View presentation
advertisement

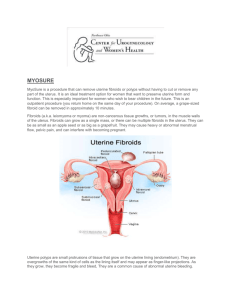
UTERINE FIBROID TREATMENT PATTERNS IN THE THREE YEARS FOLLOWING DIAGNOSIS Machaon M. Bonafede, PhD, MPH Director, Outcomes Research Truven Health Analytics Inc. Cambridge, Massachusetts USA (603) 580-5587 machaon.bonafede@truvenhealth.com Machaon M. Bonafede, PhD, MPH1; Ellen Riehle, MPH1; Scott Pohlman, MS2; Kathleen A. Troeger, MPH2 Truven Health Analytics; 2Hologic, Inc. 1 BACKGROUND ANALYSIS RESULTS (CONT’D) Uterine fibroids (also known as leiomyomas or myomas) are the most common benign tumors in women. • Although often asymptomatic, some uterine fibroids can cause abnormal uterine bleeding and pelvic pain.1,2 • Research suggests that over 60% of women will develop uterine fibroids in their lifetime, with incidence increasing with age.3,4 • Treatments options include symptom management, removal of fibroids, and hysterectomy. • Uterine fibroids are the leading indication for hysterectomies in the US.4 • There is evidence supporting the use of minimally-invasive treatments to remove fibroids with lower costs, complication rates and higher quality-of-life outcomes compared to hysterectomies.2,5-7 Figure 2. Pharmacological Treatments &XPXODWLYH3HUFHQWDJH • OBJECTIVE • To describe treatment patterns and diagnostic pathways for women with uterine fibroids in the three years following a new diagnosis. METHODS %DVHOLQH <HDU • <HDUV )ROORZ8S3HULRG Data Sources • <HDUV Truven Health MarketScan® Commercial Database 3UHVFULSWLRQ16$,'V — Contains medical and prescription data on approximately 35 million US employees annually and their dependents with employer-sponsored private health insurance. +RUPRQDOELUWKFRQWUROLQFOXGHV,8' *RQDGRWURSLQUHOHDVLQJKRUPRQHDJRQLVWV MarketScan Medicare Supplemental Database — Contains medical and prescription data for approximately 3 million retirees annually with Medicare supplemental insurance paid for by employers. — Includes the Medicare-covered portion of payment (coordination of benefits amount, or COB) and the employer-paid portion. Figure 3. Non-Pharmacological Treatments Patient Selection The MarketScan Commercial and Medicare Supplemental Databases were used to identify women with a new diagnosis of uterine fibroids (index event, ICD-9-CM code 218.9) from 2004 to 2013. • Women were required to have 12 months pre- and 12, 24, or 36 months of post-index continuous enrollment (the 12-month period prior to the index date was designated the baseline period) • Patients with any diagnosis of uterine fibroids or polyps (ICD-9-CM code 621.0) in the baseline period were excluded; thus, the index event diagnosis represented a new diagnosis for patients included in the analysis. &XPXODWLYH3HUFHQWDJH • Treatment Pattern Description • The use of diagnostic procedures, pharmacologic treatments, and non-pharmacologic treatments, as identified by administrative claims, were measured in the 12-month baseline period and the following 12, 24, and 36 months after the initial uterine fibroid diagnosis. • Patients could use multiple medications or procedures throughout the study period. ANALYSIS RESULTS Demographics • A total of 359,672 patients with 12 months of follow-up met the selection criteria. • Mean age at diagnosis was 46.1 years (SD=9.3). — Samples with longer follow-up: 24 months, N = 244,827; 36 months, N = 164,645. <HDU <HDUV — Age groups: 22.8% were <40; 45.8% were 40–49; 31.3% were ≥50. )ROORZ8S3HULRG Imaging Procedures • • <HDUV The most common imaging procedures during the three years after uterine fibroid diagnosis were transvaginal ultrasounds, abdominal/pelvic ultrasounds, computerized tomography, and pelvic magnetic resonance imaging (Figure 1). +\VWHURVFRSLFP\RPHFWRP\ /DSDURVFRSLFURERWLFP\RPHFWRP\ $EGRPLQDOP\RPHFWRP\ (QGRPHWULDODEODWLRQ +\VWHUHFWRP\ &XUHWWDJHFHUYL[RUXWHUXV Hysterosonography, hysterosalpingography, and hysteroscopy, were each performed in less than 5% of women in all follow-up timeframes. Pharmacological Treatment • The most commonly prescribed pharmacological treatment was prescription NSAIDs; the proportion of women receiving this treatment increased during the three years of follow-up, so a direct relationship between NSAIDs for fibroid-related complications versus other possibilities cannot be determined. Hormonal contraceptives (including intrauterine devices) and gonadotropin-releasing hormone agents were the next most common prescription therapy, and utilization appeared to remain steady in the 36 months following the uterine fibroid diagnosis (Figure 2). DISCUSSION • Many minimally invasive procedures are available for the treatment of uterine fibroids, yet approximately one in three women diagnosed with uterine fibroids will undergo a hysterectomy within the first year of a uterine fibroid diagnosis. • Hysterectomy was the most commonly performed procedure in the years following uterine fibroid diagnosis, increasing from 29.3% in the first year to 35.5% after three years (Figure 3). Hysterectomy is less commonly performed among women diagnosed before the age of 40 compared to women past peak childbearing years, although the rate is still substantial considering that fertility-sparing treatments are available. • — The proportion of women undergoing hysterectomy within one year of diagnosis in each age group was: <40years old, 21.9%; 40–49 years old, 35.7%; and ≥50 years old, 25.4%. This treatment patterns study shows that minimally invasive procedures were not commonly used in this patient population (<7% for a single modality within three years of initial diagnosis). • Increasing the utilization of minimally invasive procedures may reduce the clinical and economic burden of treating uterine fibroids. Non-Pharmacological Treatments • — The proportion of hysterectomies performed in conjunction with removal of leiomyoma (CPT code 58572 or 58290) was 1.9%. — Approximately 1% of women undergoing hysterectomy had a prior myomectomy procedure (from the beginning of the baseline period to hysterectomy date). • Minimally invasive procedures were utilized at much lower rates than hysterectomy. • Within three years of diagnosis, 6.4% of women underwent endometrial ablation, 5.6% underwent curettage procedures, and 5.4% underwent myomectomy. • Overall, hysteroscopic myomectomy was the most common myomectomy procedure (2.5% in three years), followed by abdominal (2.1%) and laparoscopic/robotic (1.0%). Figure 1. Imaging Procedures &XPXODWLYH3HUFHQWDJH LIMITATIONS • Diagnostic and procedural coding are limited in their ability to capture disease severity as it relates to the necessity of hysterectomy versus a minimally invasive approach. — The data sources used do not contain information on potential comorbidities or fibroid location, volume, or severity. These factors would impact the necessity of hysterectomy. Future research should explore this further to identify the potential number of avoidable hysterectomy cases. • This analysis was conducted among women with commercial health insurance in the US and may not apply to other patient populations, including patients with Medicaid, the uninsured, or women with full Medicare. REFERENCES %DVHOLQH <HDU <HDUV <HDUV )ROORZ8S3HULRG Ultrasound,transvaginal Ultrasound,abdominal/pelvic Computerizedtomography(pelvis) Magneticresonanceimaging(pelvis) MISC-03349-001 Hologic Inc. 1. Okolo S. Incidence, aetiology and epidemiology of uterine fibroids. Best Practice & Research. Clinical Obstetrics & Gynaecology Aug 2008; 22(4): 571–588. 2. Hirst A, Dutton S, Wu O, et al. A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study. Health Technology Assessment Mar 2008; 12(5): 1–248, iii. 3. Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. International Journal of Women's Health 2014; 6: 95–114. 4. Zimmermann A, Bernuit D, Gerlinger C, Schaefers M, Geppert K. Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Women's Health 2012; 12: 6. 5. Smeets AJ, Nijenhuis RJ, Boekkooi PF, et al. Safety and effectiveness of uterine artery embolization in patients with pedunculated fibroids. Journal of Vascular and Interventional Radiology: JVIR Sep 2009; 20(9): 1172–1175. 6. Scheurig-Muenkler C, Lembcke A, Froeling V, Maurer M, Hamm B, Kroencke TJ. Uterine artery embolization for symptomatic fibroids: long-term changes in disease-specific symptoms and quality of life. Human Reproduction Aug 2011; 26(8): 2036–2042. 7. Fennessy FM, Kong CY, Tempany CM, Swan JS. Quality-of-life assessment of fibroid treatment options and outcomes. Radiology Jun 2011; 259(3): 785–792. This study was funded by Hologic, Inc