Delay in diagnosis of appendicitis (PDF 262K)
advertisement

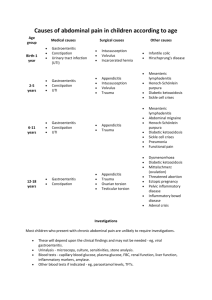
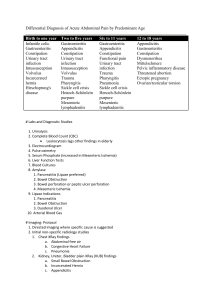
Treatment injury case study March 2012 – Issue 42 Sharing information to enhance patient safety Delay in diagnosis of appendicitis EVENT: Perforated appendix and peritonitis INJURY: Case Study Michaela, a 19-year-old hospitality worker, saw her GP for lower abdominal pain that had been getting worse during the previous week. She was normally healthy, and the only medication she took was a contraceptive pill. The GP initially diagnosed a urinary tract infection and prescribed an antibiotic, but Michaela returned two days later with worsening abdominal pain, diarrhoea, vomiting and fever. An examination found a raised temperature, right iliac fossa tenderness with rebound and a positive Rovsing’s sign (pain in the right lower quadrant elicited by palpating the left). The GP suspected appendicitis, so referred Michaela to the local emergency department (ED) and gave her a letter detailing events so far. Michaela was seen by a doctor in the ED, who recorded a slightly different history. He noted the abdominal pain to be “spasmodic” and was more focused on Michaela’s persistent watery diarrhoea. The examination found a temperature of 37.8°C, dehydration and abdominal tenderness throughout, but no more specific findings were recorded. Key points • The most important sign of appendicitis is localised tenderness in the right lower quadrant, but the classical symptoms and signs are only seen in 60% of patients • Diarrhoea may be a prominent symptom in (some) patients with acute appendicitis • Distinguishing appendicitis from gastroenteritis can be a diagnostic challenge; the MANTRELS score can be useful in judging the risk of appendicitis • There is no single diagnostic test to confirm appendicitis, but ultrasound or abdominal CT may be useful • If the diagnosis of abdominal pain is unclear, appendicitis must be considered. Observation and serial abdominal examinations may assist. 383158-ACC6337-Pr01 copy.indd 1 Michaela was given intravenous fluids, an antiemetic and analgesia, and blood tests were taken. These blood tests showed a very high white cell count (37.1 x 109/L with left shift), but no comment was made in the clinical record about the significance of this. The doctor’s impression was of gastroenteritis, and as she appeared to be stabilising, Michaela was soon discharged. The following day Michaela came back to her GP very unwell. She had a temperature of 39.1°C, constant abdominal pain with tenderness and guarding. Her GP again referred her immediately to hospital. That evening Michaela had an open appendicectomy and drainage. The appendix was found to be gangrenous and perforated. Her recovery was complicated with multiple intra-abdominal collections, pleural effusions and persisting abdominal pain. Owing to these complications she was transferred to a tertiary hospital where she had several returns to theatre for abdominal washout and drainage. A treatment injury claim was lodged for a delay in diagnosis of appendicitis at the ED, leading to perforation and recurrent intra-abdominal infections. ACC received advice from an emergency physician and a general surgeon, who agreed that the ED doctor should not have disregarded the GP’s findings and the very high white cell count. As a result, further observation and investigation had been warranted at the first presentation. This would have likely led to earlier surgery, preventing perforation of the appendix and the subsequent peritonitis, so the claim was accepted. ACC was able to assist Michaela with her recovery and gradual return to work. Expert Commentary Mr Kenneth W Menzies MBBS FRCS FRACS This case highlights the difficulties that can occur in the diagnosis of acute appendicitis. Symptoms of appendicitis overlap considerably with other clinical conditions that include gastroenteritis, urinary tract infection and (in the female) pelvic inflammatory disease. The main symptom of appendicitis is abdominal pain. 14/02/12 10:31 AM Case study Typically the pain is initially in the peri-umbilical region and it is colicky in nature. This is a visceral pain that is due to distension of the appendix. After a period of some hours the pain shifts to the right iliac fossa where the inflamed appendix irritates the parietal peritoneum. This is a constant pain that is aggravated by movement. Accompanying symptoms include anorexia, nausea and vomiting. When vomiting occurs in appendicitis, it follows the onset of pain. Examination findings include mild tachycardia and lowgrade fever (i.e. approximately 37.5°C) in the early stages. When the pathology progresses, as in the case of Michaela, the temperature can increase up to 39°C. The most important sign is localised tenderness in the right lower quadrant of the abdomen. This is usually accompanied by involuntary muscle rigidity (guarding) in that region. Unfortunately this classical constellation of symptoms and signs is only seen in approximately 60% of patients with appendicitis. The principal clinical manifestation of gastroenteritis is diarrhoea. The World Health Organization defines gastroenteritis as three or more abnormally loose or fluid stools in a 24-hour period. Abdominal pain is common in gastroenteritis and is most often described as “diffuse, intermittent, colicky pain” situated centrally in the abdomen. Vomiting may be present, particularly early in the illness. On clinical examination of the abdomen there may be some general abdominal tenderness. Diarrhoea can be a significant symptom in a minority of patients with appendicitis. Diarrhoea is more likely when the inflamed appendix is post-ileal or situated in the pelvis. As in the case of Michaela, when a patient presents with abdominal pain and diarrhoea, the ED physician often diagnoses gastroenteritis and initiates treatment appropriate for gastroenteritis. If at this stage the patient is discharged home, there is likely to be a delay in the surgical treatment of appendicitis being performed, and this in turn results in a higher incidence of postoperative complications. An increase in the white cell count (and neutrophilia) is present in 80% of patients presenting with appendicitis, whereas this is much less likely in gastroenteritis. Michaela’s white cell count was markedly elevated. Ultrasound may be helpful in the diagnosis of acute appendicitis, but it is quite often operator dependent. Likewise abdominal CT has a high sensitivity and specificity in diagnosing appendicitis. However, there is no single diagnostic test that can accurately diagnose appendicitis in all cases. Uncomplicated gastroenteritis is extremely unlikely if the abdominal examination reveals localised tenderness or signs of peritoneal irritation. Guarding may be difficult to elicit in the obese. The most useful clinical tools in assessing acute appendicitis are still: a good history and physical examination, serial abdominal examinations, and a high index of suspicion. A study from Hong Kong (1) shows that discharge at the first visit to an ED is the most significant factor associated with advanced-stage appendicitis and postoperative complications. The MANTRELS (Alvarado) clinical diagnostic score (migration of abdominal pain to the right iliac fossa, anorexia, nausea/vomiting, tenderness in the right iliac fossa, rebound tenderness, elevated temperature, leukocystosis and shift of leukocytes to the left) can be useful in the diagnosis of appendicitis. When the cause of abdominal pain is uncertain, acute appendicitis should be considered. Serial abdominal examinations will help to clarify the situation. References 1. Chung CH, Ng CP, Lai KK. Delays by patients, emergency physicians and surgeons in the management of acute appendicitis: retrospective study. HKMJ 2000 Sep; 6(3):245-9 2. Cappendijk VC, Hazebroek FWJ. The impact of diagnostic delay on the course of acute appendicitis. Arch Dis Child 2000; 83:64-66 3. Cameron P, Jelinek G, Kelly AM et al. Textbook of adult emergency medicine. 3rd ed. Philadelphia: Churchill Livingstone; 2009 4. Dunn RJ. The Emergency Medicine Manual. 4th ed. Tennyson: Venom Publishing; 2003 Claims information Between 1 July 2005 and 31 December 2011, ACC decided 20 claims for alleged delays in diagnosis leading to the progression of appendicitis. Of these, six were accepted. How ACC can help your patients following treatment injury Many patients may not require assistance following their treatment injury. The most common reason for declining a claim was that there was no causal link between the injury and treatment from a registered health professional. This was most often because external clinical advice did not substantiate that there had been a delay in timely diagnosis and treatment. However, for those who need help and have an accepted ACC claim, a range of assistance is available, depending on the specific nature of the injury and the person’s circumstances. Help may include things like: About this case study • • This case study is based on information amalgamated from a number of claims. The name given to the patient is therefore not a real one. • contributions towards treatment costs weekly compensation for lost income (if there’s an inability to work because of the injury) help at home, with things like housekeeping and childcare. No help can be given until a claim is accepted, so it’s important to lodge a claim for a treatment injury as soon as possible after the incident, with relevant clinical information attached. This will ensure ACC is able to investigate, make a decision and, if covered, help your patient with their recovery. ACCxxxx March 2012 ©ACC 2012 383158-ACC6337-Pr01 copy.indd 2 Printed in New Zealand on paper sourced from well-managed sustainable forests using oil free, soy-based vegetable inks. The case studies are produced by ACC’s Treatment Injury Centre, to provide health professionals with: • • an overview of the factors leading to treatment injury expert commentary on how similar injuries might be avoided in the future. The case studies are not intended as a guide to treatment injury cover. Send your feedback to: TI.info@acc.co.nz 14/02/12 10:31 AM