Questions Answers
advertisement

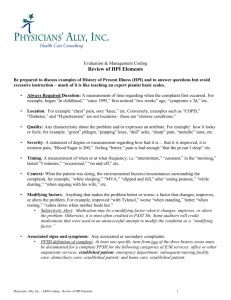
Audit Challenges with E/M Services Questions Answers Webinar Subscription Access Expires December 31. How long can I access the on demand version? You will find that in the same instructions box you utilized to access this presentation. Subscription access expires December 31, individual purchases will not expire for at least two years. If you are the purchaser, you can find your information through following these steps: 1. Go to http://www.aapc.com & login 2. Go to Purchases/Items 3. Click on “Webinars” tab 4. Click on “Details” next to the webinar 5. Find the instructions box in the middle of the page. Click on the link to the item you need (Presentation, MP3 file, Certificate, Quiz) Where can I ask questions after the webinar? The online member forums, where over 100,000 AAPC members have access to help each other with all types of questions. *Forum Posting Instructions* 1.Login to your online account 2.In the middle of the page you will see “discussion forums” 3.Click on “view all” – top right hand side 4.Select “general discussion” under “medical coding” unless you see a topic that suits you more – 5.On the top left side of the forum box, you will see a blue button, “new thread” – click on that 6.Type your question and submit 7.Check back in that location for answers as you please Can the term "non contributory" be used for PFSH? For inpatient rounding E/M servcies, is a chief complaint required for every note? If ROS is unavailable due to patient being intubated in a coma can credit be given if they note what all they did to tery and collect the ROS? If an established patient presents to the office location and the provider documents a detailed history and exam but the overall medical decision making is of "low complexity," how would you code this service? The risk would be moderate. Would this be a 99213 or 99214? For inpatient rehab-can a chief complaint be pulled from the assessment? It depends upon your MAC carrier. Some allow the use, while others require that the specific questions asked be documented. Yes the chief complaint is still required. Each note must be able to stand alone. Yes. The provider just needs to indicate why the ROS was unobtainable. It depends if you are using MDM as a required element for 2 of the 3 key components. If you are then the correct code selection would be 99213. If not then you would look at the nature of the presenting problem to see if using the history and exam as your 2 components is appropriate and code 99214. You need to consider possible overdocumentation when using just history and exam. Also, you would need to know what your MAC carrier allows. For all visits types CMS does state that the CC can be inferred from the HPI. It does not state it can be inferred from the Assessment and plan however we can use the entire record. Just use caution and do not count plan elements for HPI. Because this is a grey area you should define in your practice. Follow up to my ROS question...do you give the provider a You could allow a complete ROS as if 10+ systems were score of comprehensive ROS or how else would you score documented. it? When the provider states "HPI/ROS/PFSH" same as from prior visit, does the same level of history from the prior visit carry over? I would not recommend using the HPI documentation from a previous visit. CMS states that the ROS and PFSH can be referenced from previous visits, they do not say the HPI can. The definition of the HPI implies that these documented elements need to be a description of events from the previous visit or from the first sign/symptom to the present. For established visits, it seems that many carriers require MDM as one of the elements (out of 3) . Is this correct? Correct. You need to know what your MAC carrier requires. Requiring MDM as 2 of the 3 supports the medical necessity of the E/M level. We work with practices that even though their MAC may not require MDM for 2 of the 3, they do and have made this a requirement as part of their compliance standards. What is the source document for slide 12? CMS Internet Only Manual (IOM) Medicare Claims Processing Manual, Publication 100-04, Chapter 12, Section 30.6.1, The link that I had no longer is in use. I will have research and get back to you. Do you have the CMS regulation that states they have adopted the Marshfield guidelines or a reference for us to use? Can we pull something from the chief complaint to use in the HPI? If the provider documented the chief complaint and included elements of HPI then yes, you could count these elements towards you HPI. You do not want to count elements more than once. If the provider did not document the CC then no, this would not be best practice. At what point in the audit process do you make a note non- In this example the entire service does not need to be nonbillable, other than the blatant omissions. Example: Do billable. If the date can be inferred or an amendment done you make a consult non-billable if the providers does not then you could bill using a different E/M category. have a date and/or referring physician in his note, although he dictated on the date he saw the patient. When auditing a note and determining the MDM level, how would you score results from lab work or x rays that are pulled forward from a previous note. Also, if the provider orders the test on 1 date and reviews the results on the next date of service, would you give credit for reviewing/ordering test on both dates of service? If the EHR system auto populates previous tests, it would be appropriate to count toward the MDM. However, if the provider references these test or pulls the tests himself/herself then you could. Tests that are pending are counted in MDM under DATA as tests "ordered" or reviewed. You could also count this a new problem with work up IF in fact the problem is new to the provider. Isn't it required that out of the 2/3 for MDM, one must be the risk? I have not seen this requirement. That is not to say that a MAC carried has not provided further clarification of their requirements. Where could we find written documentation regarding authentication for all users? In our EMR it does not print out on the note. http://www.cms.gov/Outreach-and-Education/Medicare-LearningNetworkMLN/MLNProducts/downloads/Signature_Requirements_Fact_Sheet_ICN9 05364.pdf What would you recommend if the ROS/PFSH (not You could code the E/M level based all elements of the cloned/carried over) are complete, because the provider history or exam, using MDM as 2 of the 3 components. So chooses to document this way, but the HPI, CC, and MDM if MDM was SF you would level your E/M as SF. are straightforward? Since medical necessity is overarching for most carriers, code then to the lower level? When providers restate the complete history of a condition and then state "today the pt. is ...", is it appropriate to use the restating of the condition has past history and the HPI start from the statement of Today the pt is experiencing? If I'm understanding the question correctly, it appears that the provider us documenting the history as the interval history, the events between visits or leading up to this visit. In which case, yes you could count elements for HPI. Just use caution and never count 1 element twice. Can providers use "10 point review of systems done" Yes, as long as they also document the pertinent positives or negatives for the systems related to the reason for visit. Only stating a 10 point review of systems was done is not acceptable. The date in which the past ROS/PFSH was documented needs to be included in the provider's note. The statement does not necessarily need to also say "reviewed". The statement "as before" implies the provider reviewed the previous elements and there were not changes. Again, look to your MAC carrier for guidance. If the provider states ROS/PFSH "as before" (referencing date of last encounter), do they still need to state "reviewed"? When providers restate the complete history of a condition Yes, you can use the elements starting from "Today the and then state "today the pt is ...", is it appropriate to use patient is experiencing." as HPI elements. the restating of the condition has past history and the HPI start from the statement of Today the pt is experiencing? When auditing ROS and or exam elements not pertinent to the chief complaint, how can this be supported as a valid over documentation issue vs the physician performing good medicine? Is it not good medicine to check heart and lungs on all patients even if coming in for say pink eye or sprained ankle? As coders, we are not qualified to determine what specific elements should or should not be documented. This is up to the provider and his/her clinical judgment. This is an area in which the coder/audit needs to work closely with their providers and make a determination together. is "all other negative" under ROS acceptable ? Yes if the pertinent positives and negatives based on the reason for visit are documented. Stating only "all other negative" is not acceptable. Look for guidance from your MAC carrier as to whether or not they allow counting associated signs and symptoms for ROS. If the provider states patient returned for review of diagnostic results (labs, imaging), but no HPI, ROS, PFSH, documented, and no exam done, do we go by time (counseling on next steps)? or just code lowest level E&M? This visit could be leveled using time based coding as long as the documentation supported this. If no time is listed then you would have to level based on the key components. If there are not enough key components then this visit may be support reporting an E/M. Can elements of the HPI be pulled from other areas of the note like the A/P? ex: HPI-breast Ca = location; A/P=Stage II Breast Ca, ER/PR +; Can I use the stage II and ER/PR + in the A/P for severity and quality in the HPI? When the provider documentation includes elements of HPI in the plan, you can count these elements for HPI points. We can use the entire medical records for counting E/M elements. Use caution with double dipping. For this specific example, in my opinion, I would not consider the description of the provider's final assessment as HPI elements. How do you obtain a complete HPI/ROS and PMSH on a newborn that is 3 hours old? Mom is unavailable due to newborn in nicu. Do you use the nurse documenation , may the physician document that due to the patient age HPI/ROS unobtainable? For RAT/STAT, OIG does extrapolation (in terms of potential overpayment). Would you recommend doing some type of extrapolation for internal purposes? or just expand the audit sample? Can the ROS/PFSH from another provider in the same practice (most recent visit) be used if referenced? If the doctor of one specialty references the ROS/PFSH of a doctor in a different specialty in the same practice, it would still count as new patient (because of different specialty/subspecialty), regardless of the ROS reference; correct? If the physician is unable to obtain additional HPI/ROS and documents why then we can count full credit for these elements. We can use the nurse documentation for ROS but not for HPI. So signature log should contain signature of scribes or other ancillary staff as well as the physicians? My question with regard to a provider documenting history as HPI would I use the old information as past medical history and only the portion that is stated as current for the HPI of that current encounter? Yes. The signature logs should include anyone that makes entries into the medical record. If I understand the question correctly, you are using the old history as Past history and using the "interval history" for your HPI. If my understanding is correct, yes you can use interval history for HPI point. I would recommend just expanding your audit sample. Expand the sample as far as you need to, to obtain a clear understanding of the potential issue. Yes, the provider can do this if its part of the same patient medical record, the provider references it with the date and if there are any updates. can a resident be a scribe? can an APRN or PA be a scribe? Yes they can. The documentation would still need to meet the CMS or MAC carrier scribe requirements and the claim could not be billed under their NPI. For new condition with work-up planned (4 points) and lab ordered (to performed on another day) worth one data point, do you also get 4 (new condition with lab) and 1 data point (lab ordered), or is this double-dipping on the lab point? Can you count past medical, family, or social history if it is present in an electronic medical note for a specific date of service but it is not specified that it was reviewed and updated on that date of service? You can count the 4 points for new problem with work and the order/review of the lab for 1 point. is it okay to bill an office E/M with a dialysis code? When reporting an E/M service on the same day as a procedure, the E/M needs to be significant and separate from the routine or pre procedure evaluation. If not, then reporting and E/M would not be appropriate. No, the provide needs to reference it when collected from a previous date of service. So you are saying that is a provider orders lab work on one The guidelines to not specify the time in which the order or visit and then reviews that same test on the next visit, he reviewed results can be counted. Think of it this way, MDM is about the provider considering all diagnoses, is given credit in both situations? options to treat the patient and what tests to perform and how all of these things impact the patient and their other conditions. So if the initial decision is to order a lab, that is 1 element of MDM. Then when the lab results come back then the provider has to make another decision on what to do next. If that decision happens at the next visit, then you can count it during that visit. can an ED physician bill for their ER servcies if the patient is admitted from the ER?m Do we change the code to some other hospital f/u code? Thanks If the ED provider is the one admitting the patient then no. If the ED physician saw the patient and called in another provider who made the decision to admit the patient then yes. Each provider who evaluated the patient can bill for their E/M service in most instances. Look for guidance on acceptable E/M benchmarks from Is there a sample of the acceptable table to have our physicians review for E&M coding via graph or color chart? CMS and MGMA. CPT states that the ROS should be age specific so there How do you get a complete HPI/ROS on a 3 hour old newborn? Is it appropriate for the physician to document may not be evidence of 10+ systems for the provider to document on. As an auditor we need to remember the "unable to obtain HPI due to the patient age?" documentation for baby's and small children is different and should be age specific. For new condition with additional lab work-up, can you count 4 points for the new condition and 1 for the lab in data, if your practice does the draw on the same day, but not the actual analysis? I know you're not supposed to double-count the additional work-up if you actual do it and bill for it on the same day. In this instance I do not believe this is double counting. Is there an industry standard on the accuracy rate that a coder should be? There is not an "industry standard" for accuracy of a coder. This is something each practice needs to determine and include as part of their compliance standards. For moderate MDM based on prescription drugs, do they have to the drugs prescribed by the doctor, or can it be sufficient to score based on note of the drugs in the medical history (so member seeing a doctor in one specialty, taking drugs ordered by another doctor in another specialty for a different condition)? Would the doctor at least have to comment on how the drugs were considered in part of the treatment being rendered? Remember the CMS risk table state's prescription drug management. If the provider is not managing Rx drugs during the visit then it would not be appropriate to count this in your MDM. What is Rx drug management? This is another grey area. Look to your MAC carrier to see if they have defined or define this in your practice as part of your compliance standards.