence rates, New Zealand had a rate of 25 per cent, ranking eighth out of 17 OECD countries, ahead of the Netherlands (34%) and the United Kingdom (27%), but well behind Australia (19.8%), the United States (18.5%), and Canada (18%) (Ministry of Social Development, 2004). When compared to other wealthy countries, New Zealand smoking levels are relatively low for males and relatively high for females (Ministry of Health, 2003f), and smoking is more prevalent among those with lower incomes, beneficiaries, and those living in the most deprived areas (Howden-Chapman & Tobias, 2000). Smoking is most prevalent among people aged 25-34 years, followed by those aged 15-24 years, and those aged 35-54. Maori women have the highest smoking prevalence (52%) followed by Maori men (39%). Among Pacific peoples smoking is more prevalent among men (35%) than among women (29%) (Ministry of Social Development, 2004). Peto, Lopez, Boreham, Thun, and Heath (1994) suggest 50 per cent of smoker’s who die prematurely die on average 14 years earlier than non49 smokers. In New Zealand about 4700 people die each year as a result of tobacco smoking ("Tobacco in New Zealand," n.d.). Unhealthy changes in dietary patterns, reduced physical activity, and increased illicit drug use may seem minor compared to the destruction caused by tobacco, however, these negative changes in life-style are increasing globally and are associated with chronic health problems. In 1997, 35 per cent of New Zealand adults aged 15 and over were overweight and 17 per cent were obese (15% of adult males and 19% of adult females) (Ministry of Health, 1999). New Zealand has a relatively high prevalence of obesity compared to an OECD median of 11.5 per cent24 (Ministry of Social Development, 2004). In 2002, 10 per cent of children aged 5-14 years were obese (Ministry of Health, 2003d). Obesity increases with age, peaking in the 45-64 year age group, and adult females are more likely than adult males to be obese. For females there is an association between obesity and the level of deprivation in the area where people live, and Maori and Pacific people have higher rates of obesity than other ethnic groups. Obesity is associated with heart disease, diabetes, stroke, high blood pressure and some cancers (Ministry of Social Development, 2002). Globally, increasing levels of obesity are related to social changes, including convenience foods high in fat and energy, passive leisure, less physically demanding work, greater use of automated transport, and labour-saving technology in the home. Twelve per cent of New Zealand adults have never experienced stress that has a negative effect, whilst 88 per cent have experienced stress that has a negative effect in the last 12 months, with three per cent always experiencing this negative stress (Gravitas Research and Strategy Limited, 2005). Half of all New Zealand adults (57% males and 48% females) take part in 30 minutes or more of physical activity a day, on five or more days a week and three out of four adults take part in more than 2.5 hours of physical activity each week. Overall, men are more active than women, 24 The United States has the worst prevalence rate of obesity (31% in 1999), with the United Kingdom (22% in 2001) and Australia (21% in 1999) higher than New Zealand. The rate in Canada was slightly lower (15% in 2001) than New Zealand and Japan (3% in 2001) had the lowest prevalence of obesity (Ministry of Social Development, 2004). 50 and Asian people, particularly Asian women, are the least physically active (Ministry of Health, 2004d). The Ministry of Health (2003c) estimated that as many as 11,000 deaths in 1997 (40% of all deaths) may have been attributable to the joint effect of sub-optimal diet and physical activity levels. This includes over 85 per cent of ischaemic heart disease, 70 per cent of stroke mortality, 80 per cent of diabetes mortality and six per cent of all cancer mortality. Alcohol is the most commonly used recreational drug in New Zealand and excessive consumption of alcohol is a major personal and public health issue. Heavy drinking over a long period of time is associated with causing cirrhosis of the liver, pancreatitis, endocrine disorders, cardiomyopathy, gastritis, high blood pressure, haemorrhagic stroke, cancers of the mouth, pharynx, larynx, oesophagus, breast and liver. Alcohol dependence and abuse are related to high levels of alcohol consumption, and alcohol during pregnancy can lead to birth defects in infants (Ministry of Health, 2004d). In New Zealand eight out of 10 adults reported having a drink that contained alcohol in the last year. One-sixth of adult drinkers (17.2%) had a potentially hazardous drinking problem, and male drinkers (27.1%) were more likely than female drinkers (11.4%) to display drinking patterns that put them at risk of negative health effects. The proportion of adult drinkers with a potentially hazardous drinking problem was highest in the 15-24 year age group, and decreased with age (Statistics New Zealand, 2004). 3.2.3 Economic impact Health care costs become excessive when chronic conditions are poorly managed. However, the impacts of chronic health problems extend beyond the expenses associated with medical treatment. Individuals pay the measurable costs of clinical interventions, reduced workdays, and lost employment. Other costs that are difficult to measure precisely include condition-related disability, shortened lifespan, and lowered quality of life. Governments and health care organisations pay the direct and indirect costs associated with medical care. Health professionals and families can find 51 it frustrating and difficult to provide care across settings, time, and within available resources and governments, employers, and societies suffer the loss of productivity associated with chronic conditions. Table 2 cites studies in different countries that vary in method and degree of rigor but consistently demonstrate the high economic costs related to chronic conditions. Table 2: Studies addressing costs related to chronic conditions Asthma Total estimated cost (direct & indirect) in 1999 Direct cost: Germany Diabetes India United States Obesity 3.2.3.1 United Kingdom Heart Disease Inpatient (hospital) Є$48.2 million; Rehabilitation Є$62.5 million; Total drug prescription Є$6,411 million NZ$4.71853 (Є$2.74 billion) (Stock et al., 2005) Indirect cost: Sickness benefit payments Є$1,194.8 million Lost years of productivity/early retirement Є$610.2 million Lost years of productivity/premature death Є$244.5million Total estimated direct cost to patient in the management of diabetes mellitus (direct cost included medicines, laboratory costs, doctors fees, hospitalisation, surgery, and transportation in the last year) *20 million people have diabetes in India Total estimated cost (direct & indirect) in 2001 Direct cost: NZ$3.14332 billion (US$2.2 billion) (Shobhana et al., 2000) NZ$167.167 billion (US$117 billion) Health care costs: $61 billion Indirect cost: Loss of production Total costs of CVD and CHD in 2003 Direct cost: (Weight-control Information Network, 2004) NZ$86.9646 billion (UK£33.709 billion) Health care costs: CVD: £14,732 million; CHD: £3,527 million Indirect cost: Productivity losses due to mortality: CVD: £3,677 million; CHD: £2,173 million Productivity loss due to morbidity: CVD: £2,556 million; CHD: £961 million Informal care: CVD: £4,835 million; CHD: £7,910 million (Petersen, Peto, Scarborough, & Rayner, 2005) New Zealand: Health care costs Health expenditure is the result of a mix of social, political and economic factors. Although there is no ‘right’ amount to spend on health, health expenditure as a proportion of ‘Gross Domestic Product’ (GDP) is often used in international 52 comparisons25. In New Zealand total health expenditure in 2000/01, as a percentage of GDP, was 8.8 per cent, increasing to 9.2 per cent when the funding for non-health items (mostly disability support activities) was included. Public health expenditure accounts for about three-quarters of total health expenditure (Ministry of Health, 2004c). Expenditure on health care in New Zealand is similar to that which could be expected for another OECD country with a similar level of GDP. Table 3 demonstrates the high costs associated with chronic conditions that cause the burden of disease in New Zealand. Table 3: New Zealand studies addressing costs related to chronic conditions Asthma Total estimated cost (direct & indirect) late 1990s NZ$825 million Direct cost: Pharmaceuticals $50.0 (Holt & Beasley, 2001) Hospital inpatient $14.0 million; Emergency Department services $6.7 million Primary care services $19.3 million Specialist services $0.8 million Patient costs $25.6 million Others $8.8 million Indirect cost: Work loss $105 million Premature death $254 million Disability adjusted life years $340 million Diabetes Total estimated cost (direct & indirect) 1999 Direct cost: NZ$540 million $270 million (Protemix, 2003) Indirect cost: At least $270 million Obesity Direct costs to the health sector in 2000/1 NZ$247.1 million $274.1 million (A. King, 2003) Heart Disease Direct costs 1999: Hospital cardiac services: >$150 million 2001/02: Cardiovascular drugs: $110 million 3.2.4 NZ$260 million (Health News, 2004) Impact on the poor The relationship between poverty and chronic conditions can be described as complex and interdependent. Chronic conditions disproportionately affect the poor who are 25 Reasons for differences in international health spending include: health service cost variations; higher costs of medical care consumed, given higher labour costs and prices for services; intensity of treatments; rates at which invasive procedures are performed; rapid and extensive introduction of new medical technologies; demographic characteristics; cultural and religious factors; welfare philosophies; private insurance coverage; origin of funding, and the incidence of litigation. 53 caught in a cycle of poverty and poor health. The poor may lack knowledge about ways to protect themselves from disease or when to seek health services, lack power to protect their rights, and lack income to access services or obtain coverage for essential interventions. In fact, interventions that could significantly reduce deaths and disease burden and improve health do not reach the world’s poorest populations (World Health Organization, 2001b). The path from poverty to chronic conditions involves a number of socioenvironmental factors that are critical determinants of health status. These include prenatal factors, age, education, environment, and access to care. Mothers who are malnourished are more likely to bear children who experience chronic conditions such as diabetes, hypertension, and heart disease in adulthood (Law et al., 2001). Poverty and poor health in childhood has been associated with cancer, pulmonary disease, cardiovascular disease and arthritis in adulthood (Blackwell, Hayward, & Crimmins, 2001; Law et al., 1993). In the United Kingdom, impoverished elderly were at high risk of physical dysfunction and unable to afford care for chronic conditions (Lynch, Kaplan, & Shema, 1997) and in Brazil, receiving less education was linked with higher rates of mental disorders (Ludermir & Lewis, 2001). Unemployment has been associated with health problems and morbidity, and mortality rates are higher in the unemployed than the general population (Buffat, 2000). The poor tend to work in more physically demanding roles increasing the risk of injury due to accidents (Marmot & Bobak, 2000; Warden, 1998) and in poor countries hazardous chemical exposure has been linked with local prevalence rates of cancer, cardiovascular, and respiratory diseases (Mengesha & Bekele, 1998). The poor frequently lack access to health care or preventative measures that, in turn, have been associated with poor health outcomes and exacerbations of chronic conditions. Care is often delayed because of cost for indigent groups. In New Zealand cost, transport, acceptability of the provider, and the Maori concept of whakama26 have been identified as barriers to Maori accessing services (Pomare et al., 1995). Changes to the cost structure of services can affect utilisation, which was evidenced when levels of utilisation fell by 15 per cent after the New Zealand government introduced a 26 Whakama is a term used to describe embarrassment, losing face and shyness. 54 new charging regime in general practice. Beneficiaries were the group most affected, even though this group was supposedly the focus of increased assistance (P. Davis, Gribben, Lee, & McAvoy, 1994). In Vietnam the poor are often observed to delay treatment, use less government provided health services, and pay more for each episode of care compared with the rich (Ensor & San, 1996). In Mexico the poor experience inadequate care because of restricted access to medications and health professionals due to unavailability or expense (Leyva-Flores, Kageyama, & ErvitiErice, 2001). The path from poverty to chronic health problems is bi-directional and the ‘chronic conditions – poverty’ relationship also requires consideration. Loss of income, the costs of interventions and marginalisation because of chronic health problems negatively affect the economic status of those with chronic conditions. Chronic conditions have been linked to work disability, early retirement, and reduced productivity placing employees at risk of premature job termination (Dooley, Fielding, & Levi, 1996; Herrin, Cangialose, Boccuzzi, Weintraub, & Ballard, 2000) and treatment costs can be prohibitive when conditions are initially not managed well or prevented (Rice, Kelman, & Miller, 1992). People with chronic conditions are also at risk of stigmatisation, which can result in limiting employment opportunities and causing an exacerbation of chronic problems (Alem, 2001). 3.3 Current health systems are not designed for chronic problems The World Health Organisation (2000) has described a health system as including “all the activities whose primary purpose is to promote, restore or maintain health” (p. 5). Controversy has always surrounded the central objectives of health systems, however there is general consensus that health promotion and health restoration are overarching purposes. The World Health Organisation contend that improving the health of the population, responding to peoples expectations, and providing financial protection against the costs of ill-health are fundamental objectives. Medical attention, interventions by traditional healers, and home care of the sick, which is how 70-90 per cent of all sickness is managed (Kleinman, 1978) are services provided within the health system, in addition to public health activities such as health 55 promotion and disease prevention, and environmental safety improvement. In general, however, information about health systems refers to either the provision or investment in health services, which relates to the ‘the health care system’27 as opposed to the wider ‘health system’. Global spending on health care alone in 1997 was approximately $2985 billion, almost eight percent of world GDP, and represents only a part of the cost of population health (World Health Organization, 2000). Historically, the New Zealand health care system evolved around identifying infectious diseases, treating symptoms, and sometimes producing cures, and today performs best when addressing individual episodic and urgent concerns. The acute care approach, appropriate in the past, cannot successfully manage the burden presented by chronic conditions. The acute care approach still permeates the thinking of clients, the public, health organisations, health workers, and governments. It affects all levels of the health care system, and is perpetuated by out-dated health training and education, and workforce employment practices (World Health Organization, 2002a). This is because health professionals learning and formative experiences were in hospitals, as opposed to less acute settings, and knowledge, beliefs and methods were aimed at achieving outcomes in this intense, acute setting. Currently the New Zealand health care system is difficult to characterise because it includes a wide and diverse range of organisations, health professionals/workers and consumers. Financial arrangements underpinning the health care system are complex and include combinations of funding from public, private, and not-for-profit organisations (Boyd & Sheridan, 2000). Nevertheless, there is an increased recognition of the importance of a comprehensive approach to health care services and longer-term outcomes as a consequence of health care costs, population focused information, and outcomes based knowledge. The New Zealand Health Strategy (Ministry of Health, 2000) provided the direction for government action on health, identifying the need to prevent and manage chronic diseases and their disabling consequences, and acknowledged the importance of an adequate support workforce. The newly established Health Workforce Advisory Committee reported “…past health workforce structures are not an adequate guide as we look to the future…new 27 The health care system includes preventative, curative, and palliative interventions for individuals or populations. 56 models of clinical practice to manage continuity of care for people experiencing chronic conditions have become a major challenge and opportunity for workforce development” (Ministry of Health, 2002e, p. 16). Nursing in a review of practice and education identified that chronic care and increased screening and prevention needs as influencing future primary health care roles for nurses (Nursing Council of New Zealand, 2001a). Reform within the New Zealand health care system is occurring on many levels. Information and skills are recognised as essential for clients to manage their conditions and client behaviours and provider communications are receiving increased attention. Coordinated approaches are evidence-informed, consumer voice and participation is greater, and the need to maximise community resources is acknowledged (Ministry of Health, 2001c). Globally, health care organisations are challenged to streamline services, up-skill health professionals/workers, focus on prevention, and continue ongoing development of information systems to enable planned care for predictable complications. Without an investment in considerable change, the New Zealand health care system, like that of other countries, will remain inefficient and ineffective as the prevalence of chronic conditions rises. Unnecessary hospital admissions, expensive technologies, and the collection of useless clinical information will continue to cost millions, and improvements in population health status will not keep pace (World Health Organization, 2002b). An important role for governments includes setting standards for quality, aligning financial incentives with the development and strengthening of intersectoral partnerships, and establishing policies that encourage the coordination of care. Clearly the most fundamental issue highlighted by this discussion is the urgent need to shift away from an acute, reactive, episodic model of care that is unable to achieve the necessary population health outcomes that are possible. 3.3.1 Changing the systems of care “Current care systems cannot do the job. Trying harder will not work. Changing the systems of care will” (Institute of Medicine (U.S.) Committee on Quality of Health Care in America, 2001, p. x). In New Zealand important changes to health policy and 57 legislation, and the reorganisation of health care financing to support care for chronic conditions is occurring (Ministry of Health, 2001b, 2001c, 2004a). Developing a more comprehensive system of care is aligned to the realisation that simple unidimensional solutions do not work for complex problems. No longer are conditions such as asthma, diabetes, arthritis and depression being considered in isolation. Awareness is growing that similar strategies can be as effective in managing many different conditions (R. Davis, Wagner, & Groves, 2000). Improving the care of the chronically ill begins with primary care, where the large majority of patients receive the bulk of their care and are likely to do so for the foreseeable future (Hiss, 1996). “The defining characteristics of primary care (that is, continuity, coordination, and comprehensiveness) are well suited to care of chronic illness” (Rothman & Wagner, 2003), suggesting the redesign of the system of care is the primary determinant of chronic care quality. Primary care can only expand and strengthen the role in chronic illness care with system support. The Chronic Care Model, which addresses necessary health system changes for improving chronic illness care, was developed as a framework to guide quality improvement, particularly within primary care (Bodenheimer, Wagner, & Grumbach, 2002a, 2002b). Changes necessary to reorient the current acute health system include refocusing on the delivery of effective preventative care, which is fundamentally what is recommended by the chronic care model of effective chronic-disease management. For this reason, the model is presented as a blueprint for changing the current system of care. The chronic care model constitutes a major rethinking of primary care practice, based on the knowledge that chronic care takes place within the entire community, the health care system, and the provider organisation (Bodenheimer et al., 2002a). Endorsed by the World Health Organisation as a framework to guide practice, the model has been implemented in more than 300 health care organisations in the United States (Bodenheimer et al., 2002a; Glasgow, Orleans, & Wagner, 2001). The extent to which the model can improve the management of chronic conditions, such as diabetes, asthma, congestive heart failure, and depression, and reduce health care costs has been demonstrated (Bodenheimer et al., 2002b). Recently, the chronic care model was adopted by several district health boards in New Zealand as a generic 58 template, applicable across diseases and health care organisations within regions (J. Wellingham, personal communication, November 11, 2004). The chronic care model seeks systems change to enable improved patient outcomes, which occur when patients are informed and activated, and health professionals comprise prepared, proactive teams. The interaction between the two groups is intended to improve functional and clinical outcomes (see Figure 2). Figure 2: The Chronic Care Model From “A survey of leading chronic disease management programs: Are they consistent with the literature?” by E.H. Wagner, C. Davis, J. Schaefer, M. Von Korff, and B. Austin, 1999, Managed Care Quarterly, 7,3, p.56-66. Copyright 1999 by Aspen Publishers Incorporated. Reprinted with permission of the author. The model recommends evidence-based interventions within six areas known to improve processes of care and patient outcomes. These are described in the sections following. 59 3.3.1.1 Community resources and policies The health care system can enhance care for its patients by looking outside itself. Health organisations and health professionals are often poorly organised to use community resources. Community resources support community care for chronic illnesses and include both government and community-based voluntary programmes. Mobilising community resources to meet the needs of patients involves partnerships with community organisations to assist the development of interventions in needed services. Other strategies include encouraging patient participation in community programmes, creating linkages to community resources through resource directories, referral pathways and joint programmes, and advocating for policies that improve patient care. 3.3.1.2 Health system organisation of care Health care systems create an environment in which organised efforts to improve health care for chronic illness occurs. Critical elements include a coherent approach to system improvement, leadership committed to improving clinical outcomes and incentives to providers and patients to improve care. A system must be motivated and prepared for change throughout the organisation. The systematic handling of errors and quality problems, and the prevention of breakdowns in communication and care coordination can be resolved through agreements that facilitate information sharing. 3.3.1.3 Self-management support Self-management support empowers and prepares patients to take responsibility for their health and the management of their chronic conditions in ways that reduce symptoms, complications, and disability. Strategies include assessment, goal setting, action planning, problem solving and follow-up. Skills training and psychosocial support interventions are central components of a delivery systems self-management support structure. 60 3.3.1.4 Delivery system design Delivery system design focuses on the delivery of effective, efficient clinical care and self-management support. An interdisciplinary team with defined roles carries out the tasks required to manage complex conditions. Planned visits, continuity of care and regular follow up are important components. Clinical case management services are recommended for complex patients and the care that the patient understands, and that is appropriate to their cultural background, is advocated. 3.3.1.5 Decision support Treatment decisions need to be based on explicit, proven guidelines underpinned by research. Evidence based guidelines embedded in routine practice supported by reminders, effective provider education, and collaborative support from relevant clinical specialists, including primary care, along with patient preferences are recommended. 3.3.1.6 Clinical information systems Timely information about patients and populations with chronic conditions ensures efficient and effective care. Disease registers, for example, can include information about the performance of elements of care and can be accessed by health care teams to track and plan care, monitor performance and provide reminders about needed services. Sharing information with patients and providers to coordinate care is a critical feature. 61 3.4 Risk prevention Improving health requires a major emphasis on the prevention of disease causation, with the underlying risks28 to health treated in addition to established diseases. Almost half of global mortality is attributed to 20 risk factors and managing these risks effectively may result in as many as 10 extra years of healthy life expectancy. Reducing risk by 25 per cent will result in the avoidance of much of the burden of disease29, and in human terms, millions of premature deaths may be averted, and many more millions of people may be spared years of disease, disability and ill health (World Health Organization, 2002b). Quantifying the burden of disease attributable to major risk factors, and estimating the potentially avoidable burden, if the population distribution of risk is reduced across the board, are the first steps. Following, an assessment of the types of interventions available to decrease exposure to risks or minimise the impact of exposure on health, the extent to which interventions can improve population health singly and in combination, and the resources to implement them are required. “Reducing risks to health is the responsibility of governments” (World Health Organization, 2002b, Message from the Director-General, p. ix), who need to invest heavily in risk prevention to contribute substantially to future healthy populations and sustainable development. Health policies for the prevention of well-known risks require choices to be made between different strategies. In most cases it is more effective to give priority to population-based interventions rather than those aimed at high risk individuals, to give priority to primary over secondary prevention, and to control distal, rather than proximal risks to health. Population wide interventions have the greatest potential for prevention. For example in reducing risks from blood pressure and cholesterol, shifting the mean of the whole population will be cost effective in avoiding future heart attacks and strokes, rather than screening programmes that identify and treat people with defined hypertension or 28 ‘Risk’ is the probability of an adverse outcome, or a factor that raises this probability. A prediction of the measure of inaction suggests that by the year 2020 there will be nine million deaths caused by tobacco worldwide, compared to almost five million a year now (World Health Organization, 2002b). 29 62 raised cholesterol levels. The more immediate risks for major disease have been the focus of most epidemiological research and interventional analysis. Tackling distal factors such as reducing poverty and improving access to education is well-known to have a positive impact on health and survival, and there is potential for major health gains through sustained intersectoral collaboration across ministries concerned with policy development and implementation. Primary prevention targets well populations and keeps problems from occurring in the first instance, promoting resiliency and protective factors, or reducing susceptibility and exposure to risk factors (Minnesota Department of Health, 2001). Immunisation is an example of risk reduction through primary prevention as it lowers future exposures, and therefore the incidence of new disease episodes over time. Primary prevention must consider how common and widely distributed the risk is and the availability and costs of effective interventions. Significant health gains can be achieved through inexpensive treatments when primary prevention has failed. Secondary prevention detects and treats problems in the early stages, preventing serious or long-term effects or from affecting others (Minnesota Department of Health, 2001). Targeting problems with common risk factors, secondary prevention screens exposed populations for the early onset of sub-clinical illness and offers treatment. If disease processes are reversible, valid screening tests exist, and treatments are available, secondary prevention is effective. Identifying and preventing risks to health is a political process (Dowie, 2001) and factors that influence whether policies are adopted include the public’s perception of the risk, scientific uncertainty, distribution of risk, and inequity of health outcomes (Slovic & Gregory, 1999). The success of risk prevention is determined by the strength of the political leadership and support by sectors of society concerned with promoting health. 63 3.4.1 Government responsibility for health Governments in all wealthy countries play a major role in the funding30 of health care. The New Zealand Government purchases public health services directly, but has devolved purchasing responsibility to district health boards for most health care provision. The extent to which a government is involved in health care is often a result of decisions made in response to economic, political, technical and demographic pressures, combined with the social and cultural preferences of a society. The World Health Organisation (2002b) maintains that governments should take a greater role in tackling major risks to health because: reducing major risks to health will promote sustainable development; reducing major risks can reduce inequalities in society; government’s need to prioritise and focus on the most important risks, and exercising stewardship means fulfilling the government’s responsibility to protect its citizens. Population-based strategies directed by government benefit entire communities and the poor, who experience the greatest risks, usually benefit most thereby reducing inequalities. Tackling major risk has the potential to reduce inequalities globally. Actions that governments can take in risk reduction include: formulating risk reduction policies, including more support for scientific research, improved surveillance systems and better access to global information; prioritising the development of policies for the prevention of large risks to health; prioritising highest, interventions that are cost-effective and affordable in preventing and reducing risks; collaboration to reduce major risks to health such as unsafe water, sanitation and lack of education; collaboration to improve risk management and increase public awareness and understanding of risks to health, and encouraging the actions of communities and individuals to achieve a balance among all groups (World Health Organization, 2002b). The world faces some large, common, and certain risks to health, which are generally well understood scientifically, with estimates of risk probability and consequence, available. The cost-effectiveness of many interventions is also known and can inform policy decisions. Focused government-led action to 30 The term funding applies to the insurance function, that is, the raising of revenue to be spent on health services. 64 reduce risks to health, address determinants of health and promote healthy life is essential. 3.5 In conclusion The global burden of disease has shifted from acute conditions towards chronic conditions worldwide, although the New Zealand health system, like that of other countries has not changed accordingly. Current health care systems continue to provide episodic, acute care, demonstrating a mismatch with chronic conditions, which are lengthy and require continuity of care. Without a system that assures ongoing support, technological advances will not stop heart disease, acquired immunodeficiency syndrome, diabetes, and other chronic conditions. By 2020 chronic conditions will contribute to more than 60 per cent of the global burden of disease (World Health Organization, 2001a). In New Zealand demographic transitions and population ageing, consumption patterns and risk behaviours, are clear determinants in this trend. Chronic conditions disproportionately affect the poor, economically challenge patients, families, and governments and jeopardise the sustainability of health care systems. The changes necessary to improve the health care systems delivery of effective preventative care are fundamentally the same as those recommended in the chronic care model of effective chronic-disease management. If improvements in chronic care prevention and management follow a common set of system changes and improvement strategies, progress will be faster, more efficient, and less confusing. The chronic care model provides a functional template, as well as a set of organised principles, for basic changes to support care that is evidence-based, population-based and patient-centred. Defining broad areas, it is a framework in which improvement strategies can be adapted to local conditions. This is probably the reason why it is advocated by the World Health Organisation. Improving health requires a major emphasis on the prevention of disease causation, with the underlying risks to health treated in addition to established diseases. The 20 top risk factors are attributed to almost half of global mortality and much of the 65 burden of disease. Tackling major risk has the potential to reduce inequalities globally, and governments have a central role in leading action that reduces risks, promotes health and protects populations. In addition, health provider organisations, health professionals such as nurses, and the wider society, have roles in reducing risk. The following chapter discusses nursing and the development of primary health care. The management of chronic conditions is a burden to the individual and state, and tackling major risks poses a challenge to health professionals. Much of this work will be undertaken in the community, by those (nurses) involved in primary health care. 66 4 Chapter 4 Primary health care nursing 4.1 Introduction Nurses are the largest health professional group working in the health sector and number approximately 38,000 people (Health News, 2004). The New Zealand government has committed resources to the development of primary health care (PHC) nursing, a recently defined specialty area of practice (Hughes, 2003; Ministry of Health, 2002a; Ministry of Health). The PHC nursing workforce comprises nurses working outside of hospitals in community settings and the Ministry has stated “The extensive contribution that PHC nursing can make to reducing health inequalities, achieving population health gains and promoting and preventing disease is yet to be realised” (Ministry of Health, 2003b, p. vii, Executive Summary). The most widely used definition, constructed by a Ministry appointed expert nursing advisory group, states primary health care nurses are: …registered nurses with knowledge and expertise in primary health care practice. Primary health care nurses work autonomously and collaboratively to promote, improve, maintain and restore health. Primary health care nursing encompasses population health, health promotion, disease prevention, wellness care, first-point-of-contact care and disease management across the lifespan. The setting and the ethnic and cultural grouping of the people determine models of practice. Partnership with people - individuals, whanau (family), communities and populations - to achieve the shared goal of health for all, is central to primary health care nursing (Ministry of Health, 2003b, p. 9). The overarching ‘primary health care specialty’ encompasses many groups of nurses who have historically worked in community settings, developing various nursing roles that have focused on different activities or interventions, and individuals or groups. Bringing these groups together and establishing a common ‘core knowledge’ as the basis for PHC nursing practice has in part been a response to the New Zealand Public Health and Disability Act (Ministry of Health, 2001b). The Act, requiring the 67 development of national strategies, was accompanied by health care system restructuring to achieve the overall vision of improving population health through the activation of the PHC strategy (see section 4.4.1). The purpose of this chapter is two fold. First, to describe the diverse nursing groups that now comprise the PHC nursing workforce, their different historical backgrounds, and recent developments to promote the combining of these groups under a new title and specialty area of practice. Second, to present a model, which expands the understanding of the range of interventions, and levels of population-based practice that are available to PHC nurses. The model is also used to analyse nurses’ practice in the ‘Nurses in integrated care projects study’ (see chapter 6). Concepts underpinning the model are explained and have additional relevance to the implementation of population-based practice (see section 4.5.1.1). 4.2 The current PHC nursing workforce “The term ‘primary health care workforce’ covers the collective practice of registered nurses providing care in the community….public health nurses, Plunket nurses31, practice nurses32, district nurses, rural nurses, nurses providing care to specific groups (e.g., respiratory and diabetic patients) and nurses working in Maori and Pacific health provider organisations” (Ministry of Health, 2003b, p. 11). Community settings include urban and rural general practices, community-based clinics, (situated on marae, in schools or workplaces) and in peoples homes. Many nurses practice within relatively narrow areas of practice, such as wound management, and some clients may receive care from several practitioners at one time. Other practitioners, such as those working in rural communities, generally adopt a wider field of practice, responsive to the needs of clients in an effort to achieve integrated care (Litchfield, 2001). The Nursing Council of New Zealand (Nursing Council), who governs the practice of nurses and midwives by monitoring standards of registration and enrolment, 31 Plunket nurse is a title used in New Zealand to describe nurses who initially provided care to mothers and their newborn babies, and later expanded services to include older children (see pp. 74-75). 32 Practice nurse is a title used in New Zealand to describe nurses who work alongside general practice physicians, who are generally their employer (see pp. 77-78). 68 completes a workforce survey each year, which provides statistical information about the active registered nurses and midwives in New Zealand. As of 31 March, 2004 there were 34,660 practising registered nurses in New Zealand, of whom 91 per cent were female, over a third were aged between 40-50 years, 68.3 per cent were New Zealand European, 7.5 per cent were New Zealand Maori, and 2.9 per cent were Pacific peoples (New Zealand Health Information Service, 2004). The Nursing Council survey collects statistics on employment settings and types of work, although this does not always capture the number and range of nurses working in the community and primary health care. In 2004, registered nurses or midwives identified as working in primary health care, including practice nursing, numbered 3672 (10.6%). Many other nurses may work in PHC or community settings but are classified in other categories, such as, public health (1.5%); palliative care (1.7%); child health (5.4%); district nursing (2.6%); occupational health (0.9%); assessment and rehabilitation (3.0%) (New Zealand Health Information Service, 2004). 4.2.1 Primary health care and community survey 2001 A voluntary survey sent to 7617 registered nurses who had indicated in the 2000 workforce survey that their type of work or employment setting could include PHC, had a response rate of 47.9 per cent (n=3562). Results from the survey found the ‘work type’ of the majority of the PHC nursing workforce was classified as practice nursing33 (45%). Other nursing categories included: health education and promotion (28%); specialist PHC (28%); well child or child health (21%); district (18%); mental health (16%); family planning/sexual health (12%); public health (10%); rural health (8%); Maori health (7%); occupational health (6%); Pacific health (3%) and other (9%). Other results revealed the average age of a PHC nurse was 48 years, the main ethnic group was New Zealand European (80.5%), with 7 per cent of nurses selfidentifying as Maori. The two main employer groups were general practice (32%) and district health boards (32%), with the majority of Maori nurses employed by Maori providers (5%) and 140 nurses worked on a marae. The three main settings of 33 Respondents could indicate more than one work type. 69 service delivery were the home, a clinic, or general practice. When asked if specific strategies to reduce inequalities in health outcomes were part of their work, 44 per cent of respondents reported they were (Ministry of Health, 2003e). 4.2.2 Education preparation Registered nurses in New Zealand are educated to baccalaureate degree level today, although, this has not always been the case. Nursing training was undertaken in hospitals until the late-1980s, when an amendment to the Nurses Act of 1977 provided for polytechnics (later called technical institutes) to offer nursing education and award diplomas. This accompanied a transfer of nursing education from hospitals to technical institutes, although for a number of years hospital-based nursing training programmes overlapped with those taught in technical institutes. The reasons for the transition of nursing education from hospitals to technical institutes included: reducing the high rate of withdrawal among trainee nurses (Dow, 1995); supporting the new technical institute movement (M. Brown et al., 1997), and shifting the focus from a service-based model, dominated by the secondary sector (hospital) to an education-based model that presented the opportunity for primary sector (community) influence (M. Horsburgh, personal communication, July 15, 2005). A review of nursing education commissioned by the Nursing Council found that the location of nursing education within a technical institute had not resulted in the adoption of a community or primary health care nursing orientation (KPMG Consulting, 2001). In the early 1990s, with the introduction of baccalaureate and graduate education in technical institutes and universities, opportunities for nurses began to develop. Currently, there are six approved clinical masters in nursing programmes in New Zealand, assisting nurses to prepare for nurse practitioner status (see section 4.4.3). In the specialty area of primary health care, nurse practitioner development has been slow. Judy Kilpatrick, Head of the School of Nursing, the University of Auckland, suggests this is because the primary care sector has undergone significant restructuring, whilst the focus has been placed on the development of new primary health care organisations. She also contends nurse practitioner roles and positions have not been clearly identified or resourced, and there has been resistance by some 70 general practice physicians to accept this role as complementary (J. Kilpatrick, personal communication, July 21, 2005). The Ministry of Health (2003b) has proposed an education and career pathway in primary health care nursing. This framework links education programmes with generic New Zealand Nursing Council competencies, but does not identify knowledge that is specific to primary health care. In fact, the Ministry of Health (2003b) states “most programmes include reflection on practice and self-development in the area of clinical practice, but are not specific to primary health care nursing” (Ministry of Health, 2003b, p. 38). 4.3 Nursing groups in communities Historically, a number of different nursing groups have worked in New Zealand communities, and these combined groups now comprise the PHC nursing workforce. Not surprisingly, the differences in histories have had a significant bearing on the cultures that exist within the distinct nursing groups. The challenge for advancing a PHC agenda is the development of a common knowledge and culture, whilst building on past developments and strengths. The roles of community nurses in early New Zealand are discussed first, and include the district nurse, public health nurse, Plunket nurse and school nurse. Following on, the more recent practice nurse role situated in the domain of general practice is discussed. Finally, PHC nursing roles, such as disease-state management, Maori health, Pacific health, Asian health, migrant health, older persons’ health, child health and occupational health are identified. Most of these roles undertake practice interventions consistent with those undertaken by public health, district and practice nursing roles. 4.3.1 Community nurses in early New Zealand In the 1800s nurses were mostly untrained and unskilled and care was provided by male attendants and older women from the domestic classes (Burgess, 1984). In early New Zealand pioneering life, local women also carried out nursing work. Nursing as a profession that required training is related to the dominance of the medical profession. Women of higher social standing considered nursing because it was seen 71 as a legitimate charitable activity and an excellent preparation for marriage and motherhood. Alternatively, it was also seen as a substitute for a large number of women that statistically, were unlikely to marry (McKegg, 1991). The first nursing training programme in New Zealand was established at Wellington Hospital in 1883 with an intake of ‘lady nurses’ (Burgess, 1984). Community nursing in New Zealand was strongly influenced by two women, Suzanne Aubert de Laye (1835-1926) and Sibylla Maude (1862-1935). Aubert de Laye later became Mother Mary Joseph Aubert, founder of the Congregation of the Daughters of Our Lady of Compassion, and is claimed to be the first trained community nurse (public health) in New Zealand. She trained in Paris under the Sisters of Charity, and secretly followed a complete medical course of lectures at Lyons. In the late 1800s, early in her nursing career, she worked with Maori in Hawkes Bay and the poor in Wellington (McKegg, 1991). Maude travelled to London in 1889 and trained for a year as a ‘paying lady probationer’ at the Middlesex Hospital (Burgess, 1984) and on her return to New Zealand became the matron at Christchurch Hospital. She had an interest in older people’s health and left her position to become the first district nurse in New Zealand, later founding the Nurse Maude District Nursing Service in Christchurch (Stonehouse, 1972). The four early divisions of labour for community health nursing in New Zealand were district nursing, public health nursing, Plunket nursing and school health nursing (Durkheim, 1984). 4.3.2 District Nursing In addition to the Nurse Maude District Nursing Service and the District Nursing Association of New Zealand also established in the early 1900s (Stonehouse, 1972), the district nursing service developed under sponsorship of the Saint Johns Ambulance Association with nurses appointed in Dunedin and Palmerston North in 1906 and 1909 respectively (Blue, 1995). Care for the sick outside of the hospital became possible in 1909 with the introduction of the Hospital and Charitable Institutions Act. Backblocks district nursing schemes developed and by 1913, nine district nurses were employed by Hospital Boards in rural areas. The introduction of the Government social security benefit for district nursing services in the 1940s 72 resulted in a major expansion of services (Burgess, 1984). District nursing roles today can be very specialised centring on for example, ulcer management, or can be more widely oriented in rural communities where there is a limited availability of other services within the region. 4.3.3 Public Health Nursing Public health nursing developed in New Zealand at the turn of the century when major threats to health were communicable disease and malnutrition. After an outbreak of dysentery in Papawai, the Chief Health Officer, Doctor Mason, recommended to the Native Department that a nurse be sent to assist the local doctor and teach the Maori women food preparation and care of the sick. Under the Native Department a native health nursing scheme developed with Maori women trained as nurses. Akenehi Hei and Heni Whangapirita were the first two Maori registered nurses to graduate as part of the scheme in 1909, although several others had previously gained partial registration by way of nursing certificates (McKegg, 1992). The service developed in response to concerns for the future of the Maori race as a result of reduced immunity to newly acquired diseases such as tuberculosis, influenza, enteric fever and small pox. McKegg (1991) argues nurses work reflected unspoken agendas, which included removing the threat that contagious diseases in Maori posed to the European community, and as “forces for assimilation” (p. 4). Nurses responsibilities included relaying the notions of ‘scientific motherhood’ to Maori by providing advice on hygiene, food preparation, care of their children, pregnancy, childbirth, inspecting kainga and native schools, and keeping a record of Maori births and deaths in the district (Burgess, 1984). Reluctance by hospital authorities to train Maori women as nurses prevented the scheme expanding, and in 1911 when the Native Department was transferred to the Department of Health the majority of nurses employed to work in the service were non-Maori (McKegg, 1992). The native health nurses were increasingly expected to attend to Europeans living in the backblocks. The title ‘district health nurse’ was adopted and the special nurse to Maori ceased to exist (Blue, 1995). At this time nurses were undertaking 73 interventions related to venereal disease, tuberculosis, child health, immunisation, health education, Maori health, and school health (Department of Health, 1986). Such activities suggest a distinct nursing role with a primary health care orientation, which is consistent with McKillop’s proposition that by 1930, native nurses who provided care specifically for Maori were superseded by public health nursing for all Maori and non-Maori in a geographically defined area (McKillop, 1998). In 1953, the service combined with Industrial Health Nursing and the title changed to ‘public health nurse’ as it remains today. Blue (1995) contends that because of the traditional conceptions of the native health nurse working with Maori, for many years a segregated system of delivery of child health services existed in New Zealand. Many Maori opted for care by a public health nurse (formerly a native health nurse), and most non-Maori utilised the services of the Plunket nurse. In the late 1980s Plunket nurses in mutual agreement with Area Health Boards assumed primary responsibility for the well childcare of all pre-schoolchildren leaving public health nurses with assigned responsibility for children under five, considered to be at risk or living in rural areas (Ministry of Health, 1996). Later in 1995, the demise of the Public Health Commission was labelled a “…retrograde step for the advancement of public health and population based health” (Carryer, Dignam, Horsburgh, Hughes, & Martin, 1999, p. 6). It was suggested that this would become evident over time with declining population health, or more immediately “as in a national emergency” (W. Armstrong & Bandaranayake, 1995, p. 23). Since this time the number of nurses has significantly reduced and the emphasis has been placed on communicable disease screening and management, health promotion, and less on family oriented health services (Martin, 2002). 4.3.4 Plunket Nursing In 1907, Doctor Truby King founded the Royal Society for the Health of Women and Children, a service which became known as the Plunket Society following the personal support of Lady Plunket, wife of the then Governor General (Parry, 1982). Concerned with the high rate of infant mortality, King promoted breast-feeding, improved methods of bottle-feeding, and mother-craft. Under the patronage of the 74 society, Plunket Nursing was established, and across New Zealand Karitane Hospitals and Karitane nurses developed with nursing services offered to all women with newborn babies. In the 1950s, 1960s and 1970s Plunket restructured both the organisation and services provided by the nurse. Karitane Hospitals closed and home visiting was negatively impacted. Over time the Plunket Society has initiated health prevention programs, household help, well child checks and crisis groups. Community health had been promoted through activities such as immunisation, water safety education, the provision of safety guards for heaters, information on poisons, safety about children’s clothing, and education on human relationships. Until the early 1990s public health nurses had provided similar services to Plunket nurses leading to a duplication of services in some areas and no services in others (Dow, 1995). In 1993 a national schedule for well childcare outlined an expectation of integrated and coordinated well child service provision, which included health education and promotion, health protection, clinical assessment, and family/whanau care and support (Ministry of Health, 1996). Today, this schedule directs the work of Plunket nurses. A number of health providers, including general practice physicians, nurses, social work services, voluntary and self-help groups continue to deliver well childcare (Malcolm, 1997) and both the duplication and fragmentation of services continue to occur. The Plunket Society has remained a national non-governmental organisation receiving significant funding from government and fundraising to provide well childcare34 to children under five and their mothers. 4.3.5 School Nursing In 1917 the first school nurses were appointed to work alongside four medical officers of health to conduct compulsory medical inspections of children in state schools because there were concerns about the health of schoolchildren. Termed the School Medical Service, the emphasis was on disease control, for example taking throat 34 ‘Well childcare’ is a current term used in New Zealand to describe routine health screening and surveillance interventions provided for children. 75 swabs during diphtheria epidemics, and conducting health and development assessments (Blue, 1995). The service grew to 31 nurses and 12 medical officers of health by 1930. The Maori schools were worst affected by diseases such as diphtheria and received the minimum of care, as only 18 Maori health nurses were in post in 1918. Consequently, much of the responsibility for the health care of schoolchildren was devolved to the 250 teachers in the native schools (Dow, 1995). In 1921 school health, which had been the responsibility of the Department of Education was devolved to the Department of Health (Burgess, 1984). The School Medical Service promoted immunisations amidst public opposition and anti-vaccinationist opinion within the Department, with estimates that 83 - 85 per cent of all schoolchildren were not vaccinated in 1924-5. Nurses active in school health were titled ‘district health nurses’ (see section 4.3.2). The School Dental Service was established in 1919, with about 30 dental nurses completing their training each year in the 1920s. In 1947 dental care extended to adolescents as well as schoolchildren, and fluoridation was a key health issue for nurses. The health camp movement was established in 1919 to combat the malnutrition traditionally associated with tuberculosis, and by the 1930s had been embraced by a number of voluntary agencies working with the Department. During the 1950s there was friction over child health between the Department of Health, the medical and dental professions and voluntary organisations such as Plunket and the new parents centre movement. Public health nurses supported controversial departmental efforts to promote immunisation, sex education, pasteurised milk and fluoridation of water supplies (Dow, 1995). Today public health nurses have a presence in schools but are often less available due to the reallocation of public health services to competing areas. Schools have independently employed nurses to support the health of schoolchildren, although the range of interventions school nurses undertake has not been well reported (Alcorn, 2002). Generally, there is a belief that school nurses promote health. This is apparent in the statement “School Principals and Boards of Trustees that support an on-site nursing service believe that an accessible and free primary health care service has the potential to promote student health and well-being and improve educational outcomes for students” (Alcorn, 2002, p. 30). 76 4.3.6 Practice Nursing Practice nursing is the most dominant of the nursing groups in the New Zealand community, with over three thousand nurses working alongside general practice physicians (S. French, Old, & Healy, 2001). Based on a United Kingdom funding model, practice nursing received government subsidies. In the United Kingdom however, the funding mechanisms established for practice nurses provided the opportunity for education to guide the development of the specialty’s practice. In New Zealand no provision was made to fund education, which was seen as a lack of commitment to the development of the practice nurse role (B. Docherty, personal communication, May 13, 2005). The practice nurse role has principally complemented primary care provided by general practice physicians (Minto, 2004). The origins lie in the development of general practice services in the 1970s when rural general practice physicians received a 50 per cent subsidy from the government as an incentive for practice nurse services, which aimed to relieve the general practice physician of activities that could be undertaken just as adequately by the nurse. The subsidy has been subject to several changes since its introduction, and in 1974 was increased to 100 per cent in an attempt to extend the role to include urban as well as rural practice settings. The full subsidy enabled practice nurse services to be provided at no cost to the client. As a ‘first point of contact’ with the health care system, nurses provided health advice and conducted clinical assessments and interventions. Despite the full subsidy, it was common for general practice physicians to insist on seeing the client in addition to the nurse, claiming a general medical services subsidy, with the result that the government paid twice for health care (Blue, 1995). The practice nurse subsidy was altered again in 1991 to NZ$11 per hour for up to a maximum of 32 hours per week (75%). This arrangement resulted in most practice nurses being employed part time and an increasing number of practice nurse services were charged to the client as general practice (physician) employers argued the need to pay for overheads such as dressings, equipment, reception staffing, power, and goods and services tax (Blue, 1995). The practice nurse subsidy has been viewed by many nurses as problematic in that general practice physicians have determined the 77 activities undertaken by the nurse outside of a nursing framework (College of Nurses Aotearoa (NZ) Inc., 2001). As a consequence of the PHC Strategy in 2001, the practice nurse subsidy along with the general medical services subsidy for laboratory and pharmaceutical costs was placed under a capitated funding formula managed by the Primary Health Organisation (see section 4.4.1) and representing general practice interests. In addition, the Accident Corporation Compensation pays the general practice physician NZ$15 for practice nurse interventions such as suturing a wound, with the doctor receiving a further NZ$28 for reviewing the same injury (B. Docherty, personal communication, May 13, 2005). Atkin and Lunt (1996) perceive the practice nurse role to have more flexibility than, for example the role of the district nurse. Other authors have described the practice role as predominantly task-oriented (Toop, Nuthall, & Hodges, 1996) with tasks delegated by general practitioners (Docherty, 1996; Michel, 1997). General practice, being located within clinical medicine, deals with the problems of individuals and does little to protect and promote the health of society (Beaglehole & Bonita, 1997), a construct that bounds the potential practice of practice nurses. Docherty contends practice nurses adopt one of two roles, either the ‘hand maiden’ role where the activities are delegated by the general practitioner, or a more autonomous role where a nurse uses a wide range of skills, makes decisions within a field of practice, and runs clinics focused on health education topics such as weight management and chronic diseases management. Carryer et al. (1999) go further, suggesting that nurses understand a strategy of health promotion that addresses the social and environmental determinants of health. It is often perceived that the general practitioner sublimates the ability of the practice nurse to contribute as a full and independent team member (Martin, 2002). Docherty (2004) maintains “…it has always been difficult for practice nurses to provide a true nursing service within a team when most of the ‘service’ has been defined and financially determined by the employer” (p. 10). Consistent with this perspective, Minto (2004) argues the capacity for expanding nursing services has been limited by the structural arrangement that place general practitioners as employers of practice nurses. Other factors that have affected practice nurses ability to contribute as equal team members include limited access to resources, physical workspace, postgraduate 78 education (Ministry of Health, 1998), and the nurses own view of their role and lack of confidence about the contribution they can make (Williams, 2000). 4.3.7 Other community nursing groups and new strategies A number of other nursing groups such as occupational health nurses, disease-state management nurses (including diabetes nurse educators and COPD case managers), Maori and Pacific health nurses, and rural health nurses have evolved. These groups commonly adopt the same types of interventions as Plunket, district, public health and practice nurses. In addition, combinations of nurses from the various groups have contributed to strategies like integrated care (see chapter 5), which required collaboration within and across the professions. Similarly, ‘Community FIRST’, which is a new service and funding model, is being evaluated by the ‘ASPIRE’35 study and engages nurses36 to lead a case management team of physiotherapists, occupational therapists, general practitioners and support workers to provide restorative and rehabilitative services to older people living in their own homes in five New Zealand cities (Ministry of Health, 2004b; Parsons et al., 2004). This model is being assessed for application in a multicultural population of all ages, with nurses again managing complex rehabilitation packages (Baird, 2004). 4.3.8 The historical legacy of community nursing The work of nurses in communities in the early 1900s reveals the development of a profession under the watchful eye of medicine. Doctors fiercely guarded clinical knowledge and clear divisions existed between nursing and medicine, with the idealised nurse one trained to take orders rather than follow her initiative (McKegg, 1991). Interestingly however, without the support of a hospital and working in isolated backblock areas far from the support of other health care workers, community 35 ASPIRE is the acronym for the ‘Assessment of Services Promoting Independence and Recovery in Elders’. 36 Community nurses who undertook lead case management roles in ASPIRE, completed a master programme of study in gerontology and rehabilitation (Parsons, Anderson, Senior, & Jacobs, 2004). 79 nurses were faced with the choice of leaving clients without treatment or taking on responsibilities outside their designated role. Most chose to provide treatment. Because it was dominated by medicine, community nursing in New Zealand did not develop autonomously as compared with primary health care practitioners such as ‘barefoot doctors’ in China and community nurses working in health centres in Sweden and Finland who were largely autonomous (Blue, 1995). New Zealand public health nurses did not commonly work from a community base, but remained attached to urban-based units of the Department of Health. Blue contends that the roles and responsibilities delegated to the public health nurse were strongly influenced by traditional gender roles and power differentials between nursing and medicine. For example, only in recent times have public health nurses been able to immunise without the supervision of a medical practitioner. Practice nursing may have developed because public health nurses did not offer ‘first point of contact’ services in primary health care in the 1970s. Autonomous decision-making by practice nurses is still limited by their need to defer to general practice physician employers, and the cost effectiveness of the service is impeded by the dual claiming of subsidies for clients by both nurses and doctors. While community nursing groups such as district nurses, public health nurses and school nurses overlap in terms of the populations they serve and the interventions they undertake, they are separate entities and do not share a common public health philosophy. Knowledge of primary health care principles (see p. xiv) and an understanding of the social and economic determinants of health would be required. Instead, many nurses appear to practice within a medical paradigm that focuses on acute symptom management (B. Docherty, personal communication, May 13, 2005). Constructing a collective primary health care workforce able to meet the diverse needs of individuals and populations poses a real challenge to the nursing profession. In particular, developing a more client centred orientation in health care requires nurses to build requisite partnerships with key providers to achieve a more comprehensive, integrated health-based delivery system. Zerwekh (1992) describes the practical wisdom of public health nurses in the 1890s who undertook a case load in the community, promoted self-management, and 80 acquired skills in clinical decision making through experience. In contrast to these early days where cases were found through inquiries in neighbourhoods, contemporary case loads result from referrals by a variety of agencies, such as schools and general practice physicians, which require a wider range of partnerships and collaboration. Collaboration produces “action that results in the attainment of mutual goals for the patient’s needs….it excludes unilateral, isolated or independent actions by professionals as a general style” (Ministry of Health, 2002f, p. 21). The nursing profession believes there is a need for more intersectoral partnerships and community development (J. Carryer, 2004). Porter-O’Grady (1999) has said “Nursing has a history of pulling together the many and disparate resources, players, and processes in health care around patients…. [and] is perhaps the only profession whose focus is the patient’s journey rather than any one given clinical event” (p. 9). However, if nursing is to play a significant role in building relationships and community development, distinctions between different models of partnership among professionals and the community must be understood. For example, a community involvement model is applied when the nurse determines the agenda and attempts to get the community on side, a community participation model is applied when the nurse gives the major role of the projects design and implementation to the community but remains in control, and a community controlled action model is applied when the nurse acts as a guide and educator of community members who learn skills to undertake their own project (J. Raeburn, personal communication, April 30, 2003). If nursing is to contribute to improving population health outcomes, nursing groups and in particular practice nurses, are well placed to promote health (Docherty, 2004; Minto, 2004). Implementing population-based practice on all levels will require an expansion of generic skills and the development of new knowledge and expertise. The PHC Strategy provides the context for change and PHC nurses have been identified as crucial to the successful implementation of the Strategy (Ministry of Health, 2001c). Section 4.4 describes the planned approach taken nationally to align and develop the PHC nursing workforce between 2002 and 2005. 81 4.4 4.4.1 Contemporary PHC nursing developments Background The New Zealand Labour government was elected to power in 1999 and introduced the New Zealand Public Health and Disability Act in 2000, which regulated the provision of health and disability services for New Zealand. Two key strategies set the overarching direction for the development of services, the New Zealand Health Strategy (Ministry of Health, 2001b) and the New Zealand Disability Strategy (Ministry of Health, 2001a). Fostering cooperation and collaboration between health and social sectors, and encouraging community voice in health and disability service decisions were central notions. Other documents were developed to provide greater detail of service, health issue, or population group specific strategies and/or action plans, such as, the New Zealand PHC Strategy (Ministry of Health, 2001c). Structural reforms to the health care system in 2001 accompanied the new strategic directions for health and disability service provision. District Health Boards were responsible for the purchasing and provision of primary, secondary and tertiary health services for defined populations. The population-based formula now used for determining a region’s share of public funding considers the demographic characteristics of each region, and adjusts for unmet need, overseas visitors and the degree of rurality (T. Ashton, 2005). Primary Health Organisations (PHOs) were the vehicle for District Health Board provision of population-based health care. PHOs are local health provider organisations that provide population-based and personal first line general practice services. In January 2005 there were 77 PHOs (A. King, 2005). The central aim of the PHO is to improve health and reduce health inequalities by targeting populations with poor health, or who are underserved. PHOs are required to: collaborate with other providers and coordinate care; demonstrate community, Iwi (tribal), and consumer participation in governing processes; respond to the needs of the community; demonstrate provider and practitioner influence in organisational decision making; apply a population needs-based formula (capitation), and demonstrate accountability for public funds, as they are ‘not-for-profit’ organisations (Ministry of Health, 2002b). 82 The PHC Strategy sought to identify and remove health inequalities and improve health through focusing on population health, health promotion and preventative care; community involvement; multidisciplinary approaches to decision making; improving accessibility, affordability and appropriateness of services; improving coordination and continuity of care and quality information; and funding, and providing services according to the population’s needs as opposed to fee-for-services when people are unwell (Ministry of Health, 2001c). In total the Government intends to commit just over NZ$1.7 billion over six years starting 2002/03 specifically for implementing the PHC Strategy using the PHO model (Ministry of Health, 2004e). The level of funding indicates a genuine attempt to establish a stronger PHC orientation within the New Zealand health care system. Existing PHC services include generalist first level services, such as general practice services, mobile nursing services, community health services for certain conditions (maternity, family planning and sexual health, mental health, dentistry, and pharmacy) or for particular therapies (physiotherapy, chiropractic, and osteopathy). Development of a PHC workforce that includes nurses has been central to achieving the Strategy (Ministry of Health, 2001c). 4.4.2 PHC Nursing scholarships and innovative models of practice The PHC Strategy required the MOH to facilitate a national approach to PHC nursing, which addressed capabilities, professional practice, educational and career frameworks, and employment arrangements (Ministry of Health, 2001c). Nursing received NZ$8.1 million of the funding committed to PHC for workforce development. Primary health care nursing scholarships were established to assist nurses working in the sector to gain postgraduate qualifications. Initially in 2003/04, about 390 scholarships were allocated. In early 2005, further scholarships were allocated, and the total cost so far stands at NZ$850,000. In another nursing initiative, 11 innovative models of PHC nursing were selected from over 130 proposals at a cost of NZ$7.25 million including the evaluation (Hughes, 2003; A. King, 2005). The 11 models focused on population strategies that fell under the New Zealand Health Strategy and assisted in the implementation of the PHC Strategy, over a four year period. Almost half of the innovative nursing models sought to reduce the 83 fragmentation and duplication of services, which had also been a feature of integrated care, and to support the transition of PHC service provision through PHOs (Hughes, 2003; Ministry of Health, 2004e). Selected from across New Zealand, examples included: coalition of nursing groups aiming to reduce inequalities (Northland District Health Board); Tuwharetoa health services partnership with whanau to reduce inequalities (Lakes District Health Board); combined PHC nursing groups to support nurses in the transition to PHOs (Mid-Central District Health Board); expanding nursing services to improve access to care, early interventions, and disease management (West Coast District Health Board), and a kupapa Maori PHC nursing service to develop nurse practitioner roles (Auckland District Health Board) (H. Hunter, personal communication, June 25, 2003). The decision to allocate the majority of the funding to PHC nursing innovations resulted from earlier findings by the Ministerial Taskforce on Nursing (Ministry of Health, 1998). The Taskforce identified few established nursing structures for entry into community practice, under-developed community nursing leadership, and no systematic approach to transition into practice for new graduates. Recommendations of the Taskforce included the development of a framework to guide PHC nursing over the next decade, which resulted in a national advisory group publication, ‘Investing in health: A framework for primary health care nursing’ (Ministry of Health, 2003b). This PHC nursing framework suggested: the need for developing innovative methods of service delivery; improving coordination of care across services; strengthening collaboration in multidisciplinary teams, and building stronger links across sectors. Funding streams, employment practices, and coordinated service provision that incorporated population and personal health strategies were advocated. Emphasis was placed on new models of PHC nursing practice that improved access to PHC services, health outcomes and reduced inequalities. PHC nurses were expected to be active in the governance of PHOs and hold leadership positions, and the framework highlighted a need for postgraduate education to support the development of PHC nursing practice. These recommendations were acted upon by the Ministry, represented in the funding of innovative nursing practice models and postgraduate nursing education. 84 4.4.3 Nurse Practitioner scope of practice The Health Practitioners Competence Assurance Act 2003 came into effect in September 2004 replacing the Nurses Act 1977 (Nursing Council of New Zealand, 2004). The term ‘nurse practitioner’ is protected under the new Act and is registered as a distinct ‘scope of practice’37. The Ministry of Health (2002f) stated “nurse practitioners are the highest level of clinical expert within nursing” (see p. v, preface). Similar to registered nurses, nurse practitioners do not require supervision by other disciplines. However, they differ from registered nurses in that they are required to have a clinically focused masters degree or equivalence, and a minimum of four years experience at an advanced level in a specific specialty area (Ministry of Health, 2002f). As at July 2005, there were 17 nurse practitioners registered in a range of specialty areas, which included neonatology, mental health, diabetes and related conditions, wound care, urology, gerontology, child and youth health, and whanau ora - family health (P. Renouf, personal communication, July 29, 2005). The majority of the nurse practitioners work in primary health care settings. The nurse practitioner with a sub-specialty in child and youth health is currently the only nurse in New Zealand to have prescribing authority38. The nurse practitioners in the whanau ora specialty have a Maori health focus. Prescribing is an important tool for nurse practitioners and over time it is envisaged that the majority will need prescribing competencies (Ministry of Health, 2002f). “The introduction of the role of the primary health care nurse practitioner is a fundamental opportunity to showcase their expert practice and leadership qualities, and to be inspirational role-models for primary health care nurses” (Ministry of Health, 2003b, p. 32). Competencies for the nurse practitioner scope of practice include: the ability to articulate a specialty area of practice and advancement; demonstrate expert practice across settings and within interdisciplinary environments; provide effective nursing leadership and consultancy; conduct scholarly research inquiry into nursing practice; 37 In 2004 four areas of registration were defined as ‘scopes of practice’, nurse practitioner, registered nurse, nurse assistant, and enrolled nurse (Nursing Council of New Zealand, 2004). 38 In 2003 Paula Renouf was registered as the first nurse practitioner with prescribing authority by the Nursing Council of New Zealand. She had worked for the previous ten years in California as a nurse practitioner in primary care. 85 develop and influence health and socioeconomic policies and nursing practice at local and national levels, and prescribe interventions, appliances, treatments and authorised medicines within a specialty area of practice. “Advocating health promotion and disease prevention, nurse practitioners will look beyond treating the ailment and consider non-medical interventions and encourage self-care. They will also be able to diagnose, evaluate health problems, including prescribing and monitoring medication” (Ministry of Health, 2002f, p. v, preface). In summary, New Zealand has planned and invested in the development of a PHC nursing workforce. Funding has been available for nurses to experiment with innovative models of nursing practice and the evaluation of these models is in progress. A number of PHOs have nurses represented in governance positions and further postgraduate scholarships are being allocated to nurses. Workforce surveys are informing nursing recruitment and retention strategies, and the first nurse practitioners in PHC are demonstrating advanced practice. In order to progress PHC nursing in the period 2002 to 2005, an incremental plan of action was proposed (see p. 87, Table 4). Most of the 2002 to 2004 milestones have been achieved, although areas that continue to be developed include: the registration of nurse practitioners, particularly in relation to prescribing and attaining a wider authority; leadership structures; credentialing PHC teams, and integrating new knowledge into primary health care nursing practice. 86 Table 4: Milestones for PHC nursing development 2002/3 • • • • • • • • Development of the framework for PHC nursing Innovative models of PHC nursing practice funded by the MOH Funding for postgraduate education accessed by PHC nurses First PHOs established and nurses represented in governance positions PHC leadership structure developed in district health boards and PHOs PHC education framework established PHC nursing resources focus on needs analysis as a basis for service planning PHC workforce analysis and recruitment and retention strategies developed Nurse practitioners implemented in PHC 2003/04 • • • • • Innovative models of PHC nursing practice funded by the MOH Beginning evaluation of innovative models of PHC nursing practice Introduction of PHC nurse practitioners Nursing leadership positions in place in district health boards and PHOs PHC education framework in place 2004/05 • Continue evaluation of innovative models and promulgate successful models PHC nurses supported to gain competency based annual practicing certificates Evaluation of initial gains to community - satisfaction surveys PHC nursing framework fully implemented PHC nurses have access to appropriate postgraduate education PHC nurses credentialed and functioning in PHC nursing teams • • • • • • From “Investing in Health: Whakatohutia te Oranga Tangata: A framework for activating primary health care nursing in New Zealand,” by the Ministry of Health, 2003, p.8. Wellington: Ministry of Health. 4.5 A model for PHC Nursing: The public health interventions wheel The public health interventions wheel (interventions wheel or wheel) is a public health model that has the capacity to demonstrate PHC nursing as a specialty area of practice. Initially developed as a means of identifying and documenting interventions undertaken by nurses in the United States, the intervention wheel became a tool for enabling practitioners to articulate their practice. The intervention wheel identifies population-based practice at three levels – individual and family, community, and systems and recognises 17 public health interventions. The concept is that each intervention and level of practice contributes to improving overall population health. The intervention wheel can describe nurses’ practice, despite the different locations nurses work in because a core set of interventions are commonly used, and the wheel 87 clarifies what is similar across settings (Keller, Strohschein, Lia-Hoagberg, & Schaffer, 1998). The intervention wheel was first introduced in 1998 by public health nurses in the Minnesota Department of Health (Keller et al., 1998). The wheel has been disseminated widely throughout the United States and is also used by disciplines39 in public health, other than nursing. Interest in the model has been influenced by the move towards population-based practice and the intervention wheel provides a guide for public health orientation, documentation, job descriptions, performance evaluations, programme planning and evaluation, and budgeting. Presented to boards and legislators, it has also provided a policy structure for health decision making, and is currently a component of nursing education programmes (Keller, Strohschein, Schaffer, & Lia-Hoagberg, 2004b). The author visited the United States in 2003 to explore the intervention wheel’s multiple applications to nursing practice, education, research and management. Public health nurses in Minnesota, working in the counties of Bloomington and Carver were observed applying the intervention wheel to the planning and evaluation of population health programmes. It formed the basis of job descriptions and was used to support pay equity adjustments. Student nurses at Bethel College, Minneapolis-Saint Paul attributed their understanding of population-based nursing practice to the wheel, which was introduced as a learning tool in year one of the undergraduate program. Postgraduate nursing students at the University of Minnesota used the wheel as a framework for critically analysing their practice. Nurses from the Shiprock Community Health Service Unit integrated Navajo values into the intervention wheel as a guide to both clinical and cultural practice. Overall, the intervention wheel appeared versatile and adaptable. 39 The intervention wheel describes the breadth of public health work, so nutritionists, health educators, planners, physicians, and epidemiologists may use the same interventions within interdisciplinary teams. 88 Figure 3: The Public Health Interventions Wheel From “Population-Based Public Health Nursing Interventions: A Model from Practice,” by L. Keller, S. Strohschein, B. Lia-Hoagberg, and M. Schaffer, 1998, Public Health Nursing, 15, p.208. Copyright 1998 by Blackwell Science Incorporated. Printed with permission of the author. 4.5.1 Describing the Public Health Intervention Wheel The intervention wheel shown in Figure 3 comprises three distinct elements of equal importance. The wheel is population-based, encompasses three levels of practice (community, systems, individual and family), and defines 17 public health interventions. The three elements are described successively. 89 4.5.1.1 Population-based According to the Minnesota Department of Health (2001), five criteria determine population-based practice. First, population-based practice focuses on entire populations and interventions are not restricted to those who seek service, are poor, or otherwise vulnerable. This is consistent with the concept ‘new universalism’, which infers high quality essential care, defined by the criteria of effectiveness, cost, and social acceptability that are available to the entire population. It implies explicit choice of priorities among interventions, respecting the ethical principle that it may be necessary and efficient to ration services, but that it is inadmissible to exclude whole groups of the population (World Health Organization, 2000). Population-based practice identifies everyone who is in the population-of-interest40 or the population-atrisk41. Second, population-based practice is guided by an assessment of population health status, which is determined by a community health assessment. Risk factors, problems, protective factors, and assets within populations that impact health status are analysed, priorities are established, and interventions are planned, implemented and evaluated. The focus on community needs allows programmes to remain responsive. Third, population-based practice considers the determinants of health, such as income and poverty, employment and occupation, education, housing, social cohesion, culture and ethnicity (National Health Committee, 1998), which promote or prevent health (R. Wilkinson & Marmot, 2003). Fourth, population-based practice considers all levels of prevention and prioritises primary prevention, promoting health and preventing problems before they occur. Prevention is an action taken to prevent the occurrence of an event or to reduce the effect after it has occurred (Turnock, 2001). Population-based practice presumes that prevention may occur before a problem occurs, when a problem has begun but before signs appear, or after a problem has occurred. 40 “A population-of-interest…is essentially healthy, but who could improve factors that promote or protect health” (Minnesota Department of Health, 2001, p. 2). 41 “A population-at-risk…has a common identified risk factor or risk-exposure that poses a threat to health” (Minnesota Department of Health, 2001, p. 2). 90 Finally, population-based practice considers interventions at all levels of practice. Interventions may be directed at entire populations within a community, the system that affects the health of those populations, and/or the individuals or families within those populations known to be at risk. Interventions at each of these levels of practice contribute to the overall goal of improving population health status. Public health professionals determine the most appropriate level/s of practice based on community need and the availability of effective strategies and resources (Keller, Schaffer, LiaHoagberg, & Strohschein, 2002). 4.5.1.2 Individual and family, community, and systems levels of practice Nurses, where possible are expected to use interventions at all three levels of practice, although traditionally nurses have documented their work with individuals and families for reimbursement, reporting and productivity purposes (Keller et al., 2004a). Keller et al. contend work with communities and systems has equal if not greater importance compared to work with individuals and families, when considering the goal of improving population health. This principle is central to the intervention wheel. Figure 4: Population-based systems level of practice 91 Population-based systems practice has the potential to change organisations, policies, laws, and power structures (Keller et al., 2004a). At the systems level the focus is on the systems that impact health, not directly on individuals and communities. Changing systems is considered a more effective and sustainable way of impacting on population health than requiring change from every individual in a community. An example of systems level practice is demonstrated when a nurse who works with a network of health provider organisations establishes best practice standards around depression management and all parties adopt these guidelines. Figure 5: Population-based community level of practice Population-based community practice changes community norms, community attitudes, community awareness, community practices, and community behaviours. It is directed towards entire populations within a community or occasionally towards targeted groups within this population. Community practice is measured in terms of what proportion of the population actually changes (Keller et al., 2004a). An example of community level practice is demonstrated by a nurse who works with community agencies and health provider organisations to increase community awareness of mental illness, seeking to change community attitudes and behaviours and thereby reduce the stigma of mental illness experienced by many people. 92 Figure 6: Population-based individual and family level of practice Population-based individual practice changes knowledge, attitudes, beliefs, practices, and the behaviours of individuals. This practice level is directed at individuals, alone or as part of a family, class or group. Services to individuals and families are population-based if they meet specific criteria, such as individuals receiving services because they are members of an identified population, and those services clearly contribute to improving the overall health status of the population (Keller et al., 2004a). An example of individual level practice is demonstrated by a nurse who case manages health care services on behalf of a frail older person with chronic mental health problems. In summary nurses determine the most appropriate level/s of practice based on community need and the availability of effective strategies and resources. All levels of practice are important and as shown can address an issue simultaneously. 4.5.1.3 Seventeen public health interventions Interventions are actions taken on behalf of communities, systems, and individuals and families to improve or protect health status. The 17 interventions comprise surveillance, disease and other health investigation, outreach, screening, case finding, 93 referral and follow-up, case management, delegated functions, health teaching, consultation, counselling, collaboration, coalition building, community organising, advocacy, social marketing, and policy development and enforcement (see p. 95, Table 5). These interventions can be implemented at all three levels, with the exceptions of case finding, which occurs only at the individual level, and coalition building and community organising, which occurs only at the community and systems levels. Related interventions have also been grouped into ‘wedges’. Surveillance, disease and health investigation, outreach, screening, and case finding comprise one wedge. Interventions comprising other wedges are: referral and follow-up, case management, and delegated functions; health teaching, consultation, and counselling; collaboration, coalition building, and community organising, and finally advocacy, social marketing, and policy development and enforcement. The wedges are placed on the wheel in an order that reflects their relationship, with surveillance placed at the top of the wheel because it is the place where most public health work begins (Keller et al., 2004a). 94 Table 5: Definitions of public health interventions Intervention Definition Surveillance Describes and monitors health events through ongoing and systematic collection, analysis, and interpretation of health data for the purpose of planning, implementing, and evaluating public health interventions Disease & health event investigation Systematically gathers and analyses data regarding threats to the health of populations, ascertains the source of the threat, identifies cases and others at risk, and determines control measures Outreach Locates populations-of-interest or populations-at-risk and provides information about the nature of the concern, what can be done about it, and how services can be obtained Screening Identifies individuals with unrecognised health risk factors or asymptomatic disease conditions in populations Case-finding Locates individuals and families with identified risk factors and connects them with resources Referral & follow-up Assists individuals, families, groups, organisations, and/or communities to identify and access necessary resources in to prevent or resolve problems or concerns Case management Optimises self-care capabilities of individuals and families and the capacity of systems and communities to coordinate and provide services Delegated functions Direct care tasks a registered professional nurse carries out under the authority of a health care practitioner as allowed by law. Delegated functions also include direct care tasks a registered nurse entrusts to other appropriate personnel to perform Health teaching Communicates facts, ideas and skills that change knowledge, attitudes, values, beliefs, behaviours, and the practices of individuals/families, systems, communities Counselling Establishes an interpersonal relationship with a community, a system, family or individual intended to increase or enhance their capacity for self-care and coping. Counselling engages the community, system, family or individual at an emotional level Consultation Seeks information and generates optional solutions to perceived problems or issues through interactive problem solving with a community, system, family or individual. The community, system, family or individual selects and acts on the option best meeting the circumstances Collaboration Commits two or more persons or organisations to achieve a common goal through enhancing the capacity of one or more of the members to promote and protect health Coalition building Promotes and develops alliances among organisations or constituencies for a common purpose. It builds linkages, solves problems, and enhances local leadership to address health concerns Community organising Helps community groups to identify common problems or goals, mobilise resources, and develop and implement strategies for reaching the goals they have agreed Advocacy Pleads someone’s cause or act on someone’s behalf, with a focus on developing the community, system, individual or family’s capacity to plead their own cause or act on their own behalf Social marketing Utilises commercial marketing principles and technologies for programmes designed to influence the knowledge, attitudes, values, beliefs, behaviours, and practices of the population-of-interest Policy development & policy enforcement Places health issues on decision-makers’ agendas, acquires a plan of resolution, and determines resources. Policy development results in laws, rules, regulations, ordinances, and policies. Policy enforcement compels others to comply with the laws, rules, regulations, ordinances and policies. From “Population-Based Public Health Nursing Interventions: A Model from Practice,” by L. Keller, S. Strohschein, B. LiaHoagberg, and M. Schaffer, 1998, Public Health Nursing, 3, p.210. Copyright 1998 by Blackwell Science Incorporated. Adapted with permission of the author. 95 4.5.2 Validated and evidence-informed The idea of the intervention wheel began in 1994 with a collection of practice examples from over 200 experienced public health nurses in Minnesota. A panel of practice experts identified common themes from the examples, which were then depicted as spokes of the wheel. Numerous copies of the interventions were critiqued throughout the nation. A federal research grant in 1998 enabled a systematic review of the evidence relating to the interventions, and this information combined with theory and expert opinion informed the intervention wheel. The process involved hundreds of public health nurses in the United States over an 18 month period (Keller et al., 2004a; Minnesota Department of Health, 2001). The following six questions guided the review process: 1. Did the 17 interventions encompass the breadth of public health practice? 2. Did the interventions occur at all levels of practice? 3. Were there missing interventions, or public health nursing activities that could not be classified into existing interventions? 4. Were there overlaps or duplications among the interventions? 5. Did the evidence support the original interventions? 6. How could these interventions be implemented with excellence? 4.5.2.1 Findings of the review of the intervention wheel The intervention wheel was found to capture the breadth and scope of populationbased nursing, and provided a solid foundation for nursing practice and research. The original assumption that the interventions occurred at all levels was revised to reflect the three interventions that were exceptions to this assumption (see p. 94). There were no missing interventions, although there was a recommendation that the original ‘policy development’ be expanded to include ‘policy development and enforcement’ to reflect the expert consensus that without enforcement, policy development is ineffective. The interventions were found to be distinct and separate, although many were interrelated or occurred simultaneously or sequentially. This resulted in a 96 reordering of the interventions on the outside of the wheel to reflect relatedness. In addition, several interventions were modified, such as provider education, which was integrated into health teaching, because of the recognition that provider education was actually health teaching at the systems level. Other modifications included ‘delegated medical’ being expanded and renamed ‘delegated functions’ to reflect nursing responsibility for delegating to others as well as accepting delegation, and ‘disease investigation’ was expanded to ‘disease and other health investigation’ to encompass other threats to health including acts of bio-terrorism, chemical or other hazardous waste spills, and natural disasters. The evidence confirmed the definitions of the interventions and was used to identify basic steps and recommend best practices for each intervention. A significant challenge to documenting best practices was a lack of evidence, so best practices were a combination of research, other evidence from the literature and practice expertise (Keller et al., 2004a). In 1999, a 46-member panel of public health nurse experts and academics from several states participated in a consensus meeting and agreed the set of interventions. These regional recommendations were reviewed by a national panel of public health nurse experts who required few changes to the original set of 17 interventions presented in Figure 3 (see p. 89) (Keller et al., 2004a; Minnesota Department of Health, 2001). 4.6 In conclusion The New Zealand PHC nursing workforce is a collection of nursing groups with differing historic experiences and knowledge. Building a combined workforce with expertise in primary health care will require more than “ongoing education…in specific practice areas (e.g., district nursing, practice nursing) or for additional skills (e.g., asthma management, immunisation)” as suggested by the Ministry of Health (2003b, p. 9). Repositioning the PHC nursing workforce to work with communities, improve population health outcomes and reduce health inequalities to meet the objectives of the PHC Strategy will require new public health knowledge and a way to integrate these concepts into PHC nursing practice. 97 The New Zealand Government has identified the potential future contribution PHC nursing can make in reducing inequalities, and to this end has invested in PHC nursing workforce development through the funding of postgraduate education and innovative models for nursing practice. The direction is clear and the road map drawn, however, access to education does not necessarily translate into major shifts in nursing practice and the culture surrounding practice, just as new models of practice (of varying degrees of innovation) may not necessarily result in a redesign of service delivery. Whilst Government has progressed important nursing initiatives, without a common core PHC nursing knowledge and an understanding of how to implement community care and promote community development, in addition to the conventional care provided to individuals and families, the potential contribution of PHC nursing will be limited. The public health interventions wheel provides a vision of the range and levels of future population-based practice. Presented as a model that has the capacity to demonstrate PHC nursing as a specialty area of practice, it can assist nurses to understand practice at the community and systems levels, in addition to the individual and family level. Each intervention and level of practice contributes to improving overall population health making the wheel a useful tool in the implementation of PHC nursing practice. To date, New Zealand has not articulated a national framework for guiding population-based practice and this model has the potential to contribute to meet that challenge. Chapter five presents integrated care, a public health reform strategy of the 1990s as an outcome of the socio-political environment that aimed to promote primary health care. The notion of integrated care was tested by the government funding of a number of national experimental, demonstration pilot projects, within which health professionals including nurses were employed. The purpose, design, and evaluation of demonstration pilot projects are comprehensively described. 98 5 5.1 Chapter 5 Integrated Care Introduction In New Zealand the duplication and fragmentation of health care services during the twentieth century was in part due to the way services were provided. Independent general practice physicians provided primary care, public hospitals provided community services, secondary and tertiary care, and various other providers provided community care services (Russell, Cumming, Slack, Paterson, & Gilbert, 2003). They suggested integrated care was not a new strategy, and for more than a decade had been considered a solution to the fragmentation of service delivery between primary and secondary care. In 1975 the government identified the need for closer liaisons between general practices and hospital services and favoured the strategy of integrated care (Department of Health, 1974). A health system review in 1986 advised on changes to better integrate care (Health Benefits Review, 1986), and this theme was again followed up in the 1990s linking integrated care with the total management of an individual’s health care, including the funding of all services by the purchasing authorities (Upton & New Zealand Department of Health, 1991). Integrated care, by the mid-1990s, was also strongly associated with the idea of ‘chains of care’ (Ovretveit, 1998) and the containment of health care costs (Russell et al., 2003). Internationally, a central purpose of integrated care was the development of a systems approach, maximising health gain from targeted resources, effective interventions, and emphasising care and prevention in the management of chronic conditions (Bringewatt, 1997; Ovretveit, 1998). Integrated care was a consistent objective of health reforms in the 1990s in Australia, the United States, Canada, the United Kingdom, Scotland, and New Zealand, although there were a number of reasons for seeking integrated care and many methods for achieving it. In recent times the New Zealand health system has restructured more rapidly than any other system in the world (T. Ashton, 1998), and despite the successive bouts of semantic redesign, it is not clear that either those in the health sector or the public agree precisely what integrated care is. The risk of this uncertainty is that advocates and opponents of 99 specific approaches to integrated care can pursue individual agendas within an environment of confusion. The purpose of this chapter is twofold. First, the background and environment within which integrated care developed is discussed and the various meanings attributed to integrated care, including beliefs by Maori, are identified. This is followed by a description of national demonstration pilot projects that sought to test the strategy of integrated care. As the planning and implementation of these projects was documented, the context and understanding of integrated care in New Zealand during this time is illustrated. The chapter concludes with the identification of the need for research to clarify aspects of integrated care. In particular, the need for research on the practice of nurses in integrated care projects is highlighted. 5.2 Recent background In New Zealand, in December 1996, the coalition Government announced changes to the health sector. In just 18 months (July 1998) one funding body was to replace the four regional health authorities and regional hospital and community services. The assets and liabilities of the four regional health authorities were vested in a transitional health authority one year earlier (Health Funding Authority, 1998). Lack of the migration of ideas across regional health authorities is the major reason for restructuring (Scott, 1997). At this time integrated care was recognised as critical to the development of an effective and efficient health care system (Entwistle, 1997) and as a health reform strategy, was inherited by the transitional health authority. The steering group advising Government on changes to the coalition agreement considered integrated care one of the most promising developments in contracting in New Zealand and internationally in regard to coordination, cost-effectiveness of treatments and improved health and independence outcomes (New Zealand Steering Group to Oversee Health and Disability Changes, 1997). Integrated care policy had 100 been actively supported by regional health authorities and health provider organisations since the early nineties, with the northern regional health authority focusing on improved integration and population purchasing in 1993 (Boyd, 1998). Issues for ongoing discussions included implementation issues, such as provider behaviour, public lack of understanding, political actions, levels of provider trust, and the coordination of care. Fiscal risks, such as limited budgets, cash flow, and risks of provider failure, and information systems were also concerns on the same agenda. Integrated care was a strategic objective in the Transitional Health Authority’s ‘statement of intent’, tabled in the House of Representatives as a purchasing method to develop appropriate services that bridge the interface between primary, secondary and tertiary health services, and health and disability support services, ensuring coordinated care and intersectoral collaboration (Scott, 1997). In January 1998 the Transitional Health Authority became the Health Funding Authority, responsible for purchasing all publicly funded personal health and disability services within a capped annual budget (see Appendix 1). Ashton (1998) suggests the Health Funding Authority viewed integrated care as a mechanism for aligning both clinical and financial objectives. More specifically, the aim was to integrate care for patients by addressing the linkages between the chains of service providers, and provide solutions to the management of financial risk in the funding of health services. 5.3 Central problem: Fragmentation between services In New Zealand, consumers move through a chain of providers42 for diagnosis and treatment. The fragmentation of service delivery between primary and secondary care has been noticeable for two main reasons. Historically, primary and secondary care has been funded and organised in different ways. General practice physicians are commonly self-employed and paid on a fee-for-service basis, and consultations are time-limited with clients frequently referred on to other services. In contrast, public 42 For the purpose of this thesis, providers are defined as entities that provide health and disability support services either directly or indirectly through, for example, subcontracting type arrangements. 101 hospitals have generally been paid by block budgets with hospital doctors on salaries. This arrangement provides little incentive to increase throughput or speed service delivery and because of the lack of integrated care, both primary and secondary providers have the incentive to cost shift to each other43 (T. Ashton, 1998). A second reason for fragmentation of patient care is because general practice physicians act as gatekeepers for referral to publicly funded hospital specialists and services, and cannot admit their patients to public hospitals or provide care in the hospital setting44. Links between general practice physicians and hospital specialists have depended primarily upon the exchange of records, letters and telephone calls, and whilst these types of arrangements constitute simple forms of shared care (Hickman, Drummond, & Grimshaw, 1994), integrated care is more than provider cooperation, centring on changing the way services are organised (Central Health, 1997a). In 1993 the introduction of a quasi-market for health services necessitated contracting between purchasers and providers, and the problem of fragmentation of services was exacerbated. Many services were broken down into separate packages, and single provider organisations would often hold a range of contracts with the same purchaser for a related set of services. Breaking services down in this way could increase competition and consumer choice because it encouraged smaller providers to offer particular components of care rather than a whole spectrum of services. However, this method of contracting created new service boundaries and had the potential to negatively affect the way patients’ moved between services. Fragmentation of service delivery not only reduces the quality of care, but also is likely to be inefficient. Fragmentation produces both a duplication of services and a lack of necessary services to patients who falls though the gaps between services. 43 Another influential factor in this pattern of service use has been the fact that patients must pay a copayment for general practice consultations and also pharmaceuticals, whereas specialists and hospital services are free of charge. Therefore, patients have an incentive to choose hospital services whenever possible, and general practice physicians may also seek hospital care as a means of reducing out-ofpocket payments for their patients. 44 There are some exceptions, most notably for maternity services, and in some rural hospitals. 102 Providers referring patients on to other providers have no incentive and often little information to consider the marginal costs of that referral in relation to the value of the expected outcome. The purchaser, on the other hand, has more information about service costs, but has no information about the potential value of a service for individual patients, and is largely responsible for determining the level of services. This situation is based upon historical utilisation patterns and fiscal capacity rather than upon any analysis of the correct level and mix of services. General practice fund-holding was a main response to the dual problems of costshifting and service fragmentation in the United Kingdom. In New Zealand almost 70 per cent of general practice physicians are involved in budget holding arrangements for pharmaceuticals. However, incentives to promote integrated care or to contain expenditure have been limited because: budgets are held by organisations called Independent Practitioner Associations, rather than by individual general practice physicians or groups of practices; budgets do not cover hospital services, and are limited to pharmaceuticals, laboratory tests, and sometimes selected community services; budgets are nominal rather than real, so money does not change hands unless there is a surplus at the end of the contract period45, and any budget constraint on general practice physicians is weakened by the fact that patients must pay a copayment for consultations. New Zealand Independent Practitioner Associations were expected to play an important role in promoting integrated care, although the Health Funding Authority considered a wider range of options. Most notably, Aetna Incorporated, a United States insurance company, established a network of general practices throughout northern New Zealand and offered medical services to the Health Funding Authority at a discounted rate. Aetna held the full risk for primary care, pharmaceuticals, and laboratory services, supplied by member general practice physicians, and the shift of financial risk to private insurers proved attractive to the Health Funding Authority. 45 Surpluses are usually shared between the budget holder and the purchaser, with any losses usually taken by the purchaser. 103 5.4 Integrated care: Different definitions and meanings International literature reveals that in different countries a range of terms have been attached to integrated care (Anderson, 1998; Feek, 1998; Kodner & Spreeuwenberg, 2002) and the lack of a commonly accepted definition has been a barrier to the promotion of integrated care theory and practice (Kodner & Spreeuwenberg, 2002). In the United States ‘managed care’ is used, whereas ‘coordinated care’ has been adopted in Australia, and ‘shared care’ is the preferred term in the United Kingdom. Other terms in usage in Europe include ‘seamless care’, ‘continuous care’ and ‘chronic care management’ (Schrijvers, 2001). As previously stated, the ideas behind integrated care in New Zealand were not new (Russell et al., 2003). In the early 1990s, politicians, health professionals, managers and policy-makers commonly used the term integrated care interchangeably with ‘coordinated care’ (Ministry of Health & Coopers & Lybrand, 1995) and ‘managed care’ (Marwick, 1996). Malcolm and Shalowitz (1997) argued managed care had been led in New Zealand by Independent Practitioner Associations and was linked to the commercialisation of the health system. Independent Practitioner Associations promoted the benefits of managed care to clients and practitioners, and their involvement with large American insurance companies such as Aetna Incorporated generated concern because of the possible prioritisation of profit before care. However, after the 1996 general elections in New Zealand, ‘managed care’ was replaced by the euphemism ‘integrated care’. This change was in response to negative publicity in New Zealand surrounding the failure of the United States health care system to contain costs and provide adequate access to services (D. Armstrong, 1988; Pert, 1998). Like Malcolm and Shalowitz (1997), they proposed that managed care and coordinated or integrated care were synonymous and the name change was purely to remove the stigma attached to United States managed care models. Wano (2003) contended integrated care was never fully embraced by Maori because it was identified as synonymous with managed care and cost cutting. The notion that the central purpose of integrated care was to accommodate to reduced government funding had been argued a few years earlier in countries such as Canada (Wilson, 1996). In 1999, Wyatt Creech, the acting New Zealand Minister of Health, officially 104 grouped managed care and coordinated care approaches under the banner of integrated care (Creech, 1999), although the meaning remained contested. Wood (2001) argues that the adoption of the term integrated care in New Zealand as in Scotland, represented a decisive shift against competition as the mechanism for service quality and cost control. It has been strongly argued that integrated care in New Zealand placed an emphasis on intersectoral collaboration for the purpose of coordinating clinical care and producing better patient outcomes (R. McCormick, 1997; R . McCormick & Ranger, 1997), whereas managed care emphasises containing health care costs (Ovretveit, 1998). This understanding is similar to one proposed in a position paper for the World Health Organisation, in which integrated care is defined as “a concept bringing together inputs, delivery, management and the organisation of services related to diagnosis, treatments, care, rehabilitation and health promotion” (Grone & GarciaBarbero, 2001, p. 4). The following section 5.4.1 identifies the definition of integrated care for use in the NICPS before discussing various other meanings and definitions attributed to integrated care. The practice environment of health professionals can be better understood by clarifying the complexity of integrated care. 5.4.1 NICPS definition of integrated care Integrated care is the “methods and type of organisation which will provide the most cost effective preventative and caring services to those with the greatest health needs and which will ensure continuity of care and coordination between different services” (Ovretveit, 1998, p. 1). This understanding of integrated care is used in the study of nurses in integrated care projects and describes integrated care in terms of working collaboratively whilst also focusing on positive economic outcomes. Ovretveit’s definition contrasts with that of McCormick and Rainger (1997) who argue integrated care stresses processes and agreements, unlike managed care which begins by defining structures for health provision and agreeing financial incentives. 105 Cost effectiveness is a central requirement in the definition of integrated care (Ovretveit, 1998), as are notions of continuity and coordination. In the New Zealand health care system, which has a public market46, the term integrated care can describe both managed care ideas applied within public systems and other ideas such as ‘chains of care’ or ‘care pathways’. The aim of integrated care within this definition is to maximise health gain from a defined resource by targeting populations, applying effective interventions and linking different services. The focus is placed on the most serious health needs to create an effective health care system that includes prevention and health promotion, with interventions working synergistically. Ovretveit (1998) maintains that within the New Zealand public market system the objectives are to: increase access to care for those most in need and who can benefit; improve the continuity of care and coordination between services for individuals; reduce costs by reducing inappropriate use of services, influencing the choice of interventions, introducing cost-saving substitution, shifting resources from tertiary and secondary care to primary and preventative services, overcoming financial barriers to effective interventions, and creating financial risk-sharing arrangements with providers to encourage more cost-effective actions. The methods for achieving this include: agreements and contracts, improved information systems, guidelines and protocols, utilisation controls such as gate-keeping, and discharge planning, pooling finance from separate sources, financial incentives (removing financial disincentives), new organisation, and integrated care. These methods assist in the management of a complete episode of care, and combined with an overview of the populations needs can lead to improving the range of services designed to meet those needs over the longer term. Integrated care and devolved purchasing is potentially a way to increase systems quality. 46 Health systems in both the United Kingdom and Sweden have also introduced public markets, whereby a public purchaser or funder contracts services from separate and often competing organisations. This system often results in professions and services concentrating upon the elements of service that they are contracted to provide, despite consumers needing a range of services provided by different organisations. 106 5.4.2 Perspectives of Ministers, advisors and purchasers Previous Ministers of Health described integrated care in terms of new provider relationships and strategic alliances (Shipley, 1995) and as a process driven from the grassroots, starting with communities and individuals working in partnership (English, 1997). These ideas are similar to those held by regional health authorities, who stated integrated care was the coordination of primary and secondary health and disability support services, and providers would partner patients in their journey through the health care system (Central Health, 1997b; Coster, 1998; Crombie & Gedye, 1997). Such statements implied integrated care was about people, partnerships and services to improve health, although they revealed little about the processes required to achieve integrated care. Davies (1999) suggests that there are two separate but potentially complementary aspects to integrated care, service coordination and devolution of purchasing responsibilities. Keating (1998) conceives integrated care provides services to meet peoples’ needs, improves coordination and communication between providers and reduces the duplication of administrative and clinical procedures, a notion synonymous with service coordination. Marwick (1996) maintains integrated care includes the management of budgets for the care of a population, consistent with the devolution of purchasing responsibilities. Whilst these perspectives are potentially complementary and Davies, Keating and Marwick are all senior employees within the Ministry of Health, it is interesting that they are not expressed in any related way. Karen Wells, the national integration manager for the Health Funding Authority in 1997, stated integrated care was a policy solution to manage resource allocation and systematically devolve economic decision-making, or rationing decisions, to the providers of services. Implementation was to result in structural reform of the New Zealand public health system, and integrated care was the key reform strategy (Wells, 1998). The reason for devolving decision making to providers related to the health professional (rather than the Health Funding Authority) having consumer level information, necessary for determining appropriate service decisions. In addition, 107 providers were also considered able to better determine specific service levels and where to make trade-offs between services (McKenzie, 1997). Whilst these are advantages, there were also accompanying risks for providers who had to provide specified services within restricted budgets. As a contracting strategy, integrated care used incentives to: align clinical decision making with the right mix of health and disability support services, purchase services on an outcome basis, influence provider responsiveness to consumers, and manage risks related to increased demand and reduced utilisation. The scope of integrated care ranged from a group of related services currently contracting with the funder using shared guidelines and information systems, to a capitation payment for wide scale integrated care between primary and secondary services (McKenzie & Webster, 1997). If the implementation of integrated care was to result in reform of the public health system as suggested by Wells (1998) it is difficult to see how this would have occurred given the predominant focus on health care provision. A public health system requires consideration of the social and economic determinants of health (Beaglehole & Bonita, 1997). Definitions of integrated care previously referred to partnerships with health providers and clients within the primary and secondary care sectors, rather than intersectoral partnerships with for example, housing, education, and welfare. However, integrated care could potentially have adopted a wider approach across other sectors and have directed attention to inequalities in housing, employment, and education, factors known to impact upon health (R. Davis, Wagner, & Groves, 1999). Such an approach is consistent with the public health concept of primary health care, and accords closely with the views of some Maori (Russell et al., 2003). Feek (1998) suggests the allocation of health resources in integrated care is an important ethical issue, and it becomes even more complex when social services and providers in sectors other than health are included. Changes to the New Zealand Public Health and Disability Act 1999 resulted in the development of national strategies including the PHC Strategy, which signposted a way to improve the primary health care of New Zealanders and was accompanied by structural reforms. District health boards and primary health organisations (see p. 82) were established (see Appendix 2), building on the strengths of earlier integrated care developments, which 108 had encouraged intersectoral collaboration and in particular, health provider partnerships. 5.4.3 Types of integrated care The direction of organisational relationships across and within sectors has been differentiated as either vertical or horizontal (Shortell, Gillies, Anderson, Erickson, & Mitchell, 1996). Vertical integration occurs between organisations in different sectors such as general practice (primary) and the hospital (secondary). In contrast, horizontal integration occurs between organisations within the same sector, such as general practice and other primary health care organisations. Both horizontal and vertical integration were promoted by the Health Funding Authority (1998) as a means of reducing the fragmentation of services by improving collaboration and coordination between providers. Critics such as Anderson (1998) however, suggest viewing integrated care in this way is not useful because it is constrained by primary and secondary care boundaries. Anderson’s interpretation attributes considerable weight to a description that has sought only to define the direction of the relationship. In addition to the idea of vertical and horizontal integration, Shortell et al. (1996) described three components of integrated care - functional, physician-system, and clinical, maintaining all were important. Functional integration referred to organisations having shared systems, such as, information, financial management, and quality, and also engaging in strategic planning. Physician-system integration referred to the need for physicians to be actively involved in the planning, management, and governance of integrated care, and clinical integration referred to the coordination of health services delivered by provider organisations to clients. The three components define ways of ‘doing’ integrated care and can relate to both vertical and horizontal integration, allowing a fuller description of integrated care to be ascertained in differing contexts. 109 5.4.4 Strategies for integrated care A range of strategies for promoting integrated care were advocated, with collaboration the most widely discussed overarching strategy (Health Funding Authority, 1998). Specifically, strategies of case management and guideline development were encouraged and promulgated as a means of achieving integrated care by the Health Funding Authority. Literature relating to these key ideas is outlined in sections 5.4.4.1 to 5.4.4.3. 5.4.4.1 Collaboration Collaboration commits more than one person or organisation to achieve a common purpose through enhancing the capacity of one or more people or organisations to promote and protect health (Henneman, Lee, & Cohen, 1995). Promoted as a strategy for integrated care (Health Funding Authority, 1998), collaboration was tested in the early 1990s by Independent Practitioner Associations. Woods (2001) observed, New Zealand GPs who participate in associations of independent practitioners have had budgets for an expanded range of services devolved to them….the trick appears to be to develop an approach that builds on professional relationships by progressively extending the influence of primary care practitioners over other parts of the health care system as reward for demonstrable competence in their discharge of increased management and financial autonomy (p. 9). Malcolm (1997) suggests “professional incentives, based on collaboration, can be much more effective than market and commercial incentives in modifying professional behaviour…” (p. 4). Integrated care presented an opportunity for medical clinicians to develop professional relationships in the interests of longer term clinical outcomes, and the devolution of services benefited general practice physicians 110 financially without any loss incurred by hospital clinicians who were generally on salaries. By contrast, there have not been professional incentives based on collaboration for the expansion of nurses’ practice, which also has the ability to influence clinical outcomes. Within the primary sector, (practice) nurses roles have been described as assistive and compensatory (to general practice physicians) with limitations to the access of resources, physical workspace, and postgraduate education, preventing their potential contribution (College of Nurses Aotearoa (NZ) Inc., 2001). Although collaboration between general practice physicians and nurses is critical to the success of primary health care teams, nurses have not been supported by general practice physician colleagues to contribute at a governance level influencing funding and service delivery. 5.4.4.2 Case management The Minnesota Department of Health (2001) contend that “case management optimises self-care capabilities of individuals and families and the capacity of systems and communities to coordinate and provide services” (p. 93). Case management has similarly been defined as a “purposeful interaction coordinated among multiple providers and vendors with the intention of meeting the client’s needs effectively” (Weil & Karls, 1985, p. 123). Numerous case management models are described in literature relating to social services, health care, and nursing (Brault & Kissinger, 1991; DeSimone, 1988; Papenhausen, 1990; Weil & Karls, 1985). Two common case management models are the ‘brokerage model’ and the ‘clinical case management model’. Facilitating access, brokering, and coordinating services are features of the brokerage model, emphasising the “coordination and organisation of services for clients” (Kanter, 1989, p. 114). The term care management rather than case management is used by the British Social Services with regard to the brokerage model (Burns, 1997). Providing clinical care and delegating and supervising other nurses with clinical care are features of a clinical case management model, which follow the ‘Assertive 111 Community Treatment (ACT) model’ emphasising assertive outreach (Stein & Test, 1980). Assertive outreach involves the case manager maintaining contact with the client over the long-term (Ford, Beadsmoore, Ryan, Repper, & Mattmuijen, 1995) and there is wide consensus that all models should include this element. Maurin (1990) maintains “that assertive outreach helps clients to achieve maximum levels of functioning in the least restrictive settings” (p. 115). Marshall, Gray, Lockwood and Green (1998) noted the ACT model utilised multidisciplinary case management teams that provided interventions in the community and clients homes, held case loads of 10 - 15 clients, and the team undertook most of the interventions as opposed to referring onto other services. There is mounting evidence of clinical case management models being more effective than the brokerage type of model in maintaining a client’s health in a primary health care setting (Thomas & Lovell, 1999). The clinical case management model overlaps with certain aspects of other models, such as, the development of an individual’s strengths (Modrcin, Rapp, & Poertner, 1988), rehabilitation, medication management and social skills (Goering, Wasylenki, Farkas, Lancee, & Ballantyne, 1988), or the coordination of services (Kanter, 1989). Marshall et al. (1998) in reviewing case management found the ACT model was the only model to have been used as an alternative to acute hospital admissions. Hospitalisation as an outcome measure has received criticism (Bachrach, 1982), but remains the most frequently reported variable. Other variables include economic analysis, symptom reduction, compliance with medication, quality of life measures, and social functioning, which have been more difficult to compare across studies due to the differences in client groups, methodology, case loads, assessment tools, period of follow-up and case management models (Thomas & Lovell, 1999). 5.4.4.3 Guideline development Clinical or practice guidelines, pathways, care maps and protocols are referred to collectively as guidelines. Guidelines can be statements that assist practitioners and 112 clients make decisions about health care in specific clinical circumstances or can be detailed information on health care provision to assist client journeys. Guidelines cover a variety of topics including treatment, prevention and screening, and provide physicians, nurses, other health professionals, and clients with a resource for obtaining information on clinical practices. Jensen and Koerner (1999) suggest As hospital-based care moves into the community, longitudinal clinical pathways, with greater emphasis on health maintenance and self-care of chronic conditions, help to focus attention on longitudinal outcomes. In the future, visual trajectories from these outcomes may be consumer-friendly tools to help client-provider partnerships to understand and manage self-care and health maintenance (pp. 154-155). Nurses were found to champion integrated care pathways, viewing them as a tool to assist clinicians achieve a balance between the “clinical and resource dimensions of care and between the requirements of both clinical autonomy and transparent accountability” (p. 651) in a recent cross-national survey of 3065 healthcare professional’s attitudes to health reforms (Degeling, Maxwell, Kennedy, & Coyle, 2003). This seminal study found that nurse managers and nurse clinicians in four countries, including New Zealand, held systematised conceptions of clinical work, and supported multidisciplinary team based systems. This was in contrast to medical managers and medical clinicians who favoured individualist conceptions of clinical work and opposed multidisciplinary teams. Nurses, rather than doctors perceived guideline development as valuable in guiding practice decisions. 5.4.5 Implications of integrated care for Maori Jansen (1998) argues that the Treaty of Waitangi and subsequent Crown legislation established a framework for the response of providers to the Maori dimension of every (health) issue. In the case of integrated care this infers the Crown, or its agent the Health Funding Authority, is obliged to ensure Maori benefit, and Maori expectation is met, such as, the planning and provision of integrated care by Maori for 113 Maori (rangatiratanga - authority over their own affairs). As Durie (1998) suggests “central to the notion of Maori health is Maori control” (p. 1). The Health Funding Authority’s obligation to actively protect Maori interests and improve health status relates to the Treaty guarantee of equality and equity between Maori and other New Zealanders. For the period 1999-200247, a New Zealand government goal for Maori development was extending “economic and social opportunities by significantly improving the health, employment, education and housing status of Maori” (Ministry of Maori Development, 1999, p. 12). Integrated care was an opportunity for Maori provider organisations (MPOs) to address Maori/non-Maori disparities. Kiro (1997) suggests however, that there are also increasing inequalities among Iwi (tribes) that effect Maori health. The funding by government of integrated care raises issues about the way in which Maori health policy reflects other government processes for Treaty settlement with Maori, where dominant views of Iwi and Maori have been reinforced. Kiro strongly contends that these views can lead to a rigid policy approach that continues to disadvantage Maori48 most in need of help. Kelsey (1993) asserts that at the time of integrated care, the National Government’s social policies reflected underlying assumptions about: the need for government to get out of delivering social services, including health; the inherent superiority of market mechanisms for promoting efficiency and effectiveness; the need to reinforce individual responsibility (and family responsibility), and the need to reinforce the nuclear family as basic unit for social support. Commonly referred to as ‘New Right’, this thinking resembles some of the mechanisms utilised by Maori seeking rangatiratanga. A convergence of interest between Iwi Maori, and Government seemed apparent in the conceptualisation of integrated care (see p. 17, hypothesis 7), which sought to test the notion of by Maori for Maori. However, Kiro (1997) maintains the key disagreement was the extent and means to which the Health Funding Authority made provision for Maori health. 47 This timeframe coincided with the recruitment period of the NICPS, December 1999 to February 2001. 48 Pan tribal Maori who live in poor urban areas are a population that is often disadvantaged. 114 Integrated care was never fully embraced because its potential benefits were offset by arguments (within Maori) that it was another way of cutting costs and marginalising Maori based on a strategy that was set to fail (Wano, 2003). Many Maori providers associated integrated care with a capitation-based payment system and were cautious of agreeing to manage a defined Maori population’s health with very restricted funding. Jansen (1998) maintained integrated care purchased in this way would drive providers to focus on disease management because this approach could be assessed in relation to specified outcomes, limiting the financial risk to providers. Whilst numerous risks were identified, integrated care also presented prospects operationally for Maori providers such as, investing in information technology, standardising data, and developing patient management systems. New agreements with partners were considered when they enabled for example, discount benefits from bulk purchasing (Wano, 2003). Integrated care required collaboration, which often led to a change in organisational structure. Agreeing on the structure and legal entity for an integrated care organisation, and in some cases deciding on the shareholder or owner of the entity posed difficulties. Wano contends that a critical factor in developing integrated care was the lack of a clear funding path in which to develop the capacity and infrastructure of an integrated care entity. There were significant risks for many Maori health providers as they were relatively immature49 from an organisational development perspective, despite the potential benefits that collective provider arrangements can bring. With the development of organisational structures and processes, such as patient management systems, many Maori provider organisations were better able to contract with the purchaser to provide disease management services. In general, disease management approaches have an individual biomedical orientation, which can conflict with Maori perspectives of health that embrace family, mental, social, bodily, and spiritual well-being (Durie, 1998). A Maori view of health incorporates overall Iwi development and relationships to the environment and is more than an aggregation of individual health (Durie, 1985). Iwi-based health providers delivering 49 Maori health development came into focus during the 1990s, and Maori health providers grew from 20 in 1993 to more than 220 by the end of the decade (Ministry of Health, 2002c). 115 kaupapa (agenda) Maori services require a broad, inclusive integrated care approach even though this means greater financial risk. This broad inclusive integrated care approach was demonstrated in the Aboriginal coordinated care trials50 in Australia. The Aboriginal coordinated care trials demonstrated a positive or well-health focus, and included prevention and health promotion. It is difficult to say with any certainty why this occurred, although one factor of influence is an Aboriginal view of health that stresses the wider physical, social and spiritual environment (Saggers & Gray, 1991), a perspective common to other first nation people such as Maori. However, it was predicted (Jansen, 1998) that Maori integrated care projects, like the majority of non-aboriginal Australian trials studied (Baum, 1998) would adopt a focus on people with common diseases and medical management (Baum, 1998). This prediction was based on the belief that Maori provider organisations would have to specify the integrated care services provided and those services would demonstrate clinical outputs relating to disease management, as this had been the experience of Maori providers when holding other health contracts. Integrated care projects that were narrowly defined were easier to cost and Maori provider organisations had to manage financial risk for economic survival. Uncertain financial risk prevented wider integrated care experimentation despite Maori provider organisations understanding the philosophical and cultural parameters that also influence health status (Durie, 1998). 5.5 New Zealand integrated care demonstration pilot projects 5.5.1 Conceptual development The conceptualisation and subsequent implementation of integrated care in New Zealand is clearly illustrated in the development of the national demonstration pilot projects. This provides a useful context for situating the NICPS. The general objective of the demonstration projects was to test whether integrated care made a 50 Coordinated care trials in Australia paralleled integrated care in New Zealand with regard to the development of ‘chains of care’. 116 difference in the provision of cost-effective health and disability support services that improved health and independence of New Zealanders (Health Funding Authority, 1998). The demonstration projects sought to test a range of models, although the selection of projects was based upon the ability of an organisation to provide four core competencies considered by the Health Funding Authority as essential for integrated care. These competencies were: service management and coordination; provider coordination through appropriate incentives; accountability to community, providers and purchasers, and continuous quality improvement. Demonstration projects were seen as an opportunity to learn about aspects of integrated care such as costs, benefits and risks (Transitional Health Authority, 1997). Guidelines for projects outlined eight hypotheses that tested the strategy of integrated care (Health Funding Authority, 1998). These were: 1. Decision making guidelines for service provision improve health outcomes and are cost-effective; 2. Contracting strategies that align incentives and promote collaboration across traditional service boundaries improve health outcomes and are cost-effective; 3. Integrating service delivery is dependent upon integrating funding streams; 4. Budget responsibility for a wide range of primary care services improves health outcomes and is cost-effective; 5. Budget responsibility for a specified bundle of services (e.g., mental health or disease states such as asthma or diabetes) improves health outcomes and is cost- effective; 6. Budget responsibility for a full range of services improves health outcomes and is cost-effective; 7. Integrated services networks run by Maori for Maori are more effective and efficient in contributing to improved health outcomes than mainstream integrated service networks, and 117 8. Consumers who make a choice about health service options have improved health outcomes and make more cost-effective choices. In addition, health and independence gain targets for integrated care projects were outlined. Various integrated care strategies became the intervention to be evaluated relative to the hypothesis being tested. The following example was provided. A ‘by Maori for Maori’ organisation forms relationships with a primary health care group and a Crown Health Enterprise (CHE) to integrate services in a region with 50,000 people. They want to create an integrated service network and apply for and become a national demonstration project. For the first 24 months of their development project they decide to test the following hypothesis: Integrated service networks run by Maori for Maori are more effective and efficient in contributing to improved health outcomes than mainstream integrated service networks. They select their priority population: Maori diagnosed with diabetes. They specify the national health and independence gain goal: To reduce the agestandardised diabetes mortality rate among Maori to 30 per 100,000 or less by the year 2002. They specify their health and independence indicator targets for the demonstration period. For example: Improve control of blood glucose levels by x% in year 1 and y% in year 2 Improve control of serum lipid levels by x% in year 1 and y% in year 2 Improve control of blood pressure levels by x% in year 1 and y% in year 2 From: “Service Integration: Guidelines for the development of integration demonstration projects,” by The Health Funding Authority, 1998, p. 10. 5.5.2 Potential risks in integrated care Some of the potential risks in undertaking integrated care were identified by the Transitional Health Authority (see p. 119, Table 6). The purpose of undertaking demonstration projects was to explore, and ultimately manage these risks. Nine integrated care demonstration pilot projects were selected, funded and evaluated, 118 whilst other integrated care projects developed simultaneously, but from the grassroots, initiated by providers. Table 6: Risks Conceptual risk 1. Potential gains from integrated care are not pursued effectively due to insufficient incentives and there is no large improvement in the status quo. 2. The costs of change could outweigh the gains. The resulting noise surrounding the large shifts for the providers, such as loss of autonomy, reduction in income for some, loss of employment for poor quality practitioners, reductions in staff at hospitals and large hospital reconfigurations driven from changes in referral behaviour, may create an expensive resistance to change. 3. Providers forming large monopolies, particularly by vertically integrating with Crown Health Enterprises (CHEs), resisting releasing surpluses to consumers and wide-scale bilateral negotiation problems developing of the sort experienced with the CHEs and Regional Health Authorities (RHAs) in recent years. 4. Labour market and occupational regulation constraints on the supply of health professionals impeding progress. 5. Consumer resistance from provider choice being constrained by integrated care organisations (ICOs) or consumer resistance to having to choose an ICO and be enrolled. Implementation risk 1. The capacity of the Transitional Health Authority (THA) / Health Funding Authority (HFA) and providers to undertake integrated care arrangements. 2. Resistance from providers to engage in proposals that are not as favourable to them in the long term as current arrangements, such as general practice physicians on fee-for-service for general medical subsidy payments. 3. The lack of ability to deal adequately with the large scale proposals which are not well developed but have considerable traction in communities or in the political arena. 4. The ability of the THA to cancel the pilots if they do not succeed. From “Discussion paper on integrated care”, by The Transitional Health Authority, 1997. 5.5.3 Implementation: What actually happened? The Health Funding Authority identified two types of integrated care proposals, existing projects that had already received contracts, and new projects. Eighteen demonstration projects were then selected that varied greatly in size, scope and intention. Three projects were intended to focus on child and youth services. 119 Eventually, however eleven projects were finally selected and two of these did not proceed as demonstration projects. One project, ‘South Auckland chronic obstructive pulmonary disease’51 developed as an integrated care project independent of the demonstration projects, after partners decided against compromising the project’s design. The second, ‘Women’s reproductive health in Tairawhiti’ was never implemented. Of the final nine demonstration projects the Health Funding Authority was unable to prove the majority of the hypotheses (see pp. 117-118) because they did not undertake integrated care in the way that had been conceptualised. For example, four of the eight hypotheses referred to budget responsibility or funding mechanisms, but demonstration projects did not hold budgets as had been originally intended. The Health Funding Authority decided against experimenting with this type of funding arrangement. Similarly, all projects selected were mainstream (did not have a specific ethnic focus), which precluded the seventh hypothesis that related to integrated care for Maori by Maori being tested. A brief description of the nine integrated care demonstration pilot projects that were implemented is reported in Table 7 (see pp. 121-122). 51 The South Auckland chronic obstructive pulmonary disease (COPD) project successfully achieved a number of positive health outcomes with partners contributing financially to the projects sustainability. 120 Table 7: Integrated care demonstration pilot projects New Traditions Hamilton ($150,000) Diabetes Management Mangere ($125,000+$36,000) Diabetes Management North Habour ($172,000) ($150,000 funded earlier project work) Family/Whanau Support Service of Westkids Limited West Auckland ($373,350) Eldercare Canterbury Christchurch ($450,000) Development of an integrated network to provide health care to children (0-14) within the Hamilton area by: improving communication and coordination of services between primary and secondary sectors; developing best practice standards within secondary services; improving case-coordination for children with comprehensive health needs; improving data quality on child mortality and morbidity rates to inform future service provision, and identifying health needs and health care services. Integrated care for clients of the Mangere Health Centre with diabetes, this project built on earlier project work with a public health and health promotion emphasis. Integrated care focused on the use of care pathways, referral protocols, best practice guidelines, information sharing between providers, and establishing a diabetes register. A new diabetes care coordination service was also established and a randomized controlled trial of this service was conducted with clients (n=177) participating. The intervention group received education, support, and help with diabetes when home visits were provided. Integrated care for clients (n=2092) with diabetes registered with Comprehensive Health Services (IPA) in the North Habour area. This project built on an earlier diabetes project work. Integrated care focused on: developing relationships between clients and providers, including Maori; implementing a clinical pathway and referral guidelines; establishing (diabetes) registers and audits; training general practice physicians and practice nurses in diabetes management to enable more complex care to be undertaken in the primary sector and by practice nurses. ‘Westkids’ is an integrated care organisation of all major primary and secondary providers in West Auckland, including Maori providers and Pacific providers. Westkids approach to integrated care in one service, the Family/Whanau Support Service, which provides a community health worker service for sick children (0-17) and their families in need. This project included: conducting research on service users (429 case studies on children and families), developing a new service, use of care pathways, and developing new partnerships at both governance and operational levels. ‘Eldercare’ comprised a number of primary, secondary and tertiary care providers who collaborated and explored ways of integrating funding and improving services for older people (75+) in the areas of: hip fracture, stroke, and acute confusion. Generic projects arose out the three areas, such as, discharge planning, ongoing care in the community, health and home services, co-ordination of services to the elderly, and others with a health promotion component. 121 Congestive Heart Failure Christchurch ($59,800 and funding from another source) Kaipara Care Incorporated Dargaville ($65,000 initially) ProCare Paediatric Asthma Auckland ($581,407) Mental Health Integration Taskforce Auckland ($282,626) A collaborative trial (n=202) that built on earlier project work and tested: the use of best practice guidelines for cardiac failure treatment, and integrated care. The integrated care approach was client-centered and care was shifted from the secondary (hospital) sector to the primary (general practice) sector. Primary care providers gained access to specialist secondary care advice, mobile echocardiograms, and home visits for clients from a specialist (cardiac) nurse. Development of an integrated network of providers (general practice physicians, nurses, pharmacists) in Northland who enrolled and case managed the care of people with diabetes, childhood asthma (under 14 years of age) and the frail elderly, in a rural bicultural environment. Activities included: developing clinical pathways, adapting and utilising diabetes guidelines, and establishing a database of the enrolled population. Integration of paediatric (2-15 years of age) asthma care between general practice and hospital services was tested by conducting a randomized controlled trial. A clinical pathway and guidelines were developed and ProCare general practice physicians were assigned to either the intervention (trained on the use of the guideline) or control (usual asthma care) group. Participants (n=1200) completed a self-administered questionnaire. The aim was to implement a clinical pathway and guideline in general practice and reduce acute episodes of asthma needing hospitalisation. A randomized controlled trial compared the effectiveness of ‘liaison attachment shared care’ with existing models of community mental health care for clients with serious / long-term mental health problems. The intervention used guidelines and a clinical pathway for care managed by a team that included a general practice physician, specialist mental health nurse and medical specialist. This contrasted with the existing model of care in which discharged clients have little or no contact with the general practice physician and no access to specialist mental health nurses. 122 5.5.4 Evaluation findings An evaluation was planned along the lines broadly described in intensive evaluation briefs prepared for each project by KPMG Consulting52 in 1998. The election in 1999 of a Labour (centre-left) government appeared to lessen the political interest in integrated care and the Health Funding Authority contracted the Health Services Research Centre (HSRC), Victoria University, Wellington, instead to conduct a process evaluation of each demonstration project. The HSRC evaluators contended the evaluation was subject to a number of constraints. Apart from being unable to test all hypotheses, the evaluation occurred well after projects had begun, precluding the collection of baseline data and ongoing systematic data. An economic evaluation could not be undertaken because quantitative economic data was not available. In addition, some projects did not collect data, or were unwilling to provide data (Russell et al., 2003). In designing individual project evaluation briefs, the HSRC evaluators considered: project aims; project approach to integration; measures of success as perceived by project personnel and the Health Funding Authority, and the eight hypotheses identified by the Health Funding Authority to test integrated care. Overall, the results of the evaluation were mixed. Most projects could only be assessed on a small number of stated hypotheses, and the approaches to integration varied considerably. A number of these projects were self-evaluated. Aspects evaluated depended upon perceived relevance by stakeholders, project capability, and the available resource. All projects were expected to align with the Health Funding Authority’s commitment to the Treaty of Waitangi, and evidence of the implementation of Treaty principles was assessed. During the evaluation process the evaluators developed a model of integrated care as a guide to assessing integration. The models key concepts included: cooperation and collaboration; Treaty of Waitangi; tools or rules for implementing integration; implementing actions; outcomes of implemented actions, and evaluation (Health 52 KPMG Consulting was also involved in the evaluation of Coordinated Care Trials in Australia. 123 Services Research Centre & Te Ropu Rangahau Hauora a Eru Pomare, 2001). These concepts were evaluated to varying degrees in the nine demonstrate project evaluation reports. Overall, the following key findings and project examples were identified: 1. Successful integrated care projects worked on cultural and attitudinal change with providers. New Traditions, Eldercare Canterbury and Kaipara Care projects used an integrated approach and processes, and projects focusing mainly on implementing guidelines were less well integrated. 2. North Harbour Diabetes Management, Kaipara Care, New Traditions and Westkids showed a strong commitment to the Treaty of Waitangi and supported a bicultural service, responsive to Maori. These projects placed importance on formal agreements and developed focused objectives. The remaining five projects were at varying stages of relationship building. 3. Relationships were enacted or formalised around ‘tools or rules’ such as, bestpractice guidelines, clinical guidelines, referral protocols or care pathways, new information systems and new services. 4. Self-evaluation was a high priority in many of the projects. Congestive Heart Failure, Mangere Diabetes Management, ProCare Paediatric Asthma, and the Mental Health Integration Taskforce conducted trials to assess progress. Some projects incorporated, for example, before-and-after measures to assess the impact of integrated care on diabetes. Some projects lacked the mechanisms or expertise to assess their own work, and external evaluation consultants were contracted by Kaipara Care and Eldercare Canterbury. 5. Data were insufficient to assess whether integrated care results in cost savings or better cost-effectiveness, and improved health outcomes outweigh cost increases. 124 5.6 In conclusion Overall, integrated care demonstration projects did not prove the majority of hypotheses set by the Health Funding Authority. The hypotheses were clearly too ambitious for the majority of projects, as five of the eight hypotheses were unable to be tested due to the design of projects. The integrated care demonstration projects that were implemented did not hold budget responsibility for a range of services, and were not reliant upon contracting strategies to gain incentives, promote collaboration, or integrate funding. The cost effectiveness of new ways of purchasing or providing services could not be ascertained and sufficient data were not collected to access if integrated care improved health outcomes. Service networks for Maori by Maori were also not tested to determine improved effectiveness compared with mainstream approaches. Interestingly, the South Auckland COPD project that did not continue as a demonstration pilot held a budget and successfully produced clinical and financial outcome data (Rea et al., 2004). The Health Funding Authority’s initial intentions, evidenced by the hypotheses, were retrenched not only because projects were unable to test the hypotheses, but also because the Health Funding Authority perceived some risks, such as providers creating large monopolies, were too great. Integrated care demonstration pilot projects, however, established the foundations for developing more comprehensive primary health care by starting to change the culture and attitudes relating to working together across sectors and building relationships. The development of guidelines and information systems were tangible activities that offered opportunities for collaboration with financial benefits. During the time of the pilot projects, district health boards were maturing and most were carrying considerable debt. Little additional financial support for integrated care was available outside of the demonstration project funding restricting the scope of the evaluation. Consequently, the roles of health professionals such as nurses were not 125 assessed. Nurses participated in all pilot projects, and little data exists to define their roles within pilot projects. Chapter six outlines the methods for studying integrated care projects that include the nine demonstration pilots, in order that nurses’ practice can be assessed. The importance of such research is to identify how best to develop more effective and predictive primary health care nursing practice for the future. Information of this nature can inform funding strategies, which impact directly upon health care and service provision. 126 6 6.1 Chapter 6 Methods: Nurses in integrated care projects study Introduction In New Zealand integrated care was considered a major public sector reform strategy initiated from central government (Wells, 1998) that engaged health professionals, including nurses, in efforts to improve primary health care services. Demonstration pilot projects tested innovations in integrated care (Health Funding Authority, 1998). Non-demonstration integrated care projects also evolved directing attention to the provision of health care services in the primary sector. This chapter outlines the New Zealand NICPS (Nurses in integrated care projects study). The aim of the study was to determine the practice of nurses in integrated care projects in New Zealand from 1999 to early 2001. The characteristics of integrated care projects are described to create a context within which nurses’ practice can be situated. Nurses’ practice is assessed to determine the range of interventions and related levels of population-based practice nurses routinely undertake before the health promotion values embedded within this practice are identified. This special-purpose study employed a quantitative non-experimental survey design as the strategy of inquiry. The philosophical basis of the research was postpositivism. The survey design was chosen because it allowed a quantitative or numeric description of the characteristics of integrated care projects for the purpose of identifying the practice of nurses. By studying nurses in integrated care projects, generalisations can be made about this sample population that can be extrapolated more widely to primary health care nursing. A survey questionnaire was used for data collection. In recent times, the survey has become the most commonly used method of data collection in public health research because descriptive data can establish meaning by contrasting, comparing, or identifying relationships (Creswell, 2003). The descriptive survey, like the experiment, can also identify a sample and generalise to a population, but does not seek to test the impact of a treatment on an outcome, as in an experiment (Keppel, 1991). 127 The NICPS examined integrated care project characteristics in an attempt to identify factors that could potentially impact on the practice of nurses in projects. The following variables were investigated: organisational structure; funding; type of service integration; strategies for integration; project approach to level of populationbased practice; age group targeted; ethnic group targeted; low income group targeted; health or disease/condition focus targeted; practice of non-nursing personnel, and the practice of nurses. Two frameworks, the ‘Public health intervention wheel’ and ‘Beattie’s model of health promotion’ were used to analyse nurses’ practice. The former provided a standard against which to assess the range of interventions and the related levels of population-based practice undertaken by all nurses in projects, whilst the latter illustrated the health promotion values inherent within these interventions. The chapter has three distinct components: section 6.2 research questions; section 6.3 framework for the study design, and section 6.4 study methods. 6.2 Research questions Survey data on 80 New Zealand integrated care projects and the practice of nurses in projects was collected and analysed to answer the following research questions: 1. 1. Which characteristics of integrated care are more strongly associated with projects that employ53 nurses? 2. What types of population-based interventions were undertaken by nurses in integrated care projects? 3. What population-based levels of practice (individual-focused, communityfocused, and systems-focused) did nurses demonstrate in integrated care projects? 4. What underlying values are made explicit when interventions undertaken by nurses are analysed? 53 The term ‘employ’ in this thesis means to ‘provide work for’. 128 The NICPS used these research questions to shape the study. The first question investigated ten characteristics or variables of integrated care to determine the context within which nurses practiced. These are: 1. organisational structure 2. funding 3. type of service integration 4. strategies for integration 5. population-based level/s of approach 6. age group targeted 7. ethnic group targeted 8. low income group targeted 9. health or disease/condition targeted 10. non-nursing personnel The second and third questions sought to determine the range of interventions undertaken by nurses, and the extent nurses intervened with communities, the systems that impacted on the health of communities, and/or the individuals and families that comprised communities. The third question applied a theory as a standard against which to measure underlying health promotion values apparent in the practice of nurses in integrated care projects. Collectively, the four research questions sought to describe the practice and values of nurses in integrated care projects. 6.3 A framework for the study design Since many different research approaches are available to investigators, a general framework was adopted to guide the research process (see p. 130, Figure 7). Preliminary steps in designing this study included: assessing the knowledge claims brought to the study, considering the strategy of inquiry to be used, and identifying specific methods. 129 Elements of inquiry Alternative knowledge claims Approaches to research Design processes of research Qualitative Quantitative Mixed Methods Strategies of inquiry Questions Translated into practice Conceptualised By the researcher Methods Theoretical lens Data collection Data analysis Write up Validation Figure 7: Knowledge claims, strategies of inquiry, and methods leading to approaches and the design process From “Research design: Qualitative, quantitative, and mixed methods approaches” by J.W. Creswell, 2003, p.5. Copyright 2003 by Sage Publications: California. Reprinted with permission of the author. Three specific questions developed by Creswell (2003) were considered in relation to the NICPS and established the basis of the study design. They are: 1. What knowledge claims54 were made by the researcher? The NICPS adheres to the major elements of postpositivism55. This position challenges the traditional notion of absolute truth and knowledge (Phillips & Burbules, 2000), recognising that it is not possible to be ‘positive’ about claims of knowledge when studying the practice of nurses. Postpositivism reflects a deterministic philosophy therefore the problems studied examine issues that influence outcomes, such as the approach taken to health promotion and the practice of nurses. It is also reductionist because broader concepts are reduced to ideas that can be tested, such as the research questions. Knowledge developed through a postpositivist lens is based on the measurement of objective reality, such as the interventions of nurses in projects. Recording numeric measures of the practice of nurses was essential. The approach began with the theory of health promotion, and was followed by the 54 Knowledge claims have been referred to as paradigms (Lincoln & Guba, 2000; Mertens, 1998); philosophical assumptions, epistemologies, and ontologies (Crotty, 1998), or broadly conceived research methodologies (W. Neuman, 2000). 55 Postpositivism is often called quantitative research, positivist/postpositivist and empirical science. 130 collection of data on the practice of nurses. The theory provided the standard against which practice was examined. The process was about making claims and then refining or abandoning some of them for other claims more strongly warranted. Information was collected using a survey instrument based on measures obtained from participants. The study sought to develop true statements that could explain the relationships of interest, posed in terms of research questions. Objectivity was necessary to the inquiry, with methods and conclusions examined for bias. Standards of validity and reliability were important. 2. What strategies of inquiry inform the procedures? The NICPS employed a quantitative research design as the strategy of inquiry. Traditionally, strategies of inquiry associated with quantitative research were those that invoked the postpositivist perspectives56. More recently quantitative strategies have involved surveys that seek to address more complex problems, such as those raised in the NICPS. In the present study a telephone interview was used for data collection. The intent was to generalise the findings of the practice of nurses in integrated care projects to primary health care nursing more widely. 3. What methods of data collection and analysis were used? Study data were collected using a predetermined instrument based on questions. Performance data and attitudinal data were statistically analysed. These practices are consistent with accepted quantitative research methods (Creswell, 2003, p. 17). The knowledge claims, the strategies, and the methods contribute to the overall research approach, which tends to be more quantitative. The research approach for the NICPS is described in Table 8 (see p. 132). 56 These include true experiments, quasi-experiments and correlational studies (D. Campbell & Stanley, 1963), and specific single subject experiments (Cooper, Heron, & Heward, 1987; S. Neuman & McCormick, 1995). 131 Table 8: Research approach to the Nurses in Integrated Care Projects Study Knowledge Claims Strategy of Inquiry Pre-determined Quantitative Postpositivism Determinism Reductionism Methods Non-experimental design: Survey Instrument based questions Statistical analysis Empirical measurement Theory verification 6.3.1 Quantitative and descriptive: The survey The present quantitative study is descriptive and cross-sectional. Descriptive crosssectional surveys can occur at a fixed point in time or within a specific timeframe (Hennekens & Buring, 1987), like the present study. Descriptive studies provide an account of the characteristics of individuals, groups, organisations, and situations for the purpose of discovering new meaning. Such studies describe what exists, the frequency of occurrences, and categorise information. Descriptive research can be classified as exploratory in that a process of discovery underpins the research enterprise. From data generated through the process of discovery, meaning is ascribed and interpreted, allowing for the identification of concepts and themes associated with the phenomena under study. Hopkins (1980) maintains that a descriptive study is particularly appropriate when, as in the present study, the interaction of a number of independent variables, such as ‘organisational structure’ or ‘low income targeted’, and their effects on one dependent variable, the ‘practice of nurses’ is investigated. The NICPS had two distinct intentions. The first was to provide data about the practice of nurses within an integrated care environment and the second, to establish meaning by contrasting, comparing or identifying relationships. Hopkins maintains that commonly the first phase is purely descriptive, while in the second phase correlational techniques are used, resulting in knowledge that is generalisable. 132 The survey was selected because this strategy allows the collection of data by asking respondent’s questions and analysing their answers for the purpose of producing statistics. Surveys can be either mailed, delivered self-administered questionnaires, or face-to-face surveys. Better access to certain populations is an advantage of telephone studies (Fowler, 2002) and such surveys are also generally considered by respondents to be less intrusive than those conducted face-to-face (Robson, 1993). The survey can enable comprehensive information to be obtained, obvious misunderstandings to be corrected during interview, and the use of probes to gain fuller answers to survey questions. The survey enables the meaning of a question or any other aspect of the questionnaire to be clarified. Bradburn & Sudman (1979) contend rapport can be more difficult to achieve in telephone surveying compared with face-to-face surveying, although this can be compensated for by smaller interviewer effects and a lower tendency towards socially desirable responses. Overall, the survey was recognised as a strategy of inquiry that from a single source of data could provide new insights into the complexity of health service provision and primary health care nursing practice. 6.4 Study Methods 6.4.1 6.4.1.1 Study population Eligibility The unit of inquiry in the NICPS was the integrated care project. Integrated care projects were classified as two or more New Zealand organisations57 that agreed to plan and/or implement integrated care in the interests of improving the health of identified individuals and populations. In the study integrated care “refers to the methods and type of organisation which will provide the most cost effective preventative and caring services to those with the greatest health needs and which will ensure continuity of care and coordination between different services” (Ovretveit, 1998, p. 1). The inclusion criteria for the NICPS referred to New Zealand projects 57 The majority of organisations were located within the health sector. 133 defined as integrated care. Projects whose characteristics ruled them out as integrated care were excluded. The eligibility criteria focused the survey on the provision of accurate information about integrated care projects and the practice of nurses within those projects. Eighty projects met the eligibility criteria and comprised the sample population. Of the 80 projects, the first 27 were identified from a list provided by the Ministry of Health. Nine demonstration pilot projects were included in this initial 27. Following up these newly identified projects resulted in a further 53 projects being identified, and included in the overall sample. The study recruited projects between December 1999 and February 2001. The Ministry of Health appeared to be the only entity that held a record, albeit a partial list, of the number of integrated care projects in existence. No complete list of projects could be found. Twenty-seven individuals, identified as holding a key role in either project planning or implementation, were surveyed to provide data on the characteristics of the 80 projects. Some individuals provided information on several projects. Individuals surveyed were recognised as having an overall and in-depth knowledge of projects. 6.4.1.2 Sampling The study employed a non-probability or purposeful sampling method. Non- probability samples, such as integrated care projects, can be selected based on judgements regarding the needs of the survey. Non-probability sampling has no set rule regarding sample size. The 80 projects that met the study criteria within the period the study had been granted ethical approval, were surveyed. Non-probability samples do not guarantee that all eligible projects have an equal chance of being included in the sample. However, the follow-up of projects in the NICPS was rigorous and painstaking, all eligible projects were included in the sample, and a 100 per cent response rate was achieved. 134 The technique snowball sampling involved individuals initially surveyed, identifying new projects. This technique was appropriate as only a limited number of projects were known, and expert informants with knowledge of specific projects became resources in the discovery of new projects. With the NICPS representing projects spread across New Zealand the sample became less vulnerable to selection bias. 6.4.1.3 Procedures for the recruitment of projects Telephone contact was made with individuals in organisations identified as having a lead role in projects for the purpose of verifying the project’s current status. This inquiry revealed that some integrated care projects were in the planning phase, others were being implemented, some existed in name only, and a number were not eligibility for inclusion into the NICPS. The lead organisation/s of projects categorised as eligible were asked to identify an individual who held a key role within the project. On several occasions two or more organisations in partnership on the project reached agreement about who would respond to the survey. More than one person was interviewed for some projects. This occurred in situations where key roles were held by more than one person, and individuals had only partial knowledge. For example, some interviewees held project roles that focused on clinical quality and best practice, whilst others held project management roles that focused on costs and outcomes, or information management and technology. Once identified, individuals were contacted by telephone and their cooperation was sought by emphasising the significance of the study and the importance of their contribution. Following the initial contact by telephone, a letter of introduction outlining the study, participant information sheet, and consent form were posted to individuals. A stamped addressed envelope was included for the return of the consent form. Ten consent forms were received in the following week. Two non-respondents were followed up with a phone call approximately two weeks after mailing. This group all returned consent forms in the following week. A record was kept of participant’s details. Upon receipt of the signed consent form, the interview questionnaire was posted to respondents indicating the questions that would be asked in the telephone 135 interview. Approximately one week after the posting of the questionnaire, a telephone call was made to establish a date and time for the interview, and to answer any questions the respondent had about this process. From the initial twelve telephone interviews, which obtained data on the first 27 projects, potential new projects were also identified. The recruitment of new projects remained consistent with the procedures adopted for the first cohort. 6.4.2 Ethical considerations Written consent to participate was sought from all respondents prior to any information being collected at interview. Approval by the Auckland Northern Region Ethics Committee was granted for the conduct of the study between December 1999 and February 2001. 6.4.3 Data collection Data were obtained on 80 integrated care projects from expert informants during a telephone survey using a structured interview questionnaire. Twenty-seven interviews were conducted, which lasted between 50-65 minutes, with the average interview taking about 60 minutes. Robson (1993) contends anything less than half an hour is unlikely to be valuable. All respondents answered every question (item) on the interview questionnaire (see Appendix 3). Data were collected on the respondent and specific project characteristics. The extent of the data collected is indicated in Table 9: Variables, research questions and items on the survey (see p. 138). 6.4.3.1 Interview questionnaire No existing survey instrument was found that could collect data to answer the four research questions. Instruments used to measure innovation and improvements in performance across organisations were investigated and found unsuitable for use in 136 this study (Kaplan & Norton, 1997). This was because the present study needed specific baseline data on the current environment and practice of nurses, which was unknown. The information required about the practice of nurses was also specialised, and could not be captured in non-occupational specific questions. Consequentially, a specific instrument was developed to guide the content and structure of the interview. Literature was extensively reviewed on public health, health reform, health promotion, chronic conditions, integrated care, and primary health care nursing (see chapters 2 to 5). The interview questionnaire developed as a result of frameworks and central issues identified in the literature, expert advice, and the knowledge of the researcher, who had a particular interest in integrated care. Experts were consulted about the overall questionnaire design, question form and question content. As a consequence, themes (question fields) and questions (items) were identified. The themes selected were central to characterising the projects, became starting points for generating specific questions, and are shown in Table 9 (see p. 138). 137 Table 9: Variables, research questions and items on the survey Variable Research question Item on survey Independent variable #1: organisational structure Research question #1: Which characteristics of integrated care are more strongly associated with projects that employ nurses? See questions 8, 9, 10, 11, 12, 20, 21, 22 & 23: planning new services, delivering existing services differently, health services provided, general practice incentives, hospital incentives, financial incentives to project, material incentives to clients, costs to general practice, costs to hospitals Research question #2: What types of population-based interventions were undertaken by nurses in integrated care projects? Research question #3: What population-based levels of practice did nurses demonstrate in integrated care projects? Independent variable #2: funding Research questions #1, #2, #3 See question 19: dedicated funding, main funding source Independent variable #3: type of service integration Research questions #1, #2, #3 See question 5: organisations in partnership Independent variable #4: strategies for integration Research questions #1, #2, #3 See questions 6, 7 & 18: purpose of project, measure of achievement, project strategies Independent variable #5: population-based level of approach Research questions #1, #2, #3 See question 17: level of project approach Independent variable #6: age group targeted Research questions #1, #2, #3 See questions 15: age groups Independent variable #7: ethnic group targeted Research questions #1, #2, #3 See questions 13: ethnic groups, ethnic group only, ethnic group and wider population Independent variable #8: low income group targeted Research questions #1, #2, #3 See questions 14: geographic area Independent variable #9: health, disease or condition targeted Research questions #1, #2, #3 See questions 16: disease, condition, or another focus Independent variable #10: Practice of nonnursing personnel Research questions #1, #2, #3 See question 24: practice of non-nursing personnel Dependent variable #1: Practice of nurses Research questions #1, #2, #3 See questions 25 and 26: practice interventions of nurses, levels of populationbased practice of nurses Research question #4: What underlying values are made explicit when interventions undertaken by nurses are analysed? 138 6.4.3.2 Question form and content In this survey, answers were of interest not intrinsically but because of their relationship to the practice of nurses in projects, which was being measured. Most questions were designed as measures and answers were valuable only when they could be shown to have a predictable relationship to the area of interest, the practice of nurses in projects. Each question attempted to maximise the relationship between the answer recorded and what the researcher was trying to measure. Individual questions were assessed on their ability to uncover situational knowledge. Some questions were discarded because they were too general and the range of interpretation too wide, led in a particular direction, or demonstrated a bias. Finally, from over 40 initial questions, 27 comprised the survey instrument and are presented in a conventional58 sequence. A number of questions are complex and break down into a set of simpler questions. According to Fink (1995) questions take one of two primary forms. When they require the respondent to use their own words they are called open. When they are pre-selected for the respondent, they are called closed. The present survey used eight open questions, 13 closed questions, and six that used a combination of both open and closed (see p. 141, Table 10). Several open questions appeared straightforward, like question two, “Who is your employer?” Powney and Watts (1987) argued that simplicity is deceptive and draw on the allegory of writing a book, in that most of us have basic literacy skills but few attain literary art. The open questions permitted the researcher to obtain answers from the respondent who answered questions using their own words. Open question three “What is your primary role in the project?” could have been asked alternatively using pre-selected answers. The list of possible answers, however, would likely have been longer than what was feasible to present to respondents. Despite this, closed questions with a limited number of response alternatives can provide reliably answers. Schuman and Presser (1981) suggested the researcher could interpret the meaning of answers more reliably if alternatives were given to the respondent. Fowler (2002, p. 58 A conventional sequence begins with non-threatening questions, moving through the body of the interview in a way that flows easily. 139 91) suggested the provision of a constrained number of answer options increased the likelihood that there would be enough people giving any particular answer to be analytically interesting. In the NICPS, closed questions provided respondents with response alternatives in one form, called categorical. Categorical alternatives have no numerical or preferential values. For example, question eight asks respondents to answer yes or no regarding whether the project plans to deliver a new health service. “Yes” and “no” are binary (dichotomous) categories from which a selection must be made. Question 17 asks respondents which level of approach has been adopted by the project and also calls for categorical choices. This question, however, presents four categories: individuals and families; communities; system, and a combination of any of these. Fowler (2002) argued that four categories was a comfortable maximum on a telephone, and suggested that for many telephone surveys two or three category responses should predominate. In addition to the number of categories, a second issue concerns how best to group the categorical responses so that they are meaningful. Question 15 asks which age group is targeted by the project and uses standard categories: 0-20, 21-55, over 55 and all ages. These categories assumed that projects targeted different age groups within the population and did not focus predominantly on one group. If for example, older adults had been the focus of the majority of projects categories could have been constructed differently, such as: 65-74, 75-84, 85-95 and over 95. Question 13 asks about ethnicity through a series of three closed questions, and as each answer is provided more comprehensive data becomes available. Combining closed questions and open questions allowed data to be collected on a single issue with increasing detail. For example, question 14 asks about geography and combines categorical data obtained from a closed question and descriptive data from a subsequent open question. The initial question seeks a categorical binary (yes/no) response, with the follow-on question answered only when ‘yes’ is indicated. Finally, the meanings of potentially ambiguous terms like condition, non-nursing personnel, or nurse, were defined at the beginning of specific survey questions. 140 Table 10: Question form of items on the survey Question form Items on survey Open Descriptive 1, 2, 3, 4, 5, 6, 7 & 27 Closed Categorical: 2 response choices 8, 10, 20, 22 & 23 Categorical: >2 response choices 17 & 26 Categorical: Question 1: 2 response choices Questions 2&3: 2 response choices 11, 12, 13, 15, 16 & 25 Categorical: Question 1: 2 response choices Question 2: Descriptive 9, 14, 18, 19, 21 & 24 Combination of open & open 6.4.3.3 Pilot-testing the instrument The pilot-test provided the opportunity to trial the instrument before it was made final. Six practising health professionals with a sound knowledge of integrated care were surveyed by telephone. Each had a copy of the survey questionnaire during the interview. The interviewer read each question and asked the respondents to say in their own words what they thought the question was asking. The interviewer sought to determine if questions were understood and whether the wording in each question was clear. Respondents were asked to explain how they chose a particular answer when categorical alternatives were given and whether enough information was provided to answer a question adequately. Answers were repeated back to respondents and they were asked if this accurately reflected what they had said. Answers were then assessed to see if they had provided valid measures of what the question had been designed to measure. Interviewees were also asked if they had felt respected by the interviewer and if they perceived the interviewer had listened to them and appeared friendly during the interview process. The time of the interview was monitored. The interviewer identified suitable probes to encourage an interviewee to answer a question, how to keep the interviewee on the topic, how to keep the interview to the agreed time limit, and an effective method for recording information. 141 The results of the pilot test were used to revise the survey instrument and logistics. After analysing data from the pilot test, seven previously open questions were replaced by closed questions or combination closed and open questions. The question form was altered to attain more predictable and reliable responses. Questions about project funding, incentives, and costs, were identified as potential areas of sensitivity, so were placed towards the end of the interview in an attempt to maintain the flow. Minor changes to questions 25 and 26 resulted in interventions frequently implemented in conjunction with one another, like health teaching, counselling, and consultation, being grouped together. Respondents did not require the definitions to be read as often, and appeared to answer more quickly after the categories were grouped. Finally, an option for respondents to comment at the end of the interview was included. Amending the final draft of the survey instrument was uncomplicated, and an approximate timeframe of 60 minutes for the interview was established. 6.4.3.4 Reliability and validity Reliability (repeatability) and validity (accuracy) described the quality of measurements resulting from the questionnaire-based survey. Questions were reliable when they provided consistent measures in comparable situations, and valid when the answers corresponded to what they were intended to measure (Fowler, 2002). The survey instrument used the same set of standardised questions for all interviews and one interviewer asked the questions and recorded the answers (see pp. 145-146). In order to provide a consistent data collection experience for all respondents the question-and-answer process was entirely scripted, with questions written in full. The questions were also reviewed by experts and pilot-tested to establish common meaning. Respondents had expert knowledge of the survey topic and in addition, closed questions provided answers that could be communicated consistently to all respondents. Of the 27 survey items, 19 included closed questions. Twelve items asked successive questions to gain greater detail and in doing so increased reliability. 142 Obtaining accurate information from the interview questions relied upon the use of conventional language, complete sentences and the avoidance of abbreviations, colloquialisms, and jargon. In early drafts of the questionnaire, biasing words and phases, two-edged questions, and negative questions were eliminated. The use of unclear terms, such as non-nursing personnel, was a more common error than the use of unfamiliar words. The prevalence of misunderstanding of common wording has been well documented (Belson, 1981; Fowler, 1992; Oksenberg, Cannell, & Kalton, 1991; Tanur, 1992). Internal consistency reliability is applied to groups of items that are thought to measure different aspects of the same variable. Internal consistency is an indicator of how well the different items measure the same variable. A limitation of the survey instrument was that internal consistency reliability had not been calculated, however, this form of reliability was addressed by a number of survey questions measuring aspects of the same variable. For example, health services were measured in questions eight, nine and ten. Several types of validity are typically measured when assessing the performance of a survey instrument: face, content, criterion, and construct (Litwin, 1995). Assessing face validity involved discussing with colleagues the survey instrument for question appropriateness. Content validity involved a more formal expert review of how good a question or set of questions were, resulting in significant changes being made. Pilot-testing also enabled respondents to offer additional perspectives. Criterion validity has two dimensions concurrent and predictive. Concurrent validity could not be measured because an established gold standard did not exist. Predictive validity, measuring how well a question predicts expected occurrences, was used to support research questions. Peers who were unfamiliar with the research questions reviewed a summary of data and drew conclusions. Because a number of individuals drew the same conclusions a level of assurance could be inferred. Construct validity is a theoretical measure of how meaningful the survey is. It is frequently seen as a gestalt of how well a survey instrument performs in different settings, with different populations, over a number of years. 143 Data collected in the study was mostly factual. Increasing the validity of reporting factual data depends on what is being asked and how it is asked. Reasons respondent’s report events with less than perfect accuracy include: they do not understand the question; they do not know the answer; they cannot recall information, although they know it, and they do not want to report the answer in the interviewer context (Fowler, 2002). In the present study, to ensure that questions were understood, definitions were provided to all respondents and category choices assisted respondents to choose answers. Every effort was made to maximise the validity of factual data by writing questions that would be consistently understood by respondents. No respondent commented they could not recall information at the time of the interview. This may have been because the information sought by the interviewer was familiar to the respondent and very recent. Lastly, all respondents appeared interested to participate in the survey, perhaps because they perceived the survey would generate information useful to them. Respondents were informed that they could withdraw from the study after reviewing the questionnaire content, and they were free to refrain from answering any question during the interview without providing an explanation. Despite these reassurances a 100 per cent response rate was obtained and all relevant questions were answered. In addressing issues that had the potential to impact on the quality of data collected, internal validity was established. The 80 integrated care projects investigated are likely to share certain essential characteristics (see sections 5.4.3 and 5.4.4) with other projects in New Zealand that developed during the same period. The findings of the NICPS can reasonably be generalised to other New Zealand integrated care projects and primary health care nursing practice at this time. Generalisability (external validity) is an important feature of this study design. 6.4.3.5 The role of the interviewer The survey employed one interviewer59 who had three major functions. The interviewer contacted respondents to enlist cooperation, motivated respondents to 59 The researcher conducted the survey interviews. 144 perform their role, and engaged in the interview process asking questions and recording answers in a standardised way. Gaining the cooperation of respondents was challenging. The style adopted for initially engaging people was personable and professional. The study was presented as if there was ‘no question’ that the respondent would want to cooperate. What was required from respondents was clearly articulated and any issues raised were immediately addressed. The interviewer attempted to standardise the interview by introducing a similar process to all respondents about the study and its purpose (see Table 11). This was so that the context of the interview would remain as constant as possible. Confidentiality issues were discussed and the various people and organisations that might use the study findings were identified. Table 11: Interviewer approaches to contacting respondent st Telephone call was made to introduce the study and gain cooperation nd One week later a letter outlining the study purpose, a participant information sheet, and consent form were posted out rd Two weeks following the 2 contact, a telephone call was made to nonrespondents to enlist cooperation/provide more information/address any issues th One week after receiving the signed consent form, the survey questionnaire was posted out th One week after posting out the survey questionnaire a telephone call was made to set an interview time. (Each interview collected data on one project. At the completion of the first interview, a second interview was scheduled for those providing data on >1 project) 1 contact 2 contact 3 contact 4 contact 5 contact nd Before the interview began, a standardised instruction (Fink, 1995) was used to explain the respondents’ tasks to them, and to explain the question-and-answer process. This instruction was given: Before we start, let me tell you a little about the interview process, since most people have not been in a survey like this before. You will be asked two kinds 145 of questions in this survey. In some cases, I will be asking you to answer questions in your own words. In those cases, I will have to write down every word you say, not summarising anything. For other questions, you will be given a set of answers, and you will be asked to choose the one that is closest to your own view. Even though none of the answers may fit your ideas exactly, choosing the response closest to your views will enable us to compare your answers more easily with those of other people. Another standardised instruction (Fink, 1995) given to respondents was used to ensure that they had a common understanding of their priorities. It is very important that you answer as accurately as you can. Take your time. Ask me to clarify if you have any question about what is wanted. Since interviewer behaviour can reduce interviewer effects on data and increase overall accuracy, the interviewer set the pace of the interview. Reading questions slowly, the interviewer indicated to respondents they could take time to give thoughtful, accurate answers. Survey questions were asked in the same way as they were written, with no variation or wording changes. Questions that required a response alternative were read through a second time. Probes were used to encourage the respondent to provide more information when a question had not been fully answered. Standard probes, such as “Anything else?”; “Tell me more”, and “How do you mean that?” were used in the interview. The interviewer was careful not to communicate any judgement on an answer a respondent gave, did not express personal views or opinions, and sought to minimise the personal side of the communication in an effort to standardise the relationship across respondents. The recording of answers was standardised. Answers to open questions were recorded in the respondent’s own words and for closed questions the respondent’s choice was recorded. The interviewer entered data directly onto a coded survey questionnaire. Whilst the interviewer had knowledge of integrated care, this was different from respondents’ specific knowledge about projects. The interviewer did not assume to know what the respondent was saying when the respondent had not 146 been clear, or to read anything more into what the respondent said. The interviewer recognised that the interviewer role could potentially contribute to error in survey data. Fowler (2002) maintained it is unusual for researchers to make any efforts beyond training and supervision to minimise interviewer effects. In the present study, the interviewer had field experience and had received training and supervision in interviewing. These authors argue that although training and supervision are important, so is a well-designed survey instrument. The more an interviewer has to probe, explain, or clarify, the more likely they are to influence answers. The better the survey instrument the more likely it is that the interviewer will conduct a robust, standardised interview. 6.4.4 Organising the data for analysis Survey answers were transformed into data files for computer analysis. This section describes the practices used for code development and management, data format and entry, and data checking procedures. There are two kinds of errors that can occur in going from an answer to an entry in a data file. Transcription errors can occur when an interviewer records an answer and errors can be made in regard to coding decision. Quality control related to the data entry and coding procedures chosen in this study. 6.4.4.1 Constructing a code and assigning to survey data Answers were translated into numeric codes by the researcher. Codes were unambiguous. In addition, codes were designed to minimise errors during coding and analysis. For example, the same code (0) was consistently used for ‘no’ responses. When response alternatives were provided to respondents, codes were assigned to the given set of answers. When respondents were asked to answer questions in their own words the range of answers could not be predicted ahead of time. For these questions, code development became an interactive process whereby the researcher identified 147 categories that emerged from the answers, and imposed an order on the answers obtained. The purpose was to create categories that grouped answers, which were analytically similar, and to distinguish between answers that were different. The researcher found that when categorisation was too fine, a large number of categories with few entries resulted, which made analysis more difficult. The researcher also found that large, broad categories risked masking differences that may have been important. The criterion was to place answers in analytically meaningful categories and assign one code to each answer. Constructing a code required documenting the differences across answers to each question from the researcher’s perspective. A draft code for classifying these answers was constructed, tested on another 15 interviews, and revised as necessary. A separate code for ‘other’ responses was assigned. Notes recorded on this category were used to expand and clarify the code, and in some instances to add needed categories. As well, a record of answers included in the ‘other’ category was obtained. These steps allowed the coder to identify and address any problems or ambiguities that presented. Table 12: Codes assigned to questions 1 to 3 Question Code 1 Name 1=Name 2 Employer 1=Primary sector 2=Secondary sector 3=Other 3 Role 1=Financial management 2=Clinical management 3=Systems management Questions one to three related to the respondent, with categories derived from the respondent’s answers. The researcher sought to determine if informants located in one health sector were more likely to undertake a specific role. 148 Table 13: Codes assigned to questions 4 to 9 Question Code 4 Project title 1=Project title 5 Type of integration 1=Vertical 0=No 1=General Practice+Hospital 2=Hospital+PHC Provider60 3=Other 2=Horizontal 0=No 1=General Practice+PHC Provider 2=Hospital+Hospital 3=General Practice/PHC Provider+other sector 4=General Practice+General Practice 3=Vertical + horizontal 0=No 1=General Practice+PHC Provider+Hospital 2=Multiple Providers 6 Project purpose 1=Project purpose 7 Achieve purpose 0=No 1=Yes 8 New planning 0=No 1=Yes 9 Different delivery 0=No 1=GP delivering specialist care 2=Other type of different delivery Questions four to 27 related to the project. Data collected on organisations in partnership measured the variable type of service integration. Shortell (1996) differentiates integration as either vertical or horizontal to describe the direction of organisational relationships. Vertical integration occurs between organisations in different sectors such as general practice (primary) and the hospital (secondary), and horizontal integration occurs between organisations within the same sector, such as general practice and other primary health care organisations. Question nine included a successive question that required coding three categories derived from respondent’s answers. 60 “PHC Provider” refers to primary health care organisations other than general practice. 149 Table 14: Codes assigned to question 10 Question 10 Code Health service 0=No 1=Combination of all services 2=Screening and prevention 3=Health promotion 4=Diagnostic tests and expert advice 5=Treatment and follow-up 6=Rehabilitation Question 10 classified the types of services projects provided. Projects that had planned services or developed clinical guidelines but not implemented them were classified 0 (No). Screening and prevention focused mostly on diseases, but also included wider areas such as poverty by assessing housing, exercise programmes to reduce the weight of obese groups, and community health checks for at risk populations. Health promotion referred to services provided to people not known to be at risk of a disease or condition and included asthma education, and the promotion of health care services more broadly. Diagnostic tests and expert advice included conducting echocardiograms and spirometry and advice by specialist nurses to colleagues, or clients, by way of a nurse telephone triage system. Treatment and follow-up referred to primary medical care post-discharge, community care pathways and primary care follow-up services. Rehabilitation related to smoking cessation programmes and improving physical function with input from physiotherapists. Table 15: Codes assigned to questions 11 and 12 Question Code 11 General practice incentive 0=No 1=Generate income 2=Plan new health services 3=Improve existing health services 4=Gain new skills 5=Reduce hospital service demand 6=Reduce hospital specialist time 12 Hospital incentive 0=No 1=Generate income 2=Plan new health services 3=Improve existing health services 4=Reduce hospitalisations 5=Reduce hospital specialist time Question 11 classified the main incentive perceived by respondents to influence general practice being a partner in a project. Generating income referred to activities 150 like enrolling new clients, and receiving payment to case manage or vaccinate clients. Planning a new health service referred to, for example, new respiratory and cardiac services that utilised clinical guidelines, and the establishment of equipment coordination for client use. Improving an existing health service referred to, for example, extending maternity services to provide additional care, case management within mental health, and the coordination of child health services to improve access to primary care. Gaining new skills referred to, for example, general practice accessing hospital specialist advice within 24 hours, case meetings, or co-working arrangements. Reducing hospital service demand referred to services being shifted to the primary sector from the secondary sector. Reducing hospital specialists’ time referred to general practitioners and nurses’ case managing more complex clients in the community, rather than admitting them to the secondary sector. Question 12 classifies the main incentive perceived by respondents to influence a hospital being a partner in a project. Generating income referred to integrated funding generated by project services. Planning a new health service frequently referred to the development of databases. Improving existing health services referred to for example, the integration of information systems between providers, expanding services to provide more comprehensive primary health care, extending maternity services to offer additional care, case management within mental health services and enforcing the use of guidelines and protocols. Reduce hospitalisations referred most often to the management of clients with chronic conditions in the primary sector, new or improved screening and prevention services, and the implementation of clinical guidelines. Reduce hospital specialist time referred to advising and educating colleagues in the primary sector about the management of chronic conditions. 151 Table 16: Codes assigned to questions 13 to 15 Question Code 13 Ethnic group 0=No 1=Maori only 2=Maori and wider population 3=Pacific only 4=Pacific and Maori only 5=Pacific and Maori and wider population 6=Other 14 Low income 0=No 1=low decile area 15 Age group 1=0-20 2=21-55 3=over 55 4=all ages 16 Disease or condition 0=No 1=Diabetes 2=Chronic obstructive pulmonary disease 3=Acute confusion 4=Two or more chronic conditions 5=Mental health condition 6=Cardiac conditions 7=Sexual and reproductive health 8=Two or more acute conditions 9=Hip fracture 10=Asthma and other respiratory conditions 11=Cerebrovascular disease (stroke) 12=Dental health 13=Meningitis 14=Hepatitis 15=Obstetric health 16=Iron deficiency anaemia 17=Urinary tract infection Health, disease or condition, or other focus 0=Other 1=Chronic disease or condition 2=Acute disease or condition 3=Well-health Ethnic group Maori health was identified as an area for health gain to be addressed by integrated care (Health Funding Authority, 1998). Consequently, the researcher sought to determine the proportion of projects that had an exclusive Maori focus, and a focus on Maori and the wider population. This idea was further developed to explore the relationship between integrated care and Pacific people, who have also been identified as an underserved population (Ministry of Health, 2001c). The highest numbers of Maori and Pacific people in New Zealand can be found in specific geographic regions, so a classification that combined both ethnic groups was created. 152 Low income Geography was used to determine low income. The New Zealand deprivation index uses data from the Census to rank areas across the country according to relative deprivation. Deprivation is measured using nine variables: access to a telephone, income, employment, household income, access to a car, family unit support, educational qualifications, home ownership and household occupancy levels. Each geographical meshblock within New Zealand is assigned a deprivation score based on the nine variables. The meshblock scores are then divided into tenths with meshblocks of the highest values representing the 10 per cent of most deprived meshblocks in the country, and those in the lowest deprivation group representing the 10 per cent of least deprived areas. For the purposes of this study, the most deprived 30 per cent of meshblocks were coded as low decile, representing the 30 per cent most deprived areas in New Zealand. The atlas “Degrees of Deprivation in New Zealand: An atlas of socio-economic difference” (Crampton, Salmond, & Kirkpatrick, 2004) was used as a tool to identify the deprivation figure for the client catchment area of health services identified within this study. In instances where the catchment area covered more than one meshblock the average deprivation rating was taken from all relevant meshblocks. Age group The codes were assigned to answers within the four closed-response categories: children (including babies) and adolescence (0-20), adults (21-55), older adults (55+), and all ages (0-55+). Literature on integrated care suggested the strategy would target all ages (Health Funding Authority, 1998). For the purposes of this study, older adults are classified as those 55 years and over, although 65 years is internationally recognised as the point from which people are known as older adults. It is also the age at which entitlement to retirement income in New Zealand was guaranteed in 2001 (Ministry of Health, 1997). However, the term ‘kaumatua’ refers to all Maori aged 55 years and over. Kaumatua more traditionally refers to the status and role that kuia (older people) and koroua/koro (older men) attain as recognition of their contribution, leadership, knowledge and protection of whanau/hapu/iwi life (Barlow, 1991). This age range allows the flexibility to acknowledge that many Maori face 153 age-related disability and illnesses at a relatively younger age and have a shorter life expectancy than non-Maori. From a Pacific people’s perspective status customarily accorded to older Pacific peoples is not necessarily confined to chronological considerations but can also be ascribed as a consequence of increased social status. Many Pacific peoples face illness or limitation to physical participation and mobility, typically associated with older people, at a younger age than the general population (Ministry of Health, 1997). Statistical data impose an age range on population groups, which makes it necessary to adopt an age span to enable a meaningful comparison of quantitative statistical analyses. Therefore, the study adopted the definition of the kaumatua age range. Disease or condition The researcher sought to determine the disease or condition focus of projects and attributed codes accordingly. No specific condition was then reclassified. Some projects, for example, classified as sexual and reproductive health focused on wellhealth in pregnancy or women’s health. The dental health classification also related to well-health. Other classifications such as urinary tract infection were reclassified as either acute or chronic dependent upon project data. Table 17: Codes assigned to question 17 Question 17 Code Level of project approach 1=Individual/family 2=Community 3=System 4=Individual/family and Community 5=Individual/family and System 6=Community/System 7=Individual/family and Community and System Question 17 attempted to discover the overall level of the population-based approach (see pp. 90-93) adopted by the project. For example, did the project attempt to change the knowledge, attitudes, beliefs, and practices of individuals (and families) or communities; or neither individuals or communities, but rather the systems that impact health? 154 Table 18: Codes assigned to question 18 Question 18 Code Strategies for integration 1=Clinical guideline development 0=No 1=Nurses 2=Others 2=Clinical guideline promotion 0=No 1=Case management 2=Audit 3=Information to clients 4=Information to peers 3=Case management 0=No 1=Nurse 2=General practice team 3=Clinical team 4=Other 4=Database development 0=No 1=Yes 5=Information sharing 0=No 1=Peer advice/education 2=Peer referral 3=Client education 4=Relationship building 6=New coordination strategy 0=No 1=Yes Decision making guidelines, effective information systems and coordination activities such as case management, has been promoted as strategies to be tested (Health Funding Authority, 1998). These strategies formed the basis of question 18, which required a binary response to specific strategies before successive questions sought to uncover more detail. So, for example, after establishing guidelines were developed, a following question asked who had developed them. The classification of data is explicit and codes are generally predictable. The strategy case management uses the code general practice team, which includes nurses, and others employed in general practice, and the code clinical team refers to primary and secondary clinicians. Code other, refers to administrators or information managers who case managed the client’s care by coordinating different clinicians for direct service provision. Information sharing used the code peer advice and/or education, for example, when hospital specialists advised/educated general practice personnel, or when nurses with a specialty area of practice like diabetes advised/educated practice nurses. Peer referral most often referred to situations where hospital services were shifted to general practitioners, such as conducting an echocardiogram, a task usually undertaken by the cardiologist. Client education referred to education as a formal activity, rather than an educational opportunity that happened in the course of a health professional/client 155 interaction. Relationship building centred on both client and health provider relationships and focused on improving access and quality of services. New coordination strategy referred to different means of coordinating and providing health interventions (mouth guards and vaccines) and services (community health checks, dental care, and maternity care). Table 19: Codes assigned to questions 19 to 23 Question Code 19 Project funding 0=No 1=Project partners 2=Government 20 Project financial incentive 0=No 1=Yes 21 Client material incentive 22 Costs to general practice 0=No 1=Yes 23 Costs to hospital 0=No 1=Yes 0=No 1=Yes Question 19 asked initially if the project received new funding and who provided the main funding. Financial incentive for organisations that are project partners included general practice receiving additional payment for consultations with clients (additional to fee-for-service client charges and the general medical subsidy from government). Material incentive for clients included improvements to a home (see p. 164). Financial costs incurred by hospitals included transferring resources to general practice for the provision of new primary health care services. Question 24 asked if non-nursing personnel were employed in projects, and sought a description of the practice. The codes indicate the six main areas identified. Information management referred to the development of a database and the establishment of systems to share information. Administration and coordination referred to the organisation of personnel, services, clients, and data. Research and audit referred to investigations into best practices, risk factors, immunisation rates, and clinical case management. Consulting referred to advice and information provided to colleagues in the areas of clinical management and project management, 156 including evaluation. Clinical guideline development referred to all activities pertaining to the production of a guideline for a specific purpose and population. Technical support referred to equipment management and maintenance. Table 20: Codes assigned to question 24 Question 24 Code Non-nursing personnel 0=No 1=Information management 2=Administration/coordination 3=Research and audit 4=Consulting 5=Clinical guideline development 6=Technical support Question 25 asked if the project employed nurses and then sought to determine which of the 17 interventions were undertaken by nurses. Question 26 determined the level/s of population-based practice undertaken for each intervention previously identified in question 25. Table 21: Codes assigned to question 25 and 26 Question Code 25 Intervention 26 Level of practice 0=No nurses 1=Surveillance (interventions: continuous to 17) 0=No intervention 1=Individual/family 2=Community 3=Systems 4=Individual/family+Community 5=Individual/family+Systems 6=Community/Systems 7= Individual/family+Community+Systems (0-7 scale measuring level of practice was applied to each intervention) 6.4.4.2 Data entry Data were double entered into a Microsoft Excel spreadsheet and then converted to SPSS. The study code for each interview was entered into the data for a particular record61. The study code preserved the order of the data and was critical in checking 61 Record pertains to data collected at each interview about a specific project. 157 files for completeness. Data were coded in the order that questions appeared on the survey instrument, in an attempt to reduce errors. This process represented an effective and relatively cost-free means of controlling quality. Multiple codes were entered in a single column. Editing of the data was facilitated by the incorporation of range and logic checks. Cross checking of the data was undertaken so that errors in data entry could be rectified. 6.4.4.3 Coding and data reduction as a source of errors Because coding and data reduction processes were checked thoroughly, there was potential for this part of the survey process to be relatively free from errors. When dealing with closed answers the rate of data entry should be less than one per cent (Fowler, 2002). The quality of coding open questions is reported to vary with the quality of the question, the quality of the code, and the experience of the coder. In the present study, the open questions were focused and the coding categories were conceptually clear. Fowler (2002) suggests in these circumstances coding should exceed 90 per cent in reliability. Codes that depend on knowing complete definitions, such as employment categories or health conditions, require particular attention. The researcher, familiar with such definitions, maintained a level of accuracy in both the coding and data entry process. 6.4.5 Data analysis Data obtained from interviews lend themselves to extensive, descriptive statistical analyses. The data analysis was conducted to reduce, organise and give meaning to the data. The investigation aimed to establish if a relationship existed between the characteristics of integrated care projects and the practice of nurses in projects. Research questions sought to determine: the characteristics of integrated care more strongly associated with projects that employ nurses; the interventions and levels of practice undertaken by nurses, and finally the health promotion values embedded in 158 nurses’ practice overall. To achieve this two stages of interpretation were necessary, and are presented as stage one and stage two analyses. 6.4.5.1 Stage one analysis Simple frequency tables (see Appendix 4) were initially produced to describe the characteristics of integrated care projects and the practice of nurses. Frequencies take the form of numbers and percentages. Data included: the respondent’s personal details; organisational structure; funding; type of service integration; strategies for integration; level of project approach; age group targeted; ethnic group targeted; low income targeted; health, disease or condition targeted; practice of non-nursing personnel, and the practice of nurses. This primary analysis was undertaken on all variables, but it was anticipated that this would not fully address the research questions. Following several consultations with statisticians Alastair Stewart and Elizabeth Robinson it was decided that for the purpose of this research, cross tabulating primary analysis data was required. Variable ‘projects employing nurses’ was cross tabulated by: planning a new health service and delivering an existing health service differently; type of service integration; strategies of integration; health service provided; level of project approach; age group targeted; ethnic group targeted; low income targeted; disease or condition targeted, and the practice of non-nursing personnel (see section 7.3). Additional cross tabulations included: disease, condition or other focus by: health service; level of project approach; age group, and ethnic group (see pp. 183-187), and age group with or without disease or condition by: ethnic group and low income (see pp. 187-189). Nursing interventions (n=17) were cross tabulated by ethnic group (Maori); low income (low decile area); health or disease/condition (chronic condition and well- 159 health); individual level of population-based practice; community level of populationbased practice, and by system level of population-based practice (see pp. 189-191). 6.4.5.2 Stage two analysis Social values embedded within the practice of nurses were determined using Beattie’s model of health promotion (see p. 31, Figure 1). Seventeen interventions and the level of population-based practice approach most often undertaken by nurses relating to that intervention are situated within Beattie’s model of health promotion, which has been adapted for this purpose. The three levels, individual and family (individual), community and systems, were reduced to individual and community to align with Beattie’s model of health promotion (see p. 194, Figure 18). Individual and systems levels were combined. This was possible because whilst systems interventions within projects always related to data management, which has a system focus, subsequent health impacts affected individuals. For instance, a diabetes register collected regional data that was used for case managing individuals. The researcher’s project knowledge also informed classification processes. Beattie’s model refers to a collective focus of intervention, described as either participative and community-based or paternalistic and state-directed (Beattie, 1991). Community level interventions by definition are directed towards entire populations or groups within populations (Minnesota Department of Health, 2001), so are considered community-based. Interventions at the community level attempt to change community norms, attitudes, and practices, the means of which can be described as paternalistic or state-directed. For the purposes of interpretation, ‘collective focus of intervention’ translates to ‘community focus of intervention’. Interventions are situated on the x-axis between individual focus of intervention and community focus of intervention. The specific location of each intervention is determined by a simple formula measuring the degree of individual or community focus: 160 Community – Individual (individual + systems) = Position Measures of variables community, individual and systems, for each intervention were taken from the total number of projects identified (see p. 192, Figure 17). The formula was applied to provide a consistent, quantifiable total inclusive of all levels of practice approach for each intervention. The formula provided a rationale for situating interventions numerically along the x-axis. The intervention is directed along the y-axis, lying within the quadrant most representative of the approach underpinning the intervention. In order to make Figure 18 (see p. 194) more easily understood, the model was rotated 90° anti-clockwise from the original position (see p. 31, Figure 1, Beattie’s model of health promotion). 161 7 7.1 Chapter 7 Results: Nurses in integrated care projects study Introduction Chapter seven provides an overview of the study results in two distinct sections. Stage one presents descriptive statistics of the 80 integrated care projects and the practice of nurses in these projects. Univariate analyses are presented initially, and then selected variables are cross tabulated because of their potential to address the research questions. Stage two presents the health promotion values seen to be driving the overall practice of nurses in integrated care projects. Seventeen interventions and the levels of population-based practice most commonly adopted by nurses employed in these projects are situated within an adaptation of Beattie’s model of health promotion. A summary of the results is presented in Table 33 (see pp. 195-198). 7.2 7.2.1 Study results Survey respondents Twenty-seven respondents were surveyed. A 60 minute telephone interview was used to collect data on a single project. Overall, data were collected on 80 integrated care projects (see section 6.4.1, p. 133). In summary: Number of survey respondents Number of projects 12 15 27 27 53 80 (Initial MOH list) (Snowballing) Of the 27 respondents, eight were interviewed on one project, six were interviewed on two projects, and 13 were interviewed on three or more projects. Nine respondents were registered nurses. Six respondents, who were not nurses, consulted nurses in projects about their practice in order to answer interview questions 25 and 26. Fourteen respondents were female and 16 were employed in hospitals. Twenty-one respondents (78%) reported their main role as clinical management. Of these, nine had trained in medicine, nine in nursing, and three in the allied health professions. Four respondents (15%) reported their main role as financial management, whilst the remaining two respondents (7%) reported their main role as systems management. 162 7.2.2 Integrated care projects A profile of the 80 projects that comprise the NICPS is outlined below. The information is presented in the same sequence as the integrated care characteristics in Table 9 (see p. 138), with data from survey questions relating to specific characteristics reported in the same section. Bar graphs and frequency tables illustrate the data and provide greater detail. 7.2.3 Organisational structure Planning a new health service or delivering an existing service differently Sixty per cent (48/80) of projects planned to deliver new health services. In addition, 63 per cent of projects also delivered existing health services differently. Of the projects delivering existing health services differently, 60 per cent involved general practice physicians providing services that had previously been provided by hospital specialists, such as taking an echocardiogram. Health care services provided by the project Almost 70 per cent (n=55) of projects provided health care services. Services included screening and prevention (13%), diagnostic tests and expert advice (10%), rehabilitation (6%), treatment and follow up (6%), health promotion (4%), and a combination of these services (30%). Approximately 30 per cent of the projects did not provide direct health care, but planned information systems such as databases for disease management, and developed guidelines. Incentives for general practice to be a project partner Ninety per cent (n=72) of projects had general practice partners. Of these projects 84 per cent reported incentives for general practice to participate. Incentives included 163 improving existing health services (41%), generating income (19%), receiving training (13%), planning and/or delivering new health services (10%), and reducing demand for hospital services (1%). Incentives for the hospital to be a project partner Eighty-seven per cent (n=67) of projects had hospital partners. Of these projects 93 per cent reported incentives for hospitals to participate. Incentives included reducing hospital admissions (63%), improving existing health services (21%), reducing hospital specialist time (5%), planning and/or delivering new health services (3%), and generating income (1%). Financial incentives to project partners Forty per cent (n=32) of projects had partners who received financial incentives when they provided health services (see p. 165, Figure 8). Material incentives to clients Five per cent of projects had clients who received material incentives as a consequence of their participation. Material incentives included: gifts, vouchers for general practice consultations, housing brokered by the health organisation, and building repairs to homes that included installation of amenities, such as ‘inside toilets’ (see p. 165, Figure 8). New cost incurred by general practices General practices did not incur new costs as a result of participating in projects (see p. 165, Figure 8). 164 New cost incurred by hospitals Hospitals incurred new costs (11%) as a result of participating in projects (see p. 165, Figure 8). Figure 8: Incentives to clients and project partners and new costs to hospitals and general practices 7.2.4 Funding Eighty-four per cent (67/80) of projects had a main source of new funding. These projects received funding from either government (68%; n=54) or project partners jointly (16%; n=13). Sixteen per cent (n=13) of projects did not have a main source of new funding. These projects were reported as either an alteration to an existing service, which used the same resources, or a new service where project partners reallocated existing funding from within their organisations. 7.2.5 Type of service integration Projects were vertically integrated (40%; n=32), horizontally integrated (19%; n=15) or both vertically and horizontally integrated (41%; n=33). 165 The most common organisational relationship of projects vertically integrated was between general practice and the hospital (36%), with hospital and other primary health care providers (4%) also vertically integrated. Horizontal integration comprised relationships between general practice and primary health care in sectors other than health (6%), hospital and hospital (6%), general practice and general practice (4%), and general practice and primary health care in the health sector (3%). Of the projects that were both vertically and horizontally integrated organisational relationships occurred between multiple providers across health and other sectors, such as housing (23%), and general practice, primary health care and the hospital (18%) (see p. 166, Figure 9). Figure 9: Organisational relationships based on vertical and/or horizontal integration 7.2.6 Strategies for integration Six strategies for integration were identified (see p. 167, Figure 10) with the most common strategy reported to be information sharing (65%). Information sharing, included building relationships (31%), peer advice and education (16%), peer referral 166 (10%) and client education (8%). The development of a database to improve access to information also occurred in 50 per cent of projects. Developing a new coordination strategy occurred in 56 per cent of projects. This strategy included coordinating health prevention and promotion activities with community groups such as sports teams, and adopting new approaches. Clinical guidelines were promoted in 36 per cent of projects and use by case managers was found to be a central reason for promotion (26%). Other reasons for the promotion of clinical guidelines included information to peers (8%), use as an audit tool (1%), and information to clients (1%). Clinical guideline development occurred in 21 per cent of projects, with nurses the largest professional group involved in this activity (10%). Case management occurred in 33 per cent of projects, with nurses (20%), multidisciplinary teams (8%), and general practice physicians and practice nurses (5%) undertaking case management. Figure 10: Strategies for integration 7.2.7 Project level of population-based practice Twenty-three per cent of projects adopted an individual and family-focused level of practice, with another 11 per cent adopting both individual and community level 167 practice. Sixty-six per cent adopted a systems level practice, either exclusively (32%), or in conjunction with another level of practice, such as, individual (29%), or individual and community (4%) or community (1%). Overall, projects did not adopt a community level of practice exclusively (see p. 168, Figure 11). Figure 11: Project level of population-based practice 7.2.8 Age group Twenty-eight per cent (n=22) of projects targeted people of all ages. Of the projects that targeted specific age groups adults (21-55 years) were targeted in 29 per cent (n=23) of projects, older people (>55 years) in 28 per cent (n=22), and children and adolescents (0-20 years) in 16 per cent (n=13). 7.2.9 Ethnic group Over half (53%; n=42) of the projects targeted Maori and/or Pacific peoples. Projects targeting Maori included Maori exclusively (16%), Maori and the wider population (10%), Maori and Pacific people exclusively (1%), and Maori and Pacific people and the wider population (20%). Five per cent of projects targeted Pacific people exclusively. 168 7.2.10 Low income Thirty per cent (n=24) of projects targeted populations in geographic areas defined as low decile and representing the 30 per cent of most deprived areas in New Zealand. 7.2.11 Disease, condition, or other focus Eighty-two per cent (n=66) of the projects targeted diseases or conditions and were classified in relation to direct clinical intervention. Projects classified as ‘other’ (18%; n=14) included projects with a focus on well-health and the development of information systems (see p. 154). Some of these projects had a disease or condition focus, but the classification other sought to differentiate from chronic or acute condition relating to direct clinical intervention. Figure 12: Projects by specific disease or condition 169 Figure 13 (see p. 171) shows the percentage of projects that targeted chronic conditions, acute conditions, well-health, or were classified as other. Fifty per cent (n=40) of projects targeted chronic conditions. Chronic conditions included diabetes (11%), two or more chronic conditions (8%), mental health conditions (8%), cardiac conditions (6%), chronic obstructive pulmonary disease (6%), cerebrovascular disease (stroke) (5%), asthma and respiratory conditions (5%), and urinary tract infections (1%). Ten percent (n=8) of projects targeted acute conditions, which included hip fracture (3%), acute confusion (1%), acute conditions (1%), iron deficiency anaemia (1%), obstetric health (1%), and dental health (1%). Nineteen per cent (n=15) of projects targeted the well-health of either a population-ofinterest, such as pregnant women, or a population-at-risk, such as adolescents with limited access to contraception, or adults with chronic obstructive pulmonary disease at risk of exacerbations. Projects targeted sexual and reproductive health (6%), chronic obstructive pulmonary disease prevention (3%), outreach (3%), health assessments (3%), meningitis prevention (1%), health screening (1%), exercise (1%), and housing (1%). Projects targeting well-health included maintaining the health of a ‘well–ill’ population, such as those with chronic obstructive pulmonary disease, and also maintaining the health of a population without any specific illness, at risk of poorer health as a consequence of, for example, low income. Twenty-one per cent (n=17) of projects did not target the direct clinical intervention of a specific disease or condition, or have a well-health focus. Instead, these projects developed databases (7%), partnerships (6%), guidelines, care maps, protocols, frameworks for service delivery, and funding arrangements (6%), triaged services (1%) and coordinated equipment (1%). A disease or condition focus was apparent in some of these projects; for example, a care map was developed for hip fracture. 170 Figure 13: Chronic or acute condition, well-health or other 7.2.12 Non-nursing personnel Thirty-seven per cent (n=30) of the projects employed non-nursing personnel. Project coordination and administration was the most common main role (29%). Other main roles included research and audit (5%), consulting (1%), technical support (1%), and information (1%). 7.2.13 Nursing Interventions Over 80 per cent (n=65) of the projects employed nurses. Of these projects, a combined total of 411 interventions were undertaken by nurses from a range of 17 different types of interventions (see p. 95). In approximately 50 per cent (n=32) of the projects only one type of intervention was undertaken suggesting a very restricted range of practice. In 43 per cent (n=28) of projects nurses undertook nine or more interventions, and in 26 per cent (n=17) of projects nurses undertook 13 or more interventions, suggesting a more extensive range of practice. The types of intervention undertaken included case management (9%; n=36); consulting (9%; n=36); health teaching (7%; n=31); collaboration (7%; n=31); referral 171 and follow-up (7%; n=30); delegated functions (7%; n=29); counselling (7%; n=29); advocacy (7%; n=29); coalition building (7%; n=28); screening (6%; n=26); policy development and enforcement (6%; n=24); outreach (5%; n=23); disease and health event investigation (5%; n=19); community organising (4%; n=15); social marketing (3%; n=13), and surveillance (3%; n=12) (see Figure 14). The seventeenth intervention, case finding (10%; n=42), combines surveillance, screening, disease and other health event investigation, and outreach, at the individual level of practice. No distinction was made between the levels of population-based practice of the other sixteen interventions. Figure 14: Total interventions undertaken by nurses in projects Almost 50 per cent of the total interventions undertaken by nurses comprise two wedges or groups of interventions (see Figure 14). The first wedge of related interventions comprises health teaching, counselling, and consulting (23%, n=96), 172 with referral and follow up, case management, and delegated functions, comprising the second wedge (23%; n=95). Interventions by level of population-based practice Of the total number of interventions (n=411) undertaken by nurses, a level of population-based practice that was exclusive occurred at the individual level in 66 per cent (n=270) of the interventions; community level in nine per cent (n=35), and systems level in eight per cent (n=33). Figure 15: Total interventions and levels of population-based practice undertaken by nurses in projects 173 Eighteen per cent (n=73) of the total number of interventions by nurses were undertaken on either two or three levels of practice. Most (13%; n=55) of these interventions occurred at both the individual and community levels. A small number of interventions occurred at the systems and individual levels (1%; n=3); systems and community levels (2%; n=8); or the systems, individual, and community levels (2%; n=7). Figure 15 (see p. 173) shows the percentage of total interventions undertaken by nurses and the levels of the practice of each intervention. Related interventions are grouped in wedges (see Figure 16 and p. 176, Table 22). An individual level of practice occurred most in referral and follow-up, case management, and delegated functions (21%; n=87), and health teaching, counselling and consultation (19%; n=80). A community level of practice occurred most (8%; n=32) in the wedge of interventions that included collaboration, coalition building, and community organising. A systems level of practice occurred most (4%; n=18) in the wedge of interventions that included surveillance, disease and health event investigation, outreach and screening. Figure 16: Total interventions and levels of population-based practice by wedge undertaken by nurses in projects Both individual and community levels of practice occurred in all wedges. These approaches were more prominent in advocacy, social marketing and policy 174 development and enforcement (5%; n=19) and surveillance, disease and health event investigation, outreach and screening (4%; n=16) wedges. Figure 16 (see p. 174) shows the wedges that applied more than one level of practice such as, community and systems levels, and individual, community and systems levels. 175 Table 22: Total interventions and levels of population-based practice by wedge undertaken by nurses in projects Individual Community Systems Individual & Community Individual & Systems Community & Systems Individual & Community & Systems Totals n % n % n % n % n % n % n % n % Surveillance, Disease & health event investigating, Outreach, Screening 42 10 2 0 18 4 16 4 0 0 0 0 2 0 80 19 Referral & follow-up, Case management, Delegated functions 87 21 0 0 6 1 1 0 1 0 0 0 0 0 95 23 Health teaching, Counselling, Consultation 80 19 0 0 5 1 8 2 2 0 0 0 1 0 96 23 Collaboration, Coalition building, Community organising 18 4 32 8 4 1 11 3 0 0 8 2 1 0 74 18 Advocacy, Social marketing, Policy development and enforcement 43 10 1 0 0 0 19 5 0 0 0 0 3 1 66 16 TOTALS 270 66 35 9 33 8 55 13 3 1 8 2 7 2 411 100 176 7.3 7.3.1 Projects employing nurses Planning a new health service and delivering an existing health service differently by projects employing nurses Sixty per cent (48/80) of projects reported general practice physicians provided care previously delivered by hospital specialists (classified as delivering an existing service differently), and of these projects 41 (85%) employed nurses. In addition, 30 projects reporting general practice physicians provided care previously delivered by hospital specialists planned a new service and nurses were employed in 29 (97%) of these projects. Health care services by projects employing nurses Of the projects employing nurses (n=65), health care services provided included: screening (12%; n=8); diagnostic testing and expert advice (9%; n=6); health promotion (5%; n=3); treatment and follow-up (5%; n=3); rehabilitation (1%; n=1), and a combination of these services (34%; n=22). Thirty-four per cent (n=22) of these projects did not provide services. Of the projects that did not employ nurses (n=15) all services were undertaken, with the exception of health promotion. Rehabilitation was provided in 27 per cent (n=4) of these projects and 24 per cent (n=3) did not provide services. Incentives and costs by projects employing nurses Eighty-four per cent (n=67) of general practices had incentives to participate and nurses were employed in 78% (n=52) of these. General practice did not incur financial costs as a result of participating in projects. Ninety-three per cent (n=74) of hospitals had incentives to participate in projects and nurses were employed in all projects (80%; n=59). Eleven per cent (n=9) of hospitals 177 incurred financial costs as a result of participating in projects and nurses were employed in 67% (n=6) of these projects. Forty per cent (n=32) of projects had partners who received financial incentives when they provided health services and nurses were employed in 75% (n=24) of these projects. 7.3.2 Funding by projects employing nurses Sixty eight per cent (n=54) of projects received their main source of new funding from government and nurses were employed in 82% (n=44) of these projects. 7.3.3 Type of service integration by projects employing nurses Forty-one per cent (n=33) of projects were both vertically and horizontally integrated and 28 of these projects employed nurses. A further 40 per cent (n=32) of projects were vertically integrated, with 22 of these employing nurses. Vertical integration occurred most often between general practice and the hospital. The remaining 19 per cent (n=15) of projects were horizontally integrated and all of these employed nurses. Horizontal integration occurred most in the primary sector between general practices and other primary health care providers. 7.3.4 Strategies of integration by projects employing nurses Information sharing via other methods Of the projects employing nurses (n=65), information sharing occurred in 71 per cent (n=46) through relationship building (n=25), providing peer education and advice (n=11), peer referral (4), and client education (n=6). Of the projects that did not employ nurses (n=15), information sharing occurred in 40 per cent (n=6) through peer referral (n=4) and peer education and advice (n=2). 178 Information sharing via database Of the projects employing nurses (n=65), information sharing via a database was undertaken in 52 per cent (n=34). Of the projects that did not employ nurses (n=15), information sharing via a database was undertaken in 40 per cent (n=6). New coordination strategy Of the projects employing nurses (n=65), a new coordination strategy was undertaken in 58 per cent (n=38). Of the projects that did not employ nurses (n=15), a new coordination strategy was undertaken in 47 per cent (n=7). Clinical guideline promotion Of the projects employing nurses (n=65), clinical guidelines were promoted in 42 per cent (n=27), for the purposes of case management (32%; n=21), information to peers (6%; n=4), information to clients (1%; n=1), and auditing clinical practice (1%; n=1). Of the projects that did not employ nurses (n=15), guidelines were promoted in 13 per cent (n=2) of projects to provide information to peers. Clinical guideline development Of the projects employing nurses (n=65), clinical guidelines were developed in 25 per cent (n=16) and half of the developers were nurses. Of the projects that did not employ nurses (n=15), only one developed clinical guidelines. Case management Of the projects employing nurses (n=65), case management was undertaken in 38 per cent (n=25) by nurses (25%; n=16), primary and secondary sector teams (9%; n=6) 179 and general practice teams (4%; n=3). Of the projects that did not employ nurses (n=15), case management was undertaken once by a general practice team. 7.3.5 Project level of population-based practice by projects employing nurses Projects employing nurses (n=65) adopted overall, a level of practice that focused on the individual (72%; n=47), either exclusively, or in combination with other levels, such as community and/or systems. Exclusive community level practice was not adopted by any project, although 20 per cent (n=13) adopted a community level in combination with other levels. Sixty-eight per cent (n=44) of these projects adopted a systems level of practice, with 26% (n=17) exclusively systems. Exclusively individual or systems levels were adopted only in projects that did not employ nurses (see Table 23). Table 23: Project level of population-based practice by projects employing nurses Project level of practice No nurses n (%) Nurses n (%) Total n (%) Individual 6 (40.0) 12 (18.5) 18 (22.5) Systems 9 (60.0) 17 (26.2) 26 (32.5) Individual & Community 0 (0) 9 (13.8) 9 Individual & Systems 0 (0) 23 (35.4) 23 (28.8) Community & Systems Individual & Community & Systems 0 (0) 1 (1.5) 1 (1.3) 0 (0) 3 (4.6) 3 (3.8) Total 15 (100.0) 7.3.6 65 (100.0) (11.3) 80 (100.0) Age group by projects employing nurses Of the 65 projects employing nurses, 28 per cent (n=18) targeted people of all ages. Specific age groups, such as, adults (21-55 years) were targeted in 32 per cent (n=21) 180 of projects, older adults (>55 years) in 22 per cent (n=14), and children and adolescents (0-20 years) in 18 per cent (n=12). 7.3.7 Ethnicity by projects employing nurses Almost 60 per cent (n=38) of the projects employing nurses focused on Maori and/or Pacific peoples. Of these projects, 52 per cent (n=34) included Maori, and 20 per cent (n=13) were exclusively Maori. Twenty-six per cent (n=17) of the projects included Pacific peoples and six per cent (n=4) were exclusively Pacific. More than 40 per cent (n=27) of the projects employing nurses did not have an ethnic focus. In comparison 73 per cent (n=11) of the projects that did not employ nurses did not have an ethnic focus. 7.3.8 Low income by projects employing nurses Seventy per cent of projects (n=56) did not have a low income focus. Nurses were employed in 44 of these projects. Of the 30 per cent (n=24) of projects that demonstrated a low income focus, nurses were employed in the majority (n=21) of these. Whilst there were fewer (n=21) nurses employed in projects with a low income focus, these nurses accounted for a greater proportion (88%) of the projects employing nurses when compared with projects employing nurses that did not have a low income focus (79%). 181 7.3.9 Disease, condition or other by projects employing nurses Table 24: Disease or condition or other by projects employing nurses Disease, condition or other No nurses n (%) Other 2 (13.3) Diabetes Nurses n (%) Total n (%) 12 (18.5) 14 (17.5) 0 (0) 9 (13.8) 9 (11.3) Cardiac 1 (6.7) 4 (6.2) 5 (6.3) Meningitis 1 (6.7) 0 (0) 1 (1.3) Mental health 0 (0) 6 (9.2) 6 (7.5) Asthma/respiratory Chronic obstructive pulmonary disease Iron deficiency 0 (0) 4 (6.2) 4 (5.0) 2 (13.3) 5 (7.7) 7 (8.8) 0 (0) 1 (1.5) 1 (1.3) Hip fracture 3 (20.0) 1 (1.5) 4 (5.0) Hepatitis B 0 (0) 1 (1.5) 1 (1.3) Cerebrovascular disease 1 (6.7) 3 (4.6) 4 (5.0) Sexual & reproductive health 0 (0) 5 (7.7) 5 (6.3) Urinary tract infection 0 (0) 1 (1.5) 1 (1.3) Acute confusion 1 (6.7) 3 (4.6) 4 (5.0) Acute conditions 0 (0) 1 (1.5) 1 (1.3) Two or more chronic conditions 4 (26.7) 7 (10.8) 11 (13.8) Dental health 0 (0) 1 (1.5) 1 (1.3) Obstetric health 0 (0) 1 (1.5) 1 (1.3) 65 (100.0) 80 (100.0) Total 15 (100.0) Diabetes, two or more chronic conditions, mental health, chronic obstructive pulmonary disease, sexual and reproductive health, cardiac conditions, and asthma and respiratory conditions were targeted most often (n=36) by projects employing nurses (n=65). Projects that did not employ nurses (n=15) did not target diabetes, mental health, sexual and reproductive health, or asthma and respiratory conditions. Whilst projects targeted two or more chronic conditions, chronic obstructive pulmonary disease, cerebrovascular disease and cardiac conditions (n=8), there was an also an emphasis on hip fracture, meningitis and acute confusion (n=5) (see Table 24). 182 7.3.10 Chronic or acute condition, well-health, or other by projects employing nurses Of the projects employing nurses (n=65), over half (55%; n=36) targeted chronic conditions. Twenty per cent (n=13) targeted well-health, 6 per cent (n=4) acute conditions, and 19 per cent (n=12) were classified as other. 7.3.11 Non-nursing personnel by projects employing nurses Of the 80 projects, almost 40 per cent (n=30) employed non-nursing personnel. A higher percentage of non-nursing personnel were employed in projects that did not employ nurses (47%; n=7) compared with projects that employed nurses (35%; n=23). Project administration and service coordination was most often undertaken by nonnursing personnel in projects that did not employ nurses (40%; n=6) compared with projects that employed nurses (26%; n=17). It is of note that non-nursing personnel conducted research and audits in four projects, all of which employed nurses. 7.4 7.4.1 Chronic or acute condition, well-health, or other Health service by chronic or acute condition, well-health, or other A chronic condition focus was apparent in half of the 80 projects, with specific health services, and combinations of services such as treatment and follow-up and rehabilitation, provided in over 60 per cent of these projects. Screening and prevention comprised almost half of the well-health projects (see p. 184, Table 25). 183 Table 25: Health service by chronic and acute condition, well-health, or other Other Acute condition n (%) Well-health Total n (%) Chronic condition n (%) n (%) n (%) No health services 7 (41.2) 15 (37.5) 1 (12.5) 2 (13.3) 25 (31.3) Combination of services 5 (29.4) 15 (37.5) 3 (37.5) 1 (6.7) 24 (30.0) Diagnostic testing & advice 2 (11.8) 3 (7.5) 0 (0) 3 (20.0) 8 (10.0) Rehabilitation 1 (5.9) 2 (5.0) 1 (12.5) 1 (6.7) 5 (6.3) Screening & prevention 1 (5.9) 2 (5.0) 0 (0) 7 (46.7) 10 (12.5) Health promotion 1 (5.9) 1 (2.5) 0 (0) 1 (6.7) 3 (3.8) Treatment & follow-up 0 (0) 2 (5.0) 3 (37.5) 0 (0) 5 (6.3) 40 (100.0) 8 (100.0) Total 7.4.2 17 (100.0) 15 (100.0) 80 (100.0) Project level of population-based practice by chronic or acute condition, well-health, or other Of the projects with a chronic condition focus (50%; n=40), individual and systems levels of practice were adopted either exclusively (n=20), or in combination (n=15) and were clearly the preferred approach for these projects. Similarly, in projects with an acute condition focus, system, and individual levels of practice were most often adopted. A community level of practice was apparent in well-health projects, and projects classified as other most often adopted a systems level of practice consistent with the development of databases and disease-state registers (see p. 185, Table 26). 184 Table 26: Project level of population-based practice by chronic or acute condition, wellhealth, or other Individual Systems n (%) n (%) Individual & Community n (%) Individual Community & & Systems Systems n (%) n (%) Individual & Community & Systems n (%) Total n (%) 11 (42.3) 1 (11.1) 4 (17.4) 1 (100) 0 (0) 17 (21.3) Chronic 10 (55.6) 10 (38.5) condition 2 (22.2) 15 (65.2) 0 (0) 3 (100) 40 (50.0) Acute condition 2 (11.1) 4 (15.4) 1 (11.1) 0 (0) 0 (0) 8 (10.0) Wellhealth 6 (33.3) 1 (3.8) 5 (55.6) 3 (13.0) 0 (0) 0 (0) 15 (18.8) Total 18 (100) 26 (100) 9 (100) 23 (100) 1(100) 3 (100) 80 (100) Other 7.4.3 0 (0) 1 (4.3) Age group by chronic or acute condition, well-health, or other Children were the age group least represented in projects with a chronic condition focus (n=5). Children were targeted in four well-health projects and three targeting acute condition. Adults (21-55 years) were the age group best represented in projects targeting chronic condition, acute condition, and well-health. Older adults (>55 years) were targeted in projects focusing on acute condition, chronic condition, and those classified as other. Other included projects that targeted a disease or condition in the development of databases and disease-state registers, which contrasted with projects classified as chronic and acute where there was direct clinical intervention. Projects did not target the maintenance of well-health in older adults (see p. 186, Table 27). 185 Table 27: Age group by chronic or acute condition, well-health, or other All ages n (%) Other Chronic condition Children n (%) 7 (31.8) 1 (7.7) 11 (50.0) 5 (38.5) Adults n (%) 0 (0) Older adults n (%) 9 (40.9) 17 (8.9) 15 (65.2) 9 (40.9) 40 (50.0) 8 (10.0) Acute condition 0 (0) 3 (23.1) 1 (4.3) 4 (18.2) Well-health 4 (18.2) 4 (30.8) 7 (30.4) 0 (0) Total 7.4.4 22 (100.0) 13 (100.0) Total n (%) 23 (100.0) 22 (100.0) 15 (18.8) 80 (100.0) Age group by disease, condition or other Of the projects targeting children (n=13) approximately half (n=7) focused on a specific disease or condition, with asthma and respiratory conditions and two or more chronic conditions accounting for five of these projects. Of the projects targeting adults (n=23), the majority (96%; n=22) focused on a specific disease or condition. Diabetes, mental health, chronic obstructive pulmonary disease and sexual and reproductive health accounted for the greatest number of projects. Of the projects targeting older adults (n=22), the majority (95%; n=21) focused on specific diseases or conditions. Two or more chronic conditions, acute confusion, hip fracture and cerebrovascular disease accounted for the greatest number of projects. Of the projects targeting all ages (n=22), 64 per cent (n=14) focused on specific diseases or conditions. Diabetes, cardiac conditions and two or more chronic conditions accounted for the greatest number of projects. 186 7.4.5 Ethnicity by type of disease, condition or other Of the projects targeting Maori (48%; n=38) both exclusively or within the wider population, and including Pacific people, 19 targeted diseases or chronic conditions and 13 targeted well-health. Few projects targeted acute conditions (n=3) or were classified as other (n=3). Of the projects targeting Pacific peoples (26%; n=21) both exclusively or within the wider population, and including Maori, eight targeted diseases or chronic conditions and six targeted well-health. Only three projects targeted acute conditions and four were classified as other. Almost half of the projects (n=38) did not have an ethnicity focus, and more than 50 per cent (n=20) of these projects targeted chronic conditions. 7.5 7.5.1 Age group Ethnicity by age group with and without disease or condition Twelve of the 13 projects targeting children with or without a disease or condition had a Maori and/or Pacific focus. Thirteen of the 23 projects targeting adults with or without a disease or condition had a Maori and/or Pacific focus. Of these projects, 12 targeted adults with a specific disease or condition. One of the 22 projects targeting older adults with or without a disease or condition had a Maori and/or Pacific focus, and this sole project did not have a disease or condition focus. Projects did not target older Maori or Pacific adults with a specific disease or condition (see p. 188, Table 28). 187 Sixteen of the 22 projects targeting all ages with or without a disease or condition, had a Maori and/or Pacific focus. Of these projects nine focused on Maori exclusively and most also targeted a disease or condition. Table 28: Ethnicity by age group with or without disease or condition No ethnicity Maori Maori & wider population Pacific Pacific & Maori n (%) n (%) n (%) n (%) n (%) All ages 4 (10.5) 2 (15.4) 0 (0) 0 (0) All ages/ disease or condition 2 (5.3) 7 (53.8) 3 (37.5) Children 0 (0) 1 (7.7) Children/ disease or condition 1 (2.6) Adults Adults & disease/ condition Pacific & Maori & wider population n (%) Total n (%) 0 (0) 2 (12.5) 8 (10.0) 1 (25.0) 0 (0) 1 (6.3) 14 (17.5) 1 (12.5) 1 (25.0) 0 (0) 3 (18.8) 6 (7.5) 0 (0) 1 (12.5) 1 (25.0) 1 (0) 3 (18.8) 7 (8.8) 0 (0) 1 (7.7) 0 (0) 0 (0) 0 (0) 0 (0) 1 (1.3) 10 (26.3) 2 (15.4) 2 (25.0) 1 (25.0) 0 (0) 7 (43.8) 22 (27.5) Older adults 0 (0) 0 (0) 1 (12.5) 0 (0) 0 (0) 0 (0) 1 (1.3) Older adults & disease/ condition 21 (55.3) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 21 (26.3) Total 38 (100) 13 (100) 8 (100) 4 (100) 1 (100) 16 (100) 80 (100) 7.5.2 Income by age group, with or without disease or condition Populations in low decile areas, classified low income, were targeted in 30 per cent (24/80) of projects. Seventeen of these projects targeted a disease or condition in people of all ages (n=9), adults (n=7), and children (n=1). It is important to note, that projects with a low income focus did not specifically target older adults with or without a disease or condition. 188 However, 22 projects that did not target low income, but focused on all older people, targeted a disease or condition (n=21). This occurred similarly in projects focusing on adults where 22 of 23 projects targeted a disease or condition. Children were represented in five projects targeting low income and an additional 13 projects without this focus, included seven projects targeting a disease or condition. The greatest proportion of projects with a low income focus (n=11) targeted all ages, and in addition, a further 14 of 22 projects without an income focus, targeted a disease or condition. 7.6 Nursing interventions Seventeen nursing interventions are reported independently. The characteristic or variable, level of population-based practice (individual, community, or systems), was compared with a range of other variables of interest. This variable was manipulated to create the categories of individual, community and systems. The original categories (see p. 154) were combined placing all categories with individual together, with community together, and with systems together. Therefore, some of the original categories are represented in one or more of the three new categories. For each of the comparison variables, one or two categories were selected for comparison: disease, condition or well-health; low income, and ethnic group (see p. 152, Table 16). The categories for ethnic group (see p. 152, Table 16 question 13) were manipulated to create a category ‘Maori’ comprising all categories that included Maori. Individual Thirteen of the 17 interventions were undertaken most often at the individual level, relative to the community or systems level in projects. They were health teaching (n=31) (see p. 190, Table 29), consultation (n=31), collaboration (n=30), referral and follow-up (n=30), case management (n=30), delegated functions (n=29), counselling (n=29), advocacy (n=29), policy development and enforcement (n=24), screening 189 (n=23), outreach (n=22), disease and health event investigation (n=14) and social marketing (n=12) (see p. 192, Figure 17 and Appendix 4). Table 29: Health teaching intervention undertaken by nurses in projects Individual Community Systems Ethnic Group Low Income Total No. projects Maori (%) Low decile area (%) 31 4 1 21 (67.7) 3 (75) 0 (0) 16 (51.6) 2 (50) 0 (0) Disease/Condition or Well-health Chronic (%) 18 (58.1) 3 (75) 1 (100) Well-health (%) 7 (22.6) 1 (25) 0 (0) For categories Maori, low decile area, chronic (disease or condition), and well-health, the individual level of interventions consistently contained more projects (see Table 29 and Appendix 4). Community Both the community organising and coalition building interventions were undertaken most frequently at the community level, relative to the systems level. In fact, systems level community organising interventions were not undertaken in any projects (see p. 192, Figure 17). Note individual level interventions are never undertaken in these interventions (see p. 94). For categories Maori, low decile area, chronic, and wellhealth, the community level of both interventions consistently contained more projects (see p. 190, Table 30 and p. 191, Table 31). Table 30: Community organising intervention undertaken by nurses in projects Community Systems Ethnic Group Low Income Total No. projects Maori (%) Low decile area (%) 15 0 14 (93.3) 0 (0) 8 (53.3) 0 (0) Disease/Condition or Well-health Chronic (%) 7 (46.7) 0 (0) Well-health (%) 6 (40) 0 (0) 190 Table 31: Coalition building intervention undertaken by nurses in projects Community Systems Ethnic Group Low Income Total No. projects Maori (%) Low decile area (%) 24 12 20 (83.3) 8 (66.7) Disease/Condition or Well-health Chronic (%) 11 (45.8) 4 (33.3) 13 (54.2) 6 (50) Well-health (%) 7 (29.2) 3 (25) Systems The surveillance intervention was undertaken most often at the systems level relative to the individual and community levels (see p. 192, Figure 17). For categories Maori, low decile area, chronic, and well-health, the systems level of surveillance intervention consistently contained more projects (see Table 32). Table 32: Surveillance intervention undertaken by nurses in projects Individual Community Systems Ethnic Group Low Income Total No. projects Maori (%) Low decile area (%) 1 2 11 1 (100) 2 (100) 9 (81.8) 0 (0) 0 (0) 3 (27.3) Disease/Condition or Well-health Chronic (%) 0 (0) 1 (50) 5 (45.5) Well-health (%) 0 (0) 0 (0) 3 (27.3) 191 Figure 17: Interventions and levels of population-based practice undertaken by nurses in projects 7.7 Social values embedded in the practices of nurses employed in projects Beattie’s analytical model of health promotion (Beattie, 1991) allows links between health promotion values and the practice of nurses employed in projects to be identified. Figure 17 shows sixteen interventions62 and the level of population-based practice most often undertaken by nurses with regard to each intervention. Interventions are situated within Beattie’s model of health promotion, which has been 62 ‘Case finding’ the seventeenth intervention is included within the interventions surveillance, disease and health event investigation, outreach, and screening at the individual level. 192 adapted (see p. 194, Figure 18). The rationale for adapting the original model is identified in chapter six, data analysis stage two (see pp. 160-161). The majority (14/17) of the interventions are situated on the x-axis in the direction of the individual focus of intervention, ranging numerically from the highest, case management (n=37) to the lowest, social marketing (n=8). Nine of these interventions: social marketing; surveillance; disease and health event investigation; policy development and enforcement; screening; delegated functions; health teaching; referral and follow-up, and case management are situated within the quadrant titled health persuasion, reflecting a paternalist and individual-oriented philosophy (Beattie, 1991). The five remaining interventions: outreach, collaboration, advocacy, counselling and consultation are situated in the personal counselling quadrant, which highlights a negotiating approach, maintains an individual-oriented philosophy, but does not necessarily imply paternalism. Two interventions, coalition building and community organising are situated on the xaxis in the direction of the community focus of intervention. Community organising is situated in the community development quadrant, reflecting collective action that is participative and community based, whilst coalition building is situated mid-way between legislative action and community development, reflecting collective action that can be participative and community based or paternalistic and state-directed (Beattie, 1991). The authoritative mode of intervention was apparent in 10 of the 16 interventions undertaken by nurses, with coalition building the only intervention to have a collective focus. A negotiated mode of intervention was apparent in seven interventions that included coalition building, with only two having a community focus. 193 Figure 18: An adaptation of Beattie’s model of health promotion situating total interventions by nurses in projects 194 7.8 Summary of study results The current study has four central research questions (see p. 128, section 6.2). A summary of the results is included in Table 33, as a precise means of responding to the research questions. Question one precedes a list of the characteristics of integrated care projects. Selected brief evidence informs the association between project characteristics and projects employing nurses, before a rating of the strength of this association is attributed. ‘Strong association’ equates to 85 per cent and over, ‘association’ to 16 - 84 per cent, and ‘weak association’ to 0 - 15 per cent. Questions 2, 3, and 4 are answered simultaneously. Each intervention is briefly identified, with the most frequent level of practice and social values pertaining to that intervention, ascribed. Table 33: Summary of research questions and evidence informed responses Research question 1: Which characteristics of integrated care are more strongly associated with projects that employ nurses? Characteristic Evidence Rating scale Weak Association Strong association association (0 - 15%) (16 - 84%) (85-100%) Organisation (see section 7.3.1) √ Providing an existing service differently and planning a new service In 60% of projects general practice provided care previously provided by hospital specialists and nurses were employed in 85% of these projects. In addition, 38% planned a new service and nurses were employed in 97%. Health services provided by project Almost 70% of projects provided health services and nurses were employed in 78% of these projects. √ Incentives and costs: General Practice 84% of general practices received incentives to participate and nurses were employed in 78%. √ General practice did not incur financial costs as a result of participating in projects. Incentives and costs: Hospitals Material incentives to clients √ 11% of hospitals incurred financial costs as a result of participating in projects and nurses were employed in 67% of these projects. √ 93% of hospitals received incentives to participate in projects and nurses were employed in 80%. √ 5% of projects provided material incentives to clients and nurses were employed in all projects (100%). √ 195 Funding (see section 7.3.2) Type of service integration (see section 7.3.3) 68% of projects received the main source of new funding from government and nurses were employed in 82% of these projects. √ 40% of projects were vertically integrated and nurses were employed in 69% of these projects. √ 19% of projects were horizontally integrated and nurses were employed in 100%. √ 41% of projects were vertically and horizontally integrated and nurses were employed in 85%. √ Information sharing 65% of projects undertook information sharing building relationships, peer advice & education, peer referral, and client education, and nurses were employed in 88% of these projects. √ Database for information sharing 50% of projects undertook database development, and nurses were employed in 85%. √ Guideline development 21% of projects undertook guideline development and nurses were employed in 94%. √ Guideline promotion 36% of projects undertook guideline promotion and nurses were employed in 93%. √ Case management 33% of projects undertook case management and nurses were employed in 96%. √ New coordination strategy 56% of projects undertook a new coordination strategy and nurses were employed in 84%. Strategies for integrated care (see section 7.3.4) Project level of population-based practice (see section 7.3.5) √ √ 67% of projects adopted an individual level of practice and nurses were employed in 87% of these projects. √ 16% of projects adopted a community level of practice and nurses were employed in all (100%). Age group focus (see section 7.3.6) 66% of projects adopted a systems level of practice and nurses were employed in 83%. √ 28% of projects targeted people of all ages and nurses were employed in 82% of these projects. √ 16% of projects targeted children and adolescents (0-20 years) and nurses were employed in 92%. √ 29% of projects targeted adults (21-55 years) and nurses were employed in 91%. √ 28% of projects targeted older adults ( 55 years) and nurses were employed in 64%. √ 196 Ethnic group focus (see section 7.3.7) Low income focus (see section 7.3.8) Chronic or acute disease or condition, well-health or other focus (see section 7.3.9) 53% of projects targeted Maori and/or Pacific peoples exclusively or in combination with the wider population and nurses were employed in 90% of these projects. √ 30% of projects targeted populations in geographic areas defined as low decile and representing the 30% most deprived areas in New Zealand, and nurses were employed in 88% of these projects. √ 50% of projects targeted chronic conditions and nurses were employed in 90% of these projects. √ √ 21% of projects targeted ‘other’ (such as information management) and nurses were employed in 71%. √ 19% of projects targeted well or positive health and nurses were employed in 87%. Practice of nonnursing personnel (see section 7.3.10) 10% of projects targeted acute conditions and nurses were employed in 50%. √ 38% of projects employed non-nursing personnel and nurses were employed in 77% of these projects. √ Research questions 2, 3, and 4: What types of population-based interventions were undertaken by nurses in integrated care projects? What population-based levels of practice did nurses demonstrate in integrated care projects? What underlying values are made explicit when interventions undertaken by nurses are analysed? Types of interventions Levels of practice most often undertaken Values made explicit in interventions Individual Community Systems √ Surveillance Collected and analysed data on health threats, such as chronic disease Health Persuasion Authoritative mode Individual focus Disease and health event investigation Focused on chronic diseases and other health events, a key component of surveillance √ Health Persuasion Outreach Informed those at risk, of risks to inform action, used in conjunction with health teaching √ Personal counselling Authoritative mode Individual focus Negotiated mode Individual focus 197 Screening Preceded by outreach/social marketing, and in conjunction with health teaching/counselling √ Health Persuasion Referral and follow-up Nurses received referrals and referred on, always linked with another intervention √ Health Persuasion Case management Clinical case management model preferred, emphasis on clients with chronic conditions √ Health Persuasion Delegated functions Most often from GPs, and delegation to other nurses, often related with case management √ Health Persuasion Health teaching Most frequent intervention implemented sequentially with counselling and consultation √ Health Persuasion Counselling Aided problem solving, acknowledged feelings √ Personal counselling Consultation Frequently a component of case management, such ‘advice’ often followed health teaching √ Personal counselling Collaboration Changed both the client and nurse, was linked with concepts of empowerment and partnering √ Personal counselling Authoritative mode Individual focus Authoritative mode Individual focus Authoritative mode Individual focus Authoritative mode Individual focus Authoritative mode Individual focus Negotiated mode Individual focus Negotiated mode Individual focus Negotiated mode Individual focus √ Coalition building Collective action that was mandated, but sought to engage communities in projects Legislative action and Community development Authoritative & Negotiated modes Collective focus √ Community organising With social marketing, activities sought to change the health behaviours of communities Community development Negotiated mode Collective focus Advocacy Negotiated with clients, acting in a client’s interest occurred in many related interventions √ Personal counselling Social marketing ‘Health information’ congruent with a client’s values was aligned with other interventions √ Health Persuasion Policy development and enforcement Occurred most frequently at the local level, with enforcement occurring at the nation level √ Health Persuasion Negotiated mode Individual focus Authoritative mode Individual focus Authoritative mode Individual focus 198 8 8.1 Chapter 8 Discussion Introduction In this thesis data from a descriptive survey were analysed to quantitatively profile the characteristics of integrated care projects in order to identify the strength of the relationship between specific characteristics and the practice of nurses in these projects. The practice of nurses was investigated on three dimensions: the types of interventions; individual, community and systems levels of practice, and the values that could be identified from the manner in which nurses worked (see p. 128, section 6.2 research questions). Characteristics of integrated care refer to the following ten variables: organisation; funding; type of service integration; strategies for integration; level of project approach; age group targeted; ethnic group targeted; low income group targeted; health, disease or condition targeted, and the practice of non-nursing personnel, which were comprehensively discussed in chapter six (see p. 127). Sections 8.2 to 8.4 answer the four research questions, with all sections beginning by reporting relevant new findings. Section 8.2 analyses each characteristic of integrated care and the strength of the association with projects employing nurses. These findings are discussed in light of the literature reviewed. Section 8.3 identifies the interventions and population-based levels of practice undertaken by nurses and analyses these by systematic reference to the ‘public health intervention model’ presented earlier. Practice examples illustrate the range and level of work undertaken by nurses within the integrated care environment and enable deeper insights into the nature of these practices. Section 8.4 explores the health promotion values embedded within interventions and considers the implications of practice situated in a single dominant paradigm. Health promotion theory, and in particular Beattie’s model of health promotion (see pp. 30-36) is applied to help make the values within interventions explicit and as a reference point for critical analysis. Finally, on the basis of study findings the Primary Health Care Interventions Model (PHCI model), a new framework to assist the implementation of PHC nursing practice, is presented. 199 8.2 Which characteristics of integrated care are more strongly associated with projects that employ nurses? The characteristics strongly associated with projects that employ nurses are: 1. organisation: providing an existing service differently and planning a new service; providing material incentives to clients; 2. type of integration: horizontal integration; a combination of both horizontal and vertical integration; 3. strategy for integration: information sharing; database for information sharing; guideline development; guideline promotion; case management; 4. project population-based practice: individual-level; community-level; 5. age group focus: children and adolescents; adults; 6. ethnic group: Maori and Pacific; 7. low income: populations representing the 30 per cent most deprived areas in New Zealand, and 8. health, disease/condition or other focus: chronic conditions, and well-health. These characteristics, and other characteristics not as strongly associated with projects employing nurses, are described in relation to nurses’ practice (see pp. 195-198, Table 33). 8.2.1 8.2.1.1 Organisation Delivering an existing service differently and planning a new service A strong association was evidenced between general practices employing nurses and delivering an existing service differently, such as a shift in services previously provided by hospitals to general practice. This transition of existing services from secondary to primary sectors also influenced the planning of new services within the primary sector (see p. 163). Services included administering ‘free’ influenza vaccines, taking echocardiograms, sexual health management, providing (functional) rehabilitation programmes, and conducting mental health assessments. The majority of these services retained a narrow primary health care focus on individuals (see p. 184). This study identified that general practice operating within a clinical medical paradigm constructed an environment where nurses undertook tasks delegated by their employers and perpetuated a selective or narrow primary health care approach to the delivery of existing services and the planning of new services. This is probably because practice nurses have traditionally been employees of general practice 200 physicians who operate in privately owned businesses (Minto, 2004) and as Docherty (2004) suggests it has always been difficult for nurses to provide a more comprehensive nursing service when the ‘service’ is financially determined by the employer. The majority of projects employing nurses maintained a governance base, personnel, and philosophy analogous to those of general practice. There was little evidence of innovation in nurses’ approach to primary health care. Overall, there was little evidence of the primary health care approach described by the World Health Organization (1986) and advocated in the PHC Strategy (Ministry of Health, 2001c). These approaches are multi-level and comprehensive. For example, a primary health care nurse working with older adults at risk of hip fracture in the future, for example, could facilitate access to exercise programmes that improve strength, balance and gait (individual level), advocate for traffic-free walking areas (community level), and collaborate to promote the positive ageing strategy as a framework for health service provision (systems level). This type of multi-level primary health care approach develops personal skills, creates supportive environments and reorients health services - health promotion strategies that go beyond healthy life-styles to overall well-being (World Health Organization, 1986). The future contribution of nurses in primary health care has “yet to be fully realised” (Ministry of Health, 2003b, Executive summary, para. 1), with more comprehensive approaches to service provision necessary. 8.2.1.2 Health care services provided by projects An association was evidenced between health care services provided by projects, such as screening and prevention, diagnostic tests and expert advice, health promotion, treatment and follow-up, and rehabilitation, and nurses employed in projects. Only projects employing nurses undertook health promotion. The different approaches adopted by projects reflected distinctive priorities and different perspectives about clients. For example, health education that targeted children with asthma was the sole health promotion activity in one project while another project saw 201 health promotion as creating a supportive environment for physical recreation. The asthma education project was limited in scope to concepts of prevention and health protection. The physical recreation project by comparison, attempted to promote positive health and targeted people in a community setting. This project linked to other services that could offer information and education about health and social issues, empowering clients to set their own health agendas. Health promotion was not defined in the questionnaire allowing for the widest interpretation of this activity by respondents. Internationally there has been a continuing theoretical debate about whether health promotion should include disease reduction and prevention, and health protection, or whether it should be concerned solely with positive health (Downie et al., 1990; J. French, 1990). Similarly, a wide variation in perspectives was reflected in project descriptions of health promotion practice. In general an individualistic health education approach prevailed. Although Carryer et al. (1999) suggest that nurses understand a strategy of health promotion that addresses the social and environmental determinants of health (see p. 78), this study found that very few projects attempted a comprehensive approach and that nurses almost never addressed the determinants of health in health promotion activities. This may be attributed to a lack of understanding of the broad strategies of health promotion or to organisational characteristics discussed earlier that limited nurses’ influence, or both. Beattie (1991) contends it is necessary to understand how health promotion is connected to broader social, political and cultural values in order to develop practice and improve health outcomes. The absence of evidence of engagement by nurses in health promotion activities indicates a need to address both issues of understanding and governance (see p. 208). Treatment and follow up and rehabilitation were undertaken least in projects employing nurses. General practice physicians or hospital specialists saw clients most often in their clinics or practices for medical treatments and/or follow up assessments after discharge from hospital for conditions such as hip fracture or chronic obstructive pulmonary disease. Rehabilitation was ‘functional’ seeking to improve the activities of daily living for clients who had suffered a condition such as a cerebrovascular disease. Physiotherapists undertook most of the rehabilitation in projects, and services were provided in hospital out-patient departments or client’s homes. 202 Treatment and follow-up assessments, and rehabilitation were undertaken by individual clinicians, usually general practice physicians and physiotherapists, using traditional bio-medical and mechanistic approaches to health care. The reason for nurse’s limited participation is unclear, but may relate to a perception by project planners that nurses had no distinct contribution to make. Whilst nurses in integrated care projects had a lesser involvement in rehabilitation, it is a potential area for future primary health care nursing development. Recognition of the importance of the social and cultural environment to health (Ministry of Health, 2001c) has provided nurses with a legitimate framework in which to construct care such as rehabilitation, and redefine the nursing contribution. For example in the field of older people’s health, a new service and funding model ‘ASPIRE63’ is using nurses to provide restorative and rehabilitative services to older people living in their own homes (Parsons et al., 2004). Nurses lead a case management team of physiotherapists, occupational therapists, general practitioners and support workers in five New Zealand cities and this model is currently being assessed for application in a large multicultural population of all ages, with nurses again managing complex rehabilitation packages (Baird, 2004). Interestingly, whilst nurses employed in integrated care projects undertook a limited role in rehabilitation, nurses were actively engaged in case management, skills transferable to new primary health care nursing roles. 8.2.1.3 Incentives and costs for general practice to be a project partner An association was evidenced between general practice incentives and nurses employed in projects with general practice partners. Overall, integrated care benefited general practice partners financially by assisting them to develop new and/or existing services or to pay for case management. Nurses did not benefit directly as they were employees of general practice physicians and did not have a financial investment in the business. 63 ASPIRE is the acronym for ‘Assessment of Services Promoting Independence and Recovery in Elders’. 203 General practice did not incur financial costs as a result of participating in projects (see Appendix 3, Question 20), although general practice partners contributed to the funding of projects (see Appendix 3, Question 17). Investigation of these results revealed the funding of projects was not considered a cost by respondents in the same way as ‘lesser unanticipated costs’ arising in project planning and implementation, which accounted for what initially appeared to be a discrepancy in responses. 8.2.1.4 Material incentives to clients A strong association was evidenced between the projects offering material incentives to clients and projects employing nurses. Material incentives to clients were only offered in projects with a strong primary sector influence. Gifts, for example, were donated by retail business when approached by nurses employed in a general practice, and clients entitlement to gifts related, in one instance, to having achieved weight loss. Vouchers for free monthly general practice consultations however, were offered to people enrolled in the intervention group of a project that sought to test the strategy of case management for people with chronic obstructive pulmonary disease64. This incentive enabled the intervention group to attend the general practice for a routine monthly health check and ultimately ensured the success of the project. Other incentives, such as building repairs to homes, and the installation of amenities, such as inside toilets, resulted from projects that engaged both the health sector - nurses in clinical health assessments, and the housing sector - builders in home assessments. Material incentives to clients did not incur costs to project partners in the health sector, except the project using vouchers, which included these costs at the planning stage. The incentives offered to clients in a small number of projects sought to encourage people to change their health behaviours or participate in some form of health promotion. This approach is consistent with international strategies that attempt to help individuals become activated consumers (Bodenheimer et al., 2002a). In the current study incentives were offered to clients who had chronic conditions and 64 The individuals with chronic obstructive pulmonary disease who were randomised into the control group did not have access to vouchers. 204 resided in the poorest areas of New Zealand. This is a strategy similar to that of providing benefits to poorer populations in the United States to promote active participation (The Robert Wood Johnson Foundation, 2000). 8.2.1.5 Incentives and costs for the hospital to be a project partner An association was evidenced between hospitals receiving incentives to participate in projects and projects employing nurses. The most frequent incentive to participate was to reduce hospital admissions. Like general practice, incentives also included improving existing health services and planning and/or delivering new health services, which resulted in financial gains. A number of nurses in hospitals worked between the primary and secondary sectors in projects contributing, for example, to team case management. Hospitals invested in this nursing role as part of a wider strategy to prevent avoidable admissions for conditions such as diabetes, chronic obstructive pulmonary disease, and cardiac conditions. Unlike general practice however, hospitals did not seek to generate revenue. An association was also evidenced between hospitals incurring costs and the projects employing nurses. Several projects reported hospital partners incurred costs when, for example, they funded projects, paid for vaccines that were administered in general practice, coordinated the database for projects that indicated they had not received dedicated funding, developed guidelines, protocols and care maps for use in projects, conducted smoking cessation programmes, and provided clinical and technical personnel for work in primary and secondary sectors. Hospital partners supported integrated care projects financially, motivated by the need to reduce hospital admissions. This motivation influenced the part hospitals played in integrated care and the predominant bio-medical focus of many projects to managing diseases or conditions. Particular costs incurred by hospitals, such as the development of guidelines and protocols to guide best practice provided a professional incentive related in part to the development of professional relationships across the health sector between those who had shared interests in longer term clinical outcomes. Malcolm (1997) suggests 205 professional incentives can be much more effective than market and commercial incentives in modifying professional behaviour. The effectiveness of professional and/or financial incentives in encouraging project development is unclear, but an investment in the primary sector by the secondary sector was apparent. 8.2.2 Funding An association was evidenced between projects that received their main source of new funding from government and nurses employed in these projects. Projects received their main source of funding (new money) from either the Government or project partners, or used existing resources from organisations partnering in projects. Interestingly, the latter arrangement to resource projects by pooling existing resources, rather than dedicating new money from a primary source, resulted in these projects being identified as not having received funding. Direct government funding was received by 70 per cent of the projects, and as the strategy of integrated care was promoted by Government as a purchasing method to develop services that ensured coordinated care between primary, secondary and tertiary sectors (Scott, 1997), this was not unexpected. However, other than the allocation of more than NZ$1 million for the development of nine demonstration integrated care pilot projects, the study revealed new information about other projects that had received additional government funding and were defined by stakeholders as integrated care projects. Nurses employed in projects that received their main source of funding (new money) from government were noticeably larger in scale than projects receiving funding from other sources. It was not possible to establish the nature of the relationship between receiving new money directly from government and projects employing nurses, although it is likely that this additional resource was in part used to employ nurses. One large-scale project, uncharacteristic of all other projects, received similar amounts of new funding from both the Government and project partners and relied heavily upon nursing. Involving 51 general practices and 135 patients with a clinical diagnosis of chronic obstructive pulmonary disease, case management was undertaken by practice nurses, general practice physicians, respiratory nurse specialists, and respiratory physicians (Rea et al., 2004). 206 A small number of projects received their main source of funding from project partners unable to gain additional financial support from government. A number of these projects involved database development and the hospital partner was frequently the greatest contributor. Such projects commonly employed nurses who received a salary from the project partner who were their primary employer, which ensured no direct cost to the project. For example, a nurse specialising in diabetes management continued to be salaried by the hospital but worked in the project expanding the nursing role to include case management. Project partners frequently committed resources, such as nursing services, in addition to investing in the projects main source of funding. 8.2.3 Type of service integration A strong association was evidenced between projects that employed nurses and were horizontally integrated, and also projects that were both horizontally and vertically integrated. A lesser degree of association was evidenced between projects employing nurses and projects vertically integrated. Nurses were employed in all projects that were horizontally integrated with this type of integration occurring most in the primary sector between general practice and other primary health care providers. Nurses in the primary sector often refer clients to services not provided by their organisation such as family planning, sexual health, rehabilitation, mobile nursing, physiotherapy, osteopathy, chiropractic and pharmacy, and the short time often allocated in general practice physician consultations is a further reason for referral (T. Ashton, 1998). Consequently, collaborating with others in the same sector is routine nursing practice. Nurses were generally not involved in vertical integration without also engaging in horizontal integration, although exclusive vertical integration occurred between general practice physicians and hospital specialists who communicated over clients’ conditions and had authority to plan services and commit funding. Nurses, in contrast, did not have the authority to engage in planning services requiring the commitment of funds, so frequently acted in a role scripted by their employer that 207 influenced the range of interventions undertaken. The College of Nurses Aotearoa (NZ) Inc. (2001) contended that community nurses roles were assistive and compensatory (to general practice physicians) limiting their contribution, and arguing that more collegial collaboration is critical to the success of primary health care teams. They maintain that nurses need to be involved at a governance level, influencing funding and service delivery. An exception to this exclusion of nurses from governance was found in Maori provider organisations. Nurses in Maori provider organisations were involved in decision-making at a governance level and assisted projects to develop and maintain vertical integration. These nurses collaborated with clinicians in the secondary sector and with others in the primary sector (horizontal and vertical integration), during the provision of mobile nursing services to people with chronic conditions. It is likely that such roles enabled nurses to gain a wider understanding of both the health and social needs of clients and the cultural and organisational differences of providers. High visibility of new roles and knowledge appeared to influence nurse’s participation at a governance level (S. Keown, personal communication, October 11, 2004). Whilst projects employing nurses had a greater focus on horizontal integration, the study has shown that nurses who were engaged in projects that were also vertically integrated were involved in project governance, and this enabled them to be more influential. Vertical integration remains important as resources are predicted to shift toward primary and preventative services in an effort to reduce costs and prevent hospital admissions (Ovretveit, 1998) and collaboration between providers will remain a core function of nurses and other health professional’s roles (Ministry of Health, 2001c). 8.2.4 8.2.4.1 Strategies for integrated care Information sharing Projects employing nurses were strongly associated with information sharing, which included building relationships, peer advice and education, peer referral, client 208 education and the development of databases. Interestingly, building relationships and client education was not undertaken in projects without nurses. Building relationships Nurses in the majority of projects that sought to build relationships between primary and secondary sectors (vertical integration) undertook this activity alongside relationship development within the same sector (horizontal integration). Vertical integration and relationship building were actively promoted by project planners because they aligned with the purpose of constructing a coordinated continuum of care (Health Funding Authority, 1998). A few projects employing nurses, demonstrated complex relationships within the primary sector between general practice, Maori provider organisations, Pacific provider organisations, the housing sector, sports associations, and other community groups. Porter-O’Grady (1999) maintains nursing has always pulled together disparate resources, health workers, and processes and has focused on the client’s journey rather than on specific clinical events. In New Zealand, Maori provider organisations in over two decades of health reform have relied upon nursing to develop health care services (Durie, 1998). So, it was not surprising that nurses employed in Maori provider organisations, who were partners in projects, invested heavily in building relationships. The study demonstrated that projects with nurses built requisite partnerships. The nursing profession has argued the need for intersectoral partnerships and community development (Carryer, 2004). However, if nursing is to play a significant role in these areas a common understanding of the terms is necessary. For example, distinctions between different models of partnership should be understood (see p. 81). The majority of integrated care projects were designed and managed without any form of community representation65 and the few projects employing nurses that built relationships with individuals and communities applied a community involvement model, where the nurses, acting as project advocates, determined the agenda and then 65 Community representation and in particular Maori representation at governance level was evaluated in the demonstration pilot projects, signaling the expectation this would be a feature of integrated care more generally. 209 attempted to get the community on side. partnership was understood by nurses. These projects illustrated the way The interests of communities were not paramount, or even equivalent, to those of the health professional. Peer advice, education and referral Peer advice, education and referral were activities that contributed to building relationships and strengthening projects overall. Peer advice and education most commonly occurred between hospital specialists, such as diabetes specialists and general practice physicians, practice nurses or nurses in Maori or Pacific provider organisations. In a smaller number of cases, nurses with a specialist area of practice, such as mental health, advised and educated other nurses with a wider primary health care focus. Peer advice and education acted as a vehicle for building relationships and establishing trust in a context where all partners shared a common purpose. The sharing of clinical knowledge changed relationships between project partners as they established a team for undertaking functional activities and assessing clinical outcomes. The success of projects depended upon the relatedness of partners who agreed activities and outcomes. This behaviour has been described as an ‘issue of fit’ where the process of each of the partners and the comprehensiveness of the agreed outcome are critical variables in the effectiveness of services (Porter-O'Grady, 1999). Client education Client education occurred in six projects, all employing nurses. Client education was interpreted as a formal component of the project design, rather than an opportunistic activity dependent upon other interventions. Informal client education occurred in many projects and included timely information about the condition, human body, effects of medications, interventions, and available services. However, this was random and the quality and reach of the education could not be established. Client education has the potential to empower consumers to make informed decisions and thereby shape the health care system. Internationally, consumers generally do not think they receive enough information and that health care professionals do not involve them in decisions about their own care (Golodner, 1999). The formal inclusion of client education in the design of relevant projects would have reduced the 210 issue of randomness and allowed assessment of quality and reach. The majority of projects in the current study would have benefited from the inclusion of a formal client education component. This study finding has implications for ensuring client education is undertaken effectively in future projects. Development of a database Investment in information technology accompanied the legal, institutional and functional changes that occurred in the New Zealand health care system during the 1990s. New information allowed decision makers to describe their populations, assess the effectiveness of interventions, and develop better practice. Database development occurred in half of the projects and nurses established a number of health provider databases that required a comprehensive knowledge of the client population. Several projects were related to the case management of clients with chronic conditions where nurses were the sole case manager or had a central role in case management. Nurses also developed databases to plan future services collecting information on, for example: babies 0-24 months old at risk of recurrent urinary tract infections; women with iron deficiency anaemia; children with chronic illnesses and disabilities, and health services used by people residing in a defined geographic area. 8.2.4.2 Guideline development and promotion A strong association was evidenced between guideline development and promotion and projects employing nurses. Guidelines covered a variety of topics including treatment, prevention and screening and provided physicians, nurses, other health professionals, and clients with a resource for obtaining objective information on clinical practices. Nurses were the ‘developer’ of guidelines in half of the projects that undertook this strategy. In one project nurses developed guidelines for coronary heart disease through a stringent process of reviewing literature, expert opinion, selected references, peer review and critical appraisal, and in another project, participated in a team developing a guideline for the management of chronic obstructive pulmonary disease in primary health care settings. Guidelines were developed to clarify the pathway for clients with conditions such as hip fracture, placing an emphasis on 211 rehabilitation to assist health professionals and clients identify available health services as a foundation for integrated care, and later for outcomes management66. Jensen and Koerner (1999) among others support guideline use for longitudinal clinical management and the self-care of chronic conditions. The most common reason for nurses in projects to promote guidelines was their use in the case management of clients. This occurred whether guidelines were developed within projects or externally. Other reasons for promotion included the provision of information to peers and clients, and the benchmarking of clinical practice. Projects without nurses had limited involvement in guideline development and promotion. The study findings suggest nurses in projects developed and promoted guidelines (systematising processes) to guide clinical practice. In contrast, projects without nurses but with doctors had a lesser interest in systematised processes. This interpretation is supported by recent international research on healthcare professional’s attitudes to health reforms (Degeling et al., 2003). These authors found that in four countries, including New Zealand, nurses supported guidelines or integrated care pathways because it enabled them to balance the clinical and resource dimensions of care and the requirements of clinical autonomy and transparent accountability. Nurses held systematised conceptions of clinical work, unlike doctors who favoured individualist conceptions. 8.2.4.3 Case management A strong association was evidenced between projects employing nurses and case management. Nurses were the largest group of individual case managers (68%), also undertaking case management as part of a multidisciplinary team or general practice physician and practice nurse team. Case management occurred in less than half of the projects employing nurses and was seldom undertaken in projects without nurses. The most common case management role was the direct provision of clinical care by a nurse within a specialty area, such as diabetes management. Other roles included 66 Outcomes management refers to a “technology of patient experience designed to help patients, purchasers and providers make rational medical care-related choices based on insight into the effects of these choices on the patient’s life” (Ellwood, 1988, p. 155). 212 facilitating access to services, brokering services, coordinating services, and delegating and supervising other nurses providing clinical care. Whilst numerous case management models exist (Brault & Kissinger, 1991; DeSimone, 1988; Papenhausen, 1990; Weil & Karls, 1985), the key features of case management in the projects investigated revealed similarities with either the ‘clinical case management model’ (Stein & Test, 1980) or the ‘brokerage model’ (Burns, 1997; Kanter, 1989), with the former model being most commonly identified. In the clinical case management model the case manager maintained contact with the client over the long-term. This was not a feature of the brokerage model, which emphasises the “coordination and organisation of services for clients” (Kanter, 1989, p. 114), despite wide consensus that all models should include this element (Ford et al., 1995). International literature identifies additional features sometimes adopted into the clinical case management model. Three such features include the development of an individual’s strengths (Modrcin et al., 1988), a focus on rehabilitation medication management and social skills (Goering et al., 1988), and an emphasis on the coordination of services (Kanter, 1989). A number of integrated care projects demonstrated one or more of these additional features. For example, the ‘South Auckland chronic obstructive pulmonary disease project’ and the ‘Eldercare Canterbury community rehabilitation project’ both focused on rehabilitation and the coordination of services, and the ‘Supportive recreation project’ (Tairawhiti) focused on the development of an individual’s physical strength and social connectedness. The clinical case management model is the only model to have been used as an alternative to acute hospital admissions (Marshall et al., 1998) and there is mounting evidence that this model is more effective in this respect than the brokerage model (Thomas & Lovell, 1999). As integrated care projects sought to prevent avoidable hospitalisations the adoption of a clinical case management model was predictable. Integrated care also sought to coordinate services and whilst adopting the brokerage model to achieve this end relied more heavily upon partnership arrangements as the central vehicle for this activity. Integrated care projects engaged a multidisciplinary health professional workforce and interventions were often conducted in community facilities and client’s homes, similar 213 features to clinical case management in countries such as the United Kingdom (Marshall et al., 1998), with the most striking difference being the case loads of nurse case managers. Marshall et al. report case loads of 10 - 15 clients in the United Kingdom, whereas nurses studied in integrated care projects in New Zealand often held case loads well in excess of 15 clients, and sometimes reaching 80 or more clients. In these situations nurses delegated functions and supervised other nurses as a way of managing their work. 8.2.4.4 New coordination strategies An association was evidenced between projects employing nurses and the development of a new coordination strategy. New coordination strategies involved working in non-traditional ways with project partners, such as sports organisations, district councils and the housing sector. Intersectoral collaboration influenced a broader approach to health and new ways of coordinating and providing health interventions. For example, in one project nurses, plumbers and builders visited clients in rural and remote communities to provide health assessments, vaccinations, maintain sewerage systems, and repair, insulate and adapt homes to improve the quality of life for residents. 8.2.5 Level of population-based practice approach of projects A strong association was evidenced between projects that adopted an individual or a community level approach and projects that employed nurses. A lesser degree of association was evidenced between projects that adopted a systems approach and projects that employed nurses. The study demonstrated overall that exclusive individual, and individual and systems approaches were favoured over community approaches. An individual level of approach predominated in 72 per cent of the projects employing nurses, with an exclusive approach occurring in one quarter of these projects and a further 50 per cent adopted both individual and system approaches. A community approach in 214 combination with an individual, or individual and system approach, occurred in about a quarter of these projects. Projects employing nurses adopted community and systems approaches more often than projects without nurses. Strengthening community capacity and changing community norms, outcomes of community level interventions, are essential requirements of primary health care and nurses in projects contributed to the gradual development of a primary health care environment. Historically, person-to-person and individual-focused interventions have predominated in nursing with the prevailing role, the care of the sick in bed-based hospital institutions although important community roles have existed (PorterO'Grady, 1999). In New Zealand in the early 1900s for example, native health nurses worked in remote areas with Maori communities caring for individuals with typhoid and smallpox (see p. 73), shifting their focus a decade later to health promotion and disease prevention. An individual approach continued into the 1950s and through the 1970s, initially reinforced by the health system focus on hospital care and biomedicine and then as a consequence of the life-style era, which sought to persuade individuals to change their health-related behaviour (see p. 21). The life-style approach has been widely criticised for ignoring the lack of opportunities for disadvantaged people to be healthy (Crawford, 1977; J. French & Adams, 1986; Naidoo & Wills, 1994; Rodmell & Watt, 1986; Tesh, 1988). For this reason ‘new public health’ evolved advocating legislation and policy, intersectoral action, community participation and equity (Baum, 1998). Whilst this represented a different health promotion approach to that demonstrated in the life-style era, Green and Raeburn (1988) maintained that in practice both approaches were often adopted. The current study demonstrated this phenomenon when projects seeking to change the behaviour of individuals with conditions such as diabetes, chronic obstructive pulmonary disease and congestive heart failure, focused on interventions to change diets, stop smoking, and reduce blood pressure and cholesterol levels respectively. In addition, these projects undertook systems interventions, such as the establishment of ‘diabetes registers’, developed databases of people with chronic respiratory disease, and provided influenza vaccinations to those at risk of an exacerbation of this condition. 215 Community interventions in line with the increasing emphasis being placed on primary health care, which promotes community empowerment (Ministry of Health, 2001b; 2001c; 2003b), were undertaken less frequently. A community level approach was not undertaken by any project exclusively, however 16 per cent of projects adopted a community approach in combination with another level of approach and nurses were employed in all (100%) of these projects. Few projects demonstrated community participatory approaches designed to empower communities and support them to identify issues relevant to their lives. Laverack and Labonte (2000) maintain that if health planners viewed community empowerment as more than a means to achieve health behaviour change in top-down67 health promotion programmes, other important outcomes such as a community’s capacity to influence it’s health, might result. One project that adopted both community and individual levels of practice was directed at Maori women residing in a tribal region (rohe) who attended community events collectively where information, health teaching and diagnostic testing was available for cervical smears, breast examination and mammography. A second project adopted the same levels of approach targeting children and families at a community fair, providing information on dental health. Children and adults were offered free dental check ups in groups, with the nurse able to act as a broker for ongoing dental care. In both projects nurses were Maori, worked and lived in their tribal area, held cultural knowledge, encouraged clients to express their needs, and were known as advocates for Maori rights. Social justice through community empowerment and advocacy were familiar concepts to these nurses, suggesting confidence in a broader and more radical health promotion discourse compared to the discourse of the 1970s that emphasised disease prevention through life-style management (Feather & Labonte, 1995). Keller et al. (2004a) contend work with communities has equal if not more impact on improving population health than work with individuals and families. This is an area for future research, as the proportion of the community that may actually change from community population-based practice and the potential benefits from this approach has not yet been established. 67 Top-down programmes are conventional, solve a problem or deficit, focus on individual responsibility, are controlled by an outside agency, and have low community ownership (Laverack & Labonte, 2000). 216 Almost as many projects employing nurses adopted a systems level approach as adopted an individual level approach. However unlike the latter group, only 26 per cent adopted a systems approach exclusively, with most developing registers or databases to detail the health status of individuals with chronic conditions, or to record information such as immunisations for the purpose of sharing data across a provider network. This exclusive systems approach was consistent with the aim of integrated care to establish integrated networks (Health Funding Authority, 1998). Systems-focused practice has the potential to change organisations, policies, laws and power structures (Minnesota Department of Health, 2001). Over half of the systems level projects employing nurses were undertaken concurrently with individual level projects. Most of these projects established registers and databases to assist in the management of clients enrolled in disease state management programmes. Nurses began by seeking to involve targeted groups and individuals with chronic conditions in interventions largely defined by the project planners, who regarded improvement in specified behaviours as important health outcomes. Empowering individuals was viewed instrumentally, that is, as a means to the end of health behaviour change. Four projects employing nurses adopted community and system, or individual, community and system levels of approach. One multi-level project targeting chronic conditions involved the clinical case management of individuals, the establishment of regional registers and databases, advocacy for new marae-based services, and the detection of more cases within the community. Some nurses reported a tension between representing a community’s perspective and their inability to accommodate changes within the project. 8.2.6 Age group focus A strong association was evidenced between projects employing nurses and projects targeting children and adolescents, and adults. A lesser degree of association was found in projects targeting older adults, and people of all ages. Overall, fewer projects targeted children and adolescents compared with other age groups, however almost all of these projects (92%) employed nurses. Children and 217 adolescents were the group in which primary prevention was most apparent, despite the majority of these projects also demonstrating a disease or condition focus. For example, mouth guards were provided to children playing sport to prevent meningitis, and immunisation rates were improved in mobile populations through active casefinding by nurses. Both projects involved communities but did not adopt a negotiated approach that built on community strengths and capacities, a starting place for distal prevention. The project that developed an electronic information network, which held data on a large number of children for the purpose of managing morbidity relating to conditions such as asthma and rheumatic fever, has the potential to develop anti-poverty or housing development strategies. The ability to identify and tackle distal risks can yield fundamental and sustained improvements to future health status. In general, few projects included prevention strategies, and most focused on secondary rather than primary prevention. This is of concern as New Zealand has increasing problems with tobacco use (Peto et al., 1994) obesity and physical inactivity (Ministry of Health, 2003c, 2003d; Ministry of Social Development, 2004), and excessive alcohol use (Statistics New Zealand, 2004), all major risk factors for chronic conditions. Over a quarter of the projects targeted adults, with nurses employed in the majority (91%) of projects, which focused on conditions, such as diabetes, chronic obstructive pulmonary disease, and mental health. A similar percentage of projects targeted older people, yet nurses were employed in fewer of these projects (64%) proportionally. Of the 14 projects employing nurses that targeted older people, almost all adopted a disease or condition focus. The relationship between age group and disease or condition reflected the integrated care intention to make services for people with chronic disease more assessable (Health Funding Authority, 1998). A further intention to address health promotion and disease prevention was not met. All but one project focused on existing diseases, and even secondary prevention such as the maintenance of diabetic foot care was not included. It was anticipated that integrated care in New Zealand would develop to prevent risks to health and avoid future burdens of disease (Ovretveit, 1998). Latest population projections indicate the New Zealand elderly population will grow 150 per cent by 218 2051 (see p. 47). With an increase in the actual numbers of older people combined with populations throughout the world living longer, a dramatic rise in chronic conditions and associated disability is expected (World Health Organization, 2002a). Despite primary prevention being advocated over secondary prevention, few projects targeting older adults were focused on positive or well-health or on preventing or reducing risks. 8.2.7 Ethnic group focus A strong association was evidenced between projects employing nurses and projects targeting Maori and/or Pacific peoples. Over half of the projects targeted Maori and/or Pacific peoples exclusively or in combination with the wider population, and nurses were employed in 90 per cent of these projects. The study demonstrated nurses worked with different ethnic populations and commonly had a local knowledge of specific communities and families. The nursing profession has contributed to the promotion of ‘cultural safety’68. In the late 1980s changes to the education of nurses were made to support this concept. During the time of integrated care, attempts to integrate health promotion, community development, and primary health care into everyday practice assisted nurses to acquire skills to care for people in ways that respected their culture. Whilst information was not specifically collected on the ethnicity of nurses employed in integrated care projects, a number of nurses were known to self-identify as Maori, Samoan, Tongan, and Cook Island and commonly worked alongside and served people of the same ethnicity. When clinicians and patients are from the same cultural background there is greater likelihood of accurate diagnosis and compliance (Durie, 2004), an association likely to be influenced by shared cultural understandings and knowledge. 68 The New Zealand Nursing Council has defined cultural safety. Nursing Council states, “cultural safety relates to the experience of the recipient of nursing or midwifery service and extends beyond cultural awareness and cultural sensitivity” (Nursing Council of New Zealand, 2002, p. 7). 219 Improving Maori health was identified as a demonstration pilot hypothesis, and sought to test the contention that services by Maori for Maori would produce the best health outcomes (Health Funding Authority, 1998). Unfortunately, projects able to test this hypothesis were not selected as demonstration pilots and the opportunity to provide services by Maori for Maori was lost. If central to Maori health is Maori control (Durie, 1998), rangatiratanga or Maori ownership and decision making was not achieved through integrated care. Wano (2003) argues integrated care was never fully embraced because it was seen (within Maori) as another way of cutting costs and marginalising Maori. Ultimately, demonstration pilots and all other projects in the NICPS bore no resemblance to the initial strategy, which sought to experiment with cost, benefit, and risk arrangements. Similarly, guidelines for demonstration pilots identified Pacific peoples as a ‘health priority population’ (Health Funding Authority, 1998), a position the present New Zealand government recently restated (Ministry of Health, 2001c). However, integrated care projects targeting Pacific peoples, like Maori, focused on disease or condition management, rather than health more widely. Jansen (1998) argued this was because a narrow disease management approach could be assessed in relation to specified contract outcomes, and thereby limit financial risk to the provider organisation. Interestingly, of the 15 projects targeting prevention or promoting positive or wellhealth, 13 focused on Maori or Pacific peoples. Similarly, the coordinated care trials in Australia focused on people with common diseases and medical management, rather than prevention or health promotion, except for the Aboriginal trials (Baum, 1998). It is difficult to say with any certainty why projects with a positive or wellhealth focus occurred more frequently in Maori, Pacific and Aboriginal populations, though, one factor of influence may be a view of health by these populations that stresses the wider physical, social and spiritual environment (Durie, 1998; Saggers & Gray, 1991). The values of project partners influenced the design of projects, and as a general rule, projects targeting Maori and/or Pacific peoples were influenced by project partners from the same ethnic background. 220 8.2.8 Low income focus A strong association was evidenced between projects employing nurses and integrated care projects targeting populations in geographic areas defined as low decile and representing the 30 per cent of the most deprived areas in New Zealand. Of projects targeting these areas, chronic conditions were also a focus. This is not surprising as chronic conditions disproportionately affect the poor (World Health Organization, 2002a). Integrated care was intended to address the greatest and most serious health needs (Bringewatt, 1997; Ovretveit, 1998), so it is alarming that only 30 per cent of projects targeted people living in the most deprived areas in New Zealand, despite this being a priority criterion (Health Funding Authority, 1998). The strategy of integrated care failed to implement its goal of improving the health of the poor and underserved. Three generations of health care reforms have been motivated by a desire to improve the health of the poor and underserved. First generation reforms attempted to address inequalities in access to health care at a time when hospital care predominated (see p. 9). Second generation reforms introduced primary or basic health care to all people, which in poor countries was often considered primitive rather than primary. In New Zealand general practice provided primary care and relied upon medical interventions to gain health (Walsh & Warren, 1979), with the poor often getting less of the benefit than the rich (Gwatkin, 1998, as cited in World Health Organization, 2000). The technical, medical emphasis of primary care in New Zealand resulted in increased hospitalisations and services targeted to reach the poor were often used more by the rich due to the disproportionate use of hospital services by the well off. Public hospital waiting lists grew and medical insurance schemes evolved to help (rich) people pay for private hospital admissions (Boyd & Sheridan, 2000). First and second generation reforms failed to improve the health of the poor. Integrated care was located within the third generation of health reforms, coinciding with the philosophy of new public health that promoted policies on poverty and social justice. Third generation reforms responded more to demand by assuring access to services for the poor and emphasised financing rather than service provision. Integrated care planned to experiment with new ways to finance and deliver services 221 in the interests of addressing inequalities, such as access to services (Health Funding Authority, 1998). Unfortunately, project performance relied upon the standard goals, targets, and health outcome measures, familiar to both the health funder and providers in the measurement of disease management, and forced attention back on disease. Integrated care projects invested in general practice and its accompanying medical construct of health. This paradigm prevailed over broader primary health care services and more diverse social understandings of health. It is unfortunate that at a time when the World Health Organisation promoted equity in health care through intersectoral collaboration and community participation integrated care developed as an essentially reductionist strategy. Less than a third of projects targeted the poor, and in this respect as a third generation reform that sought to improve the health of the poor and underserved, integrated care had limited success. 8.2.9 Health, disease, condition or other focus A strong association was evidenced between projects employing nurses and projects targeting chronic conditions, other conditions, and well-health (see p. 183). A lesser degree of association was evidenced between projects employing nurses and projects targeting acute conditions. Half of the projects targeted chronic conditions, including seven of the nine national demonstration pilot projects. Nurses were employed in 90 per cent of the projects targeting chronic conditions and only in these projects were diabetes, two or more chronic conditions, mental health conditions, chronic obstructive pulmonary disease, cardiac conditions, asthma and other respiratory conditions managed. It is not surprising that integrated care emphasised chronic conditions and care pathways (Ovretveit, 1998) as pressure existed on the health system to find new ways to manage the escalation of chronic conditions that comprised the burden of illness in New Zealand (World Health Organization, 2002b). A primary health care approach was selectively applied to the management of specific diseases in these projects, narrowly focusing on medical care services and the 222 endeavours of health professionals, often nurses, to integrate such services. This is concerning because it is well-known that major health problems cannot be solved by medical care alone (Lalonde, 1974). Tarimo and Webster (1994) have suggested that a selective approach to primary health care usually means that while a particular problem may be resolved, it will be replaced by another problem as the underlying cause of ill health has not been dealt with. It is also commonly acknowledged that health care systems contribute to health status but are not the major factor in the determination of overall population health status. Rather, public health measures aimed at the prevention of disease, illness and disability, and lowering death rates are increasingly understood as more important in creating healthy populations (Frenk, 1994; Niessen, 2002). Beaglehole and Bonita (1997) argue that the integration of medical care under a public health umbrella would facilitate the process of setting broad health goals and targets and encourage resources to flow to prevention. Had integrated care projects been characterised by a comprehensive primary health care approach, rather than a selective approach, more sustainable health outcomes could have been expected. This raises the question of how well current public health knowledge was understood and utilised in the development of integrated care. Wells (1998) perceived integrated care as a key public sector reform strategy that would provide a solution to fragmented health care service provision. Integrated care was envisaged to include partnerships across the housing, employment and education sectors and to address inequality in relation to poverty when allocating health resources (Davies, 1999; Feek, 1998; Wells, 1998). These perspectives suggest integrated care was viewed as more than medical service provision for chronic conditions and implies a social and participatory approach to health, consistent with the philosophy of new public health (Baum, 1998). The New Zealand government has a central role in tackling major risks to reduce inequalities in society. While treating diseases and managing long-term health problems is essential, the health system is also challenged to address the underlying risks to health and adopt prevention and reduction strategies (World Health Organization, 2002b). It is therefore surprising that only 15 projects targeted 223 prevention and demonstrated a well-health focus. Nurses were employed in 87 per cent of these projects, two of which considered distal risks and centred on the broader dimensions of well-health through the promotion of exercise and improvements to housing. In both projects nurses facilitated either sports people developing sport and exercise programmes for youth or builders constructing ‘inside’ toilets, repairing drainage and sewerage systems, upgrading electrical wiring, and insulating dwellings for the poor. Maori health organisations were generally partners in the small number of projects that worked with organisations outside the health sector, and were instrumental in this happening. Nurses were employed in the majority of projects that undertook primary and secondary care, such as general health checks targeting whole populations - babies under 12 months, women, or Maori residing in a specific geographic area. Other activities included screening for hepatitis B or sexually transmitted infections in populations-at-risk, and smoking cessation programmes for people with smoking related illnesses. For individuals with a respiratory condition, such as chronic obstructive pulmonary disease, the smoking cessation programme attempted to prevent secondary complications, thereby maintaining the health of the ‘well-ill’ individual. Many nurses contributed to population health objectives through involvement in immunisation and smoking cessation programmes, but consistent with the literature, rarely participated in decisions about the distribution of resources and benefits accrued from meeting targets (Carryer, 2004). Acute conditions were targeted in ten per cent of projects and half of these projects employed nurses. The conditions targeted were disparate and included iron deficiency anaemia, bleeding in the first trimester of pregnancy, and dental health problems. All projects included Maori or Pacific project partners and nurses who emphasised prevention. In contrast, the projects that did not employ nurses focused on conditions requiring hospitalisation and medical technical support, such as acute confusion and hip fracture. This study finding is reminiscent of the primary health care approach in New Zealand during the second generation of reforms where medical technical practices predominated. 224 Nurses were employed in 90 per cent of the projects classified as ‘other’ (see p. 182). Most of these projects involved the development and implementation of health care guidelines and care pathways to assist client journeys through the health system, and memorandums of understanding or partnership protocols between organisations. The emphasis was placed more generally on developing a seamless system of care between services, with only a small number of projects selecting a specific condition, such as hip fracture or stroke, to demonstrate this approach. Ovretveit (1998) maintains care pathways benefit all individuals, and in particular the increasing number of individuals who experience acute exacerbations of a chronic condition over a longer term. Nurses were involved in establishing databases of clients in a regional area with, for example, chronic obstructive pulmonary disease or diabetes. The processes were active, ongoing and labour-intensive. The mobility of populations concerns over undiagnosed or inaccurately diagnosed conditions, and clinical management resulted in nurses undertaking this surveillance intervention for the purposes of case-finding and identifying levels of disease. Projects without nurses were principally involved in developing databases using a surveillance system that could be described as passive, with the collection of hospital discharge data comprising the main source. 8.2.10 Non-nursing personnel An association was evidenced between projects employing nurses and non-nursing personnel. Non-nursing personnel were employed in about 40 per cent of the projects and nurses were employed in 77 per cent of these projects. A higher percentage of non-nursing personnel were employed in projects that did not employ nurses. Many projects appeared to delineate between nurses roles and those of non-nursing personnel, and projects benefited from the employment of both. In other projects there were overlaps in the roles of nurses and non-nursing personnel and there was no clear reason for this overlap. Reception and administration, including service coordination, were the main roles undertaken by non-nursing personnel in projects without nurses. In a number of projects nurses undertook receptionist/administrative activities alongside, or in the absence of, non-nursing personnel. Practice nurses have 225 long been criticised for undertaking a receptionist role, rather than a clinical role in general practice (Docherty, 2004) and some nurses in integrated care projects would be subject to the same criticism. Non-nursing personnel conducted research and audits in projects and nurses were not engaged in these activities. In general, nurses engage in research utilisation, an essential activity for maintaining best practice, and a competency of the nurse practitioner scope of practice (Nursing Council of New Zealand, 2001b). Docherty (2004) argues that nursing has a responsibility to provide primary health care nursing research because it can influence a change in the current focus from ‘primary care’ to ‘primary health care’. In New Zealand these terms are often used interchangeably and cause confusion. Docherty believes there is a risk that research will continue to focus narrowly on primary (initial) care in for example the primary management of chronic conditions, rather than taking a wider view of health care that includes individual and community choice in an endeavour to sustain health and well-being. Primary health care may include primary care to address a problem, but the main goal is to build community capacity. Nursing research in primary health care can involve investigating the way health is determined through the exploration of social and economic factors. Interestingly, all research conducted by non-nursing personnel in the integrated care projects had a primary care focus, such as an audit of diabetes management, and a randomised controlled trial of chronic obstructive pulmonary disease case management. 226 8.3 Population-based interventions and levels of practice undertaken by nurses in integrated care projects What types of population-based interventions were undertaken by nurses in integrated care projects? This section systematically discusses the 17 types of interventions69 in the order they appear on the intervention wheel (see p. 89) beginning with surveillance, so that relationships between interventions comprising ‘wedges’ can be more easily shown. This order does not reflect the interventions most frequently undertaken by nurses in integrated care projects which were: case management; consulting; health teaching; collaboration; referral and follow-up; delegated functions; counselling; advocacy; coalition building; screening; policy development and enforcement; outreach; disease and health event investigation; community organising; social marketing, and surveillance (see p. 172, Figure 14). Nurses undertook nine or more types of intervention in almost half of the projects, but only one type of intervention was undertaken in the remaining 50 per cent of projects. What population-based levels of practice did nurses demonstrate in integrated care projects? Of a total 411 interventions undertaken by nurses, 66 per cent occurred exclusively at the individual level, 9 per cent at the community level and 8 per cent at the systems level. Less than a fifth of the total interventions were undertaken on either two or three levels concurrently (see p. 173, Figure 15). This section provides examples of interventions at differing practice levels70, offering deeper insights into nurses’ practice within the integrated care environment. Definitions of each intervention are not restated and can be found in Table 5 (see p. 95). 69 ‘Case-finding’, the seventeenth intervention is included within the interventions surveillance, disease and health event investigation, outreach, and screening at the individual level. 70 This refers only to interventions and practice levels undertaken by nurses in the NICPS, and excludes examples not undertaken, such as community and systems levels in referral and follow-up. 227 8.3.1 Intervention: Surveillance Surveillance was the only intervention undertaken almost entirely at the systemsfocused level of practice (see pp. 191-192, Figure 17). Surveillance collects and analyses data on health threats such as infectious diseases, but in projects was used most with other health events such as chronic diseases. Unlike ‘disease and health event investigation’ surveillance is ongoing, seeking to establish patterns and identify changes in the incidence and prevalence of disease (Minnesota Department of Health, 2001). Surveillance involved assessing health before and after health events, and whole populations were targeted (see examples following). Surveillance is different from monitoring and screening71. Individual example (Case-finding) Health provider organisations in a region forwarded information on their clients, Pacific children, who were scheduled to receive immunisations but could not be located. A project developed a Pacific nursing service that acted as a broker for other health providers, such as general practices. Nurses used their networks to locate families, conduct home visits to determine why the child had not been immunised and provide the immunisation if requested. Immunisations were registered at the local provider level and national level. Community example Nurses in a project that targeted chronic obstructive pulmonary disease management assessed the health status of a group of enrolled clients before and after a case management intervention. Clients initially completed a Short Form 36 (SF36), and Chronic Respiratory Questionnaire (CRQ), which was repeated again at 12 and 24 months. Any presenting issues were addressed. Systems example Nurses in a collaborative project with many partners used random sampling to survey the population of a geographic region to determine the prevalence of diabetes in order to establish baseline data. Existing data sources were reviewed, such as, hospital discharge data, medical management information, and other surveys. A regional register was developed for ongoing data collection of diabetes cases in this population. 8.3.2 Intervention: Disease and health event investigation Disease and health event investigation was undertaken approximately three-quarters of the time at the individual level (see pp. 190, 192, Figure 17). Traditionally, disease and health event investigation has focused on infectious diseases, however, study 71 Monitoring implies a constant adjustment of what is being done and looks at groups of individuals. Screening detects previously unknown cases in a population and may serve as the method to find cases (Minnesota Department of Health, 2001). 228 projects focused mainly on chronic conditions, injury, and other health events. This investigation identifies “cases, their contacts, and others at risk, determining control measures, and communicating with the public” (Minnesota Department of Health, 2001, p. 29). In the current study, investigation was a key component of surveillance, frequently leading to case-finding and referral and follow-up. However, investigation also stood alone when applied as a method for discovering new information. Individual example (Case-finding) Nurses initiated contact investigations of clients diagnosed with gonorrhoea, chlamydia, and other sexually transmitted diseases. The nurse made visits to people identified as sexual contacts, providing information and free primary care services. Community example Nurses were concerned with the assumed unmet health needs of children and their families with chronic and terminal conditions, so selected one District Health Board area and applied a profiling methodology to identify any existing need in this population. Unmet needs revealed by profiling resulted in specific interventions being made available to children and their families. A second profiling was planned to compare the quality of life of children and their families following interventions and to establish their satisfaction with services. Systems example Specialist nurses and physicians worked with primary care providers to establish a system of management for new cases of diabetes presenting with existing associated complications. The specialist team trained practice nurses and general practitioners in the region to manage ‘complex’ diabetes cases via case studies and conferences conducted in primary health care settings. 8.3.3 Intervention: Outreach Outreach was most frequently undertaken at the individual level with community level interventions also occurring in almost half of the projects (see p. 192, Figure 17). “Outreach success is determined by the proportion of those considered at risk who receive information and act on it” (Minnesota Department of Health, 2001, p. 41). Commonly outreach is undertaken with health teaching to inform those at risk, about the risk, and how to get attention. At the community level, outreach messages were often a precursor to screening, and disease and other health event investigation, operating like social marketing. 229 Individual example (Case-finding) A nurse conducted focus group interviews with Maori women concerned with the increasing incidence of breast cancer, which assisted in the identification of potential barriers to screening and revealed useful ways to encourage others to participate in screening programmes that were clinically and culturally safe. Community example Maori nurses provided information on the need for mammography screening to Maori women over 50 years of age at a marae-based hui (conference). Women were enrolled with a Maori provider and information was provided in te reo (Maori language) about the screening process, costs, and venues. Women were followed up and those who had been screened determined the success of the outreach message. Systems example A large project with multiple partners in west Auckland participated in the immunisation of children. Nurses convinced pharmacies, community day cares and other community facilities visited by children and their families to display information on immunisation, explaining how and where it could be accessed. Immunisations were then undertaken by nurses at home visits or at a community outreach well-child clinic. 8.3.4 Intervention: Screening Screening was most frequently undertaken at the individual practice level with community practice undertaken concurrently in about one third of the projects (see p. 192, Figure 17). Commonly, this intervention was preceded by outreach and social marketing. Screening often occurred simultaneously with health teaching, and/or counselling, and on several occasions transitioned into referral and follow-up for those requiring a further assessment of presenting symptoms. Individual example (Case-finding) An older man who had many family members with diabetes, presented to his lead primary health care provider for screening. The nurse performed urine and blood tests, and talked with the man about his understanding of diabetes. The nurse also undertook a comprehensive health assessment as a consequence of additional risk factors identified when taking his health history. Community example Nurses conducted general health checks at a community hall as a component of a collaborative project targeting older people at risk of common conditions, such as diabetes, cardiac and respiratory conditions. Nurses provided health teaching and counselling to all clients during the assessment, and then preceded to enroll clients with a health provider to ensure referrals and follow-ups would be undertaken. Systems example A rural community experienced an increase in the incidence (new cases) of diabetes. A project comprising partners from the key health provider network supported nurses to screen the general population in an attempt to identify cases, which were then referred on for follow-up. 230 8.3.5 Intervention: Referral and follow-up Referral and follow-up occurred in 30 projects at the individual practice level only. This intervention was always linked with another intervention, such as health teaching, counselling, delegated functions, consulting, screening, case finding (as related to surveillance, disease and health event investigation, or outreach), casemanagement or advocacy. Nurses were the recipients of referrals and also referred clients on, the latter function reflecting their knowledge of resources and linkages within communities. When involved in referral systems, nurses developed and implemented care pathways (see p. 192, Figure 17). As clients being case managed were followed up the success of the referral (and the system) was assessed. Individual example Nurses in a rural town clinically case managed clients with a diagnosis of congestive heart failure upon their discharge from hospital. Nurses conducted home visits to complete clinical assessments and provide health and social support, referring clients on to general practice physicians and other specialists when necessary, maintaining a central and ongoing role in case management. 8.3.6 Intervention: Case management In the study the model of case management depended upon the skills of clinicians and the ‘implementation’ context. For example, nurses focusing on chronic disease management were found to have adopted two case management models, one with a predominant focus on brokering needed services and the other on the provision of clinical care (see pp. 212-214). Both models included prevention goals, health teaching and counselling interventions, and considered the determinants that affected a client’s quality of life. These characteristics suggest that elements of a public health framework were embedded within case management models. This is not surprising as the purpose of integrated care with it’s emphasis on primary health care, was to improve the management of chronic conditions (Health Funding Authority, 1998). Case management was undertaken at the individual and systems practice levels (see p. 192, Figure 17). The majority of projects applied a clinical case management model focusing on individual clients with chronic conditions, such as diabetes (see p. 212). 231 Case-finding generally preceded case management, with health teaching, counselling, consultation, advocacy and collaboration commonly occurring in the process of case management. Individual example A general practice team comprising a practice nurse and general practice physician case managed the clinical care of a client with chronic obstructive pulmonary disease. Scheduled monthly visits were planned with the client to review their health status and revisit negotiated goals. Health teaching and counselling were features of the case management interactions, and a referral to a pulmonary rehabilitation programme was made and followed up. Systems example Nurses providing services to people with high needs and chronic conditions, such as chronic obstructive pulmonary disease, collaboratively developed a central pathway to simplify access to services for this population. 8.3.7 Intervention: Delegated functions Delegated functions occurred most often when nurses undertook tasks delegated by general practice physicians and hospital physicians, or when nurses with a specialist knowledge delegated tasks to other nurses. Delegated functions were undertaken at the individual level on all but one occasion (see p. 192, Figure 17). Critical decisions were made every time nurses delegated to others or accepted delegation, with nurses accountable for functions delegated by another nurse with the same licensure. Individual example A nurse undertook a comprehensive health assessment, which included the client’s clinical history, blood tests, spirometry, shuttle walk test, and administered the Chronic Respiratory Questionnaire. These functions were delegated by the general practice physician overseeing the client’s care. Community example Nurses administered immunisations to children in schools and other settings under standing orders issued by the New Zealand Ministry of Health. 8.3.8 Interventions: Health teaching Health teaching occurred at all levels, but overwhelmingly at the individual level (see pp. 189-190, Table 29; p. 192, Figure 17). Health teaching was undertaken more than any other intervention and occurred in conjunction with many other interventions, but 232 was most frequently implemented sequentially with counselling and consultation. This was because health teaching influenced the knowledge, beliefs, and behaviours of clients and systems, counselling focused on the emotional component of any necessary change, and consultation offered solutions to problems. It is not surprising that health teaching occurred in this context and the association between this intervention and others is consistent with the literature (Minnesota Department of Health, 2001). Individual example A nurse provided information and facilitated others providing education to 120 kuia (female elders), who attended a hui (conference) on ‘women’s health’. Topics requested for the day included menopause, nutrition, managing finance, and the dead (tu papaku), which included understanding the roles of the doctor, police, coroner and funeral director. Community example Nurses collaborated with others to reduce smoking in older adults. The project developed posters in te reo (Maori language), distributing them widely to sports clubs, marae, churches, bars and restaurants. Systems example Nurses case managing clients with mental health problems identified a need to advocate for their clients rights, concerned at the stigma associated with mental illness. Nurses collaborated with others in a campaign to reduce stigmatisation using the media (media advocacy). 8.3.9 Intervention: Counselling Counselling occurred most at the individual level, but also at the community level (see p. 192, Figure 17). This intervention sought to clarify issues, provide insight, and facilitate problem management. Tschudin (1995) suggests counselling attempts to help a person solve their problems through focusing on their feelings, and then on the meaning of those feelings. Individual example A nurse facilitated a support group for families with children who have chronic illnesses and disabilities. Health and social problems were discussed and potential solutions were explored in this supportive environment. Community example The nurse worked with project partners and the Asthma Society to raise awareness about asthma prevention. The goal was to raise community awareness about asthma and to change community acceptance of asthma as a condition that is ‘not serious’ to a realisation that asthma is a life threatening, preventable condition. Posters, local radio broadcasts, and articles in the newspaper, included peoples personal stories relating to asthma as part of a wider strategy to disseminate this message. 233 8.3.10 Intervention: Consultation Consultation occurred most frequently at the individual level, but also occurred at the community and systems levels (see p. 192, Figure 17). This intervention was almost always a component of case management, and often followed health teaching as a problem solving process. Consultation is the provision of advice to others (Puetz & Shinn, 1997), and nurses fulfilled multiple roles when consulting within projects. The variety of roles included advocate, joint problem-solver, identifier of alternatives and linker to resources, process consultant, information specialist (Ulschak & SnowAntle, 1990), coach, motivator, mentor, teacher, facilitator, confidant, sounding board, change agent, fact-finder, expert, observer, and counsellor (Puetz & Shinn, 1997). Individual example A client who had suffered a stroke and lived alone, wanted to return home. The nurse discussed with the client his needs, the options available, and together they identified financial issues before planning an ‘assisted’ rehabilitation programme that could be undertaken at home. Community example An advisory group that included nurses provided expert advice to health professionals, providers, and clients in a specific region around promoting the rehabilitation and recovery of people who had recently experienced a stroke. Systems example Concerned about the rapid growth of a region and the settlement of new populations to the area, nurses, other health professionals, and district councillors, worked on a health plan that proposed types and locations of future health care services, and identified wider social and environmental health issues. 8.3.11 Intervention: Collaboration Collaboration occurred at all levels, but most frequently at the individual level (see p. 192, Figure 17). Even though collaboration, empowerment and partnering are overlapping concepts, the intervention collaboration is distinguished by the potential of transformation for both the nurse and client, which is attributed only to the client in empowerment and partnering (Minnesota Department of Health, 2001). 234 Individual example Over a two year period a nurse began to develop a relationship with a Maori client who had renal failure. Through her interactions with the client, the nurse stated she better understood the client’s values and practices and this had helped her to reassess and clarify her own practice and values. Community example Nurses collaborated with women’s groups, such as the Maori Women’s Welfare League and developed strategies to assist women to care for themselves, such as having a cervical smear test or undertaking a smoking cessation programme, and in doing so strengthened their families. Systems example A nurse clinically case managing clients with mental health problems became concerned that clients were being evicted for unpaid housing rents during episodes of acute illness. The nurse and her manager met with key decision-makers in the housing sector and negotiated to act as broker on behalf of clients’ to ensure rents were paid. This changed the way nurses had traditionally case managed clients and extended the model to include housing and attempt more holistic primary health care. 8.3.12 Intervention: Coalition building Coalition building occurred most at the community level, but also at the systems level (see pp. 190-191, Table 31; p. 192, Figure 17). Coalition building, like community organising is an example of collective action, and empowerment, the process through which individuals and communities take control of their lives and environment. Coalition building can be brought about by organisations outside the community, unlike community organising. Because coalition building does not require enhancing the capacity of other organisations within the coalition, in this respect it is dissimilar to collaboration (Minnesota Department of Health, 2001). Study projects considered the impacts on partners, and focused on capacity building in the primary sector. This intervention frequently resulted in nurses advocating for clients as groups at the community level. Community example Nurses facilitated the development of a ‘parent’ coalition that influenced the approach to care and the provision of services in the home for children with chronic illnesses and disabilities, creating a greater awareness of the problems faced daily by children, families and carers. Systems example In a large region with a rapidly growing population comprising many young families, a coalition of community organisations and individuals invited nurses from health organisations to assist in the development of a plan for future community health and social services. 235 8.3.13 Intervention: Community organising Community organising occurred only at the community level (see p. 190, Table 30; p. 192, Figure 17). Community organising used social marketing in a number of situations as a companion intervention to change the health behaviour of a population. This intervention can also potentially be “implemented in conjunction with the policy development intervention…when the organizing intent is to change policy at the systems level” (Minnesota Department of Health, 2001, p. 237). In the current study, however, community organising did not occur at the systems level. Community example A nurse facilitated a new approach to the annual review of diabetes by bringing together health professionals, people with diabetes and their families, and the interested public. In a community centre health assessments, including diagnostic tests such as retinal screening, were performed at no cost to clients. A podiatrist provided services, and a cooking demonstration and ‘tasting’ was conducted to encourage those with diabetes to consider new approaches to food. 8.3.14 Intervention: Advocacy Advocacy occurred most at the individual and community levels and less frequently at the systems level (see p. 192, Figure 17). Advocacy was explicit in case management, when nurses acted in the interests of clients’ concerned with rights and entitlements. Communication and negotiation skills were required when advocacy was associated with referral and follow-up, community organising, policy development and enforcement, and social marketing. In the process of advocating for clients, a number of nurses encouraged clients to begin to assume this role for themselves. 236 Individual example A nurse case managing a client with mental health problems discussed with the client their skills and deficits, such as poor literacy, in order to provide assistance with employment. Having been told by the client about preferred employment activities, the nurse negotiated with potential employers on the client’s behalf. Upon gaining employment, the nurse continued to advocate for the client, whilst also assisting the client to assume this role for themselves. Community example Nurses were concerned at the number of teeth extractions of very young children, adolescences, and adults in a rural area with poor access to dental health services. A clinic was set up on the local marae and dental health checks were performed at no cost to clients. Those needing further care were referred to dentists and actively followed-up by nurses to ensure barriers, such as cost or access did not prevent treatment being undertaken. Systems example Nurses participated in coalition building to bring together health professionals and organisations concerned with the fragmented care people with chronic conditions often experienced. Collectively they advocated for more seamless and comprehensive care, presenting to the Health Funding Authority a new case management strategy for people with chronic obstructive pulmonary disease. Clinicians, particularly nurses, were involved in media advocacy and the project received national funding. 8.3.15 Intervention: Social marketing Social marketing occurred most often at the individual level, but also at the community level (see p. 192, Figure 17), and like health teaching sought to change attitudes and behaviours. Social marketing has been described as a particular application of health teaching (Minnesota Department of Health, 2001). At the individual level nurses framed information in a way that was congruent with clients’ values. Andreasen (1995) argued that measures taken to change behaviour must consider demography and culture, as behaviours are learnt within family and social environments. Processes that are empowering and culturally sensitive were also advocated. Individual example During a general health screen a man who was hypertensive, obese, and smoked heavily told the nurse he had thought about joining a gym but had not because he was embarrassed about his weight and lack of fitness. The nurse described a local walking group for people with varying health issues who met daily. The client joined the group, was monitored regularly, lost weight and eventually chose to stop smoking. Community example Nurses working in a rural area developed a communication plan with other health providers to disseminate information on how to ‘live with diabetes’ in te reo (Maori language) via a local community radio station. Community members with diabetes were interviewed about their lives, the difficulties they experienced and the ways they coped with problems. In the weeks after the interview series, local nurses and doctors reported an increase in the number of consultations about diabetes management and health promotion. 237 8.3.16 Intervention: Policy development and enforcement Policy development and enforcement occurred most at the individual level, but also at the community level (see p. 192, Figure 17). Nurses influenced local policy by developing regulations, mandates, guidelines, care pathways, and other resources to guide client care practices. Nurses involved in policy development also often enforced or implemented the policy. National policies were enforced by nurses in the interests of standardising processes in either the treatment or care pathway of clients with a specific condition. Broader ‘healthy public policies’ were not developed but rather enforced by nurses in projects (see community example). Individual example A nurse developed a primary health care pathway for clients who had recently suffered a stroke and were returning home after hospitalisation. The nurse provided clients and their families with information and a guide to the health and social services available, which included speech therapy, physiotherapy, carer assistance, pharmacy, general practice advice, and welfare assistance. Community example A nurse investigated a public health concern raised by a kuia (female elder) about the quality of the drinking water at a local kohanga reo (early childhood centre with a focus on Maori language and culture) in a rural area. The water tank supplying the kohanga reo was tested and giardia was identified. The nurse successfully worked with the health protection unit to get the tank emptied, water blasted, re-filled and re-tested, before following up known or suspected cases of giardia. 8.4 What underlying values are made explicit when interventions undertaken by nurses are analysed? The health promotion values embedded in 14 interventions overall demonstrated an individually oriented philosophy. Nine interventions reflected the values of health persuasion - paternalism, authoritarianism, and prescription, and five interventions, the values of personal counselling - self-empowerment and negotiation. Two interventions, namely coalition building and community organising, demonstrated a collective oriented philosophy. Coalition building reflected the values of legislative action, paternalism and state-directed authoritarianism. However, like community organising, this intervention also reflected the values of community development, namely participation, negotiation, and empowerment. 238 8.4.1 Beattie’s model of health promotion Beattie’s model of health promotion (see p. 30, section 2.3) provides an environmental-political framework for analysing the health promotion values embedded within the overall practice of nurses employed in the 80 integrated care projects. By situating 17 interventions by nurses within the model, each reflecting a dominant focus72, particular health promotion values were identified. The mapping of interventions in this way demonstrated the ethical and political tensions faced by nurses in the projects studied. Stewart and Thomas (2004) suggest Beattie’s model can show partnership with government in legislation and policy, and with individuals and communities also taking an active role. Consistent with this finding, the current study demonstrated both individual and community partnerships and revealed that nurses invested most in individual partnerships. Section 8.4 analyses the interventions undertaken by nurses in light of the four health promotion strategies - health persuasion, personal counselling, legislative action, and community development. Following this, the prevailing mode (authoritative/ negotiating) and focus (individual/collective) of each intervention is attributed. This is determined by the way interventions are made operational by nurses in projects (see p. 160, section 6.4.5.2). Finally, new knowledge and the challenge this poses to future primary health care nursing practice is summarised. 8.4.2 The four approaches to Beattie’s model The majority of interventions undertaken by nurses in integrated care projects reflect the strategy of health persuasion. Case management, referral and follow-up, health teaching, delegated functions, screening, policy development and enforcement, disease and health event investigation, surveillance and social marketing, all reflected the social values within health persuasion, which are based on a bio-pathological model of health that views health promotion as attempting to repair weaknesses and deficits (Beattie, 1991). Health persuasion, a strategy led by professionals and in this 72 These 17 types of interventions are derived from the total (n=411) interventions undertaken by nurses in projects. 239 case nurses, has been described as paternalistic and favouring a culture of ‘victim blaming’ (Crawford, 1977). Dealing with risk factors to health, the limited effectiveness of health persuasion as a single strategy has been well documented (Beattie, 1991). Whilst nurses in projects clearly favoured this traditional strategy, they also frequently used it in conjunction with other strategies. The health promotion value of autonomy was demonstrated in five interventions, namely consultation, counselling, advocacy, collaboration and outreach, which relate to the strategy of personal counselling. Personal counselling is client-led, often centres on personal development, and requires the health professional to act as a facilitator rather than an expert. The central precept in personal counselling is selfempowerment and the client-orientation of the process is valued by its proponents (C. Rogers, 1969). The study demonstrated that nurses undertook ‘counselling’ to facilitate problem solving, ‘consultation’ to identify alternatives or link to resources, and ‘advocacy’ to negotiate issues the client wished to address. In all of these interventions nurses identified the importance of the clients’ participatory role and the creation of autonomy through enabling clients to make their own choices. Coalition building was the only intervention to reflect the values within the strategy of legislative action, which directs behaviour towards achieving health at a macro-level, using top-down processes. Led by health professionals, this strategy seeks to protect communities (Beattie, 1991). Coalition building, an intervention of collective action73, was bought about through legislative action and community development, the former strategy directed by the government’s integrated care policy, which required projects to build partnerships, a role nurses were active in (see pp. 178-179). Coalition building was further mandated at the organisational level by local policies such as partnership charters, memorandums of understanding, and joint venture contracts, established within projects to govern the type of partnership arrangement. Two interventions, community organising and coalition building74 reflected the values within the strategy of community development, which enhances the skills of a group 73 Coalition building is only ever undertaken at community and systems levels (see p. 94). Coalition building overall reflected equally both the social values of legislative action and community development (see p. 194, Figure 18). 74 240 or community to work together to change the environment using bottom-up processes. The World Health Organization (1986) contended that health developments in communities should not only be developed for the people, but rather by the people. In general, nurses in the study undertaking community organising and coalition building facilitated groups coming together, linked the group with key people who could assist the project, and acted more widely as a resource. Chaplin and Adams (1986) confirm these are usual functions for health workers in community development. 8.4.2.1 Authoritative or negotiated modes of interventions Beattie, among others, has shown how ‘top down and bottom up’ health interventions come to be polarised by varying degrees at opposite ends of the authority-negotiation continuum (Beattie, 1986, 1991; Hardy, 1981). Ten interventions undertaken by nurses were situated in the health persuasion and legislative action quadrants suggesting they were imposed by institutions of authority, namely nurses, other health professionals, project planners, and government agents. Authoritative modes of intervention are top-down, which implies they promote individual or community responsibility, start with problems defined by health educators, clinicians and policy makers, and focus on education, improved services, and life-style (Laverack & Labonte, 2000). Seven interventions situated in the personal counselling and community development quadrants were negotiated from within the affected communities concerned. Negotiated modes of intervention are bottom-up, which implies they enable individuals and can promote empowerment, starting with health priorities defined by either individuals or communities, and in the case of communities build on community control, resources and capabilities towards economic, social and political change (Laverack & Labonte, 2000). 241 8.4.2.2 Individual and collective focus of interventions The individual/collective dimension is one of the most stable and enduring axes of conflict in social theory and social policy (Taylor-Gooby & Dale, 1981). Nursing has traditionally emphasised the care of individuals who are experiencing illness or some condition viewed as a deficit that requires medical interventions (Porter-O'Grady, 1999). The study revealed that fifteen75 interventions undertaken by nurses demonstrated an individual focus and only two interventions a collective focus. The overwhelming individual focus of nurses’ practice, with the particular emphasis on the use of a health persuasion strategy, suggests that contemporary practice is still grounded in individualism, paternalism, authoritarianism and prescription. Authoritarianism and individualism dominated political agendas in the 1980s. This orientation was challenged as leading to victim blaming and strategies that failed to address the root causes of ill health. The challenge contributed to the emergence of the community health movement and empowerment as a central concept (Beattie, 1991). The study showed that the maintenance of an individual focus perpetuated an approach that had proved inadequate in addressing the inequalities known to contribute to poor health (K. Tones et al., 1990). If interventions undertaken by nurses had sought to reduce inequalities a focus on the causes of ill health, such as housing, would have been more widely apparent. Instead the focus remained on individuals and changing behaviour, demonstrating no real capability to address the determinants of poor health. The skills required by nurses to practice using a collective orientation were rarely evidenced in integrated care projects. 8.4.2.3 The challenge for nursing In general, nurses exerted power over individuals and communities through top down approaches to interventions. Individualism dominated. Although health promotion 75 Case management is included within the sum of fifteen. 242 practice involving communities was undertaken, community control of resources and community ownership was minimal. This was because integrated care policy had been determined nationally; project funding was primarily approved by government, and the condition of partnering with clients including communities, was imposed. Coalition building demonstrated a convergence of approaches between those developed by project planners with authority influenced by national policy and those emerging in communities. Unsurprisingly, intersectoral collaboration a feature of coalition building often resulted in opposing and competing viewpoints, which in a number of projects restricted development. Coalition building, like community organising also reflected a negotiated approach, however nurses always had a predetermined agenda and were more interested in gaining community involvement (see p. 36, section 2.3.4) than in empowering communities. Communities were not enabled in ways that encouraged building capacity or improving competence, metaphors of empowerment. In general, nurses in projects did not appear to have an understanding of how community empowerment could be practically accommodated within projects. Laverack and Labonte (2000) suggest community empowerment goals must be developed alongside typical approaches to programming for a systematic change in practice to occur, and this was not observed in these projects. Care of the individual is a legitimate practice focus for nurses and when undertaken in conjunction with interventions that maintain a community focus, has the potential to address inequalities in health (Ministry of Health, 2001c). Nurses in projects undertook individual and community interventions, but only in a limited number of projects. Interestingly, a sequential effect between several interventions where progress in one area facilitated progress in another was evidenced in projects. For example nurses’ success in collaboration with clients and health providers at the individual level influenced coalition building (see section 8.3.11 intervention: collaboration, systems example). In this sense interventions at differing levels of practice were often complementary, a highly positive outcome. Insights into the health promotion values embedded within nurses’ practice have proved valuable in revealing the width of the gap between the ideal of integrated care 243 and primary health care and the actuality of practice. The context within which nurses currently work is conventional or top down, retains an individual-focus, and relates to disease management and prevention. Moving from this traditional authoritative position to a more negotiated position that promotes community participation and empowerment raises the prospect of new solutions to relevant, complex health and social issues. Section 8.5 proposes a model to guide primary health care nursing practice76 transition from individual level practice to increase the commitment to practice at the community and systems levels. The framework will assist nurses to reflect upon the interventions, associated population-based levels of practice, and distinct health promotion values embedded within that practice. In this way nurses can evaluate their current practice in relation to achieving primary health care outcomes and decide the focus and direction for structuring future practice. 8.5 Study findings provide new insights and direction The study demonstrated that PHC nursing as undertaken by nurses in integrated care projects, could not address the inequalities in health care provision experienced by underserved populations, principally because of its central reliance upon individuallyfocused population-based practice. There is wide recognition of the need to address health determinants, and consensus this is to be undertaken by nurses and other health professionals in partnership with consumers (Ministry of Health, 2001c). Nurses in the study negotiated health care interventions with individual clients, however when the client was the group or collective, notably fewer interventions were evidenced suggesting this focus was less important or practitioners did not have the required skills to practice at this level. Over several years, national strategies and international frameworks have directed attention towards working with communities and advocated the inclusion of community-focused population-based practice (Beattie, 1991; Ministry of Health, 76 Health workers other than nurses can use the model as a framework for reflecting upon, and reorienting practice. 244 2001b, 2001c, 2003b; Minnesota Department of Health, 2001). Translating overarching strategic directions into primary health care practice is an important function of the nursing profession. Recent scholarships available for the postgraduate education of primary health care nurses represented an attempt at strengthening this workforce (Ministry of Health, 2003a, 2005). However, there has not been nationally agreed core knowledge of primary health care, so it cannot be assumed that community-focused population-based practice is a feature of this education. The challenge for nursing is to understand and accept the reality that current practice defined as ‘primary health care’, which it is suggested is akin to that of nurses studied in integrated care projects, is predominantly authoritative and individually-focused. A shift is needed from health persuasion to community development, and the values associated with the strategy of community development must be embedded within nurses’ practice if primary health care is to be achieved. At the individual-focused practice level a negotiated approach results in improved health outcomes (Beattie, 1991), but even this approach, which shifts away from an authoritative position is limited. Nursing must take a collective, negotiated approach placing a greater emphasis on supporting communities to build control, resources, and capacities (see pp. 34-36, section 2.3.4) if the goal is to improve the overall health of the population. Study findings provide the basis for advocating this ideological position which is articulated in the design of a new model that brings together current public health ideas, placing an emphasis on the values intrinsic to health promotion and its central strategy ‘primary health care’ (see p. 249). Termed the ‘Primary Health Care Interventions Model’ (PHCI model), this framework can assist New Zealand nurses evaluate their practice, and implement interventions in ways that enable more comprehensive primary health care practice in the future. 8.6 The Primary Health Care Interventions Model The PHCI model was developed as a response to the current study findings and reviewed literature, most importantly the Intervention Wheel (Keller et al., 1998) and Beattie’s model of health promotion practice (Beattie, 1991). The purpose of the 245 model is to demonstrate the links between values and interventions thereby assisting nurses to reflect upon their actual practice and intrinsic values. The model allows for insights at a personal level, necessary for any practitioner contemplating practice development in primary health care. The range of interventions includes all the activities of primary health care nurses’ practice, and the framework is a guide for action as well as a tool for reflection. The profession can apply the model to the analysis of overall PHC nursing practice data to guide action about the development of this specialty. New Zealand nurses have often experienced tensions in practice that surround how to include the concerns and issues of community in top down practice approaches, such as those characteristic of the majority of integrated care projects. Laverack and Labonte (2000) contend “the dichotomy between top down disease prevention and life-style change and bottom up community empowerment approaches is not as fixed as it is sometimes portrayed” (p. 256), or as exclusive, and that community empowerment goals can be accommodated within usual approaches to practice. For nurses, who are grappling with how to implement primary health care practice, the PHCI model can describe a vision of health promotion practice not yet in operation. In this sense, theory may advance practice through critical reflection of existing practice and values, and engage nurses in the act of planning new practice, which leads towards more certain ends. The PHCI model comprises elements from the Intervention Wheel (Keller et al., 1998), defining a comprehensive set of interventions and three levels of populationbased practice, which have intrinsic values related to population-based practice and public health nursing. These elements form the foundation of the PHCI model and have been adapted to explicitly identify Beattie’s theory of health promotion. Future adaptations to the model may include new primary health care interventions as they are identified. The PHCI model also identifies changes in societal values because like Beattie’s model of health promotion, it is embedded in wider social and cultural practices, in ideologies and political struggles (see p. 30). The model has the ability to run in parallel with other frameworks, such as ‘Whare Tapa Wha’, a contemporary model that expresses a Maori perspective of health (Durie, 1998) or ‘empowerment 246 tracks’ that can systematically accommodate community empowerment goals within usual approaches to projects (Laverack & Labonte, 2000). The PHCI model was adapted as an instrument to guide the implementation of New Zealand primary health care nursing practice, although the model is not exclusive to nursing and can be used by other disciplines. Situating the framework within a pikopiko frond, the native fern, is an expression of growth and renewal, in this case symbolising a new framework created from the rejuvenation of two well-established models. The model integrates four separate components: 1. The population-basis of all public health/health promotion interventions 2. Three levels of public health/health promotion practice: Community Systems Individual and family 3. The 17 public health/health promotion interventions Surveillance Disease and health event investigation Outreach Screening Case-finding Referral and follow-up Case management Delegated functions Health teaching Counselling Consultation Collaboration Coalition building Community organising 247 Advocacy Social marketing Policy development and enforcement 4. The four public health/health promotion strategies Health persuasion Personal counselling Legislative action Community development The model comprises an outer ring of 16 interventions, with the 17th intervention case finding, occurring only at an individually-focused level of practice in surveillance, disease and health event investigation, outreach, and screening. For this reason the label case-finding is not apparent in the model, whilst the intervention itself is represented within the four interventions listed previously. The three inner rings indicate distinct levels of population-based practice labelled ‘systems-focused’, ‘community-focused’, and ‘individual-focused’. These components, based upon the Intervention Wheel (Keller et al., 1998) correspond to each of the 17 interventions in the PHCI model’s ‘spoke-less or disc wheel’, and similarly can be undertaken at all three population-based levels of practice. The PHCI model embodies the same population-based concepts as the Intervention Wheel (Minnesota Department of Health, 2001). 248 y Policpment Survei llanc o l e e He Devforcement a n E Dislth E l & a I nv ci g es eas ve tig e nt So etin k at ar io F O S C M M U E SE T O h He a t M an Cas ag e em en t Re ferr Foll al & ow-up ng lli L g eenin nity Develop m en A lative ction s i eg Scr mu n tio ra bo lla Co C om on Coaliti ng Buildi SED CU O nal Counse o Com munity Orga nizing INDIVI ersu DU P h as t l C NITY-FOCUS U M ED OM C / FAMILYL A on Pers F i ac re ut Ad vo c D n ac y S SY on su lt a tio n Co u nsellin g Health g n Teachi ed a t ns g le o De nct i Fu Primary Health Care Interventions Model From "Population-Based Public Health Nursing Interventions: A Model from Practice," by L. Keller, S. Strohschein, B. Lia-Hoagberg, and M. Schaffer, 1998, Public Health Nursing, 15, p. 208. Copyright 1998 by Blackwell Science Incorporated. Adapted with permission of the author. From "Knowledge and Control in Health Promotion: A Test Case for Social Policy and Social Theory," by A. Beattie, 1991, in J. Cabe, M.Calnan, and M. Bury (Eds.), The Sociology of the Health Service, p. 167. Copyright 1991 by Routledge. Adapted with permission of the author. Within the two most inner rings, the four health promotion strategies, components from Beattie’s model of health promotion (Beattie, 1991) are situated. Health persuasion and personal counselling are situated in the ‘individual-focused’ ring as they represent strategies focused on individuals, the former utilising an authoritative mode of intervention, and the latter a negotiated mode. Legislative action and community development, situated in the ‘community-focused’ ring represent strategies focused on communities or groups, the former utilising an authoritative mode of intervention, and the latter a negotiated mode. At a systems-focused level of practice, all four strategies of health promotion are relevant. The specific formulae developed for analysing the values embedded in nurses’ practice in integrated care projects (see p. 161) linked systems-focused practice with individuals. In other contexts however, a link between systems-focused practice and communities exclusively, or in combination with individuals would require the formulae to be adapted as discussed under study limitations (see section 9.2.5.2). It was decided to refrain from situating the four strategies on the system-focused ring because, for the purpose of assigning overall values to practice, systems-focused practice was aligned with either individuals or communities and it appeared to make the model unnecessarily complex. Further, as Beattie’s four strategies (see p. 32-36) embody distinct modes and focuses of interventions, these labels were not included in the PHCI model. 8.6.1 Strengths of the PHCI model Beattie’s model has limitations for those who want to take action (Beattie, 1991). In the PHCI model, however, this is not a limiting factor because the incorporation of interventions and levels of practice provide a clear guide to the type of activities and embedded values that distinguish the different approaches to advancing primary health care practice. For example, interventions located in the community development quadrant are related to concepts of empowerment, equity, and the mobilisation of communities to effect change (see section 234). Therefore, if nurses select to reorient their practice in line with these values, interventions will need to be undertaken at community and systems levels, in addition to the individual level. 250 Beattie’s environmental-political model is characterised by content rather than by processes or objectives. This has implications when seeking to understand information, for example, if interventions overlap quadrants the model may not allow an adequate interpretation of new formulations (Beattie, 1991). The PHCI model however captures descriptions of interventions allowing for the provision of more detail, which enables greater depth and clarity in the analysis. The PHCI model has the ability to assess interventions and values to assist nurses and others tease out some of the complexities underlying health action. Chapter nine concludes the thesis by identifying the implications of the PHCI model for future primary health care nursing practice and offers recommendations for stakeholders in advocating acceptance of the model. 251 9 9.1 Chapter 9 Conclusion: Mapping a new future Introduction The purpose of this thesis was to discover the practice of nurses within the context of integrated care projects implemented in the late 1990s. Integrated care projects intended to experiment with different methods and types of health care organisation in an attempt to better coordinating care, whilst also focusing on positive economic outcomes (Ovretveit, 1998). The NICPS found that nurses employed in projects focused most of their practice at the individual-level. Population-based individualfocused practice cannot address inequalities in health care alone. Community and systems-focused approaches are also required if improvements are to be seen in the health of the population. The use of health promotion theory in the analysis of nurses’ practice has led to the further proposition that expanding nurses’ practice to include a focus on collective groups or communities will require the adoption of health promotion values consistent with such an approach. Consequently, the PHCI model (see p. 249) was developed to assist nurses to transition their practice from an individual-level to include a greater focus on communities and community-focused population-based practice. This final chapter outlines the strengths and limitations of the study methods before discussing in section 9.3 the implications of accepting the PHCI model as a platform for practical action - a framework to advance future primary health care nursing practice. Section 9.4 offers recommendations as a means for progressing nursing practice. Recommendations are directed at six stakeholder groups who have varying roles in advocating for the acceptance of the PHCI model. Finally, summary comments are proffered in conclusion. 252 9.2 Strengths and limitations of the study The discussion of the strengths and limitations of the current study is organised under the following headings: study design; study population; questionnaire design; data collection procedures and data analysis procedures. 9.2.1 Study design The cross-sectional survey design was considered an appropriate methodology for investigating the practice of nurses in integrated care projects because it allowed a quantitative description of project characteristics (see p. 129). The current study has the ability to describe what existed, the frequency of occurrences, and to categorise information. Survey data derived from interviews on 80 integrated care projects were reduced numerically, allowing broader concepts to be tested by the research questions. The effect of reducing the perceptions of respondents to a set of numbers, a method also used in randomised controlled trials, has been criticised for over simplifying information in line with the positivistic conventions of an established (quantitative) agenda (Oakley, 1981). Whilst this perspective is not uncommon among qualitative researchers, synthesising data enabled a macro-perspective to be gained, which was a central purpose of the study. The survey also employed detailed categorisation and coding processes to ensure the quality of data were maintained (see pp. 147-158, section 6.4.4). As a strategy of inquiry, surveys have been criticised because they do not have the same power as laboratory experiments to establish causality. However, surveys were developed for a different purpose, as a precise means of measuring social phenomenon (Creswell, 2003), with the ability to identify associations between variables such as organisation, and consequently produce useful descriptive data. Unlike an experiment the researcher does not control the environment, therefore each respondent answers in different circumstances bringing to the study a diverse set of assumptions, history and values. 253 It has been argued that aggregation77 of data from surveys means making assumptions that might not be justified. This is because a particular variable is rarely considered in the context of the respondent’s wider set of ideas and values (Oakley, 1981). In the current study, interviewees shared many common features, such as, significant health sector knowledge; work in integrated care, and a high level of interest in the research subject. In addition, the survey questions were pilot-tested on a comparable health professional audience to find out if they were well understood and to ensure that the answers would provide meaningful information (see pp. 141-142, section 6.4.3.3). The descriptive survey has the ability to identify a sample and generalise to a population, but does not seek to test the impact of a treatment or intervention on an outcome, as in an experiment (Keppel, 1991). Theoretically, the current study findings about the practice of nurses in projects can be extrapolated to a wider primary health care nursing population. The interventions and levels of practice undertaken by nurses in projects occurred during a particular health reform, which the author argues was a starting place for more recent primary health care activity. Therefore, when reviewing the study findings, and disseminating to a wider primary health care nursing audience, consideration must be in the context of more recent developments in the field. Both nursing and health care policy has moved on since integrated care. For example, nursing policy led to the development of scholarships for primary health care nursing education, and pilot innovation nursing projects, and health care policy has continued to assist the maturation of PHOs. An investment in policy implementation is most notable in these areas. Of these, education provides the most likely opportunity for developing the health promotion values and philosophy that are necessary for the adoption of communityfocused practice. At present despite the availability of postgraduate nursing education, there is little evidence to demonstrate that current programmes are influencing a shift from conventional individual-focused practice to include a community-focused approach. As a consequence, the researcher has confidence in generalising the study findings to primary health care nurses more broadly. A paucity of research on the health promotion values within nursing practice is acknowledged, 77 Aggregation assumes that words have uniform and agreed meanings that are not contingent upon their context. 254 as most research on primary health care nursing has focused on the activities of nurses in different environments (Ministry of Health, 2003b) and not on the underpinning values, beliefs and culture of the nursing groups who now comprise the new primary health care nursing workforce. The NICPS, despite the use of a robust research methodology, can only draw tentative conclusions. Future research is needed to demonstrate the level of consistency of these findings. 9.2.2 Study population The unit of inquiry was the integrated care project, with projects eligible for inclusion in the study if they met the established criteria (see pp. 133-134, section 6.4.11). The non-probability sampling method employed by the study did not guarantee that all eligible projects had an equal chance of being included in the sample78, although all eligible projects were rigorously followed up. The snowballing technique used to identify projects also risked selection bias. However, as a complete list of projects was unavailable, this method was the most suitable. The issue of bias by recall can be a feature of any research that asks respondents to provide information retrospectively. In the current study the respondents were identified as having a professional knowledge of integrated care developments, and because the information sought was recent, the margin for error was considered to be relatively small. All respondents were contacted in the workplace so potential bias relating to the ‘inability to be contacted’ did not present as an issue. Concerns initially existed that in some projects an expert informant whilst having knowledge of a project at the macro level may not have had the detailed knowledge of nursing practice sought in interview questions 23 and 24. Nurses, however, were expert informants in over 50 per cent of the interviews where specific information was sought on nursing practice, and the questionnaire was available to respondents before the interview, allowing time for the clarification of any details. A 100 per cent response rate was achieved and all questions were answered. 78 This was because only those projects identified by respondents could be followed up. Eligible projects may have existed that were not identified by respondents. 255 9.2.3 Questionnaire design No survey instrument was found to exist that could collect data to answer the four research questions, so a questionnaire was developed that used a standardised set of questions for the interview. Open-ended questions, reducing complex questions into sets of simpler questions, and choosing the correct category from options provided by the interviewer were strategies employed to ensure data collected had depth and accuracy. Groves (1989) suggests variations in question form are necessary to make sure questions are answerable in a telephone survey. Detailed numerical categorisation and coding processes ensured data were standardised and quality was maintained. Internal consistency reliability was addressed by a number of survey questions measuring aspects of the same variable. For example, health services were measured in questions eight, nine and 10. As the review was conducted by experts and pilot-tested on health professionals, predictive validity, rather than concurrent validity was established (see p. 143). Overall, pilot-testing suggested the questions were understood and provided consistent measures in comparable situations. Sets of questions were found to be appropriate and provided useful data, indicating validity. Internal consistency reliability, an indicator of how well different items measure the same variable, was weak in questions 17 and 20. Question 17 asked who funded the project and question 20 asked if general practice incurred financial costs as a result of participating in the project. Some responses indicated general practice had funded projects (incurring costs), whilst also indicating no costs had been incurred. Further investigation revealed that the funding of projects was often not considered a cost in the same way as the funding of lesser costs relating to project implementation (see p. 204). 256 9.2.4 Data collection procedures The survey has become the most widely used method of data collection in public health research as descriptive data can establish meaning by contrasting, comparing, or identifying relationships (Creswell, 2003). The telephone survey was preferred as a method of data collection over face-to-face surveying by the researcher because it was less intrusive than face-to-face interviewing and importantly, enabled lower financial costs to be incurred as respondents represented a range of projects across New Zealand. A further advantage of this survey was the ability to collect detailed data in pre-selected categories within a relatively short time. Data on a large number of projects were collected in a systematic and organised manner, a feature of the telephone survey that enabled potentially better quality control than the use of a selfadministered questionnaire (Fowler, 2002). Acceptability of the telephone interview by respondents appeared to result from a perception that this was work-related and was of limited inconvenience requiring only a 60 minute interview during the work day. Whilst surveys have been criticised for constituting a ‘data raid’ with little benefit to the respondents (Wadsworth, 1997), the researcher offered interviewees access to the study results upon completion of the research. The study findings provide a source of data and insights into the complexity of health service provision, including nursing practice, that can assist these key informants as well as health policy development and action generally. 9.2.4.1 The interview The interview was fully structured as it sought to obtain “research-relevant information…on content specified by the research objectives of systematic description, prediction or explanation” (Cohen & Manion, 1989, p. 307). This style has been criticised as detached (Oakley, 1981) and telephone interviews as more difficult than other methods at building rapport (Bradburn et al., 1979). However, Bradburn et al. suggested the drawbacks of the telephone interview were compensated for by smaller interviewer effects and a lower tendency towards socially desirable responses. In the current study the researcher was not detached but rather sought to develop a friendly, interested, and professional style of relating in an attempt to build 257 rapport. Fowler and Mangione (1990) report that interviewers who take steps to relax respondents, without detracting from a professional interaction, may be able to produce a more effective interview. On occasions interviewees asked questions of the interviewer who was flexible and responded with honesty. Oakley (1981) maintains this approach ensures integrity in the interview process, although others have argued the “lack of standardisation that this implies raises concerns about reliability” (Robson, 1993, p. 229). Standardisation was ensured by the use of one interviewer who conducted all interviews. The interviewer knew several of the respondents so attempts were made to minimise personal communication in an effort to standardise the interview. Other measures to standardise the interview process were discussed in section 6.4.3.5 (see pp. 144-147). 9.2.5 9.2.5.1 Data analysis procedures Organising data analysis Two types of errors were potential issues in organising data for analysis. The first involved transcribing a response onto the questionnaire at the time of the interview. Responses perceived by the researcher to be ambiguous were clarified at this point, with the majority of questions ‘closed’ to reduce the risk of error (see p. 141, Table 10). The second type of error related to the coding of responses. Significant effort went into constructing codes that placed answers in analytically meaningful categories (see pp. 147-157, section 6.4.4.1). 9.2.5.2 Data analysis The second phase of the analysis involved the development of a formula (see p. 161) for the specific purpose of locating variables on a health promotion grid (see p. 194, Figure 18). This formula was developed for the current study, in which all interventions related to populations of individuals, rather than communities or groups. 258 To extrapolate this formula to other situations where systems include communities will require amendments to be made to the formula79. The process of attributing values to nurses practice using the frameworks of the public health intervention wheel (Keller et al., 1998) and Beattie’s model of health promotion (Beattie, 1991) is open to challenge. This is solely because the collective range of interventions that constitute health promotion practice can be contested (Beattie, 1991; Downie et al., 1990; B. Tones, 1986; K. Tones & Tilford, 1994). The definition of health promotion that was adopted for use in the thesis (see p. 27) was deliberately broad, allowing for the inclusion of activities such as ‘delegated functions’ that may be associated with illness management, which remains contentious. The interventions undertaken by nurses in projects represented a comprehensive range of activities. Analysis of these interventions undertaken by nurses studied in integrated care projects provided new insights into what was conceived as primary health care practice. 9.3 Implications of the PHCI Model for nursing practice Nursing practice is challenged with being responsive to the changing health needs of individuals and populations. The importance of addressing health disparities caused by social, economic, cultural and structural inequalities has increasingly been realised and strengthening primary health care, a vehicle for improving population health outcomes, has been mandated (Ministry of Health, 2001b). Integrated care projects, a health reform of the 1990’s, provided a primary health care context within which nurses’ practice could be assessed. During the last four years an increased focus on primary health care has influenced national strategies and continuation of structural health reform. Many contemporary projects, such as Care Plus, which targets people with chronic conditions (Ministry of Health, 2004a) have benefited from antecedent strategies, such as integrated care. New primary health care nursing initiatives are underway although to date, a national framework that demonstrates the interventions and health promotion philosophy required to advance primary health care practice has 79 A possible adaptation could be: Community (community + systems) – Individual (individual + system) = Position 259 yet to be mandated. This study has shown the reality of nurses’ practice to be restricted within a primary care environment that focused on the acute care management of an individual’s problems. Nurses appeared ill-equipped to promote primary health care in a broader community sense. Study findings indicate that integrated care, which planned to work in ‘innovative ways’ to improve the health of populations characterised by being Maori, Pacific, low income, or with chronic conditions, was exceedingly limited. In the main, nurses, like the projects they were employed in, practiced from a traditional, individually oriented paradigm. It seems apparent that the next step in advancing a primary health care nursing agenda is to identify a framework that explains current practice and can demonstrate a way to reorient future practice to achieve greater improvement in the health of groups and communities, in addition to individuals. Nursing has an important role to play in the activities of health promotion - the provision of care, the prevention of illness, and the promotion of positive health. Caraher (1994) maintains “the attempt to create a healthy population is a worthy one” (see p. 467) and nursing because of its role in health promotion, must determine the most effective way to achieve this end. Health promotion, at any level of population-based practice cannot be divorced from politics and ideology, and implementing primary health care is at present a central issue. As there is no common approach to implementation, fragmentation of health care services remains a risk. In the current study health persuasion and personal counselling strategies were adopted in the majority of interventions undertaken by nurses employed in integrated care projects. Personal counselling was considered by health promotion commentators, and health professionals including nurses, to be a more effective way of working with clients (Beattie, 1990, 1991; K. Tones et al., 1990; Wilson-Barnett, 1988). Nurses employed in projects appeared to locate health within a political agenda that was largely individualistic. Nurses did not appear to understand that this strategy could also create victims (Crawford, 1977). Interventions by nurses that target individuals is appropriate from a health promotion perspective when combined with interventions at the community and systems levels, and when the emphasis includes a wider socio-environmental perspective. Overall, nurses employed in projects did not often use the strategies of legislative action or community 260 development in promoting the health of communities. This is of note, as two decades of the ‘New public health’ have attempted to introduce these concepts and they have become increasingly visible in national strategies and advisory reports (Ministry of Health, 2001b, 2001c, 2003b). Consistent with this, structural reforms to the health care system have attempted to shift the focus from primary care to more comprehensive primary health care. More recently, nursing has received funding for scholarships and innovative projects in a concerted effort to advance primary health care (Ministry of Health, 2003a, 2005). Scholarships for post-graduate education have focused predominantly on the development of clinical skills, rather than on the relationship between the nurse and client where issues of power and control are examined and health promotion practice comes to be understood as more than a benign encounter. The shift from an individual-focus to include a community-focus is anticipated. However, without a map to guide the journey, progress is likely to be slow. The implication of this finding is the need to transition primary health care nursing from essentially, individual encounters in primary care to more comprehensive primary health care practices. The PHCI model can guide the implementation of primary health care practice in New Zealand. The Model can be used to explain and evaluate nursing practice in operation, identify gaps, and plan future practice. A strong ideological position, commonly held by all primary health care nurses is intrinsic to the development of a skilled workforce able to integrate individual and community empowerment goals within health care practice. As stated previously, the PHCI model has the ability to run in parallel with other cultural frameworks (Durie, 1998) or empowerment models (Laverack & Labonte, 2000). Research to evaluate the effectiveness of the PHCI model as a tool to guide the implementation of primary health care is recommended in settings, such as the current PHO environment. Nurses’ perceptions regarding the degree to which the model is useful in assisting them to advance their practice must also be surveyed. Future research into the range of interventions, levels of population-based practice, and health promotion values within nurses’ practice is required. As societal values 261 change, the values embedded in nurses’ practice will also change. Finally, and most importantly, the effect of community population-based practice, in conjunction with systems and individual levels of practice must be studied to determine the degree of impact a multilevel approach has on the total outcome: the health of the population. 9.4 Recommendations Advocacy for the acceptance of this model is expected to be a complex process and will have implications for health policy. Stakeholders will include: The Ministry of Health; The Nursing Council of New Zealand; health organisations such as, District Health Boards and Primary Health Organisations; educational institutions; nurses; communities, and individuals. The following recommendations are offered to facilitate this process: 1. The Ministry of Health 1.1 Formally advocate the PHCI model as a framework for implementing primary health care nursing practice. 1.2 Support individual and community empowerment approaches in primary health care policies and programmes funded by the state. 1.3 Affirm the Treaty of Waitangi by ensuring that whanau, hapu, and iwi are active in the design and delivery of primary health care programmes. 1.4 Implement national conventions for the promotion of health and the equal status of all people. 1.4 Continue to resource innovations in primary health care and to develop a skilled, competent workforce. 2. The New Zealand Nursing Council 2.1 Adopt the PHCI model as the central framework for implementing primary health care nursing practice. 262 2.2 Ensure that ‘essential knowledge’ in primary health care is defined and included in the prescribed curricula for the education of nurses at undergraduate and postgraduate levels. 2.3 Conduct ongoing research into the interventions, levels of practice, and health promotion values within primary health care nursing practice and the association with health outcomes at individual, community and population levels. 3. Health provider organisations 3.1 Formally adopt the PHCI model as a framework for implementing primary health care practice. 3.2 Ensure health professionals working in primary health care understand how to accommodate both individual and community empowerment goals within typical approaches to health promotion. 3.3 Incorporate this knowledge and appropriate practice in training and accreditation systems. 3.4 Develop strategies to promote health in partnership with clients, relevant to local conditions, and communities. Share information across health provider organisations and coordinate projects where possible. 3.5 Promote the message that individuals and communities have the right and responsibility to be involved in their own health care. 4. Educational institutions 4.1 Provide educational programmes at undergraduate and postgraduate levels for nurses that build primary health care knowledge and offer strategies for clinical practice. 4.2 Introduce the PHCI model as a conceptual framework for analysing primary health care nursing practice. 4.3 Research ways to deepen discussions with communities about health issues and acceptable, relevant, health promotion practice. 263 5. Primary health care nurses 5.1 Adopt the PHCI model as a framework for implementing primary health care nursing practice. 5.2 Evaluate the effectiveness of practice, including information on health outcomes, and client and community feedback. 5.3 Promote the PHCI model and education about health promotion concepts to nurses, other health professionals/workers and consumers. 6. Communities and individuals 6.1 Collaborate with Government and health provider organisations in identifying and prioritising health need and approaches to health and health care. 6.2 Advocate with Government and health provider organisations for the promotion of individual and community empowerment. 6.3 Participate in implementing health interventions with nurses, health professionals/workers and others to improve health outcomes. 9.5 Conclusion The contribution of this research has been to provide an understanding of the practice, and values within that practice, of nurses in integrated care projects. Theoretical frameworks provided tools for analysis in combination with a postpositivist research philosophy to clarify types of interventions and levels of population-based practice. From insights gained about this nursing practice reality, a new model has been developed to assist nurses and others to implement primary health care in New Zealand and elsewhere. This work began in 1999 in the midst of more than a decade of health reforms and has ended, contributing to sector knowledge that supports the need to transform the acute care system to one that has a chronic care focus and emphasises primary health care. Nurses as the largest health professional group demonstrated only a small measure of practice innovation in integrated care projects and little evidence exists of their collective efforts in advancing this strategy. Since 2001 the Government has invested 264 in PHC nursing and attempted to create an environment that fosters innovation. If nurses however, cannot envisage a future where interventions are directed at communities and entire populations, innovations in practice will continue to centre on individuals, predictive of the past. A major paradigmatic shift from individuals to groups and communities and an acceptance of the health promotion values associated with community development challenges nurses to turn new ideas into a working reality. The Government, health provider organisations, and nursing professional bodies, whilst espousing the rhetoric of primary health care have not advocated for a health promotion ideological and practice approach for implementation. This remains the greatest challenge because without leadership PHC nursing practice will remain inconsistent and under-developed, and will not be able to meet the needs of populations experiencing the increasing burden of illness and disability associated with chronic conditions. The journey of changing the paradigm of nursing practice to reflect a truly primary health care orientation has only just begun. There will be further changes to the structure of the health care system and the roles of the different health professional groups in New Zealand, and these changes will provide a challenge to the ongoing practice development of PHC nursing. Future research is required to understand both new health system contexts and the evolution of PHC nursing practice as it pursues a more comprehensive primary health care path that is less constrained and offers greater opportunity for both nurses and their clients. 265 References Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall. Alcorn, G. D. (2002). Giving voice to school nursing as a primary health care specialty. Unpublished master's thesis, Victoria University of Wellington, Wellington, New Zealand. Alem, A. (2001). Mental health services and epidemiology of mental health problems in Ethiopia. Ethiopian Medical Journal, 39(2), 153-165. Anderson, S. (1998, 1 September). Thoughts on integrated care. Health Care & Informatics Review Online, 2(11). Retrieved June 17, 2004, from http://hcro.enigma.co.nz/website/index.cfm?fuseaction=articledisplay&Featur eID=48 Andreasen, A. R. (1995). Marketing social change: Changing behavior to promote health, social development, and the environment. San Francisco: Jossey-Bass. Armstrong, D. (1979). The emancipation of biographical medicine. Social Science & Medicine - Medical Psychology & Medical Sociology, 13A(1), 1-8. Armstrong, D. (1988). Historical origins of health behaviour. In R. Anderson, J. Davies, I. Kickbusch, D. McQueen & J. Turner (Eds.), Health behaviour research and health promotion (pp. 8-21). Oxford, United Kingdom: Oxford University Press. Armstrong, J. (1995, September 3). India faces AIDS explosion. The Guardian Weekly, p. 17. Armstrong, W., & Bandaranayake, D. (1995). Public health in New Zealand: Recent changes and future prospects. Wellington, New Zealand: Department of Public Health. 266 Ashton, J. (1992). Healthy cities. Philadelphia: Open University Press. Ashton, J., & Seymour, H. (1988). The new public health: The Liverpool experience. Milton Keynes, United Kingdom: Open University Press. Ashton, T. (1998, June 29-July 1). Development of integrated care initiatives in New Zealand: Incentives and risks. Paper presented at the Health and Risk: An International Symposium, St Catherine's College, Oxford University, England. Ashton, T. (2001). The influence of economic theory. In P. Davis & T. Ashton (Eds.), Health and public policy in New Zealand (pp. 107-126). Auckland, New Zealand: Oxford University Press. Ashton, T. (2005). Recent developments in the funding and organisation of the New Zealand health system. Australia and New Zealand Health Policy, 2(1), 9-15. Atkin, K., & Lunt, N. (1996). The role of the practice nurse in primary health care: Managing and supervising the practice nurse resource. Journal of Nursing Management, 4(2), 85-92. Bachrach, L. L. (1982). Assessment of outcomes in community support systems: Results, problems, and limitations. Schizophrenia Bulletin, 8(1), 39-61. Baird, J. (2004). Community based support services for older people: Draft discussion. Hamilton, New Zealand: Presbyterian Support Services. Bandura, A. (1977). Social learning theory. Englewood Cliffs, NJ: Prentice Hall. Barlow, C. (1991). Tikanga whakaaro: Key concepts in Maori culture. Auckland, New Zealand: Oxford University Press. Barnum, H., & Kutzin, J. (1993). Public hospitals in developing countries: Resource use, cost, financing. Baltimore: Johns Hopkins University Press. 267 Baum, F. E. (1993). Healthy cities and change: Social movement or bureaucratic tool? Health Promotion International, 8(1), 31 - 40. Baum, F. E. (1998). The new public health: An Australian perspective. Melbourne, Australia: Oxford University Press. Baum, F. E., & Saunders, D. (1995). Can health promotion and primary health care achieve health for all without a return to their more radical agendas? Health Promotion International, 10(2), 149-160. Beaglehole, R., & Bonita, R. (1997). Public health at the crossroads: Achievements and prospects. Cambridge, England: Cambridge University Press. Beattie, A. (1986). Community development for health: From practice to theory? Radical Health Promotion, 4, 11-16. Beattie, A. (1990). Teaching and learning about health education: New directions for curriculum development. Edinburgh, United Kingdom: Health Education Board for Scotland. Beattie, A. (1991). Knowledge and control in health promotion: A test case for social policy and social theory. In J. Gabe, M. Calnan & M. Bury (Eds.), The sociology of the health service (pp. 162-202). London: Routledge. Becker, M. H. (Ed.). (1974). The Health belief model and personal health behavior. Thorofare, NJ: Charles B. Slack. Belson, W. A. (1981). The design and understanding of survey questions. Aldershot, England: Gower. Benjamin, A. E., & Newcomer, R. J. (1997). Community level indicators of chronic health conditions. In R. J. Newcomer & A. E. Benjamin (Eds.), Indicators of chronic health conditions: Monitoring community-level delivery systems (pp. 1-14). Baltimore, MD: Johns Hopkins University Press. 268 Berman, P. (2000). Organization of ambulatory care provision: A critical determinant of health system performance in developing countries. Bulletin of the World Health Organization, 78(6), 791-802. Bernstein, B. B., & Henderson, D. (1974). Social class differences in the relevance of language to socialization. In B. B. Bernstein (Ed.), Class, codes and control: Vol. 2. Primary socialization, language and education (pp. 24-47). London: Routledge & Kegan Paul. Betkowski, N. (1996). Preface. In M. Stingl & D. Wilson (Eds.), Efficiency versus equality: Health reform in Canada (pp. ix-xi). Halifax, Nova Scotia, Canada: Fernwood Publications. Blackham, H. J. (Ed.). (1978). Education for personal autonomy: An inquiry into the school's resources for furthering the personal development of pupils. London: Bedford Square Press. Blackwell, D. L., Hayward, M. D., & Crimmins, E. M. (2001). Does childhood health affect chronic morbidity in later life? Social Science & Medicine, 52(8), 12691284. Blue, R. G. (1995). "A new net goes out fishing": Options for change within the public health nursing service. Unpublished master's thesis, University of Auckland, Auckland, New Zealand. Bodenheimer, T., Wagner, E. H., & Grumbach, K. (2002a). Improving primary care for patients with chronic illness. JAMA, 288(14), 1775-1779. Bodenheimer, T., Wagner, E. H., & Grumbach, K. (2002b). Improving primary care for patients with chronic illness: The chronic care model, Part 2. JAMA, 288(15), 1909-1914. Boyd, M. (1998). Handover briefing: Integration initiatives Auckland localities. Auckland, New Zealand: Health Funding Authority. 269 Boyd, M., & Sheridan, N. F. (2000). New Zealand. In W. W. Wieners (Ed.), Global health care markets: A comprehensive guide to regions, trends, and opportunities shaping the international health arena (pp. 304-313). San Francisco: Jossey-Bass. Bradburn, N. M., Sudman, S., & Blair, E. (1979). Improving interview method and questionnaire design. San Francisco: Jossey-Bass. Brault, G. L., & Kissinger, L. D. (1991). Case management: Ambiguous at best. Journal of Pediatric Health Care, 5(4), 179-183. Bringewatt, R. J. (1997, December 9-19). Integrating for person-centered care. Paper presented at the Second Annual Washington Conference on Integrated Patient Care, Washington, DC. Brockington, C. F. (1975). The history of public health. In W. Hobson (Ed.), The theory and practice of public health (4th ed., pp. 1-7). London: Oxford University Press. Brown, M., & Crampton, P. (1997). New Zealand policy strategies concerning the funding of general practitioner care. Health Policy, 41(2), 87-104. Brown, M., Masters, D., & Smith, B. (1997). Nursing education in New Zealand: Hospital vs polytech vs university. Professional Leader, 4(1), 7-11, 14. Brundtland, G. H. (2001). Bridging the health divide: The way forward. In Address: Fifty-fourth World Health Assembly, Geneva. Retrieved July 15, 2003, from http://66.102.7.104/search?q=cache:PHgQxtL3a94J:www.who.int/directorgeneral/speeches/2001/english/20010514_wha54.html+%22world+health+ass embly%22+brundtland+2001+%22tobacco+will+cause%22&hl=en Buck, P. H. (1949). The coming of the Maori. Wellington, New Zealand: Maori Purposes Fund Board/Whitcombe and Tombs. 270 Buffat, J. (2000). Unemployment and health. Revue Medicale de la Suisse Romande, 120(4), 379-383. Bunton, R. (1992). Health promotion as social policy. In R. Bunton & G. Macdonald (Eds.), Health promotion: Disciplines and diversity (pp. 129-152). London: Routledge. Burgess, M. E. (1984). Nursing in New Zealand society. Auckland, New Zealand: Longman Paul. Burns, T. (1997). Case management, care management and care programming. British Journal of Psychiatry, 170(5), 393-395. Campbell, A. (1984). Moderated love: A theology of professional care. London: SPCK. Campbell, D. T., & Stanley, J. C. (1963). Experimental and quasi-experimental designs for research. In N. L. Gage (Ed.), Handbook of research on teaching (pp. 1-76). Chicago: Rand-McNally. Caplan, R. (1993). The importance of social theory for health promotion: From description to reflexivity. Health Promotion International, 8(2), 147-157. Caraher, M. (1994). Nursing and health promotion practice: The creation of victims and winners in a political context. Journal of Advanced Nursing, 19(3), 465468. Carryer, J. (2004). Nursing participation and governance in primary health organisation or talking primary health care, thinking primary care. Vision EIT, 12(1), 4-9, 13-14. Carryer, J., Dignam, D., Horsburgh, M., Hughes, F., & Martin, J. (1999). Locating nursing in primary health care: A report for the National Health Committee. Wellington, New Zealand: National Health Committee. 271 Central Health. (1997a). Integrated care: A beginner's guide. Wellington, New Zealand: Transitional Health Authority. Central Health. (1997b). Integrated care: Project and policy information pack: Draft report. Wellington, New Zealand: Transitional Health Authority. Chaplin, J., & Adams, D. (1986). London health action network. London: London Community Health Resource. Cohen, L., & Manion, L. (1989). Research methods in education (3rd ed.). London: Routledge. College of Nurses Aotearoa (NZ) Inc. (2001). The nursing answer to inequalities in primary health care. Palmerston North, New Zealand: Author. Collins, R. (1993). Emotional energy as the common denominator of rational action. Rationality and Society, 5(2), 203-230. Commission on Chronic Illness. (1957). Chronic illness in the United States, prevention of chronic illness. Cambridge, MA: Harvard University Press. Cooper, J. O., Heron, T. E., & Heward, W. L. (1987). Applied behavior analysis. Columbus, OH: Merrill Publications. Coster, G. (1998, August 1). An academic perspective on the development of integrated care. Health Care & Informatics Review Online, 2(10). Retrieved November 25, 2004, from http://www.enigma.co.nz/hcro/website/results/2005011212043011900977.pdf Coutts, L. C., & Hardy, L. K. (1985). Teaching for health: The nurse as health educator. New York: Churchill Livingstone. Crampton, P., Dowell, A., & Woodward, A. (2001). Third sector primary care for vulnerable populations. Social Science & Medicine, 53(11), 1491-1502. 272 Crampton, P., Salmond, C. E., & Kirkpatrick, R. (2004). Degrees of deprivation in New Zealand: An atlas of socioeconomic difference (2nd ed.). Auckland, New Zealand: David Bateman. Crawford, R. (1977). You are dangerous to your health: The ideology and politics of victim blaming. International Journal of Health Services, 7(4), 663-680. Creech, W. (1999). The Government's medium-term strategy for health and disability support services, 1999. Wellington, New Zealand: Ministry of Health. Creswell, J. W. (2003). Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage Publications. Crombie, D., & Gedye, C. (1997). Integrated care plan for North Health. Auckland, New Zealand: Northern Regional Health Authority. Crotty, M. (1998). The foundations of social research: Meaning and perspective in the research process. London: Sage. Davies, P. (1999). Making sense of integrated care in New Zealand. Australian Health Review, 22(4), 25-44; discussion 45-27. Davis, P., & Ashton, T. (2001). Health and public policy in New Zealand. Auckland, New Zealand: Oxford University Press. Davis, P., Gribben, B., Lee, R. L., & McAvoy, B. (1994). The impact of the new subsidy regime in general practice in New Zealand. Health Policy, 29(1-2), 113-125. Davis, R., Wagner, E. G., & Groves, T. (2000). Advances in managing chronic disease. Research, performance measurement, and quality improvement are key. BMJ, 320(7234), 525-526. Davis, R., Wagner, E. H., & Groves, T. (1999). Managing chronic disease. BMJ, 318(7191), 1090-1091. 273 Degeling, P., Maxwell, S., Kennedy, J., & Coyle, B. (2003). Medicine, management, and modernisation: A "danse macabre"? BMJ, 326(7390), 649-652. Department of Health. (1974). A health service for New Zealand. Wellington, New Zealand: Government Printer. Department of Health. (1986). Public health nursing: Report of the review Committee to the Director-General of Health. Wellington, New Zealand: The Committee. DeSimone, B. S. (1988). The case for case management. Continuing Care, 7(6), 2223. Docherty, B. (1996). Nursing in general practice: A New Zealand perspective. Christchurch, New Zealand: Author. Docherty, B. (2004). Nursing participation and governance in primary health organisation or talking primary health care, thinking primary care: Commentary 1. Vision EIT, 12(1), 10-11. Dooley, D., Fielding, J., & Levi, L. (1996). Health and unemployment. Annual Review of Public Health, 17, 449-465. Dow, D. A. (1995). Safeguarding the public health: A history of the New Zealand Department of Health. Wellington, New Zealand: Victoria University Press. Dowie, J. (2001). Towards value-based, science-informed public health policy: Conceptual framework and practical guidelines: Background paper for The World Health Report 2002. Geneva, Switzerland: World Health Organization. Downie, R. S., Fyfe, C., & Tannahill, A. (1990). Health promotion: Models and values. Oxford: Oxford University Press. Doyal, L., & Pennell, I. (1979). The political economy of health. London: Pluto Press. 274 Draper, P., Best, G., & Dennis, J. (1977). Heath & wealth. Royal Society of Health Journal, 97(3), 121-126. Durie, M. H. (1985). Maori health institutions. Community Mental Health in New Zealand, 2(1), 64-69. Durie, M. H. (1998). Whaiora: Maori health development (2nd ed.). Auckland, New Zealand: Oxford University Press. Durie, M. H. (2004, April 26-30). An indigenous model of health promotion. Paper presented at the 18th World Conference on Health Promotion and Health Education, Melbourne, Australia. Durkheim, E. (1984). The division of labor in society (W. D. Hall, Trans.). New York: Free Press. Ellwood, P. M. (1988). Shattuck lecture--outcomes management. A technology of patient experience. New England Journal of Medicine, 318(23), 1549-1556. English, B. (1997). Keynote Address. Paper presented at the Annual Conference of the Association of Salaried Medical Specialists, Wellington, New Zealand. Ensor, T., & San, P. B. (1996). Access and payment for health care: The poor of Northern Vietnam. International Journal of Health Planning & Management, 11(1), 69-83. Entwistle, M. (1997, September 1). Co-ordinated contracting: An enabling strategy for the development of integrated care presented to the NZIHM & NZHA Conference. Health Care & Informatics Review Online, 2(2). Retrieved May 4, 2004, from http://www.enigma.co.nz/hcro/website/results/2005011213541860300981.pdf Evans, R. G., & Stoddart, G. L. (1990). Producing health, consuming health care. Social Science & Medicine, 31(12), 1347-1363. 275 Ewles, L., & Simnett, I. (2003). Promoting health: A practical guide (5th ed.). Edinburgh: Baillière Tindall. Feather, J., & Labonte, R. (1995). Sharing knowledge from health promotion practice: Final report. Saskatoon, Canada: University of Saskatchewan, Prairie Region Health Promotion Research Centre. Feek, C. (1998, May 1). Policy and ethics. Health Care & Informatics Review Online, 2(7). Retrieved May 4, 2004, from http://www.enigma.co.nz/hcro/website/results/200501121349064100980.pdf Fink, A. (1995). How to sample in surveys. Thousand Oaks, CA: Sage. Ford, R., Beadsmoore, A., Ryan, P., Repper, J., & Mattmuijen, C. (1995). Providing the safety net: Case management for people with a serious mental illness. Journal of Mental Health, 4(1), 91-97. Foucault, M. (2002). Archaeology of knowledge. London: Routledge. Fowler, F. J., Jr. (1992). How unclear terms affect survey data. Public Opinion Quarterly, 56(2), 218-231. Fowler, F. J., Jr. (2002). Survey research methods (3rd ed.). Thousand Oaks, CA: Sage Publications. Fowler, F. J., Jr., & Mangione, T. W. (1990). Standardized survey interviewing: Minimizing interviewer-related error. Newbury Park, CA: Sage Publications. French, J. (1990). Boundaries and horizons: The role of health education within health promotion. Health Education Journal, 49(1), 7-10. French, J., & Adams, L. (1986). From analysis to synthesis: Theories of health education. Health Education Journal, 45(2), 71–74. 276 French, S., Old, A., & Healy, J. (2001). Health care systems in transition: New Zealand. European Observatory on Health Care Systems, 3(19), 1-136. Frenk, J. (1993, May). The new public health. Annual Review of Public Health, 14, 469-490. Frenk, J. (1994). Dimensions of health system reform. Health Policy, 27(1), 19-34. Garside, P. (1987, July). History of public health. Paper presented at the Rethinking public health, Birmingham, United Kingdom. Gatherer, A., Parfit, J., Partner, E., & Vessey, M. (1979). Is health education effective? London: Health Education Council. Glasgow, R. E., Orleans, C. T., & Wagner, E. H. (2001). Does the chronic care model serve also as a template for improving prevention? Milbank Quarterly, 79(4), 579-612. Goering, P. N., Wasylenki, D. A., Farkas, M., Lancee, W. J., & Ballantyne, R. (1988). What difference does case management make? Hospital & Community Psychiatry, 39(3), 272-276. Golodner, L. (1999). Consumer voice. In E. L. Cohen & V. De Back (Eds.), The outcomes mandate: Case management in health care today (pp. 20-26). St. Louis, MO: Mosby. Gott, M., & O'Brien, M. (1990). The role of the nurse in health promotion. Health Promotion International, 5(2), 137-143. Gravitas Research and Strategy Limited. (2005). Quality of life in New Zealand's largest cities: Resident's survey. Retrieved May 26, 2005, from http://www.bigcities.govt.nz/pdf2004/Survey_Quality_Of_Life_2004Exec_summary.pdf 277 Green, L. W., & Raeburn, J. (1988). Health promotion. What is it? What will it become? Health Promotion, 3(2), 151-159. Grone, O., & Garcia-Barbero, M. (2001, April-June). Integrated care: A position paper of the WHO European office for integrated health care services. International Journal of Integrated Care, 1, 1-15. Retrieved October 15, 2004, from http://www.ijic.org/publish/articles/000036/article_print.html Groves, R. M. (1989). Survey errors and survey costs. New York: Wiley. Grundy, E. (1997). Demography and gerontology: Mortality trends among the oldest old. Ageing & Society, 17(6), 713-725. Guidotti, T. L. (1989). Health promotion in perspective. Canadian Journal of Public Health, Revue Canadienne de Sante Publique. 80(6), 400-405. Gwatkin, D. R., & Guillot, M. (2000). The burden of disease among the world's poor: Current situation, future trends, and implications for policy. Washington, DC: Human Development Network of The World Bank. Halmos, P. (1965). The faith of the counsellors. London: Constable. Hamilton, N., & Bhatti, T. (1996). Population health promotion: An integrated model of population health and health promotion. Ottawa, Ontario, Canada: Health Promotion Development Division. Hardy, J. (1981). Values in social policy: Nine contradictions. London: Routledge & Kegan Paul. Health Benefits Review. (1986). Choices for health care: Report of the health benefits review. Wellington, New Zealand: Author. Health Funding Authority. (1998). Service integration: Guidelines for the development of integration demonstration projects. Wellington, New Zealand: Author. 278 Health News. (2004). Health of a nation: 29/01/2004: A year in the health of New Zealand. Retrieved June 6, 2005, from http://www.healthpages.co.nz/index.php?page=422033+152215552 Health Services Research Centre, & Te Ropu Rangahau Hauora a Eru Pomare. (2001). National demonstration integrated care pilot projects: Overview report: Final evaluation report. Wellington, New Zealand: Victoria University, Health Services Research Centre. Heffler, S., Levit, K., Smith, S., Smith, C., Cowan, C., Lazenby, H., et al. (2001). Health spending growth up in 1999: Faster growth expected in the future. Health Affairs, 20(2), 193-203. Hennekens, C. H., & Buring, J. E. (1987). Epidemiology in medicine. Boston: Little, Brown and Company. Herrin, J., Cangialose, C. B., Boccuzzi, S. J., Weintraub, W. S., & Ballard, D. J. (2000). Household income losses associated with ischaemic heart disease for US employees. Pharmacoeconomics, 17(3), 305-314. Hetzel, B. S. (1976). Health and Australian society. Ringwood, Victoria, Australia: Penguin. Hickman, M., Drummond, N., & Grimshaw, J. (1994). A taxonomy of shared care for chronic disease. Journal of Public Health Medicine, 16(4), 447-454. Hill, H. W. (1916). The new public health. New York: Macmillan. Hiss, R. G. (1996). Barriers to care in non-insulin-dependent diabetes mellitus. The Michigan experience. Annals of Internal Medicine, 124(1 Pt 2), 146-148. Holt, S., & Beasley, R. (2001). The burden of asthma in New Zealand. Wellington, New Zealand: Asthma and Respiratory Foundation of New Zealand. 279 Hopkins, C. D. (1980). Understanding educational research: An inquiry approach. Columbus, OH: Merrill. Howden-Chapman, P., & Tobias, M. (Eds.). (2000). Social inequalities in health: New Zealand 1999: A summary. Wellington, New Zealand: Ministry of Health. Hughes, F. (2003). Nursing sector update. Wellington, New Zealand: Ministry of Health. Hunn, J. K. (1961). Report on Department of Mäori Affairs: With statistical supplement, 24 August 1960. Wellington, New Zealand: Government Printer. Institute of Medicine (U.S.) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press. Jansen, P. (1998). The relationships of integrated care organisations and other health care providers with Maori. Wellington, New Zealand: Transitional Health Authority. Jensen, G. A., & G, K. J. (1999). Longitudinal profiling: A differentiated community nursing model. In E. L. Cohen & V. De Back (Eds.), The outcomes mandate: Case management in health care today (pp. 152-161). St Louis, MO: Mosby. Kanter, J. (1989). Clinical case management: Definition, principles, components. Hospital & Community Psychiatry, 40(4), 361-368. Kaplan, R., & Norton, D. (1997). Translating strategy into action: The balanced scorecard. Boston: HBA Press. Keating, G. (1998). A view from the Ministry of Health. Health Care & Informatics Review Online, 2(8). Retrieved February 8, 2005, from http://216.239.57.104/search?q=cache:3TCjtypFKu4J:www.enigma.co.nz/hcro /website/index.cfm%3Ffuseaction%3Darticledisplay%26FeatureID%3D39+ke ating+view+from+ministry+health+offers+services&hl=en 280 Keller, L. O., Schaffer, M. A., Lia-Hoagberg, B., & Strohschein, S. (2002). Assessment, program planning, and evaluation in population-based public health practice. Journal of Public Health Management and Practice, 8(5), 3043. Keller, L. O., Strohschein, S., Lia-Hoagberg, B., & Schaffer, M. (1998). Populationbased public health nursing interventions: A model from practice. Public Health Nursing, 15(3), 207-215. Keller, L. O., Strohschein, S., Lia-Hoagberg, B., & Schaffer, M. A. (2004). Population-based public health interventions: Practice-based and evidencesupported. Part I. Public Health Nursing, 21(5), 453-468. Keller, L. O., Strohschein, S., Schaffer, M. A., & Lia-Hoagberg, B. (2004). Population-based public health interventions: Innovations in practice, teaching, and management. Part II. Public Health Nursing, 21(5), 469-487. Kelly, M. P., & Charlton, B. (1995). The modern and the postmodern in health promotion. In R. Bunton, S. Nettleton & R. Burrows (Eds.), The sociology of health promotion: Critical analyses of consumption, lifestyle and risk (pp. 7890). London: Routledge. Kelsey, J. (1993). Rolling back the State: Privatisation of power in Aotearoa/New Zealand. Wellington, New Zealand: Bridget Williams Books. Kennedy, I. (1983). The unmasking of medicine (Rev. ed.). London: Granada. Keppel, G. (1991). Design and analysis: A researcher's handbook (3rd ed.). Englewood Cliffs, NJ: Prentice-Hall. Khawaja, M., & Dunstan, K. (2000, September). Changing face of New Zealand's population. Key Statistics, 7-10. Khawaja, M., & Thomson, N. (2000, January/February). Population ageing in New Zealand. Key Statistics, 7-10. 281 King, A. (2003). Childhood obesity symposium. Retrieved May 8, 2005, from http://www.beehive.govt.nz/ViewDocument.aspx?DocumentID=17723 King, A. (2005). King announces more primary nursing scholarships. In beehive.govt.nz. Retrieved April 25, 2005, from http://www.beehive.govt.nz/ViewDocument.aspx?DocumentID=22414 King, M. (2004). The Penguin history of New Zealand (Rev. ed.). Auckland, New Zealand: Penguin Books. Kiro, C. A. (1997). Tackling inequality in health. Social Work Review, 8(4), 15-17. Kleinman, A. (1978). Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine, 12(2B), 85-95. Kodner, D. L., & Spreeuwenberg, C. (2002, October-December). Integrated care: Meaning, logic, applications, and implications: A discussion paper. International Journal of Integrated Care, 2, 1-8. Retrieved January 19, 2005, from http://www.ijic.org/publish/articles/000089/article.pdf KPMG Consulting. (2001). Strategic review of undergradutate nursing education: Final report to the Nursing Council. New Zealand: Nursing Council of New Zealand. Labonte, R. N. (1996). Community development in the public health sector: The possibilities of an empowering relationship between the state and civil society. Unpublished PhD Thesis, York University, Toronto, Canada. Lalonde, M. (1974). A new perspective on the health of Canadians. Ottawa, Canada: National Health and Welfare. Lamm, R. D. (1994). The ethics of excess. Hastings Center Report, 24(6), 14. 282 Lassey, M. L., Lassey, W. R., & Jinks, M. J. (1997). Health care systems around the world: Characteristics, issues, reforms. Upper Saddle River, NJ: Prentice Hall. Last, J. M. (1998). Public health and human ecology (2nd ed.). Stamford, CT: Appleton & Lange. Laverack, G. (2005). Public health: Power, empowerment, and professional practice. New York: Palgrave Macmillan. Laverack, G., & Labonte, R. (2000). A planning framework for community empowerment goals within health promotion. Health Policy & Planning, 15(3), 255-262. Law, C. M., de Swiet, M., Osmond, C., Fayers, P. M., Barker, D. J., Cruddas, A. M., et al. (1993). Initiation of hypertension in utero and its amplification throughout life. BMJ, 306(6869), 24-27. Law, C. M., Egger, P., Dada, O., Delgado, H., Kylberg, E., Lavin, P., et al. (2001). Body size at birth and blood pressure among children in developing countries. International Journal of Epidemiology, 30(1), 52-57. Lewis, S. (1997). Regionalization and devolution: Transforming health, reshaping politics? (Occasional Paper No. 2). Saskatoon, Saskatchewan, Canada: HEALNet Regional Health Planning, Health Services Utilization and Research Commission. Leyva-Flores, R., Kageyama, M. L., & Erviti-Erice, J. (2001). How people respond to illness in Mexico: Self-care or medical care? Health Policy, 57(1), 15-26. Lincoln, Y. S., & Guba, E. G. (2000). Paradigmatic controversies, contradictions, and emerging confluences. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research (2nd ed., pp. 163-188). Thousand Oaks, CA: Sage. 283 Litchfield, M. (2001, July 28-29). The role of rural nursing: Conservative and progressive models. Paper presented at the National Conference of Rural Nurses in New Zealand, University of Otago, Dunedin, New Zealand. Litwin, M. S. (1995). How to measure survey reliability and validity. Thousand Oaks, CA: Sage. Lomas, J. (1997). Devolving authority for health care in Canada's provinces: 4. Emerging issues and prospects. CMAJ Canadian Medical Association Journal, 156(6), 817-823. Lomas, J., & Rachlis, M. (1996). Moving rocks: Block funding in PEI as an incentive for cross-sectoral reallocations among human services. Canadian Public Administration, 39(2), 581-600. Lomas, J., Woods, J., & Veenstra, G. (1997). Devolving authority for health care in Canada's provinces: 1. An introduction to the issues. CMAJ Canadian Medical Association Journal, 156(3), 371-377. Ludermir, A. B., & Lewis, G. (2001). Links between social class and common mental disorders in Northeast Brazil. Social Psychiatry & Psychiatric Epidemiology, 36(3), 101-107. Lynch, J. W., Kaplan, G. A., & Shema, S. J. (1997). Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. New England Journal of Medicine, 337(26), 1889-1895. MacLean, F. S. (1964). Challenge for health: A history of public health in New Zealand. Wellington, New Zealand: Government Printer. MacLean, F. S. (1966). Medical services. In A. H. McLintock (Ed.), An encyclopaedia of New Zealand (Vol. 2, pp. 521-542). Wellington, New Zealand: Government Printer. 284 Mahler, H. (1988, April 5-9). Opening address. Paper presented at the Healthy Public Policy, 2nd International Conference on Health Promotion, Adelaide, Australia. Malcolm, L. (1997). GP budget holding in New Zealand: Lessons for Britain and elsewhere? BMJ, 314(7098), 1890-1892. Malcolm, L., & Shalowitz, M. (1997). Managed/integrated care in New Zealand: Contrasts with the USA. Unpublished paper. Marmor, T., & Mashaw, J. (2001). Canada's health insurance and ours: The real lessons, the big choices. In P. Conrad & R. Kern (Eds.), The Sociology of health and illness: Critical perspectives (6th ed., pp. 479-489). New York: Worth Publishers. Marmot, M., & Bobak, M. (2000). International comparators and poverty and health in Europe. BMJ, 321(7269), 1124-1128. Marsden, M. (1975). God, man and the universe: A Maori view. In M. King (Ed.), Te Ao Hurihuri: The world moves on: Aspects of Maoritanga (pp. 191-219). Wellington, New Zealand: Hicks Smith. Marshall, M., Gray, A., Lockwood, A., & Green, R. (1998, Update September 22, 2003). Case management for people with severe mental disorders. In May 25, 2005, from The Cochrane Library, Wiley Interscience Martin, J. (2002). The implications of the 2001 primary health care strategy for providers and consumers. Unpublished master's thesis, Massery University, Palmerston North, New Zealand. Marwick, J. (1996, May 2-4). What do we mean by managed care? Paper presented at the Ministry of Health Managed Care Conference: Options for New Zealand, Wellington, New Zealand. 285 Maurin, J. T. (1990). Case management: Caring for psychiatric clients. Journal of Psychosocial Nursing and Mental Health Services, 28(7), 6-12, 32-13. McCormick, R. (1997). Integrated care. Auckland: Northern Regional Health Authority. McCormick, R., & Ranger, W. (1997). Integrated care: Draft North Health strategy and implementation plan: Prepared for the Integration Group. Auckland, New Zealand: Northern Regional Health Authority. McKegg, A. (1991). 'Ministering angels': The government backblock nursing service and the Maori health nurses, 1909-1939. Unpublished master's thesis, University of Auckland, Auckland, New Zealand. McKegg, A. (1992). The Maori Health Nursing Scheme: An experiment in autonomous health care. New Zealand Journal of History, 26(2), 145-160. McKenzie, L. (1997). Discussion paper on integrated care. Wellington, New Zealand: Transitional Health Authority. McKenzie, L., & Webster, J. (1997). Investigation into the ownership and purchase issues for the Crown in relation to integrated care developments in New Zealand: Report for Treasury. Wellington, New Zealand: Unpublished. McKeown, T. (1979). The role of medicine: Dream, mirage, or nemesis? Princeton, NJ: Princeton University Press. McKillop, A. M. (1998). Native health nursing in New Zealand 1911-1930: A new work and a new profession for women. Unpublished master's thesis, Massey University, Palmerston North, New Zealand. McMurray, A. (2003). Community health and wellness: A socioecological approach. Sydney, Australia: Mosby. 286 Mengesha, Y. A., & Bekele, A. (1998). Relative chronic effects of different occupational dusts on respiratory indices and health of workers in three Ethiopian factories. American Journal of Industrial Medicine, 34(4), 373-380. Mertens, D. M. (1998). Research methods in education and psychology: Integrating diversity with quantitative & qualitative approaches. Thousand Oaks, CA: Sage Publications. Michel, J. (1997). Review of practice nurse services in the northern region: Unpublished report. Auckland, New Zealand: Northern Regional Health Authority. Ministry of Health. (1996). Well child - Tamariki ora national schedule. Wellington, New Zealand: Author. Ministry of Health. (1997). The health and wellbeing of older people and kaumatua: The public health issues. Wellington, New Zealand: Author. Ministry of Health. (1998). Report of the ministerial taskforce on nursing: Releasing the potential of nursing. Wellington, New Zealand: Author. Ministry of Health. (1999). NZ food: NZ people: Key results of the 1997 national nutrition survey. Wellington, New Zealand: Author. Ministry of Health. (2000). The New Zealand Health Strategy: Discussion Document. Wellington, New Zealand: Author. Ministry of Health. (2001a). The New Zealand disability strategy: Making a world of difference: Whakanui oranga. Wellington, New Zealand: Author. Ministry of Health. (2001b). The New Zealand health strategy. Wellington, New Zealand: Author. Ministry of Health. (2001c). The Primary Health Care Strategy. Wellington, New Zealand: Author. 287 Ministry of Health. (2002a). Call for registration of interest - Primary health care nursing innovations funding. Wellington, New Zealand: Author. Ministry of Health. (2002b). A guide for establishing primary health organisations. Wellington, New Zealand: Author. Ministry of Health. (2002c). He korowai oranga: Maori health strategy. Wellington, New Zealand: Author. Ministry of Health. (2002d). Health of older people in New Zealand: A statistical reference. Wellington, New Zealand: Author. Ministry of Health. (2002e). The New Zealand health workforce: Framing future directions: Discussion document. Wellington, New Zealand: Health Workforce Advisory Committee. Ministry of Health. (2002f). Nurse Practitioners in New Zealand. Wellington, New Zealand: Author. Ministry of Health. (2003a). Funding for primary health care nursing scholarships. In Primary health care strategy. Retrieved April 29, 2005, from http://www.moh.govt.nz/moh.nsf/wpg_index/Primary+Health+Care+Publications+by+Title Ministry of Health. (2003b). Investing in health: Whakatohutia te oranga tangata: A framework for activating primary health care nursing in New Zealand. Wellington, New Zealand: Author. Ministry of Health. (2003c). Nutrition and the burden of disease: New Zealand 19972011. Wellington, New Zealand: Author. Ministry of Health. (2003d). NZ food NZ children: Key results of the 2002 national children's nutrition survey. Wellington, New Zealand: Author. 288 Ministry of Health. (2003e). Primary health care and community nursing workforce survey – 2001. Wellington, New Zealand: Author. Ministry of Health. (2003f). Tobacco facts 2003: Public Health Intelligence Occasional Report (No. 20). Wellington, New Zealand: Author. Ministry of Health. (2004a). Care plus: An overview. In Primary health care strategy. Retrieved April 29, 2005, from http://www.moh.govt.nz/moh.nsf/wpg_index/Primary+Health+Care+Care+Plus#overview Ministry of Health. (2004b). Guideline for specialist health services for older people. Wellington, New Zealand: Author. Ministry of Health. (2004c). Health expenditure trends in New Zealand 1990-2002. Wellington, New Zealand: Author. Ministry of Health. (2004d). A portrait of health: Key results of the 2002/03 New Zealand health survey. Wellington, New Zealand: Author. Ministry of Health. (2004e). Primary health care strategy implementation - Q&As. In Primary health care strategy. Retrieved April 29, 2005, from http://www.moh.govt.nz/moh.nsf/wpg_Index/AboutPrimary+Health+Care+Strategy+Implementation Ministry of Health. (2005). Primary health care nursing scholarships. Retrieved May 25, 2005, from http://www.moh.govt.nz/moh.nsf/0/8a26a197747fd6decc256fb8007ee02a?Op enDocument Ministry of Health, & Coopers & Lybrand. (1995). Co-ordinated care for Maori: Issues for development. Wellington, New Zealand: The Ministry. Ministry of Maori Development. (1999). Evaluation for Maori: Guidelines for government agencies. Wellington, New Zealand: Te Puni Kokiri. 289 Ministry of Social Development. (2002). The social report: Te purongo oranga tangata 2002. Wellington, New Zealand: Author. Ministry of Social Development. (2004). The social report: Te purongo oranga tangata 2004. Wellington, New Zealand: Author. Minnesota Department of Health. (2001). Public Health Interventions Applications for Public Health Nursing Practice. St. Paul, MN: Author. Minto, R. (2004). Nursing participation and governance in primary health organisation or talking primary health care, thinking primary care: Commentary 3. Vision EIT, 12(1), 12-13. Modrcin, M., Rapp, C. A., & Poertner, J. (1988). The evaluation of case management services with the chronically mentally ill. Evaluation and Program Planning, 11(4), 307-314. Naidoo, J., & Wills, J. (1994). Health promotion: Foundations for practice. London: Bailliere Tindall. National Health Committee. (1998). Social, economic and cultural determinants of health: Action to improve health. Wellington, New Zealand: National Advisory Committee on Health and Disability. National Health Committee. (2005). People with chronic conditions: A discussion paper. Wellington, New Zealand: National Advisory Committee on Health and Disability. Neuman, S., & McCormick, S. (Eds.). (1995). Single-subject experimental research: Applications for literacy. Newark, DE: International Reading Association. Neuman, W. (2000). Social research methods: Qualitative and quantitative approaches (4th ed.). Boston: Allyn and Bacon. 290 New Zealand Health Information Service. (2004). Nurses and midwives. In New Zealand workforce statistics 2004. Retrieved January 19, 2005, from http://www.nzhis.govt.nz/stats/nursestats-p.html New Zealand Steering Group to Oversee Health and Disability Changes. (1997). Implementing the coalition agreement on health: The report of the steering group to oversee health and disability changes. Wellington, New Zealand: Ministry of Health. Newell, K. W. (1975). Health by the people. Geneva, Switzerland: World Health Organization. Niessen, L. W. (2002). Roads to health: Multi-state modelling of population health and resource use. Amsterdam: Rozenberg Publishers/Dutch University Press. Nursing Council of New Zealand. (2001a). Framework for post-registration nursing practice education. Wellington: Author. Nursing Council of New Zealand. (2001b). The Nurse Practitioner. Wellington, New Zealand: Author. Nursing Council of New Zealand. (2002). Guidelines for cultural safety, the Treaty of Waitangi, and Maori health in nursing and midwifery education and practice. Wellington, New Zealand: Nursing Council of New Zealand. Nursing Council of New Zealand. (2004). Health Practitioners Competence Assurance Act 2003. Retrieved March 5, 2005, from http://www.nursingcouncil.org.nz/hpca.html Oakley, A. (1981). Interviewing women: A contradiction in terms. In H. Roberts (Ed.), Doing feminist research (pp. 30-61). London: Routledge & Kegan Paul. Oksenberg, L., Cannell, C., & Kalton, G. (1991). New strategies for pretesting survey questions. Journal of Official Statistics, 7(3), 349-366. 291 Ovretveit, J. (1998, March 1). Integrated care: Models and issues. Health Care & Informatics Review Online, 2(5). Retrieved May 2, 2004, from http://www.enigma.co.nz/hcro/website/index.cfm?fuseaction=articledisplay& FeatureID=29 Papenhausen, J. L. (1990). Case management: A model of advanced practice? Clinical Nurse Specialist, 4(4), 169-170. Parry, G. (1982). A fence at the top: The first 75 years of the Plunket Society. Dunedin, New Zealand: Royal New Zealand Plunket Society. Parsons, M., Anderson, C., Senior, H., & Jacobs, S. (2004, Autumn). Ageing in place: Is this a viable alternative to residential homes in New Zealand? Agendas. Pattison, S. (2000). A critique of pastoral care (3rd ed.). London: SCM Press. Pearson, G. (1973). Social work as the privatized solution of public ills. British Journal of Social Work, 3(2), 209-227. Pert, H. (1998). Experience with integration initiatives in New Zealand – A GP perspective. Healthcare Review Online, 2(10). Retrieved November 7, 2004, from http://hcro.enigma.co.nz/website/index.cfm?fuseaction=articledisplay&Featur eID=45 Petersen, S., Peto, V., Scarborough, P., & Rayner, M. (2005). Economic costs. In Coronary heart disease statistics (13th ed., pp. 197-200). London: British Heart Foundation. Peto, R., Lopez, A. D., Boreham, J., Thun, M., & Heath, C. (1994). Mortality from smoking in developed countries, 1950-2000: Indirect estimates from national vital statistics. Oxford, United Kingdom: Oxford University Press. Petrou, S. (1998). Health needs assessment is not required for priority setting. BMJ, 317(7166), 1154. 292 Phillips, D. C., & Burbules, N. C. (2000). Postpositivism and educational research. Lanham, MD: Rowman & Littlefield Publishers. Pomare, E. W., Keefe-Ormsby, V., Ormsby, C., Pearce, N., Reid, P., Robson, B., et al. (1995). Hauora, Maori standards of health. III: A study of the years, 19701991. Wellington, New Zealand: Te Ropu Rangahau Hauora a Eru Pomare/Eru Pomare Maori Health Research Centre. Porter-O'Grady, T. (1999). Sustainable partnerships: The journey toward health care integration. In E. L. Cohen & V. De Back (Eds.), The outcomes mandate: Case management in health care today (pp. 2-11). St Loius, MO: Mosby. Powles, J. (1973). On the limitations of modern medicine. Science, Medicine, & Man, 1(1), 1-30. Powles, J. (1988). Professional hygienists and the health of the nation. In R. MacLeod (Ed.), The Commonwealth of science: ANZAAS and the scientific enterprise in Australasia 1888-1988 (pp. 292-307). Auckland, New Zealand: Oxford University Press. Powney, J., & Watts, M. (1987). Interviewing in educational research. London: Routledge & Kegan Paul. Prochaska, J. O., & DiClemente, C. C. (1984). The transtheoretical approach: Crossing traditional boundaries of therapy. Homewood, IL: Dow Jones-Irwin. Protemix. (2003). Media Release - 16 November 2003. Retrieved February 21, 2005, from http://www.protemix.co.nz/corporate/Article.asp?id=8 Puetz, B. E., & Shinn, L. J. (1997). The nurse consultant's handbook. New York: Springer Pub. Co. Radical Therapist-Rough Times Collective. (1974). The Radical therapist. Harmondsworth, United Kingdom: Penguin. 293 Raeburn, J. (1996, June 17-19). How effective is strengthening community action as a strategy for health promotion. Paper presented at the First International Symposium on Health Promotion Effectiveness, University of Toronto, Ontario, Canada. Raeburn, J., & Rootman, I. (1997). People-centred health promotion. Chichester, United Kingdom: John Wiley. Rea, H., McAuley, S., Stewart, A., Lamont, C., Roseman, P., & Didsbury, P. (2004). A chronic disease management programme can reduce days in hospital for patients with chronic obstructive pulmonary disease. Internal Medicine Journal, 34(11), 608-614. Reamy, J. (1995). Health service regionalization in New Brunswick, Canada: A bold move. International Journal of Health Services, 25(2), 271-282. Rice, D. P., Kelman, S., & Miller, L. S. (1992). The economic burden of mental illness. Hospital & Community Psychiatry, 43(12), 1227-1232. Rifkin, S. B., & Walt, G. (1986). Why health improves: Defining the issues concerning 'comprehensive primary health care' and 'selective primary health care'. Social Science & Medicine, 23(6), 559-566. Robson, C. (1993). Real world research: A resource for social scientists and practitioner-researchers. Oxford, UK: Blackwell. Rodmell, S., & Watt, A. (1986). The Politics of health education: Raising the issues. London: Routledge & Kegan Paul. Rogers, C. (1969). Freedom to learn: A view of what education might become. Columbus, OH: C. E. Merrill Pub. Co. Rogers, W. (1991). Explaining health and illness: An exploration of diversity. New York: Harvester Wheatsheaf. 294 Room, G. (1979). The sociology of welfare: Social policy, stratification and political order. Oxford: Blackwell/Martin Robertson. Rosen, G. (1958). A history of public health. New York: MD Publications. Rothman, A. A., & Wagner, E. H. (2003). Chronic illness management: What is the role of primary care? Annals of Internal Medicine, 138(3), 256-261. Rotter, J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General & Applied, 80(1), 1-28. Russell, M., Cumming, J., Slack, A., Paterson, D., & Gilbert, A. (2003). Integrated care: Reflections from research. In R. Gauld (Ed.), Continuity amid chaos: Health care management and delivery in New Zealand (pp. 201-213). Dunedin, New Zealand: University of Otago Press. Saggers, S., & Gray, D. (1991). Aboriginal health and society: The traditional and contemporary Aboriginal struggle for better health. North Sydney, Australia: Allen & Unwin. Scarrow, H. A. (1972). The impact of British domestic air pollution legislation. British Journal of Political Science, 2(3), 261-282. Schon, D. A. (1983). The reflective practitioner: How professionals think in action. New York: Basic Books. Schrijvers, G. (2001, November). In pursuit of evidence based integrated care. International Journal of Integrated Care, 1. Retrieved September 16, 2003, from http://www.ijic.org/publish/articles/000060/article_toc.html Schuman, H., & Presser, S. (1981). Questions and answers in attitude surveys: Experiments on question form, wording, and context. New York: Academic Press. 295 Scott, G. (1997, August 1). Integrating purchasing and integrating care. Health Care & Informatics Review Online, 2(1). Retrieved May 4, 2004, from http://www.enigma.co.nz/hcro/website/results/200501121402444100982.pdf Shibuya, K., Mathers, C. D., Boschi-Pinto, C., Lopez, A. D., & Murray, C. J. (2002). Global and regional estimates of cancer mortality and incidence by site: II. Results for the global burden of disease 2000. BMC Cancer, 2(1), 37. Shipley, J. (1995). Advancing health in New Zealand. Wellington, New Zealand: New Zealand Government. Shobhana, R., Rama Rao, P., Lavanya, A., Williams, R., Vijay, V., & Ramachandran, A. (2000). Expenditure on health care incurred by diabetic subjects in a developing country--a study from southern India. Diabetes Research & Clinical Practice, 48(1), 37-42. Shortell, S. M., Gillies, R. R., Anderson, D. A., Erickson, K. M., & Mitchell, J. B. (1996). Remaking health care in America: Building organized delivery systems. San Francisco: Jossey-Bass Publishers. Slovic, P., & Gregory, R. (1999). Risk analysis, decision analysis, and the social context for risk decision making. In J. Shanteau, B. A. Mellers & D. A. Schum (Eds.), Decision science and technology: Reflections on the contributions of Ward Edwards (pp. 353-365). Boston, MA: Klumer Academic. Somerville, G. (1984). Community development in health: Addressing the confusions. London: King's Fund Centre. Statistics New Zealand. (2004). National Population Projections (2004(base) – 2051) - Hot Off The Press. Retrieved January 26, 2005, from http://www2.stats.govt.nz/domino/external/pasfull/pasfull.nsf/web/Hot+Off+T he+Press+National+Population+Projections+2004(base)+–+2051?open 296 Statistics New Zealand. (2005a). Births and Deaths (March 2005 quarter) - Media Release: Birth rates for older women continue to rise. Retrieved May 26, 2005, from http://www2.stats.govt.nz/domino/external/pasfull/pasfull.nsf/web/Media+Rel ease+Births+and+Deaths+March+2005+quarter?open Statistics New Zealand. (2005b). Future Pacific population - Summary of latest trends. In Population monitor. Retrieved May 27, 2005, from http://www.stats.govt.nz/popn-monitor/future-pacific-popn/future-pacific-popsummary-latest-trends.htm Stein, L. I., & Test, M. A. (1980). Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry, 37(4), 392-397. Stewart, J., & Thomas, S. (2004). Health promotion in context. Environmental Health Journal: EHJ, 112(12), 382-384. Stock, S., Redaelli, M., Luengen, M., Wendland, G., Civello, D., & Lauterbach, K. W. (2005). Asthma: Prevalence and cost of illness. European Respiratory Journal, 25(1), 47-53. Stonehouse, E. A. (1972). In the name of Nurse Maude. Christchurch, New Zealand: Nurse Maude District Nursing Association. Talbot, L., & Verrinder, G. (2005). Promoting health: The primary health care approach (3rd ed.). Marrickville, NSW, Australia: Elsevier Australia. Tanur, J. M. (Ed.). (1992). Questions about questions: Inquiries into the cognitive bases of surveys. New York: Russell Sage Foundation. Tarimo, E., & Webster, E. G. (1994). Primary health care concepts and challenges in a changing world: Alma-Ata revisited. Geneva, Switzerland: Division of Strengthening of Health Services, World Health Organization. 297 Taylor-Gooby, P., & Dale, J. (1981). Social theory and social welfare. London: Edward Arnold. Tesh, S. N. (1988). Hidden arguments: Political ideology and disease prevention policy. New Brunswick, NJ: Rutgers University Press. The Robert Wood Johnson Foundation. (2000). Patient education and consumer activation in chronic disease. In Meeting Proceedings. Retrieved June 20, 2003, from http://www.rwjf.org/files/publications/other/PatientEducation.pdf Thomas, B., & Lovell, K. (1999). Mental health nursing and case management in Great Britain. In E. L. Cohen & V. De Back (Eds.), The outcomes mandate: Case management in health care today (pp. 112-121). St Louis, MO: Mosby. Tobacco in New Zealand. (n.d.). In National Drug Policy New Zealand. Retrieved June 3, 2005, from http://www.ndp.govt.nz/publications/tobaccofacts2003.html Tones, B. (1986). Health education and the ideology of health promotion: A review of alternative approaches. Health Education Research, 1(1), 3-12. Tones, K., & Tilford, S. (1994). Health education: Effectiveness, efficiency, and equity (2nd ed.). London: Chapman & Hall. Tones, K., Tilford, S., & Robinson, Y. (1990). Health education: Effectiveness and efficiency. London: Chapman and Hall. Toop, L. J., Nuthall, J. J., & Hodges, I. D. (1996). Primary care teamwork in the Christchurch area: Part 2: Barriers to greater collaboration. New Zealand Family Physician, 23(6), 51-59. Townsend, P., Phillimore, P., & Beattie, A. (1988). Health and deprivation: Inequality and the North. London: Croom Helm. 298 Transitional Health Authority. (1997). Discussion paper on integrated care. Wellington, New Zealand: Author. Tschudin, V. (1995). Models for counselling. In Counselling skills for nurses (4th ed., pp. 38-55). London: Baillière Tindall. Tsouros, A. (1995). The WHO Healthy Cities project: State of the art and future plans. Health Promotion International, 10:(2), 133–141. Turnock, B. J. (2001). Public health: What it is and how it works. Gaithersburg, MD: Aspen Publishers. Ulschak, F. L., & SnowAntle, S. M. (1990). Consultation skills for health care professionals: How to be an effective consultant within your organization. San Francisco: Jossey-Bass Publishers. Upton, S., & New Zealand Department of Health. (1991). Health policy: Your health and the public health: Summary: A statement of government health policy. Wellington, New Zealand: Minister of Health. Wadsworth, Y. (1997). Do it yourself social research (2nd ed.). St. Leonards, NSW, Australia: Allen & Unwin. Walkerdine, V. (1984). Developmental psychology and the child-centred pedagogy. In J. Henriques, W. Hollway, C. Urwin, C. Venn & V. Walkerdine (Eds.), Changing the subject: Psychology, social regulation and subjectivity (pp. 153202). London: Methuen. Walsh, J. A., & Warren, K. S. (1979). Selective primary health care: An interim strategy for disease control in developing countries. New England Journal of Medicine, 301(18), 967-974. 299 Wano, H. (2003). Tui Ora Limited: A Taranaki experience in Maori health development. In R. Gauld (Ed.), Continuity amid chaos: Health care management and delivery in New Zealand (pp. 151-167). Dunedin, New Zealand: University of Otago Press. Warden, J. (1998). Britain's new health policy recognises poverty as major cause of illness. BMJ, 316(7130), 495. Weight-control Information Network. (2004). Economic costs related to overweight and obesity. In Statistics Related to Overweight and Obesity. Retrieved May 25, 2005, from http://win.niddk.nih.gov/statistics/#econ Weil, M., & Karls, J. M. (1985). Case management in human service practice. San Francisco: Jossey-Bass Publishers. Wells, K. P. (1998, September 1). Assessing integrated care as a solution for New Zealand. Health Care & Informatics Review Online, 2(11). Retrieved May 4, 2004, from http://www.enigma.co.nz/hcro/website/results/2005011214393051000985.pdf Werner, D., Sanders, D., Weston, J., Babb, S., & Rodriguez, B. (1997). Questioning the solution: The politics of primary health care and child survival with an indepth critique of oral rehydration therapy. Palo Alto, CA: HealthWrights. Wilkinson, R., & Marmot, M. G. (2003). Social determinants of health: The solid facts. Copenhagen, Denmark: World Health Organization, Regional Office for Europe. Wilkinson, W., & Sidel, V. W. (1991). Social applications and interventions in public health. In W. W. Holland, R. Detels & G. Knox (Eds.), Oxford textbook of public health (2nd ed., pp. 47-70). Oxford, United Kingdom: Oxford University Press. Williams, A. (2000). Nursing, medicine, and primary care. Philadelphia: Open University Press. 300 Wilson, D. (1996). Where do we go from here? The 72 billion dollar question. In M. Stingl & D. Wilson (Eds.), Efficiency versus equality: Health reform in Canada (pp. 165-177). Halifax, Novi Scotia, Canada: Fernwood Publications. Wilson-Barnett, J. (1988). Patient teaching or patient counselling? Journal of Advanced Nursing, 13(2), 215-222. Wilton, P., & Smith, R. D. (1998). Primary care reform: A three country comparison of 'budget holding'. Health Policy, 44(2), 149-166. Woods, K. J. (2001, April-June). The development of integrated health care models in Scotland. International Journal of Integrated Care, 1, 1-13. Retrieved August 12, 2004, from http://www.ijic.org/publish/articles/000033/article_print.html World Bank. (1993). World development report 1993: Investing in health: World development indicators. Oxford, United Kingdom: Oxford University Press. World Health Organization. (1978). Declaration of Alma-Ata. Retrieved May 5, 2001, from http://www.euro.who.int/AboutWHO/Policy/20010827_1 World Health Organization. (1985). Target for health for all. Copenhagen, Denmark: World Health Organization Regional Office for Europe. World Health Organization. (1986). Ottawa charter for health promotion. Geneva, Switzerland: Author. World Health Organization. (1992). Twenty steps for developing a Healthy Cities project. Copenhagen, Denmark: WHO Regional Office for Europe. World Health Organization. (1997). The Jakarta declaration on leading health promotion into the 21st century. Jakarta, Indonesia: Author. World Health Organization. (2000). The world health report 2000 - Health systems: Improving performance. Geneva, Switzerland: Author. 301 World Health Organization. (2001a). Innovative care for chronic conditions. Geneva, Switzerland: Author. World Health Organization. (2001b). Report of the commission on macroeconomics and health: Macroeconomics and health: Investing in health for economic development. Geneva, Switzerland: Author. World Health Organization. (2002a). Innovative care for chronic conditions: Building blocks for action. Geneva, Switzerland: Author. World Health Organization. (2002b). The World health report 2002: Reducing risks, promoting healthy life. Geneva, Switzerland: Author. World Health Organization. (2003). The World Health report 2003: Shaping the future. Geneva, Switzerland: Author. Zerwekh, J. V. (1992). Public health nursing legacy: Historical practical wisdom. Nursing & Health Care, 13(2), 84-91. 302 Appendices 303 Appendix 1 Structure of the New Zealand Health and Disability Support Sector 1999 304 305 Appendix 2 Structure of the New Zealand Health and Disability Support Sector 2005 306 307 Appendix 3 Questionnaire 308 Study Code Number: Today’s Date: / / HEALTH SYSTEMS & NURSING RESEARCH Day Month Year Interview Questionnaire Thank you for agreeing to take part If you have any concerns, please do not hesitate to contact: Nicolette Sheridan Department of Community Health, Telephone: 09 373 7599 extension 87811 The first questions asks about your role in the integrated care project 1. What is your full name? ______________________________________________________________ 2. Who is your employer? ______________________________________________________________ 3. What is your primary role in the project? ______________________________________________________________ ALL of the following questions ask about the integrated care project 4. What is the title of the project? ______________________________________________________________ 5. Who are the organisations in partnership in the project? ______________________________________________________________ 6. What is the purpose of the project? ______________________________________________________________ 7. Does the project achieve this purpose? ______________________________________________________________ 8. Does the project plan to deliver a new health service? Yes No If you answered yes, how does the project plan to deliver a new health service? ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 309 9. Has the project delivered an existing health service differently? Yes No If you answered yes, how does the present health service differ from the service provided before the project begun? ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 10. Does the project provide any of the following health care services? Screening and prevention Health promotion Diagnostic tests and expert advice Treatment and follow-up Rehabilitation 11. Yes Yes Yes Yes Yes No No No No No Answer this question only if one or more general practice organisations are partners in the project. In your view, are there incentives for general practice to be a partner in the project? Yes No If you answered yes which one of the following, in your view, is the main incentive for general practice to be a partner in the project? Generate income Plan and/or deliver new health services Improve existing health services Gain new skills Another incentive (specify) ______________________________________ 12. Answer this question only if one or more hospital organisations are partners in the project. In your view, are there incentives for the hospital to be a partner in the Yes No project? If you answered yes which one of the following, in your view, is the main incentive for the hospital to be a partner in the project? Generate income Plan and/or deliver new health services Improve existing health services Reduce hospital admissions Another incentive (specify) ______________________________________ 310 13. Does the project target a specific ethnic group? Yes No If you answered yes which one of the following ethnic groups was targeted? Maori Pacific Maori and Pacific Another ethnic group (specify) __________________________________ Does the project target this ethnic group only, or this ethnic group and the wider population. Ethnic group only Ethnic group and the wider population 14. Does the project target a geographic area? Yes No If you answered yes what geographic area was targeted? ______________________________________________________________ ______________________________________________________________ 15. Does the project target a specific age group? Yes No If you answered yes, which one of the following age groups was targeted? 0-20 21-55 Over 55 All ages 16. In this question, ‘condition’ refers to a state that is not a disease, such as pregnancy. Does the project target a disease or condition? Yes No If you answered yes what disease or condition was targeted? ______________________________________________________________ What approach was taken to address the disease or condition? ______________________________________________________________ If you answered no what issue was targeted? ______________________________________________________________ What approach was taken to address the issue targeted? ______________________________________________________________ 311 17. Which one of the following levels of approach was adopted by the project? Individuals and families Communities System Combination of any of the above (specify) __________________________ ______________________________________________________________ 18. Which of the following project strategies were used to achieve integration? Clinical guideline development Clinical guideline promotion Case management Database development Another strategy Yes Yes Yes Yes Yes No No No No No If you answered another strategy how was integration achieved? ______________________________________________________________ If you answered clinical guideline development who developed the guideline? _____________________________________________________ If you answered clinical guideline promotion how were they promoted? ______________________________________________________________ If you answered case management who was the case manager? ______________________________________________________________ 19. Has the project received dedicated funding? Yes No If you answered yes who provided the main funding to the project? ______________________________________________________________ ______________________________________________________________ 20. In your view, are financial incentives offered to project partners who provide health services within the project? Yes No 21. In you view, are material incentives offered to clients (or patients) who participate in the project? Yes No If you answered yes what material incentives were offered to clients? ______________________________________________________________ ______________________________________________________________ 22. Answer this question only if one or more general practice organisations are partners in the project. 312 In your view, did general practice incur financial costs as a result of participating in the project? Yes No 23. Answer this question only if one or more hospital organisations are partners in the project. In your view, did the hospital incur financial costs as a result of participating in the project? Yes No 24. In this question, ‘non-nursing personnel’ refers to all project personnel, excluding nurses. Does the project employ dedicated non-nursing personnel? Yes No If you answered yes describe the practice of non-nursing personnel. ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 25. In this question, ‘nurse’ refers only to registered general or comprehensive (or equivalent) trained nurses. Does the project employ nurses? Yes No If you answered yes continue with the following question, which asks about seventeen interventions or activities that may have been undertaken by nurses in the project. A definition of each intervention will be read to you, before you are asked to decide whether this intervention was undertaken and give a yes/no response. Surveillance Disease and health event investigation Outreach Screening Case finding Yes Yes Yes Yes Yes No No No No No Referrals and follow-up Case management Delegated functions Yes No Yes No Yes No Health teaching Counselling Consultation Yes No Yes No Yes No Collaboration Coalition building Community organising Yes No Yes No Yes No 313 Yes No Yes No Yes No Advocacy Social marketing Policy development and enforcement 26. Each of the seventeen interventions listed above can be undertaken at three levels of population-based practice. These levels are: individual and family, community, and systems. Use the following scale to select one option: (1) individual and family; (2) community; (3) system, and (4) combination of 1 and/or 2 and/or 3. For each yes response in question 25, where you indicated a particular intervention was undertaken by nurses in the project, you are now asked to decide the level of population-based practice of that intervention. Individual Community System Combination & family 27. Intervention 1 2 3 4 (specify) Surveillance Disease and health event investigation Outreach Screening Case finding 1 1 1 1 1 2 2 2 2 2 3 3 3 3 3 4 _______ 4 _______ 4 _______ 4 _______ 4 _______ Referrals and follow-up Case management Delegated functions 1 1 1 2 2 2 3 3 3 4 _______ 4 _______ 4 _______ Health teaching Counselling Consultation 1 1 1 2 2 2 3 3 3 4 _______ 4 _______ 4 _______ Collaboration Coalition building Community organising 1 1 1 2 2 2 3 3 3 4 _______ 4 _______ 4 _______ Advocacy Social marketing Policy development and enforcement 1 1 1 2 2 2 3 3 3 4 _______ 4 _______ 4 _______ If you would like to offer any other comment, please indicate below. ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ Thank you for taking part in this study 314 Appendix 4 Interventions undertaken by nurses in integrated care projects: Frequency tables 315 Screening intervention undertaken by nurses in projects Individual Community Systems Total No. projects 23 8 3 Ethnic Group Low Income Maori (%) Low decile area (%) 17 (77.3) 7 (87.5) 2 (66.7) 13 (56.5) 6 (75) 0 (0) Disease/Condition or Well-health Chronic (%) 5 (21.7) 3 (37.5) 0 (0) Well-health (%) 13 (56.5) 3 (37.5) 2 (66.7) Outreach intervention undertaken by nurses in projects Individual Community Systems Total No. projects 22 9 1 Ethnic Group Low Income Maori (%) Low decile area (%) 17 (77.3) 8 (88.8) 1 (100) 12 (54.5) 7 (77.8) 0 (0) Disease/Condition or Well-health Chronic (%) Well-health (%) 12 (54.5) 3 (33.3) 0 (0) 7 (31.8) 5 (55.6) 0 (0) Disease and health event investigation intervention undertaken by nurses in projects Individual Community Systems Total No. projects 14 1 5 Ethnic Group Low Income Disease/Condition or Well-health Maori (%) Low decile area (%) Chronic (%) Well-health (%) 9 (64.2) 1 (100) 3 (60) 4 (28.6) 0 (0) 0 (0) 6 (42.9) 0 (0) 4 (80) 6 (42.9) 1 (100) 0 (0) Advocacy intervention undertaken by nurses in projects Individual Community Systems Total No. projects 29 13 3 Ethnic Group Low Income Maori (%) Low decile area (%) 20 (67) 12 (92.3) 2 (66.7) 15 (51.7) 10 (76.9) 1 (33.3) Disease/Condition or Well-health Chronic (%) Well-health (%) 17 (58.6) 4 (30.8) 0 (0) 6 (20.7) 6 (46.2) 1 (33.3) Social marketing intervention undertaken by nurses in projects Individual Community Systems Total No. projects 12 4 0 Ethnic Group Low Income Maori (%) Low decile area (%) 10 (83.3) 3 (75) 0 (0) 10 (83.3) 2 (50) 0 (0) Disease/Condition or Well-health Chronic (%) Well-health (%) 5 (41.7) 3 (75) 0 (0) 6 (50) 1 (25) 0 (0) Policy development and enforcement intervention undertaken by nurses in projects Individual Community Systems Total No. projects 24 6 0 Ethnic Group Low Income Maori (%) Low decile area (%) 20 (83.3) 6 (100) 0 (0) 10 (41.7) 4 (66.7) 0 (0) Disease/Condition or Well-health Chronic (%) 15 (62.5) 3 (50) 0 (0) Well-health (%) 6 (25) 2 (33.3) 0 (0) 316 Collaboration intervention undertaken by nurses in projects Individual Community Systems Total No. projects 30 13 1 Ethnic Group Low Income Maori (%) Low decile area (%) 21 (70) 12 (92.3) 1 (100) Disease/Condition or Well-health Chronic (%) 15 (50) 10 (76.9) 0 (0) 18 (60) 4 (30.8) 0 (0) Well-health (%) 7 (23.3) 6 (46.2) 1 (100) Consulting intervention undertaken by nurses in projects Individual Community Systems Total No. projects 31 2 7 Ethnic Group Low Income Maori (%) Low decile area (%) 21 (67.7) 2 (100) 0 (0) Disease/Condition or Well-health Chronic (%) 16 (51.6) 0 (0) 2 (28.6) 18 (58.1) 0 (0) 3 (42.9) Well-health (%) 7 (22.6) 1 (50) 0 (0) Counselling intervention undertaken by nurses in projects Individual Community Systems Total No. projects 29 3 0 Ethnic Group Low Income Maori (%) Low decile area (%) 19 (65.5) 2 (66.7) 0 (0) Disease/Condition or Well-health Chronic (%) 14 (48.3) 2 (66.7)) 0 (0) 18 (62.1) 3 (100) 0 (0) Well-health (%) 6 (20.7) 0 (0) 0 (0) Delegated functions intervention undertaken by nurses in projects Individual Community Systems Total No. projects 29 1 0 Ethnic Group Low Income Maori (%) Low decile area (%) 21 (72.4) 1 (100) 0 (0) 16 (55.2) 0 (0) 0 (0) Disease/Condition or Well-health Chronic (%) 17 (58.6) 0 (0) 0 (0) Well-health (%) 7 (24.1) 0 (0) 0 (0) Case management intervention undertaken by nurses in projects Individual Community Systems Total No. projects 30 0 7 Ethnic Group Low Income Maori (%) Low decile area (%) 21 (70) 0 (0) 0 (0) 16 (53.3) 0 (0) 2 (28.6) Disease/Condition or Well-health Chronic (%) 17 (56.7) 0 (0) 2 (28.6) Well-health (%) 7 (23.3) 0 (0) 0 (0) Referral and follow-up intervention undertaken by nurses in projects Individual Community Systems Total No. projects 30 0 0 Ethnic Group Low Income Maori (%) Low decile area (%) 21 (70) 0 (0) 0 (0) 16 (53.3) 0 (0) 0 (0) Disease/Condition or Well-health Chronic (%) 17 (56.7) 0 (0) 0 (0) Well-health (%) 7 (23.3) 0 (0) 0 (0) 317 318