Manual Therapy 16 (2011) 26e32
Contents lists available at ScienceDirect
Manual Therapy
journal homepage: www.elsevier.com/math
3rd International conference on movement dysfunction 2009
Assessing lateral stability of the hip and pelvis
Alison Grimaldi*
Physiotec Physiotherapy, 23 Weller Rd, Tarragindi, Brisbane, Queensland 4121, Australia
a r t i c l e i n f o
a b s t r a c t
Article history:
Received 28 March 2010
Received in revised form
27 August 2010
Accepted 27 August 2010
Adequate function of the hip abductor mechanism has been shown to be integral to ideal lower limb
function and musculoskeletal health. Clinical assessment of hip abductor muscle function may include
observational assessment of postural habits, muscle bulk, and of the ability to control optimal frontal
plane femoropelvic alignment during a variety of single leg tasks. Strength testing using a hand held
dynamometer is perhaps our most robust clinical assessment tool but should not be considered a ‘gold
standard’ in the assessment of abductor muscle function. Evidence from magnetic resonance imaging
(MRI), and electromyography (EMG) studies provides a deeper understanding of specific deficits that
occur within the abductor synergy. The assessment of abductor function should not be based on a single
test, but a battery of tests. The findings should be interpreted together rather than independently, and in
the context of a thorough understanding of function of the lateral stability mechanism. Manner and
comprehensiveness of abductor assessment will have important implications for management and
particularly therapeutic exercise.
Ó 2010 Elsevier Ltd. All rights reserved.
Keywords:
Hip
Abductor muscles
Assessment
1. Introduction
Deficits in hip abductor muscle morphology, strength, activation
patterns and functional control of the pelvis on the femur have
been demonstrated in those with osteoarthritis (OA) of the hip
(Sirca and Susec-Michieli, 1980; Long et al., 1993; Arokoski et al.,
2002; Sims et al., 2002; Eimre et al., 2006; Grimaldi et al.,
2009a,b). Such deficits have also been linked with medial
compartment tibio-femoral OA (Chang et al., 2005), patellofemoral
joint pain (Ireland et al., 2003; Mascal et al., 2003; Cowan et al.,
2009), and iliotibial band (ITB) syndrome (Fredericson et al.,
2000; Fairclough et al., 2007). Assessment of the abductor mechanism, and control of femoropelvic alignment, is integral to
assessment of lower limb dysfunction.
Optimal femoropelvic alignment during single leg functional
activities could be described as that where both energy expenditure
and potentially injurious forces for the lower limb are minimised.
Femoropelvic alignment in the frontal plane will be influenced
primarily by the requirement to reach equilibrium around the hip
joint whereby the forces created by the lateral stability mechanism
will balance the loads imposed by body mass acting medial to the
centre of rotation of the femoral head (Inman, 1947; Gottschalk
et al., 1989; Kummer, 1993; Lu et al., 1997; Fetto et al., 2002;
Erceg, 2009). This requires balanced activation of the complex
ˇ
ˇ
* Tel./fax: þ61 7 3342 4284.
E-mail address: info@physiotec.com.au.
1356-689X/$ e see front matter Ó 2010 Elsevier Ltd. All rights reserved.
doi:10.1016/j.math.2010.08.005
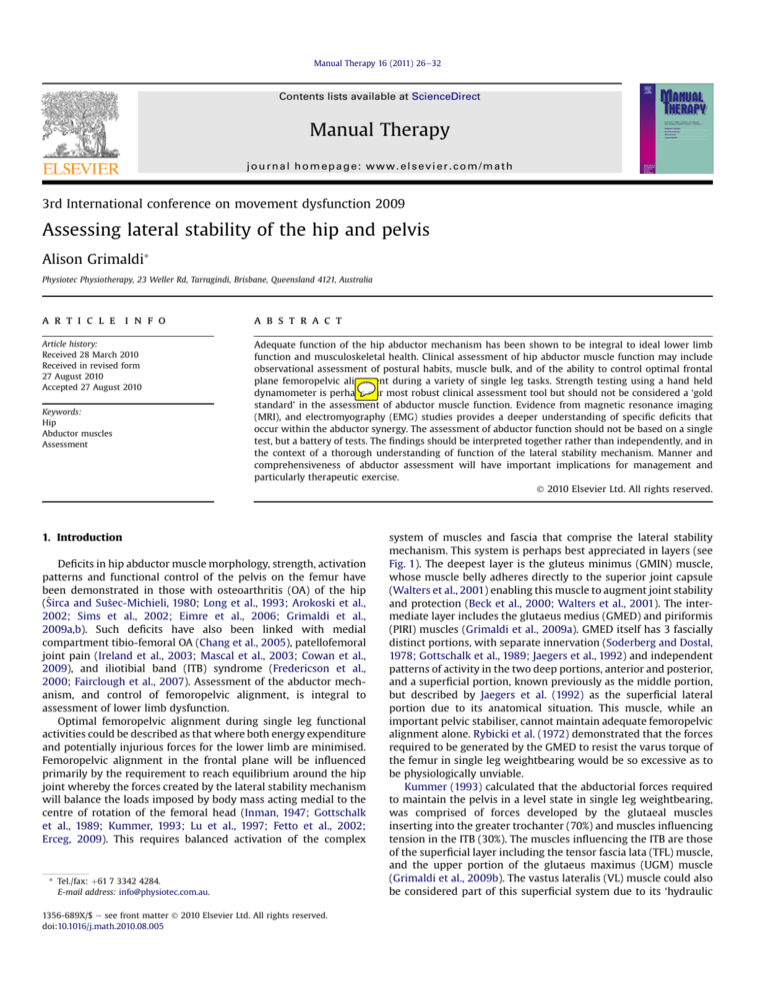
system of muscles and fascia that comprise the lateral stability
mechanism. This system is perhaps best appreciated in layers (see
Fig. 1). The deepest layer is the gluteus minimus (GMIN) muscle,
whose muscle belly adheres directly to the superior joint capsule
(Walters et al., 2001) enabling this muscle to augment joint stability
and protection (Beck et al., 2000; Walters et al., 2001). The intermediate layer includes the glutaeus medius (GMED) and piriformis
(PIRI) muscles (Grimaldi et al., 2009a). GMED itself has 3 fascially
distinct portions, with separate innervation (Soderberg and Dostal,
1978; Gottschalk et al., 1989; Jaegers et al., 1992) and independent
patterns of activity in the two deep portions, anterior and posterior,
and a superficial portion, known previously as the middle portion,
but described by Jaegers et al. (1992) as the superficial lateral
portion due to its anatomical situation. This muscle, while an
important pelvic stabiliser, cannot maintain adequate femoropelvic
alignment alone. Rybicki et al. (1972) demonstrated that the forces
required to be generated by the GMED to resist the varus torque of
the femur in single leg weightbearing would be so excessive as to
be physiologically unviable.
Kummer (1993) calculated that the abductorial forces required
to maintain the pelvis in a level state in single leg weightbearing,
was comprised of forces developed by the glutaeal muscles
inserting into the greater trochanter (70%) and muscles influencing
tension in the ITB (30%). The muscles influencing the ITB are those
of the superficial layer including the tensor fascia lata (TFL) muscle,
and the upper portion of the glutaeus maximus (UGM) muscle
(Grimaldi et al., 2009b). The vastus lateralis (VL) muscle could also
be considered part of this superficial system due to its ‘hydraulic
A. Grimaldi / Manual Therapy 16 (2011) 26e32
Fig. 1. Layers of the lateral stability mechanism of the hip as observed on an axial
magnetic resonance image through the upper pelvis. Superficial layer upper gluteus
maximus (UGM), tensor fascia lata (TFL), iliotibial band (ITB). Intermediate layer
gluteus medius (GMED) e anterior (A), middle (M) and posterior (P) portions, piriformis (PIRI). Deep layer gluteus minimus (GMIN).
amplifier’ action on the fascia lata and subsequent contribution to
lateral stability at the hip and pelvis (Vleeming et al., 1997).
Birnbaum et al. (2004) described the effect of the VL as an adjustable lever arm where contraction of this muscle increases the
distance of the ITB from the femoral shaft, thereby increasing the
tension in the ITB. The importance of this superficial system should
not be underestimated. Fetto and Austin (1994) in a cadaveric study
reported that sectioning of the capsule, GMIN, GMED, and glutaeus
maximus muscles allowed the pelvis to tilt laterally 10 from
a horizontal start position, while sectioning of the ITB alone
resulted in a marked 30 of lateral pelvic tilt. The deficiency of this
mechanism is believed to underpin the apparent difficulty above
knee amputees have with single leg stance. While below knee
amputees with ITB intact can stand without a lateral trunk list,
above knee amputees with their ITB deficiency have a positive
Trendelenburg sign and walk with a limp (Fetto et al., 2002).
Femoropelvic alignment is therefore the end result of the
complex interactions between all members of the abductor
synergy. Our ability to optimise lateral pelvic control in our patient
populations is inherently linked with our ability to assess deficits,
and tailor a management programme that adequately addresses
specific alterations in muscle size, strength, activation patterns, and
foremostly, function. This paper aims to review the clinical and
laboratory based investigations of abductor function, and implications of their findings for both assessment and management of
patients with dysfunction.
2. Clinical assessment
Clinical assessment of the lateral stability mechanism of the hip
and pelvis aims to identify abnormalities in postural habits, muscle
size and tone, and movement patterns that may reflect dysfunction
of the hip abductor muscles. Further information is gained clinically
from formal strength testing.
2.1. Standing posture
Assessment of static postures has often been criticised as having
poor association with dynamic function. It is important however to
consider what we are assessing when we assess someone’s posture
in a clinical environment. Are we assessing the patient’s perception
of ‘good posture’, or are we eliciting a realistic impression of how
this patient rests in everyday static postures? Patients will often
demonstrate for their clinician a posture they think best represents
a good standing posture. With further inquiry into what postures
the patient assumes during prolonged standing, or in a relaxed
environment, the patient often volunteers a demonstration of
27
postures that are far from our clinical ideal. The most common
potentially negative posture for the lateral hip stability mechanism
is ‘hanging on one hip’, where weight is shifted towards one side,
and the pelvis dropped down on the other, into a position of relative hip adduction. In this position the ITB is on tension and the
requirement for muscular activity is reduced. Inman (1947)
demonstrated that at 15 of hip adduction, or ‘pelvis sag’ in single
leg stance, the forces of gravity were almost entirely resisted by
fascial tension of the ITB alone. In terms of energy conservation this
may then seem to be a sensible postural habit, however over time
there may be negative consequences.
Kendall’s widely used clinical texts describe a posturally
induced ‘stretch weakness’ occurring in the hip abductor muscles
in response to standing postures in which the hip is positioned in
hip adduction, over time resulting in inner range weakness
(Kendall et al., 1952; Kendall and McCreary, 1983). Animal studies
have demonstrated that muscles immobilised in elongated positions will undergo structural change, the basis of which appears to
be to shift the optimal function of the muscle to the new, lengthened position (Goldspink, 1977; Williams and Goldspink, 1978).
These studies discovered increases in protein synthesis in skeletal
muscle, and additions of 20% or more sarcomeres in series after 3e4
weeks of immobilisation in a lengthened position. In association
with these changes, the lengthetension curve shifted so that
greater isometric tension was now able to be developed in
lengthened positions, while less tension was developed in shortened positions, relative to a control muscle (Goldspink, 1977). This
data supported Kendall’s hypothesis of ‘stretch weakness’.
Neumann et al. (1988) explored the relationship between
postural habits and muscle changes in the hip abductor muscles of
humans. They demonstrated a similar shift in the lengthetension
(hip angleetorque) relationship of hip abductor muscles held in
relatively lengthened positions.
The clinical implications of this information are that postural
habits such as ‘hanging on one hip’ in adduction, whereby the
lateral stability mechanism is held in a lengthened position, may
lead to physiological change over time within the hip abductor
muscles. These changes will result in optimal muscle function in
a position of relatively greater hip adduction, or a more elongated
position. While postural habits in this region are difficult to
measure objectively in either a clinical or research environment,
assessing these habits provides information that is important for
both the clinical reasoning process in terms of understanding
pathomechanics, and to long term outcomes of intervention.
Weightbearing in an excessively adducted hip position will result in
increased joint forces (McLeish and Charnley, 1970; Kummer, 1993),
and has been demonstrated to occur during the stance phase of gait
in patients with early hip joint pathology (Watelain et al., 2001).
While it is unknown whether such changes in abductor function are
the product of, or impetus for, degenerative joint changes, the
evidence provided by Kummer (1993) and McLeish and Charnley
(1970) suggests that increases in postural and functional adduction will be negative for the underlying joint.
A further example of the impact of postural habits on pathomechanics and long term outcomes would be in patients with
GMED tendinopathy. Compression has been well accepted as an
important aetiological factor in the development of insertional
tendinopathies or enthesopathies (Almekinders et al., 2003; Cook
and Purdam, 2009). Birnbaum et al. (2004) have clearly demonstrated that adduction of the hip rapidly increases the compressive
loading of the ITB over the greater trochanter, into which the GMED
tendon inserts. Therefore, standing for prolonged periods ‘hanging
on one hip’ in a position of hip adduction would represent
a significant amount of compressive loading on the GMED tendon,
particularly for those who have been employed in a standing
28
A. Grimaldi / Manual Therapy 16 (2011) 26e32
occupation over many years. Other postural habits such as sitting
cross-legged in hip adduction, and sleeping in sidelying in hip
flexion/adduction will add to this cumulative compressive loading.
Exercise interventions aimed at optimising hip abductor function
should provide at least short term benefits from this condition.
Research studies show us however that patients struggle to maintain an exercise programme for more than 12 weeks (vanBaar et al.,
2001). If the postural habits involving excessive hip adduction
remain, the lengthetension curve will revert to optimal function in
hip adduction, compressive loading of the GMED tendon will again
increase, and the pain is likely to return. Assessing and retraining
poor postural habits in such conditions should be an important
consideration for the clinician aiming to achieve positive long term
outcomes.
2.2. Resting muscle bulk and ‘stiffness’
Fig. 2. Profile of the quadriceps in a patient with poor hip abductor muscle function.
Note the increase in bulk in the upper portion of the vastus lateralis. This is disproportionate to the general quadriceps bulk, and may be a reflection of a compensatory
increase in recruitment of the vastus lateralis, and the superficial lateral stability
mechanism.
shifts in centre of pressure measures that have been demonstrated
as part of a normal ‘load/unload’ mechanism in symmetrical side by
side stance (Winter et al., 1996). In those with hip OA, studies have
shown a shift towards tonic activity (Long et al., 1993) and loss of
type II phasic muscle fibres in superficial hip abductor muscles (Sirca
and Susec-Michieli, 1980). Furthermore, co-contraction strategies,
where left and right GMED muscles activate simultaneously rather
than reciprocally have been linked with the development of lower
back pain (Nelson-Wong et al., 2008).
Observations of abnormal asymmetry or hypertrophy of the
superficial musculature, and palpation of abnormal co-contraction,
tonic activity, or stiffness of the superficial lateral musculature
during quiet balanced standing, are often the first indications
during the assessment process, that muscle dysfunction exists.
Abnormal findings should prompt further examination, and be
used in building a picture of abductor function or dysfunction.
ˇ
ˇ
Assessment of muscle size and tone or ‘stiffness’ as performed
routinely in a clinical environment, through visual inspection and
palpation, would not hold up to academic rigour. Should we then
discard this part of our clinical examination? While no reliance
should be placed on this examination alone, clinical assessment of
muscle size, asymmetry, and stiffness can provide supplementary
information, reflective of muscle usage, which may help guide, or
strengthen findings from functional assessments, and more traditional strength tests. Muscle size, asymmetry and stiffness will be
closely associated with activity levels, particular actions and
symmetry of occupational or sporting pursuits, or a change in
loading or specific muscle activity patterns related to pain or
pathology. Increases in TFL bulk are often noted in clinical assessment in those with abductor dysfunction, however clinicians
should also ensure there is close visual inspection of the UGM and
VL, the other members of the superficial layer of the abductor
synergy, as these muscles may also demonstrate relative hypertrophy. Fig. 2 is an example of hypertrophy of the VL muscle,
particularly the superior portion, in a patient with GMED tendinopathy and associated hip abductor dysfunction. While much
further research is required to clearly elucidate the role the VL
muscle plays in the lateral stability mechanism, early links have
been made in those with patellofemoral pain. This population has
demonstrated both dysfunction of the VL, and of the hip abductor
musculature (Ireland et al., 2003; Mascal et al., 2003; Cowan et al.,
2009). Assessment of the VL muscle not only in patients with
patellofemoral pain, but also in patients with hip abductor
dysfunction, is suggested as part of a thorough clinical examination.
Increased tone or stiffness of muscles of the abductor synergy
may also be noted on palpation during the postural assessment.
Johansson et al. (1991) described two main determinants of muscle
‘stiffness’, firstly the muscles inherent visco-elastic properties
including existing actin and myosin bonds, and secondly neural
control mechanisms including both feedforward and feedback
mechanisms, both driven by the muscle spindle unit. Background
activity is maintained by the feedforward system whereby the
central nervous system (CNS) provides stimulus for the muscle
spindle unit. By this mechanism, activity of deeper muscles which
generally have higher densities of muscle spindles (Peck et al.,1984),
is characterised as tonic in nature (Richardson et al., 2004). More
superficial muscles generally have better moment arms for torque
production, have lower densities of muscle spindles, higher
percentages of fast twitch fibres, and a more phasic pattern of
activity. Surface electromyography (EMG) recording from lateral hip
musculature has shown normal reciprocal phasic low level activity
during bilateral standing (Nelson-Wong et al., 2008). Left and right
musculature alternate their activity in an oneoff strategy (NelsonWong et al., 2008). This is consistent with reciprocal medio-lateral
2.3. Dynamic functional assessment
Dynamic assessment may typically involve single leg stance,
single leg squat, gait, stair-climbing, running, hopping and other
A. Grimaldi / Manual Therapy 16 (2011) 26e32
higher level functional tasks specific to the level of function, or
sport played by the individual. Of primary interest with respect to
assessment of the lateral stability mechanism, is the ability of the
individual to control femoropelvic alignment in the frontal plane.
The hip abductor muscles have been shown to be primarily
employed in control of medio-lateral stability in standing (Winter
et al., 1996), and links with pathology have been established with
respect to changes in normal control of the pelvis on the femur in
the frontal plane (Krebs et al., 1998; Watelain et al., 2001).
The traditional Trendelenburg test assesses the frontal plane
orientation of the pelvis and trunk. An ‘uncompensated’ positive
test result is described as pelvic tilt occurring towards the nonweightbearing side and a ‘compensated’ positive test as trunk
lateral flexion towards the weightbearing side during single leg
stance. The modified Trendelenburg test described by Hardcastle
and Nade (1985) involves maximal active elevation of the nonweightbearing side of the pelvis, while the trunk is maintained in
an upright position. An abnormal test result is an inability to
maximally elevate the pelvis, or to maintain maximal elevation for
30 s. In addition, these authors demonstrated that the hip flexion
angle of the non-weightbearing side significantly influences test
results. At 90 hip flexion, a downward pelvic tilt on this side was
never observed, resulting in false negative results. Their suggestion
was that the non-weightbearing leg should be held between 0 and
30 hip flexion during testing.
In both of the above versions the assessment of pelvic tilt,
without consideration of lateral shift of the pelvis in the frontal
plane, may underestimate abductor dysfunction. More recent
versions of the Trendelenburg test have used both laboratory based
2 dimensional kinematic analysis (Asayama et al., 2002; DiMattia
et al., 2005) or the simple clinical tool, the universal goniometer
(Youdas et al., 2007) to study hip adduction angle as that angle
produced by a line between the anterior superior iliac crests, and
the line of the femur, while the trunk is maintained upright. This
measurement accounts for both lateral pelvic tilt, and lateral pelvic
shift.
Increase in hip adduction angle moving from double to single
leg stance in normal subjects was reported as an average 5 by
DiMattia et al. (2005) with values for hip adduction increasing from
10 4 (mean standard deviation) in bilateral stance to 15 4
in single leg stance. Reflective markers identifying the anterior
superior iliac spines (ASIS) and the lateral femoral condyle were
used for their 2 dimensional analysis. Asayama et al. (2002) using
the 3SPACE magnetic sensor system with markers at both the ASISs
and the tibial tuberosity reported a mean increase of 2 of hip
adduction (range 2 abduction to 12 adduction) in normal healthy
subjects 30 s after moving from bilateral stance (0 hip adduction)
to unilateral stance. Youdas et al. (2007), using the universal
goniometer, also measured hip adduction angle after standing for
30 s on one leg. One arm of the goniometer was placed along a line
between the ASISs, with the other directed towards a midpoint
between medial and lateral femoral condyles. Mean average values
were 83 3 (range 76e94 ) for 90 normal subjects. As this
measure was reported as the ‘inside angle’ between the 2 arms of
the goniometer, rather than a true measure of hip adduction, to
compare to the previous 2 results the angles need to be inverted
(subtracted from 90 ). Mean average angles of hip adduction
therefore would be 7 3 (range 4 abduction to 14 adduction).
These authors reported an intratester reliability (ICC3,1) of 0.58,
with a standard error of measure of 2 . Furthermore they calculated
the minimally detectable change to be 4 , meaning that a change of
more than 4 would be necessary to conclude that there has been
a change in performance. Their conclusion was that, due to inadequate sensitivity, the usefulness of the Trendelenburg test is
questionable in assessing hip abductor muscle performance and
29
changes in that performance over time, in young healthy adults. A
recent paper by the same authors (Youdas et al., 2010) examined
subjects with early hip OA using this same test. The test results
were not significantly different to a control population and therefore the test was not recommended as a test to identify patients
with hip OA.
The use of a simple goniometer to measure a single angle does
not however reflect the complexities of this task. Standing on one
leg is accomplished by bringing the centre of mass over the base of
support. This may result in changes not only in the angle of hip
adduction, but also trunk position and even arm position. Youdas
et al. (2010) attempted to eliminate trunk compensation by
‘reminding the subject to keep his or her trunk erect’. We have no
assurance however that the subject did in fact achieve this, as no
analysis of trunk position was reported. Shifts in the centre of mass
may be achieved by trunk lateral flexion which is perhaps more
obvious to visual assessment, but also subtle lateral shifts. Youdas
et al. (2010) also did not standardise or control arm position.
Arms were allowed to be held out away from the side, again
allowing alterations of the centre of mass. These authors then have
demonstrated, not that the usefulness of the Trendelenburg test is
questionable, but that a simple measure of hip adduction angle
during single leg standing, without assessment or proven control of
other segmental factors, is not sensitive enough to identify
dysfunction associated with early joint pathology.
DiMattia et al. (2005) using a visual rating scale for hip adduction during performance of a single leg squat, demonstrated high
specificity but low sensitivity of the investigators ability to determine if more than 10 increase of hip adduction had occurred
during a single leg squat task. The low sensitivity suggests that
a patient may be performing inadequately and not be detected
visually. Inter-rater reliability was low to fair, with raters in
agreement primarily only when they did not see excessive hip
adduction. The authors suggest as a limitation of their study
however that low variability inherent in their healthy active sample
population may have negatively influenced these results.
DiMattia et al. (2005) also assessed the relationship between
isometric hip abduction strength, and hip adduction angles
measured in either the Trendelenburg test or the single leg squat
task. The authors found poor correlation between hip abductor
muscle strength and both static and dynamic adduction angles, and
concluded these functional tests should not be used as a reflection
of hip abductor strength, and that their usefulness in screening hip
abductor strength is limited. No evidence is apparent at present in
the literature that describes the correlation of these functional tests
and abductor strength testing in patient populations.
Overall, the scientific data available to date appears to provide
little support for the usefulness of clinical assessments of single leg
function, and validity of these tests as a reflection of abductor
muscle strength. This conclusion regarding validity however relies
on two assumptions, firstly that hip adduction angle in single leg
tasks is an accurate representation of abductor muscle function,
and secondly that hip abductor muscle strength is the truest
reflection of hip abductor function, and our ‘gold standard’ for
comparison. If we examine these tests a little more closely it is
apparent that these two tests provide quite different, and yet
complimentary information. A strength test performed from
a neutral joint position, typical of research studies (Arokoski et al.,
2002; Sims et al., 2002; DiMattia et al., 2005; Youdas et al., 2007),
provides unidimensional information on torque production at this
hip angle, the validity of which will be impacted upon by pain in
a symptomatic group (Further discussion on this test is provided in
the next section.).
In contrast, the Trendelenburg test reflects the patients ‘self
selected’ strategy for achieving balance in single leg function.
30
A. Grimaldi / Manual Therapy 16 (2011) 26e32
During motor planning, strength alone will not determine hip
adduction angle selected. With the natural drive to minimise
energy expenditure, an important consideration will be the optimal
hip angleetorque relationship for that individual (which postural
habits may strongly influence). If the optimal resting muscle length
has shifted, possibly secondary to habitually resting in a lengthened
position, greater hip adduction angles may be selected and therefore trunk position will be adjusted to achieve equilibrium. The
amount of compressive loading abductor muscle contraction
creates across a painful joint has also been suggested to be a potent
modifier of segmental alignment during function in patients with
hip OA. Krebs et al. (1998) demonstrated that the peak of acetabular
loading occurred not at the point of maximum ground reaction
force, but at the peak of GMED activity. The authors concluded that
the use of trunk lateral flexion during stance phase of gait in
subjects with advanced hip OA was an offloading strategy to
minimise GMED contraction and therefore painful joint loading.
Kapandji (1987) referred to this gait pattern with trunk compensation as Duchenne limping. During assessment of single leg
function then, it will be equally important to assess both hip
adduction angle, and segmental compensatory strategies such as
trunk lateral flexion, and trunk lateral shift which may be subtle
and missed if careful attention is not directed towards this, and
shoulder abduction. Taking the ipsilateral arm out to the side will
shift the centre of mass towards the weightbearing leg and reduce
the abductor muscle requirement.
Based on the above information, clinical approaches for optimising the value of the Trendelenburg test may include the
following. Assessment of single leg stance should occur with the
non-weightbearing leg between 0 and 30 of flexion. Arm position
should be standardised, for example arms held against the body or
crossed across the chest. Trunk translation in the frontal plane
relative to the pelvis should ideally be quantified. One method may
be to establish the relative positions of the sternal notch and
a midway point between ASISs. A goniometer centred over this
midway point with one arm aligned with the true vertical, and the
other directed towards the sternal notch would provide an indication of relative trunk position. Asking the patient to then attempt
to correct their position by bringing their pelvis to a horizontal
position and/or their trunk to a vertical position, may provide
further information regarding the mechanism for altered position.
Is this a compensatory strategy related to changes in muscle
function, or an antalgic strategy? Active correction that is just
difficult but not painful may reflect a compensatory strategy, while
a painful response to correction could reflect an antalgic ‘offloading’
mechanism. This response will have relevance to the chosen
management approach regarding appropriate re-loading strategies.
2.4. Abductor muscle strength
Isometric muscle strength testing is the most commonly
employed tool for assessing abductor muscle function. Hand held
dynamometry has been shown to be a reliable measure of hip
abductor strength in either supine or sidelying (Bohannon, 1997;
DiMattia et al., 2005; Youdas et al., 2008). This test provides information on the ability of the abductor synergy as a whole to generate
torque. The inherent nature of a global muscle test increases the risk
of false negatives in which muscle dysfunction exists and yet is not
detectable. Individual changes may occur within the abductor
synergy whereby one member of the synergy is inhibited and
reduces its contribution, while another member may be overactive
and increases its contribution, resulting in a nil net effect. This may
explain in part the considerable variability that has been reported
across many studies that have used abductor strength testing to
determine function in those with hip OA. While some authors have
reported abductor strength deficits of up to 31% (Murray and Sepic,
1968; Jandric, 1997; Arokoski et al., 2002), others have reported no
significant difference (Teshima, 1994; Sims et al., 2002). Other
factors such as stage of pathology, pain, fear of pain, motivation, and
neuromotor dysfunction all potentially impact upon the outcome
of strength testing. All considered, the difficulty in correlating
strength and the performance on the functional Trendelenburg test
is not surprising (DiMattia et al., 2005).
The information gained from strength testing will be enhanced
by multiangle testing. As discussed earlier, ‘stretch weakness’ may
be evident on a strength test performed in inner range abduction,
while this same patient may be relatively stronger than their
unaffected side when tested in a position of hip adduction (Kendall
and McCreary, 1983; Neumann et al., 1988; Sahrmann, 2002).
Optimal strength testing procedures therefore would include
testing not only in neutral but also in 10 adduction (Neumann et al.,
1988), and inner range abduction. Warm up and a submaximal test
run may also serve to reduce fear and improve performance in
patients with pain. The clinician should try to motivate the patient
to perform a maximal effort, and record pain experienced by the
patient prior to and during the testing procedure. A measure of
perceived exertion such as the Borg CR 100 scale (Borg and Borg,
2002) can also be a useful comparison between sides for an individual and a measure of progress for that individual over time.
The manner in which a patient freely performs an active
movement can also provide clinical information. The evaluation of
sidelying active hip abduction has been described by Sahrmann
(2002), and also recently as a screening tool for occupational low
back pain by Nelson-Wong et al. (2009). These authors used a rating
scale regarding the subject’s ability to maintain lower limbs, pelvis,
trunk, and shoulders in the frontal plane during performance of
sidelying hip abduction, with knee extended. The score ranges from
0, no loss of frontal plane position, to 3, severe loss of frontal plane
alignment (Nelson-Wong et al., 2009). Lack of ability to maintain
frontal plane alignment will reflect the patients level of trunk
control, but also substitution strategies associated with abductor
dysfunction. Active movement testing will provide additional
information within a battery of tests, and may be particularly
helpful in those patients who are unable, due to pain, to perform
a formal resisted strength test. Similar to a strength measure, pain
and exertion scores can also be gathered.
The information provided to this point has related to clinical
testing procedures, each test reflecting different aspects of hip
abductor muscle function and dysfunction. No single test should be
relied upon, as the development of a clinical picture will be
strengthened when consistencies can be appreciated across
a number of tests. The sections below relate to additional scientific
investigations of hip abductor function that while not generally
accessible in a clinical situation, provide further valuable insight
into the understanding of the lateral stability mechanism under
normal and pathological conditions.
3. Laboratory based assessments
3.1. Magnetic resonance imaging (MRI) assessment of muscle
function
Information from functional MRI throws a little more light on
the discrepancies between functional and strength testing of the
hip abductor muscles. In studying activity of the GMIN, and deep
and superficial layers of the GMED muscle, Kumagai et al. (1997)
demonstrated that the activity levels of these differing portions of
the abductor synergy were not homogeneous, and were influenced
by the degree of hip adduction in which these muscles were
recruited. While GMIN was substantially active regardless of the
A. Grimaldi / Manual Therapy 16 (2011) 26e32
position of the hip in the frontal plane, the GMED was much less
active if the abductors were activated in a position of hip abduction.
When activated in a neutral hip position, the deeper fibres of GMED
increased their activity, while the superficial fibres became most
active only once the hip was in a position of 20 hip adduction. It
was in this position that the GMED muscle was reported to provide
maximal contribution to abduction force (Kumagai et al., 1997).
Lack of adequate contribution by the deeper abductors, GMIN and
the deep anterior and posterior portions of GMED could then
theoretically drive increases in functional hip adduction allowing
increased contribution from the more superficial fibres of GMED,
and the superficial layer of the abductor synergy to reach equilibrium against gravitational loading. While specific deficits have been
demonstrated in deep muscles of the trunk in association with low
back pain (Hides et al., 1994, 2008), inadequate scientific evidence
currently exists to elucidate specific deficits in deep hip musculature in association with hip pain. For the researcher, Kumagai et al.’s
(1997) findings may assist in directing future studies, while for the
clinician this information reinforces the need for close attention to
femoropelvic alignment and compensatory strategies both during
assessment and therapeutic exercise.
3.2. MRI assessment of muscle size
The scientific study of muscle size using MRI provides much
more reliable information than an observational evaluation during
a clinical assessment. Arokoski et al. (2002) demonstrated that
a combined cross sectional area measure of all of the abductor
synergists (TFL, UGM, PIRI, GMED, GMIN) was significantly smaller
around the worst affected hip in subjects with bilateral OA of the
hip. Further examination by Grimaldi et al. (2009a,b) of size of
individual muscles within the synergy in subjects with hip OA,
revealed heterogeneous changes. In subjects with unilateral
advanced hip OA, the deeper abductor synergists GMED, PIRI, and
GMIN were smaller around the affected hip (Grimaldi et al., 2009a),
while the superficial synergists TFL and UGM appeared to maintain
their size on the side of pathology (Grimaldi et al., 2009b). In
subjects with mild unilateral hip OA, most assessments of size found
no significant difference except for the finding that the GMED
muscle was significantly larger on the affected side compared to the
GMED of control subjects (Grimaldi et al., 2009a). As patients with
early hip OA have been reported to use increased functional hip
adduction (Watelain et al., 2001), the larger GMED may be explained
by relatively increased activation of the superficial portion of this
muscle in a position of adduction (Kumagai et al., 1997).
3.3. EMG
In support of this hypothesis, research using surface EMG has
shown that subjects with earlier hip OA have increased levels of
GMED EMG activity during functional weightbearing tasks (Sims
et al., 2002). Surface EMG will be reflective primarily of activity in
the superficial fibres of the GMED muscle. This finding of increased
GMED activity is in contrast to the general clinical expectation of
GMED inhibition in subjects with hip pathology. This has in fact
only been demonstrated in subjects with advanced OA (Long et al.,
1993), where these muscles are antalgically offloaded through
trunk lateral flexion over the weightbearing leg during gait (Krebs
et al., 1998). This information on size and EMG changes in GMED
suggests that the appropriateness of using surface EMG in a clinical
situation for facilitating GMED activity should be carefully evaluated for each patient. Furthermore, pure strengthening as a rationale for development of therapeutic exercise prescription for
patients with hypertrophy and increased GMED activity associated
with early hip joint pathology, should be re-examined. Gossman
31
et al. (1982) in their review of length associated changes in
muscle concluded that ‘the emphasis of the correction programme
should be on restoring normal length and developing tension at the
appropriate point in the range rather than on just strengthening
the muscle’.
4. Clinical implications and conclusions
For those with pain associated with hip abductor dysfunction,
our ability as clinicians to impart both short and long term positive
change will be dependent on our ability to adequately assess the
lateral stability mechanism. The assessment of abductor function
should not be based on a single test, but a battery of tests. The
findings should be interpreted together rather than independently,
and in the context of a thorough understanding of function of the
lateral stability mechanism. The evidence covered in this paper
builds a picture that clearly demonstrates the close association
between hip abductor function and segmental alignment of the
femur, pelvis and trunk. This paper has discussed the potent effect
daily postural habits may have on hip abductor muscle structure
and function. A postural assessment should fully explore not only
how well a patient can stand on two feet, but the positions the
patient uses in everyday life. Identifying negative postural habits
such as standing ‘hanging on one hip’ in adduction, or with the legs
crossed in bilateral adduction, and working with the patient to
effect long term change may have significant impact not only on
short term, but on long term outcomes.
Hypertrophy, or increased resting muscle tone in the superficial
musculature of the lateral hip and thigh may provide impetus for
further assessment, and weight to a hypothesis of abductor
impairment. Assessment of single leg function requires close
attention to not only lateral pelvic tilt but also lateral pelvic shift
(measurable together as hip adduction angle), trunk position, arm
position, and position of the non-weightbearing leg. All of these
factors may strongly influence interpretation of these tests. Muscle
strength tests will provide maximum information if they are
undertaken as a multiangle test able to reveal ‘stretch weakness’, or
weakness in specific ranges that may be otherwise missed and
erroneously evaluated as ‘normal’.
Manner and comprehensiveness of abductor assessment will
have important implications for management and particularly
therapeutic exercise. Looking at midrange strength alone for
example may result in a patient with no loss of strength here, and yet
significant abductor dysfunction, receive no intervention. Similarly,
consideration of lateral pelvic tilt alone in the Trendelenburg test,
may result in a false negative test and no intervention, where the
patient may be achieving their position of equilibrium with lateral
pelvic shift, alteration in trunk position, or subtle combinations of
both. Careful consideration should be given to appropriate rehabilitation strategies for a patient who uses increased functional adduction in single leg stance, has increased superficial abductor muscle
bulk and activity, and tests stronger than the unaffected side in
neutral and hip adduction. Therapeutic exercise based on pure
strengthening, or single leg exercises where functional hip adduction
is not adequately controlled, may for the short term improve the
efficiency of the superficial system and control symptoms in some
conditions. In the longer term however high loads in hip adduction
will have negative impacts on the underlying joint, and the glutaeal
tendons sitting beneath the ITB.
The future will hopefully bring technological advancements that
make clinical assessment of functional weightbearing tasks simple,
rapid and yet comprehensive. In the meantime, the use of the
battery of tests described in this paper provides us best guidance
for both assessment and targeted management of abductor muscle
dysfunction.
A. Grimaldi / Manual Therapy 16 (2011) 26e32
Almekinders L, Weinhold P, Maffulli N. Compression etiology in tendinopathy.
Clinics in Sports Medicine 2003;22:703e10.
Arokoski MH, Arokoski JPA, Haara M, Kankaanpaa M, Vesterinen M, Niemitukia LH,
et al. Hip muscle strength and muscle cross sectional area in men with and
without hip osteoarthritis. Journal of Rheumatology 2002;29:2185e95.
Asayama I, Naito M, Fujisawa M, Kambe T. Relationship between radiographic
measurements of reconstructed hip joint position and the Trendelenburg sign.
The Journal of Arthroplasty 2002;17:747e51.
Beck M, Sledge J, Gautier E, Dora C, Ganz R. The anatomy and function of the gluteus
minimus muscle. Journal of Bone and Joint Surgery British 2000;82B(2):
358e63.
Birnbaum K, Siebert CH, Pandorf T, Schopphoff E, Prescher A, Niethard FU.
Anatomical and biomechanical investigations of the iliotibial tract. Surgical and
Radiological Anatomy 2004;26:433e46.
Bohannon RW. Reference values for extremity muscle strength obtained by handheld dynamometry from adults aged 20e79 years. Archives of Physical Medicine and Rehabilitation 1997;78:26e32.
Borg E, Borg G. A comparison of AME and CR100 for scaling perceived exertion. Acta
Physiologica 2002;109:157e75.
Chang A, Hayes K, Dunlop D, Song J, Hurwitz D, Cahue S, et al. Hip abduction
moment and protection against medial tibiofemoral osteoarthritis progression.
Arthritis and Rheumatism 2005;52(11):3515e9.
Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to
explain the clinical presentation of load-induced tendinopathy. British Journal
of Sports Medicine 2009;43:409e16.
Cowan SM, Crossley KM, Bennell KL. Altered hip and trunk muscle function in
individuals with patellofemoral pain. British Journal of Sports Medicine
2009;43:584e8.
DiMattia M, Livengood A, Uhl T, Mattaclola C, Malone T. What are the validity of the
single-leg-squat test and its relationship to hip-abduction strength? Journal of
Sport Rehabilitation 2005;14:108e23.
Eimre M, Puhke R, Alev K, Seppet E, Sikkut A, Peet N, et al. Altered mitochondrial
apparent affinity for ADP and impaired function of mitochondrial creatine
kinase in gluteus medius of patients with hip osteoarthritis. American Journal
of Physiology Regulatory, Integrative and Comparative Physiology
2006;290:R1274e5.
Erceg M. The influence of femoral head shift on hip biomechanics: additional
parameters accounted. International Orthopaedics 2009;33:95e100.
Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. Is iliotibial
band syndrome really a friction syndrome? Journal of Science and Medicine in
Sport 2007;10:74e6.
Fetto JF, Austin KS. A missing link in the evolution of THR: “discovery” of the lateral
femur. Orthopedics 1994;17:347e51.
Fetto J, Leali A, Moroz A. Evolution of the Koch model of the biomechanics of the
hip: clinical perspective. Journal of Orthopaedic Science 2002;7:724e30.
Fredericson M, Cookingham C, Chaudhari A, Dowdell B, Oestreicher N, Sahrmann S.
Hip abductor weakness in distance runners with iliotibial band syndrome.
Clinical Journal of Sport Medicine 2000;10:169e75.
Goldspink DF. The influence of immobilization and stretch on protein turnover of
rat skeletal muscle. Journal of Physiology (London) 1977;264:267e82.
Gossman MR, Sahmann SA, Rose SJ. Review of length-associated changes in muscle.
Physical Therapy 1982;62(12):1799e807.
Gottschalk F, Kourosh S, Leveau B. The functional anatomy of tensor fascia latae and
gluteus medius and minimus. Journal of Anatomy 1989;166:179e89.
Grimaldi A, Richardson C, Stanton W, Durbridge G, Donnelly W, Hides J. The
association between degenerative hip joint pathology and size of the gluteus
medius, gluteus minimus and piriformis muscles. Manual Therapy 2009a;14:
605e10.
Grimaldi A, Richardson C, Hides J, Donnelly W, Durbridge G, Darnell R. The
association between degenerative hip joint pathology and size of the gluteus
maximus and tensor fascia lata muscles. Manual Therapy 2009b;14:611e7.
Hardcastle P, Nade S. The significance of the trendelenburg test. Journal of Bone and
Joint Surgery British 1985;67B:741e6.
Hides J, Gilmore C, Stanton W, Bohlscheid E. Multifidus size and asymmetry among
chronic LBP and healthy asymptomatic subjects. Manual Therapy 2008;13:43e9.
Hides J, Stokes M, Saide M, Jull G, Cooper D. Evidence of lumbar multifidus muscle
wasting ipsilateral to symptoms in patients with acute/subacute low back pain.
Spine 1994;19:165e72.
Inman V. Functional aspects of the abductor muscles of the hip. Journal of Bone and
Joint Surgery 1947;29:607e19.
Ireland M, Wilson J, Ballanytne B, Davis I. Hip strength in females with and without
patellofemoral pain. Journal of Orthopaedic and Sports Physical Therapy
2003;33(11):671e6.
Jaegers S, Dantuma R, deJongh H. Three dimensional reconstruction of the hip on
the basis of magnetic resonance images. Surgical and Radiologic Anatomy
1992;14:241e9.
Jandric S. Muscule parameters in coxarthrosis. Medicinski Pregled 1997;50(7e8):
301e4.
Johansson H, Sjölander P, Sojka P. Receptors in the knee joint and their role in the
biomechanics of the joint. CRC Critical Reviews in Biomedical Engineering
1991;18:341e68.
Kapandji IA. The physiology of the joints. Edinburgh: Churchill Livingstone; 1987.
Kendall HO, Kendall FP, Boynton DA. Posture and pain. Baltimore, MD: Williams and
Wilkins; 1952.
Kendall FP, McCreary EK. Muscles: testing and function. 3rd ed. Baltimore, MD:
Williams and Wilkins; 1983.
Kumagai M, Shiba N, Higuchi F, Nishimura H, Inoue A. Functional evaluation of hip
abductor muscles with use of magnetic resonance imaging. Journal of Orthopaedic Research 1997;15:888e93.
Kummer B. Is the Pauwels theory of hip biomechanics still valid? A critical analysis,
based on modern methods. Annals of Anatomy 1993;175:203e10.
Krebs DE, Robbins CE, Lavine L, Mann RW. Hip biomechanics during gait. Journal of
Orthopaedic and Sports Physical Therapy 1998;28(1):51e9.
Long W, Dorr L, Healy B, Perry J. Functional recovery of noncemented total hip
arthroplasty. Clinical Orthopaedics and Related Research 1993;288:73e7.
Lu T, Taylor SJG, O’Connor JJ, Walker PS. Influence of muscle activity on the forces in
the femur. Journal of Biomechanics 1997;30:1101e6.
Mascal C, Landel R, Powers C. Management of patellofemoral pain targeting hip,
pelvis and trunk muscle function: 2 case reports. Journal of Sports and Physical
Therapy 2003;33(11):647e60.
McLeish R, Charnley J. Abduction forces in the one-legged stance. Journal of
Biomechanics 1970;3:191e209.
Murray MP, Sepic SB. Maximum isometric torque of hip abductor and adductor
muscle. Physical Therapy 1968;48:1327e35.
Nelson-Wong E, Fylnn T, Callaghan JP. Development of active hip abduction as
a screening test for identifying occupational low back pain. Journal of Orthopaedic and Sports Physical Therapy 2009;39:649e57.
Nelson-Wong E, Gregory DE, Winter DA, Callaghan JP. Gluteus medius muscle
activation patterns as a predictor of low back pain during standing. Clinical
Biomechanics 2008;23:545e53.
Neumann DA, Soderberg GL, Cook TM. Comparison of maximal isometric hip
abductor muscle torques between sides. Physical Therapy 1988;4:496e502.
Peck D, Buxton D, Nitz A. A comparison of spindle concentration in large and small
muscles acting in parallel combinations. Journal of Morphology 1984;180:
243e52.
Richardson C, Hodges P, Hides J. Therapeutic exercise for lumbopelvic stabilization:
a motor control approach for the treatment and prevention of low back pain.
2nd ed. Edinburgh: Churchill Livingstone; 2004.
Rybicki EF, Simonen FA, Weis Jr EB. On the mathematical analysis of stress in the
human femur. Journal of Biomechanics 1972;5:203e15.
Sims K, Richardson CA, Brauer SG. Investigation of hip abductor activation in
subjects with clinical unilateral osteoarthritis. Annals of the Rheumatic
Diseases 2002;61:687e92.
Sirca A, Susec-Michieli M. Selective type II fibre muscular atrophy in patients
with osteoarthritis of the hip. Journal of the Neurological Sciences 1980;44:
149e59.
Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St
Louis: Mosby; 2002.
Soderberg G, Dostal W. Electromyographic study of three parts of the gluteus
medius muscle during functional activities. Physical Therapy 1978;58
(6):691e6.
Teshima K. Hip abduction force in osteoarthritis of the hip. Acta Medica Nagasakiensia 1994;39(3):21e30.
vanBaar MV, Dekker J, Oostendorp R, Bijl D, Voorn T, Bijlsma J. Effectiveness of
exercise in patients with osteoarthritis of hip or knee: nine month’s follow up.
Annals of the Rheumatic Diseases 2001;60:1123e30.
Vleeming A, Mooney V, Snijders C, Doorman T, Stoeckart R. Movement, stability and
low back pain. The essential role of the pelvis. New York: Churchill Livingstone;
1997.
Watelain E, Dujardin F, Babier F, Dubois D, Allard P. Pelvic and lower limb
compensatory actions of subjects in an early stage of hip osteoarthritis. Archives
of Physical Medicine and Rehabilitation 2001;82:1705e11.
Walters J, Solomons M, Davies J. Gluteus minimus: observations on its insertion.
Journal of Anatomy 2001;198:239e42.
Williams PE, Goldspink G. Changes in sarcomere length and physiological properties in immobilized muscle. Journal of Anatomy 1978;127:459e68.
Winter DA, Prince F, Frank JS, Powell C, Zabjel K. Unified theory regarding A/P
and M/L balance in quiet stance. Journal of Neurophysiology
1996;75:2334e43.
Youdas JW, Madson TJ, Hollman JH. Usefulness of the Trendelenburg test for
identification of patients with hip joint osteoarthritis. Physiotherapy Theory
and Practice 2010;26:184e94.
Youdas JW, Mraz ST, Norstad BJ, Schinke JJ, Hollman JH. Determining meaningful
changes in pelvic-on-femoral position during the Trendelenburg test. Journal of
Sport Rehabilitation 2007;16:326e35.
Youdas JW, Mraz ST, Norstad BJ, Schinke JJ, Hollman JH. Determining meaningful
changes in hip abductor muscle strength obtained by handheld dynamometry.
Physiotherapy Theory and Practice 2008;24(3):215e20.
ˇ
References
ˇ
32