Perspectives in Diabetes - American Diabetes Association
advertisement

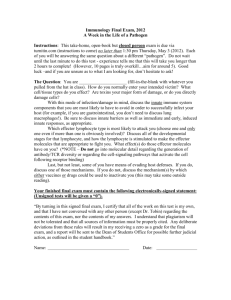
Perspectives in Diabetes The Role of Cell Adhesion Molecules in the Development of IDDM Implications for Pathogenesis and Therapy Xiao-dong Yang, S a r a A. Michie, Reina E. Mebius, Roland Tisch, Irving Weissman, and Hugh 0. McDevitt IDDM is a chronic inflammatory disease in which there is autoimmune-mediated organ-specific dtstmction of the insulin-producing p-cells in the pancreatic islets of Langerhans. 'lhe migration of autoreactive lymphocytes and other leukocytes from the bloodstream into the target organ is of clear importance in the etiology of many organ-specific autoimmunelinflanunatoqy disorders, including IllDM. In IDDM, this migration results in lymphocytic invasion of the islets (formation of insulitis) and subsequent destruction of p-cells. Migration of lymphocytes from the bloodstream into tissues is a complex process involving sequential adhesioe and activation events. This migration is controlled in part by selective expression and functional regulation of cell adhesion molecules (CAMs) on the surface of lymphocytes and vascular endothelial cells or in the extracellular matrix. Understanding the mechanisms that regalate lymphocyte migration to the pancreatic islets will lead to further understanding of the pathogenesis of IaDM. In this article, we summaxize the recent advances regarding the function of CAMs in the development of IDDM in animal models and in humans and discuss the potential for developing CAM-based therapies for IDDM. Diabetes 45: 705-710, 1996 M ost lymphocytes recirculate throughout the body, migrating from blood through organized lymphoid tissues such as lymph nodes (LNs) and Peyer's patches (PPs) or extranodal tissues such as the pancreas, then to lymph and back to blood. This migration is important in establishing effective immune surveillance ill that it allows effector lymphocytes to migrate to almost any site of antigen deposition. However, the migraFrom the Department of Immunology (X.-D.Y.), Cell Genesys, Foster City; the Departments of Microbiology and Immunology (R.T., H.O.M.) and Pathology (S.A.M., R.E.M., I.W.), Stanford Universiw School of Medicine; and the Department of Veterans Affairs (S.A.M.), Center for Molecular Biology, Palo Alto, California. Address cor~espondenceand reprint requests to Dr. Xiao-dong Yang, Department of lmrnunology, Cell Genesys Inc., 324 Lakeside Dr., Foster City, CA 94404. Received for publication 16 August 1995 and accepted in revised form 11 January 1996. CAM, celI adhesion molecule; EC, endothelial cell; ICAM, intercelIular CAM; LN, lymph node; LFA, lymphocyte function-associated antigen; mAb, monoclonal antibody; MAtlCAM-1, mucosal addressin CAM-I; PNAd, peripheral node addressin; PP, Peyer's patches; STZ, streptozotocin; TNF, tumor necrosis factor; VCAM-1, vascular CAM-1; VLA, very late antigen. DIABETES, VOL. 45, JUNE 1996 tion can also cause localized chronic inflammation that leads to damage and destruction of host tissue. IDDM is one example of such a tissue-specific chronic inflammatory disorder (1-3). Lymphocyte migration from blood into tissue is a highly complex process involving a cascade of adhesion and activation events (4-7). As illustrated in Fig. 1, many of the adhesion events involve interaction of lymphocyte cell adhesion molecules (CAMs) with their endothelial cell (EC) ligands. Some CAMs, such as lymphocyte function-associated antigen-1 (LFA-1) and EC vascular cell adhesion molecule-1 (VCAM-I),seem to be involved in lynlphocyte migration to a wide variety of tissues (8,9). In contrast, other CAMs are involved in lymphocyte migration to one or a few tissues. The lymphocyte CAMs associated with tissue-selective migration are known as homing receptors (10-13); their endothelial ligands, expressed in a tissue-selective manner either constitutively in uninflamed tissues or induced in inflamed tissues, are called vascular addressins (14-16). CELL ADHESION MOLECULES: NOMENCLATURE, STRUCTURE, AND FUNCTION CAMS can be classified into at least three major groups based on their molecular structure: selectins, integrins, and the immunoglobulin (Ig) superfamily (17). We will focus on lymphocyte and EC CAMs that appear to be involved in the pathogenesis of IDDM (Table 1). Several excellent reviews are available that give more detailed information on the other leukocyte and EC CAMs (9,17,18). L-selectinRNAd. L-selectin is a member of the selectin family of CAMs characterized by an NH,-terminal carbohydrate-binding lectin domain that binds to carbohydrate determinants on several EC glycoproteins (10,19). These glycoproteins are collectively known as peripheral node addressin (PNAd), many of which react with monoclonal antibody (mAb) MECA-79 (Table 1) (14). L-selectin is expressed on most mononuclear cells except for some activated andlor menlory lymphocytes and functions to mediate an initial and transient attachment, or rolling, of leukocytes on vascular ECs (9,17,20). L-selectin is involved in lymphocyte traficking to some extranodal sites of inflammation, including the thymus, skin, and pancreas (21-26). PNAd is highly expressed by ECs in LNs but not in PPs, implying that the degree to which L-selectin participates in tissue-selective - Altachmentl Rolling Triggering 1 Activation Firm Adhesion Blood flow I Migration A Lymphocyte receptor PNAd CD34 GlyCAM MAdCAM Endothelial ligand Selective targets for anti-adhesion molecule mAbs Cytokines Chemokines Mei-14 (anti-L-selectin) ICAM-1 ICAM-2 VCAM-1 MAdCAM-1 KBA, 2E6 (anti-a,) YN 111.7 (anti-ICAM-1) R1-2 (anti-ad) MK 2.6 (anti-VCAM-1) KBA, 2E6 (anti-aL) YN 1H.7 (antl-ICAM-1) lymphocyte migration may be partially determined by the expression pattern of its ligands. a4P7 integrin/BIAdCAM-1. The integrins are a large family of noncovalently-linked heterodimers that mediate a variety of cell-cell and cell-extracellular matrix interactions (17,27). Integrin molecules are structurally characterized by a unique combination of 1 of 15 known a-chains with 1 of 8 P-chains. Three integrins found on lymphocytes, cw4P1, a4P7, and aLP2, have well-defined roles in lymphocyte migration and in immune responses via their interactions with ligands on ECs, extracellular matrix, or antigen-presenting cells. a4P7 integrin is a lymphocyte homing receptor that mediates lymphocyte migration to mucosal sites such as PPs via binding to the mucosal addressin CAM-1 (MAdCAM-1) (11,12,28). MAdCAM-1, a glycoprotein with several Ig-like domains and a single mucin domain, is constitutively expressed by vessels in mucosal lymphoid organs (PPs and mesenteric LNs), intestinal lamina propria, and exocrine pancreas (15,19,25). a4P7 also binds to VCAM-1 and fibronectin, both of which are ligands for a4pl integrin (30). a4pl integrin/VCAM-Yfibronectin. The pl-integrh (CD29) can pair with several a-chain integrins to form a unique aXP1 FIG. 1. Sequential multistep model of lymphocyte/endothelial adhesion. Extravasculation of lymphocytes from blood into the tissue is mediated by a cascade of adhesive interactions between lymphocytes and endothelial cells. Such interactions involve a number of diverse CAMS in a sequential and multiple-step process. This model implies that lymphocyte migration can be controlled and regulated at multiple points. It also provides a working model for designing CAM-based therapeutic intervention strategies. heterodimer (previously termed very late antigen [VLA]) (31). a 4 p l integrin (VLA-4, CD49dlCD29) has at least two distinct ligands: endothelial VCAM-1 and the extracellular matrix protein fibronectin (Table 1). VCAM-1, a member of the Ig family of adhesion molecules, is strongly expressed in vivo by ECs in a wide variety of inflammatory sites (32,33). aLP2 integrin/ICAMs. The P2-integrin (CD18) can pair with various cw-chain integrins (CD11) to form functionally distinct CAMs. For instance, P2 pairing with aL forms cwLP2, known as LFA-1 (CDlla/CD18), which is expressed on all leukocytes, while Mac-1 (CDllbICDlS), formed by pairing of P2 with cwM, is predominantly expressed by macrophages and neutrophils (Table 1). Lymphocyte LFA-1 is thought to participate in the binding of lymphocytes to vascular endothelium in many tissues, including LNs, PPs, and multiple extranodal sites of inflammation (6,8). The endothelial ligands for LFA-1 include ICAM-1 and ICAM-2 (5). Multistep model of lymphocyte/endothelial adhesion. Studies on the adhesive interactions between leukocytes and vascular endothelium under flow or shear force reveal that such interactions involve a number of diverse CAMs in a multiple-step process (Fig. 1) (4,6,17). An initial transient TABLE 1 Cell adhesion molecules: nomenclature and expression Lymphocyte CAMS selecti in (Mel-14 Ag, CD62L) Expression Ligands Expression Leukocytes, including most lymphocyte subsets PNAd Peripheral LNs, activated endothelium Lymphocytes MAdCAM-1 VCAM-l(CD106) Fibronectin Mucosal lymphoid tissues, activated endothelium Activated endothelium, dendritic cells Extracellular matrix aLp2 (LFA-1, CDllaICDl8) Leukocytes aMP2 (Mac-1, CDllb/CD18) Monocytes and neutrophils ICAM-1 Factor X Fibrinogen Endothelium, activated lymphocyte, dendritic cells Serum Serum Leukocytes VCAM-1 Fibronectin Activated endothelium, dendritic cells Extracellular matrix Leukocytes ECs Epithelial cells Laminin Fibronectin Collagens Extracellular matrix Extracellular matrix Extracellular matrix (w3p1 (WAS, CD49cICD29) Endothelium, activated lymphocyte, dendritic cells Endothelium Leukocytes DIABETES, VOL. 36, JUNE l99G attachment, or rolling, is mediated by the interaction of selectins such as L-selectin with endothelial carbohydrate ligands or by the interaction of lymphocyte a4p7 with MAdCAhl-1 (step 1). If the rolling leukocytes encounter appropriate activating, chemotactic, or chemokinetic factors in the local microenvironment, they may then undergo an activation step that leads to strong adhesion, usually mediated by activated integrins (step 2). These microenvironmental factors may include cytokies, such as tumor necrosis factor (TNF)-a, which can activate both attached lymphocytes and vascular ECs, and chemokines such as RANTES (regulated upon activation, normally T-cell expressed and secreted), which may play an important role in the recruitment of different lymphocyte subsets. The strong adhesion can be followed by lymphocyte transendothelial migration (diapedesis) into tissue (step 3). Depending on the differentiation ancVor activation stages of the cells and the nature of the stimu1;atory signals they receive, different types of leukocytes and different subsets of lymphocytes may undergo this process by slightly different steps (6,7). Nevertheless, this model of sequential cellular adhesive interactions implies that lymphocyte migration can be regulated at multiple points. It also provides an important working model for designing m vivo therapeutic intervention protocols (Fig. 1). Obviously, CAMs are not only involved in lymphocyte migration but also play critical roles in many other aspects of the immune response. However, in this article we will focus our discussion on the involvement of CAMs in lymphocyte migration into the pancreatic islets. To investigate lymphocyte migration in a chronic inflammatory disease such as IDDM, a series of studies covering different time points during the disease process is necessary. For this purpose, animal models have been used to delineate the lymphocyte/endothelial adhesion pathways involved in the diabetogenic process. The NOD mouse offers an ideal model for these studies because 1) it spontaneously develops IDDM that closely resembles human IDDM; 2 ) it develops lymphocytic infiltrates in several wgans, including pancreas, thyroid, and salivary glands, allowing comparison of different tissue-selective adhesion pathways in the same animal; and 3 ) mAbs are available against a wide variety of murine lymphocyte and endothelial CAMs. TISSUE-SELECTIVE LYMPHOCYTE MIGRATION TO PANCREATIC ISLETS IN IDDM: LESSONS FROM NOD MICE The developmental biology of vascular CAM expression in NOD mouse pancreas has been investigated using immunohistochemistry. MAdCAM-1, but no PNAd, is found on many vessels in exocrine pancreas of both NOD and control C57BLKA mice during the first 3 weeks after birth. In NOD mice, T-cells and macrophages are first detected in the islets at -18-21 days of age. Macrophages (Mac-1') appear to enter the islets a few days earlier than CD3+ T-cells. Vessels with the morphology of high endothelial venules, which are the vessels involved in most lymphocyte migration from blood into LNs and PPs, develop aaacent to the islets at the time when T-cells enter the islets (X.-D.Y., S.A.M., R.E.M., I.W., H.O.M., unpublished observations). These observations suggest that monocytes or macrophages may be the initial islet-infiltrating cells and that the formation of high endothelial venules may be crucial for the early lymphocytic accumulation. From 3 weeks of age, increasing numbers of mononuclear DIABETES, VOL. 46, JUNE 1996 TABLE 2 CAM expression on infiltrating lymphocytes and vascular ECs within the endocrine pancreas of NOD mice Lymphocyte CAMS Age (weeks) Endothelial CAMS - L-selectin a4P7 LFA-1 PNAd MAdCAM-1 VCAM-1 For expression of lymphocyte CAMS on the islet infiltrating cells: -I+, <lo%; +, 10-3004 ++, 30-60%; +++, >60%of the infiltrating cells expressing CAMs. For expression of EC C.4Ms in the infiltrated islets: -/+, <5%; +, 510%) ++, 10-40%; +++, >40% of the infiltrated islets expressing CAMs. cells, including T- and p-cells, accumulate around the islets @eri-insulitis) and gradually invade the islets (intra-insulitis). In parallel with the development of insulitis, expression of some CAMs is upregulated, while that of others remains unchanged (Table 2) (25,261. MAdCAM-1 seems to be the predominant addressin expressed on ECs in and acijacent to the islets at early stages of insulitis (5-7 weeks). In contrast, very little PNAd expression is seen until there is significant insulitis (-8 weeks of age). As insulitis progresses, the number of vessels expressing MAdCAM-1 and PNAd increases (Table 2). Both of these addressins are expressed mainly by peri-islet high endothelial venules (25). While few L-selectin expressing lymphocytes are found in the islets during the early stages of insulitis, most infiltrating cells express high levels of the a4p7 integrin throughout the disease process. The expression of a4p7 by lymphocytes correlates with high expression of MAdCAM-1 by ECs, further suggesting a predominant role for the mucosal lymphocyte homing pathway in the development of insulitis (25,341. Moreover, most islet-infiltrating T-cells express low levels of L-selectin and high levels of LFA-1, u4p7, VLA-4, and CD44, a phenotype for activatedlmemory T-cells (26). The tissue nonspecific CAMs, such as LFA-1 and ICAM-1, are expressed by almost all islet-infiltrating lymphocytes during the disease process. ICAM-1 is expressed by the endothelium of most islet vessels in both uninflamed and inflamed islets (25,261. It remains uncertain whether islet endocrine cells, particularly the p-cells, express ICAM-1. If ICAM-1 is expressed, an LFA-l/ICAM-1 interaction between lymphocytes and target p-cells could have at least two potential functions: 1) delivery of costimulatory signals for activation of T-cells andlor 2 ) mediation of direct killing of p-cells by cytotoxic T-cells. The failure to detect expression of ICAM-1 on islet endocrine cells may simply be due to the low sensitivity of current immunohistochemical approaches. VCAM-1 is expressed by vessels in exocrine and endocrine pancreas of diabetes-prone NOD mice as well as nondiabetes-prone BALB/c mice (25,26,35). Only a few VCAM-Iexpressing vessels are found within the islets (uninflamed or inflamed), whereas many are found in the exocrine-pancreas (Table 2). There is also VCAM-1 expression on some dendritic cells infiltrating the NOD islets (26). These findings suggest that these tissue nonspecific CAMs may function as costimulatory molecules in the local immune response. TABLE 3 Anti-CAM-based imnmnotherapy in IDDM in mice -- --- - Inhibition of various forms of IDDM Target Spontaneous Adoptivetransfer Cyclophosphamideor STZ-induced Ref. 24, 34, 36 24, 34, 35, 36, 38 Unpublished data Unpublished data 35 41, 43 35, 36, 41, 43 41, 42, 43 41, 42, 43 45 -, no effect; -I+, 0-500h inhibition of diabetes incidence; +, 50-60% inhibition; + +, 60-80% inhibition; + + +, >80%inhibition; ND, not determined. Alternatively, they may play accessory roles in mediating lymphocytic infiltration into the pancreas. In addition to inflammation of the pancreatic islets, NOD mice develop lymphocytic infiltration of other organs such as salivary gland and thyroid. This makes NOD mice an invaluable model to study the mechanisms involved in tissueselective lymphoc-yte trafficking to sites of chronic infiammation. In contrast to insulitis, which develops in the first few weeks of life, overt lymphocytic infiltration of the salivary gland (sialadenitis) is not seen in our colony until around 6 months of age. The inflamed salivary glands show marked vascular expression of PNAd and VCAM-1 but no detectable expression of MAdCAM-1 (26,34). ICAM-1 is expressed by ECs as well as dendritic cells in the infiltrated areas. The lymphocytes infiltrating the salivary glands show CAM expression similar to that of LN lymphocytes: LFA-I+, CD44+, some L-selectin+,and many a4+ (26). Overall, these findings suggest that an interaction of mucosal homing receptor a4@7 and its vascular addressin, MAdCAM-1, is a major adhesion pathway responsible for selective lymphocytic migration to the islets, while VL4-41 VCAM-1 and probably L-selectin1PNAd interactions may primarily mediate lymphocyte migration into salivary glands and possibly other organs (34). More importantly, this type of tissue-selective homing in a chronic inflammatory disease appears t o be determined by the selective expression of vascular addressins on ECs (34). In vivo studies using mAbs that recognize lymphocyte or EC CAMS have been carried out to determine which adhesion pathway or pathways have a prominent role during the diabetogenic process (Table 3). Treatment of NOD mice with mAb Mel-14 (anti-L-selectin) leads to efficient protection against the spontaneous occurrence of IDDM if given early in the disease process, e.g., from birth to 4 weeks of age (34,36). However, Mel-14 is unable to inhibit an ongoing diabetogenic process if administered after the onset of insulitis, for instance at 10 weeks of age (34). This may simply be due to the fact that most T-cells in young animals have a naive phenotype se select in^'^^), whereas more T-cells with an activatedmemory phenotype (L-selectin- Or 'Ow ) are found in older mice. Recently, it has been shown that only the L-selectin- T-cell population from diabetic NOD mice is able t o transfer the disease (37). These data imply that L-selectin may only play a role in the initial phase of insulitis development in young animals (<4 weeks) and that in the late phase, integrins such as a4@7can function to mediate both lymphocyte rolling and strong adhesion on ECs in the mucosal lymphoid tissues (6,7). Strikingly, when the a4-integrin receptor is blocked by the Rl-2 mAb, NOD mice are signscantly protected from both spontaneous diabetes and adoptive-transfer disease (24,34,35,38). This treatment also prevents the development of insulitis, suggesting that protection from IDDM by R1-2 mAb may result from direct inhibition of lymphocyte migration into the islets (24,34). Moreover, our preliminary data demonstrate that antiLp7integrin and anti-MAdCAM-1 mAbs can also inhibit spontaneous development of IDDM in NOD mice (Table 3) (X.-D.Y., S.A.M., H.K. Sytwu, H.O.M.). Anti-VCAM-1 antibody marginally delays but fails to prevent disease in an adoptive-transfer model (35). Unlike anti-LFA-1 and anti-ICAM-1 treatment, which induces tolerance (39), blockade of L-selectin or a4-integrin receptor appears to affect neither autoimmune responses to @-cellsnor immune responses to foreign antigens, suggesting that the IDDM-protective effect induced by blocking L-selectin or a4-integrin receptors is not a result of immune suppression (24,34,40). Interestingly, the inhibition seems to be tissue-selective, because sialadenitis is unaffected by either anti-L-selectin or anti-a4integrin treatment (34). Blocking LFA-1 andlor ICAM-1 receptors in vivo by specific mAbs has been shown to inhibit the spontaneous development of IDDM in NOD mice and streptozotocin (STZ)-induced insulitis and diabetes in mice (Table 3) (4143). Nevertheless, it remains controversial whether the LFAIACAM-1 lymphocytelendothelial adhesion pathway is involved in the diabetogenic process, since administration of both anti-LFA-1 and anti-ICAM-1mAbs is required to prevent STZ-induced disease and treatment with either anti-LFA-1 or anti-ICAM-1 fails to inhibit disease in adoptive-transfer model in NOD mice (42,43). This raises the question of how LFA-1 and ICAM-1 function in the development of autoimmunity and diabetes. On one hand, it is conceivable that LFA-1ACAM-1 may be involved in strengthening the interaction between T-cells and target p-cells and facilitating p-cell killing andor provide costimulatory signals for T-cell activation (5). On the other hand, there does not appear to be increased LFA-1 and ICAM-1 expression in inflamed islets during disease progression (Table 2). Therefore, LF'A-MCAM-1 interactions may not be a s important as the a407hLAdCAM-1 pathway in the control of tissue-selective lymphocyte homDIABETES, VOL. .ZZ, JUNE 1996 ing to the islets. One potential problem in using anti-LFA-1 and anti-ICAM-1 treatment as a therapy is the risk of inducing immune suppression and/or exacerbation of the disease. Treatment of mice with anti-LFA-1 or anti-ICAM-1 enhances the severity of experimental allergic encephalomyelitis, an animal model for multiple sclerosis (44). Blocking ccMP2-integrin (Mac-1) with ahti-Mac-1 antibody also prevents dlabetes in an adoptive-transfer model in NOD mice, possibly via inhibiting recruitment of monocytes, macrophages, and other inflammatory cells in the islets (45). During the evolution of diabetes, expression of certain CAMs such as MAdCAM-1 in the islets may be developmentally programmed and may have a crucial role in initial tissue-selective lymphocyte migration and in the priming of autoreactive lymphocytes. After activation, lymphocytes and inflammatory cells release a variety of biologically active materials, such as cytokines and chemokines, which in turn activate and stimulate expression of CAMs on ECs and lymphocytes, resulting in more lyrnphocytic influx (46,47). Among these cytokines, TNF-a, y-interferon, and interleukin10, are known to be involved in stimulation of CAM expression and are essential for the formation of insulitis (48-53). Thus, expression of CAMs and their role in the diabetogenic process may in turn be regulated by cytokine production and function. THE ROLE OF CAMS IN HUMAN IDDM The function of CAMs in human IDDM has recently been investigated. However, such studies are hampered by the limited availability of human pancreatic tissues, particularly from prediabetic individuals. Much of the published work has compared expression of certain CAMs in the pancreases of diabetlc or newly diagnosed diabetic patients with the pancreases from individuals without diabetes (54-57). By immunostaining, ICAM-1 has been found on the vessels of inflamed islets but not on vessels from uninflamed pancreases. It is still unclear whether ICAM-1 i s expressed on endocrine cells found within the islets (54,57,58). LFA-3, an EC ligand for CD2, is found on ECs of pancreases taken from people with IDDM. In two IDDM patients, VCAM-1 expression was found on some dendritic cells scattered throughout the pancreas but not on vascular endothelium (65,57). The significance and implication of these results in human IDDM remains uncertain, especially with regard to the function of these molecules in the control of lymphocyte trafficking. Furthermore, since the majority of studies have used pancreatic material from overtly diabetic patients, the end stage of the diabetogenic process, it is difficult to assess the potential function of CAMs during the early development of insulitis. One interesting aspect of such studies in humans is the observation that the serum levels of the extracellular domain of CAMs such as soluble ICAM-1 (SICAM-1) appear to be increased in some IDDM patients and their first-degree relatives (59,60). In addition, SICAM-1 appears to inhibit specific anti-p-cell T-cell responses (59). Whether these observed phenomena are specific to the diabetogenic process and what role soluble CAMs may play in the autoimmune response anti diabetes process need further investigation. DIABETES, VOl,. 45, JUNE 1996 Lymphocyte-endothelial adhesion followed by transendothelial migration is a key event in the development of organspecific autoimmunity. Selective interactions of certain cellsurface molecules regulate lymphocyte migration under normal as well as pathological inflammatory conditions. NOD mice are an ideal model for investigation of the role of CAMs in regulation of lymphocyte migration t o the target organs in chronic inflammatory diseases such as IDDM. Both immunohistological and in vivo therapeutic studies in NOD mice strongly suggest that there are tissue-selective lymphocytic homing pathways for insulitis development; the mucosal (a4P7/MAdCAM-1) adhesion system appears to be one of the predominant ones. The fact that blocking these pathways leads to successful intervention in the diabetogenic process suggest that CAMs provide a potential therapeutic target for human IDDM (36,61). Further studies on IDDM patients will prove helpful for understanding IDDM pathogenesis, in addition to providing a basis for designing CAM-based therapeutic approaches. ACKNOWLEDGMENTS This work was supported by grants from the National Institutes of Health and the Department of Veterans Affairs. X.-D.Y., R.E.M., and R.T. were recipients of Juvenile Diabetes Foundation International, Arthritis Foundation, and National Institute of Health fellowships, respectively. REFERENCES 1. Castano L, Eisenbarth GS: Type-I diabetes: a chronic autoimmune disease of human, mouse, and rat. Annu Re?) Immunol 8:647-679, 1990 2. Hossini AA, Greiner DL, Friednlan HP, Mordes JP: Immunopathogenesis of diabetes mellitus. Diabetes Rev 1:43-75, 1993 3. Bach J-F: Insulin-dependent diabetes mellitus as an autoimmune disease. Endocrine Re11 15:516-542, 1994 4 . Butcher EC: Leukocyte-endothelial cell recognition: three (or more) steps to specificity and diversity. Cell 6$:10'33-1036, 1991 5. Springer TA: Adhesion receptors of the immunc system. iliituw 34k42.5434, 1990 6. Bargatze RF, Jutila MA, Butcher EC: Distinct roles of L s e l ~ c t i nand integrin alpha 4 beta 7 and LFA-I in lymphocyte honiing to Peyer's patch-HEV in situ: the multistep model confirmed and refined. I~rrrrttcnity 399-108, 1995 7. Jones DA, McIntire LV, Smith CW, Picker LJ:A two-step adhesion cascade for T cclVendothelial cell interactions under flow conditions. d Clin Invest 94:2443-2450, 1994 8. Hamann A, Jahlonski-Westrich D, Duijvestijn A, Butcher EC. Baisch H, Harder R, Thiele H-G: Evidence for an accessory role of LFA-1 in lymphocyte-high endothelium interaction during homing. J Infmc~nol 140593-699, 1988 9. Carlos TM, Harlan JM: Leukocyte-endothelial adhesion molecules. B/ood 84:2068-2101, 1994 10. Gallatin WM, Weissman lL, Butcher EC: A cell-surface molecule involved in organ-spccific homing of lynryl~ocyles.Nnturc 30430-34, 1983 11. Holzmann B, Mclntyre BW, Weissman IL: Identification of a murine Peyer's patch specific lynlphocyte homing receptor as an integrin molecule with an a chain homologous to human VL4-4a. CcLL ,5637-46, 1989 12. Hu MCT, Croue DT. Weissman IL, Holzmann R: Cloning and expression of mouse integrin Pp(p7): a functional role in Peyer's patch-specific lymphocyte homing. Proc Nntl Acad Sci USA 89:8254-8258, 1992 13. Picker W, Michie SA, Rott LS, Butcher EC: A unique phenotype of skin-associated lymphocytes in hun~an:preferential expression of the HECA-452 cpitope by benign and malignant T cells at cutaneous sites. Am J Pnthol 136:10.53-1068, 1990 14. Streeter PR, Rouse RT, Butcher EC: Immunohistologic and functional characterization of a vascular addressin involved in lynxphocyte homing into peripheral lymph nodes. J Cell Blol 107:1853-1862, 1988 15. Streeter PR, Berg EL, Rouse BTW, Bargatze RK, Butcher EC: A tissue specific endothelial cell molecuIe involved in lymphocyte homing. Natrcw 331:41-46, 1988 16. Picker LT,Kishimoto TK, Smith CW, Wernack RA, Butcher EC: ELAM-I is an adhesion molccule for skin-homing T cells. Natclw 349:796-799, 1991 17. Springer TA: Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm. Cell 76:301-314, 1994 709 18. Bevilacqua MP: Endothelial-leukocyte adhesion molecules. Annu Reu Immunol 11:767-804, 1993 19. Lasky LA, Singer MS, Yednock TA, Doebenko D, Femie C, Rodriguez 8, Nguyen T, Stachel S, Rosen SD: Cloning of a lymphocyte homing receptor reveals a lectin dommn. Cell 56:104&1055, 1989 20. Jung TM, Gallatin WM, Weissman IL, Dailey MO: Down-regulation of l 1988 homing receptors after T cell activation. J I m m u l ~ o 141:4110-4117, 21. Michie SA, Rouse RV: Tr&c of peripheral B and T lymphocytes to hyperplastic, preneoplastic thymuses of AKR mice. Am J P a l h 138:10151025, 1991 22. Michie SA, Streeter PR, Butcher EC, Rouse RV: Lselectin and a4p7 integrin hon~ingreceptor pathways mediate peripheral lyn~phocytetraffic to AKR mouse hyperplastic thymus. .4m JPothol 147:412-421, 1995 23. Dawson J, Sedgwick AD, Edwards JCW, Lees P: The n~onoclonal antibody MEL14 can block lymphocyte migration into a site of chronic inflammation. Eur J Immunol 221647-1650, 1992 24. Yang X-D, Karin N, Tisch R, Steinman L, McDevitl HO: Inhibition of insulitis and prevention of diabetes in NOD mice by blocking L-selectin and VLA4 adhesion receptors. Proc Natl Acad Sci USA 90:10494-10498, 1993 25. Hannincn A, Taylor C, Streeter PR, Stark I S , Sarte JM, Shizunl JA, Simell 0 , Michie SA: Vascular addressins are induced on islet vessels during insnlitis in nonobese diabetic mice and are involved in lymphoid cell binding to islet endothelium. J Clin Invest 92:3509-2515, 1993 26. Faveeuw C, Gagnerault MC, Lepault F: Expression of homing and adhesion niolecules in infiltrated islets of Langerhans and salivary glands of nonobese diabetic mice. J Irnw~unol1525969-5978, 1994 27. Hynes RO. Integrins: versatility, modulation, and signaling in cell adhesion. Cell 69: 11-25, 1992 28. Berlin C, Rrrg EL, Briskin MJ. Andrew DP, Kilshaw PJ, Holzmann B, Weissman IL, Hamann A, Butcher EC: a4P7 integrin mediates lymphocyte binding to the mucosal vascular addressin MAdCAh-I. Cell 74: 185195, 1993 29. Briskin MJ, McEvoy Lhl, Butcher EC: MAdCAM-I has homology to immunoglobulin and mncin-like adhesion receptors and to 1gA 1. Nnt71re 363:461-464, 1993 30. Ruegg C, Postigo k4, Sikorski EE, Butcher EC, Pytela R, Erle DJ: Role of integrin alpha 4/beta P in lymphocyte adherence to fibronectin and VCAM-I and in homotypic cell clustering. J Cell Biol 117:179-189, 1992 :31. Hemler ME: VLA proteins in the integrin family: structures, funclions, and their role on leukocytes. Annu Reu Itr~w~unol 8:365-400, 1990 :i2. Usborn L: Leukocyte adhesion to endothelium in inflammation. Cell 623-6. 1990 33. Lobb RR, Hcrnler ME: The pathophysiologiral role of alpha4 integrin in vivo. J Clin Invest 94:1722-1728, 1994 34. Yang X-D, Michie SA, Karin N, Tisch R, Steinman L, McDeritt H O A predominant role of integrin a4 in the spontaneous development of autoimmune diabetes in nonobese diabetic mice. Plac Na,tlAcad Sci USA 91:12604-12608, 1994 35. Baron JL, Reich EP, Visintin I, Janeway CW: The pathogenesis of adoptive murine autoimmune diabetes requires an interaction between alpha Cintegrins and vascular cell adhesion molecule-1. Clin Inuest 93: 1700-1708, 1994 36. Yang X-D,Michie SA, Tisch R, Karin N, Steinman L, McDevitt HO: Cell adhesion molecnles: a selective therapeutic target for allerlation of IDDM. J AutoCmmunity 7:859-864, 1994 37. Lepault F, Gagnerault MC, Faveeuw C. Bazin H, Boitard C: Lack of I.-selectir~expression by cells transferring diabetes in NOD mice: ins~ghts into the mechanisms involved in diabetes prevention by Mel-14 antibody treatment. Eur J Iw~munol25 1502-1507, 1995 38. Burkly LC, Jakubowski A, Hattori M: Protection against adoptive transfer of autoimmune diahetes mediated through very late antigen-4 integnn. Diobetes 43:529-534, 1994 39. Isobe M, Yagita H, Okunlura K, Ihara A. Specific acceptance of cardiac allografl after treatment with antibodies to ICAM-I and LFA-1. Science 255:112&1127, 1992 40. Tisch R, Yang X-D, Singer SM, Liblau RS, Fugger L, McDevitt HO: Immune response to glutamic acid decarboxylase correlates with insulitis in non-obese diabetic mice. Nature 366:72-75, 1993 41. Hasegawa Y, Yokono K, Taki T, Ammo K, Tominaga Y, Yoneda R, Yagi N, Maeda S, Yagita H, Okumua K, Kasuga M: Prevention of autoimmune insulin-dependent diabetcs in non-obese diabetic mice by anti-LFA-1 and anti-ICAM-l mAb. Int Immunol 6:831-838, 1994 42. Hayashi T, Hashimoto S, Kameyama Y: Reduced streptozotocin-induced insulitis in CD-1 mice by treatment with anti-intercellular adhesion molecule-1 and anti-lymphocyte function associated antigen-1 monoclonal antibodies together with lactic dehydrogenase v i ~ u sinfection. Int J Exp Path 75:117-121, 1994 43. Herold KC, Vrzys V, Gage A, Montag AG: Prevention of autoimmune diabetes by treatment with anti-LFA-l and anti-ICAM-1 monoclonal antibodies. Cell Immn~nol157:48R-500, 1994 44. Cannella B, Cross AH, Raine CS: Anti-adhesion molecule therapy in experimental autoimmune encephalomyelitis. J Nenoroirnmn~nol46:4356, 1993 45. Ilutchings P, Kosen H, O'Reilly L, Simpson E, Gordon S, Cooke A: Transfer of diabetes in mice prevented by blockade of adhesion-promoting receptor on macrophages. Nature 348:639-642, 1990 46. Doukas J , Pober JS: IFN-y enhances endothelial activation induced by l 1990 tumor necrosis factor but not 1L-1. J I m n ~ u n o 1451727-1733, 47. Doukas J, Mordes JP: T lymphocytes capable of activating endothelial cells in vitro are present in rats with autoimmune diabetes. .I I?nmunol 150:1036-1046, 1993 48. Yang X-D, Tisch R, Singer SM, Cao ZA, Liblau R, Schreiber RD, McDcbitt HO: Effect of tumor necrosis factor CY on insulin-dependent diabetes ~uellitusin NOD mice. I. The early development of autoimmunity and diabetogenic process. J E q Med 180:995-1004, 1994 49. Yang X-D, McDevitt HO: Role of TNF-a in the development of autoimmunity and the pathogenesis of insulin-dependent diabetes mellitus in &OD mice. Circ Shock 43:198-201, 1994 50. Picarella DE, Kralz A, Li C , Huddle NH, Flavell RA: Transgenic tumor necrosis factor (TNF)-a production in pancreatic islets leads to insulitis, not diabetes. J Irnmunol 150:4136-4150, 1993 51. Higuchi Y, EIerrera P, Muniesa PJH, Belin D, Ohashi P, Aichele P, Orci L, Vassalli J-D, Vassalli P: Expression of a tumor necrosis factor a trar~sgene in murine pancreatic p cells results in severe and permanent insulitis without evolution towards diabetes. J Exp Med 176:1719-1731, 1992 52. Lce MS, Sarvetnick N: Induction of vascular addressins and adhesion molecules in the pancreas of IFN-gamma transgenic mice. J Irnmunol 1524597-4603, 1894 53. Wogensen L, Huang X, Sawetnick N: Leukocyte extravasation into the pancreatic tissue in transgenic mice rxprrssing interleukin 10 in the islets of Langerhans. J E x p hfed 178.17&185, 1993 54. Vives M, Soldevila G, Alcalde L, Lorenzo C, Son~ozaN, wol-Borrell R: Adhesion molecoles in human islet p-cells: de novo induction of ICAM-1 but not LFA-3. Diabetes 40:1382-1390, 1991 65. Hanninen A, Jalkanen S, Salnii M, Toikkanerr S, Nikolakaros G, Simell 0 : hlacrophages, T cell receptor usage, and endothelial cell activation in the pancreas at the onset of insulin-dependent diabetes mellitus. J Clin Invest 90: 1901-1910, 1992 56. Itoh N. Hanafi~saT, Miyazaki A, Miyagawa J-1, Yamagata K, Yanlarnoto K, Waguri M, I~nagawaA, Tamura S, Inada M, Kawata S, Tarui S, Kono N, Matsr~zawaY: Mononulear cell infiltration and its relation to the expression of major histocompatibility complex antigens a r ~ dadhesion molecules in pancreas biopsy specimens from newly diagnosed insulindependent diabeles mellitus patients. J C1i.r~Invest 922313-2322, 1993 57. Somoza N, Vargas F, Roura-hlir C, Vives-Pi M, Teresa M, Jaraquemada D, Pujol-Borrell R: Pancreas in rrrent onset insulin-dependent diabetes mellitus: changes in HLA, adhesion molecules and autoantigens, restricted T cell receptor VB usage, and cytokine profile. J Imrnunol 153:1360-1377, 1994 58. Campbell IL, Cutri A, Wilkinson D, Boyd AW, Ilanison LC: Intercellular adhes~onmolecr~le1 is induced on isolated endocrine islet cells cytokines but not by reovinls infection. Pror Natl Acad Sci USA 8642824286, 1989 59. Roep BO, Heidenthal E, de Vries RR, Kolb H, Martin S: Soluble fonns of interrellr~laradhesion molecule-1 in insulin-dependent diabetes mellitus. Lancet 343:1590-1593, 1994 60. Lampeter ER, Kishimoto TK, Rothlein R, Mainolfi EA, Bertrarns J , Kolb H, Martin S: Elevated levels of circulaling adhesion molecules in IDDM patients and in subjects at risk for IDDM. Diob~fes41:1668-1671, 199'2 61. Yang X-D, Tisch R, McDcvitt HO: Selective targets for imn~unotherapyin autoimmune disease. Chem Immur~ol60:20-31, 1994 DIABETES, VOL. 45, JUNE 199G