ANATOMY and PHYSIOLOGY for DEBRIDEMENT
advertisement

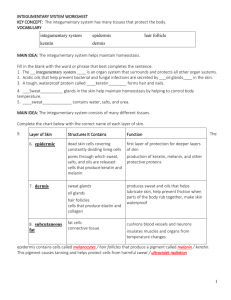
ANATOMY and PHYSIOLOGY for DEBRIDEMENT Professor Donald G. MacLellan Executive Director Health Education & Management Innovations Structures of the Skin EPIDERMIS 4 MAIN CELL TYPES: Keratinocytes - main cell type; arranged in 5 layers; perpetually being generated Melanocytes - melanin production; brown skin colour Merkel Cells - mechanoreceptor function Langerhan’s cells – immune function Stratum Germinativum • Deepest layer, in contact with dermis • Single layer of cells • Only layer of epidermis capable of cell division • Contain melanocytes Melanocytes • Capable of producing the brown pigment, melanin • Melanin can absorb energy from ultraviolet (UV) light • UV light contains high energy photons that can damage DNA – mutations • Melanin can prevent damage to DNA, helps to prevent skin cancer Stratum Spinosum • Several layers thick • Cells of this layer begin to produce keratin • Keratin is a water-insoluble protein that protects the body from water Stratum Granulosum • Multilayer and cells become compressed • Keratin crystallizes into granules within the cytoplasm • Cells are metabolically dead Stratum Lucidum • Clear layer of cells • Only present in thick skin • Cells nothing more than a bag of keratin Dermis 1. 2. Protection - physical abrasion - dehydration - ultraviolet radiation 3. Sensation - touch - vibration - pain - temperature 4. Excretion 5. Immunity/ Resistance 6. Blood Reservoir - 8 to10 % in a resting adult 7. Synthesis of vitamin D - UV light - aids absorption of calcium Dermis Papillary layer: – 1/5 of dermis – loose areolar connective tissue – Highly vascular – Dermal papillae - fingerprints Dermis Reticular layer: – Dense irregular connective tissue – Sebaceous (oil) glands – Hair follicles – Ducts of sudoriferous (sweat) glands – Meissner’s and Pacinian corpuscles Hypodermis • Attaches the reticular layer to the underlying organs • Loose connective tissue and adipose tissue • Major blood vessels Accessory organs or epidermal derivatives Hair: – Epidermal growths - for protection – 100,000 hairs on head – 100 hairs fall out daily – Sebaceous glands, arrector pili muscle, and hair root plexus (touch) – Hair growth and replacement have a cyclical pattern Nails: • Plates of highly packed, keratinized cells • Protection, scratching & manipulation • Formed by cells in nail bed called the matrix (in area of lunula) • Growth 1 mm / week • Eponychium - cuticle DEFINITIONS Endocrine - ? Exocrine - ? Merocrine - secrete into vesicles & release at cell surface Apocrine - lose part of membrane with secretion Holocrine – cell lysed with secretion Skin Glands Sebaceous (oil) glands: – Holocrine glands – Sebum is typically secreted into a hair follicle or occasionally onto the body surface. – Moistens hair and waterproofs skin – It also is quite bactericidal. – Lanolin is sheep sebum Merocrine Sweat Glands • More numerous than apocrine sweat glands. • Especially prominent on the palms, soles, and forehead. • Simple, coiled, tubular glands. • Duct empties into a funnel-shaped pore at the skin surface. • Major function of merocrine sweating is to cool the body – thermoregulation. Merocrine Sweat Glands • Merocrine sweat is a dilute watery solution of some salts (including NaCl), vitamin C, antibodies, small amounts of nitrogenous wastes (urea, uric acid, and ammonia) and lactic acid. • pH of sweat is 4-6 creating a film on the body known as the acid mantle which is bacteriostatic Apocrine Sweat Glands • Found primarily in the axillary, pubic, and anal regions of the body. – Also found in the facial region in men only. • Larger than merocrine sweat glands. • Ducts empty into hair follicles. • Apocrine sweat is thicker than merocrine sweat since it contains more lipids and proteins. • When it’s degraded by epidermal bacteria, foul odours can be produced. Apocrine Sweat Glands • Become active at puberty. • Secrete sweat during times of pain, stress, and sexual activity. • May (??) have a possible pheromone-like function. • Play no role in thermoregulation. Remember: Glands are derivatives of epithelial tissue. So even though many reside in the dermis, they are not made from connective tissue. Sensory Innervation of the Skin Physiology of Aged Skin Functional Decrement: - Epidermal turnover - Barrier function/ chemical clearance - Inflammatory response - Mechanical protection Nervous System A Dermatome is an area of skin associated with a pair of dorsal roots from the spine