PEHP - Weber State University
advertisement

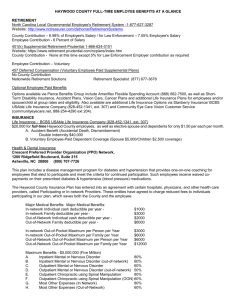
2015-2016 Benefits Preview 2015-16 Weber State University Your guide to understanding and enrolling in benefits for the new plan year. Weber State University 2015-16 » Contact Information Welcome to PEHP We want to make accessing and understanding your healthcare benefits simple. This Benefits Summary contains important information on how best to use PEHP’s comprehensive benefits. Please contact the following PEHP departments or affiliates if you have questions. ON THE WEB »Website . . . . . . . . . . . . . . . . . . . . . . . . . . . www.pehp.org PEHP FLEX$ »PEHP FLEX$ Department . . . . . . . . . . . . . 801-366-7503 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-753-7703 Create an online personal account at www.pehp.org to review your claims history, see a comprehensive list of your coverages, look up in-network providers, check your FLEX$ account balance, and more. HEALTH SAVINGS ACCOUNTS (HSA) »PEHP FLEX$ Department . . . . . . . . . . . . . 801-366-7503 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-753-7703 CUSTOMER SERVICE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 801-366-7555 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-765-7347 »HealthEquity . . . . . . . . . . . . . . . . . . . . . . . . 866-960-8058 . . . . . . . . . . . . . . . . . . www.healthequity.com/stateofutah Weekdays from 8 a.m. to 5 p.m. Have your PEHP ID or Social Security number on hand for faster service. Foreign language assistance available. PRENATAL AND POSTPARTUM PROGRAM » PEHP WeeCare . . . . . . . . . . . . . . . . . . . . . 801-366-7400 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 855-366-7400 . . . . . . . . . . . . . . . . . . . . . . . . . . . . www.pehp.org/weecare PRE-AUTHORIZATION »Inpatient hospital pre-authorization . . . . 801-366-7755 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-753-7754 WELLNESS AND DISEASE MANAGEMENT » PEHP Healthy Utah . . . . . . . . . . . . . . . . . 801-366-7300 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 855-366-7300 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . www.healthyutah.org MENTAL HEALTH/SUBSTANCE ABUSE PRE-AUTHORIZATION »PEHP Customer Service . . . . . . . . . . . . . . . 801-366-7555 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-765-7347 » PEHP Waist Aweigh . . . . . . . . . . . . . . . . 801-366-7300 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 855-366-7300 » PEHP Integrated Care . . . . . . . . . . . . . . . 801-366-7555 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-765-7347 PRESCRIPTION DRUG BENEFITS »PEHP Customer Service . . . . . . . . . . . . . . . 801-366-7555 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . or 800-765-7347 VALUE-ADDED BENEFITS PROGRAM »PEHPplus . . . . . . . . . . . . . . . . . . . . www.pehp.org/plus »Express Scripts . . . . . . . . . . . . . . . . . . . . . . . 800-903-4725 . . . . . . . . . . . . . . . . . . . . . . . . . . .www.express-scripts.com »Blomquist Hale . . . . . . . . . . . . . . . . . . . . . . . 800-926-9619 . . . . . . . . . . . . . . . . . . . . . . . . . . . www.blomquisthale.com SPECIALTY PHARMACY »Accredo . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 800-501-7260 CLAIMS MAILING ADDRESS PEHP 560 East 200 South Salt Lake City, UT 84102-2004 4-7-15 WWW.PEHP.ORG PAGE 2 Weber State University 2015-16 » Benefit Changes & Reminders Benefit Changes & Reminders The Affordable Care Act required certain plan changes to the Traditional plan. Because of this requirement, your overall out-of-pocket maximum will be consolidated/reduced to ($3,000 per person, $6,000 double, $9,000 family) July 1, 2015. All eligible medical, pharmacy, and specialty drugs will apply to the out-of-pocket maximum. The Traditional Plan: will no longer have a pharmacy deductible beginning July 1, 2015. It will have one medical deductible ($350 per person, $700 double and family). This positive change will reduce your risk on the Traditional plan from $8,350 per person (in 2014-15 plan year) to $3,350 per person (in the 2015-16 plan year). See the below table. Benefit 2014-15 2015-16 Medical Deductible $250/$500 (not included in Medical OOP) $350/$700 (not included in medical OOP) Pharmacy Deductible $100 per person/$200 per family (included in Pharmacy OOP) $0 Medical Out-of-Pocket Maximum $2,500/$5,000/$7,500 $3,000/$6,000/$9,000 Pharmacy Out-of-Pocket Maximum $2,000 per person $0 (included in Medical OOP) Specialty Pharmacy Out-of-Pocket Maximum $3,600 per person $0 (included in Medical OOP) Total Out-of-Pocket Cost $8,350 per person $3,350 per person This limit caps the amount you spend outof-pocket for any one person on your plan before you meet your family plan limit. STAR Plan: As always, all covered services on The STAR Plan will apply to a single deductible (remains $1,500 single, $3,000 double/family) and out-of-pocket max (remains $2,500 single, $5,000 double, and $7,500 family). Other Changes/Notices PEHP Healthy Utah » Your myHealthyUtah account information and resources from PEHP Healthy Utah have a new home at www.pehp.org. Schedule testing sessions, participate in health challenges, and learn about rebate programs alongside your PEHP medical benefits all in one convenient place. New PEHP Treatment Advisor » This innovative online tool helps you understand your treatment options, based on clinical evidence, patient satisfaction, and your personal preferences. WWW.PEHP.ORG PAGE 3 Weber State University 2015-16 » PEHP Online Tools PEHP Online Tools Access Benefits and Claims Access Your Pharmacy Account WWW.PEHP.ORG WWW.EXPRESS-SCRIPTS.COM Access important benefit tools and information by creating an online personal account at www.pehp.org. Create an account with Express Scripts, PEHP’s pharmacy benefit manager, and get customized information that will help you get your medications quickly and at the best price. » See your claims history — including medical, dental, and pharmacy. Search claims histories by member, plan, and date range. Go to www.express-scripts.com to create an account. All you need is your PEHP ID card and you’re on your way. » Get important plan documents, such as forms and Master Policies. You’ll be able to: » Get a simple breakdown of the PEHP benefits in which you’re enrolled. » Check prices. » Access your FLEX$ account. » Locate a pharmacy. »Cut down on clutter by opting in to paperless delivery of explanation of benefits (EOBs). Opt to receive EOBs by email, rather than paper forms through regular mail, and you’ll get an email every time a new one is available. » Refill or renew a prescription. » Check an order status. » Get mail-order instructions. » Find detailed information specific to your plan, such as drug coverage, co-pays, and cost-saving alternatives. » Change your mailing address. Find a Provider WWW.PEHP.ORG Looking for a provider, clinic, or facility that is contracted with your plan? Look no farther than www.pehp.org. Go online to search for providers by name, specialty, or location. WWW.PEHP.ORG PAGE 4 Medical Networks Weber State University 2015-16 » PEHP Medical Networks PEHP Medical Networks PEHP Advantage PEHP Summit The PEHP Advantage network of contracted providers consists of predominantly Intermountain Healthcare (IHC) providers and facilities. It includes 34 participating hospitals and more than 7,500 participating providers. The PEHP Summit network of contracted providers consists of predominantly IASIS, MountainStar, and University of Utah hospitals & clinics providers and facilities. It includes 39 participating hospitals and more than 7,500 participating providers. PARTICIPATING HOSPITALS Beaver County Beaver Valley Hospital Milford Valley Memorial Hospital Box Elder County Bear River Valley Hospital PARTICIPATING HOSPITALS Salt Lake County (cont.) The Orthopedic Specialty Hospital (TOSH) LDS Hospital Primary Children’s Medical Center Riverton Hospital Beaver County Beaver Valley Hospital Milford Valley Memorial Hospital Box Elder County Bear River Valley Hospital Brigham City Community Hospital San Juan County Blue Mountain Hospital San Juan Hospital Cache County Logan Regional Hospital Carbon County Castleview Hospital Cache County Logan Regional Hospital Sanpete County Gunnison Valley Hospital Sanpete Valley Hospital Davis County Davis Hospital Duchesne County Uintah Basin Medical Center Garfield County Garfield Memorial Hospital Grand County Moab Regional Hospital Iron County Valley View Medical Center Juab County Central Valley Medical Center Kane County Kane County Hospital Millard County Delta Community Medical Center Fillmore Community Hospital Salt Lake County Alta View Hospital Intermountain Medical Center Carbon County Castleview Hospital Sevier County Sevier Valley Medical Center Davis County Lakeview Hospital Davis Hospital Summit County Park City Medical Center Duchesne County Uintah Basin Medical Center Tooele County Mountain West Medical Center Garfield County Garfield Memorial Hospital Uintah County Ashley Valley Medical Center Grand County Moab Regional Hospital Utah County American Fork Hospital Orem Community Hospital Utah Valley Regional Medical Center Iron County Valley View Medical Center Juab County Central Valley Medical Center Wasatch County Heber Valley Medical Center Kane County Kane County Hospital Washington County Dixie Regional Medical Center Millard County Delta Community Medical Center Fillmore Community Hospital Weber County McKay-Dee Hospital Salt Lake County Huntsman Cancer Hospital Jordan Valley Hospital PEHP Preferred PAGE San Juan County Blue Mountain Hospital San Juan Hospital Sanpete County Gunnison Valley Hospital Sanpete Valley Hospital Sevier County Sevier Valley Medical Center Summit County Park City Medical Center Tooele County Mountain West Medical Center Uintah County Ashley Valley Medical Center Utah County Mountain View Hospital Timpanogos Regional Hospital Mountain Point Medical (opens soon) Wasatch County Heber Valley Medical Center Washington County Dixie Regional Medical Center Weber County Ogden Regional Medical Center Find Participating Providers The PEHP Preferred network of contracted providers consists of providers and facilities in both the Advantage and Summit networks. It includes 46 participating hospitals and more than 12,000 participating providers. WWW.PEHP.ORG Salt Lake County (cont.) Lone Peak Hospital Pioneer Valley Hospital Primary Children’s Medical Center Riverton Children’s Unit St. Marks Hospital Salt Lake Regional Medical Center University of Utah Hospital University Orthopaedic Center Go to www.pehp.org to look up participating providers for each plan. 5 Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage Traditional Traditional (Non-HSA) SUMMIT ADVANTAGE PREFERRED Refer to the Master Policy for specific criteria for the benefits listed below, as well as information on limitations and exclusions. * Services received by an out-of-network provider will be paid at a percentage of PEHP’s InNetwork Rate (In-Network Rate). You will be responsible for your assigned co-insurance and deductible (if applicable). You may also be responsible for any amounts billed by an out-of-network provider in excess of PEHP’s In-Network Rate. There is no out-of-pocket maximum for services received from an out-of-network provider. YOU PAY In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation DEDUCTIBLES, PLAN MAXIMUMS, AND LIMITS Plan Year Deductible Not included in the Out-of-Pocket Maximum $350 per individual, $700 per family Same as using an in-network provider *See above for additional information **See below for additional information Plan year Out-of-Pocket Maximum Includes amounts applied to Co-insurance and prescription drugs $3,000 per individual $6,000 per double $9,000 per family No out-of-pocket maximum *See above for additional information **See below for additional information Maximum Lifetime Benefit None None **Applicable deductibles and co-insurance for services provided by an out-of-network provider will apply to your in-network plan year deductible and Out-of- Pocket Maximum. However, once your in-network deductible and Out-of-Pocket Maximum are met, co-insurance amounts for out-ofnetwork providers will still apply. INPATIENT FACILITY SERVICES Medical and Surgical | All out-of-network facilities and some in-network facilities require pre-authorization. See the Master Policy for details 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Skilled Nursing Facility | Non-custodial Up to 60 days per plan year. Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Hospice | Up to 6 months in a 3-year period. Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Rehabilitation Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Mental Health and Substance Abuse Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Out-of-network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 6 Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage Traditional In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation OUTPATIENT FACILITY SERVICES Outpatient Facility and Ambulatory Surgery 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Ambulance (ground or air) Medical emergencies only, as determined by PEHP 20% of In-Network Rate after deductible 20% of In-Network Rate after deductible Emergency Room Medical emergencies only, as determined by PEHP. If admitted, inpatient facility benefit will be applied 20% of In-Network Rate, minimum $150 co-pay per visit 20% of In-Network Rate, minimum $150 co-pay per visit, plus any balance billing above In-Network Rate Urgent Care Facility $45 co-pay per visit 40% of In-Network Rate after deductible Preferred only: University of Utah Medical Group Urgent Care Facility: $50 co-pay per visit 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible 20% of In-Network Rate after deductible Chemotherapy, Radiation, and Dialysis Dialysis with out-of-network providers requires pre-authorization 40% of In-Network Rate after deductible Diagnostic Tests, X-rays, Minor Applicable office co-pay per visit 40% of In-Network Rate after deductible Inpatient Physician Visits Applicable office co-pay per visit 40% of In-Network Rate after deductible Surgery and Anesthesia 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Primary Care Office Visits and Office Surgeries $25 co-pay per visit 40% of In-Network Rate after deductible Physical and Occupational Therapy Requires pre-authorization after 12 visits PROFESSIONAL SERVICES Preferred only: University of Utah Medical Group Primary Care Office visits: $50 co-pay per visit Specialist Office Visits and Office Surgeries, $35 co-pay per visit 40% of In-Network Rate after deductible Preferred only: University of Utah Medical Group Specialist Office visit: $50 co-pay per visit Emergency Room Specialist $35 co-pay per visit $35 co-pay per visit, plus any balance billing above In-Network Rate Diagnostic Tests, X-rays 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Mental Health and Substance Abuse No pre-authorization required for outpatient services. Inpatient services require pre-authorization Outpatient: $35 co-pay per visit Inpatient: Applicable office co-pay per visit Outpatient: 40% of In-Network Rate after deductible Inpatient: 40% of In-Network Rate after deductible Out-of-Network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 7 Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage Traditional In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation PRESCRIPTION DRUGS Retail Pharmacy | Up to 30-day supply Tier 1: $10 co-pay Tier 2: 25% of discounted cost. $25 minimum, no maximum co-pay Tier 3: 50% of discounted cost. $50 minimum, no maximum co-pay Plan pays up to the discounted cost, minus the applicable co-pay. Member pays any balance Mail-Order Some medications available through retail pharmacy at mail order co-pay Tier 1: $20 co-pay Tier 2: 25% of discounted cost. $50 minimum, no maximum co-pay Tier 3: 50% of discounted cost. $100 minimum, no maximum co-pay Plan pays up to the discounted cost, minus the applicable co-pay. Member pays any balance Specialty Medications, retail pharmacy Up to 30-day supply Tier A: 20% of In-Network Rate. No maximum co-pay Tier B: 30% of In-Network Rate. No maximum co-pay Plan pays up to the discounted cost, minus the preferred co-pay. Member pays any balance Specialty Medications, office/outpatient Up to 30-day supply Tier A: 20% of In-Network Rate after deductible. No maximum co-pay Tier B: 30% of In-Network Rate after deductible. No maximum co-pay Tier A: 40% of In-Network Rate after deductible. Tier B: 50% of In-Network Rate after deductible. Specialty Medications, through specialty vendor Accredo | Up to 30-day supply Tier A: 20% of In-Network Rate. $150 maximum co-pay Tier B: 30% of In-Network Rate. $225 maximum co-pay Tier C: 20%. No maximum co-pay Not covered Adoption | See limitations No charge after deductible, up to $4,000 per adoption No charge after deductible, up to $4,000 per adoption Affordable Care Act Preventive Services See Master Policy for complete list No charge 40% of In-Network Rate after deductible Allergy Serum 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Chiropractic Care | Up to 10 visits per plan year Applicable office co-pay per visit 40% of In-Network Rate after deductible Dental Accident 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Durable Medical Equipment, DME Except for oxygen and Sleep Disorder Equipment, DME over $750, rentals, that exceed 60 days, or as indicated in Appendix A of the Master Policy require pre-authorization. Maximum limits apply on many items. See the Master Policy for benefit limits 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Medical Supplies 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Home Health/Skilled Nursing | Up to 60 visits per plan year. Requires pre-authorizationo 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Infertility Services** Select services only. See the Master Policy 50% of In-Network Rate after deductible 70% of In-Network Rate after deductible Injections | Requires pre-authorization if over $750 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Temporomandibular Joint Dysfunction** Up to $1,000 lifetime maximum 50% of In-Network Rate after deductible 70% of In-Network Rate after deductible MISCELLANEOUS SERVICES **Some services on your plan are payable at a reduced benefit of 50% of In-Network Rate or 30% of In-Network Rate. These services do not apply to any out-of-pocket maximum. Deductible may apply. Refer to the Master Policy for specific criteria for the benefits listed above, as well as information on limitations and exclusions. Out-of-network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 8 Weber State University 2015-16 » Medical Benefits Grid » FLEX$ PEHP FLEX$ FLEX$ saves you money by reducing your taxable income. You set aside a portion of your pre-tax salary to pay eligible expenses. PEHP offers two types of FLEX$: healthcare and dependent day care. Enroll in one or both. ENROLLMENT »You must re-enroll for FLEX$ every plan year. »Open enrollment: Enroll online at www.pehp.org between April 7 and May 15, 2015. Or fill out a paper form and return it to PEHP (fax: 801-366-7772). »New hires: Enroll within 60 days of eligibility date. PLAN YEAR CONTRIBUTION LIMITS » Up to $2,550 for healthcare expenses. FLEX$ Timeline PLAN YEAR: July 1, 2015 – June 30, 2016 Eligible FLEX$ expenses must be incurred between July 1, 2015, and Sept. 15, 2016. You must submit claims by Sept. 30, 2016. July 1, 2015 2015 FLEX$ plan year begins June 30, 2016 » Up to $5,000 for dependent day care expenses (you and your spouse combined). 2015 FLEX$ plan year ends HOW YOU CONTRIBUTE Sept. 15, 2016 » Your contributions are withheld from your paycheck pre-tax. The total amount you contribute is evenly divided among pay periods. » The total amount you choose to withhold for healthcare expenses is immediately available as soon as you begin FLEX$. Grace period for 2015 FLEX$ plan ends Sept. 30, 2016 Deadline to submit claims YOU CAN’T HAVE AN HSA WITH FLEX$ You can’t contribute to a health savings account (HSA) while you’re enrolled in healthcare FLEX$. However, you may have a dependent day care FLEX$ or a limited FSA and contribute to an HSA. OLDER CHILDREN » Children up to age 26* can remain covered regardless of marital or dependent status. (*Up to Dec. 31 of the calendar year they turn age 26.) Don’t Lose It Plan ahead wisely and set aside only what you’ll need each year. FLEX$ is use-it-or-lose-it; money doesn’t carry over from year to year. Weber State University 2015-16 » Medical Benefits Grid » FLEX$ PEHP FLEX$ Use Your FLEX$ Card as a Debit Card Now you can use your FLEX$ Benefits Card as either a credit card or a debit card. Log in to your online personal account at www.pehp.org to get your debit PIN. Click “Check Your FLEX$ Balance” from the menu at left, then click “Card Status.” This means you can now use your card at places that accept only debit cards. Choose either credit card or debit card at the point of sale. Using Your FLEX$ Card The easiest way to access your FLEX$ account is with the FLEX$ Benefits Card you will automatically receive at no extra cost. It works just like a credit card and is accepted at most places that take MasterCard. The FLEX$ card doesn’t always distinguish which purchases are eligible. You may be asked to verify expenses. For places that don’t accept the FLEX$ card, simply pay for the charges and submit a copy of the receipt and a claim form to PEHP for reimbursement. You’re responsible to keep all receipts for tax and verification purposes. PEHP may ask for verification of charges. Limitations apply. Go to www.pehp.org for eligibility and more details. Eligible Expenses Over-the-counter medications are only eligible with a prescription. FLEX$ HEALTHCARE ACCOUNT for eligible health expenses for you and your eligible dependents. A partial list of eligible expenses is on the back of this brochure. FLEX$ DEPENDENT DAY CARE ACCOUNT for eligible day care expenses for your eligible dependents to allow you and/or your spouse to work, look for work, or go to school. For more information about which expenses are eligible, visit www.pehp.org or www.irs.gov. Weber State University STAR Plan Understanding The PEHP STAR Plan The STAR Plan: What Is It? The STAR Plan has two components: 1) A High Deductible Health Plan (HDHP), which is a qualified medical plan that meets IRS guidelines for deductibles and out-of-pocket maximums; and 2) a Health Savings Account (HSA), which is an interest-bearing account designed to be coupled with an HDHP. The STAR Plan allows you to manage the cost of healthcare based on how you use it. You take more responsibility use it. You takeformore your spending withfor responsibility the your ability to save money spending with each theyear. ability to save money Couple your each STAR year. Plan with Couple an employer-funded your STAR Plan HSA with to pay an employer-funded for healthcare. HSA You canpay to also formake healthcare. tax-freeYou HSA contributions can also makeand tax-free earnHSA taxfree interest. and earn taxcontributions free interest. You must meet your You must meet deductible before your any eligible medical deductible before and any pharmacy eligible medical benefits andare paid, but you’re protected pharmacy benefits are from paid, largeyou’re but dollarprotected medical bills. from large dollar medical bills. Take Control of Your Healthcare Costs You Save... ON PREMIUM No employee cost share for the Advantage and Summit STAR plans in 2014-15. 2015-16. WITH YOUR HSA Weber State University will make semi-monthly contributions to your HSA. ON TAXES You can contibute to your HSA. Money goes in tax-free, grows tax-free, and is used tax-free for eligible expenses. PROVIDER NETWORKS You benefit from the same PEHP group discount and same network of doctors and hospitals as with the Advantage and Summit Care plans. Your Deductible: How does it work? Your deductible is the yearly dollar amount you must pay out of your own pocket for eligible medical and pharmacy expenses before PEHP begins paying benefits. The STAR Plan’s deductible is set higher than Advantage and Summit Care’s. Weber State University STAR Plan Understanding The PEHP STAR Plan Your HSA: How It Works A Health Savings Account is a taxadvantaged, interestbearing account. Your money goes in tax-free, grows taxfree, and is spent on qualified health expenses tax-free. It’s a great way to save for health expenses in both the short and long term. An HSA is like a flexible spending account, but better. You never have to worry about forfeiting HSA money you don’t spend. Money in your HSA carries over from yearto-year and even from employer-to-employer. Take Control of Your Healthcare Decisions You Choose... HOW TO SPEND YOUR HSA MONEY Eligible HSA expenses include medical, dental, pharmacy, and vision, as well as anything flex-eligible. When spending your own HSA money, you’re in control. You can spend on any flex-eligible expense, including many healthcare products and services. Note that while many expenses are HSA-eligible, they must be covered by your health plan to apply to your deductible and out-of-pocket max. You’ll automatically get this HSA debit card at no cost to you. You’ll be automatically issued a debit card to access your HSA funds. Always present your PEHP card at the time of service to receive PEHP’s discounted rate. It also allows PEHP to track your spending to apply to your deductible and out-of-pocket maximum. HOW TO INVEST YOUR HSA MONEY Your HSA earns tax-free interest. You choose how to invest your money. Options include a savings account and a number of mutual funds. Your Out-of-Pocket Max: What is it? It’s the annual dollar limit you will pay for covered medical services, including your deductible and prescription expenses. It protects you from large dollar claims, capping the amount you’re responsible to pay each plan year. Weber State University STAR Plan What WhatYou You Need Need to to Know Know ifif You You Plan Plan to to Enroll Enroll Nuts & Bolts ELIGIBLE ELIGIBLE EXPENSES EXPENSES Eligible EligibleHSA HSAexpenses expensesinclude includedeductibles, deductibles, copayments, copayments,and andcoinsurance, coinsurance,as aswell wellas asall allflexflexeligible eligiblehealth healthexpenses. expenses.However, However,while whilemany many expenses expensesare areHSA-eligible, HSA-eligible,they theyapply applyto toyour yourdeductible deductibleand andoutoutof-pocket of-pocketmaximum maximumonly onlyififthey’re they’recovered coveredby byyour yourhealth healthplan. plan. CONTRIBUTIONS CONTRIBUTIONS The Thecontribution contributionmaximum maximumapplies appliesto tothe theIRS IRScalendar calendaryear year (Jan-Dec). If you become ineligible for The STAR Plan during (Jan-Dec). If you become ineligible for The STAR Plan during the thecourse courseof ofthe theIRS IRScalendar calendaryear yearand andcontributions contributionshave havebeen been made to your HSA, you may be subject to taxes and penalties. made to your HSA, you may be subject to taxes and penalties.IfIf you youexceed exceedthe thecontribution contributionmaximum maximumduring duringthe theIRS IRScalendar calendar year and then drop the STAR Plan during Weber State’s year and then drop the STAR Plan during Weber State’sopen open enrollment period you may be subject to taxes and penalties. enrollment period you may be subject to taxes and penalties. BANKING BANKING ENROLL ENROLL IN IN A A LIMITED LIMITED FSA FSA Health HealthEquity Equity will handle will handleyour your HSA. Weber HSA. WeberState State University will University will make makeyour yourHSA HSA contributions contributions directly directlyto toHealth Health Equity into Equity intoyour your account. You account. Youare are responsible for responsible forthe the management of management of your yourHSA HSAfunds. funds. IfIfyou youare areenrolled enrolledin inThe TheSTAR STARPlan, Plan, you can also choose to enroll in a you can also choose to enroll in a Limited LimitedPurpose PurposeFlexible FlexibleSpending Spending Account. This is a tax savings Account. This is a tax savingsaccount. account. The Thepre-tax pre-taxmonies moniesyou youchoose chooseto to fund this account with can be used fund this account with can be usedfor for eligible dental and vision expenses, eligible dental and vision expenses, and andafter afteryou youhave havemet metThe TheSTAR STARPlan Plan deductible you can use these funds deductible you can use these fundsfor for eligible medical expenses. eligible medical expenses. Remember Rememberthe thefunds fundsin inthis thisaccount account are areuse useor orlose. lose.The Themaximum maximumyou you can candeposit depositisis$2,550 $2,500for forthe theplan planyear. year. Remember Rememberas asan anenrollee enrolleein inThe TheSTAR STAR Plan, Plan,you youare arealso alsoenrolled enrolledin inthe the Health HealthSavings SavingsAccount Account(HSA). (HSA). Do Do You You Qualify? Qualify? To Tobe beeligible eligiblefor forthe the HSA, HSA,you youmust mustenroll enrollinin The TheSTAR STARPlan. Plan.Also, Also,the the following followingthings thingsmust must apply applyto toyou: you: »»You’re You’renot not participating participatingininor or covered coveredby byaageneralgeneralpurpose purposeflex flexaccount account (FSA) (FSA)or orHealth Health Reimbursement Reimbursement Account Account(HRA) (HRA)or ortheir their balances balanceswill willbe be$0 $0on on or orbefore beforeJune June30. 30. »»You’re You’renot notcovered covered by another by anotherhealth health plan (unless plan (unlessit’s it’s another HSAanother HSAqualified qualifiedplan). plan). » You’re not covered by » You’re not covered by Medicare, Tricare or Medicare or Tricare. Medicaid. » You’re not a » You’re not a dependent of dependent of another taxpayer. another taxpayer. Take Note Note Take youchoose choosethe the »»IfIfyou STARPlan, Plan,Weber Weber STAR State’ssupplemental supplemental State’s pharmacyout-ofout-ofpharmacy pocketmaximum maximum pocket doesnot notapply. apply. does WeberState’s State’s »»Weber medicalbenefits benefitsare are medical basedon onaaplan planyear. year. based Weber State University STAR Plan Advantage Advantage&&Summit SummitPlan PlanComparison: Comparison: STAR STARvs. vs.Traditional Traditional Benefit Benefit STAR STAR Traditional Traditional Yes Yes No No PEHP PEHP Customer CustomerService Service 801-366-7555 801-366-7555 oror800-765-7347 800-765-7347 Does Doesthe thedeductible deductibleapply applytotothe the out-of-pocket out-of-pocketmaximum? maximum? Does Doesthe thedeductible deductibleapply applytotoinpatient inpatient and andoutpatient outpatientservices? services? Yes Yes Yes Yes Does Doesthe thedeductible deductibleapply applytoto physician office copays? physician office copays? Yes Yes No No Will WillWSU WSUcontribute contributetotomy myHSA? HSA? Yes Yes Not NotEligible Eligible Will I continue to be eligible for WSU’s supplemental pharmacy out-of-pocket Benefit STAR maximum? No Employee semimonthly Benefitcost for medical benefits Employee semiWSU semi-monthly monthly cost for Contribution medical benefits Single: $22.69 Double:Traditional $46.79 Family: $62.47 Single: $22.69 Double: $46.79 Family: Not$62.47 Eligible WSU semi-monthly Contribution Out-of-pocket Maximum Deductible (Medical & RX) Out-of-pocket Maximum $0 STAR Semi-monthly: $0 Single: $33.09 Double: $66.18 Family: Single:$66.18 $33.09 Double: $66.18 Medical RX: Family:&$66.18 Single: $2,500 Double: $1,500 $5,000 / $3,000 (Combined for medical & RX) Family: $7,500 Medical & RX: Single: $2,500 Double: $5,000 Family: $7,500 Contact Contact Information Information Yes Traditional Not Eligible Medical & RX: Single: $3,000 Double: $6,000 $250 / $500 Medical Family: $100 /$9,000 $200 RX Medical: Single: $2,500 Double: $5,000 Family: $7,500 RX: $2,000 per individual (does not apply to non preferred) 3/30/15 4/4/14 www.pehp.org www.pehp.org Inpatient InpatientMedical Medical Pre-authorization Pre-notification 801-366-7755 801-366-7755 oror800-753-7490 800-753-7490 Pre-authorization Pre-authorization 801-366-7555 801-366-7555 oror800-765-7347 800-765-7347 HealthEquity HealthEquity Member MemberServices Services Available Available2424hours hoursa aday, day, 7 7days daysa aweek week 866-346-5800 866-346-5800 To Tolearn learnmore more about aboutHSAs, HSAs,visit: visit: www.irs.gov www.irs.gov www.ustreas.gov www.ustreas.gov Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage STAR The PEHP STAR Plan (HSA-Qualified) SUMMIT* ADVANTAGE* Refer to the Master Policy for specific criteria for the benefits listed below, as well as information on limitations and exclusions. * Services received by an out-of-network provider will be paid at a percentage of PEHP’s InNetwork Rate (In-Network Rate). You will be responsible for your assigned co-insurance and deductible (if applicable). You may also be responsible for any amounts billed by an out-of-network provider in excess of PEHP’s In-Network Rate. There is no out-of-pocket maximum for services received from an out-of-network provider. YOU PAY In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation DEDUCTIBLES, PLAN MAXIMUMS, AND LIMITS Plan Year Deductible $1,500 single plan $3,000 double or family plan Same as using an in-network provider *See above for additional Information **See below for additional Information Plan Year Out-of-Pocket Maximum Includes amounts applied to Deductibles, Co-Insurance and prescription drugs $2,500 single plan $5,000 double plan $7,500 family plan No out-of-network out-of-pocket maximum *See above for additional Information **See below for additional Information Maximum Lifetime Benefit None None **Applicable deductibles and co-insurance for services provided by an out-of-network provider will apply to your in-network plan year deductible and out-of- pocket maximum. However, once your in-network deductible and out-of-pocket maximum are met, co-insurance amounts for out-ofnetwork providers will still apply. INPATIENT FACILITY SERVICES Medical and Surgical | All out-of-network facilities and some in-network facilities require pre-authorization. See the Master Policy for details 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Skilled Nursing Facility | Non-custodial Up to 60 days per plan year. Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Hospice | Up to 6 months in a 3-year period. Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Rehabilitation Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Mental Health and Substance Abuse Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Out-of-network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 15 Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage STAR In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation OUTPATIENT FACILITY SERVICES Outpatient Facility and Ambulatory Surgery 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Ambulance (ground or air) Medical emergencies only, as determined by PEHP 20% of In-Network Rate after deductible 20% of In-Network Rate after deductible Emergency Room Medical emergencies only, as determined by PEHP. If admitted, inpatient facility benefit will be applied 20% of In-Network Rate after deductible 20% of In-Network Rate after deductible, plus any balance billing above In-Network Rate Urgent Care Facility 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Diagnostic Tests, X-rays, Minor 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible 20% of In-Network Rate after deductible Chemotherapy, Radiation, and Dialysis Dialysis with out-of-network providers requires pre-authorization 40% of In-Network Rate after deductible 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Inpatient Physician Visits 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Surgery and Anesthesia 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Primary Care Office Visits and Office Surgeries 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Specialist Office Visits and Office Surgeries 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Emergency Room Specialist 20% of In-Network Rate after deductible 20% of In-Network Rate after deductible, plus any balance billing above In-Network Rate Diagnostic Tests, X-rays 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Mental Health and Substance Abuse No pre-authorization required for outpatient services. Inpatient services require pre-authorization Outpatient: 20% of In-Network Rate after deductible Inpatient: 20% of In-Network Rate after deductible Outpatient: 40% of In-Network Rate after deductible Inpatient: 40% of In-Network Rate after deductible Physical and Occupational Therapy Requires pre-authorization after 12 visits PROFESSIONAL SERVICES Out-of-network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 16 Weber State University 2015-16 » Medical Benefits Grid » Summit & Advantage STAR In-Network Provider Out-of-Network Provider You may be balance billed. See Page 9 for explanation PRESCRIPTION DRUGS Retail Pharmacy | Up to 30-day supply Tier 1: $10 co-pay after deductible Tier 2: 25% of discounted cost after deductible. $25 minimum, no maximum co-pay Tier 3: 50% of discounted cost after deductible. $50 minimum, no maximum co-pay Plan pays up to the discounted cost after deductible, minus the applicable co-pay. Member pays any balance Mail-Order Some medications available through retail pharmacy at mail order co-pay Tier 1: $20 co-pay after deductible Tier 2: 25% of discounted cost after deductible. $50 minimum, no maximum co-pay Tier 3: 50% of discounted cost after deductible. $100 minimum, no maximum co-pay Plan pays up to the discounted cost after deductible, minus the applicable co-pay. Member pays any balance Specialty Medications, retail pharmacy Up to 30-day supply Tier A: 20% of In-Network Rate after deductible. No maximum co-pay Tier B: 30% of In-Network Rate after deductible. No maximum co-pay Plan pays up to the discounted cost after deductible, minus the applicable co-pay. Member pays any balance Specialty Medications, office/outpatient Up to 30-day supply Tier A: 20% of In-Network Rate after deductible. No maximum co-pay Tier B: 30% of In-Network Rate after deductible. No maximum co-pay Tier A: 40% of In-Network Rate after deductible. Tier B: 50% of In-Network Rate after deductible. Specialty Medications, through specialty vendor Accredo Up to 30-day supply Tier A: 20% of In-Network Rate after deductible. $150 maximum co-pay Tier B: 30% of In-Network Rate after deductible. $225 maximum co-pay Tier C: 20% after deductible. No maximum co-pay Not covered Adoption | See limitations No charge after deductible, up to $4,000 per adoption No charge after deductible, up to $4,000 per adoption Affordable Care Act Preventive Services See Master Policy for complete list No charge 40% of In-Network Rate after deductible Allergy Serum 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Chiropractic Care | Up to 10 visits per plan year 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Dental Accident 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Durable Medical Equipment, DME Except for oxygen and Sleep Disorder Equipment, DME over $750, rentals, that exceed 60 days, or as indicated in Appendix A of the Master Policy require pre-authorization. Maximum limits apply on many items. See the Master Policy for benefit limits 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Medical Supplies 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Home Health/Skilled Nursing Up to 60 visits per plan year. Requires pre-authorization 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Infertility Services Select services only. See the Master Policy 50% of In-Network Rate after deductible 70% of In-Network Rate after deductible Injections | Requires pre-authorization if over $750 20% of In-Network Rate after deductible 40% of In-Network Rate after deductible Temporomandibular Joint Dysfunction Up to $1,000 lifetime maximum 50% of In-Network Rate after deductible 70% of In-Network Rate after deductible MISCELLANEOUS SERVICES Out-of-network providers may charge more than the In-Network Rate unless they have an agreement with you not to. Any amount above the In-Network Rate may be billed to you and will not count toward your deductible or out-of-pocket maximum. WWW.PEHP.ORG PAGE 17 8 99 Understanding Understanding Weber State University 2015-16 » Benefits Preview » Understanding Your EOBs Your EOB (Explanation Benefits) (Explanation of Benefits) Understanding Understanding Your EOB (Explanation of of Benefits) 88 8 Understanding Understanding 9 99 8 11 22 33 44 Your EOB Your Your EOB EOB 55 9 1 11 10 2 22 1 3 33 4 44 2 We We send an EOB each time we process a We send send an an EOB EOB each each time time we we process process a a claim for you or someone on your plan. claim for you or someone on your plan. claim for you or someone on your plan. Go Go paperless and view EOBs at your Go paperless paperless and and view view EOBs EOBs at at your your myPEHP account at www.pehp.org. myPEHP account at www.pehp.org. myPEHP account at www.pehp.org. We send an EOB each wewe process AMOUNT CHARGED send an EOB time each time process a a AMOUNT CHARGED AMOUNT CHARGED AMOUNT We CHARGED claim for you or someone on your plan. The medical provider’s (e.g., doctor, claim for you or someone on your plan. Wemedical send anprovider’s EOB each (e.g., time process a The provider’s (e.g.,we doctor, The medical doctor, The medical doctor, Goprovider’s paperless and(e.g., view EOBs at your a We sendoran EOB each time we Go paperless and view EOBs atprocess your hosptial, clinic) bill for your service. claim for you or someone on your plan. hosptial, or clinic) bill for your service. hospital, clinic) bill for your service. account www.pehp.org. hosptial, ormyPEHP clinic) bill foratyour service. claim for you or someone on your plan. 11 22 1 11 332 22 3 33 44 4 44 11/11/13 myPEHP account at www.pehp.org. Go paperless and view EOBs at your Go paperless and view EOBs at your AMOUNT INELIGIBLE AMOUNT CHARGED AMOUNT INELIGIBLE myPEHP account at www.pehp.org. AMOUNT INELIGIBLE AMOUNT INELIGIBLE 1 account at www.pehp.org. myPEHP The medical provider’s (e.g.,services doctor, The part the bill includes The part of the bill that includes services AMOUNT CHARGED The part the billorthat that includes The part of ofhosptial, the bill that includes services clinic) bill for your service. not covered by your plan. This is not covered your This is The medical provider’s (e.g., doctor, AMOUNT CHARGED not covered by your plan. plan. Thisplan. is services not by covered by your AMOUNT CHARGED AMOUNT INELIGIBLE between and the provider. between you and the provider. hosptial, or clinic) bill for your service. 2 you The medical provider’s (e.g., doctor, between you the provider. This between you and the provider. Theand part of the bill (e.g., that includes services Theismedical provider’s doctor, hosptial, or clinic) bill for your service. not covered by your plan. This is AMOUNT ELIGIBLE hosptial, or clinic) bill for your service. AMOUNT ELIGIBLE AMOUNT INELIGIBLE AMOUNT ELIGIBLE AMOUNT ELIGIBLE between you and the provider. This is PEHP’s maximum allowable This is PEHP’s maximum allowable The part of the bill that includes services AMOUNT INELIGIBLE This is PEHP’s maximum allowable This is PEHP’s allowed amount (AA). AMOUNT INELIGIBLE AMOUNT ELIGIBLE fee (MAF). This is the most we allow 3 fee (MAF). This is the most we allow not by your plan. This isservices The part the bill that includes fee (MAF). This theallow most we allow This is is PEHP’s maximum allowable This iscovered the of most we in-network The part of the bill that includes services contracted providers to charge for contracted providers toplan. charge for between you and the provider. fee (MAF). This ischarge the most we not covered by your This is allow contracted providers to for providers to charge for this service. notservice. covered by your plan. is for this However, non-contracted contracted providers toThis charge this service. However, non-contracted between you and the provider. this service. However, non-contracted However, out-of-network providers this service. However, non-contracted between you and the provider. AMOUNT ELIGIBLE providers may charge more than providers charge more than providers may may charge thanthan providers may more charge more may charge more than the AA. Avoid This is PEHP’s maximum allowable the MAF. Avoid paying more by using AMOUNT ELIGIBLE the MAF. paying more by theELIGIBLE MAF. Avoid paying by using AMOUNT the MAF. Avoid Avoid paying moremore by using using fee contracted (MAF). This is the providers most we(find allow paying by using only providers This ismore PEHP’s maximum allowable only providers (find them only contracted them in only contracted providers (find them This is PEHP’s maximum allowable only contracted providers (find them contracted providers to charge for at www.pehp.org). your network (go to www.pehp.org). fee (MAF). This is the most we allow at www.pehp.org). at www.pehp.org). (MAF). This is the most we allow atfee www.pehp.org). this service. However,tonon-contracted contracted providers charge for 4 DEDUCTIBLE contracted providers to charge for DEDUCTIBLE DEDUCTIBLE DEDUCTIBLE The set amount pay for eligible providers may chargeyou more than this service. However, non-contracted DEDUCTIBLE this service. However, non-contracted The set amount you pay for eligible charges inpaying a plan year The amount you paymore forbefore eligible The set amount you pay for eligible theset MAF. Avoid more bycost using providers may charge than The set amount you pay for eligible sharing takes place. providers may charge morecost than charges in a plan year before charges a plan year before cost charges in plan year before cost only contracted providers (find them the MAF. Avoid paying more by charges in a plan year before cost using the MAF. Avoid paying more by using sharing takes sharing takes place. sharing takes place. at www.pehp.org). only contracted providers (find them sharing takes place. place. only contracted providers (find them at www.pehp.org). at www.pehp.org). DEDUCTIBLE The set amount you pay for eligible DEDUCTIBLE DEDUCTIBLE charges in a planyou year before cost The set amount pay for eligible The set amount you pay for eligible sharing takes place. charges in a plan year before cost charges in a plan year before cost sharing takes place. sharing takes place. 5 55 3 4 We send an EOB each time we process a claim of forBenefits) 66(Explanation 77you or someone on your plan. (Explanation (Explanation of of Benefits) Benefits) Go paperless and view EOBs at your myPEHP account at www.pehp.org. 6 66 5 7 77 6 7 55 COINSURANCE COINSURANCE COINSURANCE The percentage of the cost you must pay The The percentage percentage of of the the cost cost you you must must pay pay under your plan. You may already have under under your your plan. plan. You You may may already already have have paid paid this this amount amount when when you you received received paid this amount when you received services. If so, the provider’s services. If so, the provider’s bill may be services. If so, the provider’s bill bill may may be be COINSURANCE lower than what’s shown on the EOB. COINSURANCE CO-INSURANCE 5 5 lower than what’s shown on the EOB. lower than what’s shown on the EOB. percentage of the cost must pay The percentage of the cost you pay COINSURANCE The percentage ofyou the cost youmust must 55 The COINSURANCE under your plan. You may already have under youryour plan. You may already have The percentage of the cost pay COPAY pay plan. Youyou maymust already COPAY thisunder amount when you received 66 paid COPAY The percentage of the cost you must pay paid this amount when you received under your plan. You may already have The fixed dollar amount you must pay services. If so, the provider’s bill may be The fixed dollar amount you must pay have paid this amount when you The fixed dollar amount youalready must pay under your plan. You may have lower thanyour what’s shown on the EOB. under plan. You already have services. If so, the provider’s bill may be paid this amount when received under plan. may already have received If may so,you the provider’s under your plan. You You may already have paid your this services. amount when you received paid this amount when you received lower than what’s shown on the EOB. services. If so, the provider’s billshown may be paid this when received bill mayamount be lower thanyou what’s paid this amount when you received services. If so, the provider’s bill may beon 6 COPAY lower than what’s shown on the EOB. services. If so, the provider’s bill may be The fixed dollar amount you must pay services. If the be the EOB. services. If so, so, the provider’s provider’s bill may be lower than what’s shown onbill themay EOB. under your plan.what’s You mayshown already have COPAY lower than on the EOB. 6 paid lower than what’s shown on the EOB. lower than what’s shown on the EOB. this fixed amount when you received The dollar amount you must pay COPAY CO-PAY 6 services. If so, the provider’s bill may be COPAY AMOUNT PAID AMOUNT PAID 776 lower under your plan.amount You already have The fixed dollar you must AMOUNT PAID than what’s shown on the may EOB. The fixed dollar amount you mustpay pay The fixed dollar amount you must pay The part of the bill PEHP paid. The part of the bill PEHP paid. paid this amount when you received under your plan. You may already have The part of the bill PEHP paid. under your plan. You may already have AMOUNT PAID under your plan. You may already have 7 services. If so, thepaid. provider’s bill may be paid this amount when you received The part ofthis the bill PEHP CLAIM NUMBER paid amount when you received paid this amount when you received CLAIM NUMBER 88 Keep CLAIM NUMBER lower than what’sasprovider’s shown on the EOB. services. If so, bill may bebe this number reference if you call CLAIM NUMBER services. so, the the provider’s bill may services. If so, the provider’s bill may be Keep this number as reference if you call 8 Keep this number as reference if you call lower than your what’s shown Keep this about number as reference if you on call the EOB. PEHP claim. lower than what’s shown on the EOB. lower what’s shown on the EOB. PEHP about your AMOUNT PAIDclaim. PEHP about your claim. 7 PEHP about your claim. The part of the bill PEHP paid. AMOUNT PAID YOUR TOTAL RESPONSIBILITY AMOUNT PAID YOUR TOTAL RESPONSIBILITY YOUR TOTAL RESPONSIBILITY AMOUNT PAID 999 77 The YOUR TOTAL RESPONSIBILITY The part of of the bill PEHP paid. amount ofNUMBER the billthe the provider The amount bill the provider The part of of the bill PEHP paid. The amount the bill the provider CLAIM The part the bill PEHP paid. The amount of the the you provider 8 expects you you to pay. This is bill between expects to pay. This is between you expects you to pay. This is between you Keep this number as reference if you CLAIM NUMBER expects you to pay. This is between youcall the provider. 88 and CLAIM NUMBER and the provider. CLAIM NUMBER and thethis provider. PEHP about your claim. Keep number as reference if you call and the provider. Keep this as reference call See your applicable benefitsnumber summary and master Keep this number aspolicy referenceififyou you PEHP about for complete terms of your plan. your claim. PEHP about your claim. See your applicable applicable benefits summary and master policy YOUR TOTAL RESPONSIBILITY See your benefits summary and master policy 3/26/12 call about yourand claim. your applicable benefits summary master See yourPEHP applicable summary and master policy policy 9 See for complete terms your plan. forThe complete terms of ofbenefits your plan. for complete terms of plan. amount of RESPONSIBILITY the bill the provider TOTAL forYOUR complete terms of your your plan. YOUR TOTAL RESPONSIBILITY 99 YOUR TOTAL RESPONSIBILITY expects you to Thisthe is provider between 3/26/12 you The amount of pay. the bill 3/26/12 3/26/12 The amount of the bill the provider 3/26/12 and amount the you provider. The ofpay. the This bill the provider expects to is between you expects you to pay. This is between you expects you to pay. This is between you and the provider. and the provider. See your applicable benefits summary and master policy and the provider. 10 for complete terms of your plan. See your applicable benefits summary and master policy See your applicable summary and master policy for complete terms ofbenefits your plan. CPT CODE 3/26/12 for complete terms of your plan. This code for the service you received 3/26/12 can be helpful when discussing3/26/12 your EOB with your doctor or PEHP. Weber State University 2015-16 » Benefits Preview » myPEHP How to Set Up Your myPEHP Account DURING OPEN ENROLLMENT, YOU CAN ACCESS ONLINE ENROLLMENT. YOU CAN ALSO ACCESS YOUR CLAIMS HISTORY, EXPLANATION OF BENEFITS (EOB) AND COVERAGE LEVELS ONLINE AT MY PEHP. You can enroll, access claims history, download explanation of benefits (EOB), check coverage levels, and much more by logging on to myPEHP. STEP 4: Enter your Social Security number, date of birth, and PEHP subscriber ID number to verify your identity. The 16-digit subscriber ID number can be found on your Medco/PEHP insurance card. If you do not have the number, call PEHP or fill out the online request to receive your ID number in the mail. Then, you will be asked to select a user name and password for future access. Here’s how to set up your personal account: STEP 1: Go to www.pehp.org STEP 2: Locate the “myPEHP Login” on the right side of the page. The first time you log in, you must create an account. Once you have successfully set up your profile, enter your user ID and password into the boxes to access your information. STEP 3: To set up an account, click on “Create my PEHP account.” You must agree to the conditions detailed in the document on the next page to proceed. Once you have read and agreed to the terms, click “I Agree” to continue creating your personal profile. Once you have successfully logged in, you are ready to enroll during open enrollment. You will also see a summary of all the plans you have enrolled in, a detailed list of all claims submitted to PEHP, and PDF files of your EOBs. You may also update your mailing address. However, if you wish to make any other changes outside of annual enrollment to your existing plans, you must submit a signed Change Form to PEHP. Graphical website depictions may vary from actual website.