The 4 Phases of Pharmacokinetics Pharmacokinetics Absorption
advertisement
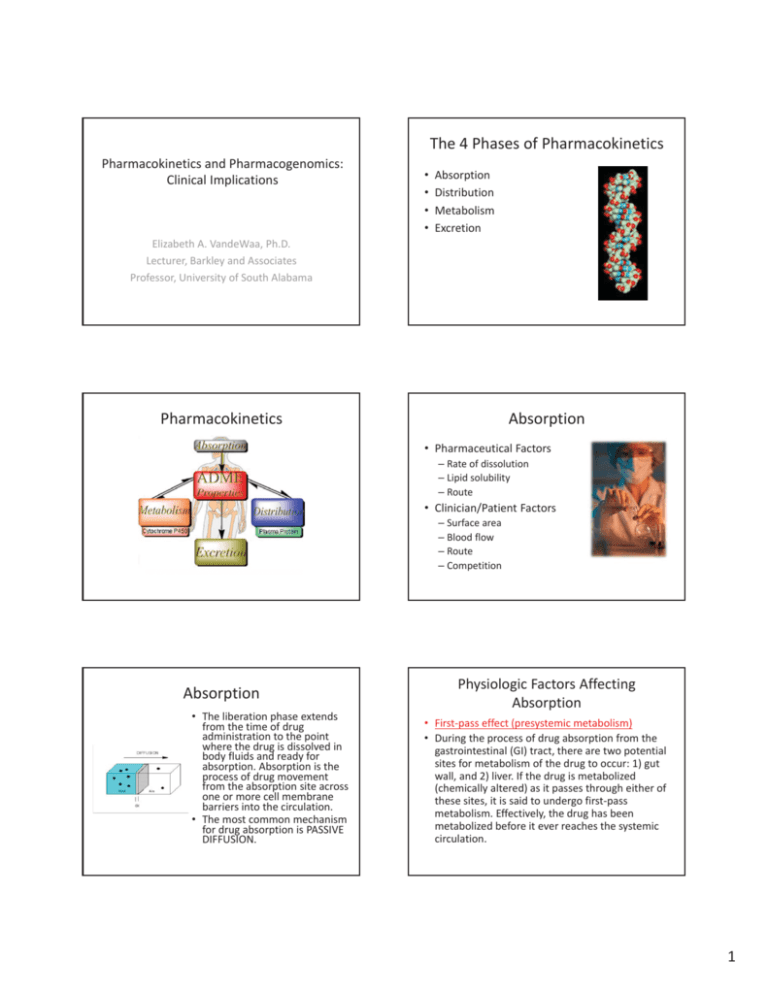
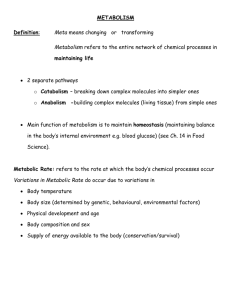
The4PhasesofPharmacokinetics PharmacokineticsandPharmacogenomics: ClinicalImplications • • • • Absorption Distribution Metabolism Excretion ElizabethA.VandeWaa,Ph.D. Lecturer,BarkleyandAssociates Professor,UniversityofSouthAlabama Pharmacokinetics Absorption • PharmaceuticalFactors – Rateofdissolution – Lipidsolubility – Route • Clinician/PatientFactors – Surfacearea – Bloodflow – Route – Competition Absorption • Theliberationphaseextends fromthetimeofdrug administrationtothepoint wherethedrugisdissolvedin bodyfluidsandreadyfor absorption.Absorptionisthe processofdrugmovement fromtheabsorptionsiteacross oneormorecellmembrane barriersintothecirculation. • Themostcommonmechanism fordrugabsorptionisPASSIVE DIFFUSION. PhysiologicFactorsAffecting Absorption • FirstͲpasseffect(presystemic metabolism) • Duringtheprocessofdrugabsorptionfromthe gastrointestinal(GI)tract,therearetwopotential sitesformetabolismofthedrugtooccur:1)gut wall,and2)liver.Ifthedrugismetabolized (chemicallyaltered)asitpassesthrougheitherof thesesites,itissaidtoundergofirstͲpass metabolism.Effectively,thedrughasbeen metabolizedbeforeiteverreachesthesystemic circulation. 1 PhysiologicFactorsAffecting Absorption • FirstͲpasseffect(presystemic metabolism) • Somedrugsaresoextensivelymetabolizedwhen takenorallythattherapeuticeffectscannotbe obtained,e.g.,lidocaine.Thesedrugsmustbe givenbyinjection.Otherdrugsmustbegivenin verylargedosesorally,comparedtoparenteral doses,toachievetherapeuticeffects;e.g. propranololperos (PO)10to30mgeverysixto eighthours(antihypertensive),intravenous1to 3mg(antiarrhythmic). ClinicalRelevance—Absorption PharmacokineticFactors AffectingAbsorption • ElevationofgastricpHbyantacids – Increasestheabsorbanceofbasicdrugs; decreasesthatofacidicdrugs • Laxatives – IncreaseperistalsisanddecreaseGItransittime • Drugsthatareconstipatingmayincrease absorptionofothermeds • Adsorbents • DrugsthatdecreaseGIbloodflow Distribution • Maychangeoverthelifespan • Presystemic metabolismisconsideredwhen drugsaredeveloped. • Highlyroutedependent • ViathePOroute,makesurethepatientis awareofthe“emptystomach”rule,ANDthat itappliestoantacids,antiͲdiarrheals • Bloodflowtotissues • Barrierstodistribution FactorsDeterminingDrugDistribution FactorsDeterminingDrugDistribution 1. Bloodflowtotissues(perfusion) 2. Bindingofdrugtoplasmaprotein – Rapidlyperfusedtissues,suchastheheart,liver, kidney,brain,andlung,areexposedtothedrugin thefirstfewminutesfollowingabsorption(initial phaseofdrugdistribution).Lessrapidlyperfused tissues(muscleandskin)andpoorlyperfused tissues(boneandfat)areexposedtothedrugas thedrugreachesitsfinaldistributionpatternover aperiodofhours. – Bloodbrainbarrier – Placenta • Proteinbinding – reversible(noncovalentbonding) – freedrug+protein<ͲͲͲͲͲͲ>drugͲproteincomplex • albumin(bindsacidicdrugs) • alphaͲ1acidglycoprotein(bindsbasicdrugs) • lipoproteins 2 FactorsDeterminingDrugDistribution FactorsDeterminingDrugDistribution 2. Bindingofdrugtoplasmaprotein 3. Specializeddistributionbarriers – Onlyfreedrugcandiffusetothesiteofaction. Pharmacologicactivitydependsonfreedrug concentrationinplasmaforveryhighlybound drugs. • Reservoireffectmayprolongboththedurationofdrug actionandhalfͲlife. • Theremaybeexcessfreedrugpresentif hypoalbuminemiaoccursandresultingtoxicity; importantonlyforhighlybounddrugs,mayrequire dosingadjustment. TheBloodBrainBarrier – BloodͲbrainbarrier(BBB) • Nointercellularporesbetweenbraincapillary endothelialmembranesduetothepresenceoftight junctionsbetweencells • Effects– severelimitationonmovementofionizedor highlypolarspecies;thesesubstancescannoteasily penetratetheBBB. – Fordrugstogainaccesstothebrainfromthecapillaries, drugsmustdiffuseacrosscells(lipidͲsoluble,nonionized form) orbeactivelytransportedbyacarrier. FactorsDeterminingDrugDistribution 3. Specializeddistributionbarriers – PlacentalBarrier • Drugscrossplacentabydiffusion;lipidͲsoluble, nonionized drugspenetratemostrapidly. • Usually, placentaltransferofdrugsisrelativelyslow, withtheequilibrationtimebetweenmaternalblood andfetaltissuesestimatedatabout15minutesfor somedrugsandalmostanhourforotherdrugs. FactorsDeterminingDrugDistribution LinkageofFetalandMaternal BloodSuppliesviathePlacenta 3. Specializeddistributionbarriers – PlacentalBarrier • Virtuallyeverydrugusedfortherapeuticpurposescan anddoescrosstheplacenta;effectively,norealbarrier exists.Inaddition,manyillicitdrugsandothertoxic substancesabsorbedbythemotherwillgainexposure tothefetus.Drugsareclassifiedonascale(A,B,C,D, X)forsafetyforuseinpregnancybasedontheirability toharmthefetus. 3 DevelopmentofPlacenta PharmacokineticFactors AffectingDistribution • Competitionforproteinbindingsites – Occasionallysignificant • AlterationofextracellularpH – Usefulincasesofoverdose,poisoning,etc. – Canalkalinizetheurinetoexcreteacidicdrugs ClinicalRelevance—Distribution • ClinicalSignificance • Veryrelevantinyoursickestpatients • Bloodflowisthedeterminanthere,soalways considerdistributiondisturbancesinthe patientwithcardiovasculardisease,vessel disease,perfusiondisorders • Rememberbarriers Metabolism • ConversionofarelativelylipidͲsolubleparent drugmoleculetoamuchmorepolar,waterͲ solubledrugmetabolitewhichcanbereadily excreted. • ThemorelipidͲsolubleparentformofthedrugis noteasilyeliminatedbythebody'sexcretory mechanisms(renalandbiliaryexcretion). • Drugmetabolismproducesapolar,waterͲsoluble substancewhichismoreeasilyexcretedfromthe body. • Thereisindividualvariationinmetabolism— pharmacogenetics. Metabolism—Purposes • Detoxification(defense)mechanism – Chemicalconversionofatoxicsubstancetoaless toxicmetaboliteforterminationofdrugaction – Chemicalconversionofapharmacologicallyactive substancetoaninactivemetabolite SitesforDrugMetabolism • LiverͲ smooth endoplasmicreticulum inhepatocytescontain manydrugͲmetabolizing enzymes;someenzymes arefoundincytosol. • Gutwallandmucosal surface • Plasma CYP450 4