Hirschsprung disease: a developmental disorder of the enteric
advertisement

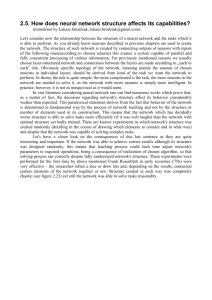
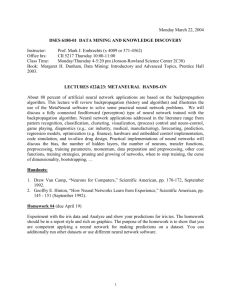
Focus Article Hirschsprung disease: a developmental disorder of the enteric nervous system Sonja J. McKeown,1 Lincon Stamp,1,2 Marlene M. Hao1 and Heather M. Young1∗ Hirschsprung disease (HSCR), which is also called congenital megacolon or intestinal aganglionosis, is characterized by an absence of enteric (intrinsic) neurons from variable lengths of the most distal bowel. Because enteric neurons are essential for propulsive intestinal motility, infants with HSCR suffer from severe constipation and have a distended abdomen. Currently the only treatment is surgical removal of the affected bowel. HSCR has an incidence of around 1:5,000 live births, with a 4:1 male:female gender bias. Most enteric neurons arise from neural crest cells that emigrate from the caudal hindbrain and then migrate caudally along the entire gut. The absence of enteric neurons from variable lengths of the bowel in HSCR results from a failure of neural crest-derived cells to colonize the affected gut regions. HSCR is therefore regarded as a neurocristopathy. HSCR is a multigenic disorder and has become a paradigm for understanding complex factorial disorders. The major HSCR susceptibility gene is RET. The penetrance of several mutations in HSCR susceptibility genes is sex-dependent. HSCR can occur as an isolated disorder or as part of syndromes; for example, Type IV Waardenburg syndrome is characterized by deafness and pigmentation defects as well as intestinal aganglionosis. Studies using animal models have shown that HSCR genes regulate multiple processes including survival, proliferation, differentiation, and migration. Research into HSCR and the development of enteric neurons is an excellent example of the cross fertilization of ideas that can occur between human molecular geneticists and researchers using animal models. © 2012 Wiley Periodicals, Inc. How to cite this article: WIREs Dev Biol 2013, 2:113–129. doi: 10.1002/wdev.57 INTRODUCTION I n 1888, Harald Hirschprung described two unrelated boys who died with abdominal distension, congenital megacolon, and severe chronic constipation.1 Although a number of studies from the early 1900s had implicated defects in neurons, the etiology of Hirschsprung disease (HSCR) was not identified until the mid-1900s when it was found that all postmortem samples of rectum from patients ∗ Correspondence to: h.young@unimelb.edu.au 1 Department of Anatomy & Cell Biology, University of Melbourne, Melbourne 3010, VIC, Australia 2 Murdoch Childrens Research Institute, Parkville 3052, VIC, Australia Volume 2, January/February 2013 with congenital megacolon lacked enteric (intrinsic) neurons.2 Overall, HSCR has an incidence of around 1:5000 live births, but there are differences in incidence between ethnic groups and there is a 4:1 male:female sex bias. HSCR can occur as an isolated disorder (70% of patients) or as part of a syndrome in which other neural crest derivatives are commonly affected. One of these syndromes, Type IV Waardenburg syndrome (WS4), is discussed in the section Type IV Waardenburg Syndrome (WS4)—An Example of a Syndrome That Includes Aganglionic Megacolon of this article. Between 2 and 15% of HSCR patients have the chromosomal abnormality, trisomy 21 (Down © 2012 Wiley Periodicals, Inc. 113 wires.wiley.com/devbio Focus Article in ENS development. This review briefly describes the ENS and the stages of ENS development relevant to HSCR. We then discuss the etiology, diagnosis, genetics, and current and potential treatments for HSCR, and finally we briefly discuss one of the syndromic forms of HSCR, WS4. D THE ENTERIC NERVOUS SYSTEM M R C A FIGURE 1 | Barium enema study, lateral view, of a 6-month-old infant with HSCR. The descending colon is greatly dilated (‘megacolon’) while the distal colon and rectum are constricted. (Reprinted with permission from Ref 5. Copyright 1999 Radiological Society of North America) syndrome).3 HSCR is a multigenic disorder with variable penetrance (see the section on Etiology below) and severity. In over 80% of cases, aganglionosis is restricted to the rectosigmoid colon (short-segment HSCR) (Figure 1), but aganglionosis can also affect significant lengths of the colon or even extend into the distal small intestine (long segment HSCR). Extremely rarely, the entire small and large intestines are aganglionic, which is termed total intestinal aganglionosis. A region of bowel with reduced enteric neuron density, the transition zone, is always present oral to the aganglionic region.4 The mechanisms controlling the development of the enteric nervous system (ENS) are highly conserved. Research into HSCR and ENS development has consequently benefitted greatly from the exchange of knowledge and ideas between human molecular geneticists and researchers using animal models, including mouse, chick, and zebrafish.6 Several HSCR susceptibility genes were first identified following studies on mice with targeted inactivation of particular genes that resulted in HSCR-like phenotypes. Likewise, genetic studies of HSCR patients identified genes that were not previously known to be involved 114 The ENS is an extensive network of neurons and glia within the wall of the bowel.7,8 The ENS is the largest part of the peripheral nervous system, and there are at least as many neurons in the gut as there are in the spinal cord.9 In the small and large intestines, enteric neurons are found in two main plexuses; the myenteric plexus is located between the circular and longitudinal muscle layers, and the submucosal plexus is found within the connective tissue of the submucosa. In humans, some neurons are also found within the mucosa.10 Neurons in myenteric ganglia are primarily involved in the control of motility whereas most submucosal neurons regulate transport of ions across the epithelium and blood flow. There are many different types of enteric neurons that differ in their targets, inputs, direction of projection, neurotransmitters, and electrophysiological characteristics. The neurons form circuits that regulate a number of gut functions, including motility. In the small and large intestines, enteric neurons are essential for all coordinated motor patterns including mixing and peristalsis. The essential role for enteric neurons in peristalsis is exemplified by the bowel obstruction that occurs in the aganglionic region of patients with HSCR. ORIGIN AND EARLY DEVELOPMENT OF THE ENTERIC NERVOUS SYSTEM Most enteric neurons arise from neural crest cells that emigrate from the neural tube adjacent to somites 1–711 (Figure 2). This region of the neural axis is called ‘vagal’, and encompasses the most caudal hindbrain (somites 1-5) and rostral trunk (somites 6-7). Sacral level neural crest cells also contribute some enteric neurons, but even in the most distal regions of the bowel, the majority of enteric neurons arise from vagal neural crest-derived cells.12–14 Studies in a variety of species, including human, have shown that vagal neural crest-derived cells enter the foregut and then migrate caudally along the gut16,17 (Figure 2). The colonization of the gastrointestinal tract by enteric neural crest-derived cells (ENCCs) is notable both because of the distance © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 Hirschsprung disease V WIREs Developmental Biology H H M FIGURE 2 | Immunostaining of E9.5 and E10.5 mice with antibodies to the neural crest cell marker, SOX10 (goat anti-SOX10, Santa Cruz). At E9.5, vagal neural crest-derived cells from the post-otic hindbrain are migrating ventrally toward and into the foregut (arrow ). At E10.5, the most caudal neural crest-derived cell is in the midgut (open arrow ). Neural crest cells that emigrate from the neural tube adjacent to somites 1–7 follow the pathway (dotted line ) that is followed later by the vagus nerve (X). The ectoderm was removed from the E10.5 mouse to enable the gut to be seen. OV, otic vesicle; BA1, branchial arch 1; BA2, branchial arch 2; asterisks, dorsal root ganglia; V, VII, IX, X—cranial nerves V, VII, IX and X. (Reprinted with permission from Ref 15. Copyright 2012 Elsevier) ENCCs migrate, and because of the length of time it takes. Because the gut grows substantially while it is being colonized, ENCCs probably migrate further than any other embryonic cell population.18 For example, in mice, the colon increases in length fivefold between when ENCC first enter the proximal colon and when they reach the distal end. In humans, it takes 3 weeks for ENCCs to migrate from the foregut to the anal end,17 and in mice it takes 5 days, which is 25% of the gestation period.16 ENS development continues after the gut has been colonized by ENCCs, and even beyond birth, at least in laboratory animals.19,20 In this article, however, we focus on the mechanisms involved in the early development of the ENS as HSCR is caused by a failure of ENCCs to colonize the entire gut. ENCCs proliferate rapidly while migrating toward and within the gut.21,22 Moreover, a subpopulation of ENCCs starts to undergo neuronal differentiation as they are migrating within the gut wall. The colonization of the gut by ENCCs requires coordinated proliferation, migration, and neuronal differentiation, as perturbations to cell number,21–23 migratory behavior,24,25 or rate of neuronal differentiation26–29 can result in aganglionosis in animal models. Although cell death is not prominent Volume 2, January/February 2013 while ENCCs are colonizing the gut,30,31 inhibition of cell death of chick vagal neural crest cells as they are migrating from the hindbrain toward the gut results in hyperganglionosis (increased density of enteric neurons),32 and cell death is common when RET signaling is conditionally abolished while ENCCs are migrating along the colon in mice.33 Many molecules involved in the colonization of the gut by ENCCs have been identified. These include molecules secreted by the gut mesenchyme that act on receptors expressed by ENCCs, as well as transcription factors, adhesion molecules and other molecules expressed by ENCCs themselves. Some of the signaling pathways involved in ENS development affect multiple processes including proliferation, migration, differentiation, and/or survival. Mutations in genes encoding components of many of these signaling pathways have been associated with HSCR (Table 1). Here we briefly summarize the main pathways and molecules known to play a role in the colonization of the gut by ENCCs. GDNF-GFRA1-RET Signaling Pathway This is a critical pathway for ENS development. Glial cell line-derived neurotrophic factor (GDNF) © 2012 Wiley Periodicals, Inc. 115 116 Frequency of Mutation in Isolated HSCR Isolated HSCR, Associated Syndrome, Phenotype © 2012 Wiley Periodicals, Inc. ∼5%48 Extremely rare (one family only and co-occurred with a RET mutation)44 Heterozygous44 NRTN HGNC:8007 Heterozygous EDNRB HGNC:3180 mutations47,48 Extremely rare (one family only, low penetrance, significance unknown)41 Very rare Extremely rare Heterozygous41 GFRA1 HGNC:4243 Heterozygous38 GDNF HGNC:4232 Homozygous missense36 Usually isolated,48 very occasional WS449,50 Isolated44 Isolated41 Isolated38 Isolated. Total intestinal aganglionosis36 Non-coding RET Non-coding mutations: Mostly isolated but HGNC:9967 mutations may be very common. Coding can also be homozygous or mutations: ∼50% of associated with a heterozygous; familial and 15–20% syndrome1 coding mutations of sporadic HSCR1 are heterozygous1 Gene Zygosity of Mutations in HSCR Patients TABLE 1 HSCR Susceptibility Genes and Mouse Models of HSCR Required for the normal projection, branching and/or survival of axons of enteric excitatory motor neurons45 EDNRB is a G EDN3-EDNRB signaling promotes protein-coupled receptor. proliferation and inhibits Main receptor for EDN3 neuronal differentiation of in ENS development. enteric neural progenitors, and Expressed by ENCCs and regulates ENCC some gut mesenchymal migration.26,29,53 EDN3-EDNRB 52 signaling is also involved in cells melanocyte development.54 Neurons are present along the Neurturin is a secreted entire gut of Nrtn−/− molecule; member of mice.45 Myenteric neuron GDNF family ligands. number is normal, but there Expressed by the are defects in submucosal mesenchyme of the neuron number and in the embryonic gut46 density of excitatory nerve fibers in Nrtn−/− mice30 Gfra1+/− mice have normal GPI-linked protein to which enteric neuron density;30 GDNF binds. Expressed Gfra1−/− mice lack neurons by ENCCs.43 42 distal to the stomach Ednrb s/sl mice have reduced neuron density in the colon (note: s is a hypomorphic mutation and sl is a null mutation).51 Role in ENS Development from Animal Studies RET tyrosine kinase. Survival, proliferation, migration, Expressed by ENCCs.34 and neuronal differentiation of Expression is maintained ENCCs6 in neurons but is down-regulated in glia.35 Expression Pattern in Mice Relevant to ENS Development Neurons are present along the Secreted molecule. entire gut of Gdnf +/− mice, Expressed by but at reduced density30 ; mesenchyme of Gdnf −/− mice lack enteric embryonic gut39 and neurons distal to the external muscle of stomach39 mature gut.40 Ret −/− mice lack neurons distal to the stomach37 Ret +/− mice have a normal ENS30 ENS Phenotype of Mouse Mutants Focus Article wires.wiley.com/devbio Volume 2, January/February 2013 Volume 2, January/February 2013 © 2012 Wiley Periodicals, Inc. Heterozygous SOX10 HGNC:11190 mutations49,68 or deletions69 Heterozygous SNPs Relatively in the coding common65 sequence that increase the risk of HSCR conferred by RET 65 NRG1 HGNC:7997 Edn3 −/− mice lack of neurons in the distal colon62 WS449,61 Sox10 homozygous null Transcription factor expressed by mutants lack neurons in the migrating neural crest cells entire gastrointestinal including ENCCs.70,74 Also 70,71 +/− Sox10 mice expressed by enteric glia and tract. lack enteric neurons in the glial progenitors, but is distal bowel, with the down-regulated upon enteric severity and penetrance of neuron differentiation.74 aganglionosis being strain-dependent.72,73 WS468,69 or PCWH49 Are multiple isoforms of neuregulin-1; type 1 is expressed in the dorsal neural tube at the time of neural crest cell emigration.67 ErbB2/ErbB3 receptors are expressed by migrating neural crest cells.67 Nrg1−/− mice die at E10.5 from heart defects.66 ECE1 is involved in the proteolytic processing of big endothelins to biologically active peptides. Expression of ECE-1 does not yet appear to have been examined in the developing gut. EDN3 is the main ligand for EDNRB in ENS development. Expressed by the mesenchyme of the embryonic gut with highest expression in the cecum27,60 Expression Pattern in Mice Relevant to ENS Development Isolated65 No reports of ENS defects in Ece1+/− mice. Ece1−/− mice lack neurons in the distal colon, lack epidermal melanocytes, and also exhibit craniofacial and cardiac defects64 Edn3 +/− mice have normal enteric neuron density59 Ednrb −/− mice lack of neurons in the distal colon54 ENS Phenotype of Mouse Mutants Isolated56 except one case of WS458 WS4; patients are deaf, have piebald pigment pattern, HSCR and neurological deficits49,55 Isolated HSCR, Associated Syndrome, Phenotype Very rare (one case Cardiac, craniofacial and autonomic reported63 ) defects, and HSCR63 <5%57 Heterozygous63 Mutations in both alleles61 Heterozygous mutations56 Mutations in both alleles49,55 Frequency of Mutation in Isolated HSCR ECE1 HGNC:3146 EDN3 HGNC:3178 Gene Zygosity of Mutations in HSCR Patients TABLE 1 Continued Required for survival and maintenance of neural crest stem/progenitors and the activation of Phox2b and Ret.75–77 Also required later in development for glial and melanocyte differentiation.78,79 ND Role in ENS Development from Animal Studies WIREs Developmental Biology Hirschsprung disease 117 118 © 2012 Wiley Periodicals, Inc. ND ENCC migration along the gut is slightly delayed in L1cam null mutants, but the entire gut is colonized.94 L1cam+/− mice have no reported ENS phenotype Goldberg–Shprintzen syndrome; patients have microcephaly, mental retardation, and facial dysmorphism. Most also have HSCR.89 X-linked hydrocephalus.92 Only a small percentage of patients also have HSCR.93 Homozygous89 L1CAM is on the X-chromosome KIAA1279 HGNC:23419 L1CAM HGNC:6470 Role in ENS Development from Animal Studies L1CAM is a cell adhesion molecule that is expressed by most ENCCs94 KIAA1279 encodes kinesin binding protein (KBP). Expression pattern of KBP not yet reported in mice. Transcription factor expressed by all ENCCs87 and in differentiated neurons and glia.88 Required for normal migration of ENCCs94 KBP promotes neurite formation and neuronal differentiation in zebrafish brain and spinal axons,90 and in CNS neurons in culture.91 Required for the activation of Ret.86 Transcription factor that is Required for the formation expressed by enteric neural of the vagal neural crest, progenitors and then by and also plays later roles enteric glia but is not in ENS development.83,84 expressed by enteric neurons.84 Also expressed by some mesenchymal cells in the developing gut.84 Expression Pattern in Mice Relevant to ENS Development CCHS, central congenital hypoventilation syndrome; ECE-1, endothelin-converting enzyme 1; EDN3, endothelin-3; EDNRB, endothelin receptor B; ENCC, enteric neural crest-derived cells; HGNC, HUGO Gene Nomenclature Committee; ND, not determined; PCWH, peripheral demyelinating neuropathy, central dysmyelinating leukodystrophy, Waardenburg syndrome and Hirschsprung’s disease; WS4, Waardenburg syndrome 4. CCHS (Ondine’s curse). Only Homozygous null mutants a small proportion of lack neurons throughout CCHS patients also have entire gastrointestinal HSCR.85 tract.86 Phox2b +/− mice have no reported ENS defects. Zeb2 −/− mice die at E9.5 and the vagal neural crest does not form.83 ENS Phenotype of Mouse Mutants Heterozygous for a polyalanine repeat expansion mutation85 Mowat–Wilson syndrome; patients have distinctive facial features, epilepsy, cardiac defects, mental retardation, and a range of other features including HSCR82 Isolated HSCR, Associated Syndrome, Phenotype PHOX2B HGNC:9143 Frequency of Mutation in Isolated HSCR Heterozyous nonsense or frameshift mutations80 or truncating mutations81 Zygosity of Mutations in HSCR Patients ZEB2 (formerly known as ZFHX1B, SIP1) HGNC:14881 Gene TABLE 1 Continued Focus Article wires.wiley.com/devbio Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease belongs to a family of four secreted neurotrophic factors that bind to GPI-anchored cell surface proteins called GDNF family receptor alphas (GFRAs).95 The GDNF family ligand–GFRA complex activates the RET tyrosine kinase.96 GDNF preferentially binds to GFRA1. GDNF is first expressed by the gut mesenchyme shortly before vagal neural crest cells enter the foregut,97 while RET and GFRA1 are expressed by ENCCs. Gdnf −/− , Gfra1−/− , and Ret−/− mice lack neurons in the small and large intestines, and from most of the stomach37,42,98 (Table 1). In vivo and in vitro studies have shown that the GDNFGFRA1-RET signaling pathway is essential for the survival, proliferation, migration, and differentiation of ENCCs.26,43,99–102 Increasing RET signaling by inactivation of negative regulators of RET signaling, or by increasing GDNF availability, results in an increased number of enteric neurons.103–105 There are two main isoforms of RET, which differ in their C-terminal domains, and are generated by alternate splicing, RET9 and RET51. Although one study found that RET9 was critical for colonization of the distal bowel by ENCCs, but RET51 was not essential,106 another group subsequently found that mice expressing only RET9 did not exhibit aganglionosis.107,108 This disparity is probably due to differences in the transgenes or strains used by the two different laboratories. Neurturin-GFRA2-Ret Signaling Pathway Neurturin (NRTN) belongs to the GDNF family ligands and binds to GFRA2 to activate RET. Neurons are present along the entire gastrointestinal tract of Nrtn and Gfra2 homozygous null mutant mice; the number of myenteric neurons is normal, but the density of excitatory nerve fibers is reduced.30,109 Thus, NRTN-GFRA2-Ret signaling promotes the projection or branching of axons from some classes of enteric neurons. Although studies in mice have not revealed a role for NRTN signaling in colonization of the gut by ENCCs, a mutation in NRTN has been found in one family with HSCR (see the section on Genetics below). Endothelin 3-Endothelin Receptor B Signaling Pathway Endothelin 3 (EDN3) is a ligand for the G proteincoupled receptor, endothelin receptor B (EDNRB). Edn3 is expressed by the gut mesenchyme, with highest levels in the cecum.27,60 Ednrb is expressed by ENCCs and some gut mesenchymal cells.52 Mice lacking EDN3 or EDNRB exhibit colonic aganglionosis62 (Figure 3) resulting from a delay in the entry of vagal neural crest-derived cells into the gut as well as reduced speed of colonization of the gut by ENCCs.25,27 Volume 2, January/February 2013 (a) A S A C C M (b) (c) T (d)A FIGURE 3 | Mouse model of HSCR. (a) Intestine from a 2-week-old Edn3 −/− mouse. The mid-colonic region is distended and termed a ‘mega-colon’. (b–d) Whole mount preparations of the external muscle of colonic wall from the regions indicated in (a) showing immunostaining with an antibody to the pan-neuronal marker, Hu. Neurons, which are clustered into ganglia, are present in the distended region (b), but are totally absent from the distal colon (d). There is a transition zone of reduced neuron density proximal to the aganglionic region (c). Scale bar = 100 μm (applies to b–d). Studies in vivo and in vitro have shown that signaling via EDNRB promotes the colonization of the gut by ENCCs by promoting the proliferation and inhibiting the neuronal differentiation of neural progenitors,26,28,29,110 and by directly promoting ENCC migration.25 EDN3-EDNRB signaling is also required for melanocyte development, as mice null for Ednrb or Edn3 have pigmentation abnormalities as well as colonic aganglionosis (WS4 phenotype, see the section on Type IV Waardenburg Syndrome (WS4)—An Example of a Syndrome That Includes Aganglionic Megacolon below), whereas Edn3 heterozygotes have no abnormalities and Ednrb heterozygous and hypomorphic mutants typically only have pigmentation abnormalities.28,49 Hence melanocyte precursors and ENCCs appear to have different dosage requirements for EDN3/EDNRB signaling, with melanocytes having a lower minimal threshold. Transcription Factors A network of transcription factors controls ENS development.111 Here we very briefly review the © 2012 Wiley Periodicals, Inc. 119 wires.wiley.com/devbio Focus Article roles of SOX10, PHOX2B, and ZEB2 (formerly known as ZFHX1B and SIP1), as mutations in the genes encoding these molecules are associated with HSCR (Table 1). However, FOXD3, HAND2, ASCL1 (formerly known as MASH1), PAX3, HLX, and the TFAP2 (formerly known as AP-2) family also play a role in ENS development. Sox10 is expressed prior to, and during, neural crest migration.70 Sox10−/− mice die at birth, and in null mutant embryos, vagal neural crest cells die around E9, prior to their entry into the gut.71 SOX10 plays an essential role in ENS development most likely because it is necessary for the expression of Ret and Phox2b, and because it maintains the multipotency of neural crest cell stem/progenitors.75,76,112,113 The expression of Sox10 is down-regulated by ENCCs that differentiate into neurons, but Sox10 expression is maintained in enteric glia and is required for glial fate acquisition.35,78 In the neural crest-derived melanocyte progenitors that migrate into the ectoderm, SOX10 regulates the expression of MITF, a key transcription factor required for melanocyte development, as well as genes required for melanin synthesis in melanocytes.79 Phox2b−/− mice do not have any peripheral autonomic neurons, including enteric neurons, and die at birth.86 During ENS development, Phox2b is first expressed just prior to the entry of vagal neural crest cells into the gut. Like SOX10, PHOX2B is required for Ret expression in ENCCs.86 Although PHOX2B is thought to be involved primarily in neuronal specification, Phox2b is expressed by both enteric neurons and glial cells.88 ZEB2 (Zinc finger E-box-binding homeobox 2) is a transcription factor involved in neural specification and in epithelial–mesenchymal transition (EMT) during early neural crest development. Zeb2−/− mice die around E9.5 and exhibit a variety of cardiovascular and neural defects, including a failure of the vagal neural crest to form.83 Mice with targeted ablation of Zeb2 in neural crest cells have craniofacial, heart, pigment, and peripheral nervous system deformities as well as aganglionosis of the entire colon that extends into the small intestine.114 Zeb2 has a similar expression pattern to Sox10 in the developing ENS,84 but the molecular mechanism by which ZEB2 regulates enteric neuron development has not yet been elucidated. Other Molecules and Interactions ENCCs express cell surface molecules, including beta1-integrins and the cell adhesion molecule L1CAM, which regulate interactions with the ECM, 120 TABLE 2 Genetic Interactions That Influence the Penetrance and Severity of Aganglionosis in Mice Interacting Genes References Ret and Ednrb 117 Ret and Edn3 27 Sox10 and Ednrb 72 Sox10 and Edn3 28 Sox10 and Sox8 118 Sox10 and L1cam 119 Sox10 and Zeb2 84 L1cam and Edrnb 120 L1cam and Edn3 120 other ENCCs and/or other cell types. Mice in which ENCCs lack beta1-integrins exhibit aganglionosis because beta1-integrins are required to overcome the inhibitory effect of high levels of tenascin-C in the hindgut.24 L1CAM is expressed by most migrating ENCCs, and perturbation of L1CAM function in vivo or in cultured explants of gut retards the migration of ENCCs, although the entire length of the gut in L1cam homozygous null mutants is eventually colonized.94 Other molecules shown to be involved in the development of the ENS from animal studies include neurotrophin-3, sonic hedgehog, Indian hedgehog, bone morphogenetic proteins (BMPs) 2 and 4, Notch, small GTPases, neuregulin, microRNAs, serotonin, the norepinephrine transporter, vitamin A, and the axon guidance molecules, SEMA3A and netrin.15 The activity of the different pathways involved in ENS development must be coordinated, and there is substantial evidence for interactions between pathways. The first evidence that interactions between pathways influence ENS development came from studies of humans with HSCR.115,116 Subsequent studies in mice have shown that interactions between a variety of signaling pathways influence the penetrance and severity of aganglionosis (Table 2). Some of the interactions are direct, for example, SOX10 binds directly to Ednrb regulatory regions,112 whereas other interactions may be indirect. HIRSCHSPRUNG DISEASE Etiology Studies using animal models have shown that the absence of enteric neurons from variable lengths of the gastrointestinal tract in HSCR results from a failure of ENCCs to colonize the affected gut regions during development (Figures 3 and 4). Aganglionosis is associated with a delay in the entry of neural crest-derived © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease C S C W A C S S C S C C S A S FIGURE 4 | Diagram showing the location of ENCCs along the gut (green) in E10.5 and E12.5 wild-type and Edn3 −/− mice. Edn3 homozygous null mutants are a mouse model of Hirschsprung’s disease. Already at E10.5, ENCCs are not as caudally advanced along the gut in Edn3 null mice compared to wild-type mice.27 There is a similar delayed entry into the gut in Ednrb homozygous null mutants.25 (Reprinted with permission from Ref 122. Copyright 2001 John Wiley and Sons) cells into the foregut, as well as a delayed progression of ENCCs along the gut.25,27 The delay is exacerbated by changes to the gut microenvironment with age that make it less permissive for ENCC migration.25 Defects in multiple processes can contribute to the delay in the colonization of the gut by ENCC (see the section Origin and Early Development of the Enteric Nervous System above), but ENCC proliferation is critical, as a minimal number of ENCCs are required for normal ENS formation.21,23 Although cell death does not play a major role during normal ENS development, it may contribute to the etiology of HSCR.121 Genetics The genetics of HSCR are complex and are reviewed in detail by Amiel et al.1 Mutations in genes encoding members of a variety of signaling pathways are associated with HSCR (Table 1), but mutations in the coding sequence of these known genes account for only about 50% of familial cases of HSCR and 15% of sporadic cases of HSCR.1 RET is the major susceptibility gene as more than 80% of identified mutations associated with HSCR are in RET; these include both coding and noncoding mutations.123,124 RET coding sequence mutations have been identified in 20–30% of HSCR cases, and alone, can result in HSCR by haploinsufficiency.1 Noncoding mutations are more common and result in reduced amounts of wild-type RET protein due to a reduction in RET transcription; these mutations probably only result in Volume 2, January/February 2013 HSCR when combined with other mutations.1,124 For example, a common noncoding mutation, a T>C SNP lying within an intronic RET enhancer, has a 20-fold greater contribution to HSCR susceptibility than RET coding sequence mutations.123 This mutation appears to account for some, but not all, of the sex ratio in HSCR.1,123 Like mutations in most genes associated with HSCR, the penetrance of RET mutations, even coding sequence mutations, is incomplete. For instance, a missense mutation in RET was found in four members of one family, of which one had long segment HSCR, two had short segment HSCR, and one was unaffected.125 There appear to be some phenotypic differences in mice and humans with reduced RET signaling. Unlike humans, Ret heterozygous mice do not show an HSCR-like phenotype30,37 (Table 1). However, colonic aganglionosis can be observed in mice when the levels of Ret are reduced to around 40% of wild-type levels.126 In addition to intestinal aganglionosis, Ret null homozygous mutant mice lack kidneys and have sympathetic and parasympathetic neuron defects. In contrast, infants with HSCR only extremely rarely have kidney defects. Studies in mice have shown that different tissues appear to require distinct RET-stimulated signaling pathways, which might partly explain why intestinal aganglionosis can occur as an isolated defect in HSCR patients with RET mutations.108 In addition to RET, mutations in a dozen or more genes have been associated with HSCR (Table 1). Although mutation in a single gene (RET, EDNRB, EDN3) can be sufficient for the development of HSCR, patients with mutations in two genes have been identified, and complex genetic interactions contribute to the variability in penetrance and severity (length of the aganglionic region). Most of the genes associated with HSCR in humans also result in aganglionosis in mice following inactivation (Table 1). However, a heterozygous mutation in NRTN that cooccurred with a RET mutation was found in one family with HSCR,44 but mice lacking NRTN do not have aganglionosis.30 L1CAM is the only known X-linked gene associated with HSCR, but as only 3% of patients with mutations in L1CAM also have HSCR, L1CAM is thought to act as an X-linked HSCR modifier gene.127 Most of the syndromes involving an HSCR phenotype are each associated with mutations in one or a small number of genes (Table 1). Copy number variants (CNVs), which are structural variations in DNA that result in an abnormal number of copies of sections of DNA, have been associated with susceptibility or resistance to some human diseases. Data from a recent study of 67 © 2012 Wiley Periodicals, Inc. 121 wires.wiley.com/devbio Focus Article proven or candidate HSCR genes from human and mice studies suggest that CNVs, particularly in regulatory sequences, can play a role in HSCR.128 HSCR has become a paradigm for understanding complex multigenetic disorders. For example, studies of HSCR have shown that small structural variants in a gene can act as powerful genetic modifiers in human disease. Furthermore HSCR studies have blurred the definition of modifier gene, as depending on the mutation, the same gene can act as a principal gene or a modifier gene. For example, large genomic mutations in RET, alone, can result in HSCR (‘principal gene’) but small structural variants in RET probably only result in HSCR when combined with other mutations (‘modifier gene’).124 Humans appear to be more sensitive to decreased levels of RET and EDNRB signaling than mice, which might be due, at least in part, to the larger area of bowel that has to be colonized by ENCCs in humans compared with mice. Although it has been assumed that all cases of HSCR have a genetic basis, vitamin A deficiency increases the penetrance and severity of aganglionosis in a mouse model of HSCR.129 Thus, environmental factors could contribute to susceptibility to HSCR. is predominantly excitatory (mediates muscle contraction), and may even be hypertrophied in some HSCR patients.4,130 Relaxation of the gut wall during propulsive motility is normally mediated by inhibitory enteric (intrinsic) motor neurons, and so an absence of intrinsic inhibitory neurons may also contribute to the aganglionic segment being persistently constricted.130 Muscle hypertrophy also occurs in the aganglionic segment in mouse and rat models of HSCR,131,132 probably as a secondary effect. Perturbation of intestinal motility is not limited to the aganglionic gut segment. HSCR patients often have motility disturbances following surgical resection. In mouse models of HSCR, spontaneous propagating motility patterns are absent or abnormal along the entire colon, including the proximal colon (oral to the transition zone) where enteric ganglia are present.51,59 The most likely cause is a reduction in enteric neuron density, although inflammation and damage to the interstitial cells of Cajal (ICC), a population of cells involved in gut motility, in regions proximal to the aganglionic bowel could also contribute to abnormal motility.133 Current Treatment and Potential Therapies Diagnosis, Pathology, and Physiology Healthy infants normally pass meconium (the earliest stools) within the first 24–48 h following birth. Most infants with HSCR, however, fail to pass meconium and suffer from severe constipation. Other symptoms include gradual distension of the abdomen, vomiting, and fever. Although infants with HSCR normally show symptoms within the first weeks after birth, other children with HSCR may not exhibit symptoms for several months. HSCR is usually diagnosed by a barium enema (Figure 1), anorectal manometry, and a biopsy of the rectum. The pathological evaluation of rectal biopsies for HSCR is reviewed by Kapur.4 Most laboratories rely on hematoxylin and eosin-stained paraffin sections to identify neuronal cell bodies, although histochemical and immunohistochemical techniques are also used by some pathologists to assist the diagnosis. During surgery to remove the aganglionic region of bowel, frozen sections are taken to localize the boundary between the ganglionic and aganglionic regions prior to resection.4 The megacolon and severe constipation experienced by patients with HSCR are caused by a lack of propulsive motility patterns in the distal bowel due to the lack of intrinsic enteric neurons. The persistent constriction of the aganglionic segment is probably mediated by the extrinsic innervation, which 122 If left untreated, HSCR can be fatal due to enterocolitis, perforation of the bowel, or malnutrition. Current treatment for HSCR involves the surgical removal of the defective, aganglionic bowel, and reanastomosis of the distal-most, normal (ganglionated) bowel to the anus. Depending on the severity of the disease (length of aganglionosis) and the general health of the patient, the surgery may be performed in one or two stages; for patients with long-segment aganglionosis or major health problems, an initial primary colostomy is often performed with the resection of the aganglionic bowel performed later. While these operative procedures are lifesaving, they can be associated with acute (anastomotic stricture, enterocolitis) and chronic (constipation, fecal incontinence) complications. Cell transplantation therapy has been proposed as an alternative to surgical resection of aganglionic bowel for the treatment of HSCR.10,57,134,135 This would involve the transplantation of neural stem/progenitor cells into the aganglionic bowel, which would colonize the defective region, generate neurons, and form the neuronal circuits required for propulsive motility. Neural stem/progenitor cells can be isolated from the bowel of postnatal and adult laboratory animals and humans, including HSCR patients.10,136 These cells are capable of both selfrenewal and of giving rise to multiple lineages in vitro including neurons and glia (Figure 5). Pluripotent stem © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease (a) (b) N N FIGURE 5 | Enteric neural crest stem/progenitor cells form neurospheres in vitro. (a) Neural crest stem/progenitors were isolated from the gut of an E14.5 mouse and cultured in suspension conditions. Neurospheres formed, which were then plated onto fibronectin for 48 h to allow for migration of neural crest-like cells (identified using an antibody to SOX10, green, Santa Cruz) and neurite outgrowth (identified using the neuronal marker, TUBB3, formerly known as TuJ1, red, Covance). (b) Higher magnification image of the outgrowth of TUBB3+ neurites and SOX10+ cells that have migrated away from the neurosphere. There are also a small number of TUBB3+ cell bodies in the outgrowth (arrows ). Scale bars: 200 μm (a); 50 μm (b). cells, such as embryonic stem (ES) cells and induced pluripotent stem (iPS) cells, are also a potential source of cells to generate enteric neurons as ES cells can give rise to neural crest-like cells and to neurons when co-cultured with explants of embryonic gut.137,138 iPS cells and ‘adult’ stem cells have the added benefit of being patient-derived and thus have reduced chance of immunological rejection after engraftment. Cell therapy to treat HSCR is currently a very active field of research.10,57,134,135 TYPE IV WAARDENBURG SYNDROME (WS4)—AN EXAMPLE OF A SYNDROME THAT INCLUDES AGANGLIONIC MEGACOLON There are four types of Waardenburg syndrome, all of which involve sensorineural hearing loss and pigmentation abnormalities.49 Type IV Waardenburg syndrome (WS4) also involves HSCR and sometimes neurological features. The sensorineural hearing loss and depigmentation are due to abnormal development of neural crest-derived melanocytes in the stria vascularis of the cochlea, skin, hair, or eyes.139 Mutations in three genes, SOX10, EDNRB, and EDN3, account for approximately 60–80% of cases of WS4.69 These three genes are required for the development of both the ENS and melanocytes (see the section Origin and Early Development of the Enteric Nervous System above). Heterozygous mutations in SOX10 account for approximately 50% of WS4 cases, mostly occurring de novo.49 The Sox10 ‘Dom’ mutation in mice Volume 2, January/February 2013 occurred spontaneously and is a single base pair insertion that results in loss of the SOX10 protein transcriptional activation domain.70 Sox10Dom/+ mice exhibit aganglionosis and pigmentation defects and therefore exhibit a similar phenotype to humans with WS4. The severity and penetrance of aganglionosis in Sox10Dom/+ mice varies with the genetic background.72 SOX10 mutations in humans can also result in a more severe phenotype that also includes central and peripheral demyelinating neuropathies, which is called PCWH syndrome (peripheral demyelinating neuropathy, central dysmyelinating leukodystrophy, Waardenburg syndrome, and Hirschsprung disease).69 This neurological phenotype has been mostly associated with SOX10 mutations resulting in a dominant negative effect, rather than haploinsufficiency.69 Of the approximately 20–30% cases of WS4 due to mutations in EDNRB or EDN3, about 70% are recessive (homozygous or compound heterozygous) mutations of EDNRB or EDN3.49 Heterozygous mutations in EDNRB or EDN3 are most commonly associated with isolated HSCR, although rare cases of WS4 with heterozygous EDNRB mutations have been reported.49 Phenotypes associated with SOX10, EDNRB and EDN3 mutations show a large degree of variability.49 Moreover, heterozygous disruptions in SOX10 account for approximately 15% of cases of Type II Waardenburg syndrome (WS2), which lacks HSCR,69 while heterozygous mutations in EDNRB or EDN3 have also been associated with WS2.49 These findings further highlight the genetic complexity of HSCR and Waardenburg syndromes, and the © 2012 Wiley Periodicals, Inc. 123 wires.wiley.com/devbio Focus Article importance of the genetic background for the severity of the phenotype. CONCLUSION Molecular genetics of HSCR patients and studies using animal models of HSCR have, in parallel, revealed much about the pathogenesis of HSCR. However, there are many outstanding questions. For example, the molecular mechanisms underlying the interactions between pathways, and how particular mutations impact on those interactions, are not well understood. The 4:1 male:female bias in the incidence of HSCR is only partly explained by current knowledge. The transplantation of neural stem/progenitor cells into the aganglionic region of HSCR patients, as an alternative treatment to surgical removal, is an exciting, but currently untested possibility. ACKNOWLEDGMENTS The authors’ work is supported by NHMRC (Australia) Senior Research Fellowship #1002506, CJ Martin Fellowship #400433 and Project grant #546473. We thank Annette Bergner for assistance with obtaining the images shown in Figures 2 and 3, and Lauren Young and John Stephenson for assistance with processing the embryos shown in Figure 2. REFERENCES 1. Amiel J, Sproat-Emison E, Garcia-Barcelo M, Lantieri F, Burzynski G, Borrego S, Pelet A, Arnold S, Miao X, Griseri P, et al. Hirschsprung disease, associated syndromes and genetics: a review. J Med Genet 2008, 45:1–14. 2. Whitehouse FR, Kernohan JW. Myenteric plexus in congenital megacolon; study of 11 cases. Arch Intern Med (Chic) 1948, 82:75–111. 3. Moore SW. Down syndrome and the enteric nervous system. Pediatr Surg Int 2008, 24:873–883. 4. Kapur RP. Practical pathology and genetics of Hirschsprung’s disease. Semin Pediatr Surg 2009, 18:212–223. 5. Berrocal T, Lamas M, Gutieerrez J, Torres I, Prieto C, del Hoyo ML. Congenital anomalies of the small intestine, colon, and rectum. Radiographics 1999, 19:1219–1236. 6. Burzynski G, Shepherd IT, Enomoto H. Genetic model system studies of the development of the enteric nervous system, gut motility and Hirschsprung’s disease. Neurogastroenterol Motil 2009, 21:113–127. 7. Furness JB. The Enteric Nervous System. MA: Blackwell Publishing; 2006. 8. Gershon MD. Developmental determinants of the independence and complexity of the enteric nervous system. Trends Neurosci 2010, 33:446–456. 9. Karaosmanoglu T, Aygun B, Wade PR, Gershon MD. Regional differences in the number of neurons in the myenteric plexus of the guinea pig small intestine and colon: an evaluation of markers used to count neurons. Anat Rec 1996, 244:470–480. 10. Metzger M, Caldwell C, Barlow AJ, Burns AJ, Thapar N. Enteric nervous system stem cells derived from 124 human gut mucosa for the treatment of aganglionic gut disorders. Gastroenterology 2009, 136:2214–2225 11. Le Douarin NM, Teillet MA. Experimental analysis of the migration and differentiation of neuroblasts of the autonomic nervous system and of neurectodermal mesenchymal derivatives, using a biological cell marking technique. Dev Biol 1974, 41:162–184. 12. Burns AJ, Le Douarin NM. The sacral neural crest contributes neurons and glia to the post-umbilical gut: spatiotemporal analysis of the development of the enteric nervous system. Development (Cambridge, England) 1998, 125:4335–4347. 13. Kapur RP. Colonization of the murine hindgut by sacral crest-derived neural precursors: experimental support for an evolutionarily conserved model. Dev Biol 2000, 227:146–155. 14. Wang X, Chan AK, Sham MH, Burns AJ, Chan WY. Analysis of the sacral neural crest cell contribution to the hindgut enteric nervous system in the mouse embryo. Gastroenterology 2011, 141:992–1002. 15. Young HM, Newgreeen DF, Enomoto H. Development of the enteric nervous system. In: Johnson L, ed. Physiology of the Gastrointestinal Tract. 5th ed. Burlington, MA: Elsevier; 2012. 16. Kapur RP, Yost C, Palmiter RD. A transgenic model for studying development of the enteric nervous system in normal and aganglionic mice. Development (Cambridge, England) 1992, 116:167–175. 17. Wallace AS, Burns AJ. Development of the enteric nervous system, smooth muscle and interstitial cells of Cajal in the human gastrointestinal tract. Cell Tissue Res 2005, 319:367–382. 18. Newgreen DF, Southwell B, Hartley L, Allan IJ. Migration of enteric neural crest cells in relation to © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease growth of the gut in avian embryos. Acta Anat 1996, 157:105–115. 19. Pham TD, Gershon MD, Rothman TP. Time of origin of neurons in the murine enteric nervous system: sequence in relation to phenotype. J Comp Neurol 1991, 314:789–798. 20. Roberts RR, Ellis M, Gwynne RM, Bergner AJ, Lewis MD, Beckett EA, Bornstein JC, Young HM. The first intestinal motility patterns in fetal mice are not mediated by neurons or interstitial cells of Cajal. J Physiol 2010, 588:1153–1169. 21. Barlow AJ, Wallace AS, Thapar N, Burns AJ. Critical numbers of neural crest cells are required in the pathways from the neural tube to the foregut to ensure complete enteric nervous system formation. Development (Cambridge, England) 2008, 135:1681–1691. 22. Simpson MJ, Landman KA, Hughes BD, Newgreen DF. Cell proliferation drives neural crest cell invasion of the intestine. Dev Biol 2007, 302:553–568. 23. Yntema CL, Hammond WS. The origin of intrinsic ganglia of trunk viscera from vagal neural crest in the chick embryo. J Comp Neurol 1954, 101:515–541. 24. Breau MA, Dahmani A, Broders-Bondon F, Thiery JP, Dufour S. Beta1 integrins are required for the invasion of the caecum and proximal hindgut by enteric neural crest cells. Development (Cambridge, England) 2009, 136:2791–2801. 25. Druckenbrod NR, Epstein ML. Age-dependent changes in the gut environment restrict the invasion of the hindgut by enteric neural progenitors. Development (Cambridge, England) 2009, 136:3195–3203. 26. Hearn CJ, Murphy M, Newgreen D. GDNF and ET-3 differentially modulate the numbers of avian enteric neural crest cells and enteric neurons in vitro. Dev Biol 1998, 197:93–105. 27. Barlow A, de Graaff E, Pachnis V. Enteric nervous system progenitors are coordinately controlled by the G protein-coupled receptor EDNRB and the receptor tyrosine kinase RET. Neuron 2003, 40:905–916. 28. Stanchina L, Baral V, Robert F, Pingault V, Lemort N, Pachnis V, Goossens M, Bondurand N. Interactions between Sox10, Edn3 and Ednrb during enteric nervous system and melanocyte development. Dev Biol 2006, 295:232–249. 29. Wu JJ, Chen JX, Rothman TP, Gershon MD. Inhibition of in vitro enteric neuronal development by endothelin-3: mediation by endothelin B receptors. Development (Cambridge, England) 1999, 126:1161–1173. 30. Gianino S, Grider JR, Cresswell J, Enomoto H, Heuckeroth RO. GDNF availability determines enteric neuron number by controlling precursor proliferation. Development (Cambridge, England) 2003, 130:2187–2198. 31. Kruger GM, Mosher JT, Tsai YH, Yeager KJ, Iwashita T, Gariepy CE, Morrison SJ. Temporally distinct Volume 2, January/February 2013 requirements for endothelin receptor B in the generation and migration of gut neural crest stem cells. Neuron 2003, 40:917–929. 32. Wallace AS, Barlow AJ, Navaratne L, Delalande JM, Tauszig-Delamasure S, Corset V, Thapar N, Burns AJ. Inhibition of cell death results in hyperganglionosis: implications for enteric nervous system development. Neurogastroenterol Motil 2009, 21:768–e49. 33. Uesaka T, Jain S, Yonemura S, Uchiyama Y, Milbrandt J, Enomoto H. Conditional ablation of GFRalpha1 in postmigratory enteric neurons triggers unconventional neuronal death in the colon and causes a Hirschsprung’s disease phenotype. Development (Cambridge, England) 2007, 134:2171–2181. 34. Pachnis V, Mankoo B, Costantini F. Expression of the c-ret proto-oncogene during mouse embryogenesis. Development (Cambridge, England) 1993, 119:1005–1017. 35. Young HM, Bergner AJ, Muller T. Acquisition of neuronal and glial markers by neural crest-derived cells in the mouse intestine. J Comp Neurol 2003, 456:1–11. 36. Inoue K, Shimotake T, Iwai N. Mutational analysis of RET/GDNF/NTN genes in children with total colonic aganglionosis with small bowel involvement. Am J Med Genet 2000, 93:278–284. 37. Schuchardt A, D’Agati V, Larsson-Blomberg L, Costantini F, Pachnis V. Defects in the kidney and enteric nervous system of mice lacking the tyrosine kinase receptor Ret. Nature 1994, 367:380–383. 38. Ivanchuk SM, Myers SM, Eng C, Mulligan LM. De novo mutation of GDNF, ligand for the RET/GDNFRalpha receptor complex, in Hirschsprung disease. Hum Mol Genet 1996, 5:2023–2026. 39. Sanchez MP, Silos-Santiago I, Frisen J, He B, Lira SA, Barbacid M. Renal agenesis and the absence of enteric neurons in mice lacking GDNF. Nature 1996, 382:70–73. 40. Peters RJ, Osinski MA, Hongo JA, Bennett GL, Okragly AJ, Haak-Frendscho M, Epstein ML. GDNF is abundant in the adult rat gut. J Auton Nerv Sys 1998, 70:115–122. 41. Borrego S, Fernandez RM, Dziema H, Niess A, Lopez-Alonso M, Antinolo G, Eng C. Investigation of germline GFRA4 mutations and evaluation of the involvement of GFRA1, GFRA2, GFRA3, and GFRA4 sequence variants in Hirschsprung disease. J Med Genet 2003, 40:e18. 42. Enomoto H, Araki T, Jackman A, Heuckeroth RO, Snider WD, Johnson EM Jr, Milbrandt J. GFR alpha1deficient mice have deficits in the enteric nervous system and kidneys. Neuron 1998, 21:317–324. 43. Young HM, Hearn CJ, Farlie PG, Canty AJ, Thomas PQ, Newgreen DF. GDNF is a chemoattractant for enteric neural cells. Dev Biol 2001, 229:503–516. 44. Doray B, Salomon R, Amiel J, Pelet A, Touraine R, Billaud M, Attie T, Bachy B, Munnich A, Lyonnet S. © 2012 Wiley Periodicals, Inc. 125 wires.wiley.com/devbio Focus Article Mutation of the RET ligand, neurturin, supports multigenic inheritance in Hirschsprung disease. Hum Mol Genet 1998, 7:1449–1452. Willems PJ, et al. Endothelin-3 gene mutations in isolated and syndromic Hirschsprung disease. Eur J Hum Genet 1997, 5:247–251. 45. Heuckeroth RO, Enomoto H, Grider JR, Golden JP, Hanke JA, Jackman A, Molliver DC, Bardgett ME, Snider WD, Johnson EM Jr, Milbrandt J. Gene targeting reveals a critical role for neurturin in the development and maintenance of enteric, sensory, and parasympathetic neurons. Neuron 1999, 22:253–263. 57. Heanue TA, Pachnis V. Enteric nervous system development and Hirschsprung’s disease: advances in genetic and stem cell studies. Nat Rev 2007, 8:466–479. 46. Golden JP, DeMaro JA, Osborne PA, Milbrandt J, Johnson EM Jr. Expression of neurturin, GDNF, and GDNF family-receptor mRNA in the developing and mature mouse. Exp Neurol 1999, 158:504–528. 47. Puffenberger EG, Hosoda K, Washington SS, Nakao K, deWit D, Yanagisawa M, Chakravart A. A missense mutation of the endothelin-B receptor gene in multigenic Hirschsprung’s disease. Cell 1994, 79:1257–1266. 48. Amiel J, Attie T, Jan D, Pelet A, Edery P, Bidaud C, Lacombe D, Tam P, Simeoni J, Flori E, et al. Heterozygous endothelin receptor B (EDNRB) mutations in isolated Hirschsprung disease. Hum Mol Genet 1996, 5:355–357. 49. Pingault V, Ente D, Dastot-Le Moal F, Goossens M, Marlin S, Bondurand N. Review and update of mutations causing Waardenburg syndrome. Hum Mutat 2010, 31:391–406. 50. Syrris P, Carter ND, Patton MA. Novel nonsense mutation of the endothelin-B receptor gene in a family with Waardenburg-Hirschsprung disease. Am J Med Genet 1999, 87:69–71. 51. Ro S, Hwang SJ, Muto M, Jewett WK, Spencer NJ. Anatomic modifications in the enteric nervous system of piebald mice and physiological consequences to colonic motor activity. Am J Physiol 2006, 290:G710–G718. 52. Lee HO, Levorse JM, Shin MK. The endothelin receptor-B is required for the migration of neural crest-derived melanocyte and enteric neuron precursors. Dev Biol 2003, 259:162–175. 53. Bondurand N, Natarajan D, Barlow A, Thapar N, Pachnis V. Maintenance of mammalian enteric nervous system progenitors by SOX10 and endothelin 3 signalling. Development (Cambridge, England) 2006, 133:2075–2086. 54. Hosoda K, Hammer RE, Richardson JA, Baynash AG, Cheung JC, Giaid A, Yanagisawa M. Targeted and natural (piebald-lethal) mutations of endothelinB receptor gene produce megacolon associated with spotted coat color in mice. Cell 1994, 79:1267–1276. 55. Attie T, Till M, Pelet A, Amiel J, Edery P, Boutrand L, Munnich A, Lyonnet S. Mutation of the endothelinreceptor B gene in Waardenburg-Hirschsprung disease. Hum Mol Genet 1995, 4:2407–2409. 56. Bidaud C, Salomon R, Van Camp G, Pelet A, Attie T, Eng C, Bonduelle M, Amiel J, Nihoul-Fekete C, 126 58. Pingault V, Bondurand N, Lemort N, Sancandi M, Ceccherini I, Hugot JP, Jouk PS, Goossens M. A heterozygous endothelin 3 mutation in WaardenburgHirschsprung disease: is there a dosage effect of EDN3/EDNRB gene mutations on neurocristopathy phenotypes? J Med Genet 2001, 38:205–209. 59. Roberts RR, Bornstein JC, Bergner AJ, Young HM. Disturbances of colonic motility in mouse models of Hirschsprung’s disease. Am J Physiol 2008, 294:G996–G1008. 60. Leibl MA, Ota T, Woodward MN, Kenny SE, Lloyd DA, Vaillant CR, Edgar DH. Expression of endothelin 3 by mesenchymal cells of embryonic mouse caecum. Gut 1999, 44:246–252. 61. Edery P, Attie T, Amiel J, Pelet A, Eng C, Hofstra RM, Martelli H, Bidaud C, Munnich A, Lyonnet S. Mutation of the endothelin-3 gene in the WaardenburgHirschsprung disease (Shah-Waardenburg syndrome). Nat Genet 1996, 12:442–444. 62. Baynash AG, Hosoda K, Giaid A, Richardson JA, Emoto N, Hammer RE, Yanagisawa M. Interaction of endothelin-3 with endothelin-B receptor is essential for development of epidermal melanocytes and enteric neurons. Cell 1994, 79:1277–1285. 63. Hofstra RM, Valdenaire O, Arch E, Osinga J, Kroes H, Loffler BM, Hamosh A, Meijers C, Buys CH. A loss-of-function mutation in the endothelin-converting enzyme 1 (ECE-1) associated with Hirschsprung disease, cardiac defects, and autonomic dysfunction. Am J Hum Genet 1999, 64:304–308. 64. Yanagisawa H, Yanagisawa M, Kapur RP, Richardson JA, Williams SC, Clouthier DE, de Wit D, Emoto N, Hammer RE. Dual genetic pathways of endothelin-mediated intercellular signaling revealed by targeted disruption of endothelin converting enzyme1 gene. Development (Cambridge, England) 1998, 125:825–836. 65. Garcia-Barcelo MM, Tang CS, Ngan ES, Lui VC, Chen Y, So MT, Leon TY, Miao XP, Shum CK, Liu FQ, et al. Genome-wide association study identifies NRG1 as a susceptibility locus for Hirschsprung’s disease. Proc Natl Acad Sci USA 2009, 106:2694–2699. 66. Meyer D, Birchmeier C. Multiple essential functions of neuregulin in development. Nature 1995, 378:386–390. 67. Britsch S, Li L, Kirchhoff S, Theuring F, Brinkmann V, Birchmeier C, Riethmacher D. The ErbB2 and ErbB3 receptors and their ligand, neuregulin-1, are essential for development of the sympathetic nervous system. Genes Dev 1998, 12:1825–1836. © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease 68. Pingault V, Bondurand N, Kuhlbrodt K, Goerich DE, Prehu MO, Puliti A, Herbarth B, Hermans-Borgmeyer I, Legius E, Matthijs G, et al. SOX10 mutations in patients with Waardenburg-Hirschsprung disease. Nat Genet 1998, 18:171–173. 69. Bondurand N, Dastot-Le Moal F, Stanchina L, Collot N, Baral V, Marlin S, Attie-Bitach T, Giurgea I, Skopinski L, Reardon W, et al. Deletions at the SOX10 gene locus cause Waardenburg syndrome types 2 and 4. Am J Hum Genet 2007, 81:1169–1185. 70. Southard-Smith EM, Kos L, Pavan WJ. Sox10 mutation disrupts neural crest development in Dom Hirschsprung mouse model. Nat Genet 1998, 18: 60–64. 71. Kapur RP. Early death of neural crest cells is responsible for total enteric aganglionosis in Sox10 (Dom)/Sox10(Dom) mouse embryos. Pediatr Dev Pathol 1999, 2:559–569. 72. Cantrell VA, Owens SE, Chandler RL, Airey DC, Bradley KM, Smith JR, Southard-Smith EM. Interactions between Sox10 and EdnrB modulate penetrance and severity of aganglionosis in the Sox10Dom mouse model of Hirschsprung disease. Hum Mol Genet 2004, 13:2289–2301. 73. Walters LC, Cantrell VA, Weller KP, Mosher JT, Southard-Smith EM. Genetic background impacts developmental potential of enteric neural crest-derived progenitors in the Sox10Dom model of Hirschsprung disease. Hum Mol Genet 2010, 19:4353–4372. 74. Young HM, Jones BR, McKeown SJ. The projections of early enteric neurons are influenced by the direction of neural crest cell migration. J Neurosci 2002, 22:6005–6018. 75. Lang D, Chen F, Milewski R, Li J, Lu MM, Epstein JA. Pax3 is required for enteric ganglia formation and functions with Sox10 to modulate expression of c-ret. J Clin Invest 2000, 106:963–971. 76. Paratore C, Eichenberger C, Suter U, Sommer L. Sox10 haploinsufficiency affects maintenance of progenitor cells in a mouse model of Hirschsprung disease. Hum Mol Genet 2002, 11:3075–3085. 77. Kim J, Lo L, Dormand E, Anderson DJ. SOX10 maintains multipotency and inhibits neuronal differentiation of neural crest stem cells. Neuron 2003, 38:17–31. 78. Paratore C, Goerich DE, Suter U, Wegner M, Sommer L. Survival and glial fate acquisition of neural crest cells are regulated by an interplay between the transcription factor Sox10 and extrinsic combinatorial signaling. Development (Cambridge, England) 2001, 128:3949–3961. Yamanaka T, Mushiake K, et al. Mutations in SIP1, encoding Smad interacting protein-1, cause a form of Hirschsprung disease. Nat Genet 2001, 27:369–370. 81. Zweier C, Albrecht B, Mitulla B, Behrens R, Beese M, Gillessen-Kaesbach G, Rott HD, Rauch A. ‘‘MowatWilson’’ syndrome with and without Hirschsprung disease is a distinct, recognizable multiple congenital anomalies-mental retardation syndrome caused by mutations in the zinc finger homeo box 1B gene. Am J Med Genet 2002, 108:177–181. 82. Garavelli L, Donadio A, Zanacca C, Banchini G, Della Giustina E, Bertani G, Albertini G, Del Rossi C, Zweier C, Rauch A, et al. Hirschsprung disease, mental retardation, characteristic facial features, and mutation in the gene ZFHX1B (SIP1): confirmation of the Mowat-Wilson syndrome. Am J Med Genet A 2003, 116A:385–388. 83. Van De Putte T, Maruhashi M, Francis A, Nelles L, Kondoh H, Huylebroeck D, Higashi Y. Mice lacking Zfhx1b, the gene that codes for Smad-interacting protein-1, reveal a role for multiple neural crest cell defects in the etiology of Hirschsprung disease-mental retardation syndrome. Am J Hum Genet 2003, 72:2. 84. Stanchina L, Van de Putte T, Goossens M, Huylebroeck D, Bondurand N. Genetic interaction between Sox10 and Zfhx1b during enteric nervous system development. Dev Biol 2010, 341:416–428. 85. Amiel J, Laudier B, Attie-Bitach T, Trang H, De Pontual L, Gener B, Trochet D, Etchevers H, Ray P, Simonneau M, et al. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet 2003, 33:459–461. 86. Pattyn A, Morin X, Cremer H, Goridis C, Brunet JF. The homeobox gene Phox2b is essential for the development of autonomic neural crest derivatives. Nature 1999, 399:366–370. 87. Young HM, Hearn CJ, Ciampoli D, Southwell BR, Brunet JF, Newgreen DF. A single rostrocaudal colonization of the rodent intestine by enteric neuron precursors is revealed by the expression of Phox2b, Ret, and p75 and by explants grown under the kidney capsule or in organ culture. Dev Biol 1998, 202:67–84. 88. Corpening JC, Cantrell VA, Deal KK, Southard-Smith EM. A Histone2BCerulean BAC transgene identifies differential expression of Phox2b in migrating enteric neural crest derivatives and enteric glia. Dev Dyn 2008, 237:1119–1132. 79. Harris ML, Baxter LL, Loftus SK, Pavan WJ. Sox proteins in melanocyte development and melanoma. Pigment Cell Melanoma Res 2010, 23:496–513. 89. Brooks AS, Bertoli-Avella AM, Burzynski GM, Breedveld GJ, Osinga J, Boven LG, Hurst JA, Mancini GM, Lequin MH, de Coo RF, et al. Homozygous nonsense mutations in KIAA1279 are associated with malformations of the central and enteric nervous systems. Am J Hum Genet 2005, 77:120–126. 80. Wakamatsu N, Yamada Y, Yamada K, Ono T, Nomura N, Taniguchi H, Kitoh H, Mutoh N, 90. Lyons DA, Naylor SG, Mercurio S, Dominguez C, Talbot WS. KBP is essential for axonal structure, Volume 2, January/February 2013 © 2012 Wiley Periodicals, Inc. 127 wires.wiley.com/devbio Focus Article outgrowth and maintenance in zebrafish, providing insight into the cellular basis of Goldberg-Shprintzen syndrome. Development (Cambridge, England) 2008, 135:599–608. 91. Alves MM, Burzynski G, Delalande JM, Osinga J, van der Goot A, Dolga AM, de Graaff E, Brooks AS, Metzger M, Eisel UL, et al. KBP interacts with SCG10, linking Goldberg-Shprintzen syndrome to microtubule dynamics and neuronal differentiation. Hum Mol Genet 2010, 19:3642–3651. 92. Okamoto N, Wada Y, Goto M. Hydrocephalus and Hirschsprung’s disease in a patient with a mutation of L1CAM. J Med Genet 1997, 34:670–671. 93. Okamoto N, Del Maestro R, Valero R, Monros E, Poo P, Kanemura Y, Yamasaki M. Hydrocephalus and Hirschsprung’s disease with a mutation of L1CAM. J Hum Genet 2004, 49:334–337. 94. Anderson RB, Turner KN, Nikonenko AG, Hemperly J, Schachner M, Young HM. The cell adhesion molecule L1 is required for chain migration of neural crest cells in the developing mouse gut. Gastroenterology 2006, 130:1221–1232. 95. Sariola H, Saarma M. Novel functions and signalling pathways for GDNF. J Cell Sci 2003, 116:3855–3862. 96. Manie S, Massimo S, Alfredo F, Billaud M. The RET receptor: function in development and dysfunction in congenital malformation. Trends Genet 2001, 17:580–589. 97. Natarajan D, Marcos-Gutierrez C, Pachnis V, de Graaff E. Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development (Cambridge, England) 2002, 129:5151–5160. 98. Moore MW, Klein RD, Farinas I, Sauer H, Armanini M, Phillips H, Reichardt LF, Ryan AM, CarverMoore K, Rosenthal A. Renal and neuronal abnormalities in mice lacking GDNF. Nature 1996, 382:76–79. 99. Chalazonitis A, Rothman TP, Chen J, Gershon MD. Age-dependent differences in the effects of GDNF and NT-3 on the development of neurons and glia from neural crest-derived precursors immunoselected from the fetal rat gut: expression of GFRalpha-1 in vitro and in vivo. Dev Biol 1998, 204:385–406. 100. Heuckeroth RO, Lampe PA, Johnson EM, Milbrandt J. Neurturin and GDNF promote proliferation and survival of enteric neuron and glial progenitors in vitro. Dev Biol 1998, 200:116–129. 101. Durbec PL, Larsson-Blomberg LB, Schuchardt A, Costantini F, Pachnis V. Common origin and developmental dependence on c-ret of subsets of enteric and sympathetic neuroblasts. Development (Cambridge, England) 1996, 122:349–358. 102. Laranjeira C, Pachnis V. Enteric nervous system development: recent progress and future challenges. Auton Neurosci 2009, 151:61–69. 128 103. Taketomi T, Yoshiga D, Taniguchi K, Kobayashi T, Nonami A, Kato R, Sasaki M, Sasaki A, Ishibashi H, Moriyama M, et al. Loss of mammalian Sprouty2 leads to enteric neuronal hyperplasia and esophageal achalasia. Nat Neurosci 2005, 8:855–857. 104. Zhou R, Niwa S, Homma N, Takei Y, Hirokawa N. KIF26A is an unconventional kinesin and regulates GDNF-Ret signaling in enteric neuronal development. Cell 2009, 139:802–813. 105. Wang H, Hughes I, Planer W, Parsadanian A, Grider JR, Vohra BP, Keller-Peck C, Heuckeroth RO. The timing and location of glial cell line-derived neurotrophic factor expression determine enteric nervous system structure and function. J Neurosci 2010, 30:1523–1538. 106. De Graaff E, Srinivas S, Kilkenny C, D’Agati V, Mankoo BS, Costantini F, Pachnis V. Differential activities of the RET tyrosine kinase receptor isoforms during mammalian embryogenesis. Genes Dev 2001, 15:2433–2444. 107. Jain S, Encinas M, Johnson EM Jr, Milbrandt J. Critical and distinct roles for key RET tyrosine docking sites in renal development. Genes Dev 2006, 20:321–333. 108. Jain S, Knoten A, Hoshi M, Wang H, Vohra B, Heuckeroth RO, Milbrandt J. Organotypic specificity of key RET adaptor-docking sites in the pathogenesis of neurocristopathies and renal malformations in mice. J Clin Invest 2010, 120:778–790. 109. Rossi J, Herzig KH, Voikar V, Hiltunen PH, Segerstrale M, Airaksinen MS. Alimentary tract innervation deficits and dysfunction in mice lacking GDNF family receptor alpha2. J Clin Invest 2003, 112:707–716. 110. Nagy N, Goldstein AM. Endothelin-3 regulates neural crest cell proliferation and differentiation in the hindgut enteric nervous system. Dev Biol 2006, 293:203–217. 111. Howard MJ. Mechanisms and perspectives on differentiation of autonomic neurons. Dev Biol 2005, 277:271–286. 112. Zhu L, Lee HO, Jordan CS, Cantrell VA, SouthardSmith EM, Shin MK. Spatiotemporal regulation of endothelin receptor-B by SOX10 in neural crestderived enteric neuron precursors. Nat Genet 2004, 36:732–737. 113. Kelsh RN. Sorting out Sox10 functions in neural crest development. Bioessays 2006, 28:788–798. 114. Van de Putte T, Francis A, Nelles L, van Grunsven LA, Huylebroeck D. Neural crest-specific removal of Zfhx1b in mouse leads to a wide range of neurocristopathies reminiscent of Mowat-Wilson syndrome. Hum Mol Genet 2007, 16:1423–1436. 115. Auricchio A, Griseri P, Carpentieri ML, Betsos N, Staiano A, Tozzi A, Priolo M, Thompson H, Bocciardi R, Romeo G, et al. Double heterozygosity for a RET substitution interfering with splicing and an © 2012 Wiley Periodicals, Inc. Volume 2, January/February 2013 WIREs Developmental Biology Hirschsprung disease EDNRB missense mutation in Hirschsprung disease. Am J Hum Genet 1999, 64:1216–1221. reflux and a balanced translocation t(3;17)(p12;q11). Eur J Hum Genet 2009, 17:483–490. 116. Carrasquillo MM, McCallion AS, Puffenberger EG, Kashuk CS, Nouri N, Chakravarti A. Genome-wide association study and mouse model identify interaction between RET and EDNRB pathways in Hirschsprung disease. Nat Genet 2002, 32:237–244. 128. Jiang Q, Ho YY, Hao L, Nichols Berrios C, Chakravarti A. Copy number variants in candidate genes are genetic modifiers of hirschsprung disease. PLoS One 2011, 6:e21219. 117. McCallion AS, Stames E, Conlon RA, Chakravarti A. Phenotype variation in two-locus mouse models of Hirschsprung disease: tissue-specific interaction between Ret and Ednrb. Proc Natl Acad Sci USA 2003, 100:1826–1831. 118. Maka M, Stolt CC, Wegner M. Identification of Sox8 as a modifier gene in a mouse model of Hirschsprung disease reveals underlying molecular defect. Dev Biol 2005, 277:155–169. 119. Wallace AS, Schmidt C, Schachner M, Wegner M, Anderson RB. L1cam acts as a modifier gene during enteric nervous system development. Neurobiol Dis 2010, 40:622–633. 120. Wallace AS, Tan MX, Schachner M, Anderson RB. L1cam acts as a modifier gene for members of the endothelin signaling pathway during enteric nervous system development. Neurogastroenterol Motil 2011, 23:e510–e522. 121. Uesaka T, Enomoto H. Neural precursor death is central to the pathogenesis of intestinal aganglionosis in Ret hypomorphic mice. J Neurosci 2010, 30:5211–5218. 122. Young HM, Newgreen D. Enteric neural crest-derived cells: origin, identification, migration, and differentiation. Anat Rec 2001, 262:1–15. 123. Emison ES, McCallion AS, Kashuk CS, Bush RT, Grice E, Lin S, Portnoy ME, Cutler DJ, Green ED, Chakravarti A. A common sex-dependent mutation in a RET enhancer underlies Hirschsprung disease risk. Nature 2005, 434:857–863. 124. Emison ES, Garcia-Barcelo M, Grice EA, Lantieri F, Amiel J, Burzynski G, Fernandez RM, Hao L, Kashuk C, West K, et al. Differential contributions of rare and common, coding and noncoding Ret mutations to multifactorial Hirschsprung disease liability. Am J Hum Genet 2010, 87:60–74. 125. Edery P, Pelet A, Mulligan LM, Abel L, Attie T, Dow E, Bonneau D, David A, Flintoff W, Jan D, et al. Long segment and short segment familial Hirschsprung’s disease: variable clinical expression at the RET locus. J Med Genet 1994, 31:602–606. 126. Uesaka T, Nagashimada M, Yonemura S, Enomoto H. Diminished Ret expression compromises neuronal survival in the colon and causes intestinal aganglionosis in mice. J Clin Invest 2008, 118:1890–1898. 127. Griseri P, Vos Y, Giorda R, Gimelli S, Beri S, Santamaria G, Mognato G, Hofstra RM, Gimelli G, Ceccherini I. Complex pathogenesis of Hirschsprung’s disease in a patient with hydrocephalus, vesico-ureteral Volume 2, January/February 2013 129. Fu M, Sato Y, Lyons-Warren A, Zhang B, Kane MA, Napoli JL, Heuckeroth RO. Vitamin A facilitates enteric nervous system precursor migration by reducing Pten accumulation. Development (Cambridge, England) 2010, 137:631–640. 130. Kubota M, Suita S, Kamimura T, Ito Y, Szurszewski JH. Electrophysiological properties of the aganglionic segment in Hirschsprung’s disease. Surgery 2002, 131:S288–293. 131. Won KJ, Torihashi S, Mitsui-Saito M, Hori M, Sato K, Suzuki T, Ozaki H, Karaki H. Increased smooth muscle contractility of intestine in the genetic null of the endothelin ETB receptor: a rat model for long segment Hirschsprung’s disease. Gut 2002, 50:355–360. 132. Spencer NJ, Bayguinov P, Hennig GW, Park KJ, Lee HT, Sanders KM, Smith TK. Activation of neural circuitry and Ca2+ waves in longitudinal and circular muscle during CMMCs and the consequences of rectal aganglionosis in mice. Am J Physiol 2007, 292:G546–555. 133. Suzuki T, Won KJ, Horiguchi K, Kinoshita K, Hori M, Torihashi S, Momotani E, Itoh K, Hirayama K, Ward SM, et al. Muscularis inflammation and the loss of interstitial cells of Cajal in the endothelin ETB receptor null rat. Am J Physiol 2004, 287:G638–G646. 134. Schafer KH, Micci MA, Pasricha PJ. Neural stem cell transplantation in the enteric nervous system: roadmaps and roadblocks. Neurogastroenterol Motil 2009, 21:103–112. 135. Hotta R, Natarajan D, Thapar N. Potential of cell therapy to treat pediatric motility disorders. Semin Pediatr Surg 2009, 18:263–273. 136. Kruger G, Mosher J, Bixby S, Joseph N, Iwashita T, Morrison S. Neural crest stem cells persist in the adult gut but undergo changes in self-renewal, neuronal subtype potential, and factor responsiveness. Neuron 2002, 35:657–669. 137. Hotta R, Pepdjonovic L, Anderson RB, Zhang D, Bergner AJ, Leung J, Pebay A, Young HM, Newgreen DF, Dottori M. Small-molecule induction of neural crest-like cells derived from human neural progenitors. Stem Cells (Dayton, Ohio) 2009, 27:2896–2905. 138. Kawaguchi J, Nichols J, Gierl MS, Faial T, Smith A. Isolation and propagation of enteric neural crest progenitor cells from mouse embryonic stem cells and embryos. Development (Cambridge, England) 2010, 137:693–704. 139. Read AP, Newton VE. Waardenburg syndrome. J Med Genet 1997, 34:656–665. © 2012 Wiley Periodicals, Inc. 129